User login
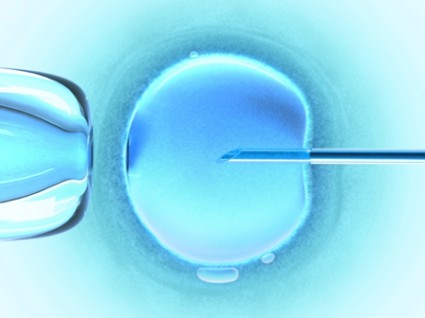
University of California, Los Angeles (UCLA): Annual In Vitro Fertilization and Embryo Transfer
Innovative pricing tried to draw fertility patients
SANTA BARBARA, CALIF. – Some fertility specialists are pairing guarantees with pricing to entice patients to their assisted reproductive technology services.
Dr. Bill Yee offers a step-by-step approach in his fees. A patient who comes in, gets monitored, and is taken to egg retrieval pays a minimum of $1,000. If no egg gets retrieved, the fee stops there. If an egg is retrieved for attempted fertilization, however, the fee increases to $2,000, where it stays if fertilization is unsuccessful. Successful fertilization that produces an embryo increases the fee to $3,000 total. If the embryo doesn’t divide on day 3 or doesn’t look to be of suitable quality for cryopreservation, the fee remains at $3,000. If the embryo does become suitable for freezing and transfer, the fee is $5,000.
"It’s very, very simple," he said at the UCLA annual in vitro fertilization and embryo transfer update 2013. While this fee structure may seem controversial, "we find that patients love this," said Dr. Yee, a reproductive endocrinology and infertility specialist in group practice in Westminster, Calif. "This certainly is an alternative, especially for your poor responders."
Keeping costs down is an important strategy for gaining patients in the competitive field of fertility treatments. "It’s very expensive to do IVF in Southern California," said Dr. Yee.
Another innovative pricing schedule at a fertility center in Davis, Calif., drew attention in a November 2012 article in the Los Angeles Times, which reported "an ethics debate over embryos on the cheap." Dr. Richard J. Paulson, who gave a separate presentation at the meeting, said that he contacted the physicians at that clinic, which uses donor eggs and donor sperm to create a batch of embryos that get divided up among several patients for attempted pregnancies.
While one horrified critic called this the "commodification of children" in the news article, Dr. Paulson noted that it sharply cuts costs. The Davis center told him that they now charge $12,500 per patient for up to three transfers of one or two blastocysts; the center matches two to five recipients per donor cycle. If a woman is not pregnant after three transfers, she can choose either to get her $12,500 back or to roll the money into another three transfers. If there’s no successful pregnancy after that, there’s no refund.
"They say they’ve had about 200 patients and 90-plus are pregnant," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
"I’m not advocating it, but it’s an interesting way of putting your money where your mouth is," he said. "If we’re so confident that sperm really doesn’t matter, and that it’s all about the egg, and that egg freezing doesn’t matter because cryopreserved or vitrified oocytes have the same efficiency as fresh, then why wouldn’t we use this same kind of model and allow patients to be able to have this kind of money-back guarantee?"
Dr. Paulson said he is bothered by modern egg donation practices that match one recipient to one egg donor with 20 embryos, 19 of which stay in a cryopreservation tank for the next 15-20 years if the recipient gets pregnant on the first elective single-embryo transfer.
"I think egg freezing would be a good way of getting around that and convincing patients that it’s worth going this way," he said. "I think if we offer them some sort of money back, it might be helpful."
At the same time, he’s not thrilled with that idea. "I don’t like money-back [strategies]. I’m a very traditional guy and I like providing a service, and they pay you," he said, adding with a smile, "I’m very confused."
Dr. Yee reported having no relevant financial disclosures. Dr. Paulson has been a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
On Twitter @sherryboschert
SANTA BARBARA, CALIF. – Some fertility specialists are pairing guarantees with pricing to entice patients to their assisted reproductive technology services.
Dr. Bill Yee offers a step-by-step approach in his fees. A patient who comes in, gets monitored, and is taken to egg retrieval pays a minimum of $1,000. If no egg gets retrieved, the fee stops there. If an egg is retrieved for attempted fertilization, however, the fee increases to $2,000, where it stays if fertilization is unsuccessful. Successful fertilization that produces an embryo increases the fee to $3,000 total. If the embryo doesn’t divide on day 3 or doesn’t look to be of suitable quality for cryopreservation, the fee remains at $3,000. If the embryo does become suitable for freezing and transfer, the fee is $5,000.
"It’s very, very simple," he said at the UCLA annual in vitro fertilization and embryo transfer update 2013. While this fee structure may seem controversial, "we find that patients love this," said Dr. Yee, a reproductive endocrinology and infertility specialist in group practice in Westminster, Calif. "This certainly is an alternative, especially for your poor responders."
Keeping costs down is an important strategy for gaining patients in the competitive field of fertility treatments. "It’s very expensive to do IVF in Southern California," said Dr. Yee.
Another innovative pricing schedule at a fertility center in Davis, Calif., drew attention in a November 2012 article in the Los Angeles Times, which reported "an ethics debate over embryos on the cheap." Dr. Richard J. Paulson, who gave a separate presentation at the meeting, said that he contacted the physicians at that clinic, which uses donor eggs and donor sperm to create a batch of embryos that get divided up among several patients for attempted pregnancies.
While one horrified critic called this the "commodification of children" in the news article, Dr. Paulson noted that it sharply cuts costs. The Davis center told him that they now charge $12,500 per patient for up to three transfers of one or two blastocysts; the center matches two to five recipients per donor cycle. If a woman is not pregnant after three transfers, she can choose either to get her $12,500 back or to roll the money into another three transfers. If there’s no successful pregnancy after that, there’s no refund.
"They say they’ve had about 200 patients and 90-plus are pregnant," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
"I’m not advocating it, but it’s an interesting way of putting your money where your mouth is," he said. "If we’re so confident that sperm really doesn’t matter, and that it’s all about the egg, and that egg freezing doesn’t matter because cryopreserved or vitrified oocytes have the same efficiency as fresh, then why wouldn’t we use this same kind of model and allow patients to be able to have this kind of money-back guarantee?"
Dr. Paulson said he is bothered by modern egg donation practices that match one recipient to one egg donor with 20 embryos, 19 of which stay in a cryopreservation tank for the next 15-20 years if the recipient gets pregnant on the first elective single-embryo transfer.
"I think egg freezing would be a good way of getting around that and convincing patients that it’s worth going this way," he said. "I think if we offer them some sort of money back, it might be helpful."
At the same time, he’s not thrilled with that idea. "I don’t like money-back [strategies]. I’m a very traditional guy and I like providing a service, and they pay you," he said, adding with a smile, "I’m very confused."
Dr. Yee reported having no relevant financial disclosures. Dr. Paulson has been a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
On Twitter @sherryboschert
SANTA BARBARA, CALIF. – Some fertility specialists are pairing guarantees with pricing to entice patients to their assisted reproductive technology services.
Dr. Bill Yee offers a step-by-step approach in his fees. A patient who comes in, gets monitored, and is taken to egg retrieval pays a minimum of $1,000. If no egg gets retrieved, the fee stops there. If an egg is retrieved for attempted fertilization, however, the fee increases to $2,000, where it stays if fertilization is unsuccessful. Successful fertilization that produces an embryo increases the fee to $3,000 total. If the embryo doesn’t divide on day 3 or doesn’t look to be of suitable quality for cryopreservation, the fee remains at $3,000. If the embryo does become suitable for freezing and transfer, the fee is $5,000.
"It’s very, very simple," he said at the UCLA annual in vitro fertilization and embryo transfer update 2013. While this fee structure may seem controversial, "we find that patients love this," said Dr. Yee, a reproductive endocrinology and infertility specialist in group practice in Westminster, Calif. "This certainly is an alternative, especially for your poor responders."
Keeping costs down is an important strategy for gaining patients in the competitive field of fertility treatments. "It’s very expensive to do IVF in Southern California," said Dr. Yee.
Another innovative pricing schedule at a fertility center in Davis, Calif., drew attention in a November 2012 article in the Los Angeles Times, which reported "an ethics debate over embryos on the cheap." Dr. Richard J. Paulson, who gave a separate presentation at the meeting, said that he contacted the physicians at that clinic, which uses donor eggs and donor sperm to create a batch of embryos that get divided up among several patients for attempted pregnancies.
While one horrified critic called this the "commodification of children" in the news article, Dr. Paulson noted that it sharply cuts costs. The Davis center told him that they now charge $12,500 per patient for up to three transfers of one or two blastocysts; the center matches two to five recipients per donor cycle. If a woman is not pregnant after three transfers, she can choose either to get her $12,500 back or to roll the money into another three transfers. If there’s no successful pregnancy after that, there’s no refund.
"They say they’ve had about 200 patients and 90-plus are pregnant," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
"I’m not advocating it, but it’s an interesting way of putting your money where your mouth is," he said. "If we’re so confident that sperm really doesn’t matter, and that it’s all about the egg, and that egg freezing doesn’t matter because cryopreserved or vitrified oocytes have the same efficiency as fresh, then why wouldn’t we use this same kind of model and allow patients to be able to have this kind of money-back guarantee?"
Dr. Paulson said he is bothered by modern egg donation practices that match one recipient to one egg donor with 20 embryos, 19 of which stay in a cryopreservation tank for the next 15-20 years if the recipient gets pregnant on the first elective single-embryo transfer.
"I think egg freezing would be a good way of getting around that and convincing patients that it’s worth going this way," he said. "I think if we offer them some sort of money back, it might be helpful."
At the same time, he’s not thrilled with that idea. "I don’t like money-back [strategies]. I’m a very traditional guy and I like providing a service, and they pay you," he said, adding with a smile, "I’m very confused."
Dr. Yee reported having no relevant financial disclosures. Dr. Paulson has been a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON IVF AND EMBRYO TRANSFER
Acupuncture does not significantly increase pregnancy rates in IVF
SANTA BARBARA, CALIF. – Acupuncture does not significantly increase pregnancy rates in women undergoing IVF, reanalyses of a prior meta-analysis of 24 studies suggested.
Although the original meta-analysis reported a significant 20% increase in the pregnancy rate with acupuncture, a more rigorous reanalysis that excluded eight lesser-quality studies found no statistically significant difference in IVF pregnancy rates between women who did or did not have acupuncture, Dr. David R. Meldrum said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
When data were looked at only from six studies that used the Streitberger mock acupuncture technique (a widely accepted control technique in acupuncture studies), the odds ratio for clinical pregnancy in the acupuncture group was 0.89 with the confidence interval crossing 1, "indicating lack of a true effect of acupuncture," he said.
When Dr. Meldrum and his associates compared separate reanalyses of studies that did or did not use Streitberger mock acupuncture, the confidence interval for results in the placebo group straddled 1 in the studies using the Streitberger technique but did not cross 1 in non-Streitberger studies.
"Based on this, we think that at the present time acupuncture appears to have a placebo effect. There are not enough data to say whether it has a specific effect," said Dr. Meldrum, a reproductive endocrinology and infertility specialist in group practice in Redondo Beach, Calif.
Studies since 1996 have reported varying results from acupuncture as part of IVF programs. Although the 2012 meta-analysis of 24 studies reported a significantly higher pregnancy rate with acupuncture compared with placebo or no acupuncture, the birth rate did not differ significantly between groups (Fertil. Steril. 2012;97:599-611).
That report "stimulated me to look at it in more detail," said Dr. Meldrum.
The authors of the meta-analysis also conducted a secondary analysis of the data minus studies that used a widely accepted type of sham control, reasoning that the sham procedure created pressure that might be therapeutic. With this more limited data set, the birth rate was significantly higher with acupuncture than without it, they reported.
That didn’t seem right to Dr. Meldrum, so he and three colleagues with epidemiologic training conducted their own reanalysis of the meta-analysis, excluding at least 8 of the 24 studies in the original data set that they felt "didn’t belong in it," he said.
One of the excluded studies was not randomized. Two studies compared acupuncture to a combination of anesthesia drugs that "we know could have a negative effect," he said. Another excluded study compared acupuncture to general anesthesia. One study compared the control to acupuncture plus "special Chinese medical drug seeds" instead of acupuncture alone. Three excluded studies compared data from multiple arms in the trials rather than just acupuncture versus control.
Without those studies, a redone meta-analysis of 16 studies yielded a statistically nonsignificant odds ratio for pregnancy of 1.14 for acupuncture (Fertil. Steril. 2013;99:1821-4).
He and his associates also reanalyzed data from just the three studies that reported birth rates, and found an odds ratio for birth of 0.74 in the acupuncture groups versus controls (confidence interval, 0.58-0.95), indicating a reduced chance of IVF success, he added. One of these studies "recorded rotating, lifting, and thrusting the needle. I think a lot of our patients might find that stressful," he said.
"We’re not saying that patients should be dissuaded from having acupuncture, because it is widely used, but I think we have to be frank that it’s questionable whether there’s a specific benefit," Dr. Meldrum said.
Most of the acupuncture studies were carried out in IVF centers, so if patients choose to receive acupuncture, it may be best for them to receive it at the IVF center if possible so there is minimal disruption. One study that found a reduced pregnancy rate after acupuncture had subjects who had never undergone acupuncture get the acupuncture at a separate location from the IVF clinic, possibly adding stress, he noted.
It would be helpful to have patients who choose acupuncture follow the techniques used in the studies that reported improved IVF success with acupuncture, but that may be difficult because the acupuncture techniques varied so widely. "I would think that if acupuncture had a specific effect, the placements of the needle would be consistent. They were widely variable in different studies. So, I am somewhat skeptical as to whether acupuncture, even with much larger experience, has a specific effect."
Dr. Meldrum is president of the Sexuality Education Network, which operates the websites erectile-function.com and lifechoicesandfertility.com. He reported having no other relevant financial disclosures.
On Twitter @sherryboschert
SANTA BARBARA, CALIF. – Acupuncture does not significantly increase pregnancy rates in women undergoing IVF, reanalyses of a prior meta-analysis of 24 studies suggested.
Although the original meta-analysis reported a significant 20% increase in the pregnancy rate with acupuncture, a more rigorous reanalysis that excluded eight lesser-quality studies found no statistically significant difference in IVF pregnancy rates between women who did or did not have acupuncture, Dr. David R. Meldrum said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
When data were looked at only from six studies that used the Streitberger mock acupuncture technique (a widely accepted control technique in acupuncture studies), the odds ratio for clinical pregnancy in the acupuncture group was 0.89 with the confidence interval crossing 1, "indicating lack of a true effect of acupuncture," he said.
When Dr. Meldrum and his associates compared separate reanalyses of studies that did or did not use Streitberger mock acupuncture, the confidence interval for results in the placebo group straddled 1 in the studies using the Streitberger technique but did not cross 1 in non-Streitberger studies.
"Based on this, we think that at the present time acupuncture appears to have a placebo effect. There are not enough data to say whether it has a specific effect," said Dr. Meldrum, a reproductive endocrinology and infertility specialist in group practice in Redondo Beach, Calif.
Studies since 1996 have reported varying results from acupuncture as part of IVF programs. Although the 2012 meta-analysis of 24 studies reported a significantly higher pregnancy rate with acupuncture compared with placebo or no acupuncture, the birth rate did not differ significantly between groups (Fertil. Steril. 2012;97:599-611).
That report "stimulated me to look at it in more detail," said Dr. Meldrum.
The authors of the meta-analysis also conducted a secondary analysis of the data minus studies that used a widely accepted type of sham control, reasoning that the sham procedure created pressure that might be therapeutic. With this more limited data set, the birth rate was significantly higher with acupuncture than without it, they reported.
That didn’t seem right to Dr. Meldrum, so he and three colleagues with epidemiologic training conducted their own reanalysis of the meta-analysis, excluding at least 8 of the 24 studies in the original data set that they felt "didn’t belong in it," he said.
One of the excluded studies was not randomized. Two studies compared acupuncture to a combination of anesthesia drugs that "we know could have a negative effect," he said. Another excluded study compared acupuncture to general anesthesia. One study compared the control to acupuncture plus "special Chinese medical drug seeds" instead of acupuncture alone. Three excluded studies compared data from multiple arms in the trials rather than just acupuncture versus control.
Without those studies, a redone meta-analysis of 16 studies yielded a statistically nonsignificant odds ratio for pregnancy of 1.14 for acupuncture (Fertil. Steril. 2013;99:1821-4).
He and his associates also reanalyzed data from just the three studies that reported birth rates, and found an odds ratio for birth of 0.74 in the acupuncture groups versus controls (confidence interval, 0.58-0.95), indicating a reduced chance of IVF success, he added. One of these studies "recorded rotating, lifting, and thrusting the needle. I think a lot of our patients might find that stressful," he said.
"We’re not saying that patients should be dissuaded from having acupuncture, because it is widely used, but I think we have to be frank that it’s questionable whether there’s a specific benefit," Dr. Meldrum said.
Most of the acupuncture studies were carried out in IVF centers, so if patients choose to receive acupuncture, it may be best for them to receive it at the IVF center if possible so there is minimal disruption. One study that found a reduced pregnancy rate after acupuncture had subjects who had never undergone acupuncture get the acupuncture at a separate location from the IVF clinic, possibly adding stress, he noted.
It would be helpful to have patients who choose acupuncture follow the techniques used in the studies that reported improved IVF success with acupuncture, but that may be difficult because the acupuncture techniques varied so widely. "I would think that if acupuncture had a specific effect, the placements of the needle would be consistent. They were widely variable in different studies. So, I am somewhat skeptical as to whether acupuncture, even with much larger experience, has a specific effect."
Dr. Meldrum is president of the Sexuality Education Network, which operates the websites erectile-function.com and lifechoicesandfertility.com. He reported having no other relevant financial disclosures.
On Twitter @sherryboschert
SANTA BARBARA, CALIF. – Acupuncture does not significantly increase pregnancy rates in women undergoing IVF, reanalyses of a prior meta-analysis of 24 studies suggested.
Although the original meta-analysis reported a significant 20% increase in the pregnancy rate with acupuncture, a more rigorous reanalysis that excluded eight lesser-quality studies found no statistically significant difference in IVF pregnancy rates between women who did or did not have acupuncture, Dr. David R. Meldrum said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
When data were looked at only from six studies that used the Streitberger mock acupuncture technique (a widely accepted control technique in acupuncture studies), the odds ratio for clinical pregnancy in the acupuncture group was 0.89 with the confidence interval crossing 1, "indicating lack of a true effect of acupuncture," he said.
When Dr. Meldrum and his associates compared separate reanalyses of studies that did or did not use Streitberger mock acupuncture, the confidence interval for results in the placebo group straddled 1 in the studies using the Streitberger technique but did not cross 1 in non-Streitberger studies.
"Based on this, we think that at the present time acupuncture appears to have a placebo effect. There are not enough data to say whether it has a specific effect," said Dr. Meldrum, a reproductive endocrinology and infertility specialist in group practice in Redondo Beach, Calif.
Studies since 1996 have reported varying results from acupuncture as part of IVF programs. Although the 2012 meta-analysis of 24 studies reported a significantly higher pregnancy rate with acupuncture compared with placebo or no acupuncture, the birth rate did not differ significantly between groups (Fertil. Steril. 2012;97:599-611).
That report "stimulated me to look at it in more detail," said Dr. Meldrum.
The authors of the meta-analysis also conducted a secondary analysis of the data minus studies that used a widely accepted type of sham control, reasoning that the sham procedure created pressure that might be therapeutic. With this more limited data set, the birth rate was significantly higher with acupuncture than without it, they reported.
That didn’t seem right to Dr. Meldrum, so he and three colleagues with epidemiologic training conducted their own reanalysis of the meta-analysis, excluding at least 8 of the 24 studies in the original data set that they felt "didn’t belong in it," he said.
One of the excluded studies was not randomized. Two studies compared acupuncture to a combination of anesthesia drugs that "we know could have a negative effect," he said. Another excluded study compared acupuncture to general anesthesia. One study compared the control to acupuncture plus "special Chinese medical drug seeds" instead of acupuncture alone. Three excluded studies compared data from multiple arms in the trials rather than just acupuncture versus control.
Without those studies, a redone meta-analysis of 16 studies yielded a statistically nonsignificant odds ratio for pregnancy of 1.14 for acupuncture (Fertil. Steril. 2013;99:1821-4).
He and his associates also reanalyzed data from just the three studies that reported birth rates, and found an odds ratio for birth of 0.74 in the acupuncture groups versus controls (confidence interval, 0.58-0.95), indicating a reduced chance of IVF success, he added. One of these studies "recorded rotating, lifting, and thrusting the needle. I think a lot of our patients might find that stressful," he said.
"We’re not saying that patients should be dissuaded from having acupuncture, because it is widely used, but I think we have to be frank that it’s questionable whether there’s a specific benefit," Dr. Meldrum said.
Most of the acupuncture studies were carried out in IVF centers, so if patients choose to receive acupuncture, it may be best for them to receive it at the IVF center if possible so there is minimal disruption. One study that found a reduced pregnancy rate after acupuncture had subjects who had never undergone acupuncture get the acupuncture at a separate location from the IVF clinic, possibly adding stress, he noted.
It would be helpful to have patients who choose acupuncture follow the techniques used in the studies that reported improved IVF success with acupuncture, but that may be difficult because the acupuncture techniques varied so widely. "I would think that if acupuncture had a specific effect, the placements of the needle would be consistent. They were widely variable in different studies. So, I am somewhat skeptical as to whether acupuncture, even with much larger experience, has a specific effect."
Dr. Meldrum is president of the Sexuality Education Network, which operates the websites erectile-function.com and lifechoicesandfertility.com. He reported having no other relevant financial disclosures.
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Major finding: The odds ratio for clinical pregnancy was 1.14 in those who got acupuncture, compared with control groups.
Data source: A more rigorous reanalysis of a prior meta-analysis, excluding data from 8 of the original 24 studies.
Disclosures: Dr. Meldrum is president of the Sexuality Education Network, which operates the websites erectile-function.com and lifechoicesandfertility.com. He reported having no other relevant financial disclosures.
IVF aneuploidies may be fewer with CoQ10
SAN FRANCISCO – Two months of pre-IVF supplementation with coenzyme Q10 was associated with a 41% rate of aneuploidies in 9 oocytes, compared with aneuploidies in 51% of 13 oocytes from women randomized to placebo, a small prospective study found.
"This difference didn’t reach significance because of the small numbers, but at least it’s trending in the right direction," Dr. Robert F. Casper said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
The study took 2-3 years to enroll and randomize 39 women aged 38 years or older who were undergoing IVF at his institution, a lengthy process because of patient reluctance to enter the study.
He said the investigators didn’t really know how long to pretreat with coenzyme Q10 (CoQ10) in hopes of rejuvenating the mitochondria of aging oocytes, so they settled on 2 months because they didn’t think these older women would agree to a longer time frame. Even with that compromise, most eligible patients still were unwilling to risk being randomized to placebo and so refused enrollment, said Dr. Casper, professor of ob.gyn. and of medicine (division of endocrinology) at the University of Toronto and the Camille Dan Family research chair in translational cell biology at the Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto.
The encouraging trend in reduced risk of aneuploidy suggests that a much larger prospective study should be conducted, perhaps with younger IVF patients who "wouldn’t be so stressed about being randomized to placebo for a few months," he said.
Patients took six capsules per day that gave them either placebo or 600 mg/day of CoQ10 in the form of ubiquinone.
The study originally randomized 39 women, 27 of whom completed 2 months of pretreatment. Twenty-two oocytes were available for aneuploidy analysis after IVF and embryo transfer: 9 in the CoQ10 group and 13 in the placebo group.
Although the average estradiol level on the day of human chorionic gonadotropin (HCG) was higher in the CoQ10 group and the average progesterone level was lower on the day of HCG than in the placebo group, these differences did not reach statistical significance. The groups also did not differ significantly in average age, follicle-stimulating hormone level on cycle day 3, the day of HCG, or total international units of Menopur (menotropins) used.
No major side effects were seen. Most women in the CoQ10 group reported feeling more energetic, Dr. Casper said. Some who complained of insomnia were instructed to take all six capsules in the morning.
The study was inspired by two previous studies in mice by the same investigators. One found that CoQ10 supplementation in old mice improved ovarian response to stimulation, increased the number of cumulus cells and oocyte mitochondrial function, restored normal nuclear spindles, and delayed ovarian follicle loss due to aging. The second study showed that disrupting CoQ10 production in mice oocytes mimicked reproductive aging. Disrupting CoQ10 production accelerated oocyte loss and premature ovarian failure, impaired mitochondrial function with reduced energy production, and increased chromosomal abnormalities, all of which were bypassed with CoQ10 supplementation.
Dr. Casper has been a consultant for Fertility Nutraceuticals, which is making a brand of CoQ10, and he disclosed financial relationships with multiple other companies unrelated to this topic.
On Twitter @sherryboschert
SAN FRANCISCO – Two months of pre-IVF supplementation with coenzyme Q10 was associated with a 41% rate of aneuploidies in 9 oocytes, compared with aneuploidies in 51% of 13 oocytes from women randomized to placebo, a small prospective study found.
"This difference didn’t reach significance because of the small numbers, but at least it’s trending in the right direction," Dr. Robert F. Casper said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
The study took 2-3 years to enroll and randomize 39 women aged 38 years or older who were undergoing IVF at his institution, a lengthy process because of patient reluctance to enter the study.
He said the investigators didn’t really know how long to pretreat with coenzyme Q10 (CoQ10) in hopes of rejuvenating the mitochondria of aging oocytes, so they settled on 2 months because they didn’t think these older women would agree to a longer time frame. Even with that compromise, most eligible patients still were unwilling to risk being randomized to placebo and so refused enrollment, said Dr. Casper, professor of ob.gyn. and of medicine (division of endocrinology) at the University of Toronto and the Camille Dan Family research chair in translational cell biology at the Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto.
The encouraging trend in reduced risk of aneuploidy suggests that a much larger prospective study should be conducted, perhaps with younger IVF patients who "wouldn’t be so stressed about being randomized to placebo for a few months," he said.
Patients took six capsules per day that gave them either placebo or 600 mg/day of CoQ10 in the form of ubiquinone.
The study originally randomized 39 women, 27 of whom completed 2 months of pretreatment. Twenty-two oocytes were available for aneuploidy analysis after IVF and embryo transfer: 9 in the CoQ10 group and 13 in the placebo group.
Although the average estradiol level on the day of human chorionic gonadotropin (HCG) was higher in the CoQ10 group and the average progesterone level was lower on the day of HCG than in the placebo group, these differences did not reach statistical significance. The groups also did not differ significantly in average age, follicle-stimulating hormone level on cycle day 3, the day of HCG, or total international units of Menopur (menotropins) used.
No major side effects were seen. Most women in the CoQ10 group reported feeling more energetic, Dr. Casper said. Some who complained of insomnia were instructed to take all six capsules in the morning.
The study was inspired by two previous studies in mice by the same investigators. One found that CoQ10 supplementation in old mice improved ovarian response to stimulation, increased the number of cumulus cells and oocyte mitochondrial function, restored normal nuclear spindles, and delayed ovarian follicle loss due to aging. The second study showed that disrupting CoQ10 production in mice oocytes mimicked reproductive aging. Disrupting CoQ10 production accelerated oocyte loss and premature ovarian failure, impaired mitochondrial function with reduced energy production, and increased chromosomal abnormalities, all of which were bypassed with CoQ10 supplementation.
Dr. Casper has been a consultant for Fertility Nutraceuticals, which is making a brand of CoQ10, and he disclosed financial relationships with multiple other companies unrelated to this topic.
On Twitter @sherryboschert
SAN FRANCISCO – Two months of pre-IVF supplementation with coenzyme Q10 was associated with a 41% rate of aneuploidies in 9 oocytes, compared with aneuploidies in 51% of 13 oocytes from women randomized to placebo, a small prospective study found.
"This difference didn’t reach significance because of the small numbers, but at least it’s trending in the right direction," Dr. Robert F. Casper said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
The study took 2-3 years to enroll and randomize 39 women aged 38 years or older who were undergoing IVF at his institution, a lengthy process because of patient reluctance to enter the study.
He said the investigators didn’t really know how long to pretreat with coenzyme Q10 (CoQ10) in hopes of rejuvenating the mitochondria of aging oocytes, so they settled on 2 months because they didn’t think these older women would agree to a longer time frame. Even with that compromise, most eligible patients still were unwilling to risk being randomized to placebo and so refused enrollment, said Dr. Casper, professor of ob.gyn. and of medicine (division of endocrinology) at the University of Toronto and the Camille Dan Family research chair in translational cell biology at the Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto.
The encouraging trend in reduced risk of aneuploidy suggests that a much larger prospective study should be conducted, perhaps with younger IVF patients who "wouldn’t be so stressed about being randomized to placebo for a few months," he said.
Patients took six capsules per day that gave them either placebo or 600 mg/day of CoQ10 in the form of ubiquinone.
The study originally randomized 39 women, 27 of whom completed 2 months of pretreatment. Twenty-two oocytes were available for aneuploidy analysis after IVF and embryo transfer: 9 in the CoQ10 group and 13 in the placebo group.
Although the average estradiol level on the day of human chorionic gonadotropin (HCG) was higher in the CoQ10 group and the average progesterone level was lower on the day of HCG than in the placebo group, these differences did not reach statistical significance. The groups also did not differ significantly in average age, follicle-stimulating hormone level on cycle day 3, the day of HCG, or total international units of Menopur (menotropins) used.
No major side effects were seen. Most women in the CoQ10 group reported feeling more energetic, Dr. Casper said. Some who complained of insomnia were instructed to take all six capsules in the morning.
The study was inspired by two previous studies in mice by the same investigators. One found that CoQ10 supplementation in old mice improved ovarian response to stimulation, increased the number of cumulus cells and oocyte mitochondrial function, restored normal nuclear spindles, and delayed ovarian follicle loss due to aging. The second study showed that disrupting CoQ10 production in mice oocytes mimicked reproductive aging. Disrupting CoQ10 production accelerated oocyte loss and premature ovarian failure, impaired mitochondrial function with reduced energy production, and increased chromosomal abnormalities, all of which were bypassed with CoQ10 supplementation.
Dr. Casper has been a consultant for Fertility Nutraceuticals, which is making a brand of CoQ10, and he disclosed financial relationships with multiple other companies unrelated to this topic.
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Chromosome screening, single-embryo transfer improve outcomes
SANTA BARBARA, CALIF. – Comprehensive chromosomal screening followed by single-embryo transfer resulted in similar delivery rates but significantly fewer multiple gestations, and better maternal and fetal outcomes, compared with conventional transfer of two embryos without screening, a prospective randomized trial of 175 patients found.
As a result, overall costs per delivery are so much lower after comprehensive chromosomal screening and single-embryo transfer (eSET) that these techniques may prove to be the most cost-effective development ever in the field of IVF, Dr. Richard T. Scott Jr. said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
An intent-to-treat analysis by Dr. Scott and his associates found that 61% of 89 patients in the study who received single-euploid blastocysts gave birth, compared with 65% of 86 patients who received two embryos without screening,
All single-euploid blastocysts produced singletons. "We were fortunate enough to have no monozygotic twins, at least not yet," he said. In the double-embryo transfer group (DET), 48% developed multiple gestations, including one set of triplets due to monozygotic twins from one of the embryos.
In general, approximately 99% of long-term sequelae from in vitro fertilization (IVF) relates to multiple gestations, he noted. Comprehensive chromosomal screening plus eSET may be a way to maintain high delivery rates without multiple gestations, said Dr. Scott, professor of obstetrics, gynecology and reproductive services and director of the division reproductive endocrinology at Robert Wood Johnson Medical School, New Brunswick, N.J.
Clinical miscarriages were greatly reduced in the eSET group (12%) compared with the DET group (20%). For each single gestational sac, the difference was even more pronounced, with a 31% clinical miscarriage rate for DET.* Five women in the eSET group required dilation and curettage for clinical miscarriage, none due to aneuploidy, as did eight in the DET group, two with documented aneuploidy. Two nonviable second-trimester twins were delivered in the DET group.
The rate of preterm deliveries in the eSET group (8.9%) was similar to the U.S. average for the general population of pregnancies in women who did not receive IVF services (8%), both of which were significantly lower than the 28% preterm birth rate in the DET group.
Admissions to the neonatal intensive care unit affected 11% in the eSET group and 26% after DET, but the difference did not reach statistical significance. Stays in the neonatal ICU were shorter after eSET than after DET, with the exception of one infant who underwent elective premature delivery because of acute maternal health problems.
"The most compelling data" from the study showed significantly better obstetrical outcomes from comprehensive chromosomal screening and eSET, Dr. Scott said. Mean birth weights were 3,408 g in the eSET group and 2,745 g in the DET group. Rates of low birth weight (less than 2,500 g) were 4% after eSET and 32% after DET. No infants in the eSET group had a very low birth weight (less than 1,500 g), compared with 7% of the DET group, although this difference did not reach statistical significance.
"These are dramatic, dramatic differences" just from reducing double-embryo transfers to single embryos with comprehensive chromosomal screening, Dr. Scott said. "This is not putting three and four [embryos] back; this is not Octomom. We’re talking about two-embryo transfers in the other group."
The study has been submitted to the journal Fertility and Sterility for publication, said Dr. Scott, who is the clinical and scientific director of Reproductive Medicine Associates of New Jersey, Morristown, the clinical center that serves the medical school’s division of reproductive endocrinology.
The findings should be applicable to the general IVF population, not just selected patients, he added. A separate analysis of 210 single-euploid blastocyst transfers and 1,435 untested double-blastocyst transfers at his institution found similar ongoing pregnancy rates (68% each) but a nearly threefold higher risk for preterm delivery after DET (30%) compared with eSET (11%), which was statistically significant.
Dr. Scott and his associates also analyzed actual cost data for comprehensive chromosomal screening and eSET, which averaged less than $40,000 per live-born delivery, compared with more than $70,000 per delivery with conventional IVF treatment, both national and regional averages showed. The costs included sometimes multiple cycles of IVF, the costs of comprehensive chromosomal screening and medications, and the costs for delivery and subsequent hospital stays through 28 days of life, he said.
The savings come from fewer IVF cycles with comprehensive chromosomal screening and eSET, better outcomes, and reduced obstetric and pediatric costs that, combined, "could more than pay for all of their infertility care," Dr. Scott said.
"This is not only cost effective, this is massively cost effective, perhaps the most cost-effective thing we’ve ever done in our field," he said.
Dr. Scott has been an adviser to EMD Serono and Ferring Pharmaceuticals.
On Twitter @sherryboschert
*Correction, 9/11/2013: An earlier version of this story attributed the 31% clinical miscarriage rate per single gestational sac to the wrong treatment group.
SANTA BARBARA, CALIF. – Comprehensive chromosomal screening followed by single-embryo transfer resulted in similar delivery rates but significantly fewer multiple gestations, and better maternal and fetal outcomes, compared with conventional transfer of two embryos without screening, a prospective randomized trial of 175 patients found.
As a result, overall costs per delivery are so much lower after comprehensive chromosomal screening and single-embryo transfer (eSET) that these techniques may prove to be the most cost-effective development ever in the field of IVF, Dr. Richard T. Scott Jr. said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
An intent-to-treat analysis by Dr. Scott and his associates found that 61% of 89 patients in the study who received single-euploid blastocysts gave birth, compared with 65% of 86 patients who received two embryos without screening,
All single-euploid blastocysts produced singletons. "We were fortunate enough to have no monozygotic twins, at least not yet," he said. In the double-embryo transfer group (DET), 48% developed multiple gestations, including one set of triplets due to monozygotic twins from one of the embryos.
In general, approximately 99% of long-term sequelae from in vitro fertilization (IVF) relates to multiple gestations, he noted. Comprehensive chromosomal screening plus eSET may be a way to maintain high delivery rates without multiple gestations, said Dr. Scott, professor of obstetrics, gynecology and reproductive services and director of the division reproductive endocrinology at Robert Wood Johnson Medical School, New Brunswick, N.J.
Clinical miscarriages were greatly reduced in the eSET group (12%) compared with the DET group (20%). For each single gestational sac, the difference was even more pronounced, with a 31% clinical miscarriage rate for DET.* Five women in the eSET group required dilation and curettage for clinical miscarriage, none due to aneuploidy, as did eight in the DET group, two with documented aneuploidy. Two nonviable second-trimester twins were delivered in the DET group.
The rate of preterm deliveries in the eSET group (8.9%) was similar to the U.S. average for the general population of pregnancies in women who did not receive IVF services (8%), both of which were significantly lower than the 28% preterm birth rate in the DET group.
Admissions to the neonatal intensive care unit affected 11% in the eSET group and 26% after DET, but the difference did not reach statistical significance. Stays in the neonatal ICU were shorter after eSET than after DET, with the exception of one infant who underwent elective premature delivery because of acute maternal health problems.
"The most compelling data" from the study showed significantly better obstetrical outcomes from comprehensive chromosomal screening and eSET, Dr. Scott said. Mean birth weights were 3,408 g in the eSET group and 2,745 g in the DET group. Rates of low birth weight (less than 2,500 g) were 4% after eSET and 32% after DET. No infants in the eSET group had a very low birth weight (less than 1,500 g), compared with 7% of the DET group, although this difference did not reach statistical significance.
"These are dramatic, dramatic differences" just from reducing double-embryo transfers to single embryos with comprehensive chromosomal screening, Dr. Scott said. "This is not putting three and four [embryos] back; this is not Octomom. We’re talking about two-embryo transfers in the other group."
The study has been submitted to the journal Fertility and Sterility for publication, said Dr. Scott, who is the clinical and scientific director of Reproductive Medicine Associates of New Jersey, Morristown, the clinical center that serves the medical school’s division of reproductive endocrinology.
The findings should be applicable to the general IVF population, not just selected patients, he added. A separate analysis of 210 single-euploid blastocyst transfers and 1,435 untested double-blastocyst transfers at his institution found similar ongoing pregnancy rates (68% each) but a nearly threefold higher risk for preterm delivery after DET (30%) compared with eSET (11%), which was statistically significant.
Dr. Scott and his associates also analyzed actual cost data for comprehensive chromosomal screening and eSET, which averaged less than $40,000 per live-born delivery, compared with more than $70,000 per delivery with conventional IVF treatment, both national and regional averages showed. The costs included sometimes multiple cycles of IVF, the costs of comprehensive chromosomal screening and medications, and the costs for delivery and subsequent hospital stays through 28 days of life, he said.
The savings come from fewer IVF cycles with comprehensive chromosomal screening and eSET, better outcomes, and reduced obstetric and pediatric costs that, combined, "could more than pay for all of their infertility care," Dr. Scott said.
"This is not only cost effective, this is massively cost effective, perhaps the most cost-effective thing we’ve ever done in our field," he said.
Dr. Scott has been an adviser to EMD Serono and Ferring Pharmaceuticals.
On Twitter @sherryboschert
*Correction, 9/11/2013: An earlier version of this story attributed the 31% clinical miscarriage rate per single gestational sac to the wrong treatment group.
SANTA BARBARA, CALIF. – Comprehensive chromosomal screening followed by single-embryo transfer resulted in similar delivery rates but significantly fewer multiple gestations, and better maternal and fetal outcomes, compared with conventional transfer of two embryos without screening, a prospective randomized trial of 175 patients found.
As a result, overall costs per delivery are so much lower after comprehensive chromosomal screening and single-embryo transfer (eSET) that these techniques may prove to be the most cost-effective development ever in the field of IVF, Dr. Richard T. Scott Jr. said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
An intent-to-treat analysis by Dr. Scott and his associates found that 61% of 89 patients in the study who received single-euploid blastocysts gave birth, compared with 65% of 86 patients who received two embryos without screening,
All single-euploid blastocysts produced singletons. "We were fortunate enough to have no monozygotic twins, at least not yet," he said. In the double-embryo transfer group (DET), 48% developed multiple gestations, including one set of triplets due to monozygotic twins from one of the embryos.
In general, approximately 99% of long-term sequelae from in vitro fertilization (IVF) relates to multiple gestations, he noted. Comprehensive chromosomal screening plus eSET may be a way to maintain high delivery rates without multiple gestations, said Dr. Scott, professor of obstetrics, gynecology and reproductive services and director of the division reproductive endocrinology at Robert Wood Johnson Medical School, New Brunswick, N.J.
Clinical miscarriages were greatly reduced in the eSET group (12%) compared with the DET group (20%). For each single gestational sac, the difference was even more pronounced, with a 31% clinical miscarriage rate for DET.* Five women in the eSET group required dilation and curettage for clinical miscarriage, none due to aneuploidy, as did eight in the DET group, two with documented aneuploidy. Two nonviable second-trimester twins were delivered in the DET group.
The rate of preterm deliveries in the eSET group (8.9%) was similar to the U.S. average for the general population of pregnancies in women who did not receive IVF services (8%), both of which were significantly lower than the 28% preterm birth rate in the DET group.
Admissions to the neonatal intensive care unit affected 11% in the eSET group and 26% after DET, but the difference did not reach statistical significance. Stays in the neonatal ICU were shorter after eSET than after DET, with the exception of one infant who underwent elective premature delivery because of acute maternal health problems.
"The most compelling data" from the study showed significantly better obstetrical outcomes from comprehensive chromosomal screening and eSET, Dr. Scott said. Mean birth weights were 3,408 g in the eSET group and 2,745 g in the DET group. Rates of low birth weight (less than 2,500 g) were 4% after eSET and 32% after DET. No infants in the eSET group had a very low birth weight (less than 1,500 g), compared with 7% of the DET group, although this difference did not reach statistical significance.
"These are dramatic, dramatic differences" just from reducing double-embryo transfers to single embryos with comprehensive chromosomal screening, Dr. Scott said. "This is not putting three and four [embryos] back; this is not Octomom. We’re talking about two-embryo transfers in the other group."
The study has been submitted to the journal Fertility and Sterility for publication, said Dr. Scott, who is the clinical and scientific director of Reproductive Medicine Associates of New Jersey, Morristown, the clinical center that serves the medical school’s division of reproductive endocrinology.
The findings should be applicable to the general IVF population, not just selected patients, he added. A separate analysis of 210 single-euploid blastocyst transfers and 1,435 untested double-blastocyst transfers at his institution found similar ongoing pregnancy rates (68% each) but a nearly threefold higher risk for preterm delivery after DET (30%) compared with eSET (11%), which was statistically significant.
Dr. Scott and his associates also analyzed actual cost data for comprehensive chromosomal screening and eSET, which averaged less than $40,000 per live-born delivery, compared with more than $70,000 per delivery with conventional IVF treatment, both national and regional averages showed. The costs included sometimes multiple cycles of IVF, the costs of comprehensive chromosomal screening and medications, and the costs for delivery and subsequent hospital stays through 28 days of life, he said.
The savings come from fewer IVF cycles with comprehensive chromosomal screening and eSET, better outcomes, and reduced obstetric and pediatric costs that, combined, "could more than pay for all of their infertility care," Dr. Scott said.
"This is not only cost effective, this is massively cost effective, perhaps the most cost-effective thing we’ve ever done in our field," he said.
Dr. Scott has been an adviser to EMD Serono and Ferring Pharmaceuticals.
On Twitter @sherryboschert
*Correction, 9/11/2013: An earlier version of this story attributed the 31% clinical miscarriage rate per single gestational sac to the wrong treatment group.
AT A MEETING ON IVF AND EMBRYO TRANSFER
Major finding: Delivery rates were similar after comprehensive chromosomal screening and single-embryo transfer (61%) or unscreened double-embryo transfer (65%), but the former led to lower rates of multiple gestation (0% vs. 48%, respectively), clinical miscarriage (12% vs. 20%), preterm delivery (9% vs. 28%), and low birth weights (4% vs. 32%).
Data source: A prospective randomized study of deliveries in 175 IVF patients at one institution.
Disclosures: Dr. Scott has been an adviser to EMD Serono and Ferring Pharmaceuticals.
Vitrification efficiently preserves oocytes, embryos
SAN FRANCISCO – Recent data show that vitrification of oocytes or embryos can be as efficient as using slow-frozen or fresh oocytes for in vitro fertilization, and so far it appears to be just as safe.
Oocytes from 22 women aged 32-39 years that were randomly allocated for fresh embryo transfer (204 oocytes) or vitrification and warming before transfer (186 oocytes) produced similar rates of fertilization, good-quality embryos at day 3, and blastocysts at day 5 or 6, Zsolt Peter Nagy, Ph.D., reported at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Eighty percent of vitrified oocytes survived freezing and warming. Fertilization succeeded in 75% of fresh oocytes and 67% of vitrified oocytes, a slight difference that was not statistically significant. On day 3 of in vitro fertilization (IVF), 50% of fresh oocytes and 48% of vitrified oocytes produced good-quality embryos; by days 5 or 6, 53% of fresh embryos and 55% of vitrified embryos had produced blastocysts, results that did not differ significantly between groups, said Dr. Nagy, scientific and laboratory director of Reproductive Biology Associates, Atlanta.
The study at his institution found that 11 of the 186 vitrified oocytes (6%) achieved a live birth (Fertil. Steril. 2013;99:1891-7).
Maternal age did affect outcomes. Among 11 women aged 30-36 years, 56% of oocytes produced a good embryo by day 3 of IVF, compared with 40% of oocytes from 11 women aged 37-39 years, a significant difference.
The findings support previous data by other investigators on 224 oocytes, 120 of which underwent intracytoplasmic sperm injection (ICSI) as fresh oocytes and 124 of which underwent vitrification and warming before ICSI. Fertilization rates were statistically similar (83% and 77%, respectively). Excellent-quality embryos were produced by 52% in the fresh ICSI group and 52% in the vitrification group. The mean maternal age in the study was 36 years (Hum. Reprod. 2010;25:66-73).
The 39 embryo transfers in the vitrification group resulted in 15 clinical pregnancies (38% per cycle and per embryo transfer) and an implantation rate of 20%. Twelve pregnancies beyond 12 weeks’ gestation were ongoing (30% per cycle and 31% per embryo transfer).
Separate data from Molecular Biometrics suggest that vitrification is efficient for freezing donor oocytes in egg banks, Dr. Nagy said. Among 11,553 eggs from 342 donors that were vitrified, 7,063 were warmed and 90% survived warming, leading to a clinical pregnancy rate of 57% and an implantation rate of 43%.
Cryopreserving eggs has advantages over fresh ovum donation programs, which have long waiting lists, require more complex synchronization between the donor and recipient, offer relatively limited choice, and have other logistical disadvantages. "A couple of years ago, most of us were doing slow freezing" for cryopreservation, Dr. Nagy said. "Many of us have changed to vitrification because we have realized that it is more efficient than slow freezing."
Before, two to four embryos were needed to achieve a clinical pregnancy under slow-freeze methods at his institution, but only one or two are needed using vitrification, he said.
Oocyte cryopreservation programs make elective single-embryo transfer (eSET) a viable option, Dr. Nagy said. In 98 recipients of eSET, 52% achieved a clinical pregnancy, compared with clinical pregnancies in 72% of 109 elective double-embryo transfers, but 51% of the double-embryo transfers resulted in multiple pregnancies, a retrospective study of data from his institution showed. Among nonelective double-embryo transfers, 52% achieved clinical pregnancies, with multiple pregnancies in 30% of recipients.
Double vitrification also appears to be efficient for egg/embryo banking – cryopreserving an oocyte, thawing it, and then freezing the resulting embryo to later be warmed and transferred. One study that compared 471 warming cycles of double-vitrified embryos with 2,629 warming cycles of vitrified embryos derived from fresh oocytes found overall embryo survival rates of 97% and 96%, respectively, with a delivery rate per warming cycle of 34% in the double-vitrified group and 31% in the single-vitrified group (Fertil. Steril. 2013;99:1623-30).
At Dr. Nagy’s institution, 99% of 190 warmed double-vitrified embryos have survived, leading to a 53% clinical pregnancy rate, a 39% implantation rate, and 33 live births so far. "It shows that if you do the procedure correctly, you are able to preserve the viability of those embryos," he said.
The rate of congenital anomalies in live births from donor eggs cryopreserved at his institution does not seem to be significantly higher than the rate in live births from fresh donor eggs – 3 congenital anomalies among 91 live births using fresh donor eggs and 5 congenital anomalies in 338 live births using cryopreserved donor eggs. Case reports from 1986 to 2008 suggest there’s no increased incidence of birth defects using vitrification compared with slow-freeze methods for cryopreservation.
In the future, registry data should provide further evidence of the safety of vitrification, he said.
Dr. Nagy reported having financial associations with Molecular Biometrics, Origio, and other companies.
On Twitter @sherryboschert
SAN FRANCISCO – Recent data show that vitrification of oocytes or embryos can be as efficient as using slow-frozen or fresh oocytes for in vitro fertilization, and so far it appears to be just as safe.
Oocytes from 22 women aged 32-39 years that were randomly allocated for fresh embryo transfer (204 oocytes) or vitrification and warming before transfer (186 oocytes) produced similar rates of fertilization, good-quality embryos at day 3, and blastocysts at day 5 or 6, Zsolt Peter Nagy, Ph.D., reported at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Eighty percent of vitrified oocytes survived freezing and warming. Fertilization succeeded in 75% of fresh oocytes and 67% of vitrified oocytes, a slight difference that was not statistically significant. On day 3 of in vitro fertilization (IVF), 50% of fresh oocytes and 48% of vitrified oocytes produced good-quality embryos; by days 5 or 6, 53% of fresh embryos and 55% of vitrified embryos had produced blastocysts, results that did not differ significantly between groups, said Dr. Nagy, scientific and laboratory director of Reproductive Biology Associates, Atlanta.
The study at his institution found that 11 of the 186 vitrified oocytes (6%) achieved a live birth (Fertil. Steril. 2013;99:1891-7).
Maternal age did affect outcomes. Among 11 women aged 30-36 years, 56% of oocytes produced a good embryo by day 3 of IVF, compared with 40% of oocytes from 11 women aged 37-39 years, a significant difference.
The findings support previous data by other investigators on 224 oocytes, 120 of which underwent intracytoplasmic sperm injection (ICSI) as fresh oocytes and 124 of which underwent vitrification and warming before ICSI. Fertilization rates were statistically similar (83% and 77%, respectively). Excellent-quality embryos were produced by 52% in the fresh ICSI group and 52% in the vitrification group. The mean maternal age in the study was 36 years (Hum. Reprod. 2010;25:66-73).
The 39 embryo transfers in the vitrification group resulted in 15 clinical pregnancies (38% per cycle and per embryo transfer) and an implantation rate of 20%. Twelve pregnancies beyond 12 weeks’ gestation were ongoing (30% per cycle and 31% per embryo transfer).
Separate data from Molecular Biometrics suggest that vitrification is efficient for freezing donor oocytes in egg banks, Dr. Nagy said. Among 11,553 eggs from 342 donors that were vitrified, 7,063 were warmed and 90% survived warming, leading to a clinical pregnancy rate of 57% and an implantation rate of 43%.
Cryopreserving eggs has advantages over fresh ovum donation programs, which have long waiting lists, require more complex synchronization between the donor and recipient, offer relatively limited choice, and have other logistical disadvantages. "A couple of years ago, most of us were doing slow freezing" for cryopreservation, Dr. Nagy said. "Many of us have changed to vitrification because we have realized that it is more efficient than slow freezing."
Before, two to four embryos were needed to achieve a clinical pregnancy under slow-freeze methods at his institution, but only one or two are needed using vitrification, he said.
Oocyte cryopreservation programs make elective single-embryo transfer (eSET) a viable option, Dr. Nagy said. In 98 recipients of eSET, 52% achieved a clinical pregnancy, compared with clinical pregnancies in 72% of 109 elective double-embryo transfers, but 51% of the double-embryo transfers resulted in multiple pregnancies, a retrospective study of data from his institution showed. Among nonelective double-embryo transfers, 52% achieved clinical pregnancies, with multiple pregnancies in 30% of recipients.
Double vitrification also appears to be efficient for egg/embryo banking – cryopreserving an oocyte, thawing it, and then freezing the resulting embryo to later be warmed and transferred. One study that compared 471 warming cycles of double-vitrified embryos with 2,629 warming cycles of vitrified embryos derived from fresh oocytes found overall embryo survival rates of 97% and 96%, respectively, with a delivery rate per warming cycle of 34% in the double-vitrified group and 31% in the single-vitrified group (Fertil. Steril. 2013;99:1623-30).
At Dr. Nagy’s institution, 99% of 190 warmed double-vitrified embryos have survived, leading to a 53% clinical pregnancy rate, a 39% implantation rate, and 33 live births so far. "It shows that if you do the procedure correctly, you are able to preserve the viability of those embryos," he said.
The rate of congenital anomalies in live births from donor eggs cryopreserved at his institution does not seem to be significantly higher than the rate in live births from fresh donor eggs – 3 congenital anomalies among 91 live births using fresh donor eggs and 5 congenital anomalies in 338 live births using cryopreserved donor eggs. Case reports from 1986 to 2008 suggest there’s no increased incidence of birth defects using vitrification compared with slow-freeze methods for cryopreservation.
In the future, registry data should provide further evidence of the safety of vitrification, he said.
Dr. Nagy reported having financial associations with Molecular Biometrics, Origio, and other companies.
On Twitter @sherryboschert
SAN FRANCISCO – Recent data show that vitrification of oocytes or embryos can be as efficient as using slow-frozen or fresh oocytes for in vitro fertilization, and so far it appears to be just as safe.
Oocytes from 22 women aged 32-39 years that were randomly allocated for fresh embryo transfer (204 oocytes) or vitrification and warming before transfer (186 oocytes) produced similar rates of fertilization, good-quality embryos at day 3, and blastocysts at day 5 or 6, Zsolt Peter Nagy, Ph.D., reported at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Eighty percent of vitrified oocytes survived freezing and warming. Fertilization succeeded in 75% of fresh oocytes and 67% of vitrified oocytes, a slight difference that was not statistically significant. On day 3 of in vitro fertilization (IVF), 50% of fresh oocytes and 48% of vitrified oocytes produced good-quality embryos; by days 5 or 6, 53% of fresh embryos and 55% of vitrified embryos had produced blastocysts, results that did not differ significantly between groups, said Dr. Nagy, scientific and laboratory director of Reproductive Biology Associates, Atlanta.
The study at his institution found that 11 of the 186 vitrified oocytes (6%) achieved a live birth (Fertil. Steril. 2013;99:1891-7).
Maternal age did affect outcomes. Among 11 women aged 30-36 years, 56% of oocytes produced a good embryo by day 3 of IVF, compared with 40% of oocytes from 11 women aged 37-39 years, a significant difference.
The findings support previous data by other investigators on 224 oocytes, 120 of which underwent intracytoplasmic sperm injection (ICSI) as fresh oocytes and 124 of which underwent vitrification and warming before ICSI. Fertilization rates were statistically similar (83% and 77%, respectively). Excellent-quality embryos were produced by 52% in the fresh ICSI group and 52% in the vitrification group. The mean maternal age in the study was 36 years (Hum. Reprod. 2010;25:66-73).
The 39 embryo transfers in the vitrification group resulted in 15 clinical pregnancies (38% per cycle and per embryo transfer) and an implantation rate of 20%. Twelve pregnancies beyond 12 weeks’ gestation were ongoing (30% per cycle and 31% per embryo transfer).
Separate data from Molecular Biometrics suggest that vitrification is efficient for freezing donor oocytes in egg banks, Dr. Nagy said. Among 11,553 eggs from 342 donors that were vitrified, 7,063 were warmed and 90% survived warming, leading to a clinical pregnancy rate of 57% and an implantation rate of 43%.
Cryopreserving eggs has advantages over fresh ovum donation programs, which have long waiting lists, require more complex synchronization between the donor and recipient, offer relatively limited choice, and have other logistical disadvantages. "A couple of years ago, most of us were doing slow freezing" for cryopreservation, Dr. Nagy said. "Many of us have changed to vitrification because we have realized that it is more efficient than slow freezing."
Before, two to four embryos were needed to achieve a clinical pregnancy under slow-freeze methods at his institution, but only one or two are needed using vitrification, he said.
Oocyte cryopreservation programs make elective single-embryo transfer (eSET) a viable option, Dr. Nagy said. In 98 recipients of eSET, 52% achieved a clinical pregnancy, compared with clinical pregnancies in 72% of 109 elective double-embryo transfers, but 51% of the double-embryo transfers resulted in multiple pregnancies, a retrospective study of data from his institution showed. Among nonelective double-embryo transfers, 52% achieved clinical pregnancies, with multiple pregnancies in 30% of recipients.
Double vitrification also appears to be efficient for egg/embryo banking – cryopreserving an oocyte, thawing it, and then freezing the resulting embryo to later be warmed and transferred. One study that compared 471 warming cycles of double-vitrified embryos with 2,629 warming cycles of vitrified embryos derived from fresh oocytes found overall embryo survival rates of 97% and 96%, respectively, with a delivery rate per warming cycle of 34% in the double-vitrified group and 31% in the single-vitrified group (Fertil. Steril. 2013;99:1623-30).
At Dr. Nagy’s institution, 99% of 190 warmed double-vitrified embryos have survived, leading to a 53% clinical pregnancy rate, a 39% implantation rate, and 33 live births so far. "It shows that if you do the procedure correctly, you are able to preserve the viability of those embryos," he said.
The rate of congenital anomalies in live births from donor eggs cryopreserved at his institution does not seem to be significantly higher than the rate in live births from fresh donor eggs – 3 congenital anomalies among 91 live births using fresh donor eggs and 5 congenital anomalies in 338 live births using cryopreserved donor eggs. Case reports from 1986 to 2008 suggest there’s no increased incidence of birth defects using vitrification compared with slow-freeze methods for cryopreservation.
In the future, registry data should provide further evidence of the safety of vitrification, he said.
Dr. Nagy reported having financial associations with Molecular Biometrics, Origio, and other companies.
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Egg banks save patients time, not money
SAN FRANCISCO – Achieving a pregnancy using frozen oocytes costs nearly $27,000, a survey of U.S. egg banks suggests.
Compared with using fresh oocytes from a matched donor, the frozen-egg route is "not really cost-saving as far as the patient is concerned, but it’s quicker and they don’t have to be matched, necessarily, to another person," Dr. Richard J. Paulson said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
He and his associates surveyed all seven commercial egg banks that they could find in the United States in April 2012, six of which used vitrification as their freezing technique and one of which used slow-freeze techniques. The cost per oocyte averaged $2,225. The egg banks estimated their "efficiency" – the clinical pregnancy rate per oocyte (calculated as the number of pregnancies divided by the number of oocytes obtained, multiplied by 100) – as 10% using slow freezing or averaging 7.5% using vitrification.
"If efficiency is 7.5% per oocyte, you would need about 12 eggs to make one baby. Twelve eggs at $2,225 brings that to around $27,000 to get a pregnancy from frozen eggs," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
The efficiency rates are not as high as hoped for, but probably acceptable. "We’re not sure if we’re going to get to 24%. That seems optimistic to me, but even 10% is not bad if you have that kind of reproducibility," he said.
Commercial egg banks came in one of three operational models. A majority are affiliated with a single assisted reproductive technology (ART) clinic and supply oocytes only to that clinic’s patients. Two or three ART clinics may jointly create a shared commercial egg bank. Last, a few commercial egg banks ship cryopreserved oocytes all over the country and all over the world.
In the survey, the egg banks recommended using a minimum of four oocytes (in slow-freeze cryopreservation) or six to seven oocytes (in vitrification) per patient to attempt pregnancy. At the time, the banks reported having 3,130 oocytes from 294 donors in storage, and said 8,780 oocytes had been used for in vitro fertilization (IVF) to achieve 602 pregnancies (Fertil. Steril. 2013;99:827-31).
The survey’s results already are out of date because the field of egg banks is moving so quickly, Dr. Paulson said. For example, the number of pregnancies from frozen eggs probably has increased 10-fold, he said. "I’m guessing that right now there are perhaps 5,000-6,000 pregnancies in the world from egg freezing."
The egg banks in the survey had been in existence for 1-8 years.
Donor screening at all seven egg banks included psychological and medical screening, genetic counseling, estradiol/follicle-stimulating hormone (FSH) testing, antral follicle count testing, and routine CT cancer testing. Four egg banks also screened donors by anti-Müllerian hormone testing, five conducted routine fragile X carrier testing, and two performed routine karyotyping.
Dr. Paulson shared statistics from his institution’s experience with oocyte cryopreservation and embryo transfer. Ten of 18 women who were recipients of their own previously frozen eggs delivered live births (56%), as did three of four women who used frozen eggs that were not their own (75%).
This year is the 30th anniversary of the first oocyte donation for a successful pregnancy, Dr. Paulson said. The American Society for Reproductive Medicine released a guideline in 2013 saying that mature oocyte cryopreservation via vitrification should no longer be considered experimental (Fertil. Steril. 2013;99:37-43).
Advances in the field and the advantages of IVF using cryopreserved oocytes make egg banks the future for egg donations, he said.
Dr. Paulson is a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
SAN FRANCISCO – Achieving a pregnancy using frozen oocytes costs nearly $27,000, a survey of U.S. egg banks suggests.
Compared with using fresh oocytes from a matched donor, the frozen-egg route is "not really cost-saving as far as the patient is concerned, but it’s quicker and they don’t have to be matched, necessarily, to another person," Dr. Richard J. Paulson said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
He and his associates surveyed all seven commercial egg banks that they could find in the United States in April 2012, six of which used vitrification as their freezing technique and one of which used slow-freeze techniques. The cost per oocyte averaged $2,225. The egg banks estimated their "efficiency" – the clinical pregnancy rate per oocyte (calculated as the number of pregnancies divided by the number of oocytes obtained, multiplied by 100) – as 10% using slow freezing or averaging 7.5% using vitrification.
"If efficiency is 7.5% per oocyte, you would need about 12 eggs to make one baby. Twelve eggs at $2,225 brings that to around $27,000 to get a pregnancy from frozen eggs," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
The efficiency rates are not as high as hoped for, but probably acceptable. "We’re not sure if we’re going to get to 24%. That seems optimistic to me, but even 10% is not bad if you have that kind of reproducibility," he said.
Commercial egg banks came in one of three operational models. A majority are affiliated with a single assisted reproductive technology (ART) clinic and supply oocytes only to that clinic’s patients. Two or three ART clinics may jointly create a shared commercial egg bank. Last, a few commercial egg banks ship cryopreserved oocytes all over the country and all over the world.
In the survey, the egg banks recommended using a minimum of four oocytes (in slow-freeze cryopreservation) or six to seven oocytes (in vitrification) per patient to attempt pregnancy. At the time, the banks reported having 3,130 oocytes from 294 donors in storage, and said 8,780 oocytes had been used for in vitro fertilization (IVF) to achieve 602 pregnancies (Fertil. Steril. 2013;99:827-31).
The survey’s results already are out of date because the field of egg banks is moving so quickly, Dr. Paulson said. For example, the number of pregnancies from frozen eggs probably has increased 10-fold, he said. "I’m guessing that right now there are perhaps 5,000-6,000 pregnancies in the world from egg freezing."
The egg banks in the survey had been in existence for 1-8 years.
Donor screening at all seven egg banks included psychological and medical screening, genetic counseling, estradiol/follicle-stimulating hormone (FSH) testing, antral follicle count testing, and routine CT cancer testing. Four egg banks also screened donors by anti-Müllerian hormone testing, five conducted routine fragile X carrier testing, and two performed routine karyotyping.
Dr. Paulson shared statistics from his institution’s experience with oocyte cryopreservation and embryo transfer. Ten of 18 women who were recipients of their own previously frozen eggs delivered live births (56%), as did three of four women who used frozen eggs that were not their own (75%).
This year is the 30th anniversary of the first oocyte donation for a successful pregnancy, Dr. Paulson said. The American Society for Reproductive Medicine released a guideline in 2013 saying that mature oocyte cryopreservation via vitrification should no longer be considered experimental (Fertil. Steril. 2013;99:37-43).
Advances in the field and the advantages of IVF using cryopreserved oocytes make egg banks the future for egg donations, he said.
Dr. Paulson is a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
SAN FRANCISCO – Achieving a pregnancy using frozen oocytes costs nearly $27,000, a survey of U.S. egg banks suggests.
Compared with using fresh oocytes from a matched donor, the frozen-egg route is "not really cost-saving as far as the patient is concerned, but it’s quicker and they don’t have to be matched, necessarily, to another person," Dr. Richard J. Paulson said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
He and his associates surveyed all seven commercial egg banks that they could find in the United States in April 2012, six of which used vitrification as their freezing technique and one of which used slow-freeze techniques. The cost per oocyte averaged $2,225. The egg banks estimated their "efficiency" – the clinical pregnancy rate per oocyte (calculated as the number of pregnancies divided by the number of oocytes obtained, multiplied by 100) – as 10% using slow freezing or averaging 7.5% using vitrification.
"If efficiency is 7.5% per oocyte, you would need about 12 eggs to make one baby. Twelve eggs at $2,225 brings that to around $27,000 to get a pregnancy from frozen eggs," said Dr. Paulson, professor of obstetrics and gynecology and chief of the division of reproductive endocrinology and infertility at the University of Southern California in Los Angeles.
The efficiency rates are not as high as hoped for, but probably acceptable. "We’re not sure if we’re going to get to 24%. That seems optimistic to me, but even 10% is not bad if you have that kind of reproducibility," he said.
Commercial egg banks came in one of three operational models. A majority are affiliated with a single assisted reproductive technology (ART) clinic and supply oocytes only to that clinic’s patients. Two or three ART clinics may jointly create a shared commercial egg bank. Last, a few commercial egg banks ship cryopreserved oocytes all over the country and all over the world.
In the survey, the egg banks recommended using a minimum of four oocytes (in slow-freeze cryopreservation) or six to seven oocytes (in vitrification) per patient to attempt pregnancy. At the time, the banks reported having 3,130 oocytes from 294 donors in storage, and said 8,780 oocytes had been used for in vitro fertilization (IVF) to achieve 602 pregnancies (Fertil. Steril. 2013;99:827-31).
The survey’s results already are out of date because the field of egg banks is moving so quickly, Dr. Paulson said. For example, the number of pregnancies from frozen eggs probably has increased 10-fold, he said. "I’m guessing that right now there are perhaps 5,000-6,000 pregnancies in the world from egg freezing."
The egg banks in the survey had been in existence for 1-8 years.
Donor screening at all seven egg banks included psychological and medical screening, genetic counseling, estradiol/follicle-stimulating hormone (FSH) testing, antral follicle count testing, and routine CT cancer testing. Four egg banks also screened donors by anti-Müllerian hormone testing, five conducted routine fragile X carrier testing, and two performed routine karyotyping.
Dr. Paulson shared statistics from his institution’s experience with oocyte cryopreservation and embryo transfer. Ten of 18 women who were recipients of their own previously frozen eggs delivered live births (56%), as did three of four women who used frozen eggs that were not their own (75%).
This year is the 30th anniversary of the first oocyte donation for a successful pregnancy, Dr. Paulson said. The American Society for Reproductive Medicine released a guideline in 2013 saying that mature oocyte cryopreservation via vitrification should no longer be considered experimental (Fertil. Steril. 2013;99:37-43).
Advances in the field and the advantages of IVF using cryopreserved oocytes make egg banks the future for egg donations, he said.
Dr. Paulson is a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Major finding: Pregnancy using frozen oocytes requires an average of 12 eggs at a cost of $2,225 per egg and an efficiency rate of 7.5%-10%, for a total cost of approximately $27,000 per pregnancy.
Data source: Survey of all seven U.S. commercial egg banks in existence in April 2012.
Disclosures: Dr. Paulson is a speaker for Ferring Pharmaceuticals and an adviser to Cooper Surgical.
Oocyte vitrification aids fertility after cancer
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Major finding: Among 26 noncancer patients and 4 cancer patients who reclaimed their frozen oocytes, 5 noncancer patients and 1 cancer patient gave birth to live newborns; 8 pregnancies are ongoing.
Data source: A review of 5 years of experience with controlled ovarian hyperstimulation and oocyte vitrification at one European center.
Disclosures: Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.