User login
Combining MRI With Prostate Ultrasound Biopsy Bests Biopsy Alone
CHICAGO – Fusing MRI with real-time, three-dimensional ultrasound allows for more targeted prostate biopsies and finds additional cancers, compared with standard systematic biopsies.
"This may lead to fewer total biopsies, improved yield and improved confidence for active surveillance," Dr. Daniel J.A. Margolis said at the annual meeting of the Radiological Society of North America.
Direct MRI-guided biopsy is not universally available, leaving most centers to use two-dimensional ultrasound to systematically biopsy 12 areas of the prostate, whether they are all suspicious or not. Not surprising, roughly 30% of systematic core biopsies are false negative, explained radiologist Dr. Margolis of the University of California, Los Angeles.
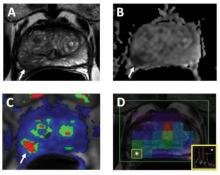
Researchers at UCLA departments and the medical device company Eigen have been using external-array 3 Tesla MRI scans, including T2-weighted, diffusion-weighted, and dynamic contrast-enhanced images to identify suspicious areas in the prostate. The areas are scored on a 5-point scale by a radiologist based on cancer risk, and the data are used to create a 3-D contoured reconstruction that is fused with real-time, transrectal ultrasound during biopsy.
Early results were promising in the two groups of men most likely to benefit from the new imaging technology – those with a prior negative biopsy and elevated prostate-specific antigen (PSA) levels and those with low-risk prostate cancer under active surveillance. In 47 such men, the biopsy-positivity rate was 33% with MRI-fusion ultrasound vs. 7% for systematic, nontargeted biopsy (Urol. Oncol. 2011;29:334-42).
At the meeting, Dr. Margolis presented data from 57 consecutive men with a previous biopsy, in whom MRI-fusion ultrasound identified 101 suspicious areas. In all, 22 men had 28 positive MRI targets.
Positive biopsies were found in 12 patients on targets only. Nine patients had positive lesions on both MRI-fusion ultrasound and systematic biopsy. In one additional patient, the positive systematic core was changed from Gleason 3+3 to 3+4 disease with the targeted biopsy.
Seven patients had positive biopsies found on systematic biopsy only, although all were Gleason score 3+3, less than 4 mm in size and less than 25% of the core, Dr. Margolis said.
A separate study presented in the same session suggests that fusing MRI with transrectal ultrasound biopsy may also be useful in identifying aggressive tumors in men with no prior prostate biopsy or suspicious digital rectal exam and a PSA of 3-10 ng/mL (mean 8 ng/mL).
The overall cancer detection rate was 52% among 323 (168/323) such men, 73% within MRI targets (144/197) and 19% with sextant biopsy (24/126), reported Dr. François Cornud, a consultant radiologist at René Descartes University, Paris.
In 98 patients with both MRI targeted- and sextant-positive biopsies, targeted biopsies identified significantly more cancers with a Gleason score greater than 6 (44% vs. 25%), with a length in any core of more than 7 mm (50% vs. 25.5%) and with a longer mean length (5.3 mm vs. 0.8 mm).
Interestingly, performance was similar whether the multiparametric MRI data were fused with the real-time ultrasound images visually or by a computerized electromagnetic navigator system.
"Targeted biopsies definitely provide better evaluation of tumor burden and Gleason score," Dr. Cornud said, adding that "a negative MRI prior to biopsy may mean no cancer or indolent cancer and may suggest that in these patients biopsy may be deferred."
Both studies were well received, although one attendee questioned whether the researchers have been able to convince frequently reluctant urologists that targeted biopsies are worth it. Dr. Margolis said his project was actually instigated by an urologist. Dr. Cornud said the majority of his urologists are now requesting an MRI and its findings.
Dr. Margolis reported a research grant from Siemens AG and a coauthor reported conflicts with several pharmaceutical and device firms. Dr. Cornud and his coauthors reported no relevant disclosures.
Direct MRI-guided biopsy, prostate, Eigen, prior negative biopsy, elevated prostate-specific antigen (PSA) levels,
CHICAGO – Fusing MRI with real-time, three-dimensional ultrasound allows for more targeted prostate biopsies and finds additional cancers, compared with standard systematic biopsies.
"This may lead to fewer total biopsies, improved yield and improved confidence for active surveillance," Dr. Daniel J.A. Margolis said at the annual meeting of the Radiological Society of North America.
Direct MRI-guided biopsy is not universally available, leaving most centers to use two-dimensional ultrasound to systematically biopsy 12 areas of the prostate, whether they are all suspicious or not. Not surprising, roughly 30% of systematic core biopsies are false negative, explained radiologist Dr. Margolis of the University of California, Los Angeles.
Researchers at UCLA departments and the medical device company Eigen have been using external-array 3 Tesla MRI scans, including T2-weighted, diffusion-weighted, and dynamic contrast-enhanced images to identify suspicious areas in the prostate. The areas are scored on a 5-point scale by a radiologist based on cancer risk, and the data are used to create a 3-D contoured reconstruction that is fused with real-time, transrectal ultrasound during biopsy.
Early results were promising in the two groups of men most likely to benefit from the new imaging technology – those with a prior negative biopsy and elevated prostate-specific antigen (PSA) levels and those with low-risk prostate cancer under active surveillance. In 47 such men, the biopsy-positivity rate was 33% with MRI-fusion ultrasound vs. 7% for systematic, nontargeted biopsy (Urol. Oncol. 2011;29:334-42).
At the meeting, Dr. Margolis presented data from 57 consecutive men with a previous biopsy, in whom MRI-fusion ultrasound identified 101 suspicious areas. In all, 22 men had 28 positive MRI targets.
Positive biopsies were found in 12 patients on targets only. Nine patients had positive lesions on both MRI-fusion ultrasound and systematic biopsy. In one additional patient, the positive systematic core was changed from Gleason 3+3 to 3+4 disease with the targeted biopsy.
Seven patients had positive biopsies found on systematic biopsy only, although all were Gleason score 3+3, less than 4 mm in size and less than 25% of the core, Dr. Margolis said.
A separate study presented in the same session suggests that fusing MRI with transrectal ultrasound biopsy may also be useful in identifying aggressive tumors in men with no prior prostate biopsy or suspicious digital rectal exam and a PSA of 3-10 ng/mL (mean 8 ng/mL).
The overall cancer detection rate was 52% among 323 (168/323) such men, 73% within MRI targets (144/197) and 19% with sextant biopsy (24/126), reported Dr. François Cornud, a consultant radiologist at René Descartes University, Paris.
In 98 patients with both MRI targeted- and sextant-positive biopsies, targeted biopsies identified significantly more cancers with a Gleason score greater than 6 (44% vs. 25%), with a length in any core of more than 7 mm (50% vs. 25.5%) and with a longer mean length (5.3 mm vs. 0.8 mm).
Interestingly, performance was similar whether the multiparametric MRI data were fused with the real-time ultrasound images visually or by a computerized electromagnetic navigator system.
"Targeted biopsies definitely provide better evaluation of tumor burden and Gleason score," Dr. Cornud said, adding that "a negative MRI prior to biopsy may mean no cancer or indolent cancer and may suggest that in these patients biopsy may be deferred."
Both studies were well received, although one attendee questioned whether the researchers have been able to convince frequently reluctant urologists that targeted biopsies are worth it. Dr. Margolis said his project was actually instigated by an urologist. Dr. Cornud said the majority of his urologists are now requesting an MRI and its findings.
Dr. Margolis reported a research grant from Siemens AG and a coauthor reported conflicts with several pharmaceutical and device firms. Dr. Cornud and his coauthors reported no relevant disclosures.
CHICAGO – Fusing MRI with real-time, three-dimensional ultrasound allows for more targeted prostate biopsies and finds additional cancers, compared with standard systematic biopsies.
"This may lead to fewer total biopsies, improved yield and improved confidence for active surveillance," Dr. Daniel J.A. Margolis said at the annual meeting of the Radiological Society of North America.
Direct MRI-guided biopsy is not universally available, leaving most centers to use two-dimensional ultrasound to systematically biopsy 12 areas of the prostate, whether they are all suspicious or not. Not surprising, roughly 30% of systematic core biopsies are false negative, explained radiologist Dr. Margolis of the University of California, Los Angeles.
Researchers at UCLA departments and the medical device company Eigen have been using external-array 3 Tesla MRI scans, including T2-weighted, diffusion-weighted, and dynamic contrast-enhanced images to identify suspicious areas in the prostate. The areas are scored on a 5-point scale by a radiologist based on cancer risk, and the data are used to create a 3-D contoured reconstruction that is fused with real-time, transrectal ultrasound during biopsy.
Early results were promising in the two groups of men most likely to benefit from the new imaging technology – those with a prior negative biopsy and elevated prostate-specific antigen (PSA) levels and those with low-risk prostate cancer under active surveillance. In 47 such men, the biopsy-positivity rate was 33% with MRI-fusion ultrasound vs. 7% for systematic, nontargeted biopsy (Urol. Oncol. 2011;29:334-42).
At the meeting, Dr. Margolis presented data from 57 consecutive men with a previous biopsy, in whom MRI-fusion ultrasound identified 101 suspicious areas. In all, 22 men had 28 positive MRI targets.
Positive biopsies were found in 12 patients on targets only. Nine patients had positive lesions on both MRI-fusion ultrasound and systematic biopsy. In one additional patient, the positive systematic core was changed from Gleason 3+3 to 3+4 disease with the targeted biopsy.
Seven patients had positive biopsies found on systematic biopsy only, although all were Gleason score 3+3, less than 4 mm in size and less than 25% of the core, Dr. Margolis said.
A separate study presented in the same session suggests that fusing MRI with transrectal ultrasound biopsy may also be useful in identifying aggressive tumors in men with no prior prostate biopsy or suspicious digital rectal exam and a PSA of 3-10 ng/mL (mean 8 ng/mL).
The overall cancer detection rate was 52% among 323 (168/323) such men, 73% within MRI targets (144/197) and 19% with sextant biopsy (24/126), reported Dr. François Cornud, a consultant radiologist at René Descartes University, Paris.
In 98 patients with both MRI targeted- and sextant-positive biopsies, targeted biopsies identified significantly more cancers with a Gleason score greater than 6 (44% vs. 25%), with a length in any core of more than 7 mm (50% vs. 25.5%) and with a longer mean length (5.3 mm vs. 0.8 mm).
Interestingly, performance was similar whether the multiparametric MRI data were fused with the real-time ultrasound images visually or by a computerized electromagnetic navigator system.
"Targeted biopsies definitely provide better evaluation of tumor burden and Gleason score," Dr. Cornud said, adding that "a negative MRI prior to biopsy may mean no cancer or indolent cancer and may suggest that in these patients biopsy may be deferred."
Both studies were well received, although one attendee questioned whether the researchers have been able to convince frequently reluctant urologists that targeted biopsies are worth it. Dr. Margolis said his project was actually instigated by an urologist. Dr. Cornud said the majority of his urologists are now requesting an MRI and its findings.
Dr. Margolis reported a research grant from Siemens AG and a coauthor reported conflicts with several pharmaceutical and device firms. Dr. Cornud and his coauthors reported no relevant disclosures.
Direct MRI-guided biopsy, prostate, Eigen, prior negative biopsy, elevated prostate-specific antigen (PSA) levels,
Direct MRI-guided biopsy, prostate, Eigen, prior negative biopsy, elevated prostate-specific antigen (PSA) levels,
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Among 57 consecutive men with a previous biopsy in whom MRI-fusion ultrasound identified 101 suspicious areas, 22 men had 28 positive MRI targets. In a second study, fusing MRI with transrectal ultrasound biopsy was useful in identifying aggressive tumors in men with no prior prostate biopsy or suspicious digital rectal exam and a PSA of 3-10 ng/mL. The overall cancer detection rate was 52% among 323 (168/323) such men, 73% within MRI targets (144/197) and 19% with sextant biopsy (24/126).
Data Source: Prospective study in 57 men with a prior prostate biopsy, and a prospective study in 323 men with no prior biopsy and PSA levels of 3-10 ng/mL.
Disclosures: Dr. Margolis reported a research grant from Siemens AG, and a coauthor reported conflicts with several pharmaceutical and device firms. Dr. Cornud and his coauthors reported no relevant disclosures.
Multiparametric Magnetic Resonance Imaging Identifies Candidates for Prostate Cancer Surveillance
CHICAGO – Multiparametric magnetic resonance imaging trumped national guidelines in correctly classifying patients with prostate cancer as candidates for active surveillance in a retrospective study of 126 men.
National Comprehensive Cancer Network (NCCN) guidelines misclassified 22 of the 126 patients, compared with 12 using multiparametric magnetic resonance imaging (MP-MRI).
When MP-MRI was added to the NCCN criteria, only 5 patients were misclassified, Dr. Baris Turkbey reported in an award-winning paper at the annual meeting of the Radiological Society of North America.
"Presently, MRI is not in any urology guideline, but we want to change this," he said. "Our future goal is to create an NCI [National Cancer Institute] prostate cancer nomogram that includes multiparametric MRI, and our scientists are close to finishing it."
Dr. Turkbey, a fellow in the division of cancer treatment and diagnosis at the National Institutes of Health in Bethesda, Md., and his colleagues evaluated 126 men with biopsy-proven prostate cancer who underwent 3T MP-MRI of the prostate and subsequent radical prostatectomy at a median of 48 days. Their mean age was 59 years and mean prostate-specific antigen (PSA) level 6.67 ng/mL.
MP-MRI images were obtained of the largest and most aggressive lesion using T2-weighted MRI, diffusion-weighted MRI, MR spectroscopy, and dynamic contrast-enhanced MRI. Each dominant lesion was then assigned an MP-MRI score of low (at least two positive sequences), moderate (three positive sequences), or high (four positive sequences).
Patients were eligible for active surveillance on MP-MRI if they had a dominant tumor of less than 0.5 cm3 without extracapsular extension or seminal vesicle invasion and a low imaging score. The NCCN criteria for active surveillance are T1c disease, Gleason score of 6 or less, fewer than three positive biopsy cores, PSA less than 10 ng/mL, and PSA density less than 0.15 ng/mL/g.
Based on histopathological findings, 14 of 126 patents were eligible for active surveillance, with the remaining 112 candidates for active whole gland treatment.
NCCN guidelines wrongly classified 5 of 14 active surveillance patients and 17 of the 112 active treatment patients, whereas MP-MRI wrongly classified 1 active surveillance and 11 active treatment patients, Dr. Turkbey said.
The sensitivity, specificity, and overall accuracy of the NCCN guidelines were 64%, 35%, and 83%, respectively (P = .00002), compared with 93%, 54%, and 91% with MP-MRI (P less than .000001).
The study was limited by using a relatively simple, nonweighted MP-MRI scoring system and comparing MP-MRI with NCCN guidelines only, he acknowledged. Dr. Turkbey said the researchers are currently evaluating a system in which the various parameters are weighted to obtain better predictions.
When asked whether MP-MRI would be cost effective in routine clinical practice, Dr. Turkbey said that "compared to the costs of doing the wrong thing to a patient, an annual or semiannual MRI is well worth it."
Dr. Turkbey reported having no conflicts of interest. A coauthor reported serving as a researcher for Koninklijke Philips Electronics, General Electric, Siemens, Hoffman-La Roche, and iCAD.
National Comprehensive Cancer Network, NCCN, guidelines, misclassified, MP-MRI, Dr. Baris Turkbey, the Radiological Society of North America, NCI, National Cancer Institute, prostate cancer nomogram, multiparametric MRI, prostatectomy, MP-MRI images, MR spectroscopy, dynamic contrast-enhanced MRI,
CHICAGO – Multiparametric magnetic resonance imaging trumped national guidelines in correctly classifying patients with prostate cancer as candidates for active surveillance in a retrospective study of 126 men.
National Comprehensive Cancer Network (NCCN) guidelines misclassified 22 of the 126 patients, compared with 12 using multiparametric magnetic resonance imaging (MP-MRI).
When MP-MRI was added to the NCCN criteria, only 5 patients were misclassified, Dr. Baris Turkbey reported in an award-winning paper at the annual meeting of the Radiological Society of North America.
"Presently, MRI is not in any urology guideline, but we want to change this," he said. "Our future goal is to create an NCI [National Cancer Institute] prostate cancer nomogram that includes multiparametric MRI, and our scientists are close to finishing it."
Dr. Turkbey, a fellow in the division of cancer treatment and diagnosis at the National Institutes of Health in Bethesda, Md., and his colleagues evaluated 126 men with biopsy-proven prostate cancer who underwent 3T MP-MRI of the prostate and subsequent radical prostatectomy at a median of 48 days. Their mean age was 59 years and mean prostate-specific antigen (PSA) level 6.67 ng/mL.
MP-MRI images were obtained of the largest and most aggressive lesion using T2-weighted MRI, diffusion-weighted MRI, MR spectroscopy, and dynamic contrast-enhanced MRI. Each dominant lesion was then assigned an MP-MRI score of low (at least two positive sequences), moderate (three positive sequences), or high (four positive sequences).
Patients were eligible for active surveillance on MP-MRI if they had a dominant tumor of less than 0.5 cm3 without extracapsular extension or seminal vesicle invasion and a low imaging score. The NCCN criteria for active surveillance are T1c disease, Gleason score of 6 or less, fewer than three positive biopsy cores, PSA less than 10 ng/mL, and PSA density less than 0.15 ng/mL/g.
Based on histopathological findings, 14 of 126 patents were eligible for active surveillance, with the remaining 112 candidates for active whole gland treatment.
NCCN guidelines wrongly classified 5 of 14 active surveillance patients and 17 of the 112 active treatment patients, whereas MP-MRI wrongly classified 1 active surveillance and 11 active treatment patients, Dr. Turkbey said.
The sensitivity, specificity, and overall accuracy of the NCCN guidelines were 64%, 35%, and 83%, respectively (P = .00002), compared with 93%, 54%, and 91% with MP-MRI (P less than .000001).
The study was limited by using a relatively simple, nonweighted MP-MRI scoring system and comparing MP-MRI with NCCN guidelines only, he acknowledged. Dr. Turkbey said the researchers are currently evaluating a system in which the various parameters are weighted to obtain better predictions.
When asked whether MP-MRI would be cost effective in routine clinical practice, Dr. Turkbey said that "compared to the costs of doing the wrong thing to a patient, an annual or semiannual MRI is well worth it."
Dr. Turkbey reported having no conflicts of interest. A coauthor reported serving as a researcher for Koninklijke Philips Electronics, General Electric, Siemens, Hoffman-La Roche, and iCAD.
CHICAGO – Multiparametric magnetic resonance imaging trumped national guidelines in correctly classifying patients with prostate cancer as candidates for active surveillance in a retrospective study of 126 men.
National Comprehensive Cancer Network (NCCN) guidelines misclassified 22 of the 126 patients, compared with 12 using multiparametric magnetic resonance imaging (MP-MRI).
When MP-MRI was added to the NCCN criteria, only 5 patients were misclassified, Dr. Baris Turkbey reported in an award-winning paper at the annual meeting of the Radiological Society of North America.
"Presently, MRI is not in any urology guideline, but we want to change this," he said. "Our future goal is to create an NCI [National Cancer Institute] prostate cancer nomogram that includes multiparametric MRI, and our scientists are close to finishing it."
Dr. Turkbey, a fellow in the division of cancer treatment and diagnosis at the National Institutes of Health in Bethesda, Md., and his colleagues evaluated 126 men with biopsy-proven prostate cancer who underwent 3T MP-MRI of the prostate and subsequent radical prostatectomy at a median of 48 days. Their mean age was 59 years and mean prostate-specific antigen (PSA) level 6.67 ng/mL.
MP-MRI images were obtained of the largest and most aggressive lesion using T2-weighted MRI, diffusion-weighted MRI, MR spectroscopy, and dynamic contrast-enhanced MRI. Each dominant lesion was then assigned an MP-MRI score of low (at least two positive sequences), moderate (three positive sequences), or high (four positive sequences).
Patients were eligible for active surveillance on MP-MRI if they had a dominant tumor of less than 0.5 cm3 without extracapsular extension or seminal vesicle invasion and a low imaging score. The NCCN criteria for active surveillance are T1c disease, Gleason score of 6 or less, fewer than three positive biopsy cores, PSA less than 10 ng/mL, and PSA density less than 0.15 ng/mL/g.
Based on histopathological findings, 14 of 126 patents were eligible for active surveillance, with the remaining 112 candidates for active whole gland treatment.
NCCN guidelines wrongly classified 5 of 14 active surveillance patients and 17 of the 112 active treatment patients, whereas MP-MRI wrongly classified 1 active surveillance and 11 active treatment patients, Dr. Turkbey said.
The sensitivity, specificity, and overall accuracy of the NCCN guidelines were 64%, 35%, and 83%, respectively (P = .00002), compared with 93%, 54%, and 91% with MP-MRI (P less than .000001).
The study was limited by using a relatively simple, nonweighted MP-MRI scoring system and comparing MP-MRI with NCCN guidelines only, he acknowledged. Dr. Turkbey said the researchers are currently evaluating a system in which the various parameters are weighted to obtain better predictions.
When asked whether MP-MRI would be cost effective in routine clinical practice, Dr. Turkbey said that "compared to the costs of doing the wrong thing to a patient, an annual or semiannual MRI is well worth it."
Dr. Turkbey reported having no conflicts of interest. A coauthor reported serving as a researcher for Koninklijke Philips Electronics, General Electric, Siemens, Hoffman-La Roche, and iCAD.
National Comprehensive Cancer Network, NCCN, guidelines, misclassified, MP-MRI, Dr. Baris Turkbey, the Radiological Society of North America, NCI, National Cancer Institute, prostate cancer nomogram, multiparametric MRI, prostatectomy, MP-MRI images, MR spectroscopy, dynamic contrast-enhanced MRI,
National Comprehensive Cancer Network, NCCN, guidelines, misclassified, MP-MRI, Dr. Baris Turkbey, the Radiological Society of North America, NCI, National Cancer Institute, prostate cancer nomogram, multiparametric MRI, prostatectomy, MP-MRI images, MR spectroscopy, dynamic contrast-enhanced MRI,
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: The sensitivity, specificity and overall accuracy of the NCCN guidelines were 64%, 35%, and 83% (P = .00002), compared with 93%, 54%, and 91% with MP-MRI (P less than .000001).
Data Source: Retrospective analysis of 126 patients with prostate cancer.
Disclosures: Dr. Turkbey reported no conflicts of interest. A coauthor reported serving as a researcher for Koninklijke Philips Electronics, General Electric, Siemens, Hoffman-La Roche, and iCAD.
Automated EMR Search Speeds ED Evaluations
CHICAGO – In as little as 15 seconds, an automated electronic medical record search application can retrieve vital past medical history for patients presenting to the emergency department.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record," Dr. Arun Krishnaraj said at the annual meeting of the Radiological Society of North America.
The researchers also hope that the novel search tool, known as QPID (Queriable Patient Inference Dossier), will help reduce inappropriate imaging in the emergency department (ED), where incomplete awareness of past imaging studies often leads to duplication.
QPID is a programmable, ontology-driven semantic search application that extracts data from multiple data repositories and then indexes or prepares that information for a search, explained Dr. Krishnaraj of Massachusetts General Hospital and Harvard Medical School in Boston. It gathers data through Web services available in Harvard’s network and can be automated to run against a service schedule or care unit census. It is not a data repository nor does it store personal health information.
QPID goes beyond the simple key word search by allowing a clinician to use a variety of natural language expressions to perform Boolean searches for two terms such as "hepatitis and cirrhosis"; negate a target phrase to exclude unwanted hits, for example, "the patient does not have hepatitis"; and to find exact or partial matches for acronyms, synonyms, or misspellings such as "hepatitis/heputytus," he said.
The three distinct advantages of QPID over a traditional manual record search is that it can search for a concept such as "Does the patient have a malignancy?"; it enables complex structured queries to be run automatically; and it integrates the search output into a web browser or office application, Dr. Krishnaraj said.
The automated queries can be retrieved with a simple search string such as "*malignancy." QPID would then search for evidence of malignancy including synonyms such as tumor, mass, and neoplasm. It will exclude the term "mass" when used in other ways, as in "Mass." for Massachusetts, while also matching exact acronyms for types of malignancy such as NSCLC (non–small cell lung cancer).
QPID has been live for about 6 months at the Massachusetts General ED and about 1 month at the Brigham and Women’s Hospital ED, Dr. Krishnaraj said in an interview. It is available as a search platform to any clinician within Massachusetts General, with custom interfaces developed for several divisions including radiology and gastroenterology, among others.
The researchers validated QPID by performing an automated search for each of the 74 topics included in the application for 500 consecutive patients who presented to the hospital’s ED in 2010. The automated results were then compared with those from two clinicians who performed an untimed manual review for the same 74 search topics on 30 randomly selected patients in the cohort.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record."
The average search time for QPID to research all 74 topics was 15 seconds, plus or minus 5 seconds, Dr. Krishnaraj said. To complete a thorough review of all available data, the manual review averaged 5-10 minutes per patient.
For finding laboratory results, QPID demonstrated a sensitivity of 97% and specificity of 99%, with a positive predictive value (PPV) of 99% and negative predictive value (NPV) of 96%.
Excellent results were also seen for free text searches, such as "is there a history of PE in the last 10 years?" For these, QPID had a sensitivity of 98%, specificity of 93%, PPV of 90%, and NPV of 98%.
Dr. Krishnaraj acknowledged that the overall results could be affected by data in the EMR not detected by either QPID or manual review. Other limitations include the potential for false positives, overestimation of low-prevalence conditions, and missing data for care received outside the hospital network and not recorded electronically.
The researchers are currently evaluating how best to measure the effect of QPID use on imaging use in the two hospitals’ large and busy EDs.
Dr. Krishnaraj and a coauthor reported research support/grants from General Electric.
CHICAGO – In as little as 15 seconds, an automated electronic medical record search application can retrieve vital past medical history for patients presenting to the emergency department.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record," Dr. Arun Krishnaraj said at the annual meeting of the Radiological Society of North America.
The researchers also hope that the novel search tool, known as QPID (Queriable Patient Inference Dossier), will help reduce inappropriate imaging in the emergency department (ED), where incomplete awareness of past imaging studies often leads to duplication.
QPID is a programmable, ontology-driven semantic search application that extracts data from multiple data repositories and then indexes or prepares that information for a search, explained Dr. Krishnaraj of Massachusetts General Hospital and Harvard Medical School in Boston. It gathers data through Web services available in Harvard’s network and can be automated to run against a service schedule or care unit census. It is not a data repository nor does it store personal health information.
QPID goes beyond the simple key word search by allowing a clinician to use a variety of natural language expressions to perform Boolean searches for two terms such as "hepatitis and cirrhosis"; negate a target phrase to exclude unwanted hits, for example, "the patient does not have hepatitis"; and to find exact or partial matches for acronyms, synonyms, or misspellings such as "hepatitis/heputytus," he said.
The three distinct advantages of QPID over a traditional manual record search is that it can search for a concept such as "Does the patient have a malignancy?"; it enables complex structured queries to be run automatically; and it integrates the search output into a web browser or office application, Dr. Krishnaraj said.
The automated queries can be retrieved with a simple search string such as "*malignancy." QPID would then search for evidence of malignancy including synonyms such as tumor, mass, and neoplasm. It will exclude the term "mass" when used in other ways, as in "Mass." for Massachusetts, while also matching exact acronyms for types of malignancy such as NSCLC (non–small cell lung cancer).
QPID has been live for about 6 months at the Massachusetts General ED and about 1 month at the Brigham and Women’s Hospital ED, Dr. Krishnaraj said in an interview. It is available as a search platform to any clinician within Massachusetts General, with custom interfaces developed for several divisions including radiology and gastroenterology, among others.
The researchers validated QPID by performing an automated search for each of the 74 topics included in the application for 500 consecutive patients who presented to the hospital’s ED in 2010. The automated results were then compared with those from two clinicians who performed an untimed manual review for the same 74 search topics on 30 randomly selected patients in the cohort.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record."
The average search time for QPID to research all 74 topics was 15 seconds, plus or minus 5 seconds, Dr. Krishnaraj said. To complete a thorough review of all available data, the manual review averaged 5-10 minutes per patient.
For finding laboratory results, QPID demonstrated a sensitivity of 97% and specificity of 99%, with a positive predictive value (PPV) of 99% and negative predictive value (NPV) of 96%.
Excellent results were also seen for free text searches, such as "is there a history of PE in the last 10 years?" For these, QPID had a sensitivity of 98%, specificity of 93%, PPV of 90%, and NPV of 98%.
Dr. Krishnaraj acknowledged that the overall results could be affected by data in the EMR not detected by either QPID or manual review. Other limitations include the potential for false positives, overestimation of low-prevalence conditions, and missing data for care received outside the hospital network and not recorded electronically.
The researchers are currently evaluating how best to measure the effect of QPID use on imaging use in the two hospitals’ large and busy EDs.
Dr. Krishnaraj and a coauthor reported research support/grants from General Electric.
CHICAGO – In as little as 15 seconds, an automated electronic medical record search application can retrieve vital past medical history for patients presenting to the emergency department.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record," Dr. Arun Krishnaraj said at the annual meeting of the Radiological Society of North America.
The researchers also hope that the novel search tool, known as QPID (Queriable Patient Inference Dossier), will help reduce inappropriate imaging in the emergency department (ED), where incomplete awareness of past imaging studies often leads to duplication.
QPID is a programmable, ontology-driven semantic search application that extracts data from multiple data repositories and then indexes or prepares that information for a search, explained Dr. Krishnaraj of Massachusetts General Hospital and Harvard Medical School in Boston. It gathers data through Web services available in Harvard’s network and can be automated to run against a service schedule or care unit census. It is not a data repository nor does it store personal health information.
QPID goes beyond the simple key word search by allowing a clinician to use a variety of natural language expressions to perform Boolean searches for two terms such as "hepatitis and cirrhosis"; negate a target phrase to exclude unwanted hits, for example, "the patient does not have hepatitis"; and to find exact or partial matches for acronyms, synonyms, or misspellings such as "hepatitis/heputytus," he said.
The three distinct advantages of QPID over a traditional manual record search is that it can search for a concept such as "Does the patient have a malignancy?"; it enables complex structured queries to be run automatically; and it integrates the search output into a web browser or office application, Dr. Krishnaraj said.
The automated queries can be retrieved with a simple search string such as "*malignancy." QPID would then search for evidence of malignancy including synonyms such as tumor, mass, and neoplasm. It will exclude the term "mass" when used in other ways, as in "Mass." for Massachusetts, while also matching exact acronyms for types of malignancy such as NSCLC (non–small cell lung cancer).
QPID has been live for about 6 months at the Massachusetts General ED and about 1 month at the Brigham and Women’s Hospital ED, Dr. Krishnaraj said in an interview. It is available as a search platform to any clinician within Massachusetts General, with custom interfaces developed for several divisions including radiology and gastroenterology, among others.
The researchers validated QPID by performing an automated search for each of the 74 topics included in the application for 500 consecutive patients who presented to the hospital’s ED in 2010. The automated results were then compared with those from two clinicians who performed an untimed manual review for the same 74 search topics on 30 randomly selected patients in the cohort.
"We believe this kind of innovative interface allows for a more efficient view of the entire patient history in the electronic health record."
The average search time for QPID to research all 74 topics was 15 seconds, plus or minus 5 seconds, Dr. Krishnaraj said. To complete a thorough review of all available data, the manual review averaged 5-10 minutes per patient.
For finding laboratory results, QPID demonstrated a sensitivity of 97% and specificity of 99%, with a positive predictive value (PPV) of 99% and negative predictive value (NPV) of 96%.
Excellent results were also seen for free text searches, such as "is there a history of PE in the last 10 years?" For these, QPID had a sensitivity of 98%, specificity of 93%, PPV of 90%, and NPV of 98%.
Dr. Krishnaraj acknowledged that the overall results could be affected by data in the EMR not detected by either QPID or manual review. Other limitations include the potential for false positives, overestimation of low-prevalence conditions, and missing data for care received outside the hospital network and not recorded electronically.
The researchers are currently evaluating how best to measure the effect of QPID use on imaging use in the two hospitals’ large and busy EDs.
Dr. Krishnaraj and a coauthor reported research support/grants from General Electric.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Tomosynthesis Shines in Dense Breast Cases
CHICAGO – Adding tomosynthesis to full-field digital mammography improved cancer detection and reduced recall rates in women with dense breasts in a study of 293 patients.
"Both clinically and in trials, we’ve seen that tomosynthesis offers benefit for all women, but I think there is a particular benefit, the increased gains are more, for women with dense breast tissue," Dr. Elizabeth Rafferty said at the annual meeting of the Radiological Society of North America. "I think that underscores where we may start our triage efforts with limited resources."
She reported on an enriched case set of 69 biopsy-proven cancers, 74 benign biopsies, 50 recalled screening cases, and 100 negative screening cases, all with a BI-RADS (Breast Imaging Reporting and Data System) density score of 3 (heterogeneously dense) or 4 (extremely dense). Calcification was present in 25% and noncalcification in 75% of cases.
Eight radiologists read the cases in two separate sessions separated by 1 month, with half of the cases read in each mode for each reading session. Identification of the lesion location and type and initial BI-RADS score (0, 1, 2) were used to determine the recall rate. A probability of malignancy score from 0% to 100% was used to calculate the receiver operating area under the curve (AUC).
The difference in the AUC between standard full-field digital mammography (FFDM) plus tomosynthesis and FFDM alone was significantly higher at 8.3% for all cases (AUC 0.940 vs. 0.857, P value less than .0001), 4.1% for calcification cases (0.818 vs. 0.777, P = .048), and 11% for noncalcification cases (0.977 vs. 0.867, P = .0001), reported Dr. Rafferty, director of breast imaging at Massachusetts General Hospital in Boston.
The recall rate for all cancer cases was 9.7% higher for FFDM plus tomosynthesis vs. FFDM alone. Specifically, it was 3.8% higher for calcification cases and 14.3% higher for noncalcification cases.
Seven of the eight readers increased their cancer detection rate using FFDM plus tomosynthesis, while one reader had the same detection rate on the two modalities. For six of the seven readers, the improvement in cancer detection was statistically significant, she said.
For noncancer screening cases, the recall rate for FFDM plus tomosynthesis was 23.3% vs. 33.9% for FFDM alone, representing a 31% reduction in the noncancer recall rate.
Six of the eight readers had significant decreases in their screening recall rate using the combined imaging modality, while the other two readers had no significant change.
"In women with dense breast tissue, tomosynthesis, when added to FFDM, appears to offer particular value both in terms of sensitivity as well as specificity of the examination," Dr. Rafferty said.
She noted that the numbers were too small to identify a difference in performance with FFDM plus tomosynthesis between dense and extremely dense breasts.
"In women with dense breast tissue, tomosynthesis ... appears to offer particular value."
An attendee also asked whether she would recommend using tomosynthesis in lieu of screening ultrasound.
"In terms of the positive predictive value of screening ultrasound, I think that screening mammography, or some form of screening mammography, is going to remain the mainstay," she said. "But in terms of our diagnostic evaluation, I think ultrasound has become an incredibly important tool in the diagnostic evaluation.
"Basically, tomosynthesis examination plus ultrasound has become for me, and I think for many other people, kind of the go-to regimen instead of using additional views. The two are very complementary."
Dr. Rafferty reported no relevant financial disclosures. A coauthor reported serving as a patent holder and employee of Hologic.
CHICAGO – Adding tomosynthesis to full-field digital mammography improved cancer detection and reduced recall rates in women with dense breasts in a study of 293 patients.
"Both clinically and in trials, we’ve seen that tomosynthesis offers benefit for all women, but I think there is a particular benefit, the increased gains are more, for women with dense breast tissue," Dr. Elizabeth Rafferty said at the annual meeting of the Radiological Society of North America. "I think that underscores where we may start our triage efforts with limited resources."
She reported on an enriched case set of 69 biopsy-proven cancers, 74 benign biopsies, 50 recalled screening cases, and 100 negative screening cases, all with a BI-RADS (Breast Imaging Reporting and Data System) density score of 3 (heterogeneously dense) or 4 (extremely dense). Calcification was present in 25% and noncalcification in 75% of cases.
Eight radiologists read the cases in two separate sessions separated by 1 month, with half of the cases read in each mode for each reading session. Identification of the lesion location and type and initial BI-RADS score (0, 1, 2) were used to determine the recall rate. A probability of malignancy score from 0% to 100% was used to calculate the receiver operating area under the curve (AUC).
The difference in the AUC between standard full-field digital mammography (FFDM) plus tomosynthesis and FFDM alone was significantly higher at 8.3% for all cases (AUC 0.940 vs. 0.857, P value less than .0001), 4.1% for calcification cases (0.818 vs. 0.777, P = .048), and 11% for noncalcification cases (0.977 vs. 0.867, P = .0001), reported Dr. Rafferty, director of breast imaging at Massachusetts General Hospital in Boston.
The recall rate for all cancer cases was 9.7% higher for FFDM plus tomosynthesis vs. FFDM alone. Specifically, it was 3.8% higher for calcification cases and 14.3% higher for noncalcification cases.
Seven of the eight readers increased their cancer detection rate using FFDM plus tomosynthesis, while one reader had the same detection rate on the two modalities. For six of the seven readers, the improvement in cancer detection was statistically significant, she said.
For noncancer screening cases, the recall rate for FFDM plus tomosynthesis was 23.3% vs. 33.9% for FFDM alone, representing a 31% reduction in the noncancer recall rate.
Six of the eight readers had significant decreases in their screening recall rate using the combined imaging modality, while the other two readers had no significant change.
"In women with dense breast tissue, tomosynthesis, when added to FFDM, appears to offer particular value both in terms of sensitivity as well as specificity of the examination," Dr. Rafferty said.
She noted that the numbers were too small to identify a difference in performance with FFDM plus tomosynthesis between dense and extremely dense breasts.
"In women with dense breast tissue, tomosynthesis ... appears to offer particular value."
An attendee also asked whether she would recommend using tomosynthesis in lieu of screening ultrasound.
"In terms of the positive predictive value of screening ultrasound, I think that screening mammography, or some form of screening mammography, is going to remain the mainstay," she said. "But in terms of our diagnostic evaluation, I think ultrasound has become an incredibly important tool in the diagnostic evaluation.
"Basically, tomosynthesis examination plus ultrasound has become for me, and I think for many other people, kind of the go-to regimen instead of using additional views. The two are very complementary."
Dr. Rafferty reported no relevant financial disclosures. A coauthor reported serving as a patent holder and employee of Hologic.
CHICAGO – Adding tomosynthesis to full-field digital mammography improved cancer detection and reduced recall rates in women with dense breasts in a study of 293 patients.
"Both clinically and in trials, we’ve seen that tomosynthesis offers benefit for all women, but I think there is a particular benefit, the increased gains are more, for women with dense breast tissue," Dr. Elizabeth Rafferty said at the annual meeting of the Radiological Society of North America. "I think that underscores where we may start our triage efforts with limited resources."
She reported on an enriched case set of 69 biopsy-proven cancers, 74 benign biopsies, 50 recalled screening cases, and 100 negative screening cases, all with a BI-RADS (Breast Imaging Reporting and Data System) density score of 3 (heterogeneously dense) or 4 (extremely dense). Calcification was present in 25% and noncalcification in 75% of cases.
Eight radiologists read the cases in two separate sessions separated by 1 month, with half of the cases read in each mode for each reading session. Identification of the lesion location and type and initial BI-RADS score (0, 1, 2) were used to determine the recall rate. A probability of malignancy score from 0% to 100% was used to calculate the receiver operating area under the curve (AUC).
The difference in the AUC between standard full-field digital mammography (FFDM) plus tomosynthesis and FFDM alone was significantly higher at 8.3% for all cases (AUC 0.940 vs. 0.857, P value less than .0001), 4.1% for calcification cases (0.818 vs. 0.777, P = .048), and 11% for noncalcification cases (0.977 vs. 0.867, P = .0001), reported Dr. Rafferty, director of breast imaging at Massachusetts General Hospital in Boston.
The recall rate for all cancer cases was 9.7% higher for FFDM plus tomosynthesis vs. FFDM alone. Specifically, it was 3.8% higher for calcification cases and 14.3% higher for noncalcification cases.
Seven of the eight readers increased their cancer detection rate using FFDM plus tomosynthesis, while one reader had the same detection rate on the two modalities. For six of the seven readers, the improvement in cancer detection was statistically significant, she said.
For noncancer screening cases, the recall rate for FFDM plus tomosynthesis was 23.3% vs. 33.9% for FFDM alone, representing a 31% reduction in the noncancer recall rate.
Six of the eight readers had significant decreases in their screening recall rate using the combined imaging modality, while the other two readers had no significant change.
"In women with dense breast tissue, tomosynthesis, when added to FFDM, appears to offer particular value both in terms of sensitivity as well as specificity of the examination," Dr. Rafferty said.
She noted that the numbers were too small to identify a difference in performance with FFDM plus tomosynthesis between dense and extremely dense breasts.
"In women with dense breast tissue, tomosynthesis ... appears to offer particular value."
An attendee also asked whether she would recommend using tomosynthesis in lieu of screening ultrasound.
"In terms of the positive predictive value of screening ultrasound, I think that screening mammography, or some form of screening mammography, is going to remain the mainstay," she said. "But in terms of our diagnostic evaluation, I think ultrasound has become an incredibly important tool in the diagnostic evaluation.
"Basically, tomosynthesis examination plus ultrasound has become for me, and I think for many other people, kind of the go-to regimen instead of using additional views. The two are very complementary."
Dr. Rafferty reported no relevant financial disclosures. A coauthor reported serving as a patent holder and employee of Hologic.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: The recall rate for cancer cases was 9.7% higher with tomosynthesis plus full-field digital mammography vs. FFDM alone, while the recall rate for noncancer screening cases was reduced 31% with tomosynthesis plus FFDM.
Data Source: Enriched case set of 293 cases with heterogeneously dense or extremely dense breast tissue.
Disclosures: Dr. Rafferty reported no relevant financial disclosures. A coauthor reported serving as a patent holder and employee of Hologic.
Breast-Mammogram Detector Mismatch Results in Excess Radiation
CHICAGO – A mismatch between breast size and detector size during mammography resulted in significantly higher doses of radiation for women with large breasts in a study of 886 patients.
On average, women with large breasts screened on a small detector received almost 5 milligray (mGy) of radiation, which exceeds the American College of Radiology guidelines of 3-4 mGy or less for a standard two-view mammogram.
When a mismatch occurs, women with large breasts receive significantly higher doses of radiation than women with small breasts or their counterparts with large breasts correctly matched to a large detector, Dr. Cathy Wells said when presenting the award-winning study at the annual meeting of the Radiological Society of North America.
"Women with large breasts should be imaged with a large detector to avoid an unnecessary increase in radiation dose," she urged.
The quality assurance study involved 886 women who presented for screening or diagnostic mammography during a 6-week period in late 2009. The exams were performed with a phosphor charge-coupled device detector, which is available in pre-set sizes (large or small) due to manufacturing constraints, she said. Insufficient data for 22 patients left 426 screening and 438 diagnostic patients evaluable for analysis.
A sizeable number, or almost 20% of patients, were affected by a mismatch between breast and detector size, said Dr. Wells, who completed the study at Beth Israel Deaconess Medical Center and is now a breast imaging fellow at Massachusetts General Hospital, both in Boston.
The percentage of mismatches varied from 10% of screening patients with large breasts, defined as a "C" cup or larger, to 27% of screening patients with small breasts imaged with a large detector.
A mismatch occurred in 22% of diagnostic mammography patients with large breasts and 17% of diagnostic patients with small breasts.
Despite the sizeable number of mismatches in the study, not all women will be faced with this problem when they arrive for their mammogram, Dr. Wells said in an interview. The phosphor charge-coupled device detector is one of four types of digital detectors currently available in the United States, and to her knowledge the only type that has such size constraints. In addition, not all imaging centers use this detector type.
Some centers, including her own, have both large- and small-size detectors available, although there can be a wait for the proper size, she noted. Women can choose to wait or be imaged with a different detector after a discussion with the technologist.
"The best option for women to ensure a correct match between breast size and detector size would be to talk with the technologist who performs the actual mammogram, [as] the scheduler or person at the check-in desk will likely not know the answer," Dr. Wells said.
"Women could ask the technologist whether the detector comes in different sizes, since not all do, and if so, whether they are correctly matched."
Screening mammogram patients with correctly matched breast and detector sizes received an average mean glandular dose per breast of 3.3 mGy, compared with 4.9 mGy for mismatched patients with large breasts (P value less than .05).
This was due to significantly more views obtained in mismatched patients with large breasts, compared with both the large-breast patients imaged on a large detector and small-breast patients imaged on a small detector (mean 5.9 views vs. 4.6 views vs. 4.7 views, P less than .05), Dr. Wells said. Interestingly, small-breast patients mismatched to a large detector underwent a similar number of views at a mean of 4.6, but actually received slightly less radiation at mean dose of 2.9 mGy (P less than .05).
During diagnostic mammograms, the radiation dose was again significantly higher among mismatched patients with large breasts, compared with the correctly matched large- and small-breast groups (8.2 mGy vs. 6.7 mGy, P less than .05), but it did not appear to be related to the number of views obtained, she said, adding that other factors must be at work. Several variables contribute to radiation dose, but in this case, the most likely culprit is compression thickness, Dr. Wells said.
"It may be more difficult to adequately compress a large breast with a small detector, resulting in a larger radiation dose," she said. "We hope to analyze the data again, to answer this question."
Dr. Wells and her coauthors reported having no conflicts of interest.
CHICAGO – A mismatch between breast size and detector size during mammography resulted in significantly higher doses of radiation for women with large breasts in a study of 886 patients.
On average, women with large breasts screened on a small detector received almost 5 milligray (mGy) of radiation, which exceeds the American College of Radiology guidelines of 3-4 mGy or less for a standard two-view mammogram.
When a mismatch occurs, women with large breasts receive significantly higher doses of radiation than women with small breasts or their counterparts with large breasts correctly matched to a large detector, Dr. Cathy Wells said when presenting the award-winning study at the annual meeting of the Radiological Society of North America.
"Women with large breasts should be imaged with a large detector to avoid an unnecessary increase in radiation dose," she urged.
The quality assurance study involved 886 women who presented for screening or diagnostic mammography during a 6-week period in late 2009. The exams were performed with a phosphor charge-coupled device detector, which is available in pre-set sizes (large or small) due to manufacturing constraints, she said. Insufficient data for 22 patients left 426 screening and 438 diagnostic patients evaluable for analysis.
A sizeable number, or almost 20% of patients, were affected by a mismatch between breast and detector size, said Dr. Wells, who completed the study at Beth Israel Deaconess Medical Center and is now a breast imaging fellow at Massachusetts General Hospital, both in Boston.
The percentage of mismatches varied from 10% of screening patients with large breasts, defined as a "C" cup or larger, to 27% of screening patients with small breasts imaged with a large detector.
A mismatch occurred in 22% of diagnostic mammography patients with large breasts and 17% of diagnostic patients with small breasts.
Despite the sizeable number of mismatches in the study, not all women will be faced with this problem when they arrive for their mammogram, Dr. Wells said in an interview. The phosphor charge-coupled device detector is one of four types of digital detectors currently available in the United States, and to her knowledge the only type that has such size constraints. In addition, not all imaging centers use this detector type.
Some centers, including her own, have both large- and small-size detectors available, although there can be a wait for the proper size, she noted. Women can choose to wait or be imaged with a different detector after a discussion with the technologist.
"The best option for women to ensure a correct match between breast size and detector size would be to talk with the technologist who performs the actual mammogram, [as] the scheduler or person at the check-in desk will likely not know the answer," Dr. Wells said.
"Women could ask the technologist whether the detector comes in different sizes, since not all do, and if so, whether they are correctly matched."
Screening mammogram patients with correctly matched breast and detector sizes received an average mean glandular dose per breast of 3.3 mGy, compared with 4.9 mGy for mismatched patients with large breasts (P value less than .05).
This was due to significantly more views obtained in mismatched patients with large breasts, compared with both the large-breast patients imaged on a large detector and small-breast patients imaged on a small detector (mean 5.9 views vs. 4.6 views vs. 4.7 views, P less than .05), Dr. Wells said. Interestingly, small-breast patients mismatched to a large detector underwent a similar number of views at a mean of 4.6, but actually received slightly less radiation at mean dose of 2.9 mGy (P less than .05).
During diagnostic mammograms, the radiation dose was again significantly higher among mismatched patients with large breasts, compared with the correctly matched large- and small-breast groups (8.2 mGy vs. 6.7 mGy, P less than .05), but it did not appear to be related to the number of views obtained, she said, adding that other factors must be at work. Several variables contribute to radiation dose, but in this case, the most likely culprit is compression thickness, Dr. Wells said.
"It may be more difficult to adequately compress a large breast with a small detector, resulting in a larger radiation dose," she said. "We hope to analyze the data again, to answer this question."
Dr. Wells and her coauthors reported having no conflicts of interest.
CHICAGO – A mismatch between breast size and detector size during mammography resulted in significantly higher doses of radiation for women with large breasts in a study of 886 patients.
On average, women with large breasts screened on a small detector received almost 5 milligray (mGy) of radiation, which exceeds the American College of Radiology guidelines of 3-4 mGy or less for a standard two-view mammogram.
When a mismatch occurs, women with large breasts receive significantly higher doses of radiation than women with small breasts or their counterparts with large breasts correctly matched to a large detector, Dr. Cathy Wells said when presenting the award-winning study at the annual meeting of the Radiological Society of North America.
"Women with large breasts should be imaged with a large detector to avoid an unnecessary increase in radiation dose," she urged.
The quality assurance study involved 886 women who presented for screening or diagnostic mammography during a 6-week period in late 2009. The exams were performed with a phosphor charge-coupled device detector, which is available in pre-set sizes (large or small) due to manufacturing constraints, she said. Insufficient data for 22 patients left 426 screening and 438 diagnostic patients evaluable for analysis.
A sizeable number, or almost 20% of patients, were affected by a mismatch between breast and detector size, said Dr. Wells, who completed the study at Beth Israel Deaconess Medical Center and is now a breast imaging fellow at Massachusetts General Hospital, both in Boston.
The percentage of mismatches varied from 10% of screening patients with large breasts, defined as a "C" cup or larger, to 27% of screening patients with small breasts imaged with a large detector.
A mismatch occurred in 22% of diagnostic mammography patients with large breasts and 17% of diagnostic patients with small breasts.
Despite the sizeable number of mismatches in the study, not all women will be faced with this problem when they arrive for their mammogram, Dr. Wells said in an interview. The phosphor charge-coupled device detector is one of four types of digital detectors currently available in the United States, and to her knowledge the only type that has such size constraints. In addition, not all imaging centers use this detector type.
Some centers, including her own, have both large- and small-size detectors available, although there can be a wait for the proper size, she noted. Women can choose to wait or be imaged with a different detector after a discussion with the technologist.
"The best option for women to ensure a correct match between breast size and detector size would be to talk with the technologist who performs the actual mammogram, [as] the scheduler or person at the check-in desk will likely not know the answer," Dr. Wells said.
"Women could ask the technologist whether the detector comes in different sizes, since not all do, and if so, whether they are correctly matched."
Screening mammogram patients with correctly matched breast and detector sizes received an average mean glandular dose per breast of 3.3 mGy, compared with 4.9 mGy for mismatched patients with large breasts (P value less than .05).
This was due to significantly more views obtained in mismatched patients with large breasts, compared with both the large-breast patients imaged on a large detector and small-breast patients imaged on a small detector (mean 5.9 views vs. 4.6 views vs. 4.7 views, P less than .05), Dr. Wells said. Interestingly, small-breast patients mismatched to a large detector underwent a similar number of views at a mean of 4.6, but actually received slightly less radiation at mean dose of 2.9 mGy (P less than .05).
During diagnostic mammograms, the radiation dose was again significantly higher among mismatched patients with large breasts, compared with the correctly matched large- and small-breast groups (8.2 mGy vs. 6.7 mGy, P less than .05), but it did not appear to be related to the number of views obtained, she said, adding that other factors must be at work. Several variables contribute to radiation dose, but in this case, the most likely culprit is compression thickness, Dr. Wells said.
"It may be more difficult to adequately compress a large breast with a small detector, resulting in a larger radiation dose," she said. "We hope to analyze the data again, to answer this question."
Dr. Wells and her coauthors reported having no conflicts of interest.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Screening mammogram patients with correctly matched breast and detector sizes received an average mean glandular dose per breast of 3.3 mGy vs. 4.9 mGy for mismatched patients with large breasts (P value less than .05).
Data Source: Quality assurance study in 886 mammography patients.
Disclosures: Dr. Wells and her coauthors reported having no conflicts of interest.
Violent Video Games Alter Brain Activity
CHICAGO – One week of violent video game play produced significant changes in brain function, a small study of men aged 18-28 shows.
Violent video games were associated with reduced activity in regions of the brain involved in attention, inhibition, and monitoring of emotions, Dr. Vincent P. Mathews, of Indiana University reported.
The study is one of the first to document the effects of violent video games on brain activity, Dr. Mathews said in a press briefing at the annual meeting of the Radiological Society of North America.
Although numerous behavioral studies have shown a correlation between violent video games and increased aggression, few neuroimaging studies have been done, said Dr. Mathews, of the Northwest Radiology Network in Indianapolis. Gathering that neurophysiologic data is important, because researchers believe the active role-playing involved in violent video games might make them more harmful than violent television shows or movies, he said.
The detrimental effects of violent video games described in behavioral studies include desensitization to violence; observational learning, in which repeated exposure to violent behavior is rewarded and aggressive behavior becomes encoded as appropriate; an increasingly hostile view of the world; and behavioral and cognitive scripts that might counteract positive environmental influences and in which violence can come to be seen as acceptable or even necessary.
Recent work by Dr. Mathews and his colleagues demonstrated the short-term effects of violent video games on brain function in adolescents. Functional magnetic resonance imaging (fMRI) revealed decreased activity in areas of the brain involved in inhibition and attention after 30 minutes of game time.
"In this study we wanted to look at longer-term violent video game play and its potential to alter brain function," Dr. Mathews said.
For the study, 28 young men, none of whom were heavy video game players, were randomized to experimental and control groups. The groups did not differ significantly in age, IQ, or video game experience.
Subjects in the video game group were given a computer loaded with a first-person shooter video game (industry-rated for mature audiences) for home use and were asked to play the game 2 hours daily for 1 week, followed by 1 week of no game play. Subjects averaged a total of 10 hours of game time. The control group refrained from video games throughout the study period.
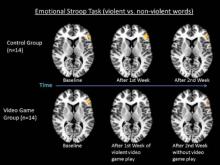
Functional MRI was performed on all subjects at baseline, 1 week, and 2 weeks. Subjects performed two Stroop psychological tests: an emotional task and a counting task. The emotional task required participants to name the color of words in a series, which included both neutral (run, walk) and emotional (hit, kill) words. Emotionally charged words have been shown to produce a subconscious interference effect that results in a delayed response.
The counting task required subjects to view number words (two, three) and respond with the number of visual stimuli presented, not the words themselves (for example, the correct response to the word "three" shown twice would be "two"). This task also is designed to produce an interference effect.
Dr. Mathews and his colleagues looked specifically at changes in the dorsolateral prefrontal cortex, the area of the brain known to be most highly activated by the interference effect and an area involved in emotional modulation and inhibition, and the anterior cingulate cortex, which is involved in attention.
Statistical maps showed that brain activation in these regions remained unchanged in the nongame group from baseline to week 1 and week 2. Brain activation in the video game group did not differ significantly from the nongame group at baseline.
However, activation decreased significantly in the video game group, compared with the nongame group, after 1 week of daily violent video game playing. Activation in this group returned almost to baseline at week 2 after 1 week of no game playing. Maps of brain activation also showed significant differences in the video game group between baseline and week 1 and between weeks 1 and 2.
"What we’re seeing is that there’s a decrease in normal blood flow to that area after a week of playing violent games," Dr. Mathews said.
"Because the groups were randomly assigned and didn’t have any significant differences in their demographics, the differences can be assumed to be a result of the violent video game playing," he said. "Our results may be an explanation for these behavioral studies that show increased aggressive behavior following violent video games. So this actually is a physiologic explanation for what others have previously measured in behavioral studies."
This study was supported by the Center for Successful Parenting, a group that seeks to help parents understand the consequences of "children watching video violence." Dr. Mathews had no disclosures.
attention, inhibition, monitoring of emotions, Dr. Vincent P. Mathews, brain activity, Radiological Society of North America, aggression, neuroimaging studies, neurophysiologic data, desensitization to violence,
CHICAGO – One week of violent video game play produced significant changes in brain function, a small study of men aged 18-28 shows.
Violent video games were associated with reduced activity in regions of the brain involved in attention, inhibition, and monitoring of emotions, Dr. Vincent P. Mathews, of Indiana University reported.
The study is one of the first to document the effects of violent video games on brain activity, Dr. Mathews said in a press briefing at the annual meeting of the Radiological Society of North America.
Although numerous behavioral studies have shown a correlation between violent video games and increased aggression, few neuroimaging studies have been done, said Dr. Mathews, of the Northwest Radiology Network in Indianapolis. Gathering that neurophysiologic data is important, because researchers believe the active role-playing involved in violent video games might make them more harmful than violent television shows or movies, he said.
The detrimental effects of violent video games described in behavioral studies include desensitization to violence; observational learning, in which repeated exposure to violent behavior is rewarded and aggressive behavior becomes encoded as appropriate; an increasingly hostile view of the world; and behavioral and cognitive scripts that might counteract positive environmental influences and in which violence can come to be seen as acceptable or even necessary.
Recent work by Dr. Mathews and his colleagues demonstrated the short-term effects of violent video games on brain function in adolescents. Functional magnetic resonance imaging (fMRI) revealed decreased activity in areas of the brain involved in inhibition and attention after 30 minutes of game time.
"In this study we wanted to look at longer-term violent video game play and its potential to alter brain function," Dr. Mathews said.
For the study, 28 young men, none of whom were heavy video game players, were randomized to experimental and control groups. The groups did not differ significantly in age, IQ, or video game experience.
Subjects in the video game group were given a computer loaded with a first-person shooter video game (industry-rated for mature audiences) for home use and were asked to play the game 2 hours daily for 1 week, followed by 1 week of no game play. Subjects averaged a total of 10 hours of game time. The control group refrained from video games throughout the study period.
Functional MRI was performed on all subjects at baseline, 1 week, and 2 weeks. Subjects performed two Stroop psychological tests: an emotional task and a counting task. The emotional task required participants to name the color of words in a series, which included both neutral (run, walk) and emotional (hit, kill) words. Emotionally charged words have been shown to produce a subconscious interference effect that results in a delayed response.
The counting task required subjects to view number words (two, three) and respond with the number of visual stimuli presented, not the words themselves (for example, the correct response to the word "three" shown twice would be "two"). This task also is designed to produce an interference effect.
Dr. Mathews and his colleagues looked specifically at changes in the dorsolateral prefrontal cortex, the area of the brain known to be most highly activated by the interference effect and an area involved in emotional modulation and inhibition, and the anterior cingulate cortex, which is involved in attention.
Statistical maps showed that brain activation in these regions remained unchanged in the nongame group from baseline to week 1 and week 2. Brain activation in the video game group did not differ significantly from the nongame group at baseline.
However, activation decreased significantly in the video game group, compared with the nongame group, after 1 week of daily violent video game playing. Activation in this group returned almost to baseline at week 2 after 1 week of no game playing. Maps of brain activation also showed significant differences in the video game group between baseline and week 1 and between weeks 1 and 2.
"What we’re seeing is that there’s a decrease in normal blood flow to that area after a week of playing violent games," Dr. Mathews said.
"Because the groups were randomly assigned and didn’t have any significant differences in their demographics, the differences can be assumed to be a result of the violent video game playing," he said. "Our results may be an explanation for these behavioral studies that show increased aggressive behavior following violent video games. So this actually is a physiologic explanation for what others have previously measured in behavioral studies."
This study was supported by the Center for Successful Parenting, a group that seeks to help parents understand the consequences of "children watching video violence." Dr. Mathews had no disclosures.
CHICAGO – One week of violent video game play produced significant changes in brain function, a small study of men aged 18-28 shows.
Violent video games were associated with reduced activity in regions of the brain involved in attention, inhibition, and monitoring of emotions, Dr. Vincent P. Mathews, of Indiana University reported.
The study is one of the first to document the effects of violent video games on brain activity, Dr. Mathews said in a press briefing at the annual meeting of the Radiological Society of North America.
Although numerous behavioral studies have shown a correlation between violent video games and increased aggression, few neuroimaging studies have been done, said Dr. Mathews, of the Northwest Radiology Network in Indianapolis. Gathering that neurophysiologic data is important, because researchers believe the active role-playing involved in violent video games might make them more harmful than violent television shows or movies, he said.
The detrimental effects of violent video games described in behavioral studies include desensitization to violence; observational learning, in which repeated exposure to violent behavior is rewarded and aggressive behavior becomes encoded as appropriate; an increasingly hostile view of the world; and behavioral and cognitive scripts that might counteract positive environmental influences and in which violence can come to be seen as acceptable or even necessary.
Recent work by Dr. Mathews and his colleagues demonstrated the short-term effects of violent video games on brain function in adolescents. Functional magnetic resonance imaging (fMRI) revealed decreased activity in areas of the brain involved in inhibition and attention after 30 minutes of game time.
"In this study we wanted to look at longer-term violent video game play and its potential to alter brain function," Dr. Mathews said.
For the study, 28 young men, none of whom were heavy video game players, were randomized to experimental and control groups. The groups did not differ significantly in age, IQ, or video game experience.
Subjects in the video game group were given a computer loaded with a first-person shooter video game (industry-rated for mature audiences) for home use and were asked to play the game 2 hours daily for 1 week, followed by 1 week of no game play. Subjects averaged a total of 10 hours of game time. The control group refrained from video games throughout the study period.
Functional MRI was performed on all subjects at baseline, 1 week, and 2 weeks. Subjects performed two Stroop psychological tests: an emotional task and a counting task. The emotional task required participants to name the color of words in a series, which included both neutral (run, walk) and emotional (hit, kill) words. Emotionally charged words have been shown to produce a subconscious interference effect that results in a delayed response.
The counting task required subjects to view number words (two, three) and respond with the number of visual stimuli presented, not the words themselves (for example, the correct response to the word "three" shown twice would be "two"). This task also is designed to produce an interference effect.
Dr. Mathews and his colleagues looked specifically at changes in the dorsolateral prefrontal cortex, the area of the brain known to be most highly activated by the interference effect and an area involved in emotional modulation and inhibition, and the anterior cingulate cortex, which is involved in attention.
Statistical maps showed that brain activation in these regions remained unchanged in the nongame group from baseline to week 1 and week 2. Brain activation in the video game group did not differ significantly from the nongame group at baseline.
However, activation decreased significantly in the video game group, compared with the nongame group, after 1 week of daily violent video game playing. Activation in this group returned almost to baseline at week 2 after 1 week of no game playing. Maps of brain activation also showed significant differences in the video game group between baseline and week 1 and between weeks 1 and 2.
"What we’re seeing is that there’s a decrease in normal blood flow to that area after a week of playing violent games," Dr. Mathews said.
"Because the groups were randomly assigned and didn’t have any significant differences in their demographics, the differences can be assumed to be a result of the violent video game playing," he said. "Our results may be an explanation for these behavioral studies that show increased aggressive behavior following violent video games. So this actually is a physiologic explanation for what others have previously measured in behavioral studies."
This study was supported by the Center for Successful Parenting, a group that seeks to help parents understand the consequences of "children watching video violence." Dr. Mathews had no disclosures.
attention, inhibition, monitoring of emotions, Dr. Vincent P. Mathews, brain activity, Radiological Society of North America, aggression, neuroimaging studies, neurophysiologic data, desensitization to violence,
attention, inhibition, monitoring of emotions, Dr. Vincent P. Mathews, brain activity, Radiological Society of North America, aggression, neuroimaging studies, neurophysiologic data, desensitization to violence,
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Brain activation decreased significantly in the video game group, compared to the nongame group, after 1 week of daily violent video game playing. Activation in this group returned almost to baseline at week 2 after 1 week of no game playing.
Data Source: Twenty-eight men aged 18-28 who were randomized to experimental and control groups.
Disclosures: The study was sponsored by the Center for Successful Parenting. Dr. Matthews had no disclosures.
Regular Fish Intake Lowers Dementia Risk
CHICAGO – Consumption of baked or broiled fish on a weekly basis improved brain health and significantly reduced the risk of mild cognitive impairment and Alzheimer’s disease in a 20-year longitudinal study of older adults presented at the annual meeting of the Radiological Society of North America.
Fish consumption improved brain volume in the frontal lobes, temporal lobes (including the hippocampus) and posterior cingulate gyrus, as shown on high-resolution, three-dimensional volumetric magnetic resonance imaging (MRI). "That’s important because these are areas of the brain that are responsible for memory and learning and are severely affected by Alzheimer’s disease," reported Dr. Cyrus A. Raji of the University of Pittsburgh.
Dr. Raji and his colleagues analyzed data collected at three time points from the ongoing Cardiovascular Health Study-Cognition Study. In 1989-1990, 260 subjects (mean age 71 years) completed standardized diet questionnaires. In 1998-1999, these individuals (mean age 78 years) underwent volumetric MRI.
An analysis of clinical conversion to mild cognitive impairment (MCI) or Alzheimer’s disease (AD) in 2002 among study participants (mean age 82 years) found that individuals with larger brain volumes as a result of weekly baked or broiled fish consumption had a greatly reduced incidence of MCI or AD, compared with individuals who did not eat fish regularly.
Clinical conversion rates to MCI or AD were 30.8% for non–fish eaters, compared with 8% for individuals whose brains benefited partially from fish consumption (as shown on volumetric MRI), and 3.2% for individuals whose brains benefited fully from fish consumption.
These findings indicate "a large reduction in the risk for developing AD or MCI as a result of consuming baked or broiled fish," Dr. Raji said
The benefits of regular fish intake persisted even after accounting for such potential confounding variables as age, gender, head size, and cerebrovascular disease.
Study participants who were not fish eaters and who showed atrophy in the hippocampus – the region most frequently affected by AD – had a 47% incidence of MCI or AD, compared with only 28% of fish eaters with larger hippocampal volumes, he reported.
In addition, mean scores on cognitive tests of working memory were significantly higher (P less than .05) in individuals who ate fish weekly compared with those who did not. The improvement remained even after accounting for potential confounders such as age, gender, and education.
The researchers also looked at cognitive test scores and brain volumes and found a relationship between larger frontal lobe volumes in fish eaters and higher working memory test scores. "This makes a lot of sense, because the frontal lobes are responsible for working memory function," Dr. Raji said.
The reduced risk of MCI and AD among fish eaters in this study probably stems from the protective benefits of omega-3 fatty acids, he noted. Omega-3 fatty acids are believed to increase blood flow to the brain, act as antioxidants and anti-inflammatories, and prevent the accumulation of the amyloid plaques characteristic of AD. Consumption of fried fish, which is high in cholesterol and low in omega-3 fatty acids, did not confer any benefits.
Data presented by Dr. Raji at last year’s meeting of the Radiological Society of North America (Internal Medicine News, Dec. 20, 2010) showed the protective benefits of physical activity in preserving brain volume and reducing the risk of AD and MCI in the same cohort. "What we’re adding to the picture this year is specific information on diet," he said. "The long-term goal of this research is to incorporate our understanding of all the various lifestyle factors that could reduce risk and give us a unified picture of how to best prevent the disease."
Dr. Raji had no disclosures related to this study.
CHICAGO – Consumption of baked or broiled fish on a weekly basis improved brain health and significantly reduced the risk of mild cognitive impairment and Alzheimer’s disease in a 20-year longitudinal study of older adults presented at the annual meeting of the Radiological Society of North America.
Fish consumption improved brain volume in the frontal lobes, temporal lobes (including the hippocampus) and posterior cingulate gyrus, as shown on high-resolution, three-dimensional volumetric magnetic resonance imaging (MRI). "That’s important because these are areas of the brain that are responsible for memory and learning and are severely affected by Alzheimer’s disease," reported Dr. Cyrus A. Raji of the University of Pittsburgh.
Dr. Raji and his colleagues analyzed data collected at three time points from the ongoing Cardiovascular Health Study-Cognition Study. In 1989-1990, 260 subjects (mean age 71 years) completed standardized diet questionnaires. In 1998-1999, these individuals (mean age 78 years) underwent volumetric MRI.
An analysis of clinical conversion to mild cognitive impairment (MCI) or Alzheimer’s disease (AD) in 2002 among study participants (mean age 82 years) found that individuals with larger brain volumes as a result of weekly baked or broiled fish consumption had a greatly reduced incidence of MCI or AD, compared with individuals who did not eat fish regularly.
Clinical conversion rates to MCI or AD were 30.8% for non–fish eaters, compared with 8% for individuals whose brains benefited partially from fish consumption (as shown on volumetric MRI), and 3.2% for individuals whose brains benefited fully from fish consumption.
These findings indicate "a large reduction in the risk for developing AD or MCI as a result of consuming baked or broiled fish," Dr. Raji said
The benefits of regular fish intake persisted even after accounting for such potential confounding variables as age, gender, head size, and cerebrovascular disease.
Study participants who were not fish eaters and who showed atrophy in the hippocampus – the region most frequently affected by AD – had a 47% incidence of MCI or AD, compared with only 28% of fish eaters with larger hippocampal volumes, he reported.
In addition, mean scores on cognitive tests of working memory were significantly higher (P less than .05) in individuals who ate fish weekly compared with those who did not. The improvement remained even after accounting for potential confounders such as age, gender, and education.
The researchers also looked at cognitive test scores and brain volumes and found a relationship between larger frontal lobe volumes in fish eaters and higher working memory test scores. "This makes a lot of sense, because the frontal lobes are responsible for working memory function," Dr. Raji said.
The reduced risk of MCI and AD among fish eaters in this study probably stems from the protective benefits of omega-3 fatty acids, he noted. Omega-3 fatty acids are believed to increase blood flow to the brain, act as antioxidants and anti-inflammatories, and prevent the accumulation of the amyloid plaques characteristic of AD. Consumption of fried fish, which is high in cholesterol and low in omega-3 fatty acids, did not confer any benefits.
Data presented by Dr. Raji at last year’s meeting of the Radiological Society of North America (Internal Medicine News, Dec. 20, 2010) showed the protective benefits of physical activity in preserving brain volume and reducing the risk of AD and MCI in the same cohort. "What we’re adding to the picture this year is specific information on diet," he said. "The long-term goal of this research is to incorporate our understanding of all the various lifestyle factors that could reduce risk and give us a unified picture of how to best prevent the disease."
Dr. Raji had no disclosures related to this study.
CHICAGO – Consumption of baked or broiled fish on a weekly basis improved brain health and significantly reduced the risk of mild cognitive impairment and Alzheimer’s disease in a 20-year longitudinal study of older adults presented at the annual meeting of the Radiological Society of North America.
Fish consumption improved brain volume in the frontal lobes, temporal lobes (including the hippocampus) and posterior cingulate gyrus, as shown on high-resolution, three-dimensional volumetric magnetic resonance imaging (MRI). "That’s important because these are areas of the brain that are responsible for memory and learning and are severely affected by Alzheimer’s disease," reported Dr. Cyrus A. Raji of the University of Pittsburgh.
Dr. Raji and his colleagues analyzed data collected at three time points from the ongoing Cardiovascular Health Study-Cognition Study. In 1989-1990, 260 subjects (mean age 71 years) completed standardized diet questionnaires. In 1998-1999, these individuals (mean age 78 years) underwent volumetric MRI.
An analysis of clinical conversion to mild cognitive impairment (MCI) or Alzheimer’s disease (AD) in 2002 among study participants (mean age 82 years) found that individuals with larger brain volumes as a result of weekly baked or broiled fish consumption had a greatly reduced incidence of MCI or AD, compared with individuals who did not eat fish regularly.
Clinical conversion rates to MCI or AD were 30.8% for non–fish eaters, compared with 8% for individuals whose brains benefited partially from fish consumption (as shown on volumetric MRI), and 3.2% for individuals whose brains benefited fully from fish consumption.
These findings indicate "a large reduction in the risk for developing AD or MCI as a result of consuming baked or broiled fish," Dr. Raji said
The benefits of regular fish intake persisted even after accounting for such potential confounding variables as age, gender, head size, and cerebrovascular disease.
Study participants who were not fish eaters and who showed atrophy in the hippocampus – the region most frequently affected by AD – had a 47% incidence of MCI or AD, compared with only 28% of fish eaters with larger hippocampal volumes, he reported.
In addition, mean scores on cognitive tests of working memory were significantly higher (P less than .05) in individuals who ate fish weekly compared with those who did not. The improvement remained even after accounting for potential confounders such as age, gender, and education.
The researchers also looked at cognitive test scores and brain volumes and found a relationship between larger frontal lobe volumes in fish eaters and higher working memory test scores. "This makes a lot of sense, because the frontal lobes are responsible for working memory function," Dr. Raji said.
The reduced risk of MCI and AD among fish eaters in this study probably stems from the protective benefits of omega-3 fatty acids, he noted. Omega-3 fatty acids are believed to increase blood flow to the brain, act as antioxidants and anti-inflammatories, and prevent the accumulation of the amyloid plaques characteristic of AD. Consumption of fried fish, which is high in cholesterol and low in omega-3 fatty acids, did not confer any benefits.
Data presented by Dr. Raji at last year’s meeting of the Radiological Society of North America (Internal Medicine News, Dec. 20, 2010) showed the protective benefits of physical activity in preserving brain volume and reducing the risk of AD and MCI in the same cohort. "What we’re adding to the picture this year is specific information on diet," he said. "The long-term goal of this research is to incorporate our understanding of all the various lifestyle factors that could reduce risk and give us a unified picture of how to best prevent the disease."
Dr. Raji had no disclosures related to this study.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Eating baked or broiled fish on a weekly basis improved brain health and significantly reduced the risk of mild cognitive impairment and Alzheimer’s disease.
Data Source: A 20-year longitudinal study of older adults.
Disclosures: Dr. Raji had no disclosures related to this study.
Growth Hormone Strengthens Bone in Obese Women
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in a press briefing at the annual meeting of the Radiological Society of North America.
The study builds on work presented by Dr. Bredella at last year’s RSNA meeting showing an association between abdominal obesity and low bone mineral density in women. That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella’s work zeroed in on visceral fat.
In the present study, 79 women (mean age, 36 years; mean BMI, 35 kg/m2) with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months. Subjects were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between –2.5 and –1) at baseline and that one had developed osteoporosis (T-score below –2.5). "It’s important that people become aware that obesity doesn’t protect against bone loss," she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation. Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
"Overall, our patients didn’t lose weight, but they had a redistribution of their body fat and muscle mass," Dr. Bredella noted. "They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight didn’t change."
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities. "It’s not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease, and it could be used in the aging population because we know as we get older our growth hormone levels go down," she said.
Dr. Bredella had no disclosures related to this study.
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in a press briefing at the annual meeting of the Radiological Society of North America.
The study builds on work presented by Dr. Bredella at last year’s RSNA meeting showing an association between abdominal obesity and low bone mineral density in women. That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella’s work zeroed in on visceral fat.
In the present study, 79 women (mean age, 36 years; mean BMI, 35 kg/m2) with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months. Subjects were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between –2.5 and –1) at baseline and that one had developed osteoporosis (T-score below –2.5). "It’s important that people become aware that obesity doesn’t protect against bone loss," she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation. Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
"Overall, our patients didn’t lose weight, but they had a redistribution of their body fat and muscle mass," Dr. Bredella noted. "They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight didn’t change."
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities. "It’s not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease, and it could be used in the aging population because we know as we get older our growth hormone levels go down," she said.
Dr. Bredella had no disclosures related to this study.
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in a press briefing at the annual meeting of the Radiological Society of North America.
The study builds on work presented by Dr. Bredella at last year’s RSNA meeting showing an association between abdominal obesity and low bone mineral density in women. That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella’s work zeroed in on visceral fat.
In the present study, 79 women (mean age, 36 years; mean BMI, 35 kg/m2) with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months. Subjects were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between –2.5 and –1) at baseline and that one had developed osteoporosis (T-score below –2.5). "It’s important that people become aware that obesity doesn’t protect against bone loss," she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation. Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
"Overall, our patients didn’t lose weight, but they had a redistribution of their body fat and muscle mass," Dr. Bredella noted. "They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight didn’t change."
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities. "It’s not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease, and it could be used in the aging population because we know as we get older our growth hormone levels go down," she said.
Dr. Bredella had no disclosures related to this study.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of abdominally obese women.
Data Source: A total of 79 women with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months.
Disclosures: Dr. Bredella had no disclosures related to this study.
Mammography: Family History Data Support Yearly Screening
CHICAGO – Women aged 40-49 years with and without a family history of breast cancer had virtually the same rates of invasive disease in a retrospective analysis of data on more than 1,000 patients diagnosed over a 10-year period at a single site.
The finding adds weight to the American Cancer Society’s recommendation in favor of annual screening mammograms for women beginning at age 40, said principal author Dr. Stamatia V. Destounis of Elizabeth Wende Breast Care LLC in Rochester, N.Y. Dr. Destounis presented the results of her study in a press briefing at the annual meeting of the Radiological Society of North America.
A study presented at last year’s meeting by researchers at the London Breast Institute of the Princess Grace Hospital indicated that annual mammograms could reduce by half the risk of mastectomy in women who were diagnosed with breast cancer between the ages of 40 and 50 years.
Both studies challenge the recommendation against routine annual mammography for women under the age of 50 made in 2009 by the United States Preventive Services Task Force.
"These conflicting recommendations have led to confusion among patients and physicians," Dr. Destounis said.
In the present study, Dr. Destounis and her colleagues analyzed data on women between the ages of 40 and 49 years who underwent screening mammography at the center between 2000 and 2010.
In all, 1,116 cancers were found in 1,071 patients aged 40-49 years. Of these patients, 373 were diagnosed by screening mammography. Of these 373 women, 144 (39%) had a family history of breast cancer, 228 (61%) did not, and 1 patient did not know her family history. (A total of 7 patients with and 16 patients without a family history of breast cancer also had a personal history of breast cancer.)
Among women with a family history, 32% (46) had a first-degree relative with a premenopausal history, 38% (54) had a first-degree relative with a postmenopausal history, and 31% (44) had a second- or third-degree relative with a pre- or postmenopausal history of the disease.
The incidence of invasive breast cancer was virtually the same – 63% (91) and 64% (146), respectively – in women with and without a family history. The incidence of noninvasive disease in the two groups was also similar, at 37% and 36%, respectively. Those with and without a family history shared similar rates of lymph node metastatic disease (31% and 29%) as well.
"Family history does not seem to [affect] the rate of invasive disease in our patient cohort," Dr. Destounis said.
The following types of lesions were found in women with and without a family history, respectively: mass (42, 86), microcalcification (69, 97), mass with calcification (21, 18), architectural distortion (11, 18), and asymmetry (1, 9).
All 144 patients with a family history and 227 of 228 patients in the no family history group proceeded to surgery. One patient had metastatic disease and opted for no surgery or treatment.
Among women with and without a family history, 63% and 68%, respectively, underwent a lumpectomy. Some of these patients did not have clear margins after surgery and went on to mastectomy. In all, 38% (54) of women with a family history and 31% (71) women without a family history went on to mastectomy.
Since no difference in the rate of invasive breast cancer between women with and without a family history was found in this population, "the recommendation should be that women in their 40s have a screening mammogram yearly," she said.
Dr. Destounis and her colleagues are currently collecting additional data on breast density, demographics, and survival rates for this patient group.
Dr. Destounis disclosed that she has been an investigator for Siemens AG, Fujifilm Holdings, Hologic Inc., and Koning Corp. She has also served as an advisory board member for Philips Electronics and Matakina International Ltd.
CHICAGO – Women aged 40-49 years with and without a family history of breast cancer had virtually the same rates of invasive disease in a retrospective analysis of data on more than 1,000 patients diagnosed over a 10-year period at a single site.
The finding adds weight to the American Cancer Society’s recommendation in favor of annual screening mammograms for women beginning at age 40, said principal author Dr. Stamatia V. Destounis of Elizabeth Wende Breast Care LLC in Rochester, N.Y. Dr. Destounis presented the results of her study in a press briefing at the annual meeting of the Radiological Society of North America.
A study presented at last year’s meeting by researchers at the London Breast Institute of the Princess Grace Hospital indicated that annual mammograms could reduce by half the risk of mastectomy in women who were diagnosed with breast cancer between the ages of 40 and 50 years.
Both studies challenge the recommendation against routine annual mammography for women under the age of 50 made in 2009 by the United States Preventive Services Task Force.
"These conflicting recommendations have led to confusion among patients and physicians," Dr. Destounis said.
In the present study, Dr. Destounis and her colleagues analyzed data on women between the ages of 40 and 49 years who underwent screening mammography at the center between 2000 and 2010.
In all, 1,116 cancers were found in 1,071 patients aged 40-49 years. Of these patients, 373 were diagnosed by screening mammography. Of these 373 women, 144 (39%) had a family history of breast cancer, 228 (61%) did not, and 1 patient did not know her family history. (A total of 7 patients with and 16 patients without a family history of breast cancer also had a personal history of breast cancer.)
Among women with a family history, 32% (46) had a first-degree relative with a premenopausal history, 38% (54) had a first-degree relative with a postmenopausal history, and 31% (44) had a second- or third-degree relative with a pre- or postmenopausal history of the disease.
The incidence of invasive breast cancer was virtually the same – 63% (91) and 64% (146), respectively – in women with and without a family history. The incidence of noninvasive disease in the two groups was also similar, at 37% and 36%, respectively. Those with and without a family history shared similar rates of lymph node metastatic disease (31% and 29%) as well.
"Family history does not seem to [affect] the rate of invasive disease in our patient cohort," Dr. Destounis said.
The following types of lesions were found in women with and without a family history, respectively: mass (42, 86), microcalcification (69, 97), mass with calcification (21, 18), architectural distortion (11, 18), and asymmetry (1, 9).
All 144 patients with a family history and 227 of 228 patients in the no family history group proceeded to surgery. One patient had metastatic disease and opted for no surgery or treatment.
Among women with and without a family history, 63% and 68%, respectively, underwent a lumpectomy. Some of these patients did not have clear margins after surgery and went on to mastectomy. In all, 38% (54) of women with a family history and 31% (71) women without a family history went on to mastectomy.
Since no difference in the rate of invasive breast cancer between women with and without a family history was found in this population, "the recommendation should be that women in their 40s have a screening mammogram yearly," she said.
Dr. Destounis and her colleagues are currently collecting additional data on breast density, demographics, and survival rates for this patient group.
Dr. Destounis disclosed that she has been an investigator for Siemens AG, Fujifilm Holdings, Hologic Inc., and Koning Corp. She has also served as an advisory board member for Philips Electronics and Matakina International Ltd.
CHICAGO – Women aged 40-49 years with and without a family history of breast cancer had virtually the same rates of invasive disease in a retrospective analysis of data on more than 1,000 patients diagnosed over a 10-year period at a single site.
The finding adds weight to the American Cancer Society’s recommendation in favor of annual screening mammograms for women beginning at age 40, said principal author Dr. Stamatia V. Destounis of Elizabeth Wende Breast Care LLC in Rochester, N.Y. Dr. Destounis presented the results of her study in a press briefing at the annual meeting of the Radiological Society of North America.
A study presented at last year’s meeting by researchers at the London Breast Institute of the Princess Grace Hospital indicated that annual mammograms could reduce by half the risk of mastectomy in women who were diagnosed with breast cancer between the ages of 40 and 50 years.
Both studies challenge the recommendation against routine annual mammography for women under the age of 50 made in 2009 by the United States Preventive Services Task Force.
"These conflicting recommendations have led to confusion among patients and physicians," Dr. Destounis said.
In the present study, Dr. Destounis and her colleagues analyzed data on women between the ages of 40 and 49 years who underwent screening mammography at the center between 2000 and 2010.
In all, 1,116 cancers were found in 1,071 patients aged 40-49 years. Of these patients, 373 were diagnosed by screening mammography. Of these 373 women, 144 (39%) had a family history of breast cancer, 228 (61%) did not, and 1 patient did not know her family history. (A total of 7 patients with and 16 patients without a family history of breast cancer also had a personal history of breast cancer.)
Among women with a family history, 32% (46) had a first-degree relative with a premenopausal history, 38% (54) had a first-degree relative with a postmenopausal history, and 31% (44) had a second- or third-degree relative with a pre- or postmenopausal history of the disease.
The incidence of invasive breast cancer was virtually the same – 63% (91) and 64% (146), respectively – in women with and without a family history. The incidence of noninvasive disease in the two groups was also similar, at 37% and 36%, respectively. Those with and without a family history shared similar rates of lymph node metastatic disease (31% and 29%) as well.
"Family history does not seem to [affect] the rate of invasive disease in our patient cohort," Dr. Destounis said.
The following types of lesions were found in women with and without a family history, respectively: mass (42, 86), microcalcification (69, 97), mass with calcification (21, 18), architectural distortion (11, 18), and asymmetry (1, 9).
All 144 patients with a family history and 227 of 228 patients in the no family history group proceeded to surgery. One patient had metastatic disease and opted for no surgery or treatment.
Among women with and without a family history, 63% and 68%, respectively, underwent a lumpectomy. Some of these patients did not have clear margins after surgery and went on to mastectomy. In all, 38% (54) of women with a family history and 31% (71) women without a family history went on to mastectomy.
Since no difference in the rate of invasive breast cancer between women with and without a family history was found in this population, "the recommendation should be that women in their 40s have a screening mammogram yearly," she said.
Dr. Destounis and her colleagues are currently collecting additional data on breast density, demographics, and survival rates for this patient group.
Dr. Destounis disclosed that she has been an investigator for Siemens AG, Fujifilm Holdings, Hologic Inc., and Koning Corp. She has also served as an advisory board member for Philips Electronics and Matakina International Ltd.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Women aged 40-49 years with and without a family history of breast cancer had virtually the same rates of invasive disease in a retrospective analysis of data on more than 1,000 patients diagnosed over a 10-year period at a single site.
Data Source: Data analysis of women between the ages of 40 and 49 years who underwent screening mammography at a single site between 2000 and 2010.
Disclosures: Dr. Destounis disclosed that she has been an investigator for Siemens AG, Fujifilm Holdings, Hologic, and Koning. She has also served as an advisory board member for Philips Electronics and Matakina International Limited.
Diabetes: Calorie Restriction Yields Lasting Cardiac Benefit
CHICAGO – Four months of a restricted-calorie diet produced lasting reductions in pericardial fat and improvements in left ventricular diastolic function in a study of obese adults with type 2 diabetes.
The diet eliminated insulin dependence in all patients during treatment. After returning to a normal diet, approximately 75% of patients remained insulin-free at 18 months, reported Dr. Sebastiaan Hammer of Leiden (the Netherlands) University Medical Center.
The finding underscores the value of lifestyle interventions as a tool for diabetes management, Dr. Hammer said in a press briefing at the annual meeting of the Radiological Society of North America.
The reductions in pericardial fat also persisted at 18 months from baseline – more than a year after patients had resumed their normal eating habits, Dr. Hammer said. These improvements were sustained even in patients who regained weight that had been lost during the 4-month period of caloric restriction.
Dr. Hammer and his colleagues analyzed changes in cardiac function, pericardial fat, and body mass index (BMI) using cardiac magnetic resonance imaging (MRI) in eight men and seven women with obesity-related type 2 diabetes. At the beginning of the study, all patients had a BMI greater than 30 kg/m2, were being treated with insulin, and had no cardiac complaints.
Insulin treatment was stopped at baseline. Patients consumed a standardized, low-carbohydrate, 500 calorie/day diet for 4 months and were monitored weekly for blood glucose and weight loss. At months 4 through 6, patients were gradually reintroduced to normal caloric intake. For the following 12 months, patients received treatment by their own physicians. Dr. Hammer and his colleagues performed cardiac MRI on all patients at baseline, 4 months, and 18 months.
Caloric restriction resulted in a decrease in mean BMI from 35.3 to 27.5 over 4 months. Pericardial fat decreased from a mean of 39 mL to 31 mL. The researchers also quantified the elasticity of the left ventricle by quantifying blood flow across the valve between the left atrium and the left ventricle, using the ratio between the early filling phase (vessel filling phase) and the atrial filling phase as a measure of diastolic heart function. The mean E/A ratio improved from 0.96 to 1.2.
At 14 months of follow-up on a regular diet (18 months from baseline), mean BMI increased to 31.7 (P less than .05). However, despite this weight gain, improvements in pericardial fat levels (32 mL, P less than .05) and E/A ratios (mean 1.06, P less than .05) persisted.
Dr. Hammer noted recent findings that "the fat around the heart is not an inert adipose tissue compartment, but it is metabolically active, it is associated with coronary plaque formation, and it may be associated with cardiac dysfunction in patients with diabetes." Pericardial fat shows promise as a marker for cardiac risk in patients with type 2 diabetes because it can be quantified using standard MRI, he said.
Although the patients in this study were obese and insulin dependent at baseline, none had cardiac disease, kidney disease, or other diabetic complications. "We are also testing if this strategy works in patients who do have some cardiac complaints," Dr. Hammer said. "It would also be good to know if this strategy is safe to use in those patients."
Dr. Hammer had no financial disclosures related to this study.
CHICAGO – Four months of a restricted-calorie diet produced lasting reductions in pericardial fat and improvements in left ventricular diastolic function in a study of obese adults with type 2 diabetes.
The diet eliminated insulin dependence in all patients during treatment. After returning to a normal diet, approximately 75% of patients remained insulin-free at 18 months, reported Dr. Sebastiaan Hammer of Leiden (the Netherlands) University Medical Center.
The finding underscores the value of lifestyle interventions as a tool for diabetes management, Dr. Hammer said in a press briefing at the annual meeting of the Radiological Society of North America.
The reductions in pericardial fat also persisted at 18 months from baseline – more than a year after patients had resumed their normal eating habits, Dr. Hammer said. These improvements were sustained even in patients who regained weight that had been lost during the 4-month period of caloric restriction.
Dr. Hammer and his colleagues analyzed changes in cardiac function, pericardial fat, and body mass index (BMI) using cardiac magnetic resonance imaging (MRI) in eight men and seven women with obesity-related type 2 diabetes. At the beginning of the study, all patients had a BMI greater than 30 kg/m2, were being treated with insulin, and had no cardiac complaints.
Insulin treatment was stopped at baseline. Patients consumed a standardized, low-carbohydrate, 500 calorie/day diet for 4 months and were monitored weekly for blood glucose and weight loss. At months 4 through 6, patients were gradually reintroduced to normal caloric intake. For the following 12 months, patients received treatment by their own physicians. Dr. Hammer and his colleagues performed cardiac MRI on all patients at baseline, 4 months, and 18 months.
Caloric restriction resulted in a decrease in mean BMI from 35.3 to 27.5 over 4 months. Pericardial fat decreased from a mean of 39 mL to 31 mL. The researchers also quantified the elasticity of the left ventricle by quantifying blood flow across the valve between the left atrium and the left ventricle, using the ratio between the early filling phase (vessel filling phase) and the atrial filling phase as a measure of diastolic heart function. The mean E/A ratio improved from 0.96 to 1.2.
At 14 months of follow-up on a regular diet (18 months from baseline), mean BMI increased to 31.7 (P less than .05). However, despite this weight gain, improvements in pericardial fat levels (32 mL, P less than .05) and E/A ratios (mean 1.06, P less than .05) persisted.
Dr. Hammer noted recent findings that "the fat around the heart is not an inert adipose tissue compartment, but it is metabolically active, it is associated with coronary plaque formation, and it may be associated with cardiac dysfunction in patients with diabetes." Pericardial fat shows promise as a marker for cardiac risk in patients with type 2 diabetes because it can be quantified using standard MRI, he said.
Although the patients in this study were obese and insulin dependent at baseline, none had cardiac disease, kidney disease, or other diabetic complications. "We are also testing if this strategy works in patients who do have some cardiac complaints," Dr. Hammer said. "It would also be good to know if this strategy is safe to use in those patients."
Dr. Hammer had no financial disclosures related to this study.
CHICAGO – Four months of a restricted-calorie diet produced lasting reductions in pericardial fat and improvements in left ventricular diastolic function in a study of obese adults with type 2 diabetes.
The diet eliminated insulin dependence in all patients during treatment. After returning to a normal diet, approximately 75% of patients remained insulin-free at 18 months, reported Dr. Sebastiaan Hammer of Leiden (the Netherlands) University Medical Center.
The finding underscores the value of lifestyle interventions as a tool for diabetes management, Dr. Hammer said in a press briefing at the annual meeting of the Radiological Society of North America.
The reductions in pericardial fat also persisted at 18 months from baseline – more than a year after patients had resumed their normal eating habits, Dr. Hammer said. These improvements were sustained even in patients who regained weight that had been lost during the 4-month period of caloric restriction.
Dr. Hammer and his colleagues analyzed changes in cardiac function, pericardial fat, and body mass index (BMI) using cardiac magnetic resonance imaging (MRI) in eight men and seven women with obesity-related type 2 diabetes. At the beginning of the study, all patients had a BMI greater than 30 kg/m2, were being treated with insulin, and had no cardiac complaints.
Insulin treatment was stopped at baseline. Patients consumed a standardized, low-carbohydrate, 500 calorie/day diet for 4 months and were monitored weekly for blood glucose and weight loss. At months 4 through 6, patients were gradually reintroduced to normal caloric intake. For the following 12 months, patients received treatment by their own physicians. Dr. Hammer and his colleagues performed cardiac MRI on all patients at baseline, 4 months, and 18 months.
Caloric restriction resulted in a decrease in mean BMI from 35.3 to 27.5 over 4 months. Pericardial fat decreased from a mean of 39 mL to 31 mL. The researchers also quantified the elasticity of the left ventricle by quantifying blood flow across the valve between the left atrium and the left ventricle, using the ratio between the early filling phase (vessel filling phase) and the atrial filling phase as a measure of diastolic heart function. The mean E/A ratio improved from 0.96 to 1.2.
At 14 months of follow-up on a regular diet (18 months from baseline), mean BMI increased to 31.7 (P less than .05). However, despite this weight gain, improvements in pericardial fat levels (32 mL, P less than .05) and E/A ratios (mean 1.06, P less than .05) persisted.
Dr. Hammer noted recent findings that "the fat around the heart is not an inert adipose tissue compartment, but it is metabolically active, it is associated with coronary plaque formation, and it may be associated with cardiac dysfunction in patients with diabetes." Pericardial fat shows promise as a marker for cardiac risk in patients with type 2 diabetes because it can be quantified using standard MRI, he said.
Although the patients in this study were obese and insulin dependent at baseline, none had cardiac disease, kidney disease, or other diabetic complications. "We are also testing if this strategy works in patients who do have some cardiac complaints," Dr. Hammer said. "It would also be good to know if this strategy is safe to use in those patients."
Dr. Hammer had no financial disclosures related to this study.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Four months of a restricted-calorie diet produced lasting reductions in pericardial fat and improvements in left ventricular diastolic function in a study of obese adults with type 2 diabetes.
Data Source: Investigators analyzed changes in cardiac function, pericardial fat, and BMI using cardiac MRI in eight men and seven women with obesity-related type 2 diabetes. At the beginning of the study, all patients had a BMI greater than 30 kg/m2, were being treated with insulin, and had no cardiac complaints.
Disclosures: Dr. Hammer had no financial disclosures related to this study.