User login
THE CASE
Steven R,* a 21-year-old man, visited the clinic accompanied by his mother. He did not speak much, and his mother provided his history. Over the previous 2 months, she had overheard him whispering in an agitated voice, even though no one else was nearby. And, lately, he refused to answer or make calls on his cell phone, claiming that if he did it would activate a deadly chip that had been implanted in his brain by evil aliens. He also stopped attending classes at the community college. He occasionally had a few beers with his friends, but he had never been known to abuse alcohol or use other recreational drugs.
How would you proceed with this patient?
* The patient’s name has been changed to protect his identity.
CHARACTERISTICS AND SCOPE OF SCHIZOPHRENIA
Schizophrenia is a psychotic illness in which the individual loses contact with reality and often experiences hallucinations, delusions, or thought disorders. Criteria for schizophrenia described in the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) include signs and symptoms of at least 6 months’ duration, as well as at least one month of active-phase positive and negative symptoms.1
Delusions, hallucinations, disorganized speech, and disorganized behavior are examples of positive symptoms. Negative symptoms include a decrease in the range and intensity of expressed emotions (ie, affective flattening) and a diminished initiation of goal-directed activities (ie, avolition).
Approximately 7 in 1000 people will develop the disorder in their lifetime.2 Schizophrenia is considered a “serious mental illness” because of its chronic course and often poor long-term social and vocational outcomes.3,4 Symptom onset is generally between late adolescence and the mid-30s.5
Getting closer to understanding its origin
Both genetic susceptibility and environmental factors influence the incidence of schizophrenia.4 Newer models of the disease have identified genes (ZDHHC8 and DTNBP1) whose mutations may increase the risk of schizophrenia.6 Physiologic insults during fetal life—hypoxia, maternal infection, maternal stress, and maternal malnutrition—account for a small portion of schizophrenia cases.6
Abnormalities in neurotransmission are the basis for theories on the pathophysiology of schizophrenia. Most of these theories center on either an excess or a deficiency of neurotransmitters, including dopamine, serotonin, and glutamate. Other theories implicate aspartate, glycine, and gamma-aminobutyric acid as part of the neurochemical imbalance of schizophrenia.7
ESTABLISHING A DIAGNOSIS
Although psychotic symptoms may be a prominent part of schizophrenia, not all psychoses indicate a primary psychiatric disorder such as schizophrenia. Broadly, psychoses can be categorized as primary or secondary.
Primary psychoses include schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, and mood disorders (major depressive disorder and borderline personality disorder) with psychotic features.1 Difficulty in distinguishing between these entities can necessitate referral to a psychiatrist.
Secondary psychoses arise from a precursor such as delirium, dementia, medical illness, or adverse effects of medications or illicit substances. Medical illnesses that cause psychotic symptoms include: 5,8
- seizures (especially temporal lobe epilepsy),
- cerebrovascular accidents,
- intracranial space-occupying lesions,
- neuropsychiatric disorders (eg, Wilson’s or Parkinson’s disease),
- endocrine disorders (eg, thyroid or adrenal disease),
- autoimmune disease (eg, systemic lupus erythematosus, Hashimoto encephalopathy),
- deficiencies of vitamins A, B1, B12, or niacin,
- infections (eg, human immunodeficiency virus [HIV], encephalitis, parasites, and prion disease),
- narcolepsy, and
- metabolic disease (eg, acute intermittent porphyria, Tay-Sach’s disease, Niemann-Pick disease).
Several recreational drugs can cause psychotic symptoms: cocaine, amphetamines, cannabis, synthetic cannabinoids, inhalants, opioids, and hallucinogens. Psychotic symptoms can also appear during withdrawal from alcohol (delirium tremens) and from sedative hypnotics such as benzodiazepines. Prescribed medications such as anticholinergics, corticosteroids, dopaminergic agents (L-dopa), stimulants (amphetamines), and interferons can also induce psychotic symptoms.
First rule out causes of secondary psychosis
Rule out causes of secondary psychosis by conducting a detailed history and physical examination and ordering appropriate lab tests and imaging studies. If the patient’s psychosis is of recent onset, make sure the laboratory work-up includes
Consider cranial computed tomography or magnetic resonance imaging if there are focal neurologic deficits or if the patient’s presentation is atypical (eg, new onset psychosis in old age).9 Clinical presentation may also indicate a need for electroencephalography, ceruloplasmin measurement, a dexamethasone suppression test, a corticotropin stimulation test, 24-hour urine porphyrin and copper assays, chest radiography, or cerebrospinal fluid analysis.9
FACTORS TO CONSIDER IN TREATMENT DECISIONS
Although primary care physicians may encounter individuals experiencing their first episode of psychosis, it’s more likely that patients presenting with signs and symptoms of the disorder have been experiencing them for some time and have received no psychiatric care. In both instances, schizophrenia is best managed in conjunction with a psychiatrist until symptoms are stabilized.5 Psychosis does not always require hospitalization. But urgent psychiatry referral is recommended, if possible. Consider admission to a psychiatric inpatient unit for anyone who poses a danger to self or others.8,10
Treatment for schizophrenia is most effective with an interprofessional and collaborative approach that includes medication, psychological treatment, social supports, and primary care clinical management.11,12 The last aspect takes on particular importance given that people with schizophrenia, compared with the general population, have a higher incidence of medical illness, particularly cardiovascular disease.13
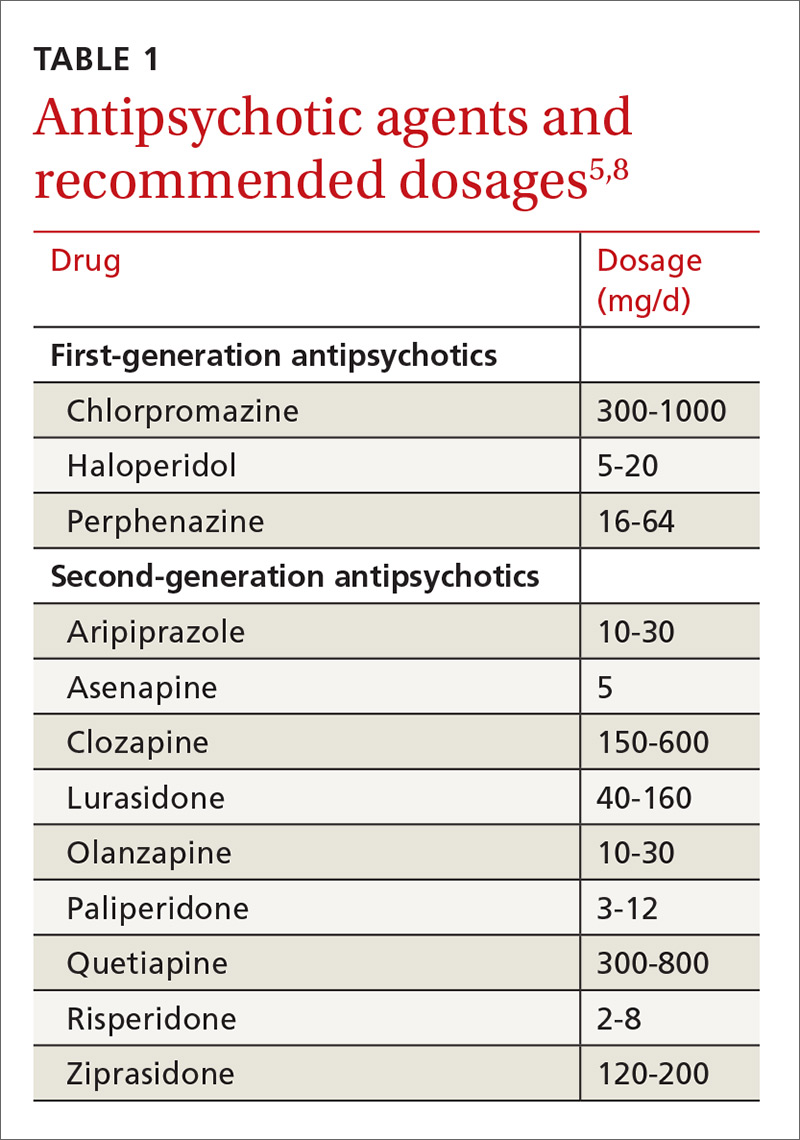
Medications (TABLE 15,8) are grouped into first-generation antipsychotics (FGAs) and second-generation, or atypical, antipsychotics (SGAs), with the 2 classes being equally effective.14-16 Quality of life is also similar at one year for patients treated with either drug class.14
Adverse effects can differ. The main difference between these medications is their adverse effect profiles. FGAs cause extrapyramidal symptoms (dystonia, akathisia, and tardive dyskinesia) more often than SGAs. Among the SGAs, olanzapine, asenapine, paliperidone, clozapine, and quetiapine cause significant weight gain, glucose dysregulation, and lipid abnormalities.5,8,12,17 Clozapine is associated with agranulocytosis, as well. Risperidone causes mild to moderate weight gain.5,8,12,17 Aripiprazole, lurasidone, and ziprasidone are considered weight neutral and cause no significant glucose dysregulation or lipid abnormalities.5,8,12,17 All antipsychotics can cause QT prolongation and neuroleptic malignant syndrome.5,8,12,17
Keys to successful treatment. Antipsychotics are most effective in treating positive symptoms of schizophrenia and show limited, if any, effect on negative or cognitive symptoms.18,19 Give patients an adequate trial of therapy (at least 4 weeks at a therapeutic dose) before discontinuing the drug or offering a different medication.20 All patients who report symptom relief while receiving antipsychotics should receive maintenance therapy.12
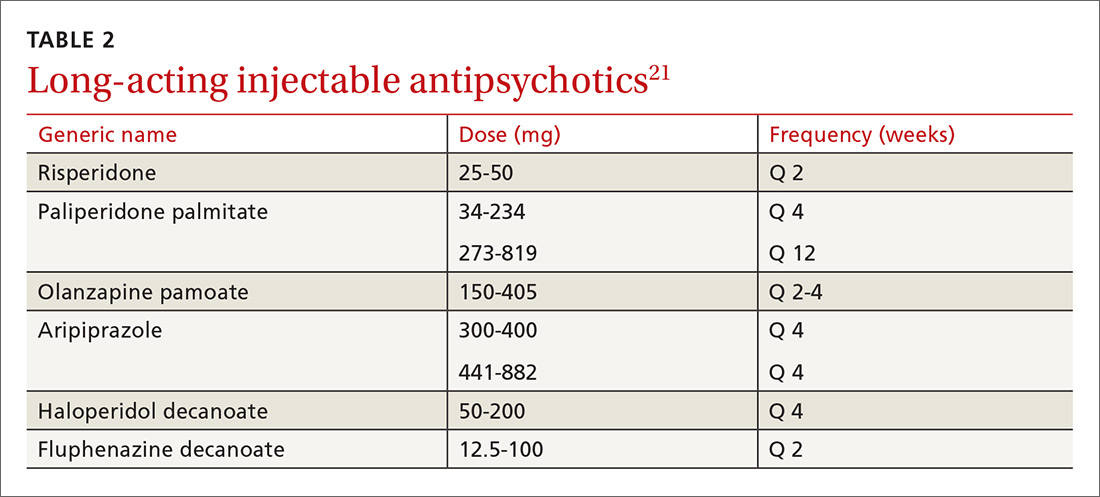
As with all chronic illnesses, success in managing schizophrenia requires patient adherence to the medication regimen. Discontinuation of antipsychotics is a common problem in schizophrenia, resulting in relapse. Long-acting injectable agents (LAIs) were developed to address this problem (TABLE 2).21 Although LAIs are typically used to ensure adherence during maintenance treatment, recent research has suggested they may also be effective for patients with early-phase or first-episode disease.22
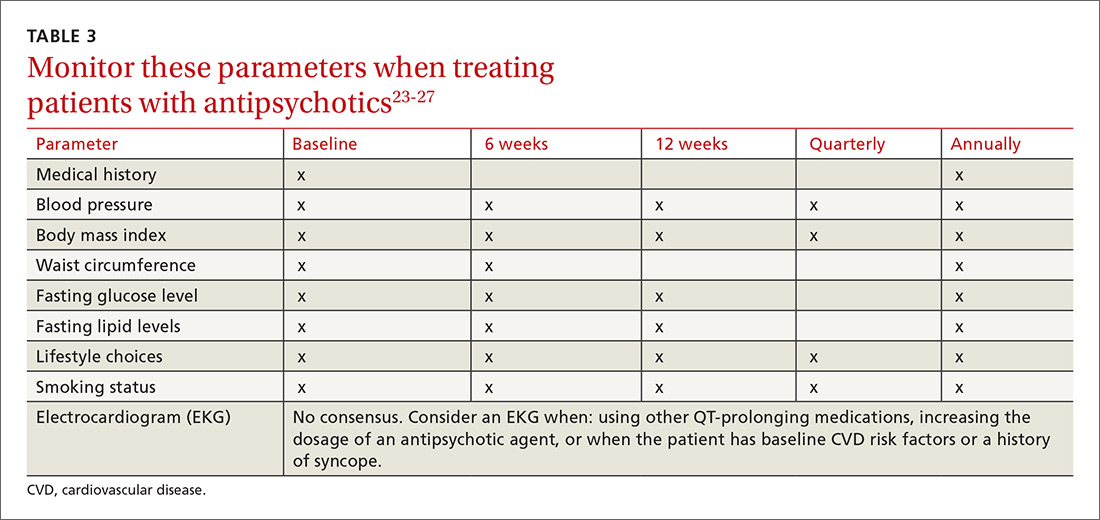
What to watch for. Patients on SGAs may develop metabolic abnormalities, and ongoing monitoring of relevant parameters is key (TABLE 323-27). More frequent monitoring may be necessary in patients with cardiovascular risk factors. Continue antipsychotics for at least 6 months to prevent relapse.12 Also keep in mind the “Choosing Wisely” recommendation from the American Psychiatric Association of not prescribing 2 or more antipsychotics concurrently.28
Adjunctive treatment should also be offered
In addition to receiving medication, patients with schizophrenia should be offered adjunctive therapies such as cognitive behavioral therapy, family intervention, and social skills training.10-12 Among patients with schizophrenia, the incidences of anxiety disorder, panic symptoms, posttraumatic stress disorder, and obsessive compulsive disorder are higher than in the general population.29 To address these conditions, medications such as selective serotonin reuptake inhibitors and anxiolytics can be used simultaneously with antipsychotic agents.
CLINICAL COURSE AND PROGNOSIS CAN VARY
Schizophrenia can have a variable clinical course that includes remissions and exacerbations, or it can follow a more persistently chronic course.
Mortality for patients with schizophrenia is 2 to 3 times higher than that of the general population.30 Most deaths are due to an increased incidence of cardiovascular disease, respiratory illness, cancer, stroke, and other thromboembolic events.30
The lifetime prevalence of suicide attempts among individuals with schizophrenia is 20% to 40%,31 and approximately 5% complete suicide.32 Risk factors include command hallucinations, a history of suicide attempts, intoxication with substances, anxiety, and physical pain.32 Clozapine has been shown to reduce suicide risk and may be considered for patients who are at high risk for suicide.32
Therapeutic response varies among patients with schizophrenia, with one-third remaining symptomatic despite adequate treatment regimens.4
CARE MANAGERS CAN HELP ADDRESS BARRIERS TO CARE
A review of the literature suggests that up to one-third of individuals with serious mental illnesses who have had some contact with the mental health system disengage from care.12 Poor engagement may lead to worse clinical outcomes, with symptom relapse and re-hospitalizations. Disengagement from treatment may indicate a patient’s belief that treatment is not necessary, is not meeting his or her needs, or is not being provided in a collaborative manner.
Although shared decision-making is difficult with patients who have schizophrenia, emerging evidence suggests that this approach coupled with patient-centered care will improve engagement with mental health treatment.12 Models of integrated care are being developed and have shown promise in ensuring access to behavioral health for these patients.34
CASE
The primary care physician talked with Mr. R and his mother about the diagnosis of schizophrenia. He screened for suicide risk, and the patient denied having suicidal thoughts. Both the patient and his mother agreed to his starting medication.
Blood and urine samples were collected for a CBC and ESR, as well as to evaluate renal function, electrolytes, glucose, TSH, vitamin B12, folic acid, ANAs, and HIV antibodies. A serum FTA-ABS test was done, as was a urine culture and sensitivity test and a toxicology screen. Because of the patient’s obesity, the physician decided to prescribe a weight-neutral SGA, aripiprazole 10 mg/d. The physician spoke with the clinic’s care coordinator to schedule an appointment with the psychiatry intake department and to follow up on the phone with the patient and his mother. He also scheduled a follow-up appointment for 2 weeks later.
At the follow-up visit, the patient showed no improvement. His blood and urine test results revealed no metabolic abnormalities or infectious or inflammatory illnesses. His urine toxicology result showed no illicit substances. The physician increased the dosage of aripiprazole to 15 mg/d and asked the patient to return in 2 weeks.
At the next follow-up visit, the patient was more verbal and said he was not hearing voices. His mother also acknowledged an improvement. He had already been scheduled for a psychiatry intake appointment, and he and his mother were reminded about this. Mr. R was also asked to make a follow-up primary care appointment for one month from the current visit.
CORRESPONDENCE
Rajesh (Fnu) Rajesh, MD, MetroHealth Medical Center, 2500 MetroHealth Drive, Cleveland, OH 44109; frajesh@metrohealth.org.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
2. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67-76.
3. Henry LP, Amminger GP, Harris MG, et al. The EPPIC follow-up study of first-episode psychosis: longer-term and clinical and functional outcome 7 years after index admission. J Clin Psychiatry. 2010;71:716-728.
4. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635-645.
5. Holder SD, Wayhs A. Schizophrenia. Am Fam Phys. 2014;90:775-82.
6. Lakhan SE, Vieira KF. Schizophrenia pathophysiology: are we any closer to a complete model? Ann Gen Psychiatry. 2009;8:12.
7. Crismon L, Argo TR, Buckley PF. Schizophrenia. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 9th ed. New York, New York: McGraw-Hill; 2014:1019-1046.
8. Viron M, Baggett T, Hill M, et al. Schizophrenia for primary care providers: how to contribute to the care of a vulnerable patient population. Am J Med. 2012;125:223-230.
9. Freudenreich O, Charles Schulz SC, Goff DC. Initial medical work-up of first-episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3:10-18.
10. National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: Prevention and management. 2014. Available at: http://www.nice.org.uk/Guidance/CG178. Accessed January 3, 2017.
11. Guo X, Zhai J, Liu Z, et al. Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: a randomized 1-year study. Arch Gen Psychiatry. 2010;67:895-904.
12. Kreyenbuhl J, Buchanan RW, Dickerson FB, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2009;36:94-103.
13. Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51:458-465.
14. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006;63:1079-1087.
15. Hartling L, Abou-Setta AM, Dursun S, et al. Antipsychotics in adults with schizophrenia: comparative effectiveness of first-generation versus second-generation medications: a systematic review and meta-analysis. Ann Intern Med. 2012;157:498-511.
16. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209-1223.
17. Tandon R. Antipsychotics in the treatment of schizophrenia: an overview. J Clin Psychiatry. 2011;72(suppl 1):4-8.
18. Salimi K, Jarskog LF, Lieberman JA. Antipsychotic drugs for first-episode schizophrenia: a comparative review. CNS Drugs. 2009;23:837-855.
19. Fusar-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41:892-899.
20. Moore TA, Buchanan RW, Buckley PF, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry. 2007;68:1751-1762.
21. Bera R. Patient outcomes within schizophrenia treatment: a look at the role of long-acting injectable antipsychotics. J Clin Psychiatry. 2014;75(suppl 2):30-33.
22. Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(suppl 3):1-24.
23. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225-233.
24. De Hert M, Vancampfort D, Correll CU, et al. Guidelines for screening and monitoring of cardiometabolic risk in schizophrenia: systematic evaluation. Br J Psychiatry. 2011;199:99-105.
25. Mitchell AJ, Vancampfort D, Sweers K, et al. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders—a systematic review and meta-analysis. Schizophr Bull. 2013;39:306-318.
26. Lieberman JA, Merrill D, Parameswaran S. APA guidance on the use of antipsychotic drugs and cardiac sudden death.
27. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161:1334-1349.
28. American Psychiatric Association. Five things physicians and patients should question. Available at: http://www.choosingwisely.org/societies/american-psychiatric-association/. Accessed February 28, 2017.
29. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35:383-402.
30. Lwin AM, Symeon C, Jan F, et al. Morbidity and mortality in schizophrenia. Br J Hosp Med (Lond). 2011;72:628-630.
31. Pompili M, Amador XF, Girardi P, et al. Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry. 2007;6:10.
32. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(4 suppl):81-90.
33. Druss BG, von Esenwein SA, Compton MT, et al. A randomized trial of medical care management for community mental health settings: the Primary Care Access, Referral, and Evaluation (PCARE) study. Am J Psychiatry. 2010;167:151-159.
34. Gerrity M. Evolving models of behavioral health integration: Evidence update 2010-2015. Milbank Memorial Fund. Available at: https://www.milbank.org/wp-content/uploads/2016/05/Evolv ing-Models-of-BHI.pdf. Accessed January 11, 2018.
THE CASE
Steven R,* a 21-year-old man, visited the clinic accompanied by his mother. He did not speak much, and his mother provided his history. Over the previous 2 months, she had overheard him whispering in an agitated voice, even though no one else was nearby. And, lately, he refused to answer or make calls on his cell phone, claiming that if he did it would activate a deadly chip that had been implanted in his brain by evil aliens. He also stopped attending classes at the community college. He occasionally had a few beers with his friends, but he had never been known to abuse alcohol or use other recreational drugs.
How would you proceed with this patient?
* The patient’s name has been changed to protect his identity.
CHARACTERISTICS AND SCOPE OF SCHIZOPHRENIA
Schizophrenia is a psychotic illness in which the individual loses contact with reality and often experiences hallucinations, delusions, or thought disorders. Criteria for schizophrenia described in the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) include signs and symptoms of at least 6 months’ duration, as well as at least one month of active-phase positive and negative symptoms.1
Delusions, hallucinations, disorganized speech, and disorganized behavior are examples of positive symptoms. Negative symptoms include a decrease in the range and intensity of expressed emotions (ie, affective flattening) and a diminished initiation of goal-directed activities (ie, avolition).
Approximately 7 in 1000 people will develop the disorder in their lifetime.2 Schizophrenia is considered a “serious mental illness” because of its chronic course and often poor long-term social and vocational outcomes.3,4 Symptom onset is generally between late adolescence and the mid-30s.5
Getting closer to understanding its origin
Both genetic susceptibility and environmental factors influence the incidence of schizophrenia.4 Newer models of the disease have identified genes (ZDHHC8 and DTNBP1) whose mutations may increase the risk of schizophrenia.6 Physiologic insults during fetal life—hypoxia, maternal infection, maternal stress, and maternal malnutrition—account for a small portion of schizophrenia cases.6
Abnormalities in neurotransmission are the basis for theories on the pathophysiology of schizophrenia. Most of these theories center on either an excess or a deficiency of neurotransmitters, including dopamine, serotonin, and glutamate. Other theories implicate aspartate, glycine, and gamma-aminobutyric acid as part of the neurochemical imbalance of schizophrenia.7
ESTABLISHING A DIAGNOSIS
Although psychotic symptoms may be a prominent part of schizophrenia, not all psychoses indicate a primary psychiatric disorder such as schizophrenia. Broadly, psychoses can be categorized as primary or secondary.
Primary psychoses include schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, and mood disorders (major depressive disorder and borderline personality disorder) with psychotic features.1 Difficulty in distinguishing between these entities can necessitate referral to a psychiatrist.
Secondary psychoses arise from a precursor such as delirium, dementia, medical illness, or adverse effects of medications or illicit substances. Medical illnesses that cause psychotic symptoms include: 5,8
- seizures (especially temporal lobe epilepsy),
- cerebrovascular accidents,
- intracranial space-occupying lesions,
- neuropsychiatric disorders (eg, Wilson’s or Parkinson’s disease),
- endocrine disorders (eg, thyroid or adrenal disease),
- autoimmune disease (eg, systemic lupus erythematosus, Hashimoto encephalopathy),
- deficiencies of vitamins A, B1, B12, or niacin,
- infections (eg, human immunodeficiency virus [HIV], encephalitis, parasites, and prion disease),
- narcolepsy, and
- metabolic disease (eg, acute intermittent porphyria, Tay-Sach’s disease, Niemann-Pick disease).
Several recreational drugs can cause psychotic symptoms: cocaine, amphetamines, cannabis, synthetic cannabinoids, inhalants, opioids, and hallucinogens. Psychotic symptoms can also appear during withdrawal from alcohol (delirium tremens) and from sedative hypnotics such as benzodiazepines. Prescribed medications such as anticholinergics, corticosteroids, dopaminergic agents (L-dopa), stimulants (amphetamines), and interferons can also induce psychotic symptoms.
First rule out causes of secondary psychosis
Rule out causes of secondary psychosis by conducting a detailed history and physical examination and ordering appropriate lab tests and imaging studies. If the patient’s psychosis is of recent onset, make sure the laboratory work-up includes
Consider cranial computed tomography or magnetic resonance imaging if there are focal neurologic deficits or if the patient’s presentation is atypical (eg, new onset psychosis in old age).9 Clinical presentation may also indicate a need for electroencephalography, ceruloplasmin measurement, a dexamethasone suppression test, a corticotropin stimulation test, 24-hour urine porphyrin and copper assays, chest radiography, or cerebrospinal fluid analysis.9
FACTORS TO CONSIDER IN TREATMENT DECISIONS
Although primary care physicians may encounter individuals experiencing their first episode of psychosis, it’s more likely that patients presenting with signs and symptoms of the disorder have been experiencing them for some time and have received no psychiatric care. In both instances, schizophrenia is best managed in conjunction with a psychiatrist until symptoms are stabilized.5 Psychosis does not always require hospitalization. But urgent psychiatry referral is recommended, if possible. Consider admission to a psychiatric inpatient unit for anyone who poses a danger to self or others.8,10
Treatment for schizophrenia is most effective with an interprofessional and collaborative approach that includes medication, psychological treatment, social supports, and primary care clinical management.11,12 The last aspect takes on particular importance given that people with schizophrenia, compared with the general population, have a higher incidence of medical illness, particularly cardiovascular disease.13
Medications (TABLE 15,8) are grouped into first-generation antipsychotics (FGAs) and second-generation, or atypical, antipsychotics (SGAs), with the 2 classes being equally effective.14-16 Quality of life is also similar at one year for patients treated with either drug class.14
Adverse effects can differ. The main difference between these medications is their adverse effect profiles. FGAs cause extrapyramidal symptoms (dystonia, akathisia, and tardive dyskinesia) more often than SGAs. Among the SGAs, olanzapine, asenapine, paliperidone, clozapine, and quetiapine cause significant weight gain, glucose dysregulation, and lipid abnormalities.5,8,12,17 Clozapine is associated with agranulocytosis, as well. Risperidone causes mild to moderate weight gain.5,8,12,17 Aripiprazole, lurasidone, and ziprasidone are considered weight neutral and cause no significant glucose dysregulation or lipid abnormalities.5,8,12,17 All antipsychotics can cause QT prolongation and neuroleptic malignant syndrome.5,8,12,17
Keys to successful treatment. Antipsychotics are most effective in treating positive symptoms of schizophrenia and show limited, if any, effect on negative or cognitive symptoms.18,19 Give patients an adequate trial of therapy (at least 4 weeks at a therapeutic dose) before discontinuing the drug or offering a different medication.20 All patients who report symptom relief while receiving antipsychotics should receive maintenance therapy.12
As with all chronic illnesses, success in managing schizophrenia requires patient adherence to the medication regimen. Discontinuation of antipsychotics is a common problem in schizophrenia, resulting in relapse. Long-acting injectable agents (LAIs) were developed to address this problem (TABLE 2).21 Although LAIs are typically used to ensure adherence during maintenance treatment, recent research has suggested they may also be effective for patients with early-phase or first-episode disease.22
What to watch for. Patients on SGAs may develop metabolic abnormalities, and ongoing monitoring of relevant parameters is key (TABLE 323-27). More frequent monitoring may be necessary in patients with cardiovascular risk factors. Continue antipsychotics for at least 6 months to prevent relapse.12 Also keep in mind the “Choosing Wisely” recommendation from the American Psychiatric Association of not prescribing 2 or more antipsychotics concurrently.28
Adjunctive treatment should also be offered
In addition to receiving medication, patients with schizophrenia should be offered adjunctive therapies such as cognitive behavioral therapy, family intervention, and social skills training.10-12 Among patients with schizophrenia, the incidences of anxiety disorder, panic symptoms, posttraumatic stress disorder, and obsessive compulsive disorder are higher than in the general population.29 To address these conditions, medications such as selective serotonin reuptake inhibitors and anxiolytics can be used simultaneously with antipsychotic agents.
CLINICAL COURSE AND PROGNOSIS CAN VARY
Schizophrenia can have a variable clinical course that includes remissions and exacerbations, or it can follow a more persistently chronic course.
Mortality for patients with schizophrenia is 2 to 3 times higher than that of the general population.30 Most deaths are due to an increased incidence of cardiovascular disease, respiratory illness, cancer, stroke, and other thromboembolic events.30
The lifetime prevalence of suicide attempts among individuals with schizophrenia is 20% to 40%,31 and approximately 5% complete suicide.32 Risk factors include command hallucinations, a history of suicide attempts, intoxication with substances, anxiety, and physical pain.32 Clozapine has been shown to reduce suicide risk and may be considered for patients who are at high risk for suicide.32
Therapeutic response varies among patients with schizophrenia, with one-third remaining symptomatic despite adequate treatment regimens.4
CARE MANAGERS CAN HELP ADDRESS BARRIERS TO CARE
A review of the literature suggests that up to one-third of individuals with serious mental illnesses who have had some contact with the mental health system disengage from care.12 Poor engagement may lead to worse clinical outcomes, with symptom relapse and re-hospitalizations. Disengagement from treatment may indicate a patient’s belief that treatment is not necessary, is not meeting his or her needs, or is not being provided in a collaborative manner.
Although shared decision-making is difficult with patients who have schizophrenia, emerging evidence suggests that this approach coupled with patient-centered care will improve engagement with mental health treatment.12 Models of integrated care are being developed and have shown promise in ensuring access to behavioral health for these patients.34
CASE
The primary care physician talked with Mr. R and his mother about the diagnosis of schizophrenia. He screened for suicide risk, and the patient denied having suicidal thoughts. Both the patient and his mother agreed to his starting medication.
Blood and urine samples were collected for a CBC and ESR, as well as to evaluate renal function, electrolytes, glucose, TSH, vitamin B12, folic acid, ANAs, and HIV antibodies. A serum FTA-ABS test was done, as was a urine culture and sensitivity test and a toxicology screen. Because of the patient’s obesity, the physician decided to prescribe a weight-neutral SGA, aripiprazole 10 mg/d. The physician spoke with the clinic’s care coordinator to schedule an appointment with the psychiatry intake department and to follow up on the phone with the patient and his mother. He also scheduled a follow-up appointment for 2 weeks later.
At the follow-up visit, the patient showed no improvement. His blood and urine test results revealed no metabolic abnormalities or infectious or inflammatory illnesses. His urine toxicology result showed no illicit substances. The physician increased the dosage of aripiprazole to 15 mg/d and asked the patient to return in 2 weeks.
At the next follow-up visit, the patient was more verbal and said he was not hearing voices. His mother also acknowledged an improvement. He had already been scheduled for a psychiatry intake appointment, and he and his mother were reminded about this. Mr. R was also asked to make a follow-up primary care appointment for one month from the current visit.
CORRESPONDENCE
Rajesh (Fnu) Rajesh, MD, MetroHealth Medical Center, 2500 MetroHealth Drive, Cleveland, OH 44109; frajesh@metrohealth.org.
THE CASE
Steven R,* a 21-year-old man, visited the clinic accompanied by his mother. He did not speak much, and his mother provided his history. Over the previous 2 months, she had overheard him whispering in an agitated voice, even though no one else was nearby. And, lately, he refused to answer or make calls on his cell phone, claiming that if he did it would activate a deadly chip that had been implanted in his brain by evil aliens. He also stopped attending classes at the community college. He occasionally had a few beers with his friends, but he had never been known to abuse alcohol or use other recreational drugs.
How would you proceed with this patient?
* The patient’s name has been changed to protect his identity.
CHARACTERISTICS AND SCOPE OF SCHIZOPHRENIA
Schizophrenia is a psychotic illness in which the individual loses contact with reality and often experiences hallucinations, delusions, or thought disorders. Criteria for schizophrenia described in the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) include signs and symptoms of at least 6 months’ duration, as well as at least one month of active-phase positive and negative symptoms.1
Delusions, hallucinations, disorganized speech, and disorganized behavior are examples of positive symptoms. Negative symptoms include a decrease in the range and intensity of expressed emotions (ie, affective flattening) and a diminished initiation of goal-directed activities (ie, avolition).
Approximately 7 in 1000 people will develop the disorder in their lifetime.2 Schizophrenia is considered a “serious mental illness” because of its chronic course and often poor long-term social and vocational outcomes.3,4 Symptom onset is generally between late adolescence and the mid-30s.5
Getting closer to understanding its origin
Both genetic susceptibility and environmental factors influence the incidence of schizophrenia.4 Newer models of the disease have identified genes (ZDHHC8 and DTNBP1) whose mutations may increase the risk of schizophrenia.6 Physiologic insults during fetal life—hypoxia, maternal infection, maternal stress, and maternal malnutrition—account for a small portion of schizophrenia cases.6
Abnormalities in neurotransmission are the basis for theories on the pathophysiology of schizophrenia. Most of these theories center on either an excess or a deficiency of neurotransmitters, including dopamine, serotonin, and glutamate. Other theories implicate aspartate, glycine, and gamma-aminobutyric acid as part of the neurochemical imbalance of schizophrenia.7
ESTABLISHING A DIAGNOSIS
Although psychotic symptoms may be a prominent part of schizophrenia, not all psychoses indicate a primary psychiatric disorder such as schizophrenia. Broadly, psychoses can be categorized as primary or secondary.
Primary psychoses include schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, and mood disorders (major depressive disorder and borderline personality disorder) with psychotic features.1 Difficulty in distinguishing between these entities can necessitate referral to a psychiatrist.
Secondary psychoses arise from a precursor such as delirium, dementia, medical illness, or adverse effects of medications or illicit substances. Medical illnesses that cause psychotic symptoms include: 5,8
- seizures (especially temporal lobe epilepsy),
- cerebrovascular accidents,
- intracranial space-occupying lesions,
- neuropsychiatric disorders (eg, Wilson’s or Parkinson’s disease),
- endocrine disorders (eg, thyroid or adrenal disease),
- autoimmune disease (eg, systemic lupus erythematosus, Hashimoto encephalopathy),
- deficiencies of vitamins A, B1, B12, or niacin,
- infections (eg, human immunodeficiency virus [HIV], encephalitis, parasites, and prion disease),
- narcolepsy, and
- metabolic disease (eg, acute intermittent porphyria, Tay-Sach’s disease, Niemann-Pick disease).
Several recreational drugs can cause psychotic symptoms: cocaine, amphetamines, cannabis, synthetic cannabinoids, inhalants, opioids, and hallucinogens. Psychotic symptoms can also appear during withdrawal from alcohol (delirium tremens) and from sedative hypnotics such as benzodiazepines. Prescribed medications such as anticholinergics, corticosteroids, dopaminergic agents (L-dopa), stimulants (amphetamines), and interferons can also induce psychotic symptoms.
First rule out causes of secondary psychosis
Rule out causes of secondary psychosis by conducting a detailed history and physical examination and ordering appropriate lab tests and imaging studies. If the patient’s psychosis is of recent onset, make sure the laboratory work-up includes
Consider cranial computed tomography or magnetic resonance imaging if there are focal neurologic deficits or if the patient’s presentation is atypical (eg, new onset psychosis in old age).9 Clinical presentation may also indicate a need for electroencephalography, ceruloplasmin measurement, a dexamethasone suppression test, a corticotropin stimulation test, 24-hour urine porphyrin and copper assays, chest radiography, or cerebrospinal fluid analysis.9
FACTORS TO CONSIDER IN TREATMENT DECISIONS
Although primary care physicians may encounter individuals experiencing their first episode of psychosis, it’s more likely that patients presenting with signs and symptoms of the disorder have been experiencing them for some time and have received no psychiatric care. In both instances, schizophrenia is best managed in conjunction with a psychiatrist until symptoms are stabilized.5 Psychosis does not always require hospitalization. But urgent psychiatry referral is recommended, if possible. Consider admission to a psychiatric inpatient unit for anyone who poses a danger to self or others.8,10
Treatment for schizophrenia is most effective with an interprofessional and collaborative approach that includes medication, psychological treatment, social supports, and primary care clinical management.11,12 The last aspect takes on particular importance given that people with schizophrenia, compared with the general population, have a higher incidence of medical illness, particularly cardiovascular disease.13
Medications (TABLE 15,8) are grouped into first-generation antipsychotics (FGAs) and second-generation, or atypical, antipsychotics (SGAs), with the 2 classes being equally effective.14-16 Quality of life is also similar at one year for patients treated with either drug class.14
Adverse effects can differ. The main difference between these medications is their adverse effect profiles. FGAs cause extrapyramidal symptoms (dystonia, akathisia, and tardive dyskinesia) more often than SGAs. Among the SGAs, olanzapine, asenapine, paliperidone, clozapine, and quetiapine cause significant weight gain, glucose dysregulation, and lipid abnormalities.5,8,12,17 Clozapine is associated with agranulocytosis, as well. Risperidone causes mild to moderate weight gain.5,8,12,17 Aripiprazole, lurasidone, and ziprasidone are considered weight neutral and cause no significant glucose dysregulation or lipid abnormalities.5,8,12,17 All antipsychotics can cause QT prolongation and neuroleptic malignant syndrome.5,8,12,17
Keys to successful treatment. Antipsychotics are most effective in treating positive symptoms of schizophrenia and show limited, if any, effect on negative or cognitive symptoms.18,19 Give patients an adequate trial of therapy (at least 4 weeks at a therapeutic dose) before discontinuing the drug or offering a different medication.20 All patients who report symptom relief while receiving antipsychotics should receive maintenance therapy.12
As with all chronic illnesses, success in managing schizophrenia requires patient adherence to the medication regimen. Discontinuation of antipsychotics is a common problem in schizophrenia, resulting in relapse. Long-acting injectable agents (LAIs) were developed to address this problem (TABLE 2).21 Although LAIs are typically used to ensure adherence during maintenance treatment, recent research has suggested they may also be effective for patients with early-phase or first-episode disease.22
What to watch for. Patients on SGAs may develop metabolic abnormalities, and ongoing monitoring of relevant parameters is key (TABLE 323-27). More frequent monitoring may be necessary in patients with cardiovascular risk factors. Continue antipsychotics for at least 6 months to prevent relapse.12 Also keep in mind the “Choosing Wisely” recommendation from the American Psychiatric Association of not prescribing 2 or more antipsychotics concurrently.28
Adjunctive treatment should also be offered
In addition to receiving medication, patients with schizophrenia should be offered adjunctive therapies such as cognitive behavioral therapy, family intervention, and social skills training.10-12 Among patients with schizophrenia, the incidences of anxiety disorder, panic symptoms, posttraumatic stress disorder, and obsessive compulsive disorder are higher than in the general population.29 To address these conditions, medications such as selective serotonin reuptake inhibitors and anxiolytics can be used simultaneously with antipsychotic agents.
CLINICAL COURSE AND PROGNOSIS CAN VARY
Schizophrenia can have a variable clinical course that includes remissions and exacerbations, or it can follow a more persistently chronic course.
Mortality for patients with schizophrenia is 2 to 3 times higher than that of the general population.30 Most deaths are due to an increased incidence of cardiovascular disease, respiratory illness, cancer, stroke, and other thromboembolic events.30
The lifetime prevalence of suicide attempts among individuals with schizophrenia is 20% to 40%,31 and approximately 5% complete suicide.32 Risk factors include command hallucinations, a history of suicide attempts, intoxication with substances, anxiety, and physical pain.32 Clozapine has been shown to reduce suicide risk and may be considered for patients who are at high risk for suicide.32
Therapeutic response varies among patients with schizophrenia, with one-third remaining symptomatic despite adequate treatment regimens.4
CARE MANAGERS CAN HELP ADDRESS BARRIERS TO CARE
A review of the literature suggests that up to one-third of individuals with serious mental illnesses who have had some contact with the mental health system disengage from care.12 Poor engagement may lead to worse clinical outcomes, with symptom relapse and re-hospitalizations. Disengagement from treatment may indicate a patient’s belief that treatment is not necessary, is not meeting his or her needs, or is not being provided in a collaborative manner.
Although shared decision-making is difficult with patients who have schizophrenia, emerging evidence suggests that this approach coupled with patient-centered care will improve engagement with mental health treatment.12 Models of integrated care are being developed and have shown promise in ensuring access to behavioral health for these patients.34
CASE
The primary care physician talked with Mr. R and his mother about the diagnosis of schizophrenia. He screened for suicide risk, and the patient denied having suicidal thoughts. Both the patient and his mother agreed to his starting medication.
Blood and urine samples were collected for a CBC and ESR, as well as to evaluate renal function, electrolytes, glucose, TSH, vitamin B12, folic acid, ANAs, and HIV antibodies. A serum FTA-ABS test was done, as was a urine culture and sensitivity test and a toxicology screen. Because of the patient’s obesity, the physician decided to prescribe a weight-neutral SGA, aripiprazole 10 mg/d. The physician spoke with the clinic’s care coordinator to schedule an appointment with the psychiatry intake department and to follow up on the phone with the patient and his mother. He also scheduled a follow-up appointment for 2 weeks later.
At the follow-up visit, the patient showed no improvement. His blood and urine test results revealed no metabolic abnormalities or infectious or inflammatory illnesses. His urine toxicology result showed no illicit substances. The physician increased the dosage of aripiprazole to 15 mg/d and asked the patient to return in 2 weeks.
At the next follow-up visit, the patient was more verbal and said he was not hearing voices. His mother also acknowledged an improvement. He had already been scheduled for a psychiatry intake appointment, and he and his mother were reminded about this. Mr. R was also asked to make a follow-up primary care appointment for one month from the current visit.
CORRESPONDENCE
Rajesh (Fnu) Rajesh, MD, MetroHealth Medical Center, 2500 MetroHealth Drive, Cleveland, OH 44109; frajesh@metrohealth.org.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
2. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67-76.
3. Henry LP, Amminger GP, Harris MG, et al. The EPPIC follow-up study of first-episode psychosis: longer-term and clinical and functional outcome 7 years after index admission. J Clin Psychiatry. 2010;71:716-728.
4. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635-645.
5. Holder SD, Wayhs A. Schizophrenia. Am Fam Phys. 2014;90:775-82.
6. Lakhan SE, Vieira KF. Schizophrenia pathophysiology: are we any closer to a complete model? Ann Gen Psychiatry. 2009;8:12.
7. Crismon L, Argo TR, Buckley PF. Schizophrenia. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 9th ed. New York, New York: McGraw-Hill; 2014:1019-1046.
8. Viron M, Baggett T, Hill M, et al. Schizophrenia for primary care providers: how to contribute to the care of a vulnerable patient population. Am J Med. 2012;125:223-230.
9. Freudenreich O, Charles Schulz SC, Goff DC. Initial medical work-up of first-episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3:10-18.
10. National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: Prevention and management. 2014. Available at: http://www.nice.org.uk/Guidance/CG178. Accessed January 3, 2017.
11. Guo X, Zhai J, Liu Z, et al. Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: a randomized 1-year study. Arch Gen Psychiatry. 2010;67:895-904.
12. Kreyenbuhl J, Buchanan RW, Dickerson FB, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2009;36:94-103.
13. Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51:458-465.
14. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006;63:1079-1087.
15. Hartling L, Abou-Setta AM, Dursun S, et al. Antipsychotics in adults with schizophrenia: comparative effectiveness of first-generation versus second-generation medications: a systematic review and meta-analysis. Ann Intern Med. 2012;157:498-511.
16. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209-1223.
17. Tandon R. Antipsychotics in the treatment of schizophrenia: an overview. J Clin Psychiatry. 2011;72(suppl 1):4-8.
18. Salimi K, Jarskog LF, Lieberman JA. Antipsychotic drugs for first-episode schizophrenia: a comparative review. CNS Drugs. 2009;23:837-855.
19. Fusar-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41:892-899.
20. Moore TA, Buchanan RW, Buckley PF, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry. 2007;68:1751-1762.
21. Bera R. Patient outcomes within schizophrenia treatment: a look at the role of long-acting injectable antipsychotics. J Clin Psychiatry. 2014;75(suppl 2):30-33.
22. Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(suppl 3):1-24.
23. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225-233.
24. De Hert M, Vancampfort D, Correll CU, et al. Guidelines for screening and monitoring of cardiometabolic risk in schizophrenia: systematic evaluation. Br J Psychiatry. 2011;199:99-105.
25. Mitchell AJ, Vancampfort D, Sweers K, et al. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders—a systematic review and meta-analysis. Schizophr Bull. 2013;39:306-318.
26. Lieberman JA, Merrill D, Parameswaran S. APA guidance on the use of antipsychotic drugs and cardiac sudden death.
27. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161:1334-1349.
28. American Psychiatric Association. Five things physicians and patients should question. Available at: http://www.choosingwisely.org/societies/american-psychiatric-association/. Accessed February 28, 2017.
29. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35:383-402.
30. Lwin AM, Symeon C, Jan F, et al. Morbidity and mortality in schizophrenia. Br J Hosp Med (Lond). 2011;72:628-630.
31. Pompili M, Amador XF, Girardi P, et al. Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry. 2007;6:10.
32. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(4 suppl):81-90.
33. Druss BG, von Esenwein SA, Compton MT, et al. A randomized trial of medical care management for community mental health settings: the Primary Care Access, Referral, and Evaluation (PCARE) study. Am J Psychiatry. 2010;167:151-159.
34. Gerrity M. Evolving models of behavioral health integration: Evidence update 2010-2015. Milbank Memorial Fund. Available at: https://www.milbank.org/wp-content/uploads/2016/05/Evolv ing-Models-of-BHI.pdf. Accessed January 11, 2018.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
2. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67-76.
3. Henry LP, Amminger GP, Harris MG, et al. The EPPIC follow-up study of first-episode psychosis: longer-term and clinical and functional outcome 7 years after index admission. J Clin Psychiatry. 2010;71:716-728.
4. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635-645.
5. Holder SD, Wayhs A. Schizophrenia. Am Fam Phys. 2014;90:775-82.
6. Lakhan SE, Vieira KF. Schizophrenia pathophysiology: are we any closer to a complete model? Ann Gen Psychiatry. 2009;8:12.
7. Crismon L, Argo TR, Buckley PF. Schizophrenia. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 9th ed. New York, New York: McGraw-Hill; 2014:1019-1046.
8. Viron M, Baggett T, Hill M, et al. Schizophrenia for primary care providers: how to contribute to the care of a vulnerable patient population. Am J Med. 2012;125:223-230.
9. Freudenreich O, Charles Schulz SC, Goff DC. Initial medical work-up of first-episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3:10-18.
10. National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: Prevention and management. 2014. Available at: http://www.nice.org.uk/Guidance/CG178. Accessed January 3, 2017.
11. Guo X, Zhai J, Liu Z, et al. Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: a randomized 1-year study. Arch Gen Psychiatry. 2010;67:895-904.
12. Kreyenbuhl J, Buchanan RW, Dickerson FB, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2009;36:94-103.
13. Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51:458-465.
14. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006;63:1079-1087.
15. Hartling L, Abou-Setta AM, Dursun S, et al. Antipsychotics in adults with schizophrenia: comparative effectiveness of first-generation versus second-generation medications: a systematic review and meta-analysis. Ann Intern Med. 2012;157:498-511.
16. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209-1223.
17. Tandon R. Antipsychotics in the treatment of schizophrenia: an overview. J Clin Psychiatry. 2011;72(suppl 1):4-8.
18. Salimi K, Jarskog LF, Lieberman JA. Antipsychotic drugs for first-episode schizophrenia: a comparative review. CNS Drugs. 2009;23:837-855.
19. Fusar-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41:892-899.
20. Moore TA, Buchanan RW, Buckley PF, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry. 2007;68:1751-1762.
21. Bera R. Patient outcomes within schizophrenia treatment: a look at the role of long-acting injectable antipsychotics. J Clin Psychiatry. 2014;75(suppl 2):30-33.
22. Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(suppl 3):1-24.
23. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225-233.
24. De Hert M, Vancampfort D, Correll CU, et al. Guidelines for screening and monitoring of cardiometabolic risk in schizophrenia: systematic evaluation. Br J Psychiatry. 2011;199:99-105.
25. Mitchell AJ, Vancampfort D, Sweers K, et al. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders—a systematic review and meta-analysis. Schizophr Bull. 2013;39:306-318.
26. Lieberman JA, Merrill D, Parameswaran S. APA guidance on the use of antipsychotic drugs and cardiac sudden death.
27. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161:1334-1349.
28. American Psychiatric Association. Five things physicians and patients should question. Available at: http://www.choosingwisely.org/societies/american-psychiatric-association/. Accessed February 28, 2017.
29. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35:383-402.
30. Lwin AM, Symeon C, Jan F, et al. Morbidity and mortality in schizophrenia. Br J Hosp Med (Lond). 2011;72:628-630.
31. Pompili M, Amador XF, Girardi P, et al. Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry. 2007;6:10.
32. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(4 suppl):81-90.
33. Druss BG, von Esenwein SA, Compton MT, et al. A randomized trial of medical care management for community mental health settings: the Primary Care Access, Referral, and Evaluation (PCARE) study. Am J Psychiatry. 2010;167:151-159.
34. Gerrity M. Evolving models of behavioral health integration: Evidence update 2010-2015. Milbank Memorial Fund. Available at: https://www.milbank.org/wp-content/uploads/2016/05/Evolv ing-Models-of-BHI.pdf. Accessed January 11, 2018.