Hospital Ward
Mental status and WBC were included on the wards to monitor for possible signs of sepsis, using MEWS + SRS, which was routinely monitored by nursing every 4 to 8 hours. When MEWS + SRS was ≥ 5 points, ward nursing staff called a sepsis alert.7,16 Early response team (ERT) members received telephone notifications of the alert. ERT staff proceeded with immediate evaluation and treatment at the bedside along with determination for most appropriate LOC. The ERT members included an ICU physician and nurse; respiratory therapist; and nursing supervisor/bed flow coordinator. During bedside evaluation, if the ERT or primary team agreed with a sepsis diagnosis, the ERT or primary team used the sepsis order set to ensure standardized procedures. Stat orders generated through the sepsis order set pathway conveyed a sense of urgency and need for immediate order verification and administration of antibiotics.
In addition to clinical care process improvement, accurate documentation also was emphasized in the EWSS. When a sepsis alert was called, a clinician from the primary team was expected to complete a standardized progress note, which communicated clinical findings, a treatment plan, and captured severity of illness (eAppendix 4 available at doi:10.12788/fp.0194). It included sections for subjective, objective, assessment, and plan. In addition, data objects were created for vital signs and common laboratory findings that retrieved important clinical data from VistA and inserted it into the CPRS note.21
Nursing staff on the wards were expected to communicate results with the primary team for clinical decision making when a patient had a MEWS + SRS of 3 to 4. A sepsis alert may have been called at the discretion of clinical team members but was not required if the score was < 5. Additionally, vital signs were expected to be checked by the nursing staff on the wards at least every 4 hours for closer monitoring.
Sepsis Review Meetings
Weekly meetings were scheduled to review sepsis cases to assess diagnosis, treatment, and documentation entered in the patient record. The team conducting sepsis reviews comprised the chief of staff, chief of quality management, director of patient safety, physician utilization management advisor, chief resident in quality and patient safety (CRQS), and inpatient pharmacy supervisor. In addition, ad hoc physicians and nurses from different specialty areas, such as infectious diseases, hospitalist section, ICU, and the ED participated on request for subject matter expertise when needed. At the conclusion of weekly sepsis meetings, sepsis team members provided feedback to the clinical staff for continuous improvement purposes.
Results
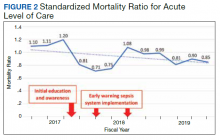
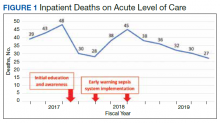
Before implementation of an EWSS at NF/SGVHS, a plan was devised to increase awareness and educate staff on sepsis-related mortality in late FY 2017. Awareness and education about sepsis-related mortality was organized at physician, nursing, and pharmacy leadership clinical staff meetings. Posters about early warning signs of sepsis also were displayed on the nursing units for educational purposes and to convey the importance of early recognition/treatment of sepsis. In addition, the CRQS was the quality leader for house staff and led sepsis campaign change efforts for residents/fellows. An immediate improvement in unadjusted mortality at MRVAMC was noted with initial sepsis awareness and education. From FY 2017, quarter 3 to FY 2018, quarter 1, the number of acute LOC inpatient deaths decreased from 48 to 28, a 42% reduction in unadjusted mortality at MRVAMC (Figure 1). Additionally, the acute LOC SMR improved from 1.20 during FY 2017, quarter 3 down to as low as 0.71 during FY 2018, quarter 1 (Figure 2).