User login
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
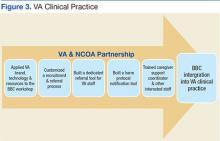
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.