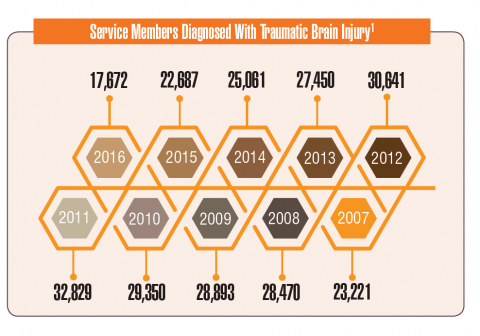
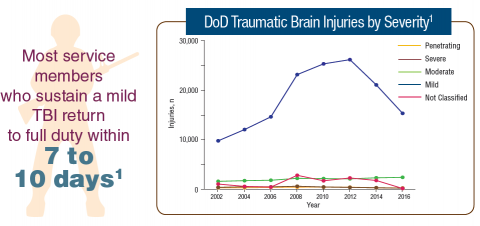
Traumatic brain injury (TBI) is now recognized as a significant health issue that impacts both activeduty service members and veterans. Blast injuries sustained in operations in Iraq and Afghanistan have led to a rising incidence of TBI in the DoD and VA patient populations.
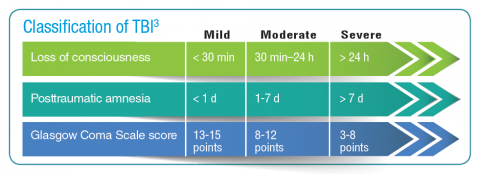
A TBI can result from a significant injury or even during day-to-day activities. Mild TBIs, also known as a concussion, typically result in short-term impacts. However, increasing evidence suggests that multiple mild TBIs can have a cumulative effect and longer term impact on patients. Moderate, severe, and penetrating TBIs can have a more serious impact on the patient.
Active-duty and reserve service members are at increased risk for TBI compared with civilians. Not only do combat operations increase the chance of blast-related injuries, but active-duty service members are often drawn from at-risk populations: men between the ages of 18 to 24 years are at greatest risk for TBI. Studies have suggested that between 10% and 20% of post-9/11 veterans experienced a mild-to-moderate TBI.
Posttraumatic stress disorder (PTSD) and TBI are closely linked. Nearly half of the active-duty service members with mild TBI also screen positive for PTSD. For clinicians, diagnosis remains a challenge because of an overlap in symptoms.