User login
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
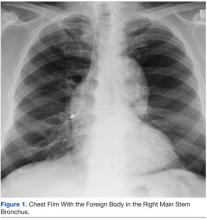
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
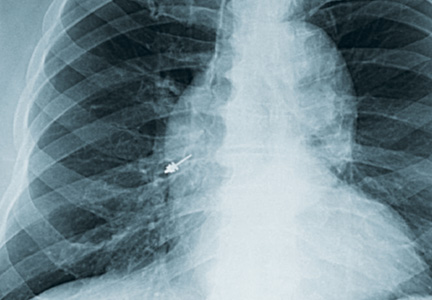
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.