User login
A 48-year-old man presents to your office for follow-up of right knee pain that has been bothering him for the past 12 months. He denies any trauma or inciting incident for the pain. On physical exam, he does not have crepitus but does have medial joint line tenderness of his right knee. An MRI shows a partial medial meniscal tear. Do you refer him to physical therapy (PT) or to orthopedics for arthroscopy and repair?
The meniscus—cartilage in the knee joint that provides support, stability, and lubrication to the joint during activity—can tear during a traumatic event or as a result of degeneration over time. Traumatic meniscal tears typically occur in those younger than 30 during sports (eg, basketball, soccer), whereas degenerative meniscal tears generally occur in patients ages 40 to 60.2,3 The annual incidence of all meniscal tears is 79 per 100,000.4 While some clinicians can diagnose traumatic meniscal tears based on history and physical examination, degenerative meniscal tears are more challenging and typically warrant an MRI for confirmation.3
Meniscal tears can be treated either conservatively, with supportive care and exercise, or surgically. Unfortunately, there are no national orthopedic guidelines available to help direct care. In one observational study, 95 of 117 patients (81.2%) were generally satisfied with surgical treatment at four-year follow-up; satisfaction was higher among those with a traumatic meniscal tear than in those with a degenerative tear.5
Two systematic reviews of surgery versus nonoperative management or sham therapies found no additional benefit of surgery for meniscal tears in a variety of patients with and without osteoarthritis.6,7 However, both studies were of only moderate quality, because of the number of patients in the nonoperative groups who ultimately underwent surgery. Neither of the studies directly compared surgery to nonoperative management.6,7Another investigation—a multicenter, randomized, double-blind, sham-controlled study conducted in Finland involving 1
Clinical practice recommendations devised from a vast systematic review of the literature recommend that the decision for surgery be based on patient-specific factors, such as symptoms, age, mechanism of tear, extent of damage, and occupational/social/activity needs.9
STUDY SUMMARY
Exercise is as good as surgery
The current superiority RCT compared exercise therapy to arthroscopic partial meniscectomy. Subjects (ages 35 to 60) presented to the orthopedic department of two hospitals in Norway with unilateral knee pain of more than two months’ duration and an MRI-delineated medial meniscal tear. They were included in the study only if they had radiographic evidence of minimal osteoarthritis (Kellgren-Lawrence classification grade ≤ 2). Exclusion criteria included acute trauma, locked knee, ligament injury, and knee surgery in the same knee within the previous two years.
The primary outcomes were change in patient-reported knee function (as determined by overall Knee injury and Osteoarthritis Outcome Score [KOOS] after two years) and thigh muscle strength at three months (as measured by physiotherapists). The researchers used four of the five KOOS subscales for this analysis: pain, other symptoms (swelling, grinding/noise from the joint, ability to straighten and bend), function in sports/recreation, and knee-related quality of life (QOL). The average score of each subscale was used.
Secondary outcomes included the five individual KOOS subscales (the four previously mentioned, plus activities of daily living [ADLs]), as well as thigh muscle strength and lower-extremity performance test results.
Methods. Testing personnel were blinded to group allocation; participants wore pants or neoprene sleeves to cover surgical scars. A total of 140 patients were randomized to either 12 weeks (24-36 sessions) of exercise therapy alone or a standardized arthroscopic partial meniscectomy; upon discharge, those in the latter group received written and oral encouragement to perform simple exercises at home, two to four times daily, to regain range of motion and reduce swelling.
Results. At two years, the overall mean improvement in KOOS4 score from baseline was similar between the exercise group and the meniscectomy group (25.3 pts vs 24.4 pts, respectively; mean difference [MD], 0.9). Additionally, muscle strength (measured as peak torque flexion and extension and total work flexion and extension) at both three and 12 months showed significant objective improvements favoring exercise therapy.
In the secondary analysis of the KOOS subscale scores, change from baseline was nonsignificant for four of the five (pain, ADL, sports/recreation, and QOL). Only the symptoms subscale had a significant difference favoring exercise therapy (MD, 5.3 pts); this was likely clinically insignificant on a grading scale of 0 to 100.
Of the patients allocated to exercise therapy alone, 19% crossed over and underwent surgery during the two-year study period.
WHAT’S NEW
Head-to-head comparison adds evidence
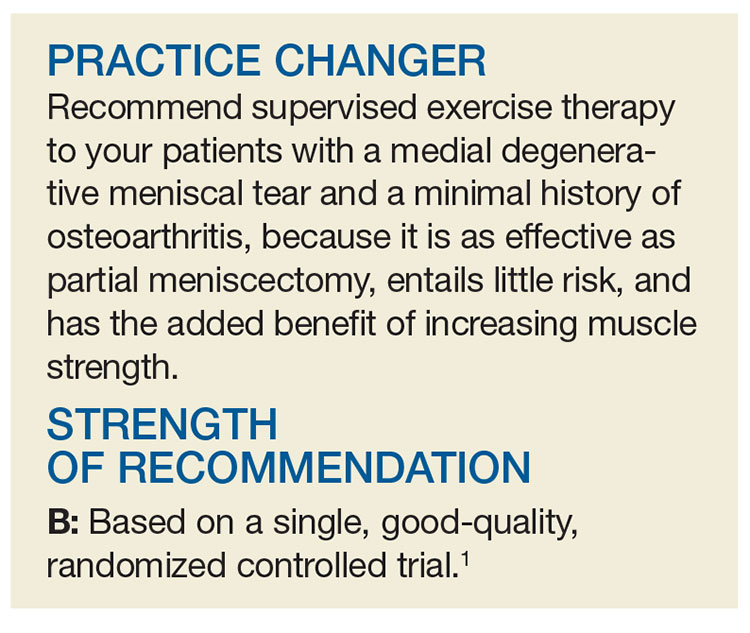
This is the first trial to directly compare exercise therapy to surgery in patients with meniscal tears. Interestingly, exercise therapy was as effective after a two-year follow-up period and was superior in the short term for thigh muscle strength.1
The results of this study build on those from the aforementioned smaller study conducted in Finland.8 In that study, both groups received instruction for the same graduated exercise plan. The researchers found that exercise was comparable to surgery for meniscal tears in patients with no osteoarthritis.
CAVEATS
What about more severe osteoarthritis?
This trial included patients with no to mild osteoarthritis in addition to their meniscal tear.1 It is unclear if the results would be maintained in those with more advanced disease. Additionally, 19% of patients crossed over from the exercise group to the surgery group, even though muscle strength improved. Therefore, education about the risks of surgery and the potential lack of benefit is important.
CHALLENGES TO IMPLEMENTATION
Cost and effort of PT
The cost of PT can be a barrier for patients who have adequate insurance coverage for surgery but inadequate coverage for PT. Additionally, exercise therapy requires significant and ongoing time and effort, which may deter those with busy lifestyles. Patients and clinicians may view surgery as an “easier” fix.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[4]:250-252).
1. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740.
2. Beals CT, Magnussen RA, Graham WC, et al. The prevalence of meniscal pathology in asymptomatic athletes. Sports Med. 2016;46:1517-1524.
3. Maffulli N, Longo UG, Campi S, et al. Meniscal tears. Open Access J Sports Med. 2010;1:45-54.
4. Peat G, Bergknut C, Frobell R, et al. Population-wide incidence estimates for soft tissue knee injuries presenting to healthcare in southern Sweden: data from the Skåne Healthcare Register. Arthritis Res Ther. 2014;16:R162.
5. Ghislain NA, Wei JN, Li YG. Study of the clinical outcome between traumatic and degenerative (non-traumatic) meniscal tears after arthroscopic surgery: a 4-years follow-up study. J Clin Diagn Res. 2016;10:RC01-RC04.
6. Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186:1057-1064.
7. Monk P, Garfjeld Roberts P, Palmer AJ, et al. The urgent need for evidence in arthroscopic meniscal surgery: a systematic review of the evidence for operative management of meniscal tears. Am J Sports Med. 2017;45:965-973.
8. Sihvonen R, Paavola M, Malmivaara A, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515-2524.
9. Beaufils P, Hulet C, Dhénain M, et al. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437-442.
A 48-year-old man presents to your office for follow-up of right knee pain that has been bothering him for the past 12 months. He denies any trauma or inciting incident for the pain. On physical exam, he does not have crepitus but does have medial joint line tenderness of his right knee. An MRI shows a partial medial meniscal tear. Do you refer him to physical therapy (PT) or to orthopedics for arthroscopy and repair?
The meniscus—cartilage in the knee joint that provides support, stability, and lubrication to the joint during activity—can tear during a traumatic event or as a result of degeneration over time. Traumatic meniscal tears typically occur in those younger than 30 during sports (eg, basketball, soccer), whereas degenerative meniscal tears generally occur in patients ages 40 to 60.2,3 The annual incidence of all meniscal tears is 79 per 100,000.4 While some clinicians can diagnose traumatic meniscal tears based on history and physical examination, degenerative meniscal tears are more challenging and typically warrant an MRI for confirmation.3
Meniscal tears can be treated either conservatively, with supportive care and exercise, or surgically. Unfortunately, there are no national orthopedic guidelines available to help direct care. In one observational study, 95 of 117 patients (81.2%) were generally satisfied with surgical treatment at four-year follow-up; satisfaction was higher among those with a traumatic meniscal tear than in those with a degenerative tear.5
Two systematic reviews of surgery versus nonoperative management or sham therapies found no additional benefit of surgery for meniscal tears in a variety of patients with and without osteoarthritis.6,7 However, both studies were of only moderate quality, because of the number of patients in the nonoperative groups who ultimately underwent surgery. Neither of the studies directly compared surgery to nonoperative management.6,7Another investigation—a multicenter, randomized, double-blind, sham-controlled study conducted in Finland involving 1
Clinical practice recommendations devised from a vast systematic review of the literature recommend that the decision for surgery be based on patient-specific factors, such as symptoms, age, mechanism of tear, extent of damage, and occupational/social/activity needs.9
STUDY SUMMARY
Exercise is as good as surgery
The current superiority RCT compared exercise therapy to arthroscopic partial meniscectomy. Subjects (ages 35 to 60) presented to the orthopedic department of two hospitals in Norway with unilateral knee pain of more than two months’ duration and an MRI-delineated medial meniscal tear. They were included in the study only if they had radiographic evidence of minimal osteoarthritis (Kellgren-Lawrence classification grade ≤ 2). Exclusion criteria included acute trauma, locked knee, ligament injury, and knee surgery in the same knee within the previous two years.
The primary outcomes were change in patient-reported knee function (as determined by overall Knee injury and Osteoarthritis Outcome Score [KOOS] after two years) and thigh muscle strength at three months (as measured by physiotherapists). The researchers used four of the five KOOS subscales for this analysis: pain, other symptoms (swelling, grinding/noise from the joint, ability to straighten and bend), function in sports/recreation, and knee-related quality of life (QOL). The average score of each subscale was used.
Secondary outcomes included the five individual KOOS subscales (the four previously mentioned, plus activities of daily living [ADLs]), as well as thigh muscle strength and lower-extremity performance test results.
Methods. Testing personnel were blinded to group allocation; participants wore pants or neoprene sleeves to cover surgical scars. A total of 140 patients were randomized to either 12 weeks (24-36 sessions) of exercise therapy alone or a standardized arthroscopic partial meniscectomy; upon discharge, those in the latter group received written and oral encouragement to perform simple exercises at home, two to four times daily, to regain range of motion and reduce swelling.
Results. At two years, the overall mean improvement in KOOS4 score from baseline was similar between the exercise group and the meniscectomy group (25.3 pts vs 24.4 pts, respectively; mean difference [MD], 0.9). Additionally, muscle strength (measured as peak torque flexion and extension and total work flexion and extension) at both three and 12 months showed significant objective improvements favoring exercise therapy.
In the secondary analysis of the KOOS subscale scores, change from baseline was nonsignificant for four of the five (pain, ADL, sports/recreation, and QOL). Only the symptoms subscale had a significant difference favoring exercise therapy (MD, 5.3 pts); this was likely clinically insignificant on a grading scale of 0 to 100.
Of the patients allocated to exercise therapy alone, 19% crossed over and underwent surgery during the two-year study period.
WHAT’S NEW
Head-to-head comparison adds evidence
This is the first trial to directly compare exercise therapy to surgery in patients with meniscal tears. Interestingly, exercise therapy was as effective after a two-year follow-up period and was superior in the short term for thigh muscle strength.1
The results of this study build on those from the aforementioned smaller study conducted in Finland.8 In that study, both groups received instruction for the same graduated exercise plan. The researchers found that exercise was comparable to surgery for meniscal tears in patients with no osteoarthritis.
CAVEATS
What about more severe osteoarthritis?
This trial included patients with no to mild osteoarthritis in addition to their meniscal tear.1 It is unclear if the results would be maintained in those with more advanced disease. Additionally, 19% of patients crossed over from the exercise group to the surgery group, even though muscle strength improved. Therefore, education about the risks of surgery and the potential lack of benefit is important.
CHALLENGES TO IMPLEMENTATION
Cost and effort of PT
The cost of PT can be a barrier for patients who have adequate insurance coverage for surgery but inadequate coverage for PT. Additionally, exercise therapy requires significant and ongoing time and effort, which may deter those with busy lifestyles. Patients and clinicians may view surgery as an “easier” fix.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[4]:250-252).
A 48-year-old man presents to your office for follow-up of right knee pain that has been bothering him for the past 12 months. He denies any trauma or inciting incident for the pain. On physical exam, he does not have crepitus but does have medial joint line tenderness of his right knee. An MRI shows a partial medial meniscal tear. Do you refer him to physical therapy (PT) or to orthopedics for arthroscopy and repair?
The meniscus—cartilage in the knee joint that provides support, stability, and lubrication to the joint during activity—can tear during a traumatic event or as a result of degeneration over time. Traumatic meniscal tears typically occur in those younger than 30 during sports (eg, basketball, soccer), whereas degenerative meniscal tears generally occur in patients ages 40 to 60.2,3 The annual incidence of all meniscal tears is 79 per 100,000.4 While some clinicians can diagnose traumatic meniscal tears based on history and physical examination, degenerative meniscal tears are more challenging and typically warrant an MRI for confirmation.3
Meniscal tears can be treated either conservatively, with supportive care and exercise, or surgically. Unfortunately, there are no national orthopedic guidelines available to help direct care. In one observational study, 95 of 117 patients (81.2%) were generally satisfied with surgical treatment at four-year follow-up; satisfaction was higher among those with a traumatic meniscal tear than in those with a degenerative tear.5
Two systematic reviews of surgery versus nonoperative management or sham therapies found no additional benefit of surgery for meniscal tears in a variety of patients with and without osteoarthritis.6,7 However, both studies were of only moderate quality, because of the number of patients in the nonoperative groups who ultimately underwent surgery. Neither of the studies directly compared surgery to nonoperative management.6,7Another investigation—a multicenter, randomized, double-blind, sham-controlled study conducted in Finland involving 1
Clinical practice recommendations devised from a vast systematic review of the literature recommend that the decision for surgery be based on patient-specific factors, such as symptoms, age, mechanism of tear, extent of damage, and occupational/social/activity needs.9
STUDY SUMMARY
Exercise is as good as surgery
The current superiority RCT compared exercise therapy to arthroscopic partial meniscectomy. Subjects (ages 35 to 60) presented to the orthopedic department of two hospitals in Norway with unilateral knee pain of more than two months’ duration and an MRI-delineated medial meniscal tear. They were included in the study only if they had radiographic evidence of minimal osteoarthritis (Kellgren-Lawrence classification grade ≤ 2). Exclusion criteria included acute trauma, locked knee, ligament injury, and knee surgery in the same knee within the previous two years.
The primary outcomes were change in patient-reported knee function (as determined by overall Knee injury and Osteoarthritis Outcome Score [KOOS] after two years) and thigh muscle strength at three months (as measured by physiotherapists). The researchers used four of the five KOOS subscales for this analysis: pain, other symptoms (swelling, grinding/noise from the joint, ability to straighten and bend), function in sports/recreation, and knee-related quality of life (QOL). The average score of each subscale was used.
Secondary outcomes included the five individual KOOS subscales (the four previously mentioned, plus activities of daily living [ADLs]), as well as thigh muscle strength and lower-extremity performance test results.
Methods. Testing personnel were blinded to group allocation; participants wore pants or neoprene sleeves to cover surgical scars. A total of 140 patients were randomized to either 12 weeks (24-36 sessions) of exercise therapy alone or a standardized arthroscopic partial meniscectomy; upon discharge, those in the latter group received written and oral encouragement to perform simple exercises at home, two to four times daily, to regain range of motion and reduce swelling.
Results. At two years, the overall mean improvement in KOOS4 score from baseline was similar between the exercise group and the meniscectomy group (25.3 pts vs 24.4 pts, respectively; mean difference [MD], 0.9). Additionally, muscle strength (measured as peak torque flexion and extension and total work flexion and extension) at both three and 12 months showed significant objective improvements favoring exercise therapy.
In the secondary analysis of the KOOS subscale scores, change from baseline was nonsignificant for four of the five (pain, ADL, sports/recreation, and QOL). Only the symptoms subscale had a significant difference favoring exercise therapy (MD, 5.3 pts); this was likely clinically insignificant on a grading scale of 0 to 100.
Of the patients allocated to exercise therapy alone, 19% crossed over and underwent surgery during the two-year study period.
WHAT’S NEW
Head-to-head comparison adds evidence
This is the first trial to directly compare exercise therapy to surgery in patients with meniscal tears. Interestingly, exercise therapy was as effective after a two-year follow-up period and was superior in the short term for thigh muscle strength.1
The results of this study build on those from the aforementioned smaller study conducted in Finland.8 In that study, both groups received instruction for the same graduated exercise plan. The researchers found that exercise was comparable to surgery for meniscal tears in patients with no osteoarthritis.
CAVEATS
What about more severe osteoarthritis?
This trial included patients with no to mild osteoarthritis in addition to their meniscal tear.1 It is unclear if the results would be maintained in those with more advanced disease. Additionally, 19% of patients crossed over from the exercise group to the surgery group, even though muscle strength improved. Therefore, education about the risks of surgery and the potential lack of benefit is important.
CHALLENGES TO IMPLEMENTATION
Cost and effort of PT
The cost of PT can be a barrier for patients who have adequate insurance coverage for surgery but inadequate coverage for PT. Additionally, exercise therapy requires significant and ongoing time and effort, which may deter those with busy lifestyles. Patients and clinicians may view surgery as an “easier” fix.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[4]:250-252).
1. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740.
2. Beals CT, Magnussen RA, Graham WC, et al. The prevalence of meniscal pathology in asymptomatic athletes. Sports Med. 2016;46:1517-1524.
3. Maffulli N, Longo UG, Campi S, et al. Meniscal tears. Open Access J Sports Med. 2010;1:45-54.
4. Peat G, Bergknut C, Frobell R, et al. Population-wide incidence estimates for soft tissue knee injuries presenting to healthcare in southern Sweden: data from the Skåne Healthcare Register. Arthritis Res Ther. 2014;16:R162.
5. Ghislain NA, Wei JN, Li YG. Study of the clinical outcome between traumatic and degenerative (non-traumatic) meniscal tears after arthroscopic surgery: a 4-years follow-up study. J Clin Diagn Res. 2016;10:RC01-RC04.
6. Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186:1057-1064.
7. Monk P, Garfjeld Roberts P, Palmer AJ, et al. The urgent need for evidence in arthroscopic meniscal surgery: a systematic review of the evidence for operative management of meniscal tears. Am J Sports Med. 2017;45:965-973.
8. Sihvonen R, Paavola M, Malmivaara A, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515-2524.
9. Beaufils P, Hulet C, Dhénain M, et al. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437-442.
1. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740.
2. Beals CT, Magnussen RA, Graham WC, et al. The prevalence of meniscal pathology in asymptomatic athletes. Sports Med. 2016;46:1517-1524.
3. Maffulli N, Longo UG, Campi S, et al. Meniscal tears. Open Access J Sports Med. 2010;1:45-54.
4. Peat G, Bergknut C, Frobell R, et al. Population-wide incidence estimates for soft tissue knee injuries presenting to healthcare in southern Sweden: data from the Skåne Healthcare Register. Arthritis Res Ther. 2014;16:R162.
5. Ghislain NA, Wei JN, Li YG. Study of the clinical outcome between traumatic and degenerative (non-traumatic) meniscal tears after arthroscopic surgery: a 4-years follow-up study. J Clin Diagn Res. 2016;10:RC01-RC04.
6. Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186:1057-1064.
7. Monk P, Garfjeld Roberts P, Palmer AJ, et al. The urgent need for evidence in arthroscopic meniscal surgery: a systematic review of the evidence for operative management of meniscal tears. Am J Sports Med. 2017;45:965-973.
8. Sihvonen R, Paavola M, Malmivaara A, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515-2524.
9. Beaufils P, Hulet C, Dhénain M, et al. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437-442.