Knowledge of the potential dangers of mixed martial arts is valuable for Department of Defense (DoD) health care providers as the military continues to implement combatives training into regular military instruction. This case study presents an active-duty service member who developed a spontaneous vertebral artery dissection (sVAD) during mixed martial arts training, which led to a cerebellar stroke.
To the authors’ knowledge this is the first documented case of a sVAD with associated stroke related to a mixed martial arts choke hold. Understanding the diagnosis, management, and prognosis of this condition will remain important as hand-to-hand combat instruction continues to be a part of regular military training.
Case Presentation
A 39-year-old active-duty male without significant past medical history presented to the emergency department (ED) at the San Antonio Military Medical Center in Texas for evaluation of severe vertigo with associated nausea and vomiting. He had participated in a Jiu-Jitsu match the evening prior to his presentation and reported that he was placed in a choke hold within the last 12 seconds of the match. He denied losing consciousness during this hold.
Once released, he attempted to stand and developed sudden onset vertigo with severe nausea, leading to multiple bouts of emesis. He additionally developed a throbbing, left-sided headache radiating down the left side of his neck. While the vertigo resolved within an hour, he continued to experience bouts of nausea and emesis, prompting him to present to the ED for further evaluation. The patient’s past medical history was remarkable only for multiple prior concussions, and his only medication was occasional ibuprofen. He denied the usage of recreational drugs.
Upon presentation to the ED, the patient’s vital signs were 139/93 mm Hg blood pressure, 73 beats per minute heart rate, 16 breaths per minute respiration, 100% oxygen saturation on room air, and 97.7° F temperature.
His general physical exam was remarkable for a well-appearing gentleman in no distress. He had no abnormal cardiopulmonary findings. On formal neurologic assessment, he was alert and oriented to person, place, time, and situation. His speech was of normal tempo and volume without dysarthria. The remainder of his cranial nerves were intact bilaterally. He had normal muscle bulk and tone as well as full strength in his upper and lower extremities. Testing of the patient’s vibratory, pain, and temperature sensory functions disclosed no abnormalities. Cerebellar function testing was also within normal limits.The patient demonstrated normal balance and exhibited no nystagmus or limb/truncal ataxia as evaluated with finger-to-nose/heel-to-shin testing and gait exam. Complete blood count, comprehensive metabolic panel, and coagulation panel all demonstrated no abnormalities.
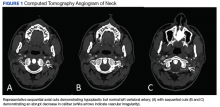
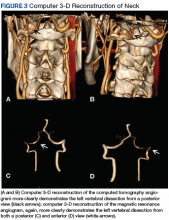
A computed tomography (CT) angiogram of his head and neck was obtained, which demonstrated a possible left VAD vs an intraluminal thrombus. To clarify this finding, a brain and neck magnetic resonance (MR) angiogram was performed. This study was remarkable for an acute infarction within the left inferior cerebellar hemisphere in the distribution of the left posterior inferior cerebellar artery (PICA). Additionally, the MR angiogram demonstrated > 50% long segment luminal narrowing of the left V2-V4 vertebral artery segments extending from C2 to the confluence with the right vertebral artery. These findings were consistent with a left VAD, complicated by left cerebellar infarction (Figures 1, 2, and 3).The patient was admitted to the hospital for symptom control and further monitoring. His headache and nausea were managed with medications, and he began antiplatelet therapy with aspirin 325 mg daily. Given the size of his cerebellar infarction, it was decided that he would be monitored in the hospital for 72 hours for the development of significant cerebellar edema. He remained stable throughout his hospitalization and had only a mild headache at the time of discharge.
The patient was last seen 3 months postinjury with no subjective complaints and a completely normal neurologic exam. The treatment plan for the patient is to continue aspirin for 6 months postinjury at which time a repeat CT will be performed to ensure resolution. He has been counseled to avoid heavy lifting and any activity with potential for sudden movement/force of the neck (grappling/wrestling, chiropractic manipulation, roller coasters, or sit-ups) until the repeat CT has been completed.