SAN FRANCISCO – Fecal microbiota transplantation via a pill appears to be as effective as other delivery methods, according to Dr. Thomas Louie.
Typically, fecal microbiota transplantation (FMT) using feces from healthy donors is delivered by enema, colonoscopy, or nasogastric tube to rebalance the bacteria in the gastrointestinal system of patients with recurrent Clostridium difficile infection, but Dr. Louie of the University of Calgary (Alta.) has developed a pill formulation that had 100% efficacy at 3-months’ follow-up in the first 32 patients he treated. Some of those patients have been followed for up to 3 years, and they remain C. difficile free.
The findings were reported at an annual scientific meeting on infectious diseases.
"I’m happy to report that we’ve basically had no recurrences in any of [the 32 patients]," Dr. Louie said during a press conference, noting that one patient who required treatment with antibiotics after FMT developed what Dr. Louie said may be a mild recurrence associated with the antibiotic use.
He has been performing FMT via the enema route since 1996and has treated numerous patients with a very high success rate. He said he came up with the idea for a pill formulation when he encountered a patient who failed to respond to FMT enema on two occasions because of an inability to retain the high-volume treatment for her C. difficile infection, and who was unable to undergo nasogastric delivery because of esophageal varices.
Using freshly passed fecal matter donated, in most cases, by patients’ family members, Dr. Louie said he concentrates the fecal bacteria using a serial centrifugation process that results in pelleted fecal microbes in the sediment of the last centrifugation, and encapsulates the product inside three layers of gelatin capsule to ensure delivery into the small intestine.
The first few patients took 10 pills daily over a period of 4 days with a successful outcome, but the technique has been refined to the ingestion of a "one-shot deal" involving ingestion of 12-34 freshly prepared pills at a single visit.
Patients come in on an empty stomach, take their pills, go home, and wait about an hour and a half, and have some lunch.
"And that’s the end of their C. diff.," he said.
While the dosing isn’t an exact science, it does appear that some patients require fewer pills. For example, a 6-year-old heart transplant patient who had had multiple C. difficile recurrences over a 9-month period was successfully treated with 12 pills, Dr. Louie said.
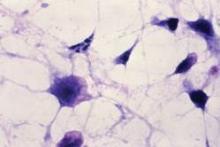
An analysis of stool following FMT in the treated patients demonstrated that healthy bacteria were significantly increased, while Enterobacteriaceae and Veillonella bacteria were significantly decreased.
Dr. Tom Moore of the University of Kansas in Wichita who moderated the press conference, said in an interview that while none of the methods for delivering FMT have been compared in head-to-head studies, the available evidence suggests they all are highly effective, and the choice depends on patient and physician preference.
Certainly there is a "yuck factor" involved in this treatment for both patients and clinicians. For patients, the pill formulation may seem more palatable; clinicians charged with assembling the capsules may feel otherwise, he said.
But he, along with Dr. Ravi Kamepalli, an infectious disease specialist in group practice in Lima, Ohio, who presented patient satisfaction data for FMT via nasogastric delivery, said clinicians just "need to get over it."
FMT is a life-altering, if not lifesaving procedure for many patients, Dr. Kamepalli said.
In a survey, 28 patients who underwent FMT via nasogastric delivery rated overall satisfaction at 9.6 on a 1-10 scale, and rated ease and likelihood of recommending the procedure to a family member or friend at 9.9 each.
The patients, who had a mean age of 67 years, were surveyed 3 months after the procedure.
To date, Dr. Kamepalli has treated 40 patients with a 98% success rate, he said.
IDWeek is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The investigators reported having no relevant financial disclosures.