User login

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
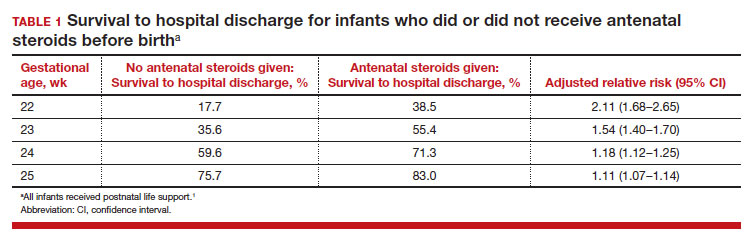
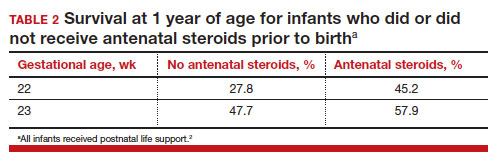
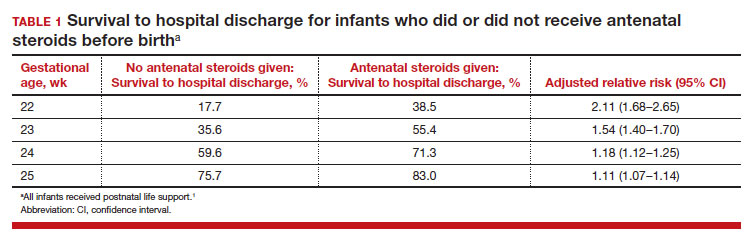
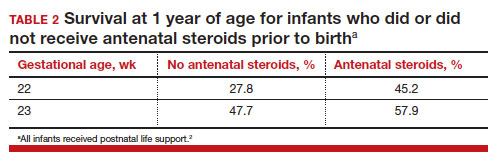
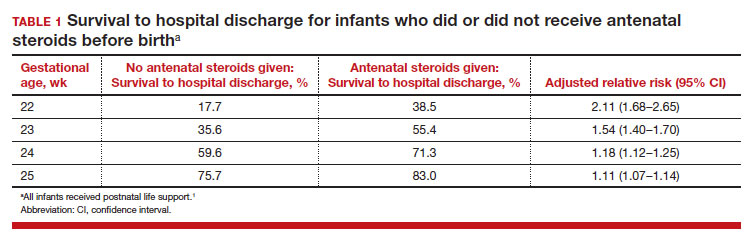
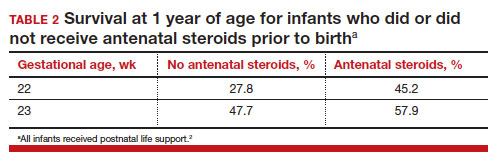
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
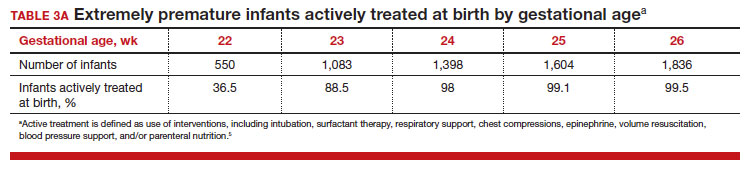
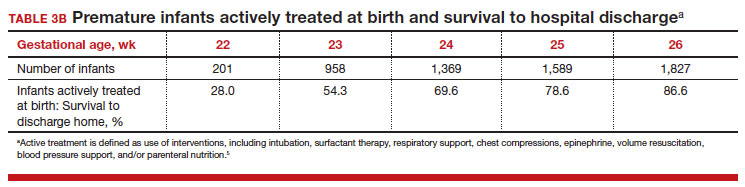
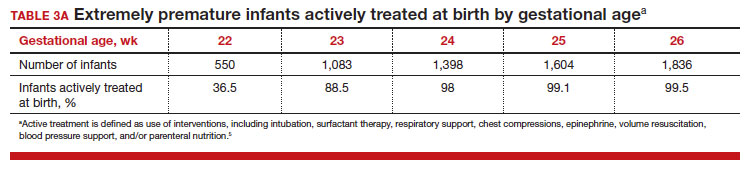
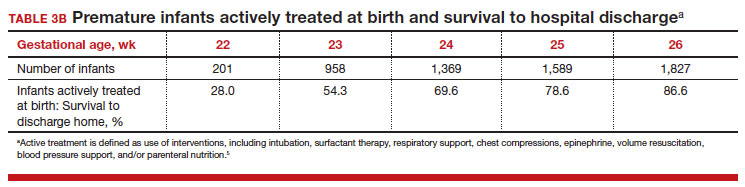
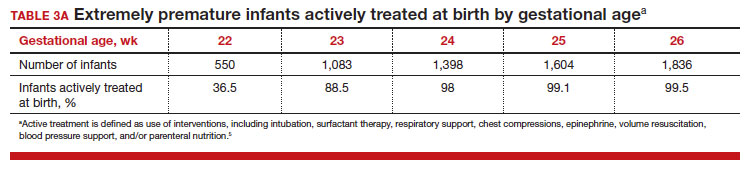
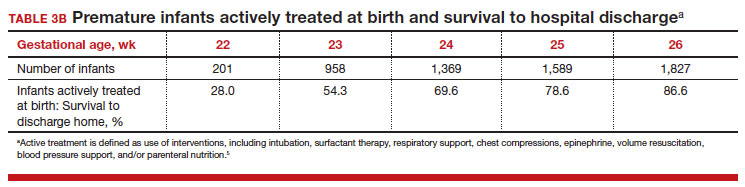
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.

