User login
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
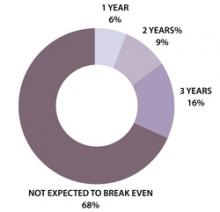
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH