User login
GI Perforation Rare in Rheumatoid Arthritis Patients
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: The incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Data Source: Retrospective study of 143,433 patients with rheumatoid arthritis with at least two nondiagnostic claims in a U.S. administrative database filed between 2001 and 2009.
Disclosures: Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
GI Perforation Rare in Rheumatoid Arthritis Patients
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
LONDON – Although a potentially serious complication, perforation of the gastrointestinal tract is rare, judging from the findings of an analysis of more than 140,000 patients with rheumatoid arthritis.
Upper or lower GI tract perforation occurred in 696 (0.5%) of patients, with an overall, unadjusted incidence rate of 1.7 cases per 1,000 person-years, according to a report by Dr. Jeffrey Curtis.
"For [most of] the rheumatoid arthritis patients someone has in their practice, [GI perforation] is going to be very uncommon; I think that should be reassuring," Dr. Curtis said during an interview at the annual European Congress of Rheumatology.
"We also observed that there were cases [of GI perforation] for every biologic group," added Dr. Curtis, a rheumatologist, epidemiologist, and associate professor of medicine at the University of Alabama at Birmingham. This should help dispel any concerns that the adverse event might occur with certain biologic agents used to treat RA, he suggested.
In a retrospective study, Dr. Curtis and his associates analyzed records of 143,433 RA patients from a large U.S.-based administrative claims database for the years 2001-2009. The investigators used a validated algorithm to identify cases of upper and lower GI perforation and to determine predictive factors. The median follow-up was 2.5 years.
Older age was found to be a predictor of GI perforation, with adjusted relative risks of 1.6 and 2.1 for people aged 40-64 years and 65 years, respectively, compared with RA patients younger than 40 years. The mean age of the 142,737 patients who did not have a GI perforation was 57.6 years, and the mean age of the 696 patients who did was 62 years (P less than .01).
Diverticulitis and diverticulosis without diverticulitis were also significantly more common in patients who experienced a GI perforation than in those who did not, although the incidence was still low, with rates of 2.9% vs. 0.3% and 1.4% vs. 0.4%, respectively (both P less than .01). Diverticulitis but not diverticulosis was a significant risk factor for perforation.
The main risk factors among the RA medication groups of most relevance were the use of oral glucocorticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), not biologics and not really the disease-modifying antirheumatic drugs (DMARDs), Dr. Curtis said in the interview. Indeed, the incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Steroid monotherapy carried an incidence of 2.86 per 1,000 patient-years. Steroids used in combination with methotrexate and biologics also increased the risk of the GI complications (2.24 and 1.87 per 1,000 patient-years, respectively).
The rates of GI perforations in patients treated with biologics, methotrexate, or other DMARDs without steroids were 1.02, 1.08, and 1.71 per 1,000 patient-years, respectively. NSAID use was associated with an incidence rate of 1.68 per 1,000 patient-years.
"In contrast to about 10 years ago, when there was a lot more GI bleeding with perforation in the upper GI tract, there are population studies now suggesting that we need to be more worried about perforations of the lower GI tract," Dr. Curtis said.
In the study, 80% of the perforations seen were in the lower GI tract, so the use of gastroprotective medications may not be that useful.
"I think that the relative contribution of NSAIDs [to GI perforation] is probably diminished, just because we are seeing more lower now than upper."
Although still important, upper GI bleeding and peptic ulcer disease are perhaps less critical than antecedent diverticulitis and its associated complications.
Minimization of NSAID and steroid use is probably warranted in higher-risk patients, Dr. Curtis advised. "In somebody with a history of diverticulitis, I would be very cautious," he noted.
Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: The incidence of GI perforation was highest in patients who used glucocorticoids in combination with DMARDs other than methotrexate (3.03 per 1,000 patient years).
Data Source: Retrospective study of 143,433 patients with rheumatoid arthritis with at least two nondiagnostic claims in a U.S. administrative database filed between 2001 and 2009.
Disclosures: Dr. Curtis disclosed research and consulting relationships with Abbot, Amgen, BMS, Centocor, CORRONA, Crescendo, Pfizer, Roche, and UCB.
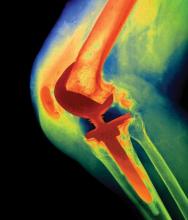
Periprosthetic Joint Infections Not Increased by RA Biologics
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Fifteen joint infections occurred in 1,495 patients, with 1% of conventional DMARD-treated and 1.5% of anti-TNF–treated patients experiencing joint infection (P less than .77).
Data Source: Data analysis of 7,536 RA patients enrolled in the German biologics register RABBIT until May 2010.
Disclosures: RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
Periprosthetic Joint Infections Not Increased by RA Biologics
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Fifteen joint infections occurred in 1,495 patients, with 1% of conventional DMARD-treated and 1.5% of anti-TNF–treated patients experiencing joint infection (P less than .77).
Data Source: Data analysis of 7,536 RA patients enrolled in the German biologics register RABBIT until May 2010.
Disclosures: RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.
Rheumatoid Arthritis Patients Have High Expectations for Biologics
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Patients treated with biologics experienced higher levels of anxiety than did DMARD-treated patients (66% vs. 53%) over switching treatment, and expressed greater disappointment (37% vs. 28%) when therapies failed.
Data Source: Anonymous survey of 165 Japanese outpatients with RA; 110 were treated with DMARDs and 55 with biologic agents.
Disclosures: Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
Rheumatoid Arthritis Patients Have High Expectations for Biologics
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
LONDON – Patients with rheumatoid arthritis have high expectations of how effective biologic therapies will be in comparison to standard disease-modifying antirheumatic drugs, according to the results of a survey conducted in Japan.
RA patients taking biologics experience higher levels of anxiety than do patients taking DMARDs (66% vs. 53%) over switching treatments, and greater disappointment (37% vs. 28%) when therapies fail to live up to their expectations, according to Keiko Funahashi, a pharmacist from the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, Kato City, Japan. She reported the results at the annual European Congress of Rheumatology.
RA treatment "has improved dramatically in the past 10 years. Due to the advent of biological products, patients’ treatment goals have also changed significantly," she added.
Indeed, the survey findings suggest that patients taking biologic agents are more likely to expect their treatment to eradicate joint pain and swelling rather than to just simply reduce it.
Ms. Funahashi and coauthor Dr. Tsukasa Matsubara, also of the Matsubara Mayflower Hospital and Research Institute of Joint Diseases, performed the outpatient survey in order to understand what patients expected of their treatment, and to determine the influence of biologic or nonbiologic DMARDs on patient attitudes.
The anonymous survey consisted of a short set of simple questions asking about the type of past and current treatment received, whether medications had been switched, what patients needed to know before starting a new treatment, their expectations of such treatment, and if they were satisfied with the results. Patients were also asked to state what their goals for treatment were.
A total of 165 patients attending the Matsubara Mayflower Hospital as outpatients during a 1-month period in October 2010 participated in the survey. In all, 110 patients were receiving treatment with DMARDs, and 55 were receiving biologics. Most patients were aged 50-70 years, and had a disease duration of 10-20 years.
While there was no significant difference between the DMARD and biologic treatment groups in terms of their current methotrexate use (70.7% vs. 63.6%, respectively), patients treated with biologic agents were less likely to be treated with steroids (40.8% vs. 21.8%, P less than .05) or nonsteroidal anti-inflammatory drugs (39.1% vs. 9.1%, P less than .01).
Before starting a new treatment, around 70% of patients in each group responded that they wanted to know about the side effects and efficacy first. Patients about to take biologics also wanted to know about the monthly cost, which they had to pay themselves, Ms. Funahashi said in an interview.
"Before treatment, patients taking biologics understood their disease better and had higher goals than those patients treated with DMARDs," Ms. Funahashi said. In particular, biologic-treated patients expected to see greater prevention of joint destruction, improved quality of life, and greater reductions in joint pain and swelling.
While patient goals hardly changed before and after treatment with DMARDs, the biologics group switched from not just wanting to reduce joint pain and swelling to wishing to eradicate them altogether.
The main cause of disappointment with treatment for patients treated with DMARDs was side effects, while a lack of efficacy was at the root of most patients’ dissatisfaction with biologic treatment.
"The results suggest that patients treated with biologics expect higher efficacy," Ms. Funahashi observed. This could be due to the perception that the higher cost equates with better efficacy. The cost of treatment is an important issue in Japan and a consideration when the rheumatologist and patient consider options.
The survey findings also highlight the need for good patient education and communication, and the development of realistic treatment goals.
"Doctors and health professionals really have a duty, I think, to give people the appropriate information, as well as do a lot of signposting to patient organizations and groups that can offer peer support," said Ms. Kate Llewelyn, who is head of information services at the U.K. charity Arthritis Care, in an interview.
"Learning to self-manage and realize that you can take control of your arthritis and rheumatism is one of the key things to feeling like you’re actually tackling the disease rather than being a passive recipient of treatment," Ms. Llewelyn suggested.
Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Patients treated with biologics experienced higher levels of anxiety than did DMARD-treated patients (66% vs. 53%) over switching treatment, and expressed greater disappointment (37% vs. 28%) when therapies failed.
Data Source: Anonymous survey of 165 Japanese outpatients with RA; 110 were treated with DMARDs and 55 with biologic agents.
Disclosures: Ms. Funahashi, her coauthor Dr. Matsubara, and Ms. Llewelyn had no conflicts of interest to declare.
Strontium Ranelate Shows Antifracture Efficacy Over 10-Year Period
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: During the 5-10 year period of extended, continuous treatment with strontium ranelate, postmenopausal women with osteoporosis at baseline had a 21% rate of vertebral fractures and a 14% rate of nonvertebral fractures, significantly less than the 28% and 20% rates, respectively, of fractures in a matched placebo group.
Data Source: Cohort of 233 postmenopausal women with osteoporosis maintained on 2 g/day strontium ranelate for 10 years, compared with a matched control group of 458 women drawn from a pivotal trial of strontium ranelate.
Disclosures: The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
Strontium Ranelate Shows Antifracture Efficacy Over 10-Year Period
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
LONDON – Strontium ranelate continued to safely and effectively prevent vertebral and nonvertebral fractures in postmenopausal women with osteoporosis during 5-10 years of continuous treatment, in a "modified" case-control study that included 233 women who maintained daily 2 g/day strontium dosing for 10 years.
"Strontium ranelate should not be considered a second-line alternative to bisphosphonates or to any other [osteoporosis] treatment," Dr. Jean-Yves Reginster said at the annual European Congress of Rheumatology. Treatment with strontium ranelate "gives you a chance to bring bone turnover back to premenopausal values," said Dr. Reginster, professor of epidemiology and chairman of the department of public health at the University of Liège in Belgium.
The ability of strontium ranelate to maintain a reduced rate of both vertebral and nonvertebral fractures over 10 years of continuous use in this study marks the first reported evidence of an antiosteoporotic drug exerting an unequivocal antifracture benefit for such a prolonged period. The only other report on 10-year treatment came from the Fracture Intervention Trial Long Term Extension, which included 1,099 women randomized to alendronate or placebo for 10 years (JAMA 2006;296:2927-38). Those results showed that 5-10 years of extended alendronate treatment did not result in a reduction of all clinical fractures or nonvertebral fracture, compared with women maintained on placebo during years 5-10, but extended alendronate did reduce the clinical vertebral fracture rate, compared with placebo.
"In our study [of strontium ranelate], we had no placebo group, but we showed that you can reduce fractures over 10 years with this drug." Strontium maintained its efficacy over 10 years "probably because of its mechanism of action, a dual action," Dr. Reginster said in an interview. "With bisphosphonates you reduce bone resorption. With strontium ranelate you reduce bone resorption by 20%-25%, and you increase bone formation by 20%-25%, so you bring the bone back to what you see in younger women. I think it is a more physiologic approach" than treatment with a bisphosphonate.
In addition, "safety is most important to me when you treat for 10 years. One of the biggest advantages of strontium ranelate is that it is a very safe drug, with little risk of adverse effects over time. I think that calculating the risk/benefit ratio of a drug over time is very important."
In his report, Dr. Reginster emphasized that the women maintained on the drug for 10 years did not have a single episode of atypical fracture, osteonecrosis of the jaw or atrial fibrillation, and their adverse-event profile showed better safety than in the original, pivotal trials of strontium ranelate. He also noted that while the extension only included 233 women on the drug, registry data on about one million patients who have taken the drug also show no reported cases of atypical fracture, osteonecrosis of the jaw, or atrial fibrillation.
The 233 women followed for 10 years on continuous strontium ranelate treatment came from either of the two pivotal, 5-year trials of the drug: the Treatment of Peripheral Osteoporosis Study (TROPOS) (J. Clin. Endocrinol. Met. 2005;90:2816-22), and the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial (New. Engl. J. Med. 2004;350:459-68). They continued to receive 2 g/day strontium ranelate, and 73% of the women completed the full extension period. Their average duration of drug use was 9.8 years, and their average compliance with the regimen was 89%.
During their additional 5 years on the drug, average lumbar spine bone mineral density continued to rise, increasing from about 20% above baseline at the start of the extension to about 27% above baseline at 10 years.
To assess the efficacy of treatment for preventing vertebral and nonvertebral fractures, Dr. Reginster and his associates "rebuilt" a control population by selecting placebo patients from the TROPOS study who matched the 233 extended-treatment women based on their baseline Fracture Risk Assessment scores. The researchers matched two TROPOS placebo-group women with each women in the extension study, assembling a total of 458 controls.
The incidence of vertebral fractures during years 5-10 in the women on strontium ranelate was 21%, compared with a 28% rate in the rebuilt control group, a statistically significant difference. In addition, the 21% reduction during the 5-10 year period was statistically similar to the 19% vertebral fracture rate among women treated during 0-5 years in SOTI.
The incidence of nonvertebral fractures during years 5-10 with strontium ranelate was 14%, significantly less than the 20% rate in the derived placebo group and statistically similar to the 13% rate seen in TROPOS, Dr. Reginster reported.
The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: During the 5-10 year period of extended, continuous treatment with strontium ranelate, postmenopausal women with osteoporosis at baseline had a 21% rate of vertebral fractures and a 14% rate of nonvertebral fractures, significantly less than the 28% and 20% rates, respectively, of fractures in a matched placebo group.
Data Source: Cohort of 233 postmenopausal women with osteoporosis maintained on 2 g/day strontium ranelate for 10 years, compared with a matched control group of 458 women drawn from a pivotal trial of strontium ranelate.
Disclosures: The SOTI and TROPOS trials were funded by Servier, which markets strontium ranelate (Protelos). Dr. Reginster reported financial relationships with Amgen, Analis, Bristol-Myers Squibb, Ebewe, Genévrier, GlaxoSmithKline, IBSA, Eli Lilly, Merck Sharp & Dohme, Merckle, Negma, Novartis, Novo Nordisk, NPS Pharmaceuticals, Nycomed, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Wyeth, UCB, and Zodiac.
ACPA-Negative RA Incidence Spikes During First Postpartum Year
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: During the year following giving birth, women had a statistically significant, 2.4-fold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women.
Data Source: Case-control study of 1,205 Swedish women enrolled in the Epidemiological Investigation of Rheumatoid Arthritis study during 1996-2006.
Disclosures: Dr. Bengtsson said that she had no disclosures.
ACPA-Negative RA Incidence Spikes During First Postpartum Year
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
LONDON – Women who give birth to a child face a twofold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women, but they have no increased risk for developing ACPA-positive disease, based on results from a Swedish epidemiologic study
The finding is consistent with a report last year from a Norwegian study that women face about a twofold increased risk for incident rheumatoid arthritis (RA) during the first 2 years after giving birth to a child, compared with their RA risk 2-4 years postpartum (Ann. Rheum. Dis. 2010;69:332-6). The reason why the new analysis, which included more than 1,200 cases and controls, showed a different relationship between partum and the onset of anticitrullinated peptide antibody (ACPA) –positive RH and ACPA-negative RA remains unclear, according to Camilla Bengtsson, Ph.D.
"Why there is only an association with ACPA-negative disease, and which biological mechanisms are involved remains to be elucidated," said Dr. Bengtsson, a researcher at the Karolinska Institute in Stockholm. The way in which this finding might apply to practice also remains unclear, she added.
Dr. Bengtsson’s analysis failed to show an increased incidence of any form of RA in women who were more than a year out from their delivery.
The study used data and blood specimens from Swedish women aged 18-50 years who were enrolled in the Epidemiological Investigation of RA (EIRA) study during 1996-2006. Among the women with incident RA enrolled in EIRA, 547 (95%) agreed to participate and provide blood specimens, and among the control women in the study, 658 (81%) provided blood. The analysis divided the cases and controls into subgroups based on their partum status. The 547 women with new-onset RA included 360 who had given birth and 187 who had not. The parous women included 226 with ACPA-positive RA and 134 with the ACPA-negative form. Among the nulliparous women with RA, 127 had the ACPA-positive form and 60 were ACPA negative.
Among the controls with no RA, 431 had given birth and 227 had never given birth.
The case-control analysis showed that among all women with incident RA, birth status during the year preceding a new RA diagnosis had no statistically significant relationship with RA onset. However, among women who developed ACPA-negative RA, their risk spiked by a statistically significant, 2.4-fold rate during the year following partum, compared with nulliparous women. In contrast, the incidence of ACPA-positive RA showed no significant relationship to partum status during the preceding year.
Further analysis examined the timing between delivery and onset of ACPA-negative RA more closely. Again, the analysis showed that, during the year following giving birth, women faced a statistically significant, 2.4-fold elevated risk for incident ACPA-negative RA, compared with nulliparous women. During the 2-10 years following giving birth, the rate of incident ACPA-negative RA dropped to a 50% higher risk, compared with nulliparous women, but this difference was not considered statistically significant. And women more than 10 years out from their most recent delivery had a risk for incident ACPA-negative RA identical to the nulliparous women, Dr. Bengtsson reported.
Dr. Bengtsson said that she had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: During the year following giving birth, women had a statistically significant, 2.4-fold increased risk of incident ACPA-negative rheumatoid arthritis, compared with nulliparous women.
Data Source: Case-control study of 1,205 Swedish women enrolled in the Epidemiological Investigation of Rheumatoid Arthritis study during 1996-2006.
Disclosures: Dr. Bengtsson said that she had no disclosures.