User login
› Order an emergent magnetic resonance imaging scan to rule out epidural hematoma for patients with severe focal acute back pain that presents with limb dysesthesia, thoracic radiculopathy, or an unusual clinical course. A
Strength of recommendation (SOR)
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case-series
CASE A 34-year-old, otherwise healthy man presented at our emergency department (ED) complaining of severe, acute,high-thoracic back pain. He had left-sided chest pain radiating to his left arm and nonspecific paresthesias that did not track along a specific dermatome. The pain started 2 days earlier while the patient was lifting a heavy object at work. He was initially seen by his family physician, who diagnosed acute back pain, prescribed a COX-2 selective nonsteroidal anti-inflammatory agent, and advised him to stay home from work. This treatment did not improve the patient’s pain, which became more severe shortly before his arrival in our ED.
On physical examination, we found the patient in general good health, with no evidence of distress. His blood pressure was 128/78 mm Hg, his respiratory rate was 16 breaths/min,and his oral temperature was 36.5°C (97.7°F). An electrocardiogram(EKG) showed a normal sinus rhythm with no evidence of ischemia. Troponin I was 0 ng/mL, and complete blood count,C-reactive protein, and erythrocyte sedimentation rate were within normal range. After observation, the patient was discharged for ambulatory follow-up, with a diagnosis of acute back pain and nonischemic chest pain.
Two days later, the patient returned to the ED. He said that the pain had not gotten better, and he reported the gradual development of numbness in both legs, along with urinary retention. Re-examination revealed an ASIA D paraplegia at T4,with 650 mL postvoid residual urine volume. (ASIA D paraplegia means no sensory loss below the level of the injury and a motorfunction score above 3/5, which indicates active joint movement is possible against gravity but not against resistance.)
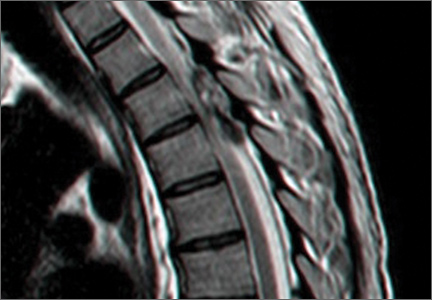
An emergent magnetic resonance imaging (MRI) scan was ordered; it revealed a large left-sided epidural mass spanning the length of T4 and T5 vertebrae with severe cord displacement and compression (FIGURE 1). On a T1-weighted MRI, the mass appeared hyperintense only on the periphery,indicating the presence of extracellular methemoglobin—a radiographic manifestation of early subacute hemorrhage.1
Surgery. We started the patient on IV dexamethasone and performed an urgent T3-T5 laminectomy, which revealed a large brown epidural mass adhering to the duramater (FIGURE 2). We removed the mass and sent it to pathology, which confirmed an epidural hematoma.
The patient’s postoperative course was uneventful, and he was discharged from the hospital with complete motor strength in both legs and complete urinary control. The patient rapidly regained all sensory function, and we re-examined him one month postop in our outpatient clinic. He was intact neurologically and completely free of pain and dysesthesia. A follow-up MRI 3 months postop revealed no residual compression or signal abnormalities within the spinal cord.
Diagnosis remains a challenge
Spinal epidural hematoma (SEH) is an uncommon entity, with an estimated incidence of 0.1/100,000 per year.2 Because there are no studies that look at a large series of patients in the literature, our knowledge of the disorder is limited to case reports and small case series.
In most reports, SEH is linked to predisposing factors such as an underlying coagulopathy or anticoagulant therapy, epidural venous malformation, spinal trauma, inflammatory spine disease, pregnancy or neoplastic encroachment, and bleeding into the spinal canal.3 Spontaneous spinal epidural hematoma (SSEH) with no recognizable underlying predisposing factor is even rarer,4 and the paucity of published data makes it difficult to estimate the true incidence.
In the largest study to date, Zhong etal5 found 7 of 30 cases of SSEH were not associated with bleeding risk factors, making the calculated incidence approximately 0.023/100,000 per year. However, it is impossible to estimate how many cases remain undetected because neurological loss does not occur, and the pain is labeled a nonspecific backache that resolves spontaneously.
The typical patient will present with nothing more than severe midline spinal pain located anywhere from the head to the buttocks. Patients with acute onset of axial back pain with no distinguishing signs or symptoms (“red flags”) are seen daily in every practice. Commonly accepted guidelines from the American College of Physicians (ACP) and the American Pain Society (APS) direct the physician away from MRI scanning that can confirm the diagnosis.6
As our patient’s case illustrates, acute pain in the axial spine is a very common complaint, and usually has a benign etiology. Compression of one or more of the exiting thoracic nerve roots can cause thoracic radiculopathy, which might confound the diagnosis even further and lead to an unnecessary cardiothoracic work-up.4 That was the case for our patient. Only when neurological loss is evident will the need for an MRI become clear, and the diagnosis became apparent.
Definitive treatment is elusive
Several authors advocate emergent surgical decompression and evacuation of the hematoma, because the neurological outcome could be catastrophic,7 resulting in complete quadri/paraplegia. This approach is equivocal, however, as spontaneous resolution of neurological symptoms has been described in many cases.1,7-11 Therefore, the decision whether to operate largely depends on the individual’s surgical risk factors and clinical course. In a high-risk patient who is improving neurologically, watchful waiting may be prudent, while in neurologically deteriorating low-risk cases little is lost with immediate surgical decompression.12
The prognosis of SSEH is also difficult to estimate. Several reports confirm that cervical and cervicothoracic hematomas carry a worse prognosis than thoracolumbar and lumbosacral hematomas.3,5 A rapid onset of neurological deterioration (less than12 hours) also heralds graver consequences, as does spinal cord edema on initial MRI.5
Two windows of opportunity
Two time periods stand out as possible course-changing opportunities for clinicians.The first occurs when the patient initially complains of an acute backache. At this point, ACP/APS guidelines direct us to look for red flags that focus attention on the more troubling etiologies for backache.6 Unfortunately, SSEH has no specific red flag, and itis misleading to suggest that such an esoteric diagnosis should routinely be considered.
A better approach would be to look for the unusual: very sharp, acute-onset, highly localized back pain that does not respond well to analgesics (TABLE [developed by NR]),along with any dysesthesia or unusual radicular complaint. A positive l’hermitte sign—anelectrical sensation that runs down the back and into the limbs—on physical examination might also warrant placing SSEH in the differential diagnosis.
The second time when swiftness might be crucial is from diagnosis to surgery. In a neurologically deteriorating patient, time is of utmost importance, and taking action at this juncture can produce a marked difference in the final outcome.3
CORRESPONDENCE
Nimrod Rahamimov, MD, Department of Orthopedics Band Spine Surgery, Western Galilee Hospital, PO Box 21, Naharia 22100, Israel; Nimrod.Rahamimov@naharia.health.gov.il
- Lipton ML. Totally Accessible MRI: A User’s Guide to Principles,Technology, and Applications. New York, NY: Springer; 2008.
- Taniguchi LU, Pahl FH, Lúcio JE, et al. Complete motor recoveryafter acute paraparesis caused by spontaneous spinal epiduralhematoma: case report. BMC Emerg Med. 2011;11:10.
- Binder DK, Sonne DC, Lawton MT. Spinal epidural hematoma.Neurosurg Q. 2004;14:51-59.
- Tsen AR, Burrows AM, Dumont TM, et al. Spinal epidural hematomamasquerading as atypical chest pain. Am J Emerg Med.2011;29:1236.e1-e3.
- Zhong W, Chen H, You C, et al. Spontaneous spinal epidural hematoma. J Clin Neurosci. 2011;18:1490-1494.
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of lowback pain: a joint clinical practice guideline from the AmericanCollege of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
- Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146:103-110.
- Subbiah M, Avadhani A, Shetty AP, et al. Acute spontaneouscervical epidural hematoma with neurological deficit after lowmolecular-weight heparin therapy: role of conservative management.Spine J. 2010;10:e11-e15.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of atraumatic cervicothoracic epidural hematoma presentingwith transient paraplegia: a case report. Spine (Phila Pa 1976). 2010;35:E564-E567.
- Sirin S, Arslan E, Yasar S, et al. Is spontaneous spinal epidural hematoma in elderly patients an emergency surgical case?Turk Neurosurg. 2010;20:557-560.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of tetraparesis because of postoperative cervical epidural hematoma.Spine J. 2010;10:e1-e5.
- Fleager K, Lee A, Cheng I, et al. Massive spontaneous epidural hematoma in a high-level swimmer: a case report. J Bone Joint Surg Am. 2010;92:2843-2846.
› Order an emergent magnetic resonance imaging scan to rule out epidural hematoma for patients with severe focal acute back pain that presents with limb dysesthesia, thoracic radiculopathy, or an unusual clinical course. A
Strength of recommendation (SOR)
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case-series
CASE A 34-year-old, otherwise healthy man presented at our emergency department (ED) complaining of severe, acute,high-thoracic back pain. He had left-sided chest pain radiating to his left arm and nonspecific paresthesias that did not track along a specific dermatome. The pain started 2 days earlier while the patient was lifting a heavy object at work. He was initially seen by his family physician, who diagnosed acute back pain, prescribed a COX-2 selective nonsteroidal anti-inflammatory agent, and advised him to stay home from work. This treatment did not improve the patient’s pain, which became more severe shortly before his arrival in our ED.
On physical examination, we found the patient in general good health, with no evidence of distress. His blood pressure was 128/78 mm Hg, his respiratory rate was 16 breaths/min,and his oral temperature was 36.5°C (97.7°F). An electrocardiogram(EKG) showed a normal sinus rhythm with no evidence of ischemia. Troponin I was 0 ng/mL, and complete blood count,C-reactive protein, and erythrocyte sedimentation rate were within normal range. After observation, the patient was discharged for ambulatory follow-up, with a diagnosis of acute back pain and nonischemic chest pain.
Two days later, the patient returned to the ED. He said that the pain had not gotten better, and he reported the gradual development of numbness in both legs, along with urinary retention. Re-examination revealed an ASIA D paraplegia at T4,with 650 mL postvoid residual urine volume. (ASIA D paraplegia means no sensory loss below the level of the injury and a motorfunction score above 3/5, which indicates active joint movement is possible against gravity but not against resistance.)
An emergent magnetic resonance imaging (MRI) scan was ordered; it revealed a large left-sided epidural mass spanning the length of T4 and T5 vertebrae with severe cord displacement and compression (FIGURE 1). On a T1-weighted MRI, the mass appeared hyperintense only on the periphery,indicating the presence of extracellular methemoglobin—a radiographic manifestation of early subacute hemorrhage.1
Surgery. We started the patient on IV dexamethasone and performed an urgent T3-T5 laminectomy, which revealed a large brown epidural mass adhering to the duramater (FIGURE 2). We removed the mass and sent it to pathology, which confirmed an epidural hematoma.
The patient’s postoperative course was uneventful, and he was discharged from the hospital with complete motor strength in both legs and complete urinary control. The patient rapidly regained all sensory function, and we re-examined him one month postop in our outpatient clinic. He was intact neurologically and completely free of pain and dysesthesia. A follow-up MRI 3 months postop revealed no residual compression or signal abnormalities within the spinal cord.
Diagnosis remains a challenge
Spinal epidural hematoma (SEH) is an uncommon entity, with an estimated incidence of 0.1/100,000 per year.2 Because there are no studies that look at a large series of patients in the literature, our knowledge of the disorder is limited to case reports and small case series.
In most reports, SEH is linked to predisposing factors such as an underlying coagulopathy or anticoagulant therapy, epidural venous malformation, spinal trauma, inflammatory spine disease, pregnancy or neoplastic encroachment, and bleeding into the spinal canal.3 Spontaneous spinal epidural hematoma (SSEH) with no recognizable underlying predisposing factor is even rarer,4 and the paucity of published data makes it difficult to estimate the true incidence.
In the largest study to date, Zhong etal5 found 7 of 30 cases of SSEH were not associated with bleeding risk factors, making the calculated incidence approximately 0.023/100,000 per year. However, it is impossible to estimate how many cases remain undetected because neurological loss does not occur, and the pain is labeled a nonspecific backache that resolves spontaneously.
The typical patient will present with nothing more than severe midline spinal pain located anywhere from the head to the buttocks. Patients with acute onset of axial back pain with no distinguishing signs or symptoms (“red flags”) are seen daily in every practice. Commonly accepted guidelines from the American College of Physicians (ACP) and the American Pain Society (APS) direct the physician away from MRI scanning that can confirm the diagnosis.6
As our patient’s case illustrates, acute pain in the axial spine is a very common complaint, and usually has a benign etiology. Compression of one or more of the exiting thoracic nerve roots can cause thoracic radiculopathy, which might confound the diagnosis even further and lead to an unnecessary cardiothoracic work-up.4 That was the case for our patient. Only when neurological loss is evident will the need for an MRI become clear, and the diagnosis became apparent.
Definitive treatment is elusive
Several authors advocate emergent surgical decompression and evacuation of the hematoma, because the neurological outcome could be catastrophic,7 resulting in complete quadri/paraplegia. This approach is equivocal, however, as spontaneous resolution of neurological symptoms has been described in many cases.1,7-11 Therefore, the decision whether to operate largely depends on the individual’s surgical risk factors and clinical course. In a high-risk patient who is improving neurologically, watchful waiting may be prudent, while in neurologically deteriorating low-risk cases little is lost with immediate surgical decompression.12
The prognosis of SSEH is also difficult to estimate. Several reports confirm that cervical and cervicothoracic hematomas carry a worse prognosis than thoracolumbar and lumbosacral hematomas.3,5 A rapid onset of neurological deterioration (less than12 hours) also heralds graver consequences, as does spinal cord edema on initial MRI.5
Two windows of opportunity
Two time periods stand out as possible course-changing opportunities for clinicians.The first occurs when the patient initially complains of an acute backache. At this point, ACP/APS guidelines direct us to look for red flags that focus attention on the more troubling etiologies for backache.6 Unfortunately, SSEH has no specific red flag, and itis misleading to suggest that such an esoteric diagnosis should routinely be considered.
A better approach would be to look for the unusual: very sharp, acute-onset, highly localized back pain that does not respond well to analgesics (TABLE [developed by NR]),along with any dysesthesia or unusual radicular complaint. A positive l’hermitte sign—anelectrical sensation that runs down the back and into the limbs—on physical examination might also warrant placing SSEH in the differential diagnosis.
The second time when swiftness might be crucial is from diagnosis to surgery. In a neurologically deteriorating patient, time is of utmost importance, and taking action at this juncture can produce a marked difference in the final outcome.3
CORRESPONDENCE
Nimrod Rahamimov, MD, Department of Orthopedics Band Spine Surgery, Western Galilee Hospital, PO Box 21, Naharia 22100, Israel; Nimrod.Rahamimov@naharia.health.gov.il
› Order an emergent magnetic resonance imaging scan to rule out epidural hematoma for patients with severe focal acute back pain that presents with limb dysesthesia, thoracic radiculopathy, or an unusual clinical course. A
Strength of recommendation (SOR)
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case-series
CASE A 34-year-old, otherwise healthy man presented at our emergency department (ED) complaining of severe, acute,high-thoracic back pain. He had left-sided chest pain radiating to his left arm and nonspecific paresthesias that did not track along a specific dermatome. The pain started 2 days earlier while the patient was lifting a heavy object at work. He was initially seen by his family physician, who diagnosed acute back pain, prescribed a COX-2 selective nonsteroidal anti-inflammatory agent, and advised him to stay home from work. This treatment did not improve the patient’s pain, which became more severe shortly before his arrival in our ED.
On physical examination, we found the patient in general good health, with no evidence of distress. His blood pressure was 128/78 mm Hg, his respiratory rate was 16 breaths/min,and his oral temperature was 36.5°C (97.7°F). An electrocardiogram(EKG) showed a normal sinus rhythm with no evidence of ischemia. Troponin I was 0 ng/mL, and complete blood count,C-reactive protein, and erythrocyte sedimentation rate were within normal range. After observation, the patient was discharged for ambulatory follow-up, with a diagnosis of acute back pain and nonischemic chest pain.
Two days later, the patient returned to the ED. He said that the pain had not gotten better, and he reported the gradual development of numbness in both legs, along with urinary retention. Re-examination revealed an ASIA D paraplegia at T4,with 650 mL postvoid residual urine volume. (ASIA D paraplegia means no sensory loss below the level of the injury and a motorfunction score above 3/5, which indicates active joint movement is possible against gravity but not against resistance.)
An emergent magnetic resonance imaging (MRI) scan was ordered; it revealed a large left-sided epidural mass spanning the length of T4 and T5 vertebrae with severe cord displacement and compression (FIGURE 1). On a T1-weighted MRI, the mass appeared hyperintense only on the periphery,indicating the presence of extracellular methemoglobin—a radiographic manifestation of early subacute hemorrhage.1
Surgery. We started the patient on IV dexamethasone and performed an urgent T3-T5 laminectomy, which revealed a large brown epidural mass adhering to the duramater (FIGURE 2). We removed the mass and sent it to pathology, which confirmed an epidural hematoma.
The patient’s postoperative course was uneventful, and he was discharged from the hospital with complete motor strength in both legs and complete urinary control. The patient rapidly regained all sensory function, and we re-examined him one month postop in our outpatient clinic. He was intact neurologically and completely free of pain and dysesthesia. A follow-up MRI 3 months postop revealed no residual compression or signal abnormalities within the spinal cord.
Diagnosis remains a challenge
Spinal epidural hematoma (SEH) is an uncommon entity, with an estimated incidence of 0.1/100,000 per year.2 Because there are no studies that look at a large series of patients in the literature, our knowledge of the disorder is limited to case reports and small case series.
In most reports, SEH is linked to predisposing factors such as an underlying coagulopathy or anticoagulant therapy, epidural venous malformation, spinal trauma, inflammatory spine disease, pregnancy or neoplastic encroachment, and bleeding into the spinal canal.3 Spontaneous spinal epidural hematoma (SSEH) with no recognizable underlying predisposing factor is even rarer,4 and the paucity of published data makes it difficult to estimate the true incidence.
In the largest study to date, Zhong etal5 found 7 of 30 cases of SSEH were not associated with bleeding risk factors, making the calculated incidence approximately 0.023/100,000 per year. However, it is impossible to estimate how many cases remain undetected because neurological loss does not occur, and the pain is labeled a nonspecific backache that resolves spontaneously.
The typical patient will present with nothing more than severe midline spinal pain located anywhere from the head to the buttocks. Patients with acute onset of axial back pain with no distinguishing signs or symptoms (“red flags”) are seen daily in every practice. Commonly accepted guidelines from the American College of Physicians (ACP) and the American Pain Society (APS) direct the physician away from MRI scanning that can confirm the diagnosis.6
As our patient’s case illustrates, acute pain in the axial spine is a very common complaint, and usually has a benign etiology. Compression of one or more of the exiting thoracic nerve roots can cause thoracic radiculopathy, which might confound the diagnosis even further and lead to an unnecessary cardiothoracic work-up.4 That was the case for our patient. Only when neurological loss is evident will the need for an MRI become clear, and the diagnosis became apparent.
Definitive treatment is elusive
Several authors advocate emergent surgical decompression and evacuation of the hematoma, because the neurological outcome could be catastrophic,7 resulting in complete quadri/paraplegia. This approach is equivocal, however, as spontaneous resolution of neurological symptoms has been described in many cases.1,7-11 Therefore, the decision whether to operate largely depends on the individual’s surgical risk factors and clinical course. In a high-risk patient who is improving neurologically, watchful waiting may be prudent, while in neurologically deteriorating low-risk cases little is lost with immediate surgical decompression.12
The prognosis of SSEH is also difficult to estimate. Several reports confirm that cervical and cervicothoracic hematomas carry a worse prognosis than thoracolumbar and lumbosacral hematomas.3,5 A rapid onset of neurological deterioration (less than12 hours) also heralds graver consequences, as does spinal cord edema on initial MRI.5
Two windows of opportunity
Two time periods stand out as possible course-changing opportunities for clinicians.The first occurs when the patient initially complains of an acute backache. At this point, ACP/APS guidelines direct us to look for red flags that focus attention on the more troubling etiologies for backache.6 Unfortunately, SSEH has no specific red flag, and itis misleading to suggest that such an esoteric diagnosis should routinely be considered.
A better approach would be to look for the unusual: very sharp, acute-onset, highly localized back pain that does not respond well to analgesics (TABLE [developed by NR]),along with any dysesthesia or unusual radicular complaint. A positive l’hermitte sign—anelectrical sensation that runs down the back and into the limbs—on physical examination might also warrant placing SSEH in the differential diagnosis.
The second time when swiftness might be crucial is from diagnosis to surgery. In a neurologically deteriorating patient, time is of utmost importance, and taking action at this juncture can produce a marked difference in the final outcome.3
CORRESPONDENCE
Nimrod Rahamimov, MD, Department of Orthopedics Band Spine Surgery, Western Galilee Hospital, PO Box 21, Naharia 22100, Israel; Nimrod.Rahamimov@naharia.health.gov.il
- Lipton ML. Totally Accessible MRI: A User’s Guide to Principles,Technology, and Applications. New York, NY: Springer; 2008.
- Taniguchi LU, Pahl FH, Lúcio JE, et al. Complete motor recoveryafter acute paraparesis caused by spontaneous spinal epiduralhematoma: case report. BMC Emerg Med. 2011;11:10.
- Binder DK, Sonne DC, Lawton MT. Spinal epidural hematoma.Neurosurg Q. 2004;14:51-59.
- Tsen AR, Burrows AM, Dumont TM, et al. Spinal epidural hematomamasquerading as atypical chest pain. Am J Emerg Med.2011;29:1236.e1-e3.
- Zhong W, Chen H, You C, et al. Spontaneous spinal epidural hematoma. J Clin Neurosci. 2011;18:1490-1494.
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of lowback pain: a joint clinical practice guideline from the AmericanCollege of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
- Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146:103-110.
- Subbiah M, Avadhani A, Shetty AP, et al. Acute spontaneouscervical epidural hematoma with neurological deficit after lowmolecular-weight heparin therapy: role of conservative management.Spine J. 2010;10:e11-e15.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of atraumatic cervicothoracic epidural hematoma presentingwith transient paraplegia: a case report. Spine (Phila Pa 1976). 2010;35:E564-E567.
- Sirin S, Arslan E, Yasar S, et al. Is spontaneous spinal epidural hematoma in elderly patients an emergency surgical case?Turk Neurosurg. 2010;20:557-560.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of tetraparesis because of postoperative cervical epidural hematoma.Spine J. 2010;10:e1-e5.
- Fleager K, Lee A, Cheng I, et al. Massive spontaneous epidural hematoma in a high-level swimmer: a case report. J Bone Joint Surg Am. 2010;92:2843-2846.
- Lipton ML. Totally Accessible MRI: A User’s Guide to Principles,Technology, and Applications. New York, NY: Springer; 2008.
- Taniguchi LU, Pahl FH, Lúcio JE, et al. Complete motor recoveryafter acute paraparesis caused by spontaneous spinal epiduralhematoma: case report. BMC Emerg Med. 2011;11:10.
- Binder DK, Sonne DC, Lawton MT. Spinal epidural hematoma.Neurosurg Q. 2004;14:51-59.
- Tsen AR, Burrows AM, Dumont TM, et al. Spinal epidural hematomamasquerading as atypical chest pain. Am J Emerg Med.2011;29:1236.e1-e3.
- Zhong W, Chen H, You C, et al. Spontaneous spinal epidural hematoma. J Clin Neurosci. 2011;18:1490-1494.
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of lowback pain: a joint clinical practice guideline from the AmericanCollege of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
- Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146:103-110.
- Subbiah M, Avadhani A, Shetty AP, et al. Acute spontaneouscervical epidural hematoma with neurological deficit after lowmolecular-weight heparin therapy: role of conservative management.Spine J. 2010;10:e11-e15.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of atraumatic cervicothoracic epidural hematoma presentingwith transient paraplegia: a case report. Spine (Phila Pa 1976). 2010;35:E564-E567.
- Sirin S, Arslan E, Yasar S, et al. Is spontaneous spinal epidural hematoma in elderly patients an emergency surgical case?Turk Neurosurg. 2010;20:557-560.
- Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of tetraparesis because of postoperative cervical epidural hematoma.Spine J. 2010;10:e1-e5.
- Fleager K, Lee A, Cheng I, et al. Massive spontaneous epidural hematoma in a high-level swimmer: a case report. J Bone Joint Surg Am. 2010;92:2843-2846.