User login
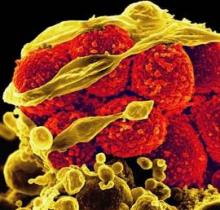
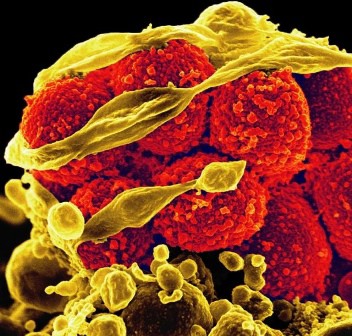
Don't Screen, Clean: MRSA Rates Slashed by ICU Scrub Down
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
AT IDWEEK 2012
Major Finding: Universal decolonization with chlorhexidine and mupirocin in adult intensive care units led to a 37% reduced risk of a methicillin-resistant S. aureus clinical isolate and a 44% reduced risk of bloodstream infections caused by all pathogens.
Data Source: These findings come from a study of 43 hospitals in 16 states that were randomized to one of three ICU strategies for reducing bloodstream infections over a period of 18 months.
Disclosures: The study was supported by funding from the Agency for Healthcare Research and Quality and from the Centers for Disease Control and Prevention. Dr. Huang said that she had no relevant financial conflicts.
IDWeek 2012 - Conference Coverage
IDWeek 2012 is being held in San Diego, Oct. 17-21. Our reporting team will provide coverage. Check back here from the latest from this meeting.
IDWeek 2012 is being held in San Diego, Oct. 17-21. Our reporting team will provide coverage. Check back here from the latest from this meeting.
IDWeek 2012 is being held in San Diego, Oct. 17-21. Our reporting team will provide coverage. Check back here from the latest from this meeting.