User login
The epidemic of opioid abuse, addiction, and overdose deaths across the U.S. has not forgone the reservations of American Indian/Alaska Native (AI/AN) tribes. Indeed, AI/ANs may be at increased risk for abuse of prescription opioids due to higher rates of reported illicit drug use and misuse of opioids. According to the 2012 National Survey on Drug Use and Mental Health, AI/ANs aged ≥ 12 years had the highest rates of illicit drug use (12.7%) with the national average being only 9.5%.1 In 2009, AI/ANs aged 12 to 17 years were found to have the highest rates of marijuana use (13.8%) and nonmedical prescription drug abuse (6.1%) compared with the overall U.S. averages of 6.9% and 3.3%, respectively, putting them at an increased risk for an opioid overdose.1,2
In 2010, the American Pain Society conducted a survey establishing that about 41% of American adults reported having chronic, recurrent, or long-lasting pain.3 People of AI/AN heritage may experience chronic pain at higher rates, as they were identified as having the greatest incidence rates of low back pain (35%), arthritis (25%), and obesity (40%), which are often significant contributing factors to chronic pain.4-6
These conditions suggest a need for intensified management of chronic pain among IHS patients. The authors’ IHS facility is a closed health-system network where pharmacists are integral components of the health care team throughout the ambulatory care, emergency, and inpatient departments.
Related: Pharmacist Pain E-Consults That Result in a Therapy Change
Given that medications play a central role in the treatment of chronic pain, pharmacists are appropriate leaders for chronic pain management teams. Pharmacists can improve patient outcomes by conducting pain assessments, managing adverse events (AEs), identifying optimal medication choices, determining equianalgesic dosing, and managing care through care protocols.7
The primary objective of the multidisciplinary chronic pain management clinic (MCPMC) is to manage complicated and postsurgical patients, using a multimodal approach. Primary care providers (PCPs), which include physicians, nurse practitioners (NPs), physician assistants (PAs), and pharmacist providers collaborate to meet this goal by minimizing disease progression, preserving activities of daily living (ADL), maintaing employment, preventing an increase in pain, using treatment plans that include pharmacologic, interventional, and complementary components, decreasing emergency department (ED) visits for chronic pain issues, improving pain agreement adherence, managing AEs, performing drug abuse and diversion surveillance, and using sustained-release (SR) opioids when appropriate. Sustained release opioids not only ease dosing schedules and increase adherence, but also improve sleep, functionality, and quality of life (QOL) for chronic pain patients.8
Methods
The MCPMC began enrolling patients in January 2011 and has continued to date. Inclusion criterion is the presence of pain lasting 3 months or more. Exclusionary criteria are the presence of malignant pain, aged < 18 years, pregnancy, unmanaged psychiatric disorders, and a referral not approved by a PCP. Referrals are accepted from providers throughout the facility, including the ED, which then require approval by the PCP before enrollment. The PCP continues to manage these patients through consultations with the MCPMC pharmacists following MCPMC appointments and at separate ambulatory care clinic appointments.
Currently, there are 2 pharmacists practicing in the MCPMC clinic in conjunction with other health care providers, including 5 physical therapists, 1 psychiatrist, 2 clinical social workers, and 15 PCPs, including NPs and PAs. Additionally in 2014, the clinic became a yearlong rotation in the PGY-1 pharmacy practice residency.
Related: Evaluation of Methadone-Induced QTc Prolongation in a Veteran Population
After enrollment, a pharmacist reviews patients’ health records for past pain medications, interventional and complementary treatments, adherence to these treatments, recent ED visits and medications received, urine toxicology results, adherence to pain agreements, and the Arizona Controlled Substances Prescription Monitoring Program Database (ACSPMPD).
During the initial MCPMC appointment, a pain assessment questionnaire (PAQ) is completed with a MCPMC pharmacist. The questionnaire, designed specifically for the MCPMC, consists of a comprehensive pain assessment, including functional status and common comorbidities, such as anxiety, depression, obesity, and insomnia. Patients provide feedback on efficacy of past or current medications, and interventional and complementary treatments if applicable. Patients also rate their satisfaction with health care received and develop goals for their treatment and overall health.
A collaborative treatment plan is then developed with the patient’s PCP. Treatment plans often consist of increasing or starting interventional and complementary treatments, SR opioids, and adjuvant medications. Common adjuvant medications include nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, antiepileptics, immunosuppressants, disease-modifying antirheumatic drugs (DMARDs), and topical agents. To maximize benefits of the medications, antidepressants are often prescribed for dual purposes among patients with comorbid conditions, such as anxiety, depression, and insomnia. Among obese patients, weight loss is encouraged, and patients may be referred to dietary counseling and exercise programs. Other intentions of the treatment plans are to decrease breakthrough pain and ED visits while attempting to decrease the use of immediate-release (IR) opioids. Treatment plans are executed in a stepwise approach over multiple MCPMC visits and may be modified throughout the course of the program.
To ensure that medication changes and other issues can be addressed when a prescriber is available, all subsequent visits are scheduled when patients are due for a pain medication refill. The MCPMC pharmacists chose not to pursue prescriptive authority but have privileges to order urine toxicology tests, make nonformulary requests, and refer patients for complementary treatments. Subsequent appointments are commonly scheduled 1 to 4 weeks apart or alternate with PCP appointments.
Related: Multidisciplinary Approach to Back Pain
During each appointment, data are collected to record changes in therapy and pain levels. Questions regarding general health and adherence to pharmacologic, interventional, and complementary treatments, exercise regimens, and specialty referrals are asked of all patients. Additionally, follow-up PAQs are completed every 6 months to track progress in therapy, pain control, treatment plan adherence, and patient satisfaction. To determine pain agreement adherence, the ACSPMPD is reviewed monthly, and urine toxicology tests and pill counts are performed randomly at MCPMC visits.
In October 2013, all PCPs who had patients in the clinic completed a survey to assess their perception of the MCPMC. Questions were related to their satisfaction with the clinic as well as their opinion of patients’ satisfaction. Other questions were related to their view of patient care and outcomes compared with those of the general chronic pain patients at the facility.
Results
As of January 2013, 106 patients had been referred to the MCPMC by 17 PCPs. Thirty-six of these patients were still actively participating in the clinic, while 25 were pending review. Of the remaining 45 patients, 30 were denied initial enrollment, and 15 were disenrolled from the clinic over the previous 2 years. Patients were determined to be inappropriate candidates and not enrolled in the clinic for the following reasons: referral not approved by the PCP, patient refused care, patient had not established care with a PCP, mental health issues, pediatric patient, oncology patient, and death prior to the initial review. Patients were disenrolled from the MCPMC clinic before 2013 for the following reasons: not participating in their treatment plan, illicit drug use, seeking care from other PCPs, suspected diversion, death due to a nonpain-related issue, and remained stable on the medication regimen and were released back to the care of their PCP.
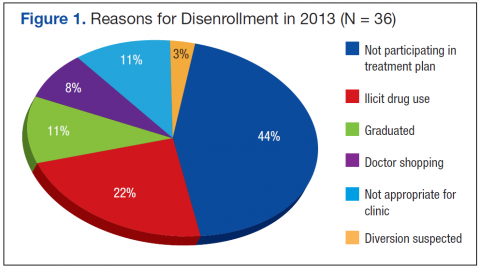
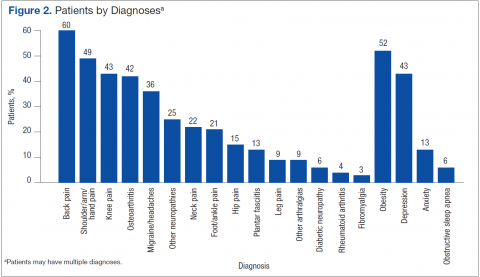
In 2013, there were 47 new referrals to the MCPMC, resulting in a total of 153 referrals since the clinic’s 2011 inception. Over the course of 2013, 31 new patients were enrolled, 32 referrals were denied (15 of which remained from 2012), and 36 patients were disenrolled (Figure 1). At the end of 2013, 31 patients remained active, while 9 referrals remained pending review. A total of 67 patients participated in the MCPMC at some point during 2013 and were included in the data collection. Patients by diagnoses are displayed in Figure 2.
In 2013, patients were scheduled for a total of 337 MCPMC appointments, and 298 (88%) were completed by patients, a 17% increase above 2012. The mean show rate of PCP ambulatory care clinic appointments was about 70%. The completed MCPMC visits for 2013 correlates to about 6.8 MCPMC visits annually per patient. Of the 67 patients included in data collection, the mean total number of months active in the clinic was 12.5. The mean number of months active in the clinic in 2013 was 6.9.
Pain Assessment Questionnaire
In 2013, 27 patients (40%) were enrolled in the clinic for 6 months or more and completed a follow-up PAQ. Throughout 2013, MCPMC patients presented to the ED for care 76 times, which correlates to about 1.8 ED visits annually per patient. MCPMC patients also attended an appointment with their PCP on average 3.7 times per year and provided urine toxicology tests on average 4.3 times per year between MCPMC and PCP visits.
Data collected from follow-up PAQs in January 2014 provided information on the 27 MCPMC patients enrolled in the clinic for 6 months or more. This review indicated alterations in patients’ reported pain levels, functional status, patient satisfaction, and adherence to pain agreements from before and after enrollment in the clinic. Additional information was collected using the electronic health record to reveal the adjustments in treatment plans, including pharmacologic, complementary, and interventional treatments, along with adherence to these treatments.
Patients’ self-reported pain levels at the time of appointment and average pain levels since the previous appointment were documented at each visit for the 27 MCPMC patients. These 2 pain levels were then compared with the levels of the initial assessment and the most recent appointment. Results were inconsistent; however, slight trends were observed with the analysis. The mean change in pain reported at the time of assessment decreased 5.1%. The mean change in average reported pain since the previous appointment also decreased 6.9%. Statistical analysis was performed using the Wilcoxon signed rank test. Both decreases in reported pain were not clinically or statistically significant (P = .21 and P = .17, respectively). Eleven (41%) patients had improvement in average pain, whereas 10 (37%) had no change, and 6 (22%) reported increased average pain levels.
Data on alterations in functional status and ADL were also collected from the 27 MCPMC patients. These patients reported the perceived degree of difficulty, on a scale of 1 to 5, required to complete tasks and get through their day. A rating of 1 represented the ability to complete activities with no difficulty, whereas 5 represented an inability to complete the tasks. For each of the 19 tasks, the differences in scores from the initial to the most recent PAQs were recorded as either a positive or negative alteration for each patient, and the sum of these differences was recorded as an overall positive or negative change in function. A positive change in function indicated an improvement in function, whereas an overall negative change indicated a decrease in ability to complete daily activities.
Twenty-six percent of the 27 pa-tients had a cumulative positive change of up to 5 points, and 19% had a positive change of 6 or more points. Alternatively, 22% of patients had a cumulative negative change of up to 5 points, and 33% of patients had a negative change of 6 points or more. The greatest positive change was 15 points, the greatest negative change was 28 points, and the median change from the initial to the most recent assessments was a negative change of 2 points.
Adjuvant Medications
The pharmacologic component of the treatment plans consisted primarily of optimizing the use of adjuvant medications and SR opioids when appropriate, while minimizing the use of IR opioids and other controlled medications. Of the 67 MCPMC patients in 2013, 55% were on IR opioids alone, a slight increase from 46% in 2012 (Table 1). Eighty-one percent of patients in this group were on ≤ 15 mg of morphine equivalent daily dose (MEDD), which would have required at least a doubling of their dose to initiate the preferred formulary SR opioid, morphine SR tablets. Six percent of patients were on SR opioids alone, also a slight increase from 3% in 2012. Twenty-seven percent of patients were prescribed a combination of IR and SR opioids. Nine percent of patients had been recently transitioned to SR opioids while in the MCPMC, of which 1 patient was prescribed the medication as monotherapy. Twelve percent of patients were not on any opioid therapy throughout 2013.
Opioids were switched to an alternative opioid at some point during the year to minimize tolerance in 15% of patients, of which 9% were IR and 6% were SR opioids. Changes in opioid therapy from the beginning to the end of the year were recorded as a decrease, increase, or no change in MEDD. Doses were decreased for 16%, increased for 27%, and not changed for the remaining 45% of patients. The sum of these changes for the 59 patients on opioids was a decrease of 172 mg MEDD or, on average, a decrease of about 3 mg MEDD per patient. Throughout the year, 36 patients were disenrolled from the clinic, and a total of 941 mg MEDD were discontinued by patients’ PCPs. This resulted in a mean of about 26 mg MEDD discontinued per patient. These statistics demonstrate small trends in decreasing overall MEDD in MCPMC patients.
Adjunctive therapies were often used in 67 MCPMC patients in addition to their opioid medications. If possible, therapies for pain management were chosen to maximize the ability to benefit comorbidities, such as depression, anxiety, and insomnia, while also treating chronic pain. The most frequently prescribed class of medications was antidepressants with 63% of patients prescribed one or more: bupropion, serotonin-norepinephrine reuptake inhibitor, selective-serotonin reuptake inhibitor, and tricyclic antidepressants. The next top 3 medication classes after antidepressants were topical medications (54%), antiepileptics (48%), and muscle relaxers (42%). The single most frequently prescribed adjunctive medication was gabapentin (37%), an antiepileptic.
Complementary Treatments
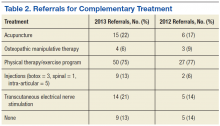
Complementary treatment referrals were followed throughout 2013 and compared with referrals from 2012 (Table 2). Physical therapy (PT) and exercise programs continued to be the most frequently referred treatment programs within the facility. Fifty-two percent of 67 MCPMC patients did not attend any PT appointments as recommended, of which the majority were required to attend as a component of their pain agreement. Of the remaining patients referred to PT, 48% went to their initial visit, 40% attended a second, and 32% attended 3 or more appointments. Of the group that attended 3 or more appointments, patients completed about 70% of the overall scheduled appointments, which was below the facility averages of 75% in 2012 and 80% in 2013.
Acupuncture, transcutaneous electrical nerve stimulation, and osteopathic manipulative therapy (OMT) were much less frequently suggested treatments, with percentages of patient referrals of 22%, 21%, and 6%, respectively. Sixty percent of patients referred to acupuncture attended the initial visit, 47% attended a second, and 40% attended 3 or more appointments. Of this group that attended at least 3 appointments, patients completed 75% of scheduled appointments, which was also below the facility averages of 86% in 2012 and 81% in 2013. Only 50% of patients referred to OMT attended the initial visit, of which these patients completed 100% of their scheduled appointments. This rate of attendance was above the facility averages of 60% in 2012 and 68% in 2013. Thirteen percent of patients were referred for interventional pain management and completed 1 of 3 types of injections (onabotulinumtoxinA, spinal, or intra-articular). There was a slight decrease in patients without complementary treatment referrals from 14% in 2012 to 13% in 2013.
Adherence
Pain agreement adherence was determined by assessing ED visits, urine toxicology results, and ACSPMPD search results. Sixty-one percent of the 67 MCPMC patients did not seek care in the ED, whereas 12% had 1 visit in 2013. This decrease in frequency of ED visits was significant compared with these same MCPMC patients from prior to participation in the clinic. The mean ED patient visits per year decreased from 5.1 to 1.8.
Urine toxicology tests were completed on 54 of the 67 MCPMC patients in 2013. Overall, urine toxicology reports were determined to be appropriate at the initial review 51% of the time, with 30% of patients having all of their reports completely appropriate. Of the 54 patients, 35% were disenrolled for inappropriate urine toxicology reports for the following reasons: negative for opioids, positive for opioids without a prescription, positive for amphetamines with additional confirmation testing, and positive for barbiturates without a prescription. Six percent of patients were discovered to have trace amphetamine results that were sent out for confirmation, but these reports were found to be negative, thus confirming an initial false-positive result.
Forty-eight percent of MCPMC patients tested negative for opioids at some point during the year when they were expected to have positive results. Of this group, 31% were prescribed morphine; the remaining patients were prescribed synthetic or semisynthetic opioids that are known to cause false-negative results: fentanyl (4%), hydrocodone (50%), and oxycodone (15%).9 Twenty-two percent of patients were disenrolled from the clinic for testing negative for opioids. The reason for disenrollment was often in conjunction with other behaviors that resulted in violations of their pain agreement. The remaining 78% reported running out of pain medications early and remained in the clinic. Two percent of patients were discovered to have a positive opioid result when it was expected to be negative. This group reported finding previously prescribed medications and subsequent results were appropriate, thus they remained in the clinic. Lastly, 2% of patients tested negative for barbiturates when it was expected to be positive. These patients reported running out of pain medication early as well.
The ACSPMPD was also used to assess pain agreement adherencee for all MCPMC patients. Six percent of patients were identified as seeking care from providers outside the IHS facility and receiving prescriptions for opioid medications, thus violating their pain agreements. Seventy-five percent of these patients were disenrolled from the MCPMC for this reason. PCPs referred the other 25% of patients, and the outside prescribers had performed procedures on them. These patients were reminded of their pain agreements, and no further violations were discovered according to the database. Each patient’s status in the MCPMC was evaluated on a case-by-case basis, and often decisions to disenroll or continue treating patients were based on the PCP’s clinical judgment.
Patient satisfaction was measured in the follow-up PAQ by asking 27 patients how they felt about their care, using a typical 5-point Likert scale. The 2 statements were, “I am pleased with the care that I have received for my pain,” and “I believe that I am receiving the best health care available.” Seventy percent of patients answered “strongly agree” or “agree” to the first statement, and 67% of patients answered the same for the second statement. Nineteen percent of patients answered “not sure” to the first statement, and 22% of patients answered the same for the other statement. Eleven percent of patients responded, “disagree” or “strongly disagree” to both statements.
In October 2013, 12 PCPs who had patients in the MCPMC completed an online survey regarding their perception of patient outcomes, time spent providing care to chronic pain patients, comparisons with general chronic pain patients, and satisfaction with the clinic. Most of the PCPs reported they spent 15 to 30 minutes on MCPMC patients compared with 30 to 60 minutes on general chronic pain patients each month. Most of the PCPs stated that they required ambulatory care clinic visits with chronic pain patients every other month, whereas MCPMC patients needed to be seen only quarterly. PCPs agreed that having their patients participate in the MCPMC resulted in better pain control, improved adherence to treatments, increased diversion and abuse surveillance, and better access to pain medications. Eleven of 12 PCPs stated that they were very satisfied with the MCPMC.
Discussion
The ultimate goal for patients of the MCPMC is to minimize disease progression, prevent an increase in pain, and improve adherence to treatment plans, including pharmacologic, interventional, and complementary components. According to the change in reported pain levels from the initial to the most recent assessment, most patients met the goal of preventing an increase in pain. There was a trend toward a decrease in reported pain, though it was not clinically or statistically significant. The follow-up PAQ measured varying changes in functional status and often demonstrated disease stabilization or progression, not improvement among patients. Forty-five percent of patients showed improvements, and 55% reported more difficulty performing daily activities. The median change between all 27 MCPMC patients was an overall decline in function of 2 points. This worsening in function over time would be expected for most of the chronic pain conditions.
In 2013, 9% of patients were initiated on SR opioids, making a clinic total of 33% of patients on SR medications. More than half the patients were on IR opioids as monotherapy, which is not an ideal treatment for chronic pain management. However, 81% of this group was on 15 mg MEDD or less. The use of SR opioids may or may not reduce abuse potential but can improve patient outcomes. Overall, there was an emphasis on using SR opioids when appropriate while continuing to improve patient outcomes. Over 61% of patients remained on the same opioid doses or were decreased over the course of 2013. There was also a significant use of adjuvant medications, primarily antidepressants, antiepileptics, and topical pain relievers. The most frequently prescribed non-opioid medication, excluding NSAIDs, was gabapentin. This medication has abuse potential and was treated as a controlled medication by the MCPMC during this period.
After enrollment in the MCPMC, patients used complementary and interventional treatments more consistently than prior to enrollment in the clinic. Treatments such as injections, acupuncture, OMT, and PT may reduce opioid medication consumption in the long term or slow the progression of disease for most patients. The improvement in QOL and lack of disease progression in these patients is not objectively measurable; however, the summative progress may be subjectively evaluated through reported pain levels and patient satisfaction.
For MCPMC patients who remained in the clinic, PT and acupuncture attendance was 70% and 75%, respectively. Although these were improvements in adherence for many MCPMC patients, the rates were still below the facility average completion rates of 80% and 81%, respectively. It could be argued that patients with acute pain are typically seen in PT for shorter periods and with fewer possibilities of missing appointments. Conversely, the single active MCPMC patient who attended OMT had a 100% completion rate compared with the average facility OMT attendance of 68%.
Other goals of the MCPMC consist of managing AEs, minimizing ED visits, monitoring for drug abuse and diversion, and improving adherence to pain agreements. The substantial 65% decrease in ED visits can be attributed to the patients’ participation in the MCPMC. Before enrollment, many patients would frequent the ED, because their PCP was not available. The cost savings from minimizing ED visits, provider and staff time, and resources is difficult to measure due to low rates of collections from insurance supplemental to IHS insurance yet is a significant benefit to the IHS facility.
Conclusions
Since the implementation of the MCPMC, patient outcomes have improved due to more consistent drug abuse and diversion surveillance of chronic pain patients rather than performing surveillance because of a suspicion of inappropriate medication use. Frequently using the pain agreement and monitoring parameters constructed a more trusting relationship between the PCP and the patient, and identified patients inappropriate for long-term opioid therapy. Identifying these patients was an unintentional, yet positive outcome.
Additionally, PCPs reported spending half the time with MCPMC patients vs general chronic pain patients. Patients who were not compliant with their pain agreements were discontinued from opioid therapy and were disenrolled from the clinic. Patients who have remained active have become more compliant with their pain agreements and treatment plans than they had been before enrollment. The MCPMC has ultimately relieved a significant burden from primary care and ED providers while improving outcomes and satisfaction of chronic pain patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-38, HHS Publication No. (SMA) 10-4586. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010.
3. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey.
J Pain. 2010;11(11):1230-1239.
4. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila PA 1976). 2006;31(23):
2724-2727.
5. Bolen J, Schieb L, Hootman JM, et al. Differences in the prevalence and impact of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis. 2010;7(3):A64.
6. Schiller JS, Lucas JW, Ward BW, Perogoy JA. Summary health statistics U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat. 2012;10(252). Centers for Disease Control and Prevention Website. http://www.cdc.gov/nchs/data/series/sr_10/sr10_252.pdf. Accessed June 26, 2015.
7. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
8. Rauck RL. What is the case for prescribing long-acting opioids over short-acting opioids for patients with chronic pain? A critical review. Pain Pract. 2009;9(6):468-479.
9. Pesce A, West C, Egan City K, Strickland J. Interpretation of urine drug testing in pain patients. Pain Med. 2012;13(7):868-885.
The epidemic of opioid abuse, addiction, and overdose deaths across the U.S. has not forgone the reservations of American Indian/Alaska Native (AI/AN) tribes. Indeed, AI/ANs may be at increased risk for abuse of prescription opioids due to higher rates of reported illicit drug use and misuse of opioids. According to the 2012 National Survey on Drug Use and Mental Health, AI/ANs aged ≥ 12 years had the highest rates of illicit drug use (12.7%) with the national average being only 9.5%.1 In 2009, AI/ANs aged 12 to 17 years were found to have the highest rates of marijuana use (13.8%) and nonmedical prescription drug abuse (6.1%) compared with the overall U.S. averages of 6.9% and 3.3%, respectively, putting them at an increased risk for an opioid overdose.1,2
In 2010, the American Pain Society conducted a survey establishing that about 41% of American adults reported having chronic, recurrent, or long-lasting pain.3 People of AI/AN heritage may experience chronic pain at higher rates, as they were identified as having the greatest incidence rates of low back pain (35%), arthritis (25%), and obesity (40%), which are often significant contributing factors to chronic pain.4-6
These conditions suggest a need for intensified management of chronic pain among IHS patients. The authors’ IHS facility is a closed health-system network where pharmacists are integral components of the health care team throughout the ambulatory care, emergency, and inpatient departments.
Related: Pharmacist Pain E-Consults That Result in a Therapy Change
Given that medications play a central role in the treatment of chronic pain, pharmacists are appropriate leaders for chronic pain management teams. Pharmacists can improve patient outcomes by conducting pain assessments, managing adverse events (AEs), identifying optimal medication choices, determining equianalgesic dosing, and managing care through care protocols.7
The primary objective of the multidisciplinary chronic pain management clinic (MCPMC) is to manage complicated and postsurgical patients, using a multimodal approach. Primary care providers (PCPs), which include physicians, nurse practitioners (NPs), physician assistants (PAs), and pharmacist providers collaborate to meet this goal by minimizing disease progression, preserving activities of daily living (ADL), maintaing employment, preventing an increase in pain, using treatment plans that include pharmacologic, interventional, and complementary components, decreasing emergency department (ED) visits for chronic pain issues, improving pain agreement adherence, managing AEs, performing drug abuse and diversion surveillance, and using sustained-release (SR) opioids when appropriate. Sustained release opioids not only ease dosing schedules and increase adherence, but also improve sleep, functionality, and quality of life (QOL) for chronic pain patients.8
Methods
The MCPMC began enrolling patients in January 2011 and has continued to date. Inclusion criterion is the presence of pain lasting 3 months or more. Exclusionary criteria are the presence of malignant pain, aged < 18 years, pregnancy, unmanaged psychiatric disorders, and a referral not approved by a PCP. Referrals are accepted from providers throughout the facility, including the ED, which then require approval by the PCP before enrollment. The PCP continues to manage these patients through consultations with the MCPMC pharmacists following MCPMC appointments and at separate ambulatory care clinic appointments.
Currently, there are 2 pharmacists practicing in the MCPMC clinic in conjunction with other health care providers, including 5 physical therapists, 1 psychiatrist, 2 clinical social workers, and 15 PCPs, including NPs and PAs. Additionally in 2014, the clinic became a yearlong rotation in the PGY-1 pharmacy practice residency.
Related: Evaluation of Methadone-Induced QTc Prolongation in a Veteran Population
After enrollment, a pharmacist reviews patients’ health records for past pain medications, interventional and complementary treatments, adherence to these treatments, recent ED visits and medications received, urine toxicology results, adherence to pain agreements, and the Arizona Controlled Substances Prescription Monitoring Program Database (ACSPMPD).
During the initial MCPMC appointment, a pain assessment questionnaire (PAQ) is completed with a MCPMC pharmacist. The questionnaire, designed specifically for the MCPMC, consists of a comprehensive pain assessment, including functional status and common comorbidities, such as anxiety, depression, obesity, and insomnia. Patients provide feedback on efficacy of past or current medications, and interventional and complementary treatments if applicable. Patients also rate their satisfaction with health care received and develop goals for their treatment and overall health.
A collaborative treatment plan is then developed with the patient’s PCP. Treatment plans often consist of increasing or starting interventional and complementary treatments, SR opioids, and adjuvant medications. Common adjuvant medications include nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, antiepileptics, immunosuppressants, disease-modifying antirheumatic drugs (DMARDs), and topical agents. To maximize benefits of the medications, antidepressants are often prescribed for dual purposes among patients with comorbid conditions, such as anxiety, depression, and insomnia. Among obese patients, weight loss is encouraged, and patients may be referred to dietary counseling and exercise programs. Other intentions of the treatment plans are to decrease breakthrough pain and ED visits while attempting to decrease the use of immediate-release (IR) opioids. Treatment plans are executed in a stepwise approach over multiple MCPMC visits and may be modified throughout the course of the program.
To ensure that medication changes and other issues can be addressed when a prescriber is available, all subsequent visits are scheduled when patients are due for a pain medication refill. The MCPMC pharmacists chose not to pursue prescriptive authority but have privileges to order urine toxicology tests, make nonformulary requests, and refer patients for complementary treatments. Subsequent appointments are commonly scheduled 1 to 4 weeks apart or alternate with PCP appointments.
Related: Multidisciplinary Approach to Back Pain
During each appointment, data are collected to record changes in therapy and pain levels. Questions regarding general health and adherence to pharmacologic, interventional, and complementary treatments, exercise regimens, and specialty referrals are asked of all patients. Additionally, follow-up PAQs are completed every 6 months to track progress in therapy, pain control, treatment plan adherence, and patient satisfaction. To determine pain agreement adherence, the ACSPMPD is reviewed monthly, and urine toxicology tests and pill counts are performed randomly at MCPMC visits.
In October 2013, all PCPs who had patients in the clinic completed a survey to assess their perception of the MCPMC. Questions were related to their satisfaction with the clinic as well as their opinion of patients’ satisfaction. Other questions were related to their view of patient care and outcomes compared with those of the general chronic pain patients at the facility.
Results
As of January 2013, 106 patients had been referred to the MCPMC by 17 PCPs. Thirty-six of these patients were still actively participating in the clinic, while 25 were pending review. Of the remaining 45 patients, 30 were denied initial enrollment, and 15 were disenrolled from the clinic over the previous 2 years. Patients were determined to be inappropriate candidates and not enrolled in the clinic for the following reasons: referral not approved by the PCP, patient refused care, patient had not established care with a PCP, mental health issues, pediatric patient, oncology patient, and death prior to the initial review. Patients were disenrolled from the MCPMC clinic before 2013 for the following reasons: not participating in their treatment plan, illicit drug use, seeking care from other PCPs, suspected diversion, death due to a nonpain-related issue, and remained stable on the medication regimen and were released back to the care of their PCP.
In 2013, there were 47 new referrals to the MCPMC, resulting in a total of 153 referrals since the clinic’s 2011 inception. Over the course of 2013, 31 new patients were enrolled, 32 referrals were denied (15 of which remained from 2012), and 36 patients were disenrolled (Figure 1). At the end of 2013, 31 patients remained active, while 9 referrals remained pending review. A total of 67 patients participated in the MCPMC at some point during 2013 and were included in the data collection. Patients by diagnoses are displayed in Figure 2.
In 2013, patients were scheduled for a total of 337 MCPMC appointments, and 298 (88%) were completed by patients, a 17% increase above 2012. The mean show rate of PCP ambulatory care clinic appointments was about 70%. The completed MCPMC visits for 2013 correlates to about 6.8 MCPMC visits annually per patient. Of the 67 patients included in data collection, the mean total number of months active in the clinic was 12.5. The mean number of months active in the clinic in 2013 was 6.9.
Pain Assessment Questionnaire
In 2013, 27 patients (40%) were enrolled in the clinic for 6 months or more and completed a follow-up PAQ. Throughout 2013, MCPMC patients presented to the ED for care 76 times, which correlates to about 1.8 ED visits annually per patient. MCPMC patients also attended an appointment with their PCP on average 3.7 times per year and provided urine toxicology tests on average 4.3 times per year between MCPMC and PCP visits.
Data collected from follow-up PAQs in January 2014 provided information on the 27 MCPMC patients enrolled in the clinic for 6 months or more. This review indicated alterations in patients’ reported pain levels, functional status, patient satisfaction, and adherence to pain agreements from before and after enrollment in the clinic. Additional information was collected using the electronic health record to reveal the adjustments in treatment plans, including pharmacologic, complementary, and interventional treatments, along with adherence to these treatments.
Patients’ self-reported pain levels at the time of appointment and average pain levels since the previous appointment were documented at each visit for the 27 MCPMC patients. These 2 pain levels were then compared with the levels of the initial assessment and the most recent appointment. Results were inconsistent; however, slight trends were observed with the analysis. The mean change in pain reported at the time of assessment decreased 5.1%. The mean change in average reported pain since the previous appointment also decreased 6.9%. Statistical analysis was performed using the Wilcoxon signed rank test. Both decreases in reported pain were not clinically or statistically significant (P = .21 and P = .17, respectively). Eleven (41%) patients had improvement in average pain, whereas 10 (37%) had no change, and 6 (22%) reported increased average pain levels.
Data on alterations in functional status and ADL were also collected from the 27 MCPMC patients. These patients reported the perceived degree of difficulty, on a scale of 1 to 5, required to complete tasks and get through their day. A rating of 1 represented the ability to complete activities with no difficulty, whereas 5 represented an inability to complete the tasks. For each of the 19 tasks, the differences in scores from the initial to the most recent PAQs were recorded as either a positive or negative alteration for each patient, and the sum of these differences was recorded as an overall positive or negative change in function. A positive change in function indicated an improvement in function, whereas an overall negative change indicated a decrease in ability to complete daily activities.
Twenty-six percent of the 27 pa-tients had a cumulative positive change of up to 5 points, and 19% had a positive change of 6 or more points. Alternatively, 22% of patients had a cumulative negative change of up to 5 points, and 33% of patients had a negative change of 6 points or more. The greatest positive change was 15 points, the greatest negative change was 28 points, and the median change from the initial to the most recent assessments was a negative change of 2 points.
Adjuvant Medications
The pharmacologic component of the treatment plans consisted primarily of optimizing the use of adjuvant medications and SR opioids when appropriate, while minimizing the use of IR opioids and other controlled medications. Of the 67 MCPMC patients in 2013, 55% were on IR opioids alone, a slight increase from 46% in 2012 (Table 1). Eighty-one percent of patients in this group were on ≤ 15 mg of morphine equivalent daily dose (MEDD), which would have required at least a doubling of their dose to initiate the preferred formulary SR opioid, morphine SR tablets. Six percent of patients were on SR opioids alone, also a slight increase from 3% in 2012. Twenty-seven percent of patients were prescribed a combination of IR and SR opioids. Nine percent of patients had been recently transitioned to SR opioids while in the MCPMC, of which 1 patient was prescribed the medication as monotherapy. Twelve percent of patients were not on any opioid therapy throughout 2013.
Opioids were switched to an alternative opioid at some point during the year to minimize tolerance in 15% of patients, of which 9% were IR and 6% were SR opioids. Changes in opioid therapy from the beginning to the end of the year were recorded as a decrease, increase, or no change in MEDD. Doses were decreased for 16%, increased for 27%, and not changed for the remaining 45% of patients. The sum of these changes for the 59 patients on opioids was a decrease of 172 mg MEDD or, on average, a decrease of about 3 mg MEDD per patient. Throughout the year, 36 patients were disenrolled from the clinic, and a total of 941 mg MEDD were discontinued by patients’ PCPs. This resulted in a mean of about 26 mg MEDD discontinued per patient. These statistics demonstrate small trends in decreasing overall MEDD in MCPMC patients.
Adjunctive therapies were often used in 67 MCPMC patients in addition to their opioid medications. If possible, therapies for pain management were chosen to maximize the ability to benefit comorbidities, such as depression, anxiety, and insomnia, while also treating chronic pain. The most frequently prescribed class of medications was antidepressants with 63% of patients prescribed one or more: bupropion, serotonin-norepinephrine reuptake inhibitor, selective-serotonin reuptake inhibitor, and tricyclic antidepressants. The next top 3 medication classes after antidepressants were topical medications (54%), antiepileptics (48%), and muscle relaxers (42%). The single most frequently prescribed adjunctive medication was gabapentin (37%), an antiepileptic.
Complementary Treatments
Complementary treatment referrals were followed throughout 2013 and compared with referrals from 2012 (Table 2). Physical therapy (PT) and exercise programs continued to be the most frequently referred treatment programs within the facility. Fifty-two percent of 67 MCPMC patients did not attend any PT appointments as recommended, of which the majority were required to attend as a component of their pain agreement. Of the remaining patients referred to PT, 48% went to their initial visit, 40% attended a second, and 32% attended 3 or more appointments. Of the group that attended 3 or more appointments, patients completed about 70% of the overall scheduled appointments, which was below the facility averages of 75% in 2012 and 80% in 2013.
Acupuncture, transcutaneous electrical nerve stimulation, and osteopathic manipulative therapy (OMT) were much less frequently suggested treatments, with percentages of patient referrals of 22%, 21%, and 6%, respectively. Sixty percent of patients referred to acupuncture attended the initial visit, 47% attended a second, and 40% attended 3 or more appointments. Of this group that attended at least 3 appointments, patients completed 75% of scheduled appointments, which was also below the facility averages of 86% in 2012 and 81% in 2013. Only 50% of patients referred to OMT attended the initial visit, of which these patients completed 100% of their scheduled appointments. This rate of attendance was above the facility averages of 60% in 2012 and 68% in 2013. Thirteen percent of patients were referred for interventional pain management and completed 1 of 3 types of injections (onabotulinumtoxinA, spinal, or intra-articular). There was a slight decrease in patients without complementary treatment referrals from 14% in 2012 to 13% in 2013.
Adherence
Pain agreement adherence was determined by assessing ED visits, urine toxicology results, and ACSPMPD search results. Sixty-one percent of the 67 MCPMC patients did not seek care in the ED, whereas 12% had 1 visit in 2013. This decrease in frequency of ED visits was significant compared with these same MCPMC patients from prior to participation in the clinic. The mean ED patient visits per year decreased from 5.1 to 1.8.
Urine toxicology tests were completed on 54 of the 67 MCPMC patients in 2013. Overall, urine toxicology reports were determined to be appropriate at the initial review 51% of the time, with 30% of patients having all of their reports completely appropriate. Of the 54 patients, 35% were disenrolled for inappropriate urine toxicology reports for the following reasons: negative for opioids, positive for opioids without a prescription, positive for amphetamines with additional confirmation testing, and positive for barbiturates without a prescription. Six percent of patients were discovered to have trace amphetamine results that were sent out for confirmation, but these reports were found to be negative, thus confirming an initial false-positive result.
Forty-eight percent of MCPMC patients tested negative for opioids at some point during the year when they were expected to have positive results. Of this group, 31% were prescribed morphine; the remaining patients were prescribed synthetic or semisynthetic opioids that are known to cause false-negative results: fentanyl (4%), hydrocodone (50%), and oxycodone (15%).9 Twenty-two percent of patients were disenrolled from the clinic for testing negative for opioids. The reason for disenrollment was often in conjunction with other behaviors that resulted in violations of their pain agreement. The remaining 78% reported running out of pain medications early and remained in the clinic. Two percent of patients were discovered to have a positive opioid result when it was expected to be negative. This group reported finding previously prescribed medications and subsequent results were appropriate, thus they remained in the clinic. Lastly, 2% of patients tested negative for barbiturates when it was expected to be positive. These patients reported running out of pain medication early as well.
The ACSPMPD was also used to assess pain agreement adherencee for all MCPMC patients. Six percent of patients were identified as seeking care from providers outside the IHS facility and receiving prescriptions for opioid medications, thus violating their pain agreements. Seventy-five percent of these patients were disenrolled from the MCPMC for this reason. PCPs referred the other 25% of patients, and the outside prescribers had performed procedures on them. These patients were reminded of their pain agreements, and no further violations were discovered according to the database. Each patient’s status in the MCPMC was evaluated on a case-by-case basis, and often decisions to disenroll or continue treating patients were based on the PCP’s clinical judgment.
Patient satisfaction was measured in the follow-up PAQ by asking 27 patients how they felt about their care, using a typical 5-point Likert scale. The 2 statements were, “I am pleased with the care that I have received for my pain,” and “I believe that I am receiving the best health care available.” Seventy percent of patients answered “strongly agree” or “agree” to the first statement, and 67% of patients answered the same for the second statement. Nineteen percent of patients answered “not sure” to the first statement, and 22% of patients answered the same for the other statement. Eleven percent of patients responded, “disagree” or “strongly disagree” to both statements.
In October 2013, 12 PCPs who had patients in the MCPMC completed an online survey regarding their perception of patient outcomes, time spent providing care to chronic pain patients, comparisons with general chronic pain patients, and satisfaction with the clinic. Most of the PCPs reported they spent 15 to 30 minutes on MCPMC patients compared with 30 to 60 minutes on general chronic pain patients each month. Most of the PCPs stated that they required ambulatory care clinic visits with chronic pain patients every other month, whereas MCPMC patients needed to be seen only quarterly. PCPs agreed that having their patients participate in the MCPMC resulted in better pain control, improved adherence to treatments, increased diversion and abuse surveillance, and better access to pain medications. Eleven of 12 PCPs stated that they were very satisfied with the MCPMC.
Discussion
The ultimate goal for patients of the MCPMC is to minimize disease progression, prevent an increase in pain, and improve adherence to treatment plans, including pharmacologic, interventional, and complementary components. According to the change in reported pain levels from the initial to the most recent assessment, most patients met the goal of preventing an increase in pain. There was a trend toward a decrease in reported pain, though it was not clinically or statistically significant. The follow-up PAQ measured varying changes in functional status and often demonstrated disease stabilization or progression, not improvement among patients. Forty-five percent of patients showed improvements, and 55% reported more difficulty performing daily activities. The median change between all 27 MCPMC patients was an overall decline in function of 2 points. This worsening in function over time would be expected for most of the chronic pain conditions.
In 2013, 9% of patients were initiated on SR opioids, making a clinic total of 33% of patients on SR medications. More than half the patients were on IR opioids as monotherapy, which is not an ideal treatment for chronic pain management. However, 81% of this group was on 15 mg MEDD or less. The use of SR opioids may or may not reduce abuse potential but can improve patient outcomes. Overall, there was an emphasis on using SR opioids when appropriate while continuing to improve patient outcomes. Over 61% of patients remained on the same opioid doses or were decreased over the course of 2013. There was also a significant use of adjuvant medications, primarily antidepressants, antiepileptics, and topical pain relievers. The most frequently prescribed non-opioid medication, excluding NSAIDs, was gabapentin. This medication has abuse potential and was treated as a controlled medication by the MCPMC during this period.
After enrollment in the MCPMC, patients used complementary and interventional treatments more consistently than prior to enrollment in the clinic. Treatments such as injections, acupuncture, OMT, and PT may reduce opioid medication consumption in the long term or slow the progression of disease for most patients. The improvement in QOL and lack of disease progression in these patients is not objectively measurable; however, the summative progress may be subjectively evaluated through reported pain levels and patient satisfaction.
For MCPMC patients who remained in the clinic, PT and acupuncture attendance was 70% and 75%, respectively. Although these were improvements in adherence for many MCPMC patients, the rates were still below the facility average completion rates of 80% and 81%, respectively. It could be argued that patients with acute pain are typically seen in PT for shorter periods and with fewer possibilities of missing appointments. Conversely, the single active MCPMC patient who attended OMT had a 100% completion rate compared with the average facility OMT attendance of 68%.
Other goals of the MCPMC consist of managing AEs, minimizing ED visits, monitoring for drug abuse and diversion, and improving adherence to pain agreements. The substantial 65% decrease in ED visits can be attributed to the patients’ participation in the MCPMC. Before enrollment, many patients would frequent the ED, because their PCP was not available. The cost savings from minimizing ED visits, provider and staff time, and resources is difficult to measure due to low rates of collections from insurance supplemental to IHS insurance yet is a significant benefit to the IHS facility.
Conclusions
Since the implementation of the MCPMC, patient outcomes have improved due to more consistent drug abuse and diversion surveillance of chronic pain patients rather than performing surveillance because of a suspicion of inappropriate medication use. Frequently using the pain agreement and monitoring parameters constructed a more trusting relationship between the PCP and the patient, and identified patients inappropriate for long-term opioid therapy. Identifying these patients was an unintentional, yet positive outcome.
Additionally, PCPs reported spending half the time with MCPMC patients vs general chronic pain patients. Patients who were not compliant with their pain agreements were discontinued from opioid therapy and were disenrolled from the clinic. Patients who have remained active have become more compliant with their pain agreements and treatment plans than they had been before enrollment. The MCPMC has ultimately relieved a significant burden from primary care and ED providers while improving outcomes and satisfaction of chronic pain patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
The epidemic of opioid abuse, addiction, and overdose deaths across the U.S. has not forgone the reservations of American Indian/Alaska Native (AI/AN) tribes. Indeed, AI/ANs may be at increased risk for abuse of prescription opioids due to higher rates of reported illicit drug use and misuse of opioids. According to the 2012 National Survey on Drug Use and Mental Health, AI/ANs aged ≥ 12 years had the highest rates of illicit drug use (12.7%) with the national average being only 9.5%.1 In 2009, AI/ANs aged 12 to 17 years were found to have the highest rates of marijuana use (13.8%) and nonmedical prescription drug abuse (6.1%) compared with the overall U.S. averages of 6.9% and 3.3%, respectively, putting them at an increased risk for an opioid overdose.1,2
In 2010, the American Pain Society conducted a survey establishing that about 41% of American adults reported having chronic, recurrent, or long-lasting pain.3 People of AI/AN heritage may experience chronic pain at higher rates, as they were identified as having the greatest incidence rates of low back pain (35%), arthritis (25%), and obesity (40%), which are often significant contributing factors to chronic pain.4-6
These conditions suggest a need for intensified management of chronic pain among IHS patients. The authors’ IHS facility is a closed health-system network where pharmacists are integral components of the health care team throughout the ambulatory care, emergency, and inpatient departments.
Related: Pharmacist Pain E-Consults That Result in a Therapy Change
Given that medications play a central role in the treatment of chronic pain, pharmacists are appropriate leaders for chronic pain management teams. Pharmacists can improve patient outcomes by conducting pain assessments, managing adverse events (AEs), identifying optimal medication choices, determining equianalgesic dosing, and managing care through care protocols.7
The primary objective of the multidisciplinary chronic pain management clinic (MCPMC) is to manage complicated and postsurgical patients, using a multimodal approach. Primary care providers (PCPs), which include physicians, nurse practitioners (NPs), physician assistants (PAs), and pharmacist providers collaborate to meet this goal by minimizing disease progression, preserving activities of daily living (ADL), maintaing employment, preventing an increase in pain, using treatment plans that include pharmacologic, interventional, and complementary components, decreasing emergency department (ED) visits for chronic pain issues, improving pain agreement adherence, managing AEs, performing drug abuse and diversion surveillance, and using sustained-release (SR) opioids when appropriate. Sustained release opioids not only ease dosing schedules and increase adherence, but also improve sleep, functionality, and quality of life (QOL) for chronic pain patients.8
Methods
The MCPMC began enrolling patients in January 2011 and has continued to date. Inclusion criterion is the presence of pain lasting 3 months or more. Exclusionary criteria are the presence of malignant pain, aged < 18 years, pregnancy, unmanaged psychiatric disorders, and a referral not approved by a PCP. Referrals are accepted from providers throughout the facility, including the ED, which then require approval by the PCP before enrollment. The PCP continues to manage these patients through consultations with the MCPMC pharmacists following MCPMC appointments and at separate ambulatory care clinic appointments.
Currently, there are 2 pharmacists practicing in the MCPMC clinic in conjunction with other health care providers, including 5 physical therapists, 1 psychiatrist, 2 clinical social workers, and 15 PCPs, including NPs and PAs. Additionally in 2014, the clinic became a yearlong rotation in the PGY-1 pharmacy practice residency.
Related: Evaluation of Methadone-Induced QTc Prolongation in a Veteran Population
After enrollment, a pharmacist reviews patients’ health records for past pain medications, interventional and complementary treatments, adherence to these treatments, recent ED visits and medications received, urine toxicology results, adherence to pain agreements, and the Arizona Controlled Substances Prescription Monitoring Program Database (ACSPMPD).
During the initial MCPMC appointment, a pain assessment questionnaire (PAQ) is completed with a MCPMC pharmacist. The questionnaire, designed specifically for the MCPMC, consists of a comprehensive pain assessment, including functional status and common comorbidities, such as anxiety, depression, obesity, and insomnia. Patients provide feedback on efficacy of past or current medications, and interventional and complementary treatments if applicable. Patients also rate their satisfaction with health care received and develop goals for their treatment and overall health.
A collaborative treatment plan is then developed with the patient’s PCP. Treatment plans often consist of increasing or starting interventional and complementary treatments, SR opioids, and adjuvant medications. Common adjuvant medications include nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, antiepileptics, immunosuppressants, disease-modifying antirheumatic drugs (DMARDs), and topical agents. To maximize benefits of the medications, antidepressants are often prescribed for dual purposes among patients with comorbid conditions, such as anxiety, depression, and insomnia. Among obese patients, weight loss is encouraged, and patients may be referred to dietary counseling and exercise programs. Other intentions of the treatment plans are to decrease breakthrough pain and ED visits while attempting to decrease the use of immediate-release (IR) opioids. Treatment plans are executed in a stepwise approach over multiple MCPMC visits and may be modified throughout the course of the program.
To ensure that medication changes and other issues can be addressed when a prescriber is available, all subsequent visits are scheduled when patients are due for a pain medication refill. The MCPMC pharmacists chose not to pursue prescriptive authority but have privileges to order urine toxicology tests, make nonformulary requests, and refer patients for complementary treatments. Subsequent appointments are commonly scheduled 1 to 4 weeks apart or alternate with PCP appointments.
Related: Multidisciplinary Approach to Back Pain
During each appointment, data are collected to record changes in therapy and pain levels. Questions regarding general health and adherence to pharmacologic, interventional, and complementary treatments, exercise regimens, and specialty referrals are asked of all patients. Additionally, follow-up PAQs are completed every 6 months to track progress in therapy, pain control, treatment plan adherence, and patient satisfaction. To determine pain agreement adherence, the ACSPMPD is reviewed monthly, and urine toxicology tests and pill counts are performed randomly at MCPMC visits.
In October 2013, all PCPs who had patients in the clinic completed a survey to assess their perception of the MCPMC. Questions were related to their satisfaction with the clinic as well as their opinion of patients’ satisfaction. Other questions were related to their view of patient care and outcomes compared with those of the general chronic pain patients at the facility.
Results
As of January 2013, 106 patients had been referred to the MCPMC by 17 PCPs. Thirty-six of these patients were still actively participating in the clinic, while 25 were pending review. Of the remaining 45 patients, 30 were denied initial enrollment, and 15 were disenrolled from the clinic over the previous 2 years. Patients were determined to be inappropriate candidates and not enrolled in the clinic for the following reasons: referral not approved by the PCP, patient refused care, patient had not established care with a PCP, mental health issues, pediatric patient, oncology patient, and death prior to the initial review. Patients were disenrolled from the MCPMC clinic before 2013 for the following reasons: not participating in their treatment plan, illicit drug use, seeking care from other PCPs, suspected diversion, death due to a nonpain-related issue, and remained stable on the medication regimen and were released back to the care of their PCP.
In 2013, there were 47 new referrals to the MCPMC, resulting in a total of 153 referrals since the clinic’s 2011 inception. Over the course of 2013, 31 new patients were enrolled, 32 referrals were denied (15 of which remained from 2012), and 36 patients were disenrolled (Figure 1). At the end of 2013, 31 patients remained active, while 9 referrals remained pending review. A total of 67 patients participated in the MCPMC at some point during 2013 and were included in the data collection. Patients by diagnoses are displayed in Figure 2.
In 2013, patients were scheduled for a total of 337 MCPMC appointments, and 298 (88%) were completed by patients, a 17% increase above 2012. The mean show rate of PCP ambulatory care clinic appointments was about 70%. The completed MCPMC visits for 2013 correlates to about 6.8 MCPMC visits annually per patient. Of the 67 patients included in data collection, the mean total number of months active in the clinic was 12.5. The mean number of months active in the clinic in 2013 was 6.9.
Pain Assessment Questionnaire
In 2013, 27 patients (40%) were enrolled in the clinic for 6 months or more and completed a follow-up PAQ. Throughout 2013, MCPMC patients presented to the ED for care 76 times, which correlates to about 1.8 ED visits annually per patient. MCPMC patients also attended an appointment with their PCP on average 3.7 times per year and provided urine toxicology tests on average 4.3 times per year between MCPMC and PCP visits.
Data collected from follow-up PAQs in January 2014 provided information on the 27 MCPMC patients enrolled in the clinic for 6 months or more. This review indicated alterations in patients’ reported pain levels, functional status, patient satisfaction, and adherence to pain agreements from before and after enrollment in the clinic. Additional information was collected using the electronic health record to reveal the adjustments in treatment plans, including pharmacologic, complementary, and interventional treatments, along with adherence to these treatments.
Patients’ self-reported pain levels at the time of appointment and average pain levels since the previous appointment were documented at each visit for the 27 MCPMC patients. These 2 pain levels were then compared with the levels of the initial assessment and the most recent appointment. Results were inconsistent; however, slight trends were observed with the analysis. The mean change in pain reported at the time of assessment decreased 5.1%. The mean change in average reported pain since the previous appointment also decreased 6.9%. Statistical analysis was performed using the Wilcoxon signed rank test. Both decreases in reported pain were not clinically or statistically significant (P = .21 and P = .17, respectively). Eleven (41%) patients had improvement in average pain, whereas 10 (37%) had no change, and 6 (22%) reported increased average pain levels.
Data on alterations in functional status and ADL were also collected from the 27 MCPMC patients. These patients reported the perceived degree of difficulty, on a scale of 1 to 5, required to complete tasks and get through their day. A rating of 1 represented the ability to complete activities with no difficulty, whereas 5 represented an inability to complete the tasks. For each of the 19 tasks, the differences in scores from the initial to the most recent PAQs were recorded as either a positive or negative alteration for each patient, and the sum of these differences was recorded as an overall positive or negative change in function. A positive change in function indicated an improvement in function, whereas an overall negative change indicated a decrease in ability to complete daily activities.
Twenty-six percent of the 27 pa-tients had a cumulative positive change of up to 5 points, and 19% had a positive change of 6 or more points. Alternatively, 22% of patients had a cumulative negative change of up to 5 points, and 33% of patients had a negative change of 6 points or more. The greatest positive change was 15 points, the greatest negative change was 28 points, and the median change from the initial to the most recent assessments was a negative change of 2 points.
Adjuvant Medications
The pharmacologic component of the treatment plans consisted primarily of optimizing the use of adjuvant medications and SR opioids when appropriate, while minimizing the use of IR opioids and other controlled medications. Of the 67 MCPMC patients in 2013, 55% were on IR opioids alone, a slight increase from 46% in 2012 (Table 1). Eighty-one percent of patients in this group were on ≤ 15 mg of morphine equivalent daily dose (MEDD), which would have required at least a doubling of their dose to initiate the preferred formulary SR opioid, morphine SR tablets. Six percent of patients were on SR opioids alone, also a slight increase from 3% in 2012. Twenty-seven percent of patients were prescribed a combination of IR and SR opioids. Nine percent of patients had been recently transitioned to SR opioids while in the MCPMC, of which 1 patient was prescribed the medication as monotherapy. Twelve percent of patients were not on any opioid therapy throughout 2013.
Opioids were switched to an alternative opioid at some point during the year to minimize tolerance in 15% of patients, of which 9% were IR and 6% were SR opioids. Changes in opioid therapy from the beginning to the end of the year were recorded as a decrease, increase, or no change in MEDD. Doses were decreased for 16%, increased for 27%, and not changed for the remaining 45% of patients. The sum of these changes for the 59 patients on opioids was a decrease of 172 mg MEDD or, on average, a decrease of about 3 mg MEDD per patient. Throughout the year, 36 patients were disenrolled from the clinic, and a total of 941 mg MEDD were discontinued by patients’ PCPs. This resulted in a mean of about 26 mg MEDD discontinued per patient. These statistics demonstrate small trends in decreasing overall MEDD in MCPMC patients.
Adjunctive therapies were often used in 67 MCPMC patients in addition to their opioid medications. If possible, therapies for pain management were chosen to maximize the ability to benefit comorbidities, such as depression, anxiety, and insomnia, while also treating chronic pain. The most frequently prescribed class of medications was antidepressants with 63% of patients prescribed one or more: bupropion, serotonin-norepinephrine reuptake inhibitor, selective-serotonin reuptake inhibitor, and tricyclic antidepressants. The next top 3 medication classes after antidepressants were topical medications (54%), antiepileptics (48%), and muscle relaxers (42%). The single most frequently prescribed adjunctive medication was gabapentin (37%), an antiepileptic.
Complementary Treatments
Complementary treatment referrals were followed throughout 2013 and compared with referrals from 2012 (Table 2). Physical therapy (PT) and exercise programs continued to be the most frequently referred treatment programs within the facility. Fifty-two percent of 67 MCPMC patients did not attend any PT appointments as recommended, of which the majority were required to attend as a component of their pain agreement. Of the remaining patients referred to PT, 48% went to their initial visit, 40% attended a second, and 32% attended 3 or more appointments. Of the group that attended 3 or more appointments, patients completed about 70% of the overall scheduled appointments, which was below the facility averages of 75% in 2012 and 80% in 2013.
Acupuncture, transcutaneous electrical nerve stimulation, and osteopathic manipulative therapy (OMT) were much less frequently suggested treatments, with percentages of patient referrals of 22%, 21%, and 6%, respectively. Sixty percent of patients referred to acupuncture attended the initial visit, 47% attended a second, and 40% attended 3 or more appointments. Of this group that attended at least 3 appointments, patients completed 75% of scheduled appointments, which was also below the facility averages of 86% in 2012 and 81% in 2013. Only 50% of patients referred to OMT attended the initial visit, of which these patients completed 100% of their scheduled appointments. This rate of attendance was above the facility averages of 60% in 2012 and 68% in 2013. Thirteen percent of patients were referred for interventional pain management and completed 1 of 3 types of injections (onabotulinumtoxinA, spinal, or intra-articular). There was a slight decrease in patients without complementary treatment referrals from 14% in 2012 to 13% in 2013.
Adherence
Pain agreement adherence was determined by assessing ED visits, urine toxicology results, and ACSPMPD search results. Sixty-one percent of the 67 MCPMC patients did not seek care in the ED, whereas 12% had 1 visit in 2013. This decrease in frequency of ED visits was significant compared with these same MCPMC patients from prior to participation in the clinic. The mean ED patient visits per year decreased from 5.1 to 1.8.
Urine toxicology tests were completed on 54 of the 67 MCPMC patients in 2013. Overall, urine toxicology reports were determined to be appropriate at the initial review 51% of the time, with 30% of patients having all of their reports completely appropriate. Of the 54 patients, 35% were disenrolled for inappropriate urine toxicology reports for the following reasons: negative for opioids, positive for opioids without a prescription, positive for amphetamines with additional confirmation testing, and positive for barbiturates without a prescription. Six percent of patients were discovered to have trace amphetamine results that were sent out for confirmation, but these reports were found to be negative, thus confirming an initial false-positive result.
Forty-eight percent of MCPMC patients tested negative for opioids at some point during the year when they were expected to have positive results. Of this group, 31% were prescribed morphine; the remaining patients were prescribed synthetic or semisynthetic opioids that are known to cause false-negative results: fentanyl (4%), hydrocodone (50%), and oxycodone (15%).9 Twenty-two percent of patients were disenrolled from the clinic for testing negative for opioids. The reason for disenrollment was often in conjunction with other behaviors that resulted in violations of their pain agreement. The remaining 78% reported running out of pain medications early and remained in the clinic. Two percent of patients were discovered to have a positive opioid result when it was expected to be negative. This group reported finding previously prescribed medications and subsequent results were appropriate, thus they remained in the clinic. Lastly, 2% of patients tested negative for barbiturates when it was expected to be positive. These patients reported running out of pain medication early as well.
The ACSPMPD was also used to assess pain agreement adherencee for all MCPMC patients. Six percent of patients were identified as seeking care from providers outside the IHS facility and receiving prescriptions for opioid medications, thus violating their pain agreements. Seventy-five percent of these patients were disenrolled from the MCPMC for this reason. PCPs referred the other 25% of patients, and the outside prescribers had performed procedures on them. These patients were reminded of their pain agreements, and no further violations were discovered according to the database. Each patient’s status in the MCPMC was evaluated on a case-by-case basis, and often decisions to disenroll or continue treating patients were based on the PCP’s clinical judgment.
Patient satisfaction was measured in the follow-up PAQ by asking 27 patients how they felt about their care, using a typical 5-point Likert scale. The 2 statements were, “I am pleased with the care that I have received for my pain,” and “I believe that I am receiving the best health care available.” Seventy percent of patients answered “strongly agree” or “agree” to the first statement, and 67% of patients answered the same for the second statement. Nineteen percent of patients answered “not sure” to the first statement, and 22% of patients answered the same for the other statement. Eleven percent of patients responded, “disagree” or “strongly disagree” to both statements.
In October 2013, 12 PCPs who had patients in the MCPMC completed an online survey regarding their perception of patient outcomes, time spent providing care to chronic pain patients, comparisons with general chronic pain patients, and satisfaction with the clinic. Most of the PCPs reported they spent 15 to 30 minutes on MCPMC patients compared with 30 to 60 minutes on general chronic pain patients each month. Most of the PCPs stated that they required ambulatory care clinic visits with chronic pain patients every other month, whereas MCPMC patients needed to be seen only quarterly. PCPs agreed that having their patients participate in the MCPMC resulted in better pain control, improved adherence to treatments, increased diversion and abuse surveillance, and better access to pain medications. Eleven of 12 PCPs stated that they were very satisfied with the MCPMC.
Discussion
The ultimate goal for patients of the MCPMC is to minimize disease progression, prevent an increase in pain, and improve adherence to treatment plans, including pharmacologic, interventional, and complementary components. According to the change in reported pain levels from the initial to the most recent assessment, most patients met the goal of preventing an increase in pain. There was a trend toward a decrease in reported pain, though it was not clinically or statistically significant. The follow-up PAQ measured varying changes in functional status and often demonstrated disease stabilization or progression, not improvement among patients. Forty-five percent of patients showed improvements, and 55% reported more difficulty performing daily activities. The median change between all 27 MCPMC patients was an overall decline in function of 2 points. This worsening in function over time would be expected for most of the chronic pain conditions.
In 2013, 9% of patients were initiated on SR opioids, making a clinic total of 33% of patients on SR medications. More than half the patients were on IR opioids as monotherapy, which is not an ideal treatment for chronic pain management. However, 81% of this group was on 15 mg MEDD or less. The use of SR opioids may or may not reduce abuse potential but can improve patient outcomes. Overall, there was an emphasis on using SR opioids when appropriate while continuing to improve patient outcomes. Over 61% of patients remained on the same opioid doses or were decreased over the course of 2013. There was also a significant use of adjuvant medications, primarily antidepressants, antiepileptics, and topical pain relievers. The most frequently prescribed non-opioid medication, excluding NSAIDs, was gabapentin. This medication has abuse potential and was treated as a controlled medication by the MCPMC during this period.
After enrollment in the MCPMC, patients used complementary and interventional treatments more consistently than prior to enrollment in the clinic. Treatments such as injections, acupuncture, OMT, and PT may reduce opioid medication consumption in the long term or slow the progression of disease for most patients. The improvement in QOL and lack of disease progression in these patients is not objectively measurable; however, the summative progress may be subjectively evaluated through reported pain levels and patient satisfaction.
For MCPMC patients who remained in the clinic, PT and acupuncture attendance was 70% and 75%, respectively. Although these were improvements in adherence for many MCPMC patients, the rates were still below the facility average completion rates of 80% and 81%, respectively. It could be argued that patients with acute pain are typically seen in PT for shorter periods and with fewer possibilities of missing appointments. Conversely, the single active MCPMC patient who attended OMT had a 100% completion rate compared with the average facility OMT attendance of 68%.
Other goals of the MCPMC consist of managing AEs, minimizing ED visits, monitoring for drug abuse and diversion, and improving adherence to pain agreements. The substantial 65% decrease in ED visits can be attributed to the patients’ participation in the MCPMC. Before enrollment, many patients would frequent the ED, because their PCP was not available. The cost savings from minimizing ED visits, provider and staff time, and resources is difficult to measure due to low rates of collections from insurance supplemental to IHS insurance yet is a significant benefit to the IHS facility.
Conclusions
Since the implementation of the MCPMC, patient outcomes have improved due to more consistent drug abuse and diversion surveillance of chronic pain patients rather than performing surveillance because of a suspicion of inappropriate medication use. Frequently using the pain agreement and monitoring parameters constructed a more trusting relationship between the PCP and the patient, and identified patients inappropriate for long-term opioid therapy. Identifying these patients was an unintentional, yet positive outcome.
Additionally, PCPs reported spending half the time with MCPMC patients vs general chronic pain patients. Patients who were not compliant with their pain agreements were discontinued from opioid therapy and were disenrolled from the clinic. Patients who have remained active have become more compliant with their pain agreements and treatment plans than they had been before enrollment. The MCPMC has ultimately relieved a significant burden from primary care and ED providers while improving outcomes and satisfaction of chronic pain patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-38, HHS Publication No. (SMA) 10-4586. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010.
3. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey.
J Pain. 2010;11(11):1230-1239.
4. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila PA 1976). 2006;31(23):
2724-2727.
5. Bolen J, Schieb L, Hootman JM, et al. Differences in the prevalence and impact of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis. 2010;7(3):A64.
6. Schiller JS, Lucas JW, Ward BW, Perogoy JA. Summary health statistics U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat. 2012;10(252). Centers for Disease Control and Prevention Website. http://www.cdc.gov/nchs/data/series/sr_10/sr10_252.pdf. Accessed June 26, 2015.
7. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
8. Rauck RL. What is the case for prescribing long-acting opioids over short-acting opioids for patients with chronic pain? A critical review. Pain Pract. 2009;9(6):468-479.
9. Pesce A, West C, Egan City K, Strickland J. Interpretation of urine drug testing in pain patients. Pain Med. 2012;13(7):868-885.
1. Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-38, HHS Publication No. (SMA) 10-4586. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010.
3. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey.
J Pain. 2010;11(11):1230-1239.
4. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila PA 1976). 2006;31(23):
2724-2727.
5. Bolen J, Schieb L, Hootman JM, et al. Differences in the prevalence and impact of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis. 2010;7(3):A64.
6. Schiller JS, Lucas JW, Ward BW, Perogoy JA. Summary health statistics U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat. 2012;10(252). Centers for Disease Control and Prevention Website. http://www.cdc.gov/nchs/data/series/sr_10/sr10_252.pdf. Accessed June 26, 2015.
7. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
8. Rauck RL. What is the case for prescribing long-acting opioids over short-acting opioids for patients with chronic pain? A critical review. Pain Pract. 2009;9(6):468-479.
9. Pesce A, West C, Egan City K, Strickland J. Interpretation of urine drug testing in pain patients. Pain Med. 2012;13(7):868-885.