Electronic Data Set
An investigator reviewed the electronic data set, and exclusion criteria that could be ascertained electronically were applied. The primary reasons for exclusion were age (18.4%), potential coagulopathy (14.5%), recent transfusion (14.6%), use of therapeutic anticoagulation (11%), or an extended LOS (7%). Less common reasons for exclusion were coagulation disorders (1.4%), heparin-induced thrombocytopenia (1.2%), recent hemorrhage (1.1%), or missing baseline laboratory values (3.2%). Subsequently, the potential sample of subjects declined to 1,018 (27%) hospitalizations. Of the remaining hospitalizations, 46 and 972 were medical CCU and nonsurgical (medical) inpatients, respectively.
In line with the sampling plan, 130 (13.4%) medical ward hospitalizations were selected using a random number generator. As the ICU sample was smaller than anticipated, the convenience sample of all 46 hospitalizations was used.
Manual Chart Abstraction
Manual chart abstraction (n = 176) clarified physician/provider decision making (eg, some patients were not appropriate for thromboprophylaxis due to upcoming invasive procedures), medical history that could not be extracted by ICD-9 coding (eg, recent non-VHA admissions for medical conditions that were contraindications to prophylaxis), and anticoagulation dosing. These exclusions led to an additional 52 (29.5%) excluded hospitalizations. Reasons for manual exclusion included recent bleeding or at high risk for bleeding (18, 34.6%), incorrect classification as nonsurgical or elective admission (5, 9.6%), no diagnosis of lung disease (21, 40.4%), invasive procedures planned (4, 7.7%), treatment anticoagulant doses selected (4, 7.7%), or patient transferred to a non-VA medical facility due to acuity level (1, 1.9%). One patient was excluded for multiple reasons.
Baseline Demographics
The sample was an elderly, male (98%), white (79.8%) cohort (Table 1). No patients were aged < 40 years. Racial information was missing for 5.6% of the patients. The chief pulmonary diagnosis was COPD, and few patients had new onset, acute, severe respiratory disease (3.2%) prompting admission, because pneumonia was not included as a qualifying diagnosis. Median body mass index (BMI) was 26.31. The median LOS was 3.8 days for the overall cohort and 4.1 days for those receiving pharmacologic thromboprophylaxis, although for the latter group a larger proportion of patients were hospitalized for < 3 days. Renal function, according to endpoint definitions, was for using enoxaparin as the appropriate strategy for thromboprophylaxis for the majority (97.5%) of hospitalizations.
Primary and Secondary Endpoints
Of those receiving pharmacologic thromboprophylaxis, heparin was prescribed most often (62.8%). One patient received both heparin and enoxaparin during a single hospitalization.
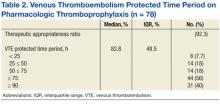
Pharmacologic thromboprophylaxis was more common in the medical CCU subgroup (80.6%) compared with the nonsurgical patient (56.9%). Pharmacologic thromboprophylaxis was used in 62.9% of patients (n = 124). However, the therapeutic appropriateness ratio was reduced to 58% of the entire sample (n = 124), because 6 patients of the cohort receiving thromboprophylaxis (n = 78) were prescribed suboptimal doses: Specifically, 1 patient was underdosed and 1 overdosed when prescribed enoxaparin (2, 2.6%). Four patients (5.1%) received underdoses of heparin, based on institutional guidance. For those prescribed pharmacologic thromboprophylaxis, the VTE protected time period ratio was 82.8% (Table 2). Overall inpatient mortality rate was low (12, 9.7%). Most deceased patients were managed in the medical CCU (10, 83.3%) and did receive pharmacologic thromboprophylaxis (10, 83.3%).
Discussion
This study demonstrated moderate rates of VTE pharmacologic thromboprophylaxis, because 62.9% of nonsurgical patients with respiratory disease who were hospitalized for various reasons were prophylaxed with either SC heparin or enoxaparin. This rate represents active clinical decision making, because there was no indication to prescribe anticoagulation at therapeutic doses. As expected, pharmacologic thromboprophylaxis was more common in the critical care subgroup (80.6%) compared with the nonsurgical patients (56.9%). Although the study did not meet the intended sample size for this subgroup analysis, results were statistically significant for location of care (P = .014) and may be beneficial for future study design by other investigators.
As early studies of nonsurgical and critical care patients document ≤ 40% of patients receive pharmacologic thromboprophylaxis, this study’s performance seems better.7,12,21 Recently, VHA investigators Quraishi and colleagues seemed to document similar findings. Although 63% of medical patients at the Dayton VAMC in Ohio received appropriate pharmacologic thromboprophylaxis, this value must be tempered by the proportion of subjects receiving therapeutic anticoagulation (5.4%).18
Similar to this study’s results, recent studies of nonveterans document pharmacologic thromboprophylaxis rates of 41% to 51.8%, 41% to 65.9%, and 74.6% to 89.9% in patients with respiratory disease, nonsurgical patients, and critical care patients, respectively. Although findings seem similar to this study’s results, adjustments in estimates again must be made, because these estimates included patients on therapeutic anticoagulation.12,14-16 This study’s results found that 58% of the patient cohort met the therapeutic appropriateness ratio, because they were administered pharmacologic thromboprophylaxis and received correct doses at indicated dosing intervals.