Inactivity and increased sedentary time are major public health problems, particularly among older adults.1-3 Inactivity increases with age and produces deleterious effects on physical health, mental health, and quality of life and leads to increased health care costs.4 The high prevalence of a sedentary lifestyle among older veterans may be due to multiple factors, including misconceptions about the health benefits of exercise, lack of motivation, or associating exercise with discomfort or pain. Older veterans living in rural areas are at high risk because they are more sedentary than are urban-dwelling veterans.5 Of veterans aged ≥ 65 years who use health care services in VISN 16, 59% live in rural or highly rural areas.
Given the large number of older veterans and their at-risk status, addressing inactivity among this population is critical. Until recently, few programs existed within the VHA that addressed this need. Despite strong evidence that physical activity helps maintain functional independence and avoids institutionalization of frail elderly veterans, the VHA had no established procedures or guidelines for assessment and counseling.
To address this void, a Geriatric Walking Clinic (GWC) was established at the Central Arkansas Veterans Healthcare System (CAVHS) in March 2013. The GWC developed a patient-centric, home-based program that implements a comprehensive approach to assess, educate, motivate, and activate older veterans to commit to, engage in, and adhere to, a long-term program of regular physical activity primarily in the form of walking. The program uses proven strategies, such as motivational counseling, follow-up phone calls from a nurse, and self-monitoring using pedometers.6-8 Funding for the GWC project was provided by the VHA Office of Geriatrics and Extended Care as part of its Transition to the 21st Century (T21) initiative and by the VHA Office of Rural Health.
Methods
Quality improvement (QI) principles were used to develop the program, which received a nonresearch determination status from the local institutional review board. The GWC is staffed by a registered nurse, health technician, and physician. Both the nurse and the health technician were trained on the use of various assessments. Several tactics were developed to promote patient recruitment to the GWC, including systemwide in-services, an easy-to-use consultation request within the electronic medical record, patient and provider brochures, and informational booths and kiosks. Collaborations were developed with various clinical services to promote referrals. Several other services, such as Primary Care, Geriatrics, the Move! Weight Management Program, Cardiology (including Congestive Heart Failure), Hematology/Oncology, and Mental Health referred patients to the GWC.
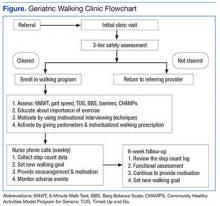
The GWC targets sedentary, community-dwelling veterans aged ≥ 60 years who are able to ambulate in their home without an assistive device, are willing to walk for exercise, and are willing to receive phone calls. All-comers are included in the program. Although most of these veterans have multiple chronic medical problems, only those with absolute contraindications to exercise per the American College of Sports Medicine guidelines and those with any medical condition that is likely to compromise their ability to safely participate in the walking program are excluded (Figure).
First Visit
At the first visit, veterans receive a brief education about GWC, highlighting its potential health benefits. If veterans want to join, they are evaluated using a 3-tier screening assessment to determine the safety of starting a new walking regimen. Veterans who fail the 3-tier safety screening are referred to their primary care physician (PCP) for further assessment (eg, cardiac stress testing) to better define eligibility status. Veterans who pass the screen complete brief tests of physical performance, including gait speed, 6-Minute Walk Test (6MWT), Timed Up and Go test, and Berg Balance Scale.9-12 Participants also complete short surveys that provide useful information about their social support, barriers to exercise, response to physical activity, and usual activity level as measured by Community Healthy Activities Model Program for Seniors.13,14 This information is used to help develop an individualized walking prescription.
After completing the baseline assessments, the GWC staff members help the veteran set realistic goals, using motivational counseling techniques. The veteran receives a walking prescription to walk indoors or outdoors, based on current physical condition, self-identified goals, perceived barriers, and strength of support system; educational material about safe walking; a log for recording daily step count; information on follow-up calls; and an invitation to return for follow-up visits. The veteran also receives a pedometer and is instructed to continue his or her usual routine for the first week. The average daily step count is recorded as the baseline. The veteran is instructed to start the walking program after the baseline week with goals tailored to the personal activity level. For example: Some patients are asked to simply add an extra minute to their walking, whereas others savvy with pedometer numbers are asked to increase their step count.