User login
American Society for Laser Medicine and Surgery (ASLMS): Laser 2014 ASLMS Annual Conference
Picosecond laser makes its mark for tattoo removal
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
AT LASER 2014
Brazilian patients favor noninvasive body contouring technique
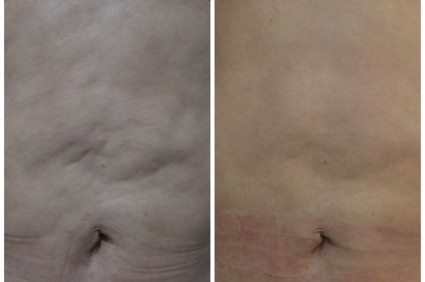
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: The findings highlight the importance of understanding patients’ preferences while managing their expectations.
Major finding: Satisfaction after treatment was "excellent" in 60% of patients and "good" in 40%.
Data source: A case series of body contouring using radiofrequency and magnetic pulse in 260 patients at five Brazilian centers.
Disclosures: Dr. Nunes reported having no disclosures.
VIDEO: ‘Three D’ for hepatitis C called ‘revolutionary’
CHICAGO – An experimental triple-drug regimen with or without ribavirin cured more than 90% of 724 previously untreated patients with hepatitis C genotype 1 who did not have cirrhosis.
And it was done without interferon.
Dr. Bruce R. Bacon called this oral regimen "revolutionary" in an interview during the annual Digestive Disease Week. Dr. Bacon is the James F. King Endowed Chair in Gastroenterology and a professor of medicine at St. Louis University. He was not involved in the study.
Hear his thoughts on treatment with ABT-450 with ritonavir, ombitasvir, and dasabuvir (known as the "three D" regimen) with or without ribavirin.
Dr. Bacon reported financial associations with AbbVie, which is developing the new drugs; Gilead Sciences; and Janssen Pharmaceuticals.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
CHICAGO – An experimental triple-drug regimen with or without ribavirin cured more than 90% of 724 previously untreated patients with hepatitis C genotype 1 who did not have cirrhosis.
And it was done without interferon.
Dr. Bruce R. Bacon called this oral regimen "revolutionary" in an interview during the annual Digestive Disease Week. Dr. Bacon is the James F. King Endowed Chair in Gastroenterology and a professor of medicine at St. Louis University. He was not involved in the study.
Hear his thoughts on treatment with ABT-450 with ritonavir, ombitasvir, and dasabuvir (known as the "three D" regimen) with or without ribavirin.
Dr. Bacon reported financial associations with AbbVie, which is developing the new drugs; Gilead Sciences; and Janssen Pharmaceuticals.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
CHICAGO – An experimental triple-drug regimen with or without ribavirin cured more than 90% of 724 previously untreated patients with hepatitis C genotype 1 who did not have cirrhosis.
And it was done without interferon.
Dr. Bruce R. Bacon called this oral regimen "revolutionary" in an interview during the annual Digestive Disease Week. Dr. Bacon is the James F. King Endowed Chair in Gastroenterology and a professor of medicine at St. Louis University. He was not involved in the study.
Hear his thoughts on treatment with ABT-450 with ritonavir, ombitasvir, and dasabuvir (known as the "three D" regimen) with or without ribavirin.
Dr. Bacon reported financial associations with AbbVie, which is developing the new drugs; Gilead Sciences; and Janssen Pharmaceuticals.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT DDW 2014
Gold-coated microparticles aid acne treatment
PHOENIX – Application of gold-coated microparticles to the skin may enhance laser photothermolysis of sebaceous glands to treat acne, according to three small, preliminary studies.
Inadequate contrast in sebaceous glands has limited the effectiveness of selective photothermolysis to treat acne. Specially engineered 0.150-mcm microparticles of inert gold coating a silica core were designed for surface plasmon resonance at near-infrared wavelengths to optimize contrast and high absorption of light in the sebaceous glands during laser treatment.
In a randomized, controlled crossover study, 48 patients with acne vulgaris received either immediate or delayed treatment for 12 weeks, after which the delayed-treatment group also began receiving the treatment. Immediate treatment included three treatments at 2-week intervals. The treatment consisted of a microparticle suspension gently massaged into facial skin for about 8 minutes, superficial skin cleansing, and pulsed irradiation with two passes of an 800-nm laser. Patients in the delayed-treatment group used an over-the-counter face wash (2% salicylic acid) twice daily.
The mean number of inflammatory lesions decreased by 34% at 12 weeks after treatment started, compared with a 16% reduction in the control group, a statistically significant difference, Dilip Paithankar, Ph.D., reported at the annual meeting of the American Society for Laser Medicine and Surgery.
At 28 weeks after the crossover to treatment for all subjects (40 weeks after the start of the study), the mean number of inflammatory lesions decreased by 61%, reported Dr. Paithankar, chief technology officer at Sebacia, Duluth, Ga., which is developing the gold-coated microparticles treatment.
In another randomized, sham-controlled study, 49 patients with acne vulgaris underwent three laser photothermolysis treatments at weekly intervals using either the gold-coated microparticles or a control vehicle without the particles. Mean inflammatory lesion counts decreased significantly more in the treatment group than in the control group at 8, 12, and 16 weeks of follow-up. In the treatment group, mean inflammatory lesion counts were 44% lower at 8 weeks, 49% lower at 12 weeks, and 53% lower at 16 weeks, compared with baseline. In the control group, mean inflammatory lesion counts were 14% lower, 22% lower, and 31% lower at those time points, respectively, compared with baseline.
Inflammatory lesions were clear or almost clear by the end of the study in 24% in the treatment group and in none of the control patients.
Data from a separate histologic study suggest that using ultrasound to assist delivery of the gold-coated microparticles may improve selective destruction from laser treatment, Dr. Girish Munavalli reported at the meeting. Ultrasound has been used in other settings to enhance delivery of small molecules through the stratum corneum.
The study used an ultrasound horn vibrating in a microparticle suspension placed in an enclosure above preauricular skin in 37 subjects, followed by 800-nm laser treatment. Biopsies taken within 15 minutes showed localized thermal injury to infundibuli and sebaceous glands with no collateral damage to surrounding tissue or to the epidermis, reported Dr. Munavalli, a dermatologist in group practice in Charlotte, N.C. The extent of thermal damage correlated with the duration of the ultrasound.
The level of damage could be expected to improve acne, but that needs confirmation in clinical trials, he said.
In each of the studies, the treatments were well tolerated, with minimal side effects including mild to moderate pain (using no anesthetic) and short-lived erythema and edema.
Dr. Paithankar works for Sebacia. Dr. Munavalli reported having no disclosures; some of his coinvestigators work for Sebacia.
On Twitter @sherryboschert
PHOENIX – Application of gold-coated microparticles to the skin may enhance laser photothermolysis of sebaceous glands to treat acne, according to three small, preliminary studies.
Inadequate contrast in sebaceous glands has limited the effectiveness of selective photothermolysis to treat acne. Specially engineered 0.150-mcm microparticles of inert gold coating a silica core were designed for surface plasmon resonance at near-infrared wavelengths to optimize contrast and high absorption of light in the sebaceous glands during laser treatment.
In a randomized, controlled crossover study, 48 patients with acne vulgaris received either immediate or delayed treatment for 12 weeks, after which the delayed-treatment group also began receiving the treatment. Immediate treatment included three treatments at 2-week intervals. The treatment consisted of a microparticle suspension gently massaged into facial skin for about 8 minutes, superficial skin cleansing, and pulsed irradiation with two passes of an 800-nm laser. Patients in the delayed-treatment group used an over-the-counter face wash (2% salicylic acid) twice daily.
The mean number of inflammatory lesions decreased by 34% at 12 weeks after treatment started, compared with a 16% reduction in the control group, a statistically significant difference, Dilip Paithankar, Ph.D., reported at the annual meeting of the American Society for Laser Medicine and Surgery.
At 28 weeks after the crossover to treatment for all subjects (40 weeks after the start of the study), the mean number of inflammatory lesions decreased by 61%, reported Dr. Paithankar, chief technology officer at Sebacia, Duluth, Ga., which is developing the gold-coated microparticles treatment.
In another randomized, sham-controlled study, 49 patients with acne vulgaris underwent three laser photothermolysis treatments at weekly intervals using either the gold-coated microparticles or a control vehicle without the particles. Mean inflammatory lesion counts decreased significantly more in the treatment group than in the control group at 8, 12, and 16 weeks of follow-up. In the treatment group, mean inflammatory lesion counts were 44% lower at 8 weeks, 49% lower at 12 weeks, and 53% lower at 16 weeks, compared with baseline. In the control group, mean inflammatory lesion counts were 14% lower, 22% lower, and 31% lower at those time points, respectively, compared with baseline.
Inflammatory lesions were clear or almost clear by the end of the study in 24% in the treatment group and in none of the control patients.
Data from a separate histologic study suggest that using ultrasound to assist delivery of the gold-coated microparticles may improve selective destruction from laser treatment, Dr. Girish Munavalli reported at the meeting. Ultrasound has been used in other settings to enhance delivery of small molecules through the stratum corneum.
The study used an ultrasound horn vibrating in a microparticle suspension placed in an enclosure above preauricular skin in 37 subjects, followed by 800-nm laser treatment. Biopsies taken within 15 minutes showed localized thermal injury to infundibuli and sebaceous glands with no collateral damage to surrounding tissue or to the epidermis, reported Dr. Munavalli, a dermatologist in group practice in Charlotte, N.C. The extent of thermal damage correlated with the duration of the ultrasound.
The level of damage could be expected to improve acne, but that needs confirmation in clinical trials, he said.
In each of the studies, the treatments were well tolerated, with minimal side effects including mild to moderate pain (using no anesthetic) and short-lived erythema and edema.
Dr. Paithankar works for Sebacia. Dr. Munavalli reported having no disclosures; some of his coinvestigators work for Sebacia.
On Twitter @sherryboschert
PHOENIX – Application of gold-coated microparticles to the skin may enhance laser photothermolysis of sebaceous glands to treat acne, according to three small, preliminary studies.
Inadequate contrast in sebaceous glands has limited the effectiveness of selective photothermolysis to treat acne. Specially engineered 0.150-mcm microparticles of inert gold coating a silica core were designed for surface plasmon resonance at near-infrared wavelengths to optimize contrast and high absorption of light in the sebaceous glands during laser treatment.
In a randomized, controlled crossover study, 48 patients with acne vulgaris received either immediate or delayed treatment for 12 weeks, after which the delayed-treatment group also began receiving the treatment. Immediate treatment included three treatments at 2-week intervals. The treatment consisted of a microparticle suspension gently massaged into facial skin for about 8 minutes, superficial skin cleansing, and pulsed irradiation with two passes of an 800-nm laser. Patients in the delayed-treatment group used an over-the-counter face wash (2% salicylic acid) twice daily.
The mean number of inflammatory lesions decreased by 34% at 12 weeks after treatment started, compared with a 16% reduction in the control group, a statistically significant difference, Dilip Paithankar, Ph.D., reported at the annual meeting of the American Society for Laser Medicine and Surgery.
At 28 weeks after the crossover to treatment for all subjects (40 weeks after the start of the study), the mean number of inflammatory lesions decreased by 61%, reported Dr. Paithankar, chief technology officer at Sebacia, Duluth, Ga., which is developing the gold-coated microparticles treatment.
In another randomized, sham-controlled study, 49 patients with acne vulgaris underwent three laser photothermolysis treatments at weekly intervals using either the gold-coated microparticles or a control vehicle without the particles. Mean inflammatory lesion counts decreased significantly more in the treatment group than in the control group at 8, 12, and 16 weeks of follow-up. In the treatment group, mean inflammatory lesion counts were 44% lower at 8 weeks, 49% lower at 12 weeks, and 53% lower at 16 weeks, compared with baseline. In the control group, mean inflammatory lesion counts were 14% lower, 22% lower, and 31% lower at those time points, respectively, compared with baseline.
Inflammatory lesions were clear or almost clear by the end of the study in 24% in the treatment group and in none of the control patients.
Data from a separate histologic study suggest that using ultrasound to assist delivery of the gold-coated microparticles may improve selective destruction from laser treatment, Dr. Girish Munavalli reported at the meeting. Ultrasound has been used in other settings to enhance delivery of small molecules through the stratum corneum.
The study used an ultrasound horn vibrating in a microparticle suspension placed in an enclosure above preauricular skin in 37 subjects, followed by 800-nm laser treatment. Biopsies taken within 15 minutes showed localized thermal injury to infundibuli and sebaceous glands with no collateral damage to surrounding tissue or to the epidermis, reported Dr. Munavalli, a dermatologist in group practice in Charlotte, N.C. The extent of thermal damage correlated with the duration of the ultrasound.
The level of damage could be expected to improve acne, but that needs confirmation in clinical trials, he said.
In each of the studies, the treatments were well tolerated, with minimal side effects including mild to moderate pain (using no anesthetic) and short-lived erythema and edema.
Dr. Paithankar works for Sebacia. Dr. Munavalli reported having no disclosures; some of his coinvestigators work for Sebacia.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: Inadequate contrast has limited the use of laser targeting of the sebaceous glands; specially designed gold-coated microparticles are designed to improve contrast and promote light absorption.
Major finding: Laser treatment of acne vulgaris preceded by application of gold-coated microparticles decreased mean inflammatory lesion counts by 34% and 49% at 12 weeks in two separate studies, compared with reductions of 16% and 22% in control groups.
Data source: Two randomized, controlled trials of 48 patients and 49 patients, respectively, with acne vulgaris, and a separate histologic study of 37 subjects.
Disclosures: Dr. Paithankar works for Sebacia, which developed the gold-coated microparticles treatment. Dr. Munavalli reported having no disclosures; some of his coinvestigators work for Sebacia.
Laser settings tested against melasma
PHOENIX – Treating moderate to severe melasma with a 50-ns, 1,064-nm Q-switched neodynium:YAG laser produced equivalent temporary results with less pain than did a 5-ns, 1,064-nm Q-switched Nd:YAG laser in a split-face study of 10 women.
In the 6-month study, scores on a melasma area and severity index decreased by 16% using the 50-ns pulse width, and by 27% using the 5-ns pulse width at month 4, which was 1 month after the last of three monthly treatments that combined microdermabrasion, laser therapy, and a topical therapy regimen. Changes from both lasers were statistically significant compared with baseline, but not significantly different between laser groups, Dr. Vineet Mishra reported at the annual meeting of the American Society for Laser Medicine and Surgery.
The investigators sought to optimize laser settings for treating melasma to see whether lasers could be used in combination with other melasma therapies, Dr. Mishra said in an interview.
"During the study, everybody improved," Dr. Mishra said.
Melanin (as measured by a reflectance spectrophotometer at each visit) decreased by 20% with the 50-ns pulse width and by 17% with the 5-ns pulse width during the study.
However, pigment relapsed in both treatment areas after the study, to a level not significantly different from that at baseline. This was not unexpected when treating melasma, and was "likely due to sun exposure in sunny San Diego," said Dr. Mishra, director of Mohs surgery and procedural dermatology at the University of Texas Health Science Center, San Antonio.
Patients who completed the study rated pain from the procedure as a mean of 1.2 on the side of the face treated with the 50-ns laser and 2.9 with the 5-ns laser, using a 10-point scale with 0 representing no pain and 10 the worst pain, Dr. Mishra said.
Each treatment session consisted of microdermabrasion of the entire face followed by treatment with the 50-ns laser on one side and treatment with the 5-ns laser on the other side. Two laser passes were applied using a fluence of 1.6 J/cm2 and a 5-mm spot size. For 2 weeks prior to each treatment session and starting 2 days after each laser treatment, patients were asked to follow a daily skin care regimen that consisted of topical 4% hydroquinone, 0.05% tretinoin cream, and sunscreen with a sun protection factor of 50.
"Lasers have exploded on the market" but can be tricky to use against melasma, Dr. Mishra said. Too-high levels of laser energy can cause postinflammatory hyperpigmentation, which can worsen melasma, he noted.
Melasma is a difficult condition to treat, but "combination therapy is optimal," Dr. Mishra added in an interview. Next steps for research should include longer-term studies to determine how patients would fare if they continued with the combination treatment regimen. In addition, using a picosecond laser for melasma "would be a new frontier" to explore in long-term studies, he said.
The study won an award at the meeting.
The study received funding from Syneron and Candela, which market the 50-ns laser, and one of Dr. Mishra’s coinvestigators reported financial associations with Syneron and Candela and with Cynosure, which markets the 5-ns laser.
On Twitter @sherryboschert
PHOENIX – Treating moderate to severe melasma with a 50-ns, 1,064-nm Q-switched neodynium:YAG laser produced equivalent temporary results with less pain than did a 5-ns, 1,064-nm Q-switched Nd:YAG laser in a split-face study of 10 women.
In the 6-month study, scores on a melasma area and severity index decreased by 16% using the 50-ns pulse width, and by 27% using the 5-ns pulse width at month 4, which was 1 month after the last of three monthly treatments that combined microdermabrasion, laser therapy, and a topical therapy regimen. Changes from both lasers were statistically significant compared with baseline, but not significantly different between laser groups, Dr. Vineet Mishra reported at the annual meeting of the American Society for Laser Medicine and Surgery.
The investigators sought to optimize laser settings for treating melasma to see whether lasers could be used in combination with other melasma therapies, Dr. Mishra said in an interview.
"During the study, everybody improved," Dr. Mishra said.
Melanin (as measured by a reflectance spectrophotometer at each visit) decreased by 20% with the 50-ns pulse width and by 17% with the 5-ns pulse width during the study.
However, pigment relapsed in both treatment areas after the study, to a level not significantly different from that at baseline. This was not unexpected when treating melasma, and was "likely due to sun exposure in sunny San Diego," said Dr. Mishra, director of Mohs surgery and procedural dermatology at the University of Texas Health Science Center, San Antonio.
Patients who completed the study rated pain from the procedure as a mean of 1.2 on the side of the face treated with the 50-ns laser and 2.9 with the 5-ns laser, using a 10-point scale with 0 representing no pain and 10 the worst pain, Dr. Mishra said.
Each treatment session consisted of microdermabrasion of the entire face followed by treatment with the 50-ns laser on one side and treatment with the 5-ns laser on the other side. Two laser passes were applied using a fluence of 1.6 J/cm2 and a 5-mm spot size. For 2 weeks prior to each treatment session and starting 2 days after each laser treatment, patients were asked to follow a daily skin care regimen that consisted of topical 4% hydroquinone, 0.05% tretinoin cream, and sunscreen with a sun protection factor of 50.
"Lasers have exploded on the market" but can be tricky to use against melasma, Dr. Mishra said. Too-high levels of laser energy can cause postinflammatory hyperpigmentation, which can worsen melasma, he noted.
Melasma is a difficult condition to treat, but "combination therapy is optimal," Dr. Mishra added in an interview. Next steps for research should include longer-term studies to determine how patients would fare if they continued with the combination treatment regimen. In addition, using a picosecond laser for melasma "would be a new frontier" to explore in long-term studies, he said.
The study won an award at the meeting.
The study received funding from Syneron and Candela, which market the 50-ns laser, and one of Dr. Mishra’s coinvestigators reported financial associations with Syneron and Candela and with Cynosure, which markets the 5-ns laser.
On Twitter @sherryboschert
PHOENIX – Treating moderate to severe melasma with a 50-ns, 1,064-nm Q-switched neodynium:YAG laser produced equivalent temporary results with less pain than did a 5-ns, 1,064-nm Q-switched Nd:YAG laser in a split-face study of 10 women.
In the 6-month study, scores on a melasma area and severity index decreased by 16% using the 50-ns pulse width, and by 27% using the 5-ns pulse width at month 4, which was 1 month after the last of three monthly treatments that combined microdermabrasion, laser therapy, and a topical therapy regimen. Changes from both lasers were statistically significant compared with baseline, but not significantly different between laser groups, Dr. Vineet Mishra reported at the annual meeting of the American Society for Laser Medicine and Surgery.
The investigators sought to optimize laser settings for treating melasma to see whether lasers could be used in combination with other melasma therapies, Dr. Mishra said in an interview.
"During the study, everybody improved," Dr. Mishra said.
Melanin (as measured by a reflectance spectrophotometer at each visit) decreased by 20% with the 50-ns pulse width and by 17% with the 5-ns pulse width during the study.
However, pigment relapsed in both treatment areas after the study, to a level not significantly different from that at baseline. This was not unexpected when treating melasma, and was "likely due to sun exposure in sunny San Diego," said Dr. Mishra, director of Mohs surgery and procedural dermatology at the University of Texas Health Science Center, San Antonio.
Patients who completed the study rated pain from the procedure as a mean of 1.2 on the side of the face treated with the 50-ns laser and 2.9 with the 5-ns laser, using a 10-point scale with 0 representing no pain and 10 the worst pain, Dr. Mishra said.
Each treatment session consisted of microdermabrasion of the entire face followed by treatment with the 50-ns laser on one side and treatment with the 5-ns laser on the other side. Two laser passes were applied using a fluence of 1.6 J/cm2 and a 5-mm spot size. For 2 weeks prior to each treatment session and starting 2 days after each laser treatment, patients were asked to follow a daily skin care regimen that consisted of topical 4% hydroquinone, 0.05% tretinoin cream, and sunscreen with a sun protection factor of 50.
"Lasers have exploded on the market" but can be tricky to use against melasma, Dr. Mishra said. Too-high levels of laser energy can cause postinflammatory hyperpigmentation, which can worsen melasma, he noted.
Melasma is a difficult condition to treat, but "combination therapy is optimal," Dr. Mishra added in an interview. Next steps for research should include longer-term studies to determine how patients would fare if they continued with the combination treatment regimen. In addition, using a picosecond laser for melasma "would be a new frontier" to explore in long-term studies, he said.
The study won an award at the meeting.
The study received funding from Syneron and Candela, which market the 50-ns laser, and one of Dr. Mishra’s coinvestigators reported financial associations with Syneron and Candela and with Cynosure, which markets the 5-ns laser.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: Finding the optimal settings for lasers in patients with melasma could help improve the condition as part of a combination treatment regimen.
Major finding: Both the 50-ns and 5-ns pulse widths significantly decreased melasma area and severity index scores temporarily, but mean pain scores were significantly lower with the 50-ns laser (1.2) than with the 5-ns laser (2.9).
Data source: A prospective, randomized split-face comparison of 50-ns and 5-ns 1,064-nm Q-switched Nd:YAG laser therapy, plus dermabrasion and topical therapy for melasma.
Disclosures: The study received funding from Syneron and Candela, which market the 50-ns laser, and one of Dr. Mishra’s coinvestigators reported financial associations with Syneron and Candela and with Cynosure, which markets the 5-ns laser.
Early look: Localized cryolysis reduced sebum by 40%
PHOENIX – One cycle of selective transepidermal cooling on the backs of 11 men with healthy, normal skin produced a transient 40% reduction in sebum production by sebaceous glands in a controlled pilot study.
Sebum production fell significantly by 1 and 2 weeks after treatment, compared with production prior to treatment, but by week 4, was not significantly different than at baseline, Dr. H. Ray Jalian and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery. Sebum production did not change significantly on untreated patches of skin that served as controls.
The results give hope that selective cryolysis of sebaceous glands might be a noninvasive treatment for acne vulgaris, which should be explored in additional studies, said Dr. Jalian of the Wellman Center for Photomedicine, Massachusetts General Hospital, Boston.
The study won a top award at the meeting and piqued the interest of attendees. Dr. Jeffrey Dover, immediate past president of the ASLMS, explained the excitement over this small pilot study.
"If you extend that to the future, after they do more studies; more cold for longer [time periods], or maybe more applications may produce prolonged sebaceous gland inactivity," he noted. "And maybe [achieve] permanent sebaceous gland inactivity, which theoretically could be a cure for acne – there could be Accutane-like results with an applicator that’s cold, with no side effects," said Dr. Dover, a dermatologist in Chestnut Hill, Mass. "Now, that would be an advance for dermatology," he said in an interview.
Sebumeter measurements at 2 weeks (the primary outcome measure) showed a 40% reduction in sebum production for two temperature settings, compared with baseline.
The study involved the off-label use of a handheld cooling applicator that has been approved for body sculpting to destroy fat in some body areas. Lipid-rich tissue is susceptible to cold injury, and the researchers hoped to target the lipid content of the sebaceous glands.
Participants were randomized to treatment on select areas of their backs at temperatures of –10° C or –15° C, and they received either a single 20-minute cooling cycle or two 10-minute cooling cycles with rewarming in between. Some skin areas on the scapulas served as control sites, and each subject had two treatment sites and one control site. Sebum measurements and standardized clinical photos were taken just before treatment and on follow-up visits at 3 days (72 hours) and at 1, 2, and 4 weeks.
Among secondary outcomes, a smaller but significant sebum reduction occurred at 1 week, but sebum production did not differ significantly at 72 hours or at 4 weeks, compared with baseline. Transient pain reported during treatment (average on a Visual Analog Scale score of approximately 3 on a 10-point scale) disappeared quickly post treatment and at follow-up visits. "It actually was a very-well-tolerated procedure," Dr. Jalian said.
Transient post-treatment erythema, dysesthesia, and edema also cleared quickly, though one subject had erythema lasting approximately 72 hours, according to blinded evaluators.
"Perhaps the most interesting part of our study was the histology," Dr. Jalian noted. Biopsies from a subset of participants showed histologic evidence of sebaceous gland damage after treatment that persisted at weeks 1 and 2.
There was no clinical or histologic evidence of damage to tissue outside of the treated areas.
"Selective cryolysis of sebaceous glands is achievable through noninvasive cooling," said Dr. Jalian. Future studies may examine whether repeated treatments could maintain the reduction in sebum output beyond 2 weeks, he added.
Previous studies have shown that a 30%-50% reduction in sebum is needed to produce a 50% improvement in acne (Br. J. Dermatol. 2010;163:683-8).
The human pilot study followed preclinical experiments on the ears of mice, sheep, and pigs that showed histologic damage in sebaceous glands after treatment, Dr. Jalian said.
The study was funded by Zeltiq Aesthetics, which makes the handheld cooling device. Dr. Jalian reported no other relevant disclosures.
On Twitter @sherryboschert
PHOENIX – One cycle of selective transepidermal cooling on the backs of 11 men with healthy, normal skin produced a transient 40% reduction in sebum production by sebaceous glands in a controlled pilot study.
Sebum production fell significantly by 1 and 2 weeks after treatment, compared with production prior to treatment, but by week 4, was not significantly different than at baseline, Dr. H. Ray Jalian and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery. Sebum production did not change significantly on untreated patches of skin that served as controls.
The results give hope that selective cryolysis of sebaceous glands might be a noninvasive treatment for acne vulgaris, which should be explored in additional studies, said Dr. Jalian of the Wellman Center for Photomedicine, Massachusetts General Hospital, Boston.
The study won a top award at the meeting and piqued the interest of attendees. Dr. Jeffrey Dover, immediate past president of the ASLMS, explained the excitement over this small pilot study.
"If you extend that to the future, after they do more studies; more cold for longer [time periods], or maybe more applications may produce prolonged sebaceous gland inactivity," he noted. "And maybe [achieve] permanent sebaceous gland inactivity, which theoretically could be a cure for acne – there could be Accutane-like results with an applicator that’s cold, with no side effects," said Dr. Dover, a dermatologist in Chestnut Hill, Mass. "Now, that would be an advance for dermatology," he said in an interview.
Sebumeter measurements at 2 weeks (the primary outcome measure) showed a 40% reduction in sebum production for two temperature settings, compared with baseline.
The study involved the off-label use of a handheld cooling applicator that has been approved for body sculpting to destroy fat in some body areas. Lipid-rich tissue is susceptible to cold injury, and the researchers hoped to target the lipid content of the sebaceous glands.
Participants were randomized to treatment on select areas of their backs at temperatures of –10° C or –15° C, and they received either a single 20-minute cooling cycle or two 10-minute cooling cycles with rewarming in between. Some skin areas on the scapulas served as control sites, and each subject had two treatment sites and one control site. Sebum measurements and standardized clinical photos were taken just before treatment and on follow-up visits at 3 days (72 hours) and at 1, 2, and 4 weeks.
Among secondary outcomes, a smaller but significant sebum reduction occurred at 1 week, but sebum production did not differ significantly at 72 hours or at 4 weeks, compared with baseline. Transient pain reported during treatment (average on a Visual Analog Scale score of approximately 3 on a 10-point scale) disappeared quickly post treatment and at follow-up visits. "It actually was a very-well-tolerated procedure," Dr. Jalian said.
Transient post-treatment erythema, dysesthesia, and edema also cleared quickly, though one subject had erythema lasting approximately 72 hours, according to blinded evaluators.
"Perhaps the most interesting part of our study was the histology," Dr. Jalian noted. Biopsies from a subset of participants showed histologic evidence of sebaceous gland damage after treatment that persisted at weeks 1 and 2.
There was no clinical or histologic evidence of damage to tissue outside of the treated areas.
"Selective cryolysis of sebaceous glands is achievable through noninvasive cooling," said Dr. Jalian. Future studies may examine whether repeated treatments could maintain the reduction in sebum output beyond 2 weeks, he added.
Previous studies have shown that a 30%-50% reduction in sebum is needed to produce a 50% improvement in acne (Br. J. Dermatol. 2010;163:683-8).
The human pilot study followed preclinical experiments on the ears of mice, sheep, and pigs that showed histologic damage in sebaceous glands after treatment, Dr. Jalian said.
The study was funded by Zeltiq Aesthetics, which makes the handheld cooling device. Dr. Jalian reported no other relevant disclosures.
On Twitter @sherryboschert
PHOENIX – One cycle of selective transepidermal cooling on the backs of 11 men with healthy, normal skin produced a transient 40% reduction in sebum production by sebaceous glands in a controlled pilot study.
Sebum production fell significantly by 1 and 2 weeks after treatment, compared with production prior to treatment, but by week 4, was not significantly different than at baseline, Dr. H. Ray Jalian and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery. Sebum production did not change significantly on untreated patches of skin that served as controls.
The results give hope that selective cryolysis of sebaceous glands might be a noninvasive treatment for acne vulgaris, which should be explored in additional studies, said Dr. Jalian of the Wellman Center for Photomedicine, Massachusetts General Hospital, Boston.
The study won a top award at the meeting and piqued the interest of attendees. Dr. Jeffrey Dover, immediate past president of the ASLMS, explained the excitement over this small pilot study.
"If you extend that to the future, after they do more studies; more cold for longer [time periods], or maybe more applications may produce prolonged sebaceous gland inactivity," he noted. "And maybe [achieve] permanent sebaceous gland inactivity, which theoretically could be a cure for acne – there could be Accutane-like results with an applicator that’s cold, with no side effects," said Dr. Dover, a dermatologist in Chestnut Hill, Mass. "Now, that would be an advance for dermatology," he said in an interview.
Sebumeter measurements at 2 weeks (the primary outcome measure) showed a 40% reduction in sebum production for two temperature settings, compared with baseline.
The study involved the off-label use of a handheld cooling applicator that has been approved for body sculpting to destroy fat in some body areas. Lipid-rich tissue is susceptible to cold injury, and the researchers hoped to target the lipid content of the sebaceous glands.
Participants were randomized to treatment on select areas of their backs at temperatures of –10° C or –15° C, and they received either a single 20-minute cooling cycle or two 10-minute cooling cycles with rewarming in between. Some skin areas on the scapulas served as control sites, and each subject had two treatment sites and one control site. Sebum measurements and standardized clinical photos were taken just before treatment and on follow-up visits at 3 days (72 hours) and at 1, 2, and 4 weeks.
Among secondary outcomes, a smaller but significant sebum reduction occurred at 1 week, but sebum production did not differ significantly at 72 hours or at 4 weeks, compared with baseline. Transient pain reported during treatment (average on a Visual Analog Scale score of approximately 3 on a 10-point scale) disappeared quickly post treatment and at follow-up visits. "It actually was a very-well-tolerated procedure," Dr. Jalian said.
Transient post-treatment erythema, dysesthesia, and edema also cleared quickly, though one subject had erythema lasting approximately 72 hours, according to blinded evaluators.
"Perhaps the most interesting part of our study was the histology," Dr. Jalian noted. Biopsies from a subset of participants showed histologic evidence of sebaceous gland damage after treatment that persisted at weeks 1 and 2.
There was no clinical or histologic evidence of damage to tissue outside of the treated areas.
"Selective cryolysis of sebaceous glands is achievable through noninvasive cooling," said Dr. Jalian. Future studies may examine whether repeated treatments could maintain the reduction in sebum output beyond 2 weeks, he added.
Previous studies have shown that a 30%-50% reduction in sebum is needed to produce a 50% improvement in acne (Br. J. Dermatol. 2010;163:683-8).
The human pilot study followed preclinical experiments on the ears of mice, sheep, and pigs that showed histologic damage in sebaceous glands after treatment, Dr. Jalian said.
The study was funded by Zeltiq Aesthetics, which makes the handheld cooling device. Dr. Jalian reported no other relevant disclosures.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: Cryolysis of the sebaceous glands might provide a noninvasive option for acne treatment.
Major finding: Sebum excretion was 40% lower 2 weeks after transepidermal cryolysis treatment of sebaceous glands, compared with baseline.
Data source: A prospective, controlled pilot study of 11 healthy men who were treated on selected areas on their backs.
Disclosures: The study was funded by Zeltiq Aesthetics, which makes the handheld cooling device used in the study. Dr. Jalian reported no other relevant disclosures.
Three laser/light devices lead injury reports
PHOENIX – Radiofrequency devices, diode lasers, and intense pulsed light devices had the most reports of suspected injuries from 1991 through 2013, based on data from a Food and Drug Administration database.
During that period, 1,212 medical device reports were submitted for suspected injuries from laser or light device use or malfunction to the FDA’s MAUDE (Manufacturer and User Facility Device Experience) database, as well as another 45 that were excluded from the study because of insufficient data. The FDA requires device users and manufacturers to submit the reports and collects voluntary reports from patients. Each report may contain more than one adverse event.
Blisters or burns were the most common problems reported to the MAUDE database for each of the top three devices, Dr. Anne Marie Tremaine and her associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Radiofrequency devices were the subject of 270 reports that included 294 adverse events. These reports included 119 burns or blisters; 85 incidents of fat loss, depression, or divot; 34 scars; 25 incidents of dyschromia (both hyper- and hypopigmentation); and 12 cases of sagging skin. In addition, a few reports noted burns in the area of the return pad, paresthesia or nerve palsy, dry eye or "floaters," and cracked dental crowns.
Insufficient coupling fluid and tearing or breakdown in the device tip membrane topped the reasons given for problems related to radiofrequency treatment, reported Dr. Tremaine of Massachusetts General Hospital’s Wellman Center for Photomedicine, Boston. Complications also were ascribed to tumescent anesthesia, intradermal lidocaine injections, and general anesthesia.
The most common treatment modality associated with adverse events was laser hair removal using diode lasers or intense pulsed light. The 252 reports on diode lasers included 297 burns or blisters, 42 incidents of dyschromia, 11 scars, and 8 cases of swelling. The 158 reports on adverse events from intense pulsed light included 126 burns or blisters; 24 incidents of dyschromia; 20 scars; 13 patients with bruising; 12 incidents of fat loss, depression, or divot; and smaller numbers of eye injury or delayed wound healing.
Many of the complications in the reports were attributed to improper settings or improperly maintained device tips.
"Physicians should be aware of the adverse events and malfunctions of the devices used in dermatology," Dr. Tremaine said. The MAUDE database "will help uncover otherwise unreported events seen in routine practice among all types of practitioners" to supplement data from initial studies and reports in the medical literature. This information should help physicians better inform patients about the potential risks of treatment, she said.
Dr. Tremaine and her associates searched the MAUDE database using terms including names of device manufacturers from a comprehensive list, specific product names, and the wavelengths and technology of the devices used in dermatology.
However, because adverse events are underreported to MAUDE, which provides only passive surveillance, the incidence or prevalence of problems with laser or light devices could not be discerned from this database, the investigators noted.
Dr. Tremaine reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Radiofrequency devices, diode lasers, and intense pulsed light devices had the most reports of suspected injuries from 1991 through 2013, based on data from a Food and Drug Administration database.
During that period, 1,212 medical device reports were submitted for suspected injuries from laser or light device use or malfunction to the FDA’s MAUDE (Manufacturer and User Facility Device Experience) database, as well as another 45 that were excluded from the study because of insufficient data. The FDA requires device users and manufacturers to submit the reports and collects voluntary reports from patients. Each report may contain more than one adverse event.
Blisters or burns were the most common problems reported to the MAUDE database for each of the top three devices, Dr. Anne Marie Tremaine and her associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Radiofrequency devices were the subject of 270 reports that included 294 adverse events. These reports included 119 burns or blisters; 85 incidents of fat loss, depression, or divot; 34 scars; 25 incidents of dyschromia (both hyper- and hypopigmentation); and 12 cases of sagging skin. In addition, a few reports noted burns in the area of the return pad, paresthesia or nerve palsy, dry eye or "floaters," and cracked dental crowns.
Insufficient coupling fluid and tearing or breakdown in the device tip membrane topped the reasons given for problems related to radiofrequency treatment, reported Dr. Tremaine of Massachusetts General Hospital’s Wellman Center for Photomedicine, Boston. Complications also were ascribed to tumescent anesthesia, intradermal lidocaine injections, and general anesthesia.
The most common treatment modality associated with adverse events was laser hair removal using diode lasers or intense pulsed light. The 252 reports on diode lasers included 297 burns or blisters, 42 incidents of dyschromia, 11 scars, and 8 cases of swelling. The 158 reports on adverse events from intense pulsed light included 126 burns or blisters; 24 incidents of dyschromia; 20 scars; 13 patients with bruising; 12 incidents of fat loss, depression, or divot; and smaller numbers of eye injury or delayed wound healing.
Many of the complications in the reports were attributed to improper settings or improperly maintained device tips.
"Physicians should be aware of the adverse events and malfunctions of the devices used in dermatology," Dr. Tremaine said. The MAUDE database "will help uncover otherwise unreported events seen in routine practice among all types of practitioners" to supplement data from initial studies and reports in the medical literature. This information should help physicians better inform patients about the potential risks of treatment, she said.
Dr. Tremaine and her associates searched the MAUDE database using terms including names of device manufacturers from a comprehensive list, specific product names, and the wavelengths and technology of the devices used in dermatology.
However, because adverse events are underreported to MAUDE, which provides only passive surveillance, the incidence or prevalence of problems with laser or light devices could not be discerned from this database, the investigators noted.
Dr. Tremaine reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Radiofrequency devices, diode lasers, and intense pulsed light devices had the most reports of suspected injuries from 1991 through 2013, based on data from a Food and Drug Administration database.
During that period, 1,212 medical device reports were submitted for suspected injuries from laser or light device use or malfunction to the FDA’s MAUDE (Manufacturer and User Facility Device Experience) database, as well as another 45 that were excluded from the study because of insufficient data. The FDA requires device users and manufacturers to submit the reports and collects voluntary reports from patients. Each report may contain more than one adverse event.
Blisters or burns were the most common problems reported to the MAUDE database for each of the top three devices, Dr. Anne Marie Tremaine and her associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Radiofrequency devices were the subject of 270 reports that included 294 adverse events. These reports included 119 burns or blisters; 85 incidents of fat loss, depression, or divot; 34 scars; 25 incidents of dyschromia (both hyper- and hypopigmentation); and 12 cases of sagging skin. In addition, a few reports noted burns in the area of the return pad, paresthesia or nerve palsy, dry eye or "floaters," and cracked dental crowns.
Insufficient coupling fluid and tearing or breakdown in the device tip membrane topped the reasons given for problems related to radiofrequency treatment, reported Dr. Tremaine of Massachusetts General Hospital’s Wellman Center for Photomedicine, Boston. Complications also were ascribed to tumescent anesthesia, intradermal lidocaine injections, and general anesthesia.
The most common treatment modality associated with adverse events was laser hair removal using diode lasers or intense pulsed light. The 252 reports on diode lasers included 297 burns or blisters, 42 incidents of dyschromia, 11 scars, and 8 cases of swelling. The 158 reports on adverse events from intense pulsed light included 126 burns or blisters; 24 incidents of dyschromia; 20 scars; 13 patients with bruising; 12 incidents of fat loss, depression, or divot; and smaller numbers of eye injury or delayed wound healing.
Many of the complications in the reports were attributed to improper settings or improperly maintained device tips.
"Physicians should be aware of the adverse events and malfunctions of the devices used in dermatology," Dr. Tremaine said. The MAUDE database "will help uncover otherwise unreported events seen in routine practice among all types of practitioners" to supplement data from initial studies and reports in the medical literature. This information should help physicians better inform patients about the potential risks of treatment, she said.
Dr. Tremaine and her associates searched the MAUDE database using terms including names of device manufacturers from a comprehensive list, specific product names, and the wavelengths and technology of the devices used in dermatology.
However, because adverse events are underreported to MAUDE, which provides only passive surveillance, the incidence or prevalence of problems with laser or light devices could not be discerned from this database, the investigators noted.
Dr. Tremaine reported having no disclosures.
On Twitter @sherryboschert
AT LASER 2014
Major finding: Radiofrequency devices had the highest number of adverse-event reports (270), followed by diode lasers (252) and intense pulsed light devices (158).
Data source: A study of 1,212 medical device reports for laser or light devices in the FDA’s MAUDE database from 1991 through 2013.
Disclosures: Dr. Tremaine reported having no disclosures.
Laser therapy improved severe hyperhidrosis
PHOENIX – Laser treatment of severe hyperhidrosis significantly reduced underarm sweating after 6 months in two separate but similar studies of 20 and 13 patients.
Patients with scores of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS) underwent a single treatment to acutely damage eccrine glands using a 1,440-nm Nd:YAG laser with a new 800-mcm side-firing fiber designed to deliver targeted energy. Patients received tumescent anesthesia in each axilla.
Sixteen of 20 patients in one study (78%) reported at least a 2-point improvement in HDSS scores at a 6-month follow-up visit, and 17 (83%) reported at least a 1-point improvement at 1 year, compared with baseline, Dr. Bruce Katz and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Average HDSS scores were 3.6 before treatment, 2.3 at 3 months, 1.7 at 6 months, and 2.2 at 1 year, said Dr. Katz, a clinical professor of dermatology at Mount Sinai Hospital, New York.
The side-firing fiber inserted through a 150-mm handpiece and set at 10-15 W delivered 1,200-1,500 J to each of four 5 cm2 × 5 cm2 areas in each armpit. Both eccrine and apocrine glands were reduced based on post-treatment histological studies. Side effects included edema, bruising, and numbness, but these conditions resolved in 1-2 weeks.
Before the study, 13 patients (65%) had an HDSS score of 4. Five patients had tried treatment with botulinum toxin type A before the study and found it effective, with results lasting an average of 6 months, but they had discontinued that therapy because of the high cost, Dr. Katz said.
In a second study of 13 patients, HDSS scores improved by a mean of 1.3 at the 6-month follow-up visit, Dr. Alina Fratila and her associates reported in a separate presentation at the meeting.
Gravimetric measurements (in milligrams per minute) showed a mean 78% reduction in sweating at 6 months, said Dr. Fratila of the Fountain of Youth Clinic in Bonn, Germany.
Physicians rated the improvement in sweat as 71%, and patients rated it as 55%. The laser in this study was set at 7.5 W, delivering an average of 6,000 J per axilla (or 1,500 J per 5 cm2 × 5 cm2 quadrant).
Ten patients had tried a prescription antiperspirant prior to participating in the study, but they stopped because they found it either irritating or ineffective. Four patients had tried botulinum toxin therapy but stopped because of the cost, Dr. Fratila said.
The laser treatment has a low risk of side effects and causes essentially no downtime, Dr. Fratila said. She added that she plans to follow the patients to assess results after 1 and 2 years.
An estimated 3% of the U.S. population has primary focal hyperhidrosis, comprising nearly 8 million people, Dr. Katz said.
Other treatment options for primary focal hyperhidrosis include topical over-the-counter antiperspirants, aluminum chloride 10%-35% topical antiperspirant, intradermal injections of botulinum toxin type A, and surgical resection of local sweat glands.
Dr. Katz reported financial associations with Cynosure, which makes the laser systems used in his study, and with Allergan, Alma, and other companies. Dr. Fratila reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Laser treatment of severe hyperhidrosis significantly reduced underarm sweating after 6 months in two separate but similar studies of 20 and 13 patients.
Patients with scores of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS) underwent a single treatment to acutely damage eccrine glands using a 1,440-nm Nd:YAG laser with a new 800-mcm side-firing fiber designed to deliver targeted energy. Patients received tumescent anesthesia in each axilla.
Sixteen of 20 patients in one study (78%) reported at least a 2-point improvement in HDSS scores at a 6-month follow-up visit, and 17 (83%) reported at least a 1-point improvement at 1 year, compared with baseline, Dr. Bruce Katz and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Average HDSS scores were 3.6 before treatment, 2.3 at 3 months, 1.7 at 6 months, and 2.2 at 1 year, said Dr. Katz, a clinical professor of dermatology at Mount Sinai Hospital, New York.
The side-firing fiber inserted through a 150-mm handpiece and set at 10-15 W delivered 1,200-1,500 J to each of four 5 cm2 × 5 cm2 areas in each armpit. Both eccrine and apocrine glands were reduced based on post-treatment histological studies. Side effects included edema, bruising, and numbness, but these conditions resolved in 1-2 weeks.
Before the study, 13 patients (65%) had an HDSS score of 4. Five patients had tried treatment with botulinum toxin type A before the study and found it effective, with results lasting an average of 6 months, but they had discontinued that therapy because of the high cost, Dr. Katz said.
In a second study of 13 patients, HDSS scores improved by a mean of 1.3 at the 6-month follow-up visit, Dr. Alina Fratila and her associates reported in a separate presentation at the meeting.
Gravimetric measurements (in milligrams per minute) showed a mean 78% reduction in sweating at 6 months, said Dr. Fratila of the Fountain of Youth Clinic in Bonn, Germany.
Physicians rated the improvement in sweat as 71%, and patients rated it as 55%. The laser in this study was set at 7.5 W, delivering an average of 6,000 J per axilla (or 1,500 J per 5 cm2 × 5 cm2 quadrant).
Ten patients had tried a prescription antiperspirant prior to participating in the study, but they stopped because they found it either irritating or ineffective. Four patients had tried botulinum toxin therapy but stopped because of the cost, Dr. Fratila said.
The laser treatment has a low risk of side effects and causes essentially no downtime, Dr. Fratila said. She added that she plans to follow the patients to assess results after 1 and 2 years.
An estimated 3% of the U.S. population has primary focal hyperhidrosis, comprising nearly 8 million people, Dr. Katz said.
Other treatment options for primary focal hyperhidrosis include topical over-the-counter antiperspirants, aluminum chloride 10%-35% topical antiperspirant, intradermal injections of botulinum toxin type A, and surgical resection of local sweat glands.
Dr. Katz reported financial associations with Cynosure, which makes the laser systems used in his study, and with Allergan, Alma, and other companies. Dr. Fratila reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Laser treatment of severe hyperhidrosis significantly reduced underarm sweating after 6 months in two separate but similar studies of 20 and 13 patients.
Patients with scores of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS) underwent a single treatment to acutely damage eccrine glands using a 1,440-nm Nd:YAG laser with a new 800-mcm side-firing fiber designed to deliver targeted energy. Patients received tumescent anesthesia in each axilla.
Sixteen of 20 patients in one study (78%) reported at least a 2-point improvement in HDSS scores at a 6-month follow-up visit, and 17 (83%) reported at least a 1-point improvement at 1 year, compared with baseline, Dr. Bruce Katz and his associates reported at the annual meeting of the American Society for Laser Medicine and Surgery.
Average HDSS scores were 3.6 before treatment, 2.3 at 3 months, 1.7 at 6 months, and 2.2 at 1 year, said Dr. Katz, a clinical professor of dermatology at Mount Sinai Hospital, New York.
The side-firing fiber inserted through a 150-mm handpiece and set at 10-15 W delivered 1,200-1,500 J to each of four 5 cm2 × 5 cm2 areas in each armpit. Both eccrine and apocrine glands were reduced based on post-treatment histological studies. Side effects included edema, bruising, and numbness, but these conditions resolved in 1-2 weeks.
Before the study, 13 patients (65%) had an HDSS score of 4. Five patients had tried treatment with botulinum toxin type A before the study and found it effective, with results lasting an average of 6 months, but they had discontinued that therapy because of the high cost, Dr. Katz said.
In a second study of 13 patients, HDSS scores improved by a mean of 1.3 at the 6-month follow-up visit, Dr. Alina Fratila and her associates reported in a separate presentation at the meeting.
Gravimetric measurements (in milligrams per minute) showed a mean 78% reduction in sweating at 6 months, said Dr. Fratila of the Fountain of Youth Clinic in Bonn, Germany.
Physicians rated the improvement in sweat as 71%, and patients rated it as 55%. The laser in this study was set at 7.5 W, delivering an average of 6,000 J per axilla (or 1,500 J per 5 cm2 × 5 cm2 quadrant).
Ten patients had tried a prescription antiperspirant prior to participating in the study, but they stopped because they found it either irritating or ineffective. Four patients had tried botulinum toxin therapy but stopped because of the cost, Dr. Fratila said.
The laser treatment has a low risk of side effects and causes essentially no downtime, Dr. Fratila said. She added that she plans to follow the patients to assess results after 1 and 2 years.
An estimated 3% of the U.S. population has primary focal hyperhidrosis, comprising nearly 8 million people, Dr. Katz said.
Other treatment options for primary focal hyperhidrosis include topical over-the-counter antiperspirants, aluminum chloride 10%-35% topical antiperspirant, intradermal injections of botulinum toxin type A, and surgical resection of local sweat glands.
Dr. Katz reported financial associations with Cynosure, which makes the laser systems used in his study, and with Allergan, Alma, and other companies. Dr. Fratila reported having no disclosures.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: Patients with severe hyperhidrosis who underwent laser treatment had minimal, short-term side effects and essentially no downtime.
Major finding: HDSS scores of underarm sweating 6 months after laser treatment improved by at least 2 points in one study and by a mean of 1.3 points in another study.
Data source: Separate single-center, uncontrolled trials of 20 and 13 patients, respectively, with severe primary focal hyperhidrosis.
Disclosures: Dr. Katz reported financial associations with Cynosure, which makes the laser systems used in the study, and with Allergan, Alma, and other companies. Dr. Fratila reported having no disclosures.
VIDEO: Laser's novel effect improves restrictive burn scars
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT LASER 2014
CO2 laser works best for hypertrophic scars
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
AT LASER 2014
Major finding: The fractional CO2 laser significantly improved scar thickness, sensation, erythema, and pigment, compared with untreated scars. The KTP laser improved sensation and the erbium glass laser improved thickness in treated scars, compared with control scars.
Data source: An analysis of data from three prospective controlled studies of laser treatments in 66 patients with 141 scars.
Disclosures: Dr. Blome-Eberwein reported having no financial disclosures.