User login
HCV Hub
AbbVie
acid
addicted
addiction
adolescent
adult sites
Advocacy
advocacy
agitated states
AJO, postsurgical analgesic, knee, replacement, surgery
alcohol
amphetamine
androgen
antibody
apple cider vinegar
assistance
Assistance
association
at home
attorney
audit
ayurvedic
baby
ban
baricitinib
bed bugs
best
bible
bisexual
black
bleach
blog
bulimia nervosa
buy
cannabis
certificate
certification
certified
cervical cancer, concurrent chemoradiotherapy, intravoxel incoherent motion magnetic resonance imaging, MRI, IVIM, diffusion-weighted MRI, DWI
charlie sheen
cheap
cheapest
child
childhood
childlike
children
chronic fatigue syndrome
Cladribine Tablets
cocaine
cock
combination therapies, synergistic antitumor efficacy, pertuzumab, trastuzumab, ipilimumab, nivolumab, palbociclib, letrozole, lapatinib, docetaxel, trametinib, dabrafenib, carflzomib, lenalidomide
contagious
Cortical Lesions
cream
creams
crime
criminal
cure
dangerous
dangers
dasabuvir
Dasabuvir
dead
deadly
death
dementia
dependence
dependent
depression
dermatillomania
die
diet
direct-acting antivirals
Disability
Discount
discount
dog
drink
drug abuse
drug-induced
dying
eastern medicine
eat
ect
eczema
electroconvulsive therapy
electromagnetic therapy
electrotherapy
epa
epilepsy
erectile dysfunction
explosive disorder
fake
Fake-ovir
fatal
fatalities
fatality
fibromyalgia
financial
Financial
fish oil
food
foods
foundation
free
Gabriel Pardo
gaston
general hospital
genetic
geriatric
Giancarlo Comi
gilead
Gilead
glaucoma
Glenn S. Williams
Glenn Williams
Gloria Dalla Costa
gonorrhea
Greedy
greedy
guns
hallucinations
harvoni
Harvoni
herbal
herbs
heroin
herpes
Hidradenitis Suppurativa,
holistic
home
home remedies
home remedy
homeopathic
homeopathy
hydrocortisone
ice
image
images
job
kid
kids
kill
killer
laser
lawsuit
lawyer
ledipasvir
Ledipasvir
lesbian
lesions
lights
liver
lupus
marijuana
melancholic
memory loss
menopausal
mental retardation
military
milk
moisturizers
monoamine oxidase inhibitor drugs
MRI
MS
murder
national
natural
natural cure
natural cures
natural medications
natural medicine
natural medicines
natural remedies
natural remedy
natural treatment
natural treatments
naturally
Needy
needy
Neurology Reviews
neuropathic
nightclub massacre
nightclub shooting
nude
nudity
nutraceuticals
OASIS
oasis
off label
ombitasvir
Ombitasvir
ombitasvir/paritaprevir/ritonavir with dasabuvir
orlando shooting
overactive thyroid gland
overdose
overdosed
Paolo Preziosa
paritaprevir
Paritaprevir
pediatric
pedophile
photo
photos
picture
post partum
postnatal
pregnancy
pregnant
prenatal
prepartum
prison
program
Program
Protest
protest
psychedelics
pulse nightclub
puppy
purchase
purchasing
rape
recall
recreational drug
Rehabilitation
Retinal Measurements
retrograde ejaculation
risperdal
ritonavir
Ritonavir
ritonavir with dasabuvir
robin williams
sales
sasquatch
schizophrenia
seizure
seizures
sex
sexual
sexy
shock treatment
silver
sleep disorders
smoking
sociopath
sofosbuvir
Sofosbuvir
sovaldi
ssri
store
sue
suicidal
suicide
supplements
support
Support
Support Path
teen
teenage
teenagers
Telerehabilitation
testosterone
Th17
Th17:FoxP3+Treg cell ratio
Th22
toxic
toxin
tragedy
treatment resistant
V Pak
vagina
velpatasvir
Viekira Pa
Viekira Pak
viekira pak
violence
virgin
vitamin
VPak
weight loss
withdrawal
wrinkles
xxx
young adult
young adults
zoloft
financial
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
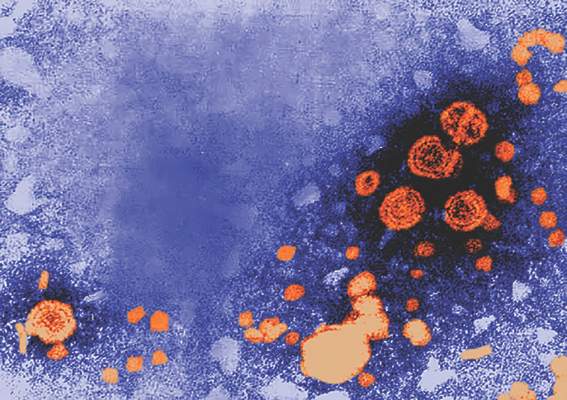
Chronic HCV boosts hospitalization risk, not just for liver
People with chronic hepatitis C infection were nearly four times more likely than other health system patients to be hospitalized, and not only with liver-related problems.
An observational cohort study of 10,131 patients with chronic hepatitis C infection (the Chronic Hepatitis Cohort Study) and 20,262 health system patients showed the overall hospitalization rate was 3.7 times higher in patients with chronic hepatitis C.
The study, published online May 15 in the Journal of Viral Hepatitis, found patients with chronic hepatitis C experienced an average of 3.5 hospitalizations over a mean of 5.5 years follow-up, compared with 1.9 hospitalizations in other patients over an average of 4.8 years. Investigators excluded HCV patients with HIV or hepatitis B coinfection, or who had received a liver transplant.
Hospitalization rates in both groups were significantly higher among patients who were older than 65 years, black, or who had a household income less than $15,000 per year (J Viral Hepat. 2016 May 15. doi: 10.1111/jvh.12548).
Patients with chronic hepatitis C had a nearly 25-fold greater risk of being hospitalized with liver-related conditions, compared with other health system patients.
“Liver-related conditions are the third leading cause of nonsurgical hospitalizations of chronic HCV patients after cardiovascular diseases and infections,” wrote Dr. E. H. Teshale, from the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta, and coauthors.
However liver-related complications only accounted for 9.1% of all hospitalizations in this group, compared with 1.3% of hospitalizations in the control group.
The analysis also revealed a sixfold greater risk of hospitalization for infection, a sevenfold greater risk for dermatologic and hematologic problems, a 10-fold greater risk of hospitalization for substance abuse, and a nearly threefold greater risk of being hospitalized for cardiovascular disease, compared with other health system patients.
Hospitalizations were significantly lower among patients receiving treatment for hepatitis C and who had achieved a sustained virologic response, the authors noted.
“Initiation of treatment prior to progression to advanced liver disease can reduce the cost of hospitalization, which in many cases may include repeated hospitalizations and other costly interventions,” the investigators reported. “Some studies have found a significant health care cost alleviation following HCV therapy, which [was] primarily due to costs associated with hospitalizations for non-HCV–related comorbidities.”
The Chronic Hepatitis Cohort Study was funded by the CDC Foundation, which receives grants from a range of pharmaceutical companies. No other conflicts of interest were declared.
People with chronic hepatitis C infection were nearly four times more likely than other health system patients to be hospitalized, and not only with liver-related problems.
An observational cohort study of 10,131 patients with chronic hepatitis C infection (the Chronic Hepatitis Cohort Study) and 20,262 health system patients showed the overall hospitalization rate was 3.7 times higher in patients with chronic hepatitis C.
The study, published online May 15 in the Journal of Viral Hepatitis, found patients with chronic hepatitis C experienced an average of 3.5 hospitalizations over a mean of 5.5 years follow-up, compared with 1.9 hospitalizations in other patients over an average of 4.8 years. Investigators excluded HCV patients with HIV or hepatitis B coinfection, or who had received a liver transplant.
Hospitalization rates in both groups were significantly higher among patients who were older than 65 years, black, or who had a household income less than $15,000 per year (J Viral Hepat. 2016 May 15. doi: 10.1111/jvh.12548).
Patients with chronic hepatitis C had a nearly 25-fold greater risk of being hospitalized with liver-related conditions, compared with other health system patients.
“Liver-related conditions are the third leading cause of nonsurgical hospitalizations of chronic HCV patients after cardiovascular diseases and infections,” wrote Dr. E. H. Teshale, from the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta, and coauthors.
However liver-related complications only accounted for 9.1% of all hospitalizations in this group, compared with 1.3% of hospitalizations in the control group.
The analysis also revealed a sixfold greater risk of hospitalization for infection, a sevenfold greater risk for dermatologic and hematologic problems, a 10-fold greater risk of hospitalization for substance abuse, and a nearly threefold greater risk of being hospitalized for cardiovascular disease, compared with other health system patients.
Hospitalizations were significantly lower among patients receiving treatment for hepatitis C and who had achieved a sustained virologic response, the authors noted.
“Initiation of treatment prior to progression to advanced liver disease can reduce the cost of hospitalization, which in many cases may include repeated hospitalizations and other costly interventions,” the investigators reported. “Some studies have found a significant health care cost alleviation following HCV therapy, which [was] primarily due to costs associated with hospitalizations for non-HCV–related comorbidities.”
The Chronic Hepatitis Cohort Study was funded by the CDC Foundation, which receives grants from a range of pharmaceutical companies. No other conflicts of interest were declared.
People with chronic hepatitis C infection were nearly four times more likely than other health system patients to be hospitalized, and not only with liver-related problems.
An observational cohort study of 10,131 patients with chronic hepatitis C infection (the Chronic Hepatitis Cohort Study) and 20,262 health system patients showed the overall hospitalization rate was 3.7 times higher in patients with chronic hepatitis C.
The study, published online May 15 in the Journal of Viral Hepatitis, found patients with chronic hepatitis C experienced an average of 3.5 hospitalizations over a mean of 5.5 years follow-up, compared with 1.9 hospitalizations in other patients over an average of 4.8 years. Investigators excluded HCV patients with HIV or hepatitis B coinfection, or who had received a liver transplant.
Hospitalization rates in both groups were significantly higher among patients who were older than 65 years, black, or who had a household income less than $15,000 per year (J Viral Hepat. 2016 May 15. doi: 10.1111/jvh.12548).
Patients with chronic hepatitis C had a nearly 25-fold greater risk of being hospitalized with liver-related conditions, compared with other health system patients.
“Liver-related conditions are the third leading cause of nonsurgical hospitalizations of chronic HCV patients after cardiovascular diseases and infections,” wrote Dr. E. H. Teshale, from the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta, and coauthors.
However liver-related complications only accounted for 9.1% of all hospitalizations in this group, compared with 1.3% of hospitalizations in the control group.
The analysis also revealed a sixfold greater risk of hospitalization for infection, a sevenfold greater risk for dermatologic and hematologic problems, a 10-fold greater risk of hospitalization for substance abuse, and a nearly threefold greater risk of being hospitalized for cardiovascular disease, compared with other health system patients.
Hospitalizations were significantly lower among patients receiving treatment for hepatitis C and who had achieved a sustained virologic response, the authors noted.
“Initiation of treatment prior to progression to advanced liver disease can reduce the cost of hospitalization, which in many cases may include repeated hospitalizations and other costly interventions,” the investigators reported. “Some studies have found a significant health care cost alleviation following HCV therapy, which [was] primarily due to costs associated with hospitalizations for non-HCV–related comorbidities.”
The Chronic Hepatitis Cohort Study was funded by the CDC Foundation, which receives grants from a range of pharmaceutical companies. No other conflicts of interest were declared.
FROM THE JOURNAL OF VIRAL HEPATITIS
Key clinical point: Individuals with chronic hepatitis C infection have significantly greater risk of hospitalization for a range of health issues than other health system patients.
Major finding: The risk of hospitalization was 3.7 times greater in individuals with chronic hepatitis C infection, compared with general health system patients.
Data source: An observational cohort study in 10,131 patients with chronic hepatitis C infection (the Chronic Hepatitis Cohort Study) and 20,262 other health system patients.
Disclosures: The Chronic Hepatitis Cohort Study was funded by the CDC Foundation, which receives grants from a range of pharmaceutical companies. No other conflicts of interest were declared.
Hepatitis A and B combo vaccinations remain effective after 15 years
Young adults who received a combined hepatitis A and B vaccination at age 12-15 years maintained immunity after 15 years, making a booster shot unnecessary, according to Dr. Jiri Beran of the Vaccination and Travel Medicine Centre, Hradec Kralove, Czech Republic, and associates.
Study participants received either a 2-dose adult formulation or a 3-dose pediatric formulation. Of the 162 participants included in the 15-year follow-up, all were seropositive for anti–hepatitis A vaccine antibodies, 81.1% of those who received the two-dose vaccination had anti–hepatitis B antibodies, and 81.8% of those who received the three-dose vaccination had anti–hepatitis B antibodies.
In a subsequent hepatitis B vaccine challenge, all of 8 participants who received the two-dose vaccination and 10 of 11 participants who received the three-dose vaccination developed an anamnastic response. No side effects inconsistent with previous experience were observed.
“The present study confirms that the combined hepatitis A and B vaccine is equally immunogenic and safe in adolescents when administered as the standard three-dose pediatric regimen or as two doses of the adult strength vacciwne,” the investigators said.
Find the full study in Vaccine (doi: 10.1016/j.vaccine.2016.04.033).
Young adults who received a combined hepatitis A and B vaccination at age 12-15 years maintained immunity after 15 years, making a booster shot unnecessary, according to Dr. Jiri Beran of the Vaccination and Travel Medicine Centre, Hradec Kralove, Czech Republic, and associates.
Study participants received either a 2-dose adult formulation or a 3-dose pediatric formulation. Of the 162 participants included in the 15-year follow-up, all were seropositive for anti–hepatitis A vaccine antibodies, 81.1% of those who received the two-dose vaccination had anti–hepatitis B antibodies, and 81.8% of those who received the three-dose vaccination had anti–hepatitis B antibodies.
In a subsequent hepatitis B vaccine challenge, all of 8 participants who received the two-dose vaccination and 10 of 11 participants who received the three-dose vaccination developed an anamnastic response. No side effects inconsistent with previous experience were observed.
“The present study confirms that the combined hepatitis A and B vaccine is equally immunogenic and safe in adolescents when administered as the standard three-dose pediatric regimen or as two doses of the adult strength vacciwne,” the investigators said.
Find the full study in Vaccine (doi: 10.1016/j.vaccine.2016.04.033).
Young adults who received a combined hepatitis A and B vaccination at age 12-15 years maintained immunity after 15 years, making a booster shot unnecessary, according to Dr. Jiri Beran of the Vaccination and Travel Medicine Centre, Hradec Kralove, Czech Republic, and associates.
Study participants received either a 2-dose adult formulation or a 3-dose pediatric formulation. Of the 162 participants included in the 15-year follow-up, all were seropositive for anti–hepatitis A vaccine antibodies, 81.1% of those who received the two-dose vaccination had anti–hepatitis B antibodies, and 81.8% of those who received the three-dose vaccination had anti–hepatitis B antibodies.
In a subsequent hepatitis B vaccine challenge, all of 8 participants who received the two-dose vaccination and 10 of 11 participants who received the three-dose vaccination developed an anamnastic response. No side effects inconsistent with previous experience were observed.
“The present study confirms that the combined hepatitis A and B vaccine is equally immunogenic and safe in adolescents when administered as the standard three-dose pediatric regimen or as two doses of the adult strength vacciwne,” the investigators said.
Find the full study in Vaccine (doi: 10.1016/j.vaccine.2016.04.033).
FROM VACCINE
Hepatitis B vaccine in infancy provides long-term protection into adolescence
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
FROM VACCINE
Initiative dramatically raises HCV screening, treatment
A hepatitis C awareness initiative dramatically raised the rate of HCV screening and treatment in a large American Indian population – the ethnic group with the highest rate of HCV infection and HCV-related mortality in the United States, according to a report published May 13 in Morbidity and Mortality Weekly Report.
Cherokee Nation Health Services undertook the effort in 2012 to improve detection and management of HCV. It included a reminder in eligible patients’ electronic health records (EHRs) to offer screening; HCV education for primary care physicians and other health care providers; establishment of an HCV registry to monitor the clinical care of patients who initiated antiviral treatment; and outreach efforts by public health nurses to HCV patients, including home visits.
In 2014, an additional initiative was implemented to expand services for the rapidly increasing number of patients diagnosed as having HCV. This allowed a transition from having a single clinic staffed by only one caregiver with expertise in HCV management to five clinics staffed by three physicians, two nurse practitioners, and two pharmacists with HCV expertise, said Dr. Jorge Mera, director of infectious diseases, Cherokee Nation Health Services, Tulsa, Okla., and his associates.
An analysis of deidentified data in the HCV registry and EHRs showed that 92,012 patients aged 20 years and older had at least one visit with Cherokee Nation Health Services after the program was implemented, between October 2012 and July 2015. The proportion of this patient population that was tested for HCV antibodies rose fivefold, from 3.6% to 18.2% during the study period. A total of 715 patients were antibody positive, and 388 of them were found to have chronic HCV infection. Approximately 60% of these patients initiated antiviral treatment, and approximately 90% of them achieved a sustained virologic response and were essentially cured, Dr. Mera and his associates said (MMWR. 2016 May 13;65[18]:461-6).
The program included a component that particularly targeted baby boomers – patients born between 1945 and 1965 – for HCV screening. Across the Indian Health Service clinics in 34 states that adopted this component of the program, such screening increased fourfold in this high-risk population during the study period (MMWR. 2016 May 13;65[18]:467-9).
These efforts, the first of their kind in the United States, may help eliminate hepatitis C as a health disparity for American Indian/Alaska Native populations and also may serve as a model for other health care settings, the investigators added.
A hepatitis C awareness initiative dramatically raised the rate of HCV screening and treatment in a large American Indian population – the ethnic group with the highest rate of HCV infection and HCV-related mortality in the United States, according to a report published May 13 in Morbidity and Mortality Weekly Report.
Cherokee Nation Health Services undertook the effort in 2012 to improve detection and management of HCV. It included a reminder in eligible patients’ electronic health records (EHRs) to offer screening; HCV education for primary care physicians and other health care providers; establishment of an HCV registry to monitor the clinical care of patients who initiated antiviral treatment; and outreach efforts by public health nurses to HCV patients, including home visits.
In 2014, an additional initiative was implemented to expand services for the rapidly increasing number of patients diagnosed as having HCV. This allowed a transition from having a single clinic staffed by only one caregiver with expertise in HCV management to five clinics staffed by three physicians, two nurse practitioners, and two pharmacists with HCV expertise, said Dr. Jorge Mera, director of infectious diseases, Cherokee Nation Health Services, Tulsa, Okla., and his associates.
An analysis of deidentified data in the HCV registry and EHRs showed that 92,012 patients aged 20 years and older had at least one visit with Cherokee Nation Health Services after the program was implemented, between October 2012 and July 2015. The proportion of this patient population that was tested for HCV antibodies rose fivefold, from 3.6% to 18.2% during the study period. A total of 715 patients were antibody positive, and 388 of them were found to have chronic HCV infection. Approximately 60% of these patients initiated antiviral treatment, and approximately 90% of them achieved a sustained virologic response and were essentially cured, Dr. Mera and his associates said (MMWR. 2016 May 13;65[18]:461-6).
The program included a component that particularly targeted baby boomers – patients born between 1945 and 1965 – for HCV screening. Across the Indian Health Service clinics in 34 states that adopted this component of the program, such screening increased fourfold in this high-risk population during the study period (MMWR. 2016 May 13;65[18]:467-9).
These efforts, the first of their kind in the United States, may help eliminate hepatitis C as a health disparity for American Indian/Alaska Native populations and also may serve as a model for other health care settings, the investigators added.
A hepatitis C awareness initiative dramatically raised the rate of HCV screening and treatment in a large American Indian population – the ethnic group with the highest rate of HCV infection and HCV-related mortality in the United States, according to a report published May 13 in Morbidity and Mortality Weekly Report.
Cherokee Nation Health Services undertook the effort in 2012 to improve detection and management of HCV. It included a reminder in eligible patients’ electronic health records (EHRs) to offer screening; HCV education for primary care physicians and other health care providers; establishment of an HCV registry to monitor the clinical care of patients who initiated antiviral treatment; and outreach efforts by public health nurses to HCV patients, including home visits.
In 2014, an additional initiative was implemented to expand services for the rapidly increasing number of patients diagnosed as having HCV. This allowed a transition from having a single clinic staffed by only one caregiver with expertise in HCV management to five clinics staffed by three physicians, two nurse practitioners, and two pharmacists with HCV expertise, said Dr. Jorge Mera, director of infectious diseases, Cherokee Nation Health Services, Tulsa, Okla., and his associates.
An analysis of deidentified data in the HCV registry and EHRs showed that 92,012 patients aged 20 years and older had at least one visit with Cherokee Nation Health Services after the program was implemented, between October 2012 and July 2015. The proportion of this patient population that was tested for HCV antibodies rose fivefold, from 3.6% to 18.2% during the study period. A total of 715 patients were antibody positive, and 388 of them were found to have chronic HCV infection. Approximately 60% of these patients initiated antiviral treatment, and approximately 90% of them achieved a sustained virologic response and were essentially cured, Dr. Mera and his associates said (MMWR. 2016 May 13;65[18]:461-6).
The program included a component that particularly targeted baby boomers – patients born between 1945 and 1965 – for HCV screening. Across the Indian Health Service clinics in 34 states that adopted this component of the program, such screening increased fourfold in this high-risk population during the study period (MMWR. 2016 May 13;65[18]:467-9).
These efforts, the first of their kind in the United States, may help eliminate hepatitis C as a health disparity for American Indian/Alaska Native populations and also may serve as a model for other health care settings, the investigators added.
FROM MORBIDITY and MORTALITY WEEKLY REPORT
Key clinical point: A new program dramatically raised the rate of HCV screening and treatment in a large American Indian population – the ethnic group with the highest rate of HCV infection and HCV-related mortality in the United States.
Major finding: The proportion of adults tested for HCV antibodies rose fivefold, from 3.6% to 18.2%, during the study period.
Data source: An observational cohort study involving 92,012 adults who had at least 1 visit to Cherokee Nation Health Services between October 2012 and July 2015.
Disclosures: The sponsor of this study was not specified, and potential financial conflicts of interest were not provided. The authors were affiliated with Cherokee Nation Health Services, the U.S. Centers for Disease Control and Prevention, the University of Oklahoma Health Sciences Center, the Oklahoma City Veterans Affairs Medical Center, the Indian Health Service, and the Northwest Portland (Ore.) Area Indian Health Board.
FDA publishes draft guidance for developing HCV antivirals
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
Hepatitis Outlook: April 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month covering a variety of the major hepatitis viruses.
Elderly patients with chronic hepatitis C disease are more likely to develop hepatocellular carcinoma (HCC) than younger patients, but they have traditionally received less antiviral treatment than younger patients, according to a study in the Journal of Viral Hepatitis. However, receipt of curative treatment is associated with a benefit in reducing cirrhosis, HCC, and overall mortality, irrespective of age, investigators said.
A report in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report from the Texas Department of State Health Services detailed how the agency dealt with a health care–associated hepatitis A outbreak in August 2015.
Researchers at McGill University in Montreal have developed a portable, paper-based electrochemical platform with multiplexing and telemedicine capabilities that may enable low-cost, point-of-care diagnosis of hepatitis C virus (HCV) and HIV co-infections within serum samples.
A study of patients at a gastroenterology clinic in Cameroon found that almost 40% of patients who were anti-hepatitis C virus antibody-positive were also asymptomatic, and some already presented with complications, including cirrhosis and hepatocellular carcinoma. The authors highlighted an urgent need to put in place programs to increase awareness and diagnosis of HCV infection in the country.
Chronic hepatitis C virus infection is an independent risk factor for osteoporosis and fractures among HIV-infected patients, even before the development of cirrhosis, according to a review of epidemiologic studies.
Quantitative maternal surface antigen (HBsAg) predicts hepatitis B virus infection in infants as well as maternal viral load does, according to a study in Hepatology. The authors conclude that antiviral therapy may be considered in pregnant women with an HBsAg level above 4-4.5 log10 IU/mL to interrupt mother-to-infant transmission.
A comprehensive literature review of cited WHO estimates for hepatitis B virus (HBV), HCV, and HIV co-infection between 2010 and 2014 showed that a wide range of co-infection estimates have been quoted using different WHO estimates. The authors detail the most recent, appropriate WHO estimates that should be used going forward.
A Chinese cohort study found that isolated anti-HBc–positive subjects can achieve good immune responses after hepatitis B vaccination, and the positive seroprotection rate and geometric mean titer (GMT) level for anti-HBs were lower than in a control group. Better responses were observed in young adults, the study authors said, and significant negative correlations were found between GMT of anti-HBc before vaccination and GMT of anti-HBs after vaccination.
New research indicates that evidence of long-lasting cellular immunity, regardless of anti-hepatitis B surface antigen level, suggests that protection afforded by primary immunization with plasma-derived hepatitis B vaccine during childhood and adulthood lasts at least 32 years.
Increased knowledge of hepatitis B cognition is an effective way for improving hepatitis B vaccination behavior and hepatitis B vaccination willingness of migrant workers, report the authors of a study in Human Vaccines & Immunotherapeutics. The researchers also found that health intervention policies should focus on older migrants (age at least 46 years) without medical insurance, with poorer self-reported health status, and poor health services accessibility.
Hepatitis B virus antibodies and galactomannan enzyme immunoassay (GM-EIA) positivity are common in patients receiving intravenous immunoglobulin and may confound diagnostic results, according to a study in Clinical Infectious Diseases.
Researchers in Niger have identified two recombinant hepatitis B virus forms and rare genotypic patterns that may affect hepatitis B surface antigen antigenicity and improve current knowledge of epidemiological, clinical, and virological patterns of hepatitis B in that country.
As viral hepatitis can be life threatening in patients with hematological malignancy, a new study suggests that all patients should be screened for hepatotropic viruses before hematological treatment, and that patients or hemopoietic stem cell donors with markers of past or current viral hepatitis should be assessed by an expert. The study also includes screening, vaccination, and treatment rules.
A study published in JAIDS suggests that lamivudine (3TC) monotherapy-based combination antiretroviral therapy is efficacious for hepatitis B virus treatment through 48 weeks in HIV/HBV coinfection, when baseline HBV DNA is less than 20,000 IU/mL.
Chinese researchers observed a significant elevation in CD4+Foxp3+ regulatory T-cells (Treg) in the peripheral blood of chronic hepatitis C patients, compared with healthy donors, in a study published in the International Journal of Infectious Diseases. The results demonstrate a decreasing trend in activated Treg cells after treatment with interferon alpha and ribavirin in vitro, the investigators also said.
Research published in Hepatology suggests hepatitis B virus e antigen (HBeAg) and its precursors promote HDM2-mediated degradation and impair the transcriptional activity of tumor suppressor p53 via interacting with the NUMB gene, consequently contributing to hepatocellular carcinoma development.
A systematic review of recent hepatitis B vaccine research highlighted the importance of introducing HBV vaccination not only for an infant universal vaccination program, but also for other settings in which patients are affected by communicable and noncommunicable diseases.
A “real-world” cohort study of 4,365 genotype 1 treatment-naïve hepatitis C virus–infected veterans treated with ledipasvir/sofosbuvir with or without ribavirin found that sustained virologic response (SVR) rates in the cohort nearly matched the SVR rates reported in clinical trials and were consistently high across all subgroups. Investigators found that noncirrhotics with HCV RNA less than 6,000,000 IU/mL were less likely to achieve SVR with 8 weeks, compared with 12 weeks of therapy, although the numeric difference in SVR rates was small.
A study in the Journal of Viral Hepatitis demonstrated that the DC-targeting protein has the ability to improve the immunogenicity and the antiviral activity of the hepatitis B DNA vaccine pSVK-HBVA, and that the DC-targeting protein can be a potential method for the delivery of DNA vaccines directly to DCs.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month covering a variety of the major hepatitis viruses.
Elderly patients with chronic hepatitis C disease are more likely to develop hepatocellular carcinoma (HCC) than younger patients, but they have traditionally received less antiviral treatment than younger patients, according to a study in the Journal of Viral Hepatitis. However, receipt of curative treatment is associated with a benefit in reducing cirrhosis, HCC, and overall mortality, irrespective of age, investigators said.
A report in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report from the Texas Department of State Health Services detailed how the agency dealt with a health care–associated hepatitis A outbreak in August 2015.
Researchers at McGill University in Montreal have developed a portable, paper-based electrochemical platform with multiplexing and telemedicine capabilities that may enable low-cost, point-of-care diagnosis of hepatitis C virus (HCV) and HIV co-infections within serum samples.
A study of patients at a gastroenterology clinic in Cameroon found that almost 40% of patients who were anti-hepatitis C virus antibody-positive were also asymptomatic, and some already presented with complications, including cirrhosis and hepatocellular carcinoma. The authors highlighted an urgent need to put in place programs to increase awareness and diagnosis of HCV infection in the country.
Chronic hepatitis C virus infection is an independent risk factor for osteoporosis and fractures among HIV-infected patients, even before the development of cirrhosis, according to a review of epidemiologic studies.
Quantitative maternal surface antigen (HBsAg) predicts hepatitis B virus infection in infants as well as maternal viral load does, according to a study in Hepatology. The authors conclude that antiviral therapy may be considered in pregnant women with an HBsAg level above 4-4.5 log10 IU/mL to interrupt mother-to-infant transmission.
A comprehensive literature review of cited WHO estimates for hepatitis B virus (HBV), HCV, and HIV co-infection between 2010 and 2014 showed that a wide range of co-infection estimates have been quoted using different WHO estimates. The authors detail the most recent, appropriate WHO estimates that should be used going forward.
A Chinese cohort study found that isolated anti-HBc–positive subjects can achieve good immune responses after hepatitis B vaccination, and the positive seroprotection rate and geometric mean titer (GMT) level for anti-HBs were lower than in a control group. Better responses were observed in young adults, the study authors said, and significant negative correlations were found between GMT of anti-HBc before vaccination and GMT of anti-HBs after vaccination.
New research indicates that evidence of long-lasting cellular immunity, regardless of anti-hepatitis B surface antigen level, suggests that protection afforded by primary immunization with plasma-derived hepatitis B vaccine during childhood and adulthood lasts at least 32 years.
Increased knowledge of hepatitis B cognition is an effective way for improving hepatitis B vaccination behavior and hepatitis B vaccination willingness of migrant workers, report the authors of a study in Human Vaccines & Immunotherapeutics. The researchers also found that health intervention policies should focus on older migrants (age at least 46 years) without medical insurance, with poorer self-reported health status, and poor health services accessibility.
Hepatitis B virus antibodies and galactomannan enzyme immunoassay (GM-EIA) positivity are common in patients receiving intravenous immunoglobulin and may confound diagnostic results, according to a study in Clinical Infectious Diseases.
Researchers in Niger have identified two recombinant hepatitis B virus forms and rare genotypic patterns that may affect hepatitis B surface antigen antigenicity and improve current knowledge of epidemiological, clinical, and virological patterns of hepatitis B in that country.
As viral hepatitis can be life threatening in patients with hematological malignancy, a new study suggests that all patients should be screened for hepatotropic viruses before hematological treatment, and that patients or hemopoietic stem cell donors with markers of past or current viral hepatitis should be assessed by an expert. The study also includes screening, vaccination, and treatment rules.
A study published in JAIDS suggests that lamivudine (3TC) monotherapy-based combination antiretroviral therapy is efficacious for hepatitis B virus treatment through 48 weeks in HIV/HBV coinfection, when baseline HBV DNA is less than 20,000 IU/mL.
Chinese researchers observed a significant elevation in CD4+Foxp3+ regulatory T-cells (Treg) in the peripheral blood of chronic hepatitis C patients, compared with healthy donors, in a study published in the International Journal of Infectious Diseases. The results demonstrate a decreasing trend in activated Treg cells after treatment with interferon alpha and ribavirin in vitro, the investigators also said.
Research published in Hepatology suggests hepatitis B virus e antigen (HBeAg) and its precursors promote HDM2-mediated degradation and impair the transcriptional activity of tumor suppressor p53 via interacting with the NUMB gene, consequently contributing to hepatocellular carcinoma development.
A systematic review of recent hepatitis B vaccine research highlighted the importance of introducing HBV vaccination not only for an infant universal vaccination program, but also for other settings in which patients are affected by communicable and noncommunicable diseases.
A “real-world” cohort study of 4,365 genotype 1 treatment-naïve hepatitis C virus–infected veterans treated with ledipasvir/sofosbuvir with or without ribavirin found that sustained virologic response (SVR) rates in the cohort nearly matched the SVR rates reported in clinical trials and were consistently high across all subgroups. Investigators found that noncirrhotics with HCV RNA less than 6,000,000 IU/mL were less likely to achieve SVR with 8 weeks, compared with 12 weeks of therapy, although the numeric difference in SVR rates was small.
A study in the Journal of Viral Hepatitis demonstrated that the DC-targeting protein has the ability to improve the immunogenicity and the antiviral activity of the hepatitis B DNA vaccine pSVK-HBVA, and that the DC-targeting protein can be a potential method for the delivery of DNA vaccines directly to DCs.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month covering a variety of the major hepatitis viruses.
Elderly patients with chronic hepatitis C disease are more likely to develop hepatocellular carcinoma (HCC) than younger patients, but they have traditionally received less antiviral treatment than younger patients, according to a study in the Journal of Viral Hepatitis. However, receipt of curative treatment is associated with a benefit in reducing cirrhosis, HCC, and overall mortality, irrespective of age, investigators said.
A report in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report from the Texas Department of State Health Services detailed how the agency dealt with a health care–associated hepatitis A outbreak in August 2015.
Researchers at McGill University in Montreal have developed a portable, paper-based electrochemical platform with multiplexing and telemedicine capabilities that may enable low-cost, point-of-care diagnosis of hepatitis C virus (HCV) and HIV co-infections within serum samples.
A study of patients at a gastroenterology clinic in Cameroon found that almost 40% of patients who were anti-hepatitis C virus antibody-positive were also asymptomatic, and some already presented with complications, including cirrhosis and hepatocellular carcinoma. The authors highlighted an urgent need to put in place programs to increase awareness and diagnosis of HCV infection in the country.
Chronic hepatitis C virus infection is an independent risk factor for osteoporosis and fractures among HIV-infected patients, even before the development of cirrhosis, according to a review of epidemiologic studies.
Quantitative maternal surface antigen (HBsAg) predicts hepatitis B virus infection in infants as well as maternal viral load does, according to a study in Hepatology. The authors conclude that antiviral therapy may be considered in pregnant women with an HBsAg level above 4-4.5 log10 IU/mL to interrupt mother-to-infant transmission.
A comprehensive literature review of cited WHO estimates for hepatitis B virus (HBV), HCV, and HIV co-infection between 2010 and 2014 showed that a wide range of co-infection estimates have been quoted using different WHO estimates. The authors detail the most recent, appropriate WHO estimates that should be used going forward.
A Chinese cohort study found that isolated anti-HBc–positive subjects can achieve good immune responses after hepatitis B vaccination, and the positive seroprotection rate and geometric mean titer (GMT) level for anti-HBs were lower than in a control group. Better responses were observed in young adults, the study authors said, and significant negative correlations were found between GMT of anti-HBc before vaccination and GMT of anti-HBs after vaccination.
New research indicates that evidence of long-lasting cellular immunity, regardless of anti-hepatitis B surface antigen level, suggests that protection afforded by primary immunization with plasma-derived hepatitis B vaccine during childhood and adulthood lasts at least 32 years.
Increased knowledge of hepatitis B cognition is an effective way for improving hepatitis B vaccination behavior and hepatitis B vaccination willingness of migrant workers, report the authors of a study in Human Vaccines & Immunotherapeutics. The researchers also found that health intervention policies should focus on older migrants (age at least 46 years) without medical insurance, with poorer self-reported health status, and poor health services accessibility.
Hepatitis B virus antibodies and galactomannan enzyme immunoassay (GM-EIA) positivity are common in patients receiving intravenous immunoglobulin and may confound diagnostic results, according to a study in Clinical Infectious Diseases.
Researchers in Niger have identified two recombinant hepatitis B virus forms and rare genotypic patterns that may affect hepatitis B surface antigen antigenicity and improve current knowledge of epidemiological, clinical, and virological patterns of hepatitis B in that country.
As viral hepatitis can be life threatening in patients with hematological malignancy, a new study suggests that all patients should be screened for hepatotropic viruses before hematological treatment, and that patients or hemopoietic stem cell donors with markers of past or current viral hepatitis should be assessed by an expert. The study also includes screening, vaccination, and treatment rules.
A study published in JAIDS suggests that lamivudine (3TC) monotherapy-based combination antiretroviral therapy is efficacious for hepatitis B virus treatment through 48 weeks in HIV/HBV coinfection, when baseline HBV DNA is less than 20,000 IU/mL.
Chinese researchers observed a significant elevation in CD4+Foxp3+ regulatory T-cells (Treg) in the peripheral blood of chronic hepatitis C patients, compared with healthy donors, in a study published in the International Journal of Infectious Diseases. The results demonstrate a decreasing trend in activated Treg cells after treatment with interferon alpha and ribavirin in vitro, the investigators also said.
Research published in Hepatology suggests hepatitis B virus e antigen (HBeAg) and its precursors promote HDM2-mediated degradation and impair the transcriptional activity of tumor suppressor p53 via interacting with the NUMB gene, consequently contributing to hepatocellular carcinoma development.
A systematic review of recent hepatitis B vaccine research highlighted the importance of introducing HBV vaccination not only for an infant universal vaccination program, but also for other settings in which patients are affected by communicable and noncommunicable diseases.
A “real-world” cohort study of 4,365 genotype 1 treatment-naïve hepatitis C virus–infected veterans treated with ledipasvir/sofosbuvir with or without ribavirin found that sustained virologic response (SVR) rates in the cohort nearly matched the SVR rates reported in clinical trials and were consistently high across all subgroups. Investigators found that noncirrhotics with HCV RNA less than 6,000,000 IU/mL were less likely to achieve SVR with 8 weeks, compared with 12 weeks of therapy, although the numeric difference in SVR rates was small.
A study in the Journal of Viral Hepatitis demonstrated that the DC-targeting protein has the ability to improve the immunogenicity and the antiviral activity of the hepatitis B DNA vaccine pSVK-HBVA, and that the DC-targeting protein can be a potential method for the delivery of DNA vaccines directly to DCs.
On Twitter @richpizzi
Cirrhosis 30-day readmissions down 40% with quality improvement initiative
Using checklists and electronic decision support in an inpatient liver unit, quality improvement (QI) care protocols reduced 30-day readmissions of patients with cirrhosis by 40%, due mostly to a drop in readmissions for hepatic encephalopathy (HE) according to a report published in the May issue of Clinical Gastroenterology and Hepatology.
For patients initially admitted for overt HE, the 30-day readmission rate was 26.0% (27 of 104), compared with 48.9% (66 of 135) before implementation of QI. The proportion of total readmissions due to HE after QI was 9.6% (14 of 146), compared with 40.7% (79 of 194) before QI. In addition, length of stay for HE patients was significantly reduced (–1.34 days; 95% confidence interval, –2.38 to –0.32; P = .01). There were no significant changes in 90-day mortality.
Source: American Gastroenterological Association
“Our study advances the current literature on QI for patients with cirrhosis by presenting an inexpensive, easy to implement, and generalizable approach,” wrote Dr. Elliot Tapper of Beth Israel Deaconess Medical Center, Boston, and his colleagues. Previous studies have addressed readmission interventions among patients with cirrhosis, but the protocols required costly infrastructure, expertise, and institutional commitments. The current study supports the value of standard checklists and education, according to the investigators, “showing that outcomes improve further when checklist items are hard-wired into the ordering system.” (Clin Gastroenterol Hepatol. 2016 Apr 7. doi: 10.1016/j.cgh.2015.08.041).
The QI initiative encompassed several aspects of care. All HE patients were designated to receive rifaximin, and their lactulose dosing was adjusted to mental status using the Richmond Agitation and Sedation Scale. For patients with spontaneous bacterial peritonitis (SBP), timely administration of the correct dose of antibiotics and albumin was promoted, as were prophylactic measures for all patients, such as variceal hemorrhage prophylaxis and subcutaneous heparin for the prevention of venous thrombosis.
The three-part program entailed a run-in phase for preliminary checklist troubleshooting, a hand-held checklist phase, including the HE protocol, SBP treatment, and prophylactic measures, and a final electronic phase in which checklist items were incorporated into the hospital’s electronic provider order entry system using mandatory preset doses and linked medications.
Individual protocol items were demonstrated to affect the readmission rate. Rifaximin use for HE patients rose from 78.1% to 96.3%, and use of rifaximin was associated with lower adjusted odds of 30-day readmission (OR, 0.39; 95% CI, 0.16-0.87; P = .02). The dose/frequency of lactulose for HE patients increased, and patients who had 6 or more cups of lactulose on the day of their readmission had significantly lower adjusted length of stay (–2.36 days; 95% CI, –3.40 to –1.31; P less than .0001). Patients taking SBP prophylaxis had lower readmission rates (OR, 0.51; 95% CI, 0.31-0.83; P = .007).
The prospective study from 2011 to 2013 evaluated patients with cirrhosis who were admitted to the liver unit of Beth Israel Deaconess Medical Center, Boston. Patients were diagnosed with cirrhosis caused by hepatitis C (44.9%), alcoholic liver disease (34%), hepatitis B (5.4%), and biliary cirrhosis (1.8%). In total, 824 unique patients were admitted 1,720 times; 485 (58.9%) were admitted once, 268 (32.5%) were admitted 2-4 times, and 71 (8.6%) were admitted 5 or more times. The median length of stay for all patients was 4.0 days (interquartile range, 2.0-8.0).
Dr. Tapper and his coauthors reported having no disclosures.
Using checklists and electronic decision support in an inpatient liver unit, quality improvement (QI) care protocols reduced 30-day readmissions of patients with cirrhosis by 40%, due mostly to a drop in readmissions for hepatic encephalopathy (HE) according to a report published in the May issue of Clinical Gastroenterology and Hepatology.
For patients initially admitted for overt HE, the 30-day readmission rate was 26.0% (27 of 104), compared with 48.9% (66 of 135) before implementation of QI. The proportion of total readmissions due to HE after QI was 9.6% (14 of 146), compared with 40.7% (79 of 194) before QI. In addition, length of stay for HE patients was significantly reduced (–1.34 days; 95% confidence interval, –2.38 to –0.32; P = .01). There were no significant changes in 90-day mortality.
Source: American Gastroenterological Association
“Our study advances the current literature on QI for patients with cirrhosis by presenting an inexpensive, easy to implement, and generalizable approach,” wrote Dr. Elliot Tapper of Beth Israel Deaconess Medical Center, Boston, and his colleagues. Previous studies have addressed readmission interventions among patients with cirrhosis, but the protocols required costly infrastructure, expertise, and institutional commitments. The current study supports the value of standard checklists and education, according to the investigators, “showing that outcomes improve further when checklist items are hard-wired into the ordering system.” (Clin Gastroenterol Hepatol. 2016 Apr 7. doi: 10.1016/j.cgh.2015.08.041).
The QI initiative encompassed several aspects of care. All HE patients were designated to receive rifaximin, and their lactulose dosing was adjusted to mental status using the Richmond Agitation and Sedation Scale. For patients with spontaneous bacterial peritonitis (SBP), timely administration of the correct dose of antibiotics and albumin was promoted, as were prophylactic measures for all patients, such as variceal hemorrhage prophylaxis and subcutaneous heparin for the prevention of venous thrombosis.
The three-part program entailed a run-in phase for preliminary checklist troubleshooting, a hand-held checklist phase, including the HE protocol, SBP treatment, and prophylactic measures, and a final electronic phase in which checklist items were incorporated into the hospital’s electronic provider order entry system using mandatory preset doses and linked medications.
Individual protocol items were demonstrated to affect the readmission rate. Rifaximin use for HE patients rose from 78.1% to 96.3%, and use of rifaximin was associated with lower adjusted odds of 30-day readmission (OR, 0.39; 95% CI, 0.16-0.87; P = .02). The dose/frequency of lactulose for HE patients increased, and patients who had 6 or more cups of lactulose on the day of their readmission had significantly lower adjusted length of stay (–2.36 days; 95% CI, –3.40 to –1.31; P less than .0001). Patients taking SBP prophylaxis had lower readmission rates (OR, 0.51; 95% CI, 0.31-0.83; P = .007).
The prospective study from 2011 to 2013 evaluated patients with cirrhosis who were admitted to the liver unit of Beth Israel Deaconess Medical Center, Boston. Patients were diagnosed with cirrhosis caused by hepatitis C (44.9%), alcoholic liver disease (34%), hepatitis B (5.4%), and biliary cirrhosis (1.8%). In total, 824 unique patients were admitted 1,720 times; 485 (58.9%) were admitted once, 268 (32.5%) were admitted 2-4 times, and 71 (8.6%) were admitted 5 or more times. The median length of stay for all patients was 4.0 days (interquartile range, 2.0-8.0).
Dr. Tapper and his coauthors reported having no disclosures.
Using checklists and electronic decision support in an inpatient liver unit, quality improvement (QI) care protocols reduced 30-day readmissions of patients with cirrhosis by 40%, due mostly to a drop in readmissions for hepatic encephalopathy (HE) according to a report published in the May issue of Clinical Gastroenterology and Hepatology.
For patients initially admitted for overt HE, the 30-day readmission rate was 26.0% (27 of 104), compared with 48.9% (66 of 135) before implementation of QI. The proportion of total readmissions due to HE after QI was 9.6% (14 of 146), compared with 40.7% (79 of 194) before QI. In addition, length of stay for HE patients was significantly reduced (–1.34 days; 95% confidence interval, –2.38 to –0.32; P = .01). There were no significant changes in 90-day mortality.
Source: American Gastroenterological Association
“Our study advances the current literature on QI for patients with cirrhosis by presenting an inexpensive, easy to implement, and generalizable approach,” wrote Dr. Elliot Tapper of Beth Israel Deaconess Medical Center, Boston, and his colleagues. Previous studies have addressed readmission interventions among patients with cirrhosis, but the protocols required costly infrastructure, expertise, and institutional commitments. The current study supports the value of standard checklists and education, according to the investigators, “showing that outcomes improve further when checklist items are hard-wired into the ordering system.” (Clin Gastroenterol Hepatol. 2016 Apr 7. doi: 10.1016/j.cgh.2015.08.041).
The QI initiative encompassed several aspects of care. All HE patients were designated to receive rifaximin, and their lactulose dosing was adjusted to mental status using the Richmond Agitation and Sedation Scale. For patients with spontaneous bacterial peritonitis (SBP), timely administration of the correct dose of antibiotics and albumin was promoted, as were prophylactic measures for all patients, such as variceal hemorrhage prophylaxis and subcutaneous heparin for the prevention of venous thrombosis.
The three-part program entailed a run-in phase for preliminary checklist troubleshooting, a hand-held checklist phase, including the HE protocol, SBP treatment, and prophylactic measures, and a final electronic phase in which checklist items were incorporated into the hospital’s electronic provider order entry system using mandatory preset doses and linked medications.
Individual protocol items were demonstrated to affect the readmission rate. Rifaximin use for HE patients rose from 78.1% to 96.3%, and use of rifaximin was associated with lower adjusted odds of 30-day readmission (OR, 0.39; 95% CI, 0.16-0.87; P = .02). The dose/frequency of lactulose for HE patients increased, and patients who had 6 or more cups of lactulose on the day of their readmission had significantly lower adjusted length of stay (–2.36 days; 95% CI, –3.40 to –1.31; P less than .0001). Patients taking SBP prophylaxis had lower readmission rates (OR, 0.51; 95% CI, 0.31-0.83; P = .007).
The prospective study from 2011 to 2013 evaluated patients with cirrhosis who were admitted to the liver unit of Beth Israel Deaconess Medical Center, Boston. Patients were diagnosed with cirrhosis caused by hepatitis C (44.9%), alcoholic liver disease (34%), hepatitis B (5.4%), and biliary cirrhosis (1.8%). In total, 824 unique patients were admitted 1,720 times; 485 (58.9%) were admitted once, 268 (32.5%) were admitted 2-4 times, and 71 (8.6%) were admitted 5 or more times. The median length of stay for all patients was 4.0 days (interquartile range, 2.0-8.0).
Dr. Tapper and his coauthors reported having no disclosures.
Key clinical point: Care protocols implemented by electronic decision support reduced 30-day readmissions of patients with cirrhosis by 40% in an inpatient liver unit.
Major finding: The drop was likely driven by fewer readmissions for hepatic encephalopathy (HE): the 30-day HE readmission rate was 26.0% (27 of 104), compared with 48.9% (66 of 135) before implementation of quality improvement.
Data sources: The prospective study evaluated 824 patients who were admitted 1,720 times to the liver unit of Beth Israel Deaconess Medical Center, Boston.
Disclosures: Dr. Tapper and his coauthors reported having no disclosures.
Study: Few HCV-infected heroin users linked to outpatient care
The results of a hepatitis C virus screening program in a suburban New Jersey acute opioid detoxification program reveal that, despite the ease of access to HCV screening and the availability of curative therapies, linkage to care after detection of infection in persons who inject drugs continues to present a challenge.
Eda Akyar, a clinical research coordinator at ID Care, New Jersey’s largest network of infectious disease specialists, and her colleagues examined the results of an HIV, HCV, and HBV infection screening program instituted between Oct. 1, 2014, and June 9, 2015, for patients admitted to an acute opioid detoxification program at Princeton House in suburban New Jersey. Study goals included assessing the prevalence of HIV, HCV, and HBV infections for these patients, the HCV genotype (GT) carried, and the subsequent linkage to care after discharge from the program. The report was published online April 13 in Emerging Infectious Diseases.
During the screening period, patients representing 10 of New Jersey’s 21 counties were tested for the presence of HCV antibodies. Approximately two-thirds of all study participants (66.6%) were between 17 and 35 years of age. In this important age demographic, 237 patients (41.4%) screened positive for HCV antibodies, and 187 were available for further study.
HCV viral load data were available from 172 patients (92.0%), with approximately one-fifth (18.6%) screening undetectable. The HCV GTs obtained from 102 patients revealed that most (62.7%) were GT1a, followed by GT3 (25.5%). In a very surprising result, all HCV antibody positive patients were also HIV antibody negative, the researchers noted.
Regarding linkage to care, 16 of the patients (8.6%) in the 17- to 35-year-old age group attended outpatient follow-up appointments, with three (1.6%) starting on an oral, direct-acting antiviral treatment regimen. Two of these three patients were nonadherent to their treatment regimens. Two additional patients expressed willingness to accept treatment, but were denied their prescriptions by their insurance providers. None of the other participants returned for continued care.
The authors said that their results indicated a high prevalence of HCV among young suburban heroin users attending an acute detoxification program serving a wide geographic area, suggesting that New Jersey is part of the second wave of HCV infection following that seen in those born from 1946 to 1964. They also highlighted their findings of a GT3 prevalence more than twice the national average, a complete lack of HIV infection in a population known to be susceptible to it, and disappointing linkage to care outcomes.
The authors said that easy-to-use curative therapy should underscore a need for improved linkage to care and treatment of HCV-infected persons who inject drugs as part of an important public health effort to prevent its continued spread.
This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. Conflict of interest information was not disclosed.
The results of a hepatitis C virus screening program in a suburban New Jersey acute opioid detoxification program reveal that, despite the ease of access to HCV screening and the availability of curative therapies, linkage to care after detection of infection in persons who inject drugs continues to present a challenge.
Eda Akyar, a clinical research coordinator at ID Care, New Jersey’s largest network of infectious disease specialists, and her colleagues examined the results of an HIV, HCV, and HBV infection screening program instituted between Oct. 1, 2014, and June 9, 2015, for patients admitted to an acute opioid detoxification program at Princeton House in suburban New Jersey. Study goals included assessing the prevalence of HIV, HCV, and HBV infections for these patients, the HCV genotype (GT) carried, and the subsequent linkage to care after discharge from the program. The report was published online April 13 in Emerging Infectious Diseases.
During the screening period, patients representing 10 of New Jersey’s 21 counties were tested for the presence of HCV antibodies. Approximately two-thirds of all study participants (66.6%) were between 17 and 35 years of age. In this important age demographic, 237 patients (41.4%) screened positive for HCV antibodies, and 187 were available for further study.
HCV viral load data were available from 172 patients (92.0%), with approximately one-fifth (18.6%) screening undetectable. The HCV GTs obtained from 102 patients revealed that most (62.7%) were GT1a, followed by GT3 (25.5%). In a very surprising result, all HCV antibody positive patients were also HIV antibody negative, the researchers noted.
Regarding linkage to care, 16 of the patients (8.6%) in the 17- to 35-year-old age group attended outpatient follow-up appointments, with three (1.6%) starting on an oral, direct-acting antiviral treatment regimen. Two of these three patients were nonadherent to their treatment regimens. Two additional patients expressed willingness to accept treatment, but were denied their prescriptions by their insurance providers. None of the other participants returned for continued care.
The authors said that their results indicated a high prevalence of HCV among young suburban heroin users attending an acute detoxification program serving a wide geographic area, suggesting that New Jersey is part of the second wave of HCV infection following that seen in those born from 1946 to 1964. They also highlighted their findings of a GT3 prevalence more than twice the national average, a complete lack of HIV infection in a population known to be susceptible to it, and disappointing linkage to care outcomes.
The authors said that easy-to-use curative therapy should underscore a need for improved linkage to care and treatment of HCV-infected persons who inject drugs as part of an important public health effort to prevent its continued spread.
This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. Conflict of interest information was not disclosed.
The results of a hepatitis C virus screening program in a suburban New Jersey acute opioid detoxification program reveal that, despite the ease of access to HCV screening and the availability of curative therapies, linkage to care after detection of infection in persons who inject drugs continues to present a challenge.
Eda Akyar, a clinical research coordinator at ID Care, New Jersey’s largest network of infectious disease specialists, and her colleagues examined the results of an HIV, HCV, and HBV infection screening program instituted between Oct. 1, 2014, and June 9, 2015, for patients admitted to an acute opioid detoxification program at Princeton House in suburban New Jersey. Study goals included assessing the prevalence of HIV, HCV, and HBV infections for these patients, the HCV genotype (GT) carried, and the subsequent linkage to care after discharge from the program. The report was published online April 13 in Emerging Infectious Diseases.
During the screening period, patients representing 10 of New Jersey’s 21 counties were tested for the presence of HCV antibodies. Approximately two-thirds of all study participants (66.6%) were between 17 and 35 years of age. In this important age demographic, 237 patients (41.4%) screened positive for HCV antibodies, and 187 were available for further study.
HCV viral load data were available from 172 patients (92.0%), with approximately one-fifth (18.6%) screening undetectable. The HCV GTs obtained from 102 patients revealed that most (62.7%) were GT1a, followed by GT3 (25.5%). In a very surprising result, all HCV antibody positive patients were also HIV antibody negative, the researchers noted.
Regarding linkage to care, 16 of the patients (8.6%) in the 17- to 35-year-old age group attended outpatient follow-up appointments, with three (1.6%) starting on an oral, direct-acting antiviral treatment regimen. Two of these three patients were nonadherent to their treatment regimens. Two additional patients expressed willingness to accept treatment, but were denied their prescriptions by their insurance providers. None of the other participants returned for continued care.
The authors said that their results indicated a high prevalence of HCV among young suburban heroin users attending an acute detoxification program serving a wide geographic area, suggesting that New Jersey is part of the second wave of HCV infection following that seen in those born from 1946 to 1964. They also highlighted their findings of a GT3 prevalence more than twice the national average, a complete lack of HIV infection in a population known to be susceptible to it, and disappointing linkage to care outcomes.
The authors said that easy-to-use curative therapy should underscore a need for improved linkage to care and treatment of HCV-infected persons who inject drugs as part of an important public health effort to prevent its continued spread.
This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. Conflict of interest information was not disclosed.
FROM EMERGING INFECTIOUS DISEASES
Key clinical point: Despite the ease of access to hepatitis C virus screening and the availability of curative therapies, linkage to care after detection of infection in persons who inject drugs continues to present a challenge, with larger implications for public health efforts to prevent its spread.
Major finding: Hepatitis C virus genotype 3 infection was highly prevalent in individuals who inject drugs who were participating in an acute heroin detoxification program serving a wide geographic area in suburban New Jersey.
Data sources: Patients admitted to Princeton House, a psychiatric facility in suburban New Jersey with an active opioid detoxification program, screened for hepatitis C virus between Oct. 1, 2014, and June 9, 2015.
Disclosures: This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. Conflict of interest information was not disclosed.
Hepatitis C virus transmission peaked in 1950
Iatrogenic factors, not high-risk behaviors, were the main cause of the exponential spread of hepatitis C virus infections in North America, according to a phylogenetic study published online in the Lancet Infectious Diseases.
The study shifted the epicenter of spread back by more than 15 years, to about 1950, when medical procedures were expanding after World War II at the same time that clinicians continued to reuse metal and glass syringes, said Dr. Jeffrey Joy of the British Columbia Centre for Excellence in HIV/AIDS, Vancouver, and his associates.
Exponential HCV transmission had mostly ended by 1965, negating “the idea that the epidemic among baby boomers and other demographic groups in North America is primarily due to injection drug use, unsafe tattooing, high-risk sex, and travel to high endemic areas during youth,” the researchers added.
The hepatitis C virus evolves rapidly, enabling researchers to characterize its spread based on the genetic divergence of infections. Dr. Joy and his associates studied 45,316 HCV genotype 1a sequences from the National Center for Biotechnology Information GenBank nucleotide database to carry out phylogenetic analyses of five HCV genes – E1, E2, NS2, NS4B, and NS5B (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]00124-9).
The combined results for all gene regions suggested that the North American HCV epidemic expanded the most between 1940 and 1965, and that transmission rates peaked in 1950, when the oldest baby boomers were only 5 years old. Thus, nosocomial transmission rather than risky behaviors was the likely driver behind most infections, the researchers said.
“Our results could help to reduce stigma related to screening and diagnosis of hepatitis C virus, potentially increasing the numbers of providers offering screening, patients accepting testing, and if positive, presenting for care and treatment,” the authors noted.
The researchers also found that HCV transmission rates plateaued between 1965 and 1989, and dropped in the early 1990s, coinciding with increases in blood product testing and needle exchange programs aimed at preventing HIV infections. Furthermore, HCV infections rose slightly after 2000, mirroring epidemiologic reports of outbreaks among young injection drug users in nonurban areas and among men who have sex with men, the researchers said.
The Canadian Institutes of Health Research, Michael Smith Foundation for Health Research, and BC Centre for Excellence in HIV/AIDS funded the study. The investigators disclosed no competing interests.
Dr. Jeffrey Joy and colleagues offer evidence that the era of high rates of transmission and rapid expansion of hepatitis C virus infections was from 1940 to 1960, when reuse of glass and metal syringes was common.
The authors conclude that attributing the spread of hepatitis C virus to the medical establishment, rather than youthful behavior long outgrown by most baby boomers, could justify changing the message around screening of baby boomers. Baby boomers came of age when nosocomial transmission could have been rampant. For this additional reason, rather than just individual behavior, all Americans born between 1945 and 1965 should be tested, say the authors.
This change of message, while effective, could backfire. By accepting responsibility for the pre-1960 spread, the medical establishment might increase stigma for patients born after the uptake of disposable syringes and safer clinical practices. Also, screening by birth cohort might already be outlasting its usefulness in some populations. Lowering the cost of hepatitis C virus testing could lead to routine, universal testing becoming the norm, making birth cohort testing obsolete.
Last, the novel method used in this study could be replaced by an even newer, more precise technology; would our message need to change once more?
Here are the facts: Hepatitis C virus is common among Americans born between 1945 and 1965. A current Centers for Disease Control and Prevention fact sheet asserts that most people infected with hepatitis C virus are unaware of their diagnosis, despite aggressive campaigns since 2012 to find cases. Let’s just go ahead and test our baby boomers.
Dr. Anne C. Spaulding and Dr. Lesley S. Miller are at the Rollins School of Public Health, Emory University, Atlanta. They reported receiving grants and other funding from Gilead Sciences and Bristol-Myers Squibb. These comments are from their editorial (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]30002-0).
Dr. Jeffrey Joy and colleagues offer evidence that the era of high rates of transmission and rapid expansion of hepatitis C virus infections was from 1940 to 1960, when reuse of glass and metal syringes was common.
The authors conclude that attributing the spread of hepatitis C virus to the medical establishment, rather than youthful behavior long outgrown by most baby boomers, could justify changing the message around screening of baby boomers. Baby boomers came of age when nosocomial transmission could have been rampant. For this additional reason, rather than just individual behavior, all Americans born between 1945 and 1965 should be tested, say the authors.
This change of message, while effective, could backfire. By accepting responsibility for the pre-1960 spread, the medical establishment might increase stigma for patients born after the uptake of disposable syringes and safer clinical practices. Also, screening by birth cohort might already be outlasting its usefulness in some populations. Lowering the cost of hepatitis C virus testing could lead to routine, universal testing becoming the norm, making birth cohort testing obsolete.
Last, the novel method used in this study could be replaced by an even newer, more precise technology; would our message need to change once more?
Here are the facts: Hepatitis C virus is common among Americans born between 1945 and 1965. A current Centers for Disease Control and Prevention fact sheet asserts that most people infected with hepatitis C virus are unaware of their diagnosis, despite aggressive campaigns since 2012 to find cases. Let’s just go ahead and test our baby boomers.
Dr. Anne C. Spaulding and Dr. Lesley S. Miller are at the Rollins School of Public Health, Emory University, Atlanta. They reported receiving grants and other funding from Gilead Sciences and Bristol-Myers Squibb. These comments are from their editorial (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]30002-0).
Dr. Jeffrey Joy and colleagues offer evidence that the era of high rates of transmission and rapid expansion of hepatitis C virus infections was from 1940 to 1960, when reuse of glass and metal syringes was common.
The authors conclude that attributing the spread of hepatitis C virus to the medical establishment, rather than youthful behavior long outgrown by most baby boomers, could justify changing the message around screening of baby boomers. Baby boomers came of age when nosocomial transmission could have been rampant. For this additional reason, rather than just individual behavior, all Americans born between 1945 and 1965 should be tested, say the authors.
This change of message, while effective, could backfire. By accepting responsibility for the pre-1960 spread, the medical establishment might increase stigma for patients born after the uptake of disposable syringes and safer clinical practices. Also, screening by birth cohort might already be outlasting its usefulness in some populations. Lowering the cost of hepatitis C virus testing could lead to routine, universal testing becoming the norm, making birth cohort testing obsolete.
Last, the novel method used in this study could be replaced by an even newer, more precise technology; would our message need to change once more?
Here are the facts: Hepatitis C virus is common among Americans born between 1945 and 1965. A current Centers for Disease Control and Prevention fact sheet asserts that most people infected with hepatitis C virus are unaware of their diagnosis, despite aggressive campaigns since 2012 to find cases. Let’s just go ahead and test our baby boomers.
Dr. Anne C. Spaulding and Dr. Lesley S. Miller are at the Rollins School of Public Health, Emory University, Atlanta. They reported receiving grants and other funding from Gilead Sciences and Bristol-Myers Squibb. These comments are from their editorial (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]30002-0).
Iatrogenic factors, not high-risk behaviors, were the main cause of the exponential spread of hepatitis C virus infections in North America, according to a phylogenetic study published online in the Lancet Infectious Diseases.
The study shifted the epicenter of spread back by more than 15 years, to about 1950, when medical procedures were expanding after World War II at the same time that clinicians continued to reuse metal and glass syringes, said Dr. Jeffrey Joy of the British Columbia Centre for Excellence in HIV/AIDS, Vancouver, and his associates.
Exponential HCV transmission had mostly ended by 1965, negating “the idea that the epidemic among baby boomers and other demographic groups in North America is primarily due to injection drug use, unsafe tattooing, high-risk sex, and travel to high endemic areas during youth,” the researchers added.
The hepatitis C virus evolves rapidly, enabling researchers to characterize its spread based on the genetic divergence of infections. Dr. Joy and his associates studied 45,316 HCV genotype 1a sequences from the National Center for Biotechnology Information GenBank nucleotide database to carry out phylogenetic analyses of five HCV genes – E1, E2, NS2, NS4B, and NS5B (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]00124-9).
The combined results for all gene regions suggested that the North American HCV epidemic expanded the most between 1940 and 1965, and that transmission rates peaked in 1950, when the oldest baby boomers were only 5 years old. Thus, nosocomial transmission rather than risky behaviors was the likely driver behind most infections, the researchers said.
“Our results could help to reduce stigma related to screening and diagnosis of hepatitis C virus, potentially increasing the numbers of providers offering screening, patients accepting testing, and if positive, presenting for care and treatment,” the authors noted.
The researchers also found that HCV transmission rates plateaued between 1965 and 1989, and dropped in the early 1990s, coinciding with increases in blood product testing and needle exchange programs aimed at preventing HIV infections. Furthermore, HCV infections rose slightly after 2000, mirroring epidemiologic reports of outbreaks among young injection drug users in nonurban areas and among men who have sex with men, the researchers said.
The Canadian Institutes of Health Research, Michael Smith Foundation for Health Research, and BC Centre for Excellence in HIV/AIDS funded the study. The investigators disclosed no competing interests.
Iatrogenic factors, not high-risk behaviors, were the main cause of the exponential spread of hepatitis C virus infections in North America, according to a phylogenetic study published online in the Lancet Infectious Diseases.
The study shifted the epicenter of spread back by more than 15 years, to about 1950, when medical procedures were expanding after World War II at the same time that clinicians continued to reuse metal and glass syringes, said Dr. Jeffrey Joy of the British Columbia Centre for Excellence in HIV/AIDS, Vancouver, and his associates.
Exponential HCV transmission had mostly ended by 1965, negating “the idea that the epidemic among baby boomers and other demographic groups in North America is primarily due to injection drug use, unsafe tattooing, high-risk sex, and travel to high endemic areas during youth,” the researchers added.
The hepatitis C virus evolves rapidly, enabling researchers to characterize its spread based on the genetic divergence of infections. Dr. Joy and his associates studied 45,316 HCV genotype 1a sequences from the National Center for Biotechnology Information GenBank nucleotide database to carry out phylogenetic analyses of five HCV genes – E1, E2, NS2, NS4B, and NS5B (Lancet Infect Dis. 2016 Mar 30. doi: 10.1016/S1473-3099[16]00124-9).
The combined results for all gene regions suggested that the North American HCV epidemic expanded the most between 1940 and 1965, and that transmission rates peaked in 1950, when the oldest baby boomers were only 5 years old. Thus, nosocomial transmission rather than risky behaviors was the likely driver behind most infections, the researchers said.
“Our results could help to reduce stigma related to screening and diagnosis of hepatitis C virus, potentially increasing the numbers of providers offering screening, patients accepting testing, and if positive, presenting for care and treatment,” the authors noted.
The researchers also found that HCV transmission rates plateaued between 1965 and 1989, and dropped in the early 1990s, coinciding with increases in blood product testing and needle exchange programs aimed at preventing HIV infections. Furthermore, HCV infections rose slightly after 2000, mirroring epidemiologic reports of outbreaks among young injection drug users in nonurban areas and among men who have sex with men, the researchers said.
The Canadian Institutes of Health Research, Michael Smith Foundation for Health Research, and BC Centre for Excellence in HIV/AIDS funded the study. The investigators disclosed no competing interests.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Iatrogenic factors, rather than high-risk behaviors, were the most likely cause of the exponential spread of hepatitis C virus infections in North America.
Major finding: Transmission of HCV genotype 1a peaked in North America in 1950, when the oldest baby boomers were 5 years old.
Data source: A retrospective phylogenetic study of five HCV genotype 1a genes from 45,316 publicly available sequences.
Disclosures: The Canadian Institutes of Health Research, Michael Smith Foundation for Health Research, and BC Centre for Excellence in HIV/AIDS funded the study. The investigators disclosed no competing interests.
VIDEO: How to recognize and treat nonalcoholic fatty liver disease
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT DIGESTIVE DISEASES: NEW ADVANCES 2016