User login
You say you want a revolution
Well, you know
We all want to change the world
—John Lennon
Gynecology was once a revolutionary specialty. Innovative and enterprising, its members were pioneers in operative laparoscopy, and they educated other surgical services on the merits and techniques of endoscopy.
Today the specialty lags behind others in both innovation and adoption of minimally invasive surgical techniques (FIGURE). By 2007, 95% of cholecystectomies were performed laparoscopically, as well as 90% of bariatric procedures and 70% of appendectomies. In contrast, only 20% of hysterectomies were performed using the laparoscopic approach. One reason for this discrepancy may be the extraordinary confidence that patients have in their gynecologist.
Consider the two sides of a coin that were revealed by the findings of an Internet survey of 526 women conducted by Russell Research and commissioned by the Patient Awareness Program of the AAGL. On one hand, investigators found that survey participants shared a steadfast opinion that their gynecologist would describe all available treatment choices, including the least traumatic and safest surgical procedures. Ninety-eight percent expected their physician to describe minimally invasive treatment options even if he or she was not proficient in them at the time—and to mention options that entail the least amount of pain. In addition, 94% of respondents expected their gynecologist to promote options with the lowest impact on lifestyle.1 Yet, on the other hand, although 517 of 528 (98%) respondents who were 18 years or older had experienced stress urinary incontinence, fibroids, or uterine prolapse, fewer than 40% were aware that a number of minimally invasive techniques could greatly reduce the need for hysterectomy. Fewer than 50% of respondents who suffered from menorrhagia were aware of endometrial ablation as a treatment, and only 21% realized that it could be performed in an office. Only 45% of women who had leiomyomata had heard of myomectomy. And one of every three women who had stress urinary incontinence was unaware of sling procedures. Fewer than 20% knew that sterilization could be performed in an office.1 Although these women expected to be thoroughly informed by their physician, their lack of awareness suggests the opposite.
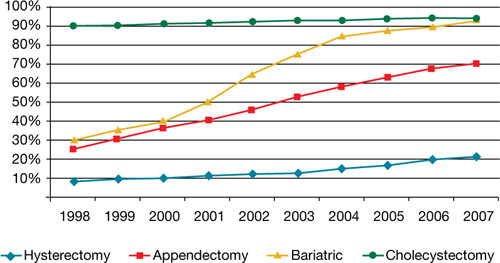
Use of minimally invasive options for 4 common surgeries
Resident physicians need more hands-on experience
A barrier to adoption of minimally invasive surgical approaches is the limited access many residents have to training and experience. This barrier could become especially problematic as third-party payers gain awareness of the advantages of minimally invasive surgery and shift reimbursement accordingly. In association with the American Society of Reproductive Medicine (ASRM), AAGL is actively engaged in enhancing surgical education through its Fellowship in Minimally Invasive Gynecology and is designing programs to supplement resident education. It is also establishing centers of excellence through its professional interest partner, the Council on Gynecologic Endoscopy (CGE).
Although the solution to our problem seems simple—increase the number of gynecologists who perform minimally invasive gynecologic surgery—that is easier said than done. According to data from the Accreditation Council for Graduate Medical Education ( ACGME), one of every three graduating residents has limited experience in minimally invasive procedures, and 30% of residents perform an average of only 12 laparoscopic operations a year as the primary surgeon. The average is even lower for hysteroscopic procedures!2

In an article published earlier this year in the Journal of Minimally Invasive Gynecology, Jon I. Einarsson, MD, MPH, and colleagues explore attitudes toward hysterectomy among gynecologists in the United States.3 Although nearly three quarters of hysterectomies are performed using an open abdominal approach, only 8% of respondents said they would choose the abdominal approach for themselves or their spouse. Among respondents who reported the highest surgical volumes, the percentage likely to choose a laparoscopic approach was significantly higher. The main barriers to laparoscopic hysterectomy? Limited opportunity for training during residency, technical difficulty, personal surgical experience, and operating time.3
We need an advanced curriculum
We have made tremendous progress in postgraduate education, thanks to the efforts of AAGL and ASRM. Nevertheless, we lack a specific, unified curriculum to train and ultimately credential gynecology residents and fellows in minimally invasive surgery.
Once again, our specialty lags behind general surgery. As of July 2009, all residents performing general surgery are required to complete and pass a course, “Fundamentals of laparoscopic surgery” (FLS). This joint undertaking of the American College of Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons has established minimum standards for basic cognitive and technical skills required for laparoscopic surgery.
Using the FLS course as a model, AAGL is designing a structured core curriculum to educate not only residents and fellows, but practicing gynecologists as well. Like the FLS course, the AAGL curriculum will emphasize both didactic teaching and lab skills, but it will be even more extensive because it will include hysteroscopy.
What we are doing now
After analyzing the needs of patients and providers around the world and acknowledging the lack of national standards to improve outcomes, AAGL and CGE have launched two other ambitious programs:
- a registry of physicians that includes operative experience and complication rate, as reviewed by their peers. This system lists physicians by level of practice, according to complexity of procedures, and by proactive experience and specialization
- a center of excellence in minimally invasive gynecology. The CGE recognizes that the achievement of best-in-class surgical outcomes requires not only an expert minimally invasive gynecologic surgeon but also an integrated, multidisciplinary surgical facility with systems and procedures to maximize quality, cost-effectiveness, and safety. For example, it is the vision of AAGL President C. Y. Liu that complex endometriosis surgery will one day be performed only by competent and experienced laparoscopic surgeons in endometriosis surgery centers.
Another initiative, launched in 2009, is the American Institute of Minimally Invasive Surgery (AIMIS). This not-for-profit organization offers member surgeons and hospitals not only accreditation and recognition, but also a number of useful products and programs, including:
- education
- guidance on technology
- business development
- insurance
- marketing strategies
- financial services
- consultation in practice management.
AIMIS is not a medical society but a national institute of which surgeons and hospitals become affiliated members.
Minimally invasive approach reduces costs, too
Rising health care costs have focused attention on ways to improve quality of care and contain costs at the same time, and minimally invasive surgery has emerged as a means of doing both. A recent study of 15,404 patients compared total abdominal hysterectomy with the minimally invasive alternatives (vaginal and laparoscopic hysterectomy) and found that the latter shortened hospitalization, reduced infection, and decreased the cost by $4,000 for the vaginal approach and $2,000 for laparoscopy.4 A study of more than 11,000 patients demonstrated a 52% reduction in the rate of hospital-acquired infection when a minimally invasive approach was utilized rather than open abdominal surgery.4
Some initiatives focus on the patient as a way of increasing utilization of minimally invasive approaches. For example, in Colorado, a 6,000-member self-funded medical plan launched a value-based program for patients undergoing colectomy, cholecystectomy, hysterectomy, appendectomy, and bariatric surgery. The program educated patients about minimally invasive options and encouraged them to seek consultation with a minimally invasive surgeon. Members who chose a minimally invasive procedure saw their copayment go down significantly. In addition, any surgeon who decided to perform one of these five procedures using an open approach was required to obtain preauthorization. Referral physicians were notified of the initiative, and minimally invasive surgeons were identified on the plan’s Web site.4
After 2 years, the plan saved nearly $1 million in direct hospital and surgeon claim costs. (Indirect savings from reduced need for prescription drugs and fewer complications were not included in this estimate. Nor were the economic advantages gained from the patient’s faster return to work and increased productivity.) After only 1 year, the utilization of minimally invasive hysterectomy rose from 28% to 80%!4
In New England, a 167-store grocery chain with 9,000 employees enrolled in the company’s self-funded health plan was able to reduce costs by identifying minimally invasive surgeons and steering members to them. The company covered 80% of surgical costs if minimally invasive surgery was performed, versus 70% for open surgery. Ultimately, the company’s per capita cost was 40% lower than all available benchmarks.4
We’re at a tipping point
The time has come for gynecologic surgeons to rejoin the revolution. Although we face many challenges, from limited experience and restricted access to training opportunities to lack of patient awareness of the benefits of minimally invasive surgery, it is imperative that we utilize minimally invasive approaches as often as possible. Educational opportunities are available, and third-party payers are beginning to demand it.
I believe it is only a matter of time before minimally invasive gynecologic procedures are the norm, not the exception.
You tell me that it’s evolution…
1. AAGL study finds women still in the dark about minimally invasive treatments for pelvic health disorders [press release]. Cypress, Calif: AAGL; 2008.
2. Accreditation Council for Graduate Medical Education. Obstetrics and gynecology case logs. National data report. 2008–2009. http://www.acgme.org/acWebsite/RRC_220/ObGynNatData0809.pdf. Accessed May 6, 2010.
3. Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar H. Minimally invasive hysterectomies—a survey on attitudes and barriers among practicing gynecologists. JMIG. 2010;17(2):167-175
4. Detweiler K, Hayes P, Cardinal A. Targeting surgery to reduce costs for employers. Employee Benefit Adviser. 2009. http://eba.benefitnews.com/news/targeting-surgery-to-reduce-costs-for-employers-2682543-1.html. Accessed May 6, 2010.
This commentary is based on the author’s 2008 presidential address to the 37th World Congress and Annual Meeting of the AAGL, which took place October 30 in Las Vegas, Nevada.
You say you want a revolution
Well, you know
We all want to change the world
—John Lennon
Gynecology was once a revolutionary specialty. Innovative and enterprising, its members were pioneers in operative laparoscopy, and they educated other surgical services on the merits and techniques of endoscopy.
Today the specialty lags behind others in both innovation and adoption of minimally invasive surgical techniques (FIGURE). By 2007, 95% of cholecystectomies were performed laparoscopically, as well as 90% of bariatric procedures and 70% of appendectomies. In contrast, only 20% of hysterectomies were performed using the laparoscopic approach. One reason for this discrepancy may be the extraordinary confidence that patients have in their gynecologist.
Consider the two sides of a coin that were revealed by the findings of an Internet survey of 526 women conducted by Russell Research and commissioned by the Patient Awareness Program of the AAGL. On one hand, investigators found that survey participants shared a steadfast opinion that their gynecologist would describe all available treatment choices, including the least traumatic and safest surgical procedures. Ninety-eight percent expected their physician to describe minimally invasive treatment options even if he or she was not proficient in them at the time—and to mention options that entail the least amount of pain. In addition, 94% of respondents expected their gynecologist to promote options with the lowest impact on lifestyle.1 Yet, on the other hand, although 517 of 528 (98%) respondents who were 18 years or older had experienced stress urinary incontinence, fibroids, or uterine prolapse, fewer than 40% were aware that a number of minimally invasive techniques could greatly reduce the need for hysterectomy. Fewer than 50% of respondents who suffered from menorrhagia were aware of endometrial ablation as a treatment, and only 21% realized that it could be performed in an office. Only 45% of women who had leiomyomata had heard of myomectomy. And one of every three women who had stress urinary incontinence was unaware of sling procedures. Fewer than 20% knew that sterilization could be performed in an office.1 Although these women expected to be thoroughly informed by their physician, their lack of awareness suggests the opposite.
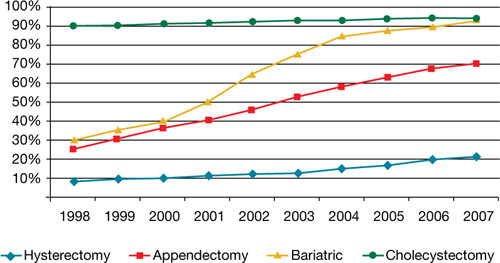
Use of minimally invasive options for 4 common surgeries
Resident physicians need more hands-on experience
A barrier to adoption of minimally invasive surgical approaches is the limited access many residents have to training and experience. This barrier could become especially problematic as third-party payers gain awareness of the advantages of minimally invasive surgery and shift reimbursement accordingly. In association with the American Society of Reproductive Medicine (ASRM), AAGL is actively engaged in enhancing surgical education through its Fellowship in Minimally Invasive Gynecology and is designing programs to supplement resident education. It is also establishing centers of excellence through its professional interest partner, the Council on Gynecologic Endoscopy (CGE).
Although the solution to our problem seems simple—increase the number of gynecologists who perform minimally invasive gynecologic surgery—that is easier said than done. According to data from the Accreditation Council for Graduate Medical Education ( ACGME), one of every three graduating residents has limited experience in minimally invasive procedures, and 30% of residents perform an average of only 12 laparoscopic operations a year as the primary surgeon. The average is even lower for hysteroscopic procedures!2

In an article published earlier this year in the Journal of Minimally Invasive Gynecology, Jon I. Einarsson, MD, MPH, and colleagues explore attitudes toward hysterectomy among gynecologists in the United States.3 Although nearly three quarters of hysterectomies are performed using an open abdominal approach, only 8% of respondents said they would choose the abdominal approach for themselves or their spouse. Among respondents who reported the highest surgical volumes, the percentage likely to choose a laparoscopic approach was significantly higher. The main barriers to laparoscopic hysterectomy? Limited opportunity for training during residency, technical difficulty, personal surgical experience, and operating time.3
We need an advanced curriculum
We have made tremendous progress in postgraduate education, thanks to the efforts of AAGL and ASRM. Nevertheless, we lack a specific, unified curriculum to train and ultimately credential gynecology residents and fellows in minimally invasive surgery.
Once again, our specialty lags behind general surgery. As of July 2009, all residents performing general surgery are required to complete and pass a course, “Fundamentals of laparoscopic surgery” (FLS). This joint undertaking of the American College of Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons has established minimum standards for basic cognitive and technical skills required for laparoscopic surgery.
Using the FLS course as a model, AAGL is designing a structured core curriculum to educate not only residents and fellows, but practicing gynecologists as well. Like the FLS course, the AAGL curriculum will emphasize both didactic teaching and lab skills, but it will be even more extensive because it will include hysteroscopy.
What we are doing now
After analyzing the needs of patients and providers around the world and acknowledging the lack of national standards to improve outcomes, AAGL and CGE have launched two other ambitious programs:
- a registry of physicians that includes operative experience and complication rate, as reviewed by their peers. This system lists physicians by level of practice, according to complexity of procedures, and by proactive experience and specialization
- a center of excellence in minimally invasive gynecology. The CGE recognizes that the achievement of best-in-class surgical outcomes requires not only an expert minimally invasive gynecologic surgeon but also an integrated, multidisciplinary surgical facility with systems and procedures to maximize quality, cost-effectiveness, and safety. For example, it is the vision of AAGL President C. Y. Liu that complex endometriosis surgery will one day be performed only by competent and experienced laparoscopic surgeons in endometriosis surgery centers.
Another initiative, launched in 2009, is the American Institute of Minimally Invasive Surgery (AIMIS). This not-for-profit organization offers member surgeons and hospitals not only accreditation and recognition, but also a number of useful products and programs, including:
- education
- guidance on technology
- business development
- insurance
- marketing strategies
- financial services
- consultation in practice management.
AIMIS is not a medical society but a national institute of which surgeons and hospitals become affiliated members.
Minimally invasive approach reduces costs, too
Rising health care costs have focused attention on ways to improve quality of care and contain costs at the same time, and minimally invasive surgery has emerged as a means of doing both. A recent study of 15,404 patients compared total abdominal hysterectomy with the minimally invasive alternatives (vaginal and laparoscopic hysterectomy) and found that the latter shortened hospitalization, reduced infection, and decreased the cost by $4,000 for the vaginal approach and $2,000 for laparoscopy.4 A study of more than 11,000 patients demonstrated a 52% reduction in the rate of hospital-acquired infection when a minimally invasive approach was utilized rather than open abdominal surgery.4
Some initiatives focus on the patient as a way of increasing utilization of minimally invasive approaches. For example, in Colorado, a 6,000-member self-funded medical plan launched a value-based program for patients undergoing colectomy, cholecystectomy, hysterectomy, appendectomy, and bariatric surgery. The program educated patients about minimally invasive options and encouraged them to seek consultation with a minimally invasive surgeon. Members who chose a minimally invasive procedure saw their copayment go down significantly. In addition, any surgeon who decided to perform one of these five procedures using an open approach was required to obtain preauthorization. Referral physicians were notified of the initiative, and minimally invasive surgeons were identified on the plan’s Web site.4
After 2 years, the plan saved nearly $1 million in direct hospital and surgeon claim costs. (Indirect savings from reduced need for prescription drugs and fewer complications were not included in this estimate. Nor were the economic advantages gained from the patient’s faster return to work and increased productivity.) After only 1 year, the utilization of minimally invasive hysterectomy rose from 28% to 80%!4
In New England, a 167-store grocery chain with 9,000 employees enrolled in the company’s self-funded health plan was able to reduce costs by identifying minimally invasive surgeons and steering members to them. The company covered 80% of surgical costs if minimally invasive surgery was performed, versus 70% for open surgery. Ultimately, the company’s per capita cost was 40% lower than all available benchmarks.4
We’re at a tipping point
The time has come for gynecologic surgeons to rejoin the revolution. Although we face many challenges, from limited experience and restricted access to training opportunities to lack of patient awareness of the benefits of minimally invasive surgery, it is imperative that we utilize minimally invasive approaches as often as possible. Educational opportunities are available, and third-party payers are beginning to demand it.
I believe it is only a matter of time before minimally invasive gynecologic procedures are the norm, not the exception.
You tell me that it’s evolution…
You say you want a revolution
Well, you know
We all want to change the world
—John Lennon
Gynecology was once a revolutionary specialty. Innovative and enterprising, its members were pioneers in operative laparoscopy, and they educated other surgical services on the merits and techniques of endoscopy.
Today the specialty lags behind others in both innovation and adoption of minimally invasive surgical techniques (FIGURE). By 2007, 95% of cholecystectomies were performed laparoscopically, as well as 90% of bariatric procedures and 70% of appendectomies. In contrast, only 20% of hysterectomies were performed using the laparoscopic approach. One reason for this discrepancy may be the extraordinary confidence that patients have in their gynecologist.
Consider the two sides of a coin that were revealed by the findings of an Internet survey of 526 women conducted by Russell Research and commissioned by the Patient Awareness Program of the AAGL. On one hand, investigators found that survey participants shared a steadfast opinion that their gynecologist would describe all available treatment choices, including the least traumatic and safest surgical procedures. Ninety-eight percent expected their physician to describe minimally invasive treatment options even if he or she was not proficient in them at the time—and to mention options that entail the least amount of pain. In addition, 94% of respondents expected their gynecologist to promote options with the lowest impact on lifestyle.1 Yet, on the other hand, although 517 of 528 (98%) respondents who were 18 years or older had experienced stress urinary incontinence, fibroids, or uterine prolapse, fewer than 40% were aware that a number of minimally invasive techniques could greatly reduce the need for hysterectomy. Fewer than 50% of respondents who suffered from menorrhagia were aware of endometrial ablation as a treatment, and only 21% realized that it could be performed in an office. Only 45% of women who had leiomyomata had heard of myomectomy. And one of every three women who had stress urinary incontinence was unaware of sling procedures. Fewer than 20% knew that sterilization could be performed in an office.1 Although these women expected to be thoroughly informed by their physician, their lack of awareness suggests the opposite.
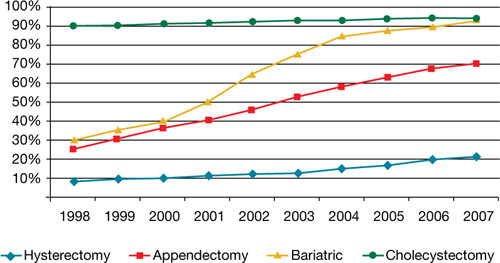
Use of minimally invasive options for 4 common surgeries
Resident physicians need more hands-on experience
A barrier to adoption of minimally invasive surgical approaches is the limited access many residents have to training and experience. This barrier could become especially problematic as third-party payers gain awareness of the advantages of minimally invasive surgery and shift reimbursement accordingly. In association with the American Society of Reproductive Medicine (ASRM), AAGL is actively engaged in enhancing surgical education through its Fellowship in Minimally Invasive Gynecology and is designing programs to supplement resident education. It is also establishing centers of excellence through its professional interest partner, the Council on Gynecologic Endoscopy (CGE).
Although the solution to our problem seems simple—increase the number of gynecologists who perform minimally invasive gynecologic surgery—that is easier said than done. According to data from the Accreditation Council for Graduate Medical Education ( ACGME), one of every three graduating residents has limited experience in minimally invasive procedures, and 30% of residents perform an average of only 12 laparoscopic operations a year as the primary surgeon. The average is even lower for hysteroscopic procedures!2

In an article published earlier this year in the Journal of Minimally Invasive Gynecology, Jon I. Einarsson, MD, MPH, and colleagues explore attitudes toward hysterectomy among gynecologists in the United States.3 Although nearly three quarters of hysterectomies are performed using an open abdominal approach, only 8% of respondents said they would choose the abdominal approach for themselves or their spouse. Among respondents who reported the highest surgical volumes, the percentage likely to choose a laparoscopic approach was significantly higher. The main barriers to laparoscopic hysterectomy? Limited opportunity for training during residency, technical difficulty, personal surgical experience, and operating time.3
We need an advanced curriculum
We have made tremendous progress in postgraduate education, thanks to the efforts of AAGL and ASRM. Nevertheless, we lack a specific, unified curriculum to train and ultimately credential gynecology residents and fellows in minimally invasive surgery.
Once again, our specialty lags behind general surgery. As of July 2009, all residents performing general surgery are required to complete and pass a course, “Fundamentals of laparoscopic surgery” (FLS). This joint undertaking of the American College of Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons has established minimum standards for basic cognitive and technical skills required for laparoscopic surgery.
Using the FLS course as a model, AAGL is designing a structured core curriculum to educate not only residents and fellows, but practicing gynecologists as well. Like the FLS course, the AAGL curriculum will emphasize both didactic teaching and lab skills, but it will be even more extensive because it will include hysteroscopy.
What we are doing now
After analyzing the needs of patients and providers around the world and acknowledging the lack of national standards to improve outcomes, AAGL and CGE have launched two other ambitious programs:
- a registry of physicians that includes operative experience and complication rate, as reviewed by their peers. This system lists physicians by level of practice, according to complexity of procedures, and by proactive experience and specialization
- a center of excellence in minimally invasive gynecology. The CGE recognizes that the achievement of best-in-class surgical outcomes requires not only an expert minimally invasive gynecologic surgeon but also an integrated, multidisciplinary surgical facility with systems and procedures to maximize quality, cost-effectiveness, and safety. For example, it is the vision of AAGL President C. Y. Liu that complex endometriosis surgery will one day be performed only by competent and experienced laparoscopic surgeons in endometriosis surgery centers.
Another initiative, launched in 2009, is the American Institute of Minimally Invasive Surgery (AIMIS). This not-for-profit organization offers member surgeons and hospitals not only accreditation and recognition, but also a number of useful products and programs, including:
- education
- guidance on technology
- business development
- insurance
- marketing strategies
- financial services
- consultation in practice management.
AIMIS is not a medical society but a national institute of which surgeons and hospitals become affiliated members.
Minimally invasive approach reduces costs, too
Rising health care costs have focused attention on ways to improve quality of care and contain costs at the same time, and minimally invasive surgery has emerged as a means of doing both. A recent study of 15,404 patients compared total abdominal hysterectomy with the minimally invasive alternatives (vaginal and laparoscopic hysterectomy) and found that the latter shortened hospitalization, reduced infection, and decreased the cost by $4,000 for the vaginal approach and $2,000 for laparoscopy.4 A study of more than 11,000 patients demonstrated a 52% reduction in the rate of hospital-acquired infection when a minimally invasive approach was utilized rather than open abdominal surgery.4
Some initiatives focus on the patient as a way of increasing utilization of minimally invasive approaches. For example, in Colorado, a 6,000-member self-funded medical plan launched a value-based program for patients undergoing colectomy, cholecystectomy, hysterectomy, appendectomy, and bariatric surgery. The program educated patients about minimally invasive options and encouraged them to seek consultation with a minimally invasive surgeon. Members who chose a minimally invasive procedure saw their copayment go down significantly. In addition, any surgeon who decided to perform one of these five procedures using an open approach was required to obtain preauthorization. Referral physicians were notified of the initiative, and minimally invasive surgeons were identified on the plan’s Web site.4
After 2 years, the plan saved nearly $1 million in direct hospital and surgeon claim costs. (Indirect savings from reduced need for prescription drugs and fewer complications were not included in this estimate. Nor were the economic advantages gained from the patient’s faster return to work and increased productivity.) After only 1 year, the utilization of minimally invasive hysterectomy rose from 28% to 80%!4
In New England, a 167-store grocery chain with 9,000 employees enrolled in the company’s self-funded health plan was able to reduce costs by identifying minimally invasive surgeons and steering members to them. The company covered 80% of surgical costs if minimally invasive surgery was performed, versus 70% for open surgery. Ultimately, the company’s per capita cost was 40% lower than all available benchmarks.4
We’re at a tipping point
The time has come for gynecologic surgeons to rejoin the revolution. Although we face many challenges, from limited experience and restricted access to training opportunities to lack of patient awareness of the benefits of minimally invasive surgery, it is imperative that we utilize minimally invasive approaches as often as possible. Educational opportunities are available, and third-party payers are beginning to demand it.
I believe it is only a matter of time before minimally invasive gynecologic procedures are the norm, not the exception.
You tell me that it’s evolution…
1. AAGL study finds women still in the dark about minimally invasive treatments for pelvic health disorders [press release]. Cypress, Calif: AAGL; 2008.
2. Accreditation Council for Graduate Medical Education. Obstetrics and gynecology case logs. National data report. 2008–2009. http://www.acgme.org/acWebsite/RRC_220/ObGynNatData0809.pdf. Accessed May 6, 2010.
3. Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar H. Minimally invasive hysterectomies—a survey on attitudes and barriers among practicing gynecologists. JMIG. 2010;17(2):167-175
4. Detweiler K, Hayes P, Cardinal A. Targeting surgery to reduce costs for employers. Employee Benefit Adviser. 2009. http://eba.benefitnews.com/news/targeting-surgery-to-reduce-costs-for-employers-2682543-1.html. Accessed May 6, 2010.
This commentary is based on the author’s 2008 presidential address to the 37th World Congress and Annual Meeting of the AAGL, which took place October 30 in Las Vegas, Nevada.
1. AAGL study finds women still in the dark about minimally invasive treatments for pelvic health disorders [press release]. Cypress, Calif: AAGL; 2008.
2. Accreditation Council for Graduate Medical Education. Obstetrics and gynecology case logs. National data report. 2008–2009. http://www.acgme.org/acWebsite/RRC_220/ObGynNatData0809.pdf. Accessed May 6, 2010.
3. Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar H. Minimally invasive hysterectomies—a survey on attitudes and barriers among practicing gynecologists. JMIG. 2010;17(2):167-175
4. Detweiler K, Hayes P, Cardinal A. Targeting surgery to reduce costs for employers. Employee Benefit Adviser. 2009. http://eba.benefitnews.com/news/targeting-surgery-to-reduce-costs-for-employers-2682543-1.html. Accessed May 6, 2010.
This commentary is based on the author’s 2008 presidential address to the 37th World Congress and Annual Meeting of the AAGL, which took place October 30 in Las Vegas, Nevada.
