User login
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
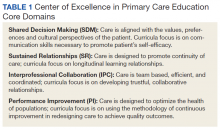
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
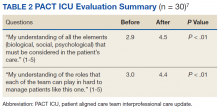
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.