User login
European Hematology Association (EHA): Annual Congress
Combo shows promise for heavily pretreated MM

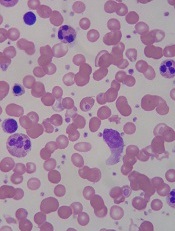
Image by Louis Heiser
and Robert Ackland
VIENNA—Combining a novel agent with dexamethasone can produce successful results where other treatments have failed, according to a presentation at the 20th Congress of the European Hematology Association.
Researchers tested low-dose dexamethasone in combination with melflufen, a peptidase-targeted therapy and antiangiogenic compound, in a phase 1/2 study of patients with relapsed or relapsed-refractory multiple myeloma (MM).
The treatment produced an overall response rate of 52%, and, although grade 3/4 hematologic adverse events were common, there were few serious adverse events related to melflufen.
These results were presented at the meeting as abstract P285.* The research was sponsored by Oncopeptides AB, the company developing melflufen.
Drug dosing and patient characteristics
In the phase 1 portion of this study, researchers evaluated 4 dose levels of melflufen—15 mg, 25 mg, 40 mg, and 55 mg—on day 1 with 40 mg of dexamethasone on days 1, 8, and 15 of 21-day cycles in a standard 3+3 design. Eight cycles of therapy were planned, but patients could continue on treatment if they experienced a clinical benefit.
There were no-dose limiting toxicities (DLTs) when melflufen was given at the 3 lower doses. However, 4 of the 6 patients who received the 55 mg dose experienced DLTs of prolonged and severe neutropenia and thrombocytopenia.
So the researchers said the MTD of melflufen, when combined with 40 mg of weekly dexamethasone, was 40 mg every 21 days.
In the ongoing phase 2 portion of the study, 29 patients have received melflufen at the MTD. The median time from the patients’ MM diagnosis to the first dose of melflufen was 5.5 years (range, 1-15), and their median number of prior therapies was 4 (range, 2-11).
Nineteen of the patients were refractory to an immunomodulatory drug (IMiD) or a proteasome inhibitor (PI); 11 were refractory to an alkylator; 10 were refractory to both an IMiD and a PI; and 5 were refractory to an IMiD, a PI, and an alkylator.
Safety data
Among the 29 patients in the phase 2 portion of the study, 22 had treatment-related grade 3-4 adverse events. These included thrombocytopenia (59%), neutropenia (48%), anemia (31%), leukopenia (21%), asthenia (7%), fatigue (7%), hyperglycemia (7%), and pyrexia/fever (7%).
To date, 12 serious adverse events have been reported in 8 of the phase 2 patients. Three events in 3 patients were considered related to melflufen—2 cases of febrile neutropenia and 1 case of pyrexia.
Fifteen patients discontinued therapy, 8 due to adverse events, 6 due to disease progression, and 1 after completing all planned cycles of treatment.
Efficacy data
Twenty-one patients were evaluable for efficacy according to the protocol, meaning they had received 2 or more cycles of therapy and completed response assessments after cycle 2.
Four patients withdrew from treatment after 1 cycle due to rapid disease progression and were included in a second response assessment (n=25). It was too early to evaluate the remaining 4 patients.
Among the 21 protocol-evaluable patients, the overall response rate was 52%, and the clinical benefit rate was 67%. Eleven patients achieved a partial response, 3 had a minimal response, 6 had stable disease, and 1 had progressive disease.
Among all 25 evaluable patients, the overall response rate was 44%, and the clinical benefit rate was 56%.
The median progression-free survival for these patients was 7.6 months (range, 3.4 months to not reached).
The researchers said enrollment in this trial is ongoing, with the goal of reaching 55 patients to further characterize the safety and efficacy of melflufen in heavily pretreated MM patients. ![]()
*Information in the abstract differs from that presented at the meeting.

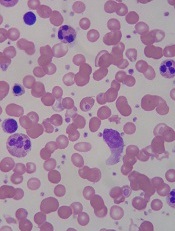
Image by Louis Heiser
and Robert Ackland
VIENNA—Combining a novel agent with dexamethasone can produce successful results where other treatments have failed, according to a presentation at the 20th Congress of the European Hematology Association.
Researchers tested low-dose dexamethasone in combination with melflufen, a peptidase-targeted therapy and antiangiogenic compound, in a phase 1/2 study of patients with relapsed or relapsed-refractory multiple myeloma (MM).
The treatment produced an overall response rate of 52%, and, although grade 3/4 hematologic adverse events were common, there were few serious adverse events related to melflufen.
These results were presented at the meeting as abstract P285.* The research was sponsored by Oncopeptides AB, the company developing melflufen.
Drug dosing and patient characteristics
In the phase 1 portion of this study, researchers evaluated 4 dose levels of melflufen—15 mg, 25 mg, 40 mg, and 55 mg—on day 1 with 40 mg of dexamethasone on days 1, 8, and 15 of 21-day cycles in a standard 3+3 design. Eight cycles of therapy were planned, but patients could continue on treatment if they experienced a clinical benefit.
There were no-dose limiting toxicities (DLTs) when melflufen was given at the 3 lower doses. However, 4 of the 6 patients who received the 55 mg dose experienced DLTs of prolonged and severe neutropenia and thrombocytopenia.
So the researchers said the MTD of melflufen, when combined with 40 mg of weekly dexamethasone, was 40 mg every 21 days.
In the ongoing phase 2 portion of the study, 29 patients have received melflufen at the MTD. The median time from the patients’ MM diagnosis to the first dose of melflufen was 5.5 years (range, 1-15), and their median number of prior therapies was 4 (range, 2-11).
Nineteen of the patients were refractory to an immunomodulatory drug (IMiD) or a proteasome inhibitor (PI); 11 were refractory to an alkylator; 10 were refractory to both an IMiD and a PI; and 5 were refractory to an IMiD, a PI, and an alkylator.
Safety data
Among the 29 patients in the phase 2 portion of the study, 22 had treatment-related grade 3-4 adverse events. These included thrombocytopenia (59%), neutropenia (48%), anemia (31%), leukopenia (21%), asthenia (7%), fatigue (7%), hyperglycemia (7%), and pyrexia/fever (7%).
To date, 12 serious adverse events have been reported in 8 of the phase 2 patients. Three events in 3 patients were considered related to melflufen—2 cases of febrile neutropenia and 1 case of pyrexia.
Fifteen patients discontinued therapy, 8 due to adverse events, 6 due to disease progression, and 1 after completing all planned cycles of treatment.
Efficacy data
Twenty-one patients were evaluable for efficacy according to the protocol, meaning they had received 2 or more cycles of therapy and completed response assessments after cycle 2.
Four patients withdrew from treatment after 1 cycle due to rapid disease progression and were included in a second response assessment (n=25). It was too early to evaluate the remaining 4 patients.
Among the 21 protocol-evaluable patients, the overall response rate was 52%, and the clinical benefit rate was 67%. Eleven patients achieved a partial response, 3 had a minimal response, 6 had stable disease, and 1 had progressive disease.
Among all 25 evaluable patients, the overall response rate was 44%, and the clinical benefit rate was 56%.
The median progression-free survival for these patients was 7.6 months (range, 3.4 months to not reached).
The researchers said enrollment in this trial is ongoing, with the goal of reaching 55 patients to further characterize the safety and efficacy of melflufen in heavily pretreated MM patients. ![]()
*Information in the abstract differs from that presented at the meeting.

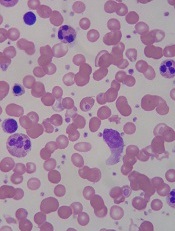
Image by Louis Heiser
and Robert Ackland
VIENNA—Combining a novel agent with dexamethasone can produce successful results where other treatments have failed, according to a presentation at the 20th Congress of the European Hematology Association.
Researchers tested low-dose dexamethasone in combination with melflufen, a peptidase-targeted therapy and antiangiogenic compound, in a phase 1/2 study of patients with relapsed or relapsed-refractory multiple myeloma (MM).
The treatment produced an overall response rate of 52%, and, although grade 3/4 hematologic adverse events were common, there were few serious adverse events related to melflufen.
These results were presented at the meeting as abstract P285.* The research was sponsored by Oncopeptides AB, the company developing melflufen.
Drug dosing and patient characteristics
In the phase 1 portion of this study, researchers evaluated 4 dose levels of melflufen—15 mg, 25 mg, 40 mg, and 55 mg—on day 1 with 40 mg of dexamethasone on days 1, 8, and 15 of 21-day cycles in a standard 3+3 design. Eight cycles of therapy were planned, but patients could continue on treatment if they experienced a clinical benefit.
There were no-dose limiting toxicities (DLTs) when melflufen was given at the 3 lower doses. However, 4 of the 6 patients who received the 55 mg dose experienced DLTs of prolonged and severe neutropenia and thrombocytopenia.
So the researchers said the MTD of melflufen, when combined with 40 mg of weekly dexamethasone, was 40 mg every 21 days.
In the ongoing phase 2 portion of the study, 29 patients have received melflufen at the MTD. The median time from the patients’ MM diagnosis to the first dose of melflufen was 5.5 years (range, 1-15), and their median number of prior therapies was 4 (range, 2-11).
Nineteen of the patients were refractory to an immunomodulatory drug (IMiD) or a proteasome inhibitor (PI); 11 were refractory to an alkylator; 10 were refractory to both an IMiD and a PI; and 5 were refractory to an IMiD, a PI, and an alkylator.
Safety data
Among the 29 patients in the phase 2 portion of the study, 22 had treatment-related grade 3-4 adverse events. These included thrombocytopenia (59%), neutropenia (48%), anemia (31%), leukopenia (21%), asthenia (7%), fatigue (7%), hyperglycemia (7%), and pyrexia/fever (7%).
To date, 12 serious adverse events have been reported in 8 of the phase 2 patients. Three events in 3 patients were considered related to melflufen—2 cases of febrile neutropenia and 1 case of pyrexia.
Fifteen patients discontinued therapy, 8 due to adverse events, 6 due to disease progression, and 1 after completing all planned cycles of treatment.
Efficacy data
Twenty-one patients were evaluable for efficacy according to the protocol, meaning they had received 2 or more cycles of therapy and completed response assessments after cycle 2.
Four patients withdrew from treatment after 1 cycle due to rapid disease progression and were included in a second response assessment (n=25). It was too early to evaluate the remaining 4 patients.
Among the 21 protocol-evaluable patients, the overall response rate was 52%, and the clinical benefit rate was 67%. Eleven patients achieved a partial response, 3 had a minimal response, 6 had stable disease, and 1 had progressive disease.
Among all 25 evaluable patients, the overall response rate was 44%, and the clinical benefit rate was 56%.
The median progression-free survival for these patients was 7.6 months (range, 3.4 months to not reached).
The researchers said enrollment in this trial is ongoing, with the goal of reaching 55 patients to further characterize the safety and efficacy of melflufen in heavily pretreated MM patients. ![]()
*Information in the abstract differs from that presented at the meeting.
Activin receptors continue to show efficacy in ß-thalassemia

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.
Drug won’t advance to phase 3 in ß-thalassemia
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
Jury still out on combo for elderly AML

Photo courtesy of NIH
VIENNA—A 2-drug combination can produce complete responses (CRs) in elderly patients with newly diagnosed acute myeloid leukemia (AML), but whether the treatment confers a survival benefit remains to be seen.
The combination consists of the HDAC inhibitor pracinostat and the antineoplastic agent azacitidine.
In a phase 2 study, the treatment produced CRs in nearly a third of AML patients, and follow-up has shown that responses improve over time.
However, the median overall survival has not been reached.
“The combination of pracinostat and azacitidine continues to demonstrate compelling clinical activity in these elderly patients with newly diagnosed AML,” said Daniel P. Gold, PhD, President and Chief Executive Officer of MEI Pharma, the company developing pracinostat.
“While the overall survival trend in this study is encouraging, we believe that longer follow-up is needed to gain an accurate survival estimate. Ultimately, this survival estimate will be critical in determining the development path forward for this combination. We look forward to providing an update when these data mature, which we expect to occur later this year.”
The current data were presented at the 20th Congress of the European Hematology Association (abstract P568*). The trial was sponsored by MEI Pharma.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML. Fifty-four percent of patients had intermediate-risk cytogenetics, 42% had high-risk, and 4% were not evaluable.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
To date, half of patients have discontinued treatment, 8% due to death, 36% because of progressive disease, 32% due to adverse events, and 24% for other reasons.
Response and survival
Thus far, 54% of patients (n=27) have achieved the primary endpoint of CR plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Thirty-two percent of patients had a CR, 14% had a CRi, 8% achieved MLFS, and 6% had a partial response (PR) or PR with incomplete count recovery (PRi).
Among the 27 patients with intermediate-risk cytogenetics, 63% achieved a CR/CRi/MLFS, and 7% had a PR/PRi. Among the 21 patients with high-risk cytogenetics, 48% achieved a CR/CRi/MLFS, and none had a PR/PRi.
The researchers said these response rates compare favorably with previous studies of azacitidine alone in this patient population. In this trial, most responses occurred within the first 2 cycles of therapy and continued to improve with ongoing therapy.
The median overall survival has not yet been reached. Sixty-four percent of patients (n=32) are still being followed (range, 6-15 months).
The survival rate of patients with intermediate-risk cytogenetics appears greater than that for patients with high-risk cytogenetics, though neither subset of patients has reached median survival.
The 60-day mortality rate was 10% (n=5).
Safety and tolerability
The most common treatment-emergent adverse events (AEs) were nausea (66%), constipation (58%), fatigue (48%), febrile neutropenia (40%), thrombocytopenia (32%), diarrhea (30%), vomiting (28%), decreased appetite (28%), anemia (26%), hypokalemia (26%), neutropenia (24%), pyrexia (24%), dizziness (24%), dyspnea (24%), and rash (20%).
Treatment-emergent AEs led to discontinuation in 8 patients. Two of these patients developed sepsis that proved fatal.
The other events included grade 3 peripheral motor neuropathy (which was resolved), grade 3 parainfluenza (resolved with sequelae), grade 3 prolonged QTc/atrial fibrillation (resolved), grade 2 failure to thrive (not resolved), grade 3 mucositis (not resolved), and grade 2 fatigue (not resolved).
AEs resulting in dose reductions were frequently due to disease, according to the researchers.
The team also noted that nearly half of the patients in this study (n=22) have received pracinostat and azacitidine beyond 6 months, and 5 patients have received it for more than a year, which reflects long-term tolerability. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo courtesy of NIH
VIENNA—A 2-drug combination can produce complete responses (CRs) in elderly patients with newly diagnosed acute myeloid leukemia (AML), but whether the treatment confers a survival benefit remains to be seen.
The combination consists of the HDAC inhibitor pracinostat and the antineoplastic agent azacitidine.
In a phase 2 study, the treatment produced CRs in nearly a third of AML patients, and follow-up has shown that responses improve over time.
However, the median overall survival has not been reached.
“The combination of pracinostat and azacitidine continues to demonstrate compelling clinical activity in these elderly patients with newly diagnosed AML,” said Daniel P. Gold, PhD, President and Chief Executive Officer of MEI Pharma, the company developing pracinostat.
“While the overall survival trend in this study is encouraging, we believe that longer follow-up is needed to gain an accurate survival estimate. Ultimately, this survival estimate will be critical in determining the development path forward for this combination. We look forward to providing an update when these data mature, which we expect to occur later this year.”
The current data were presented at the 20th Congress of the European Hematology Association (abstract P568*). The trial was sponsored by MEI Pharma.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML. Fifty-four percent of patients had intermediate-risk cytogenetics, 42% had high-risk, and 4% were not evaluable.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
To date, half of patients have discontinued treatment, 8% due to death, 36% because of progressive disease, 32% due to adverse events, and 24% for other reasons.
Response and survival
Thus far, 54% of patients (n=27) have achieved the primary endpoint of CR plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Thirty-two percent of patients had a CR, 14% had a CRi, 8% achieved MLFS, and 6% had a partial response (PR) or PR with incomplete count recovery (PRi).
Among the 27 patients with intermediate-risk cytogenetics, 63% achieved a CR/CRi/MLFS, and 7% had a PR/PRi. Among the 21 patients with high-risk cytogenetics, 48% achieved a CR/CRi/MLFS, and none had a PR/PRi.
The researchers said these response rates compare favorably with previous studies of azacitidine alone in this patient population. In this trial, most responses occurred within the first 2 cycles of therapy and continued to improve with ongoing therapy.
The median overall survival has not yet been reached. Sixty-four percent of patients (n=32) are still being followed (range, 6-15 months).
The survival rate of patients with intermediate-risk cytogenetics appears greater than that for patients with high-risk cytogenetics, though neither subset of patients has reached median survival.
The 60-day mortality rate was 10% (n=5).
Safety and tolerability
The most common treatment-emergent adverse events (AEs) were nausea (66%), constipation (58%), fatigue (48%), febrile neutropenia (40%), thrombocytopenia (32%), diarrhea (30%), vomiting (28%), decreased appetite (28%), anemia (26%), hypokalemia (26%), neutropenia (24%), pyrexia (24%), dizziness (24%), dyspnea (24%), and rash (20%).
Treatment-emergent AEs led to discontinuation in 8 patients. Two of these patients developed sepsis that proved fatal.
The other events included grade 3 peripheral motor neuropathy (which was resolved), grade 3 parainfluenza (resolved with sequelae), grade 3 prolonged QTc/atrial fibrillation (resolved), grade 2 failure to thrive (not resolved), grade 3 mucositis (not resolved), and grade 2 fatigue (not resolved).
AEs resulting in dose reductions were frequently due to disease, according to the researchers.
The team also noted that nearly half of the patients in this study (n=22) have received pracinostat and azacitidine beyond 6 months, and 5 patients have received it for more than a year, which reflects long-term tolerability. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo courtesy of NIH
VIENNA—A 2-drug combination can produce complete responses (CRs) in elderly patients with newly diagnosed acute myeloid leukemia (AML), but whether the treatment confers a survival benefit remains to be seen.
The combination consists of the HDAC inhibitor pracinostat and the antineoplastic agent azacitidine.
In a phase 2 study, the treatment produced CRs in nearly a third of AML patients, and follow-up has shown that responses improve over time.
However, the median overall survival has not been reached.
“The combination of pracinostat and azacitidine continues to demonstrate compelling clinical activity in these elderly patients with newly diagnosed AML,” said Daniel P. Gold, PhD, President and Chief Executive Officer of MEI Pharma, the company developing pracinostat.
“While the overall survival trend in this study is encouraging, we believe that longer follow-up is needed to gain an accurate survival estimate. Ultimately, this survival estimate will be critical in determining the development path forward for this combination. We look forward to providing an update when these data mature, which we expect to occur later this year.”
The current data were presented at the 20th Congress of the European Hematology Association (abstract P568*). The trial was sponsored by MEI Pharma.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML. Fifty-four percent of patients had intermediate-risk cytogenetics, 42% had high-risk, and 4% were not evaluable.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
To date, half of patients have discontinued treatment, 8% due to death, 36% because of progressive disease, 32% due to adverse events, and 24% for other reasons.
Response and survival
Thus far, 54% of patients (n=27) have achieved the primary endpoint of CR plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Thirty-two percent of patients had a CR, 14% had a CRi, 8% achieved MLFS, and 6% had a partial response (PR) or PR with incomplete count recovery (PRi).
Among the 27 patients with intermediate-risk cytogenetics, 63% achieved a CR/CRi/MLFS, and 7% had a PR/PRi. Among the 21 patients with high-risk cytogenetics, 48% achieved a CR/CRi/MLFS, and none had a PR/PRi.
The researchers said these response rates compare favorably with previous studies of azacitidine alone in this patient population. In this trial, most responses occurred within the first 2 cycles of therapy and continued to improve with ongoing therapy.
The median overall survival has not yet been reached. Sixty-four percent of patients (n=32) are still being followed (range, 6-15 months).
The survival rate of patients with intermediate-risk cytogenetics appears greater than that for patients with high-risk cytogenetics, though neither subset of patients has reached median survival.
The 60-day mortality rate was 10% (n=5).
Safety and tolerability
The most common treatment-emergent adverse events (AEs) were nausea (66%), constipation (58%), fatigue (48%), febrile neutropenia (40%), thrombocytopenia (32%), diarrhea (30%), vomiting (28%), decreased appetite (28%), anemia (26%), hypokalemia (26%), neutropenia (24%), pyrexia (24%), dizziness (24%), dyspnea (24%), and rash (20%).
Treatment-emergent AEs led to discontinuation in 8 patients. Two of these patients developed sepsis that proved fatal.
The other events included grade 3 peripheral motor neuropathy (which was resolved), grade 3 parainfluenza (resolved with sequelae), grade 3 prolonged QTc/atrial fibrillation (resolved), grade 2 failure to thrive (not resolved), grade 3 mucositis (not resolved), and grade 2 fatigue (not resolved).
AEs resulting in dose reductions were frequently due to disease, according to the researchers.
The team also noted that nearly half of the patients in this study (n=22) have received pracinostat and azacitidine beyond 6 months, and 5 patients have received it for more than a year, which reflects long-term tolerability. ![]()
*Information in the abstract differs from that presented at the meeting.
Unsickling red blood cells

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()
Triplet can provide clinical benefit in rel/ref MM

VIENNA—Combination therapy consisting of the HDAC6 inhibitor ricolinostat, pomalidomide, and dexamethasone can provide a clinical benefit for patients with relapsed and refractory multiple myeloma (MM), according to a researchers.
In a phase 1b/2 trial, the triplet produced an overall response rate (ORR) of 29% and a clinical benefit rate of 50%.
The most common treatment-related adverse events were fatigue, diarrhea, and neutropenia.
“As a physician, it is encouraging to see patients whose multiple myeloma has progressed while receiving standard-of-care therapy achieve clinical benefit with the combination of ricolinostat, [pomalidomide], and dexamethasone,” said study investigator Noopur Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston.
Dr Raje and her colleagues presented results with this combination at the 20th Congress of the European Hematology Association (abstract P279*). The research was sponsored by Acetylon Pharmaceuticals, Inc., the company developing ricolinostat.
The phase 1b portion of this trial was a 3+3 design in which ricolinostat (160 mg) was given once daily (QD) or twice daily (BID) along with pomalidomide (4 mg) for 21 days of a 28-day cycle with dexamethasone (40 mg) on days 1, 8, 15, and 22. Seven patients were treated in the phase 1b portion, with 3 at 160 mg QD and 4 at 160 mg BID.
In the ongoing phase 2 portion of the study, 32 patients were enrolled as of April 27, 2015, and 28 of these patients were evaluable for response. Nineteen of the patients received ricolinostat at 160 mg QD, and 9 received the drug at 160 mg BID.
The median age for all 39 patients was 68 (range, 48-80), and they had received a median of 3 prior therapies (range, 2-5). Seventy-four percent of patients were refractory to lenalidomide, 59% to bortezomib, and 38% to both drugs.
Treatment results
At a median follow-up of 12 weeks, the ORR among the 28 evaluable phase 2 patients was 29%. Clinical benefit, defined as minimal response or greater, was 50%.
Three patients had a very good partial response, 5 had a partial response, 6 had a minimal response, 5 had stable disease, 3 progressed, and 6 had an unconfirmed response at the time of data cutoff.
All 7 patients in the phase 1b portion of the study had discontinued treatment due to progressive disease.
Of the 28 evaluable patients in the phase 2 portion, 57% (n=16) remained on the study after a median of 3 months on therapy. The other 43% discontinued treatment due to progressive disease (n=6), a non-fatal adverse event (n=3), patient decision (n=2), or investigator decision (n=1).
The researchers said the optimal dose and schedule for ricolinostat in combination with pomalidomide and dexamethasone was 160 mg QD on days 1-21 of a 28-day cycle. Patients treated at this dose experienced no dose-limiting toxicities. At 160 mg BID, some clinically relevant grade 2 diarrhea was observed.
In all 39 patients, the common treatment-emergent adverse events were fatigue (41%), diarrhea (38%), neutropenia (36%), anemia (31%), a decrease in platelet count (26%), constipation (21%), hypertension (18%), hyponatremia (18%), upper respiratory tract infection (15%), and a decrease in white cell count (15%).
Grade 3 and 4 adverse events, apart from neutropenia (26%), were uncommon (occurring in 8% of patients or fewer).
Grade 3/4 adverse events considered possibly related to ricolinostat included neutropenia (n=5), diarrhea (n=3), bronchitis (n=1), anemia (n=1), chronic cardiac failure (n=1), leukopenia (n=1), lymphopenia (n=1), pneumonia (n=1), increased alanine aminotransferase (n=1), fatigue (n=1), thrombocytopenia (n=1), and renal failure (n=1).
“This all-oral combination has been very well-tolerated,” Dr Raje said, “making it potentially suitable for treatment of a broad range of patients, including older patients, patients for whom a non-oral drug regimen is limiting, and potentially as a part of an all-oral maintenance regimen.” ![]()
*Information in the abstract differs from that presented at the meeting.

VIENNA—Combination therapy consisting of the HDAC6 inhibitor ricolinostat, pomalidomide, and dexamethasone can provide a clinical benefit for patients with relapsed and refractory multiple myeloma (MM), according to a researchers.
In a phase 1b/2 trial, the triplet produced an overall response rate (ORR) of 29% and a clinical benefit rate of 50%.
The most common treatment-related adverse events were fatigue, diarrhea, and neutropenia.
“As a physician, it is encouraging to see patients whose multiple myeloma has progressed while receiving standard-of-care therapy achieve clinical benefit with the combination of ricolinostat, [pomalidomide], and dexamethasone,” said study investigator Noopur Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston.
Dr Raje and her colleagues presented results with this combination at the 20th Congress of the European Hematology Association (abstract P279*). The research was sponsored by Acetylon Pharmaceuticals, Inc., the company developing ricolinostat.
The phase 1b portion of this trial was a 3+3 design in which ricolinostat (160 mg) was given once daily (QD) or twice daily (BID) along with pomalidomide (4 mg) for 21 days of a 28-day cycle with dexamethasone (40 mg) on days 1, 8, 15, and 22. Seven patients were treated in the phase 1b portion, with 3 at 160 mg QD and 4 at 160 mg BID.
In the ongoing phase 2 portion of the study, 32 patients were enrolled as of April 27, 2015, and 28 of these patients were evaluable for response. Nineteen of the patients received ricolinostat at 160 mg QD, and 9 received the drug at 160 mg BID.
The median age for all 39 patients was 68 (range, 48-80), and they had received a median of 3 prior therapies (range, 2-5). Seventy-four percent of patients were refractory to lenalidomide, 59% to bortezomib, and 38% to both drugs.
Treatment results
At a median follow-up of 12 weeks, the ORR among the 28 evaluable phase 2 patients was 29%. Clinical benefit, defined as minimal response or greater, was 50%.
Three patients had a very good partial response, 5 had a partial response, 6 had a minimal response, 5 had stable disease, 3 progressed, and 6 had an unconfirmed response at the time of data cutoff.
All 7 patients in the phase 1b portion of the study had discontinued treatment due to progressive disease.
Of the 28 evaluable patients in the phase 2 portion, 57% (n=16) remained on the study after a median of 3 months on therapy. The other 43% discontinued treatment due to progressive disease (n=6), a non-fatal adverse event (n=3), patient decision (n=2), or investigator decision (n=1).
The researchers said the optimal dose and schedule for ricolinostat in combination with pomalidomide and dexamethasone was 160 mg QD on days 1-21 of a 28-day cycle. Patients treated at this dose experienced no dose-limiting toxicities. At 160 mg BID, some clinically relevant grade 2 diarrhea was observed.
In all 39 patients, the common treatment-emergent adverse events were fatigue (41%), diarrhea (38%), neutropenia (36%), anemia (31%), a decrease in platelet count (26%), constipation (21%), hypertension (18%), hyponatremia (18%), upper respiratory tract infection (15%), and a decrease in white cell count (15%).
Grade 3 and 4 adverse events, apart from neutropenia (26%), were uncommon (occurring in 8% of patients or fewer).
Grade 3/4 adverse events considered possibly related to ricolinostat included neutropenia (n=5), diarrhea (n=3), bronchitis (n=1), anemia (n=1), chronic cardiac failure (n=1), leukopenia (n=1), lymphopenia (n=1), pneumonia (n=1), increased alanine aminotransferase (n=1), fatigue (n=1), thrombocytopenia (n=1), and renal failure (n=1).
“This all-oral combination has been very well-tolerated,” Dr Raje said, “making it potentially suitable for treatment of a broad range of patients, including older patients, patients for whom a non-oral drug regimen is limiting, and potentially as a part of an all-oral maintenance regimen.” ![]()
*Information in the abstract differs from that presented at the meeting.

VIENNA—Combination therapy consisting of the HDAC6 inhibitor ricolinostat, pomalidomide, and dexamethasone can provide a clinical benefit for patients with relapsed and refractory multiple myeloma (MM), according to a researchers.
In a phase 1b/2 trial, the triplet produced an overall response rate (ORR) of 29% and a clinical benefit rate of 50%.
The most common treatment-related adverse events were fatigue, diarrhea, and neutropenia.
“As a physician, it is encouraging to see patients whose multiple myeloma has progressed while receiving standard-of-care therapy achieve clinical benefit with the combination of ricolinostat, [pomalidomide], and dexamethasone,” said study investigator Noopur Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston.
Dr Raje and her colleagues presented results with this combination at the 20th Congress of the European Hematology Association (abstract P279*). The research was sponsored by Acetylon Pharmaceuticals, Inc., the company developing ricolinostat.
The phase 1b portion of this trial was a 3+3 design in which ricolinostat (160 mg) was given once daily (QD) or twice daily (BID) along with pomalidomide (4 mg) for 21 days of a 28-day cycle with dexamethasone (40 mg) on days 1, 8, 15, and 22. Seven patients were treated in the phase 1b portion, with 3 at 160 mg QD and 4 at 160 mg BID.
In the ongoing phase 2 portion of the study, 32 patients were enrolled as of April 27, 2015, and 28 of these patients were evaluable for response. Nineteen of the patients received ricolinostat at 160 mg QD, and 9 received the drug at 160 mg BID.
The median age for all 39 patients was 68 (range, 48-80), and they had received a median of 3 prior therapies (range, 2-5). Seventy-four percent of patients were refractory to lenalidomide, 59% to bortezomib, and 38% to both drugs.
Treatment results
At a median follow-up of 12 weeks, the ORR among the 28 evaluable phase 2 patients was 29%. Clinical benefit, defined as minimal response or greater, was 50%.
Three patients had a very good partial response, 5 had a partial response, 6 had a minimal response, 5 had stable disease, 3 progressed, and 6 had an unconfirmed response at the time of data cutoff.
All 7 patients in the phase 1b portion of the study had discontinued treatment due to progressive disease.
Of the 28 evaluable patients in the phase 2 portion, 57% (n=16) remained on the study after a median of 3 months on therapy. The other 43% discontinued treatment due to progressive disease (n=6), a non-fatal adverse event (n=3), patient decision (n=2), or investigator decision (n=1).
The researchers said the optimal dose and schedule for ricolinostat in combination with pomalidomide and dexamethasone was 160 mg QD on days 1-21 of a 28-day cycle. Patients treated at this dose experienced no dose-limiting toxicities. At 160 mg BID, some clinically relevant grade 2 diarrhea was observed.
In all 39 patients, the common treatment-emergent adverse events were fatigue (41%), diarrhea (38%), neutropenia (36%), anemia (31%), a decrease in platelet count (26%), constipation (21%), hypertension (18%), hyponatremia (18%), upper respiratory tract infection (15%), and a decrease in white cell count (15%).
Grade 3 and 4 adverse events, apart from neutropenia (26%), were uncommon (occurring in 8% of patients or fewer).
Grade 3/4 adverse events considered possibly related to ricolinostat included neutropenia (n=5), diarrhea (n=3), bronchitis (n=1), anemia (n=1), chronic cardiac failure (n=1), leukopenia (n=1), lymphopenia (n=1), pneumonia (n=1), increased alanine aminotransferase (n=1), fatigue (n=1), thrombocytopenia (n=1), and renal failure (n=1).
“This all-oral combination has been very well-tolerated,” Dr Raje said, “making it potentially suitable for treatment of a broad range of patients, including older patients, patients for whom a non-oral drug regimen is limiting, and potentially as a part of an all-oral maintenance regimen.” ![]()
*Information in the abstract differs from that presented at the meeting.
Combo delays progression in relapsed CLL

VIENNA—Results of the COMPLEMENT 2 trial indicate that adding ofatumumab to treatment with fludarabine and cyclophosphamide (OFC) can improve some outcome measures in patients with relapsed chronic lymphocytic leukemia (CLL), when compared to fludarabine and cyclophosphamide alone (FC).
Patients who received OFC had a significantly higher overall response rate and longer median progression-free survival than patients who received FC.
On the other hand, there was no significant difference between the treatment arms with regard to response duration or overall survival. And there were more grade 3 or higher adverse events (AEs) in the 3-drug arm than the 2-drug arm.
“There are limited treatment options for patients who have stopped responding to current CLL treatments, which happens in many patients with this disease over time,” said study investigator Tadeusz Robak, MD, PhD, of the Medical University of Lodz and Copernicus Memorial Hospital in Lodz, Poland.
“These data showed that the addition of ofatumumab to fludarabine and cyclophosphamide extended the amount of time before a patient’s CLL progressed, and further add to the body of evidence supporting the potential use of ofatumumab for these patients.”
The data were presented at the 20th Congress of the European Hematology Association (abstract LB219). The study was sponsored by GlaxoSmithKline and Genmab, which were previously co-developing ofatumumab. The drug is now an asset of Novartis AG.
Efficacy data
COMPLEMENT 2 is a phase 3 trial of 365 patients with relapsed CLL. Patients were randomized 1:1 to receive treatment with up to 6 cycles of OFC or FC. Baseline characteristics were well-balanced between the treatment arms.
The overall response rate was higher in the OFC arm than the FC arm—84% and 68%, respectively (P=0.0003)—as was the complete response rate—27% and 7%, respectively.
However, there was no significant difference in time to response or response duration. The median duration of response was 29.6 months in the OFC arm and 24.9 months in the FC arm (P=0.0878). And the median time to response was 0.99 months in both arms (P=0.449).
Still, patients in the OFC arm experienced a 54% improvement in progression-free survival. The median progression-free survival was 28.9 months in the OFC arm and 18.8 months in the FC arm (P=0.0032). And time to progression was 42.1 months and 26.8 months, respectively (P=0.0036).
But there was no significant difference in overall survival or time to next cancer treatment between the arms. The median overall survival was 56.4 months in the OFC arm and 45.8 months in the FC arm (P=0.1410). The median time to next therapy was 48.13 months and 40.08 months, respectively (P=0.0735).
Safety data
The rate of treatment-related AEs was 93% in the OFC arm and 85% in the FC arm. The rate of grade 3 or higher AEs was 74% and 69%, respectively.
The most common treatment-related AEs occurring in the OFC and FC arms, respectively, were neutropenia (58% vs 41%), thrombocytopenia (26% vs 32%), anemia (15% vs 26%), nausea (19% in both), leukopenia (14% vs 6%), vomiting (7% vs 10%), pyrexia (10% vs 3%), rash (10% vs 2%), fatigue (6% vs 4%), and pneumonia (6% vs 4%).
Treatment-related infections occurred in 20% of patients in the OFC arm and 15% in the FC arm. Infusion reactions occurred in 60% and 28% of patients, respectively. ![]()

VIENNA—Results of the COMPLEMENT 2 trial indicate that adding ofatumumab to treatment with fludarabine and cyclophosphamide (OFC) can improve some outcome measures in patients with relapsed chronic lymphocytic leukemia (CLL), when compared to fludarabine and cyclophosphamide alone (FC).
Patients who received OFC had a significantly higher overall response rate and longer median progression-free survival than patients who received FC.
On the other hand, there was no significant difference between the treatment arms with regard to response duration or overall survival. And there were more grade 3 or higher adverse events (AEs) in the 3-drug arm than the 2-drug arm.
“There are limited treatment options for patients who have stopped responding to current CLL treatments, which happens in many patients with this disease over time,” said study investigator Tadeusz Robak, MD, PhD, of the Medical University of Lodz and Copernicus Memorial Hospital in Lodz, Poland.
“These data showed that the addition of ofatumumab to fludarabine and cyclophosphamide extended the amount of time before a patient’s CLL progressed, and further add to the body of evidence supporting the potential use of ofatumumab for these patients.”
The data were presented at the 20th Congress of the European Hematology Association (abstract LB219). The study was sponsored by GlaxoSmithKline and Genmab, which were previously co-developing ofatumumab. The drug is now an asset of Novartis AG.
Efficacy data
COMPLEMENT 2 is a phase 3 trial of 365 patients with relapsed CLL. Patients were randomized 1:1 to receive treatment with up to 6 cycles of OFC or FC. Baseline characteristics were well-balanced between the treatment arms.
The overall response rate was higher in the OFC arm than the FC arm—84% and 68%, respectively (P=0.0003)—as was the complete response rate—27% and 7%, respectively.
However, there was no significant difference in time to response or response duration. The median duration of response was 29.6 months in the OFC arm and 24.9 months in the FC arm (P=0.0878). And the median time to response was 0.99 months in both arms (P=0.449).
Still, patients in the OFC arm experienced a 54% improvement in progression-free survival. The median progression-free survival was 28.9 months in the OFC arm and 18.8 months in the FC arm (P=0.0032). And time to progression was 42.1 months and 26.8 months, respectively (P=0.0036).
But there was no significant difference in overall survival or time to next cancer treatment between the arms. The median overall survival was 56.4 months in the OFC arm and 45.8 months in the FC arm (P=0.1410). The median time to next therapy was 48.13 months and 40.08 months, respectively (P=0.0735).
Safety data
The rate of treatment-related AEs was 93% in the OFC arm and 85% in the FC arm. The rate of grade 3 or higher AEs was 74% and 69%, respectively.
The most common treatment-related AEs occurring in the OFC and FC arms, respectively, were neutropenia (58% vs 41%), thrombocytopenia (26% vs 32%), anemia (15% vs 26%), nausea (19% in both), leukopenia (14% vs 6%), vomiting (7% vs 10%), pyrexia (10% vs 3%), rash (10% vs 2%), fatigue (6% vs 4%), and pneumonia (6% vs 4%).
Treatment-related infections occurred in 20% of patients in the OFC arm and 15% in the FC arm. Infusion reactions occurred in 60% and 28% of patients, respectively. ![]()

VIENNA—Results of the COMPLEMENT 2 trial indicate that adding ofatumumab to treatment with fludarabine and cyclophosphamide (OFC) can improve some outcome measures in patients with relapsed chronic lymphocytic leukemia (CLL), when compared to fludarabine and cyclophosphamide alone (FC).
Patients who received OFC had a significantly higher overall response rate and longer median progression-free survival than patients who received FC.
On the other hand, there was no significant difference between the treatment arms with regard to response duration or overall survival. And there were more grade 3 or higher adverse events (AEs) in the 3-drug arm than the 2-drug arm.
“There are limited treatment options for patients who have stopped responding to current CLL treatments, which happens in many patients with this disease over time,” said study investigator Tadeusz Robak, MD, PhD, of the Medical University of Lodz and Copernicus Memorial Hospital in Lodz, Poland.
“These data showed that the addition of ofatumumab to fludarabine and cyclophosphamide extended the amount of time before a patient’s CLL progressed, and further add to the body of evidence supporting the potential use of ofatumumab for these patients.”
The data were presented at the 20th Congress of the European Hematology Association (abstract LB219). The study was sponsored by GlaxoSmithKline and Genmab, which were previously co-developing ofatumumab. The drug is now an asset of Novartis AG.
Efficacy data
COMPLEMENT 2 is a phase 3 trial of 365 patients with relapsed CLL. Patients were randomized 1:1 to receive treatment with up to 6 cycles of OFC or FC. Baseline characteristics were well-balanced between the treatment arms.
The overall response rate was higher in the OFC arm than the FC arm—84% and 68%, respectively (P=0.0003)—as was the complete response rate—27% and 7%, respectively.
However, there was no significant difference in time to response or response duration. The median duration of response was 29.6 months in the OFC arm and 24.9 months in the FC arm (P=0.0878). And the median time to response was 0.99 months in both arms (P=0.449).
Still, patients in the OFC arm experienced a 54% improvement in progression-free survival. The median progression-free survival was 28.9 months in the OFC arm and 18.8 months in the FC arm (P=0.0032). And time to progression was 42.1 months and 26.8 months, respectively (P=0.0036).
But there was no significant difference in overall survival or time to next cancer treatment between the arms. The median overall survival was 56.4 months in the OFC arm and 45.8 months in the FC arm (P=0.1410). The median time to next therapy was 48.13 months and 40.08 months, respectively (P=0.0735).
Safety data
The rate of treatment-related AEs was 93% in the OFC arm and 85% in the FC arm. The rate of grade 3 or higher AEs was 74% and 69%, respectively.
The most common treatment-related AEs occurring in the OFC and FC arms, respectively, were neutropenia (58% vs 41%), thrombocytopenia (26% vs 32%), anemia (15% vs 26%), nausea (19% in both), leukopenia (14% vs 6%), vomiting (7% vs 10%), pyrexia (10% vs 3%), rash (10% vs 2%), fatigue (6% vs 4%), and pneumonia (6% vs 4%).
Treatment-related infections occurred in 20% of patients in the OFC arm and 15% in the FC arm. Infusion reactions occurred in 60% and 28% of patients, respectively.
Dose reductions make ponatinib safer for CP-CML

VIENNA—Administering ponatinib at lower doses can reduce the risk of arterial occlusive events (AOE) without hindering responses in patients with chronic-phase chronic myeloid leukemia (CP-CML), data from the PACE trial suggest.
When earlier results of this phase 2 study showed that ponatinib can cause AOEs, trials of the drug were put on partial clinical hold. Enrollment was stalled temporarily, and investigators began reducing ponatinib doses.
Now, updated data from the PACE trial suggest ponatinib can be administered safely and effectively in certain patients with CP-CML.
At a median follow-up of about 3.5 years, 95% of CP-CML patients who underwent dose reductions maintained a major cytogenetic response (MCyR). And AOEs occurred in 7% of patients who underwent dose reductions, compared to 13% of patients who did not.
“These continued responses . . . in such a heavily pretreated patient population are very encouraging,” said study investigator Jorge E. Cortes, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Careful assessment of the benefit and risk of initiating ponatinib therapy, particularly in patients who may be at increased risk for arterial occlusive events, can help identify patients with refractory, Ph+ leukemias who can benefit most from this treatment.”
Dr Cortes and his colleagues presented data from the PACE trial at the 20th Congress of the European Hematology Association as abstract P234*. The study was sponsored by Ariad Pharmaceuticals, the company developing ponatinib.
Updated results
The trial included patients with resistant or intolerant CML or Philadelphia chromosome-positive acute lymphoblastic leukemia. A total of 449 patients received ponatinib at a starting dose of 45 mg/day.
Ninety-three percent of patients had previously received 2 or more approved tyrosine kinase inhibitors (TKI), and 55% had previously received 3 or more approved TKIs.
Dr Cortes and his colleagues presented data on 270 CP-CML patients. At a median follow-up of 42.3 months (data as of February 2, 2015), 114 patients (42%) continue to receive ponatinib.
Eighteen percent of patients discontinued treatment due to adverse events (AEs), 10% due to disease progression, 3% due to death, and 27% for other reasons.
Fifty-nine percent of CP-CML patients achieved an MCyR at any time during the study, and 83% of responders are estimated to remain in MCyR at 3 years. Thirty-nine percent of patients achieved a major molecular response (MMR).
The estimated progression-free survival at 3 years is 60%, and the estimated overall survival is 81%.
Twenty-three percent of CP-CML patients experienced an AOE designated a serious AE, and 28% experienced any AOE. The median time to onset for AOEs was 14.1 months (range, 0.3–44.0).
Four percent of CP-CML patients experienced a venous thromboembolism (VTE) that was considered an serious AE, and 5% experienced any VTE.
The most common all-grade, treatment-emergent AEs occurring in at least 40% of CP-CML patients were abdominal pain (46%), rash (46%), thrombocytopenia (45%), headache (43%), constipation (41%), and dry skin (41%).
Outcomes after dose reductions
On October 10, 2013, Ariad provided dose-reduction recommendations to investigators for patients remaining on the PACE trial. The following dose reductions were recommended, unless the benefit-risk analysis warranted treatment with a higher dose:
- CP-CML patients who already achieved an MCyR should have their ponatinib dose reduced to 15 mg/day
- CP-CML patients who had not already achieved an MCyR should have their dose reduced to 30 mg/day
- Advanced-phase patients should have their dose reduced to 30 mg/day.
As of February 2015, with 1.3 years (16 months) of follow-up after these recommendations, 95% of CP-CML patients maintained their response, whether or not they underwent prospective dose reductions.
Of the patients who were in MCyR as of October 10, 2013, and had a prospective dose reduction, 95% (61/64) maintained their response at 1.3 years. Of the patients who were in MMR as of October 10, 2013, and had a prospective dose reduction, 94% (44/47) maintained their response at 1.3 years.
Forty-two patients in MCyR did not undergo prospective dose reductions (the majority of which were already at a reduced dose of 30 mg or 15 mg as of October 10, 2013). Of these patients, 93% (n=39) maintained an MCyR after 1.3 more years of ponatinib treatment.
Twenty-four patients in MMR did not undergo prospective dose reductions, and 96% of these patients (n=22) maintained their response at 1.3 years.
Seven percent (5/71) of patients without prior AOEs who underwent dose reductions had a new AOE during the 1.3-year interval after dose reduction.
Thirteen percent (9/67) of patients without prior AOEs who did not undergo dose reductions had a new AOE in the same time interval.
*Information in the abstract differs from that presented at the meeting.

VIENNA—Administering ponatinib at lower doses can reduce the risk of arterial occlusive events (AOE) without hindering responses in patients with chronic-phase chronic myeloid leukemia (CP-CML), data from the PACE trial suggest.
When earlier results of this phase 2 study showed that ponatinib can cause AOEs, trials of the drug were put on partial clinical hold. Enrollment was stalled temporarily, and investigators began reducing ponatinib doses.
Now, updated data from the PACE trial suggest ponatinib can be administered safely and effectively in certain patients with CP-CML.
At a median follow-up of about 3.5 years, 95% of CP-CML patients who underwent dose reductions maintained a major cytogenetic response (MCyR). And AOEs occurred in 7% of patients who underwent dose reductions, compared to 13% of patients who did not.
“These continued responses . . . in such a heavily pretreated patient population are very encouraging,” said study investigator Jorge E. Cortes, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Careful assessment of the benefit and risk of initiating ponatinib therapy, particularly in patients who may be at increased risk for arterial occlusive events, can help identify patients with refractory, Ph+ leukemias who can benefit most from this treatment.”
Dr Cortes and his colleagues presented data from the PACE trial at the 20th Congress of the European Hematology Association as abstract P234*. The study was sponsored by Ariad Pharmaceuticals, the company developing ponatinib.
Updated results
The trial included patients with resistant or intolerant CML or Philadelphia chromosome-positive acute lymphoblastic leukemia. A total of 449 patients received ponatinib at a starting dose of 45 mg/day.
Ninety-three percent of patients had previously received 2 or more approved tyrosine kinase inhibitors (TKI), and 55% had previously received 3 or more approved TKIs.
Dr Cortes and his colleagues presented data on 270 CP-CML patients. At a median follow-up of 42.3 months (data as of February 2, 2015), 114 patients (42%) continue to receive ponatinib.
Eighteen percent of patients discontinued treatment due to adverse events (AEs), 10% due to disease progression, 3% due to death, and 27% for other reasons.
Fifty-nine percent of CP-CML patients achieved an MCyR at any time during the study, and 83% of responders are estimated to remain in MCyR at 3 years. Thirty-nine percent of patients achieved a major molecular response (MMR).
The estimated progression-free survival at 3 years is 60%, and the estimated overall survival is 81%.
Twenty-three percent of CP-CML patients experienced an AOE designated a serious AE, and 28% experienced any AOE. The median time to onset for AOEs was 14.1 months (range, 0.3–44.0).
Four percent of CP-CML patients experienced a venous thromboembolism (VTE) that was considered an serious AE, and 5% experienced any VTE.
The most common all-grade, treatment-emergent AEs occurring in at least 40% of CP-CML patients were abdominal pain (46%), rash (46%), thrombocytopenia (45%), headache (43%), constipation (41%), and dry skin (41%).
Outcomes after dose reductions
On October 10, 2013, Ariad provided dose-reduction recommendations to investigators for patients remaining on the PACE trial. The following dose reductions were recommended, unless the benefit-risk analysis warranted treatment with a higher dose:
- CP-CML patients who already achieved an MCyR should have their ponatinib dose reduced to 15 mg/day
- CP-CML patients who had not already achieved an MCyR should have their dose reduced to 30 mg/day
- Advanced-phase patients should have their dose reduced to 30 mg/day.
As of February 2015, with 1.3 years (16 months) of follow-up after these recommendations, 95% of CP-CML patients maintained their response, whether or not they underwent prospective dose reductions.
Of the patients who were in MCyR as of October 10, 2013, and had a prospective dose reduction, 95% (61/64) maintained their response at 1.3 years. Of the patients who were in MMR as of October 10, 2013, and had a prospective dose reduction, 94% (44/47) maintained their response at 1.3 years.
Forty-two patients in MCyR did not undergo prospective dose reductions (the majority of which were already at a reduced dose of 30 mg or 15 mg as of October 10, 2013). Of these patients, 93% (n=39) maintained an MCyR after 1.3 more years of ponatinib treatment.
Twenty-four patients in MMR did not undergo prospective dose reductions, and 96% of these patients (n=22) maintained their response at 1.3 years.
Seven percent (5/71) of patients without prior AOEs who underwent dose reductions had a new AOE during the 1.3-year interval after dose reduction.
Thirteen percent (9/67) of patients without prior AOEs who did not undergo dose reductions had a new AOE in the same time interval.
*Information in the abstract differs from that presented at the meeting.

VIENNA—Administering ponatinib at lower doses can reduce the risk of arterial occlusive events (AOE) without hindering responses in patients with chronic-phase chronic myeloid leukemia (CP-CML), data from the PACE trial suggest.
When earlier results of this phase 2 study showed that ponatinib can cause AOEs, trials of the drug were put on partial clinical hold. Enrollment was stalled temporarily, and investigators began reducing ponatinib doses.
Now, updated data from the PACE trial suggest ponatinib can be administered safely and effectively in certain patients with CP-CML.
At a median follow-up of about 3.5 years, 95% of CP-CML patients who underwent dose reductions maintained a major cytogenetic response (MCyR). And AOEs occurred in 7% of patients who underwent dose reductions, compared to 13% of patients who did not.
“These continued responses . . . in such a heavily pretreated patient population are very encouraging,” said study investigator Jorge E. Cortes, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Careful assessment of the benefit and risk of initiating ponatinib therapy, particularly in patients who may be at increased risk for arterial occlusive events, can help identify patients with refractory, Ph+ leukemias who can benefit most from this treatment.”
Dr Cortes and his colleagues presented data from the PACE trial at the 20th Congress of the European Hematology Association as abstract P234*. The study was sponsored by Ariad Pharmaceuticals, the company developing ponatinib.
Updated results
The trial included patients with resistant or intolerant CML or Philadelphia chromosome-positive acute lymphoblastic leukemia. A total of 449 patients received ponatinib at a starting dose of 45 mg/day.
Ninety-three percent of patients had previously received 2 or more approved tyrosine kinase inhibitors (TKI), and 55% had previously received 3 or more approved TKIs.
Dr Cortes and his colleagues presented data on 270 CP-CML patients. At a median follow-up of 42.3 months (data as of February 2, 2015), 114 patients (42%) continue to receive ponatinib.
Eighteen percent of patients discontinued treatment due to adverse events (AEs), 10% due to disease progression, 3% due to death, and 27% for other reasons.
Fifty-nine percent of CP-CML patients achieved an MCyR at any time during the study, and 83% of responders are estimated to remain in MCyR at 3 years. Thirty-nine percent of patients achieved a major molecular response (MMR).
The estimated progression-free survival at 3 years is 60%, and the estimated overall survival is 81%.
Twenty-three percent of CP-CML patients experienced an AOE designated a serious AE, and 28% experienced any AOE. The median time to onset for AOEs was 14.1 months (range, 0.3–44.0).
Four percent of CP-CML patients experienced a venous thromboembolism (VTE) that was considered an serious AE, and 5% experienced any VTE.
The most common all-grade, treatment-emergent AEs occurring in at least 40% of CP-CML patients were abdominal pain (46%), rash (46%), thrombocytopenia (45%), headache (43%), constipation (41%), and dry skin (41%).
Outcomes after dose reductions
On October 10, 2013, Ariad provided dose-reduction recommendations to investigators for patients remaining on the PACE trial. The following dose reductions were recommended, unless the benefit-risk analysis warranted treatment with a higher dose:
- CP-CML patients who already achieved an MCyR should have their ponatinib dose reduced to 15 mg/day
- CP-CML patients who had not already achieved an MCyR should have their dose reduced to 30 mg/day
- Advanced-phase patients should have their dose reduced to 30 mg/day.
As of February 2015, with 1.3 years (16 months) of follow-up after these recommendations, 95% of CP-CML patients maintained their response, whether or not they underwent prospective dose reductions.
Of the patients who were in MCyR as of October 10, 2013, and had a prospective dose reduction, 95% (61/64) maintained their response at 1.3 years. Of the patients who were in MMR as of October 10, 2013, and had a prospective dose reduction, 94% (44/47) maintained their response at 1.3 years.
Forty-two patients in MCyR did not undergo prospective dose reductions (the majority of which were already at a reduced dose of 30 mg or 15 mg as of October 10, 2013). Of these patients, 93% (n=39) maintained an MCyR after 1.3 more years of ponatinib treatment.
Twenty-four patients in MMR did not undergo prospective dose reductions, and 96% of these patients (n=22) maintained their response at 1.3 years.
Seven percent (5/71) of patients without prior AOEs who underwent dose reductions had a new AOE during the 1.3-year interval after dose reduction.
Thirteen percent (9/67) of patients without prior AOEs who did not undergo dose reductions had a new AOE in the same time interval.
*Information in the abstract differs from that presented at the meeting.
JAK inhibitor can provide long-term disease control in PV

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”
mAb produces responses in AL amyloidosis

VIENNA—A monoclonal antibody (mAb) can produce responses in patients with light chain (AL) amyloidosis and persistent organ dysfunction, according to research presented at the 20th Congress of the European Hematology Association.
In an ongoing phase 1/2 trial, the mAb, known as NEOD001, produced a cardiac response in 57% of evaluable patients and a renal response in 60% of evaluable patients.
Michaela Liedtke, MD, of the Stanford University School of Medicine in California, presented these results as abstract S104*. The research was sponsored by Prothena Therapeutics Ltd., the company developing NEOD001.
Dr Liedtke presented results of an interim analysis as of February 28, 2015. The analysis included 27 patients with AL amyloidosis who had received 1 or more anti-plasma-cell systemic therapies, had a partial response or better, and did not require additional chemotherapy. The patients also had persistent organ dysfunction.
Patients received a dose of NEOD001 every 28 days, in 1 of 7 dosing cohorts (0.5 mg/kg, 1 mg/kg, 2 mg/kg, 4 mg/kg, 8 mg/kg, 16 mg/kg, and 24 mg/kg). They received a total of 327 infusions, with an average treatment duration of 12 months.
The patients’ median age was 60 (range, 38-80), and they had received a median of 2 prior treatments (range, 1-7). A third of patients each had 1 organ system involved (n=9), 2 organ systems involved (n=9), or 3 or more organ systems involved (n=9).
Safety data
The most frequently reported treatment-emergent adverse events (occurring in more than 10% of subjects) were fatigue (37%), upper respiratory tract infection (26%), cough (19%), dyspnea (19%), headache (15%), anemia (15%), increased blood creatinine (15%), peripheral edema (15%), edema (11%), diarrhea (11%), nausea (11%), and hyponatremia (11%).
There were no reports of hypersensitivity reactions to NEOD001 or drug-related serious adverse events, and no anti-NEOD001 antibodies were detected. There were no dose-limiting toxicities, and none of the patients discontinued treatment due to drug-related adverse events.
All patients remaining in the study were escalated to a dose of 24 mg/kg as of December 2, 2014.
Renal and cardiac responses
In a best-response analysis, 60% (9/15) of renal-evaluable patients demonstrated a renal response to NEOD001, defined as a 30% decrease in proteinuria in the absence of estimated glomerular filtration rate (eGFR) worsening. The other 40% of patients (n=6) had stable disease.
In another best-response analysis, 57% (8/14) of cardiac-evaluable patients had a cardiac response to NEOD001, defined as more than 30% and 300 pg/mL decrease in levels of N-terminal pro-brain natriuretic peptide (NT-proBNP). The other 43% of patients (n=6) had stable disease.
Longer treatment with NEOD001 was significantly associated with NT-proBNP decline (P<0.0001).
“[M]onthly infusions of NEOD001 correlate significantly with decreases in both cardiac and renal biomarkers over time,” Dr Liedtke said. “Decreases in cardiac biomarkers predict increased survival, and decreases in renal biomarkers predict delayed time to kidney failure.”
*Information in the abstract differs from that presented at the meeting.

VIENNA—A monoclonal antibody (mAb) can produce responses in patients with light chain (AL) amyloidosis and persistent organ dysfunction, according to research presented at the 20th Congress of the European Hematology Association.
In an ongoing phase 1/2 trial, the mAb, known as NEOD001, produced a cardiac response in 57% of evaluable patients and a renal response in 60% of evaluable patients.
Michaela Liedtke, MD, of the Stanford University School of Medicine in California, presented these results as abstract S104*. The research was sponsored by Prothena Therapeutics Ltd., the company developing NEOD001.
Dr Liedtke presented results of an interim analysis as of February 28, 2015. The analysis included 27 patients with AL amyloidosis who had received 1 or more anti-plasma-cell systemic therapies, had a partial response or better, and did not require additional chemotherapy. The patients also had persistent organ dysfunction.
Patients received a dose of NEOD001 every 28 days, in 1 of 7 dosing cohorts (0.5 mg/kg, 1 mg/kg, 2 mg/kg, 4 mg/kg, 8 mg/kg, 16 mg/kg, and 24 mg/kg). They received a total of 327 infusions, with an average treatment duration of 12 months.
The patients’ median age was 60 (range, 38-80), and they had received a median of 2 prior treatments (range, 1-7). A third of patients each had 1 organ system involved (n=9), 2 organ systems involved (n=9), or 3 or more organ systems involved (n=9).
Safety data
The most frequently reported treatment-emergent adverse events (occurring in more than 10% of subjects) were fatigue (37%), upper respiratory tract infection (26%), cough (19%), dyspnea (19%), headache (15%), anemia (15%), increased blood creatinine (15%), peripheral edema (15%), edema (11%), diarrhea (11%), nausea (11%), and hyponatremia (11%).
There were no reports of hypersensitivity reactions to NEOD001 or drug-related serious adverse events, and no anti-NEOD001 antibodies were detected. There were no dose-limiting toxicities, and none of the patients discontinued treatment due to drug-related adverse events.
All patients remaining in the study were escalated to a dose of 24 mg/kg as of December 2, 2014.
Renal and cardiac responses
In a best-response analysis, 60% (9/15) of renal-evaluable patients demonstrated a renal response to NEOD001, defined as a 30% decrease in proteinuria in the absence of estimated glomerular filtration rate (eGFR) worsening. The other 40% of patients (n=6) had stable disease.
In another best-response analysis, 57% (8/14) of cardiac-evaluable patients had a cardiac response to NEOD001, defined as more than 30% and 300 pg/mL decrease in levels of N-terminal pro-brain natriuretic peptide (NT-proBNP). The other 43% of patients (n=6) had stable disease.
Longer treatment with NEOD001 was significantly associated with NT-proBNP decline (P<0.0001).
“[M]onthly infusions of NEOD001 correlate significantly with decreases in both cardiac and renal biomarkers over time,” Dr Liedtke said. “Decreases in cardiac biomarkers predict increased survival, and decreases in renal biomarkers predict delayed time to kidney failure.”
*Information in the abstract differs from that presented at the meeting.

VIENNA—A monoclonal antibody (mAb) can produce responses in patients with light chain (AL) amyloidosis and persistent organ dysfunction, according to research presented at the 20th Congress of the European Hematology Association.
In an ongoing phase 1/2 trial, the mAb, known as NEOD001, produced a cardiac response in 57% of evaluable patients and a renal response in 60% of evaluable patients.
Michaela Liedtke, MD, of the Stanford University School of Medicine in California, presented these results as abstract S104*. The research was sponsored by Prothena Therapeutics Ltd., the company developing NEOD001.
Dr Liedtke presented results of an interim analysis as of February 28, 2015. The analysis included 27 patients with AL amyloidosis who had received 1 or more anti-plasma-cell systemic therapies, had a partial response or better, and did not require additional chemotherapy. The patients also had persistent organ dysfunction.
Patients received a dose of NEOD001 every 28 days, in 1 of 7 dosing cohorts (0.5 mg/kg, 1 mg/kg, 2 mg/kg, 4 mg/kg, 8 mg/kg, 16 mg/kg, and 24 mg/kg). They received a total of 327 infusions, with an average treatment duration of 12 months.
The patients’ median age was 60 (range, 38-80), and they had received a median of 2 prior treatments (range, 1-7). A third of patients each had 1 organ system involved (n=9), 2 organ systems involved (n=9), or 3 or more organ systems involved (n=9).
Safety data
The most frequently reported treatment-emergent adverse events (occurring in more than 10% of subjects) were fatigue (37%), upper respiratory tract infection (26%), cough (19%), dyspnea (19%), headache (15%), anemia (15%), increased blood creatinine (15%), peripheral edema (15%), edema (11%), diarrhea (11%), nausea (11%), and hyponatremia (11%).
There were no reports of hypersensitivity reactions to NEOD001 or drug-related serious adverse events, and no anti-NEOD001 antibodies were detected. There were no dose-limiting toxicities, and none of the patients discontinued treatment due to drug-related adverse events.
All patients remaining in the study were escalated to a dose of 24 mg/kg as of December 2, 2014.
Renal and cardiac responses
In a best-response analysis, 60% (9/15) of renal-evaluable patients demonstrated a renal response to NEOD001, defined as a 30% decrease in proteinuria in the absence of estimated glomerular filtration rate (eGFR) worsening. The other 40% of patients (n=6) had stable disease.
In another best-response analysis, 57% (8/14) of cardiac-evaluable patients had a cardiac response to NEOD001, defined as more than 30% and 300 pg/mL decrease in levels of N-terminal pro-brain natriuretic peptide (NT-proBNP). The other 43% of patients (n=6) had stable disease.
Longer treatment with NEOD001 was significantly associated with NT-proBNP decline (P<0.0001).
“[M]onthly infusions of NEOD001 correlate significantly with decreases in both cardiac and renal biomarkers over time,” Dr Liedtke said. “Decreases in cardiac biomarkers predict increased survival, and decreases in renal biomarkers predict delayed time to kidney failure.”
*Information in the abstract differs from that presented at the meeting.