Methods
According to policy activities that constitute research at MRVAMC, no institutional review board approval was required as this work met criteria for operational improvement activities exempt from ethics review.
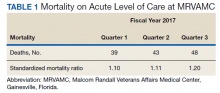
The North Florida/South Georgia Veterans Health System (NF/SGVHS) includes MRVAMC, a large academic hospital with rotating residents/fellows and multiple specialty care services. MRVAMC comprised 144 beds on the medicine/surgery wards; 48 beds in the psychiatry unit; 18 intermediate LOC beds; and 27 ICU beds. The MRVAMC SMR was identified as an improvement opportunity during fiscal year (FY) 2017 (Table 1). Its adjusted mortality for acute LOC demonstrated an observed/expected ratio of > 1.0 suggesting more inpatient deaths were observed than expected. The number of deaths (unadjusted mortality) on acute LOC at MRVAMC was noted to be rising during the first 3 quarters of FY 2017. A deeper examination of data by Pyramid Analytics (www.pyramidanalytics.com) discovered that sepsis was the primary driver for inpatient mortality on acute LOC at MRVAMC. Our goal was to reduce inpatient sepsis-related mortality via development of an EWSS that leveraged VistA/CPRS to improve early identification and treatment of sepsis in the ED and inpatient wards.
Emergency Department
Given the importance of recognizing sepsis early, the sepsis team focused on improvement opportunities at the initial point of patient contact: ED triage. The goal was to incorporate automated VistA/CPRS decision support to assist clinicians with identifying sepsis in triage using MEWS, which was chosen to optimize immediate hospital-wide buy-in. Clinical staff were already familiar with MEWS, which was in use on the inpatient wards.
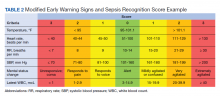
Flow through the ED and availability of resources differed from the wards. Hence, modification to MEWS on the wards was necessary to fit clinical workflow in the ED. Temperature, heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), mental status, and white blood cell count (WBC) factored into a MEWS + SRS score on the wards (Table 2). For the ED, MEWS included temperature, HR, RR and SBP, but excluded mental status and WBC. Mental status assessment was excluded due to technical infeasibility (while vital signs could be automatically calculated in real time for a MEWS score, that was not possible for mental status changes). WBC was excluded from the ED as laboratory test results would not be available in triage.
MEWS + SRS scores were calculated in VistA by using clinical reminders. Clinical reminder logic included a series of conditional statements based on various combinations of MEWS + SRS clinical data entered in the EHR. When ED triage vital signs data were entered in CPRS, clinical data were stored and processed according to clinical reminder logic in VistA and displayed to the user in CPRS. While MEWS of ≥ 5 triggered a sepsis alert on the wards, the ≥ 4 threshold was used in the ED given mental status and WBC were excluded from calculations in triage (eAppendix 1 available at doi:10.12788/fp.0194).
Once a sepsis alert was triggered in triage for MEWS ≥ 4, ED nursing staff prioritized bed location and expedited staffing with an ED attending physician for early assessment. The ED attending then performed an assessment to confirm whether sepsis was present and direct early treatment. Although every patient who triggered a sepsis alert in triage did not meet clinical findings of sepsis, patients with MEWS ≥ 4 were frequently ill and required timely intervention.
If an ED attending physician agreed with a sepsis diagnosis, the physician had access to a sepsis workup and treatment order set in CPRS (eAppendix 2 available at doi:10.12788/fp.0194). The sepsis order set incorporated recommendations from the Surviving Sepsis Campaign guidelines and included orders for 2 large-bore peripheral IV lines; aggressive fluid resuscitation (30 mL/kg) for patients with clinical findings of hypoperfusion; broad-spectrum antibiotics; and frequent ordering of laboratory tests and imaging during initial sepsis workup.6 Vancomycin and cefepime were selected as routine broad-spectrum antibiotics in the order set when sepsis was suspected based on local antimicrobial stewardship and safety-efficacy profiles. For example, Luther and colleagues demonstrated that cefepime has lower rates of acute kidney injury when combined with vancomycin vs vancomycin + piperacillin-tazobactam.20 If a β-lactam antibiotic could not be used due to a patient’s drug allergy history, aztreonam was available as an alternative option.
The design of the order set also functioned as a communication interface with clinical pharmacists. Given the large volume of antibiotics ordered in the ED, it was difficult for pharmacists to prioritize antibiotic order verification. While stat orders convey high priority, they often lack specificity. When antibiotic orders were selected from the sepsis order set, comments were already included that stated: “STAT. First dose for sepsis protocol” (eAppendix 3 available at doi:10.12788/fp.0194). This standardized communication conveyed a sense of urgency and a collective understanding that patients with suspected sepsis required timely order verification and administration of antibiotics.