User login
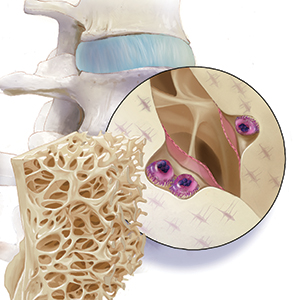
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.