News
Mindfulness yoga reduced stress and motor symptoms in patients with Parkinson’s disease
Yoga was as effective as conventional exercise in improving motor function in patients with Parkinson’s disease.
Jill Bormann is a Research Health Scientist at the VA San Diego Healthcare System in California and a Clinical Professor at the Hahn School of Nursing and Health Science in San Diego and University of San Diego Beyster Institute of Nursing. Traci Abraham is an Assistant Professor at the University of Arkansas for Medical Sciences and a Research Health Scientist and Medical Anthropologist at the Center for Mental Healthcare Outcomes & Research South Central Mental Illness Research, Education, and Clinical Center at the Central Arkansas Veterans Healthcare System in North Little Rock.
Correspondence: Jill Bormann (jillbormannphd@gmail.com)
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies.
According to the National Institute for Occupational Safety and Health (NIOSH), stress is a major problem for more than 18 million US health care workers (HCWs).1 Increases in technology, high patient acuity, and new demands for meeting institutional benchmarks create stressful clinical work environments. HCWs at the US Department of Veterans Affairs (VA) are perhaps at particular risk of experiencing burnout due to the unique needs of VA patients and bureaucratic demands.2 Stress may lead to depression, decreased job satisfaction, and other psychological distress among HCWs.3 This, in turn, affects the delivery of care. High levels of burnout have been associated with increased medication errors, lower quality of care, and lower patient satisfaction scores.4-10
A Cochrane Review found that mental and physical relaxation reduce stress in HCWs.11 Among these, meditative interventions (eg, mindfulness, meditation, yoga) have demonstrated promise.12-14 Results from a systematic meta-analysis of meditative interventions for HCWs indicated small-to-moderate improvements in emotional exhaustion, sense of personal accomplishment, and life satisfaction. Additional research is needed to determine effects of meditative interventions on burnout and caregiver burden.15
Unfortunately, many meditative intervention programs are lengthy and require a significant investment of time. They also require some form of sitting meditation every day, placing additional demands on busy HCWs. There remains a need for practical strategies to reduce HCW stress that are easier to master and practice.
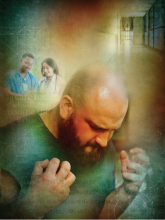
We developed, implemented, evaluated, and modified an evidence-based meditative intervention called the Mantram Repetition Program (MRP) to address workplace stress and burnout. The MRP is a mind-body, spiritually enhanced intervention that offers benefits similar to other types of meditative interventions.16 MRP is composed of 3 primary components: (1) silently repeating a self-selected, meaningful word or phrase (here called a mantram); (2) intentionally slowing down thoughts and behaviors; and (3) developing the ability to focus on a single task at a time (ie, one-pointed attention). The MRP does not require participants to set aside a specific place to practice, and mantram repetition can be initiated intermittently and privately throughout the day (eg, between tasks, while walking or waiting). Examples of 4 sessions (eg, Mantram 1, 2, 3, and 4) can be found on the PsychArmor Institute website (www.psycharmor.org; San Diego, CA).
Initially, the MRP was offered in a group format, in 6 or 8 weekly, 90-minute face-to-face sessions to both patient and nonpatient populations. Studies in veterans with chronic diseases demonstrated improvements in perceived stress, anxiety, and anger, and increased levels of spiritual well-being and quality of life (QOL).17-19 Veterans with posttraumatic stress disorder (PTSD) reported improvements in PTSD symptoms, QOL, and spiritual well-being.20-23 Family caregivers of veterans with dementia reported significant reductions in caregiver burden, depression, and anxiety after participating in the MRP.24
Similar results have substantiated the effects of the MRP among HCWs, including reductions in perceived stress, stress of conscience (ie, the conflict that results from competing values and behaviors in the workplace), and burnout.25-27 HCWs also reported improvements in mindfulness and spiritual well-being.28 In a randomized controlled trial, South Korean nurse managers who completed the MRP demonstrated significant improvements in psychosocial and spiritual well-being and leadership practice and experienced reductions in burnout compared with that of the control group.27 In a qualitative study, the most frequently reported benefits of the MRP were improvements in managing symptoms of stress, anxiety, and feeling out of control.18
HCWs reported they found it difficult to attend the 8-week MRP face-to-face group classes. Therefore, we developed a shorter online version of the MRP consisting of six 1-hour educational sessions: 4 online self-learning modules, and 2 live meeting webinars with the course facilitator.28 VA employees were invited to enroll in the program from June 2013 through 2016 through group e-mails and announcements in the VA Employee Education Service newsletters. Those eligible to participate could earn up to 6 hours of continuing education.
Although the program was generally well accepted, feedback from HCWs indicated that providers still lacked enough time to participate fully. We therefore condensed the MRP into one 90-minute, videotaped webinar entitled “Mind-Body-Spiritual Strategies for a Healthy Workforce: The Mantram Repetition Program.” The webinar was delivered in real time in June 2013 and archived for viewing later. This condensed course provided an overview of the development, theory, and practice of MRP core components. Specific instructions included how to choose and use a mantram; the importance of acting slowly with intention to avoid mistakes; and ways of developing single-pointed attention. Participants were invited to complete a standard course evaluation using an online survey.
This article presents results from qualitative analyses of participant feedback for the condensed MRP in a nationwide sample of more than 1,700 HCWs within the VA. We used template summary analysis to identify themes in participants’ responses to 2 open-ended questions: “What about this learning activity was most useful to you?” and “What about this learning activity was least useful to you?” These results have implications for reducing HCW stress and developing training programs for HCWs.
Yoga was as effective as conventional exercise in improving motor function in patients with Parkinson’s disease.
National survey data show a rise in mindfulness-based activities within various occupations and employment status.
Accurate reporting of disruptive behavior enables the development of strategies that provide for the safe delivery of health...
