Promising New Approaches for Testicular and Prostate Cancer
Bruce Montgomery, MD
Medicine and Oncology,
University of Washington
Fred Hutchinson Cancer Center
VA Puget Sound HCS
Seattle, WA
Slideshow below.
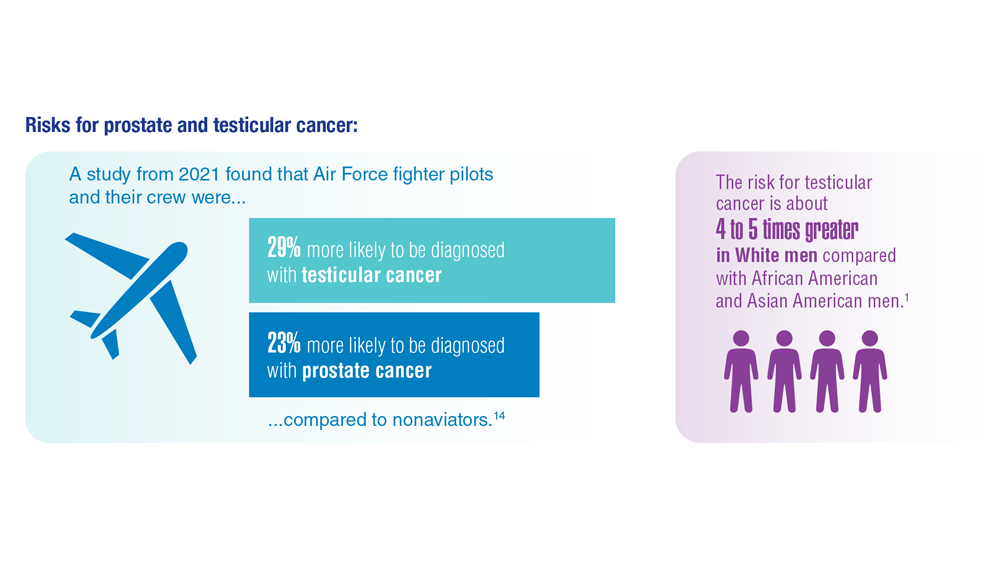
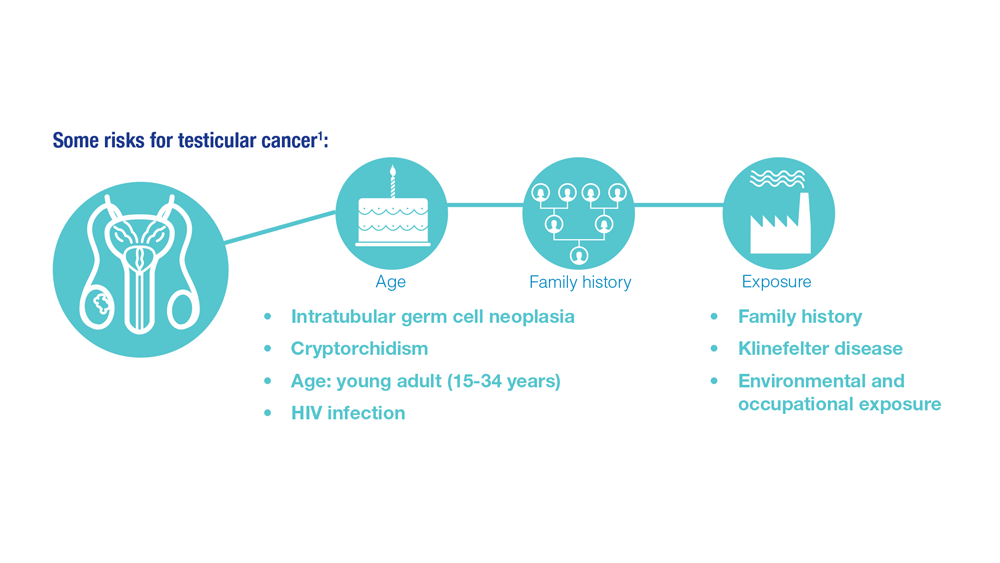
Although testicular cancer is rare, it is most common in boys and men between 15 and 34 years of age—the age range of many active-duty military members. Risk factors include a personal history of an undescended testicle or prior testicular cancer, a family history of testicular cancer, HIV infection, having Klinefelter disease, age, and race.1
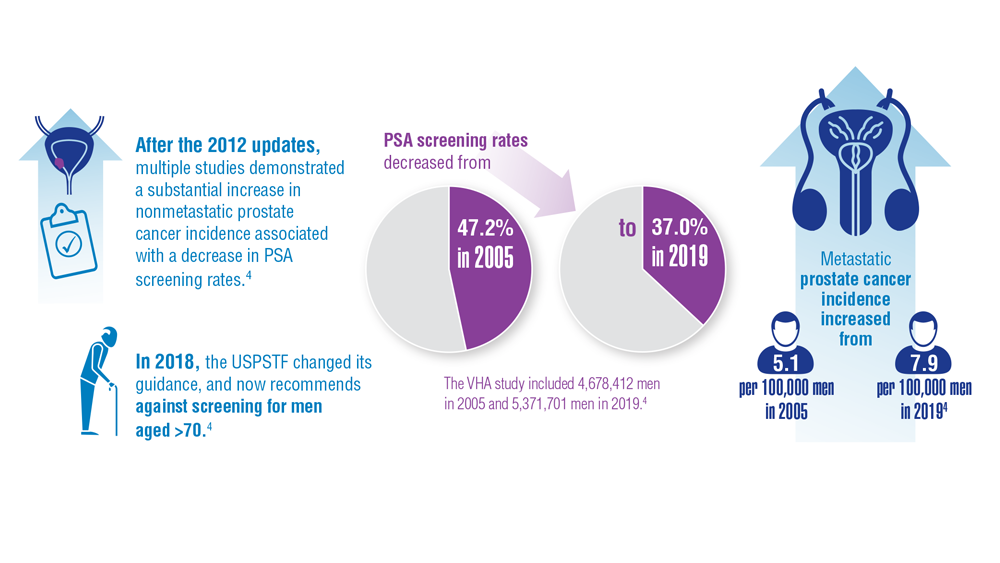
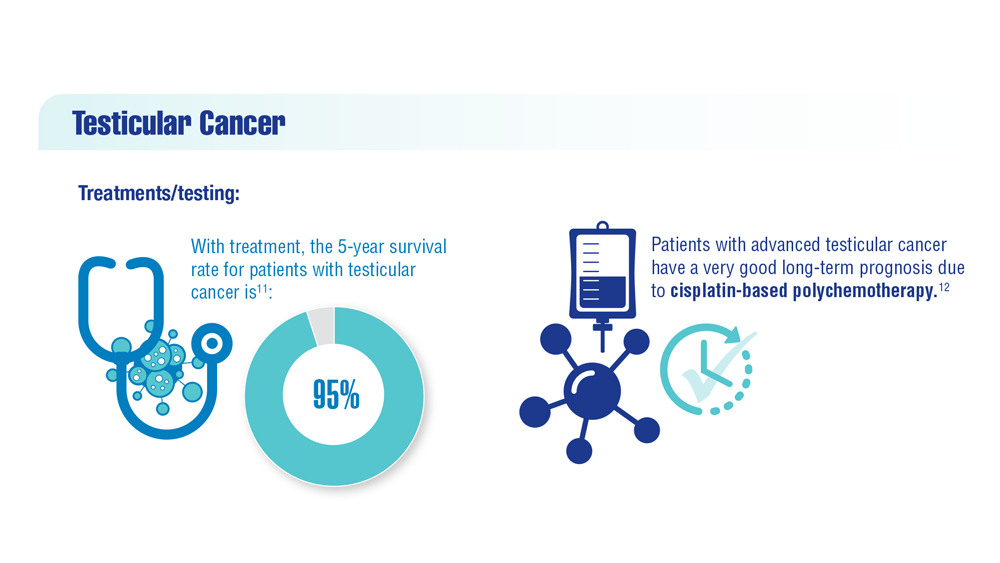
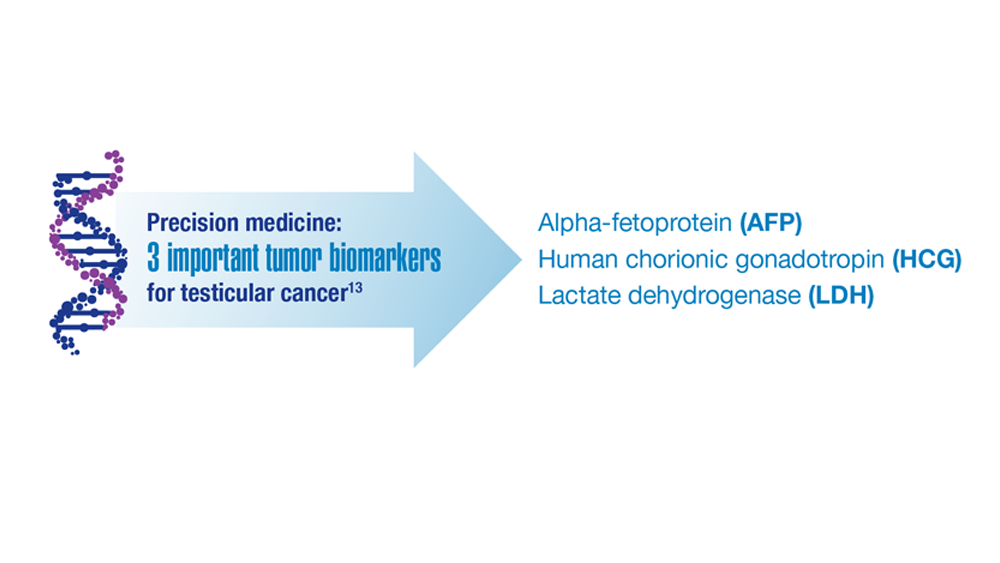
Treatment for testicular cancer can involve surgery, radiation, or chemotherapy. For patients with metastatic testicular cancer, the development of cisplatin-based chemotherapy has made this one of the most curable malignancies of any type.2,3 Advances in the treatment of men with testicular cancer continue to be made. A recently described serum biomarker, miR-371a-3p, is more sensitive for detecting the presence of subclinical disease than those currently used and is poised to be in clinical use shortly.3 New approaches to treatment, including high-dose therapy and drugs targeting the epigenetic regulation of testicular cancer, continue to be explored. Prostate cancer, on the other hand, is the second most common cancer in men worldwide.4 The use of prostate-specific antigen (PSA) screening for the detection of prostate cancer has been controversial in the United States for years. Because the US Preventive Services Task Force recommended against PSA screening, PSA screening rates decreased in the VHA and across the United States from 2005 to 2019.
A recent study was conducted within the VHA to determine whether the lower PSA screening rates had an impact on the occurrence of metastatic prostate cancer in VHA patients. The results showed that facilities with higher PSA screening rates had lower rates of metastatic prostate cancer; conversely, higher long-term nonscreening rates were associated with higher metastatic prostate cancer diagnosis rates for patients within the VHA system.4
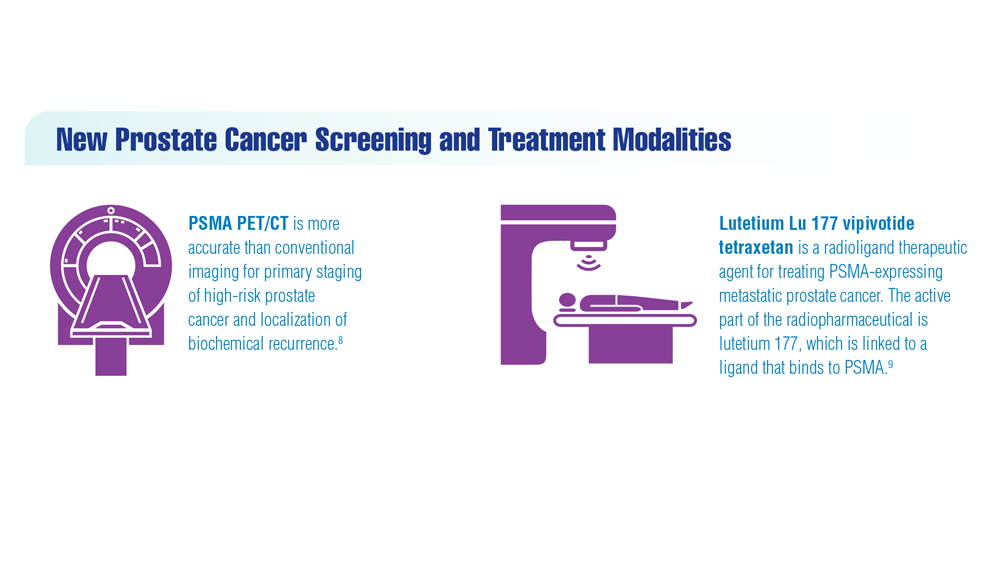
These results strongly suggest that PSA screening does aid in the early detection and reduction of the development of prostate cancer. New imaging and treatments for prostate cancer are also available and have shown promise for patients. Prostate-specific membrane antigen (PSMA) imaging can effectively detect prostate cancer that has spread at earlier time points and help with informed decision-making for treatment. Where available, PSMA positron emission tomography/computed tomography (PET/CT) is preferred over other forms of noninvasive diagnostic imaging for staging before local therapy and for detection of sites of recurrence after local therapy because of its greater sensitivity at low PSA levels.5
Lutetium Lu 177 vipivotide tetraxetan (Pluvicto), the newest FDA-approved drug for treating prostate cancer, is an IV radioligand therapy that delivers β-particle radiation to PSMA-expressing cells.6 It can target prostate cancer cells without affecting most normal tissues in patients with the use of imaging to confirm radionuclide binding.7 The use of Lutetium in men with advanced prostate cancer improved survival compared with the standard of care.6,7 Strategies for early detection of these 2 cancers affecting veterans should include testicular self-examination for the presence of any masses and the use of the PSA test should be considered for the early detection of prostate cancer in the appropriate patient.
1
-

Over the past 15 years, the USPSTF recommendations for PSA screening have changed several times.4
-
-

While studies have indicated that overall cancer incidence rates among men in the VHA mirrored those of the general population, statistics now show that the incidence rate for military personnel is 1 in 5.4
-
-
Testicular cancer is the most common cancer in active-duty males. Cancer incidence patterns in active-duty service members differ from those in the general US population and from veterans. Tumor etiology in active-duty service members may be influenced by military exposures.10
-
-
-