User login
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
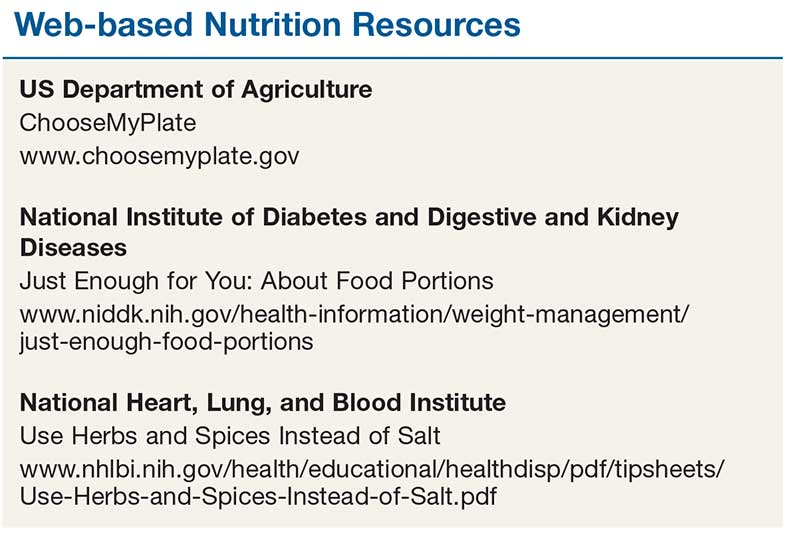
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.