Limitations
The variables on which logistic regression were performed differed among the studies. Therefore, results cannot be averaged or compared quantitatively, as AORs varied, depending on the variables included. In addition, data were drawn from multiple geographic locations that may impact MDRO prevalence within each patient population. Finally, this review examines the utility of the risk factors formerly included in HCAP. However, other risk factors for MDRO pneumonia outlined by the ATS/IDSA guidelines still should be considered when evaluating patient risk. The 2016 guidelines recommend local incidence of resistant strains be considered when initiating empiric therapy. Review of medical records for previous positive cultures and duration of current hospitalization also should be considered. Although the 2016 ATS/IDSA HAP guidelines are not intended for immunosuppressed patients, this risk factor also may be taken into account.
Conclusion
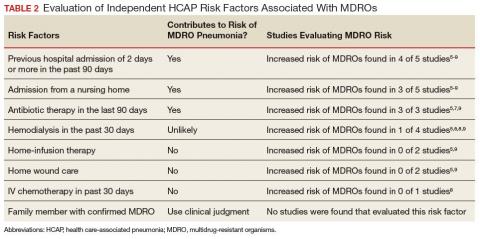
Review and synthesis of published literature found previous hospital admission (of ≥ 2 days in the past 90 days), admission from a nursing home, and IV antibiotic therapy in the last 90 days to be independent risk factors for identification of MDRO pneumonia in previously nonhospitalized patients (Table 2). Additionally, although no data were found to support this risk factor, existence of an in-home (close contact) source of MDROs would provide ample opportunity for transmission, so evaluation of known exposure to MDROs from contacts should be considered. When choosing empiric antibiotic therapy for patients admitted to the hospital for treatment of pneumonia, consideration of patient history and risk factors that may contribute to infection with a MDRO are recommended.