User login
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
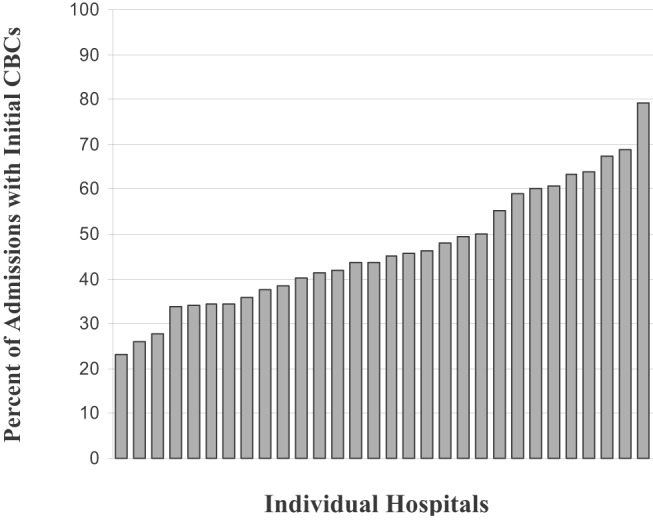
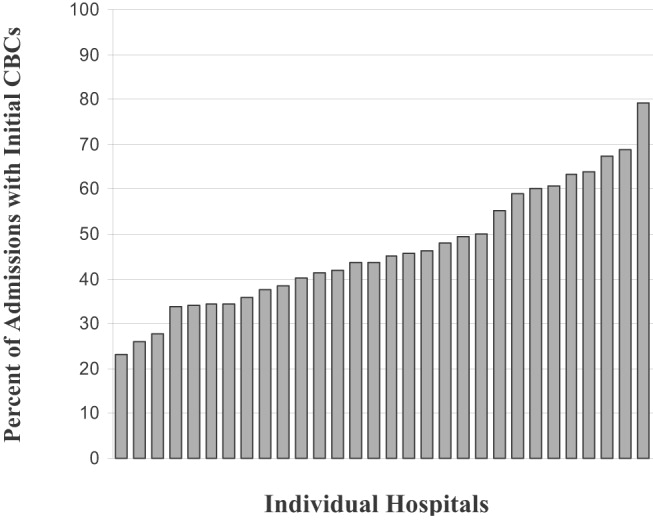
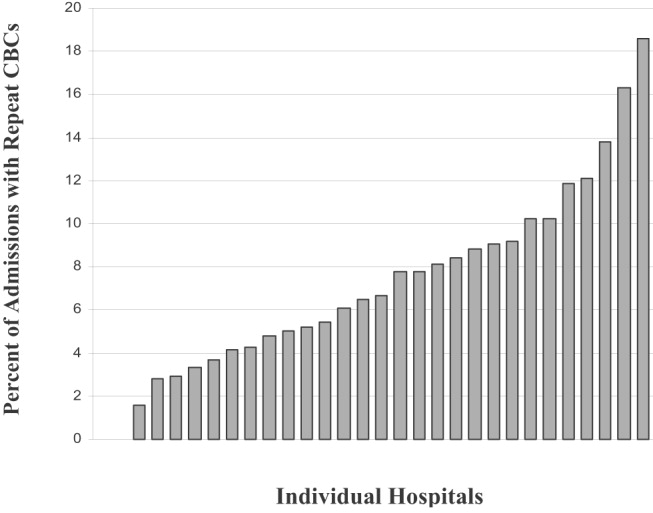
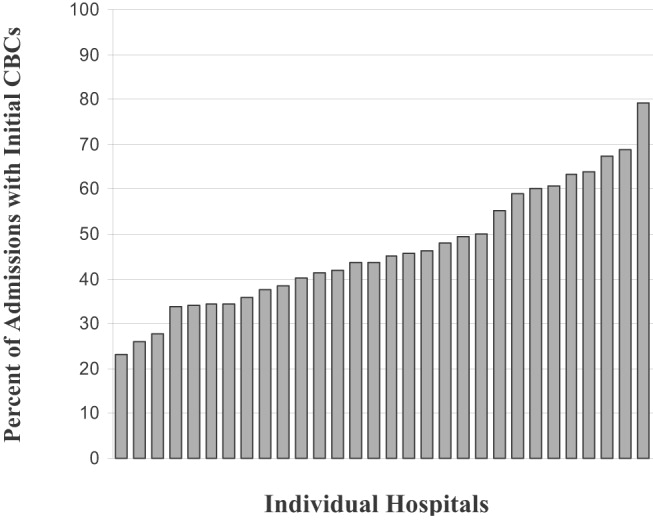
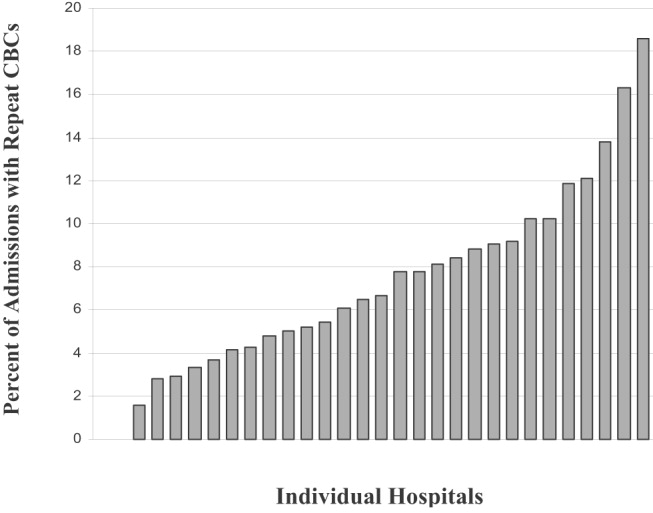
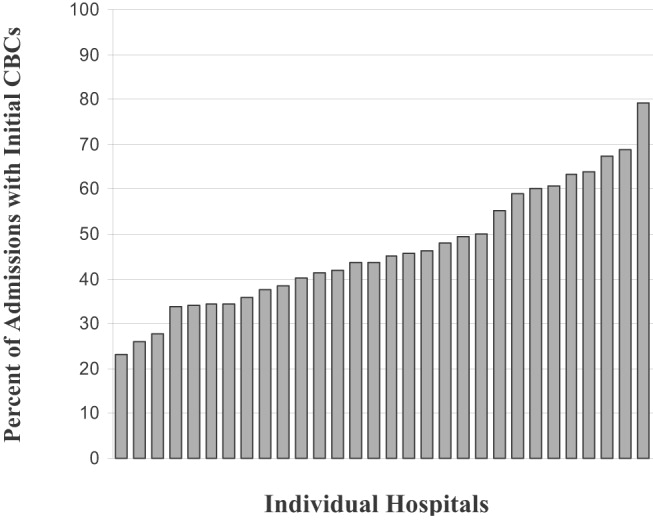
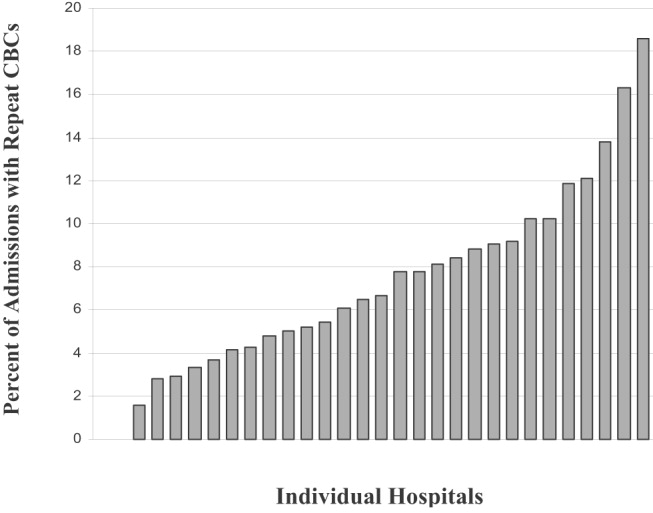
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
Copyright © 2007 Society of Hospital Medicine