User login
Society of Critical Care Medicine (SCCM): Critical Care Congress
Sepsis resuscitation efforts help beyond 6 hours
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign's resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who didn’t reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
Financial disclosures for the investigators were not available at press time.
On Twitter @sherryboschert
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign's resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who didn’t reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
Financial disclosures for the investigators were not available at press time.
On Twitter @sherryboschert
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign's resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who didn’t reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
Financial disclosures for the investigators were not available at press time.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Comfort care informs critical care societies’ Choosing Wisely list
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
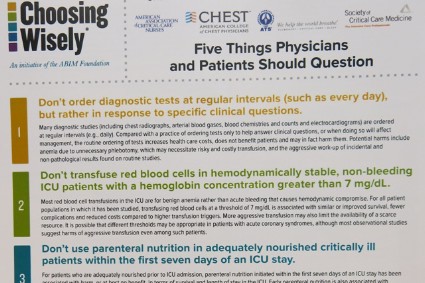
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS