User login
ANSWER
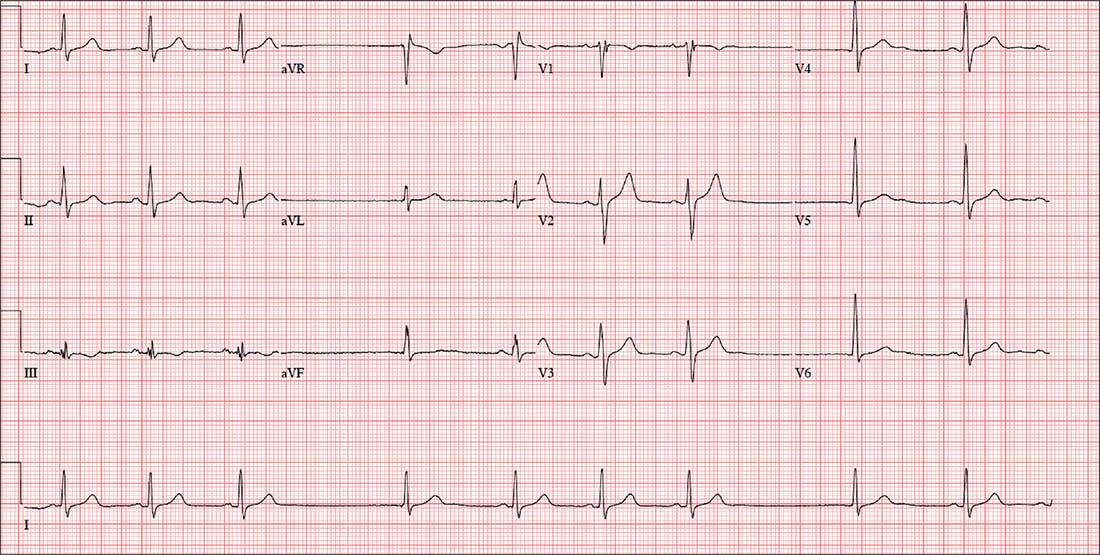
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
ANSWER
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
ANSWER
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
For four days, a 66-year-old man with New York Heart Association Class II congestive heart failure has been short of breath. Over the three years he has been your patient, he has generally done well on maximum medical therapy. He has never had a myocardial infarction (MI), atrial fibrillation, or symptoms suggestive of ischemia.
Three months ago, he was hospitalized following a robust meal. At the time, his left ventricular ejection fraction was 42% on echocardiogram, and he was in normal sinus rhythm; he responded quickly to diuresis. This time, he says, he feels “different.” He’s tired and lethargic, he can’t seem to catch his breath, and he just wants to sleep.
Medical history is remarkable for type 2 diabetes and cholecystitis. Surgical history includes a cholecystectomy and an open reduction and internal fixation of a right high ankle fracture. His current medications include metformin, lisinopril, metoprolol, spironolactone, furosemide, potassium chloride, and atorvastatin.
The patient, an accountant at a busy firm, is married with three healthy adult children. He has never smoked, and he drinks alcohol rarely on weekends. His father died during cardiac revascularization surgery at age 58, his mother died of heart failure complications at age 69, and his older brother had an inferior MI at age 68.
Review of systems is remarkable for a recent upper respiratory infection. The patient has also noticed that his abdomen seems distended and his urine output has diminished.
Vital signs include a blood pressure of 98/62 mm Hg; pulse, 50 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 97.6°F. His weight is 224 lb—a 7-lb increase since his last clinic visit—and his height, 68 in.
On physical exam, you note a well-groomed male in mild distress. Pertinent findings include distended neck veins with visible cannon waves and jugular venous distention to 10 cm. There are no carotid bruits. Auscultation of the chest reveals scattered rhonchi in all fields, with bilateral rales in both bases that do not clear with coughing.
Cardiac exam reveals a regular rhythm at a rate of 58 beats/min, with a grade II/VI systolic murmur best heard at the left sternal border. There are no gallops or clicks. On abdominal exam, the liver edge is palpable 2 cm below the right costal margin. Bowel tones are present in all quadrants. There is no hepatojugular reflux or tenderness.
The lower extremities have 3+ pitting edema below the knees. Peripheral pulses are present and equal bilaterally, and there is no cyanosis or clubbing. The neurologic exam reveals mild sensory loss in both feet, with no perception of 2-point discrimination in the toes of the left foot.
An ECG reveals a ventricular rate of 55 beats/min; PR interval, 146 ms; QRS duration, 122 ms; QT/QTc interval, 424/405 ms; P axis, 60°; R axis, 38°; and T axis, 29°. What is your interpretation?