User login
Highlights from the ‘Updates in ACS’ session (VIDEO)
Hospital Medicine 2019 attendees outlined their key takeaways from the Updates in Acute Coronary Syndrome session, presented by Jeffrey Trost, MD, of Johns Hopkins University, Baltimore.

Dr. Trost’s discussion focused on the relationship between dual antiplatelet therapy, in-stent thrombosis, and in-stent restenosis. He also explored the diagnostic role of fractional flow reserve, and he outlined effective approaches to PCSK9 inhibitor use.
Hospital Medicine 2019 attendees outlined their key takeaways from the Updates in Acute Coronary Syndrome session, presented by Jeffrey Trost, MD, of Johns Hopkins University, Baltimore.

Dr. Trost’s discussion focused on the relationship between dual antiplatelet therapy, in-stent thrombosis, and in-stent restenosis. He also explored the diagnostic role of fractional flow reserve, and he outlined effective approaches to PCSK9 inhibitor use.
Hospital Medicine 2019 attendees outlined their key takeaways from the Updates in Acute Coronary Syndrome session, presented by Jeffrey Trost, MD, of Johns Hopkins University, Baltimore.

Dr. Trost’s discussion focused on the relationship between dual antiplatelet therapy, in-stent thrombosis, and in-stent restenosis. He also explored the diagnostic role of fractional flow reserve, and he outlined effective approaches to PCSK9 inhibitor use.
REPORTING FROM HM19
HM19: Pediatric medical and surgical co-management
Anticipatory and prevention-heavy approach
Presenter
Erin Shaughnessy, MD, MSHCM
Session title
Reaching Across the Aisle: Pediatric Co-Management with Surgery and Subspecialists
Session summary
Dr. Shaughnessy articulated a balanced approach to the importance of careful selection of patients needing to be co-managed by pediatric hospitalists. She compared two personal and very different experiences.
She initially managed a well-developed surgical co-management service at a quaternary, academic, free-standing children’s hospital, in which surgeons and subspecialists also admitted and managed patients to their own services. Currently, Dr. Shaughnessy is a division chief at Phoenix Children’s Hospital, a free-standing children’s hospital with a community hospital background, in which hospitalists admit most, if not all the patients, while subspecialty services have been transitioning only recently to having their own admitting services and employing the ideas of limited co-management.
She reminded the HM19 audience of the essential principles of co-management: shared responsibility, authority and accountability for the care of a hospitalized patient, discussing the scenarios, both from literature and real life, in which the line could become blurry at times.
Many pediatric programs are moving away from a traditional consultation model, Dr. Shaughnessy said, in which a consult is called for a new or a persistent problem with a patient, and where a consulting team signs off upon the resolved issue.
The more modern co-management model infuses a need for anticipatory and prevention-heavy approach, intertwined with fiscally responsible ideas that must be palatable for all: administration, hospitalists, and patients.
Dr. Shaughnessy reviewed a number of articles from both adult and pediatric literature with varied results, some that have shown decreased length of stay, decreased number of medical complications, decreased readmissions, decreased number of tests, but some that have also shown an increase in median hospital costs, emphasizing perhaps the importance of context in which one practices.
Finally, she identified patient selection, collaborative relationships, clear roles delineation, and excellence in communication as four main factors deciding the faith of a co-management model.
Key takeaways for HM
1. Careful selection of patients to be co-managed is essential and can prevent potential increase in costs and negative outcomes.
2. Success in medical and surgical co-management relies on well-delineated roles, collaborative culture, and immaculate communication.
Dr. Giordano is a pediatric neurosurgery hospitalist and assistant professor in pediatrics at Columbia University Irving Medical Center in New York.
Anticipatory and prevention-heavy approach
Anticipatory and prevention-heavy approach
Presenter
Erin Shaughnessy, MD, MSHCM
Session title
Reaching Across the Aisle: Pediatric Co-Management with Surgery and Subspecialists
Session summary
Dr. Shaughnessy articulated a balanced approach to the importance of careful selection of patients needing to be co-managed by pediatric hospitalists. She compared two personal and very different experiences.
She initially managed a well-developed surgical co-management service at a quaternary, academic, free-standing children’s hospital, in which surgeons and subspecialists also admitted and managed patients to their own services. Currently, Dr. Shaughnessy is a division chief at Phoenix Children’s Hospital, a free-standing children’s hospital with a community hospital background, in which hospitalists admit most, if not all the patients, while subspecialty services have been transitioning only recently to having their own admitting services and employing the ideas of limited co-management.
She reminded the HM19 audience of the essential principles of co-management: shared responsibility, authority and accountability for the care of a hospitalized patient, discussing the scenarios, both from literature and real life, in which the line could become blurry at times.
Many pediatric programs are moving away from a traditional consultation model, Dr. Shaughnessy said, in which a consult is called for a new or a persistent problem with a patient, and where a consulting team signs off upon the resolved issue.
The more modern co-management model infuses a need for anticipatory and prevention-heavy approach, intertwined with fiscally responsible ideas that must be palatable for all: administration, hospitalists, and patients.
Dr. Shaughnessy reviewed a number of articles from both adult and pediatric literature with varied results, some that have shown decreased length of stay, decreased number of medical complications, decreased readmissions, decreased number of tests, but some that have also shown an increase in median hospital costs, emphasizing perhaps the importance of context in which one practices.
Finally, she identified patient selection, collaborative relationships, clear roles delineation, and excellence in communication as four main factors deciding the faith of a co-management model.
Key takeaways for HM
1. Careful selection of patients to be co-managed is essential and can prevent potential increase in costs and negative outcomes.
2. Success in medical and surgical co-management relies on well-delineated roles, collaborative culture, and immaculate communication.
Dr. Giordano is a pediatric neurosurgery hospitalist and assistant professor in pediatrics at Columbia University Irving Medical Center in New York.
Presenter
Erin Shaughnessy, MD, MSHCM
Session title
Reaching Across the Aisle: Pediatric Co-Management with Surgery and Subspecialists
Session summary
Dr. Shaughnessy articulated a balanced approach to the importance of careful selection of patients needing to be co-managed by pediatric hospitalists. She compared two personal and very different experiences.
She initially managed a well-developed surgical co-management service at a quaternary, academic, free-standing children’s hospital, in which surgeons and subspecialists also admitted and managed patients to their own services. Currently, Dr. Shaughnessy is a division chief at Phoenix Children’s Hospital, a free-standing children’s hospital with a community hospital background, in which hospitalists admit most, if not all the patients, while subspecialty services have been transitioning only recently to having their own admitting services and employing the ideas of limited co-management.
She reminded the HM19 audience of the essential principles of co-management: shared responsibility, authority and accountability for the care of a hospitalized patient, discussing the scenarios, both from literature and real life, in which the line could become blurry at times.
Many pediatric programs are moving away from a traditional consultation model, Dr. Shaughnessy said, in which a consult is called for a new or a persistent problem with a patient, and where a consulting team signs off upon the resolved issue.
The more modern co-management model infuses a need for anticipatory and prevention-heavy approach, intertwined with fiscally responsible ideas that must be palatable for all: administration, hospitalists, and patients.
Dr. Shaughnessy reviewed a number of articles from both adult and pediatric literature with varied results, some that have shown decreased length of stay, decreased number of medical complications, decreased readmissions, decreased number of tests, but some that have also shown an increase in median hospital costs, emphasizing perhaps the importance of context in which one practices.
Finally, she identified patient selection, collaborative relationships, clear roles delineation, and excellence in communication as four main factors deciding the faith of a co-management model.
Key takeaways for HM
1. Careful selection of patients to be co-managed is essential and can prevent potential increase in costs and negative outcomes.
2. Success in medical and surgical co-management relies on well-delineated roles, collaborative culture, and immaculate communication.
Dr. Giordano is a pediatric neurosurgery hospitalist and assistant professor in pediatrics at Columbia University Irving Medical Center in New York.
HM19: Lessons from the Update in Hospital Medicine session

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.
REPORTING FROM HM19
HM19: Key takeaways on quality and innovation

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.
REPORTING FROM HM19
‘Update in Hospital Medicine’ offered practice pearls at HM19
Studies that question common practices
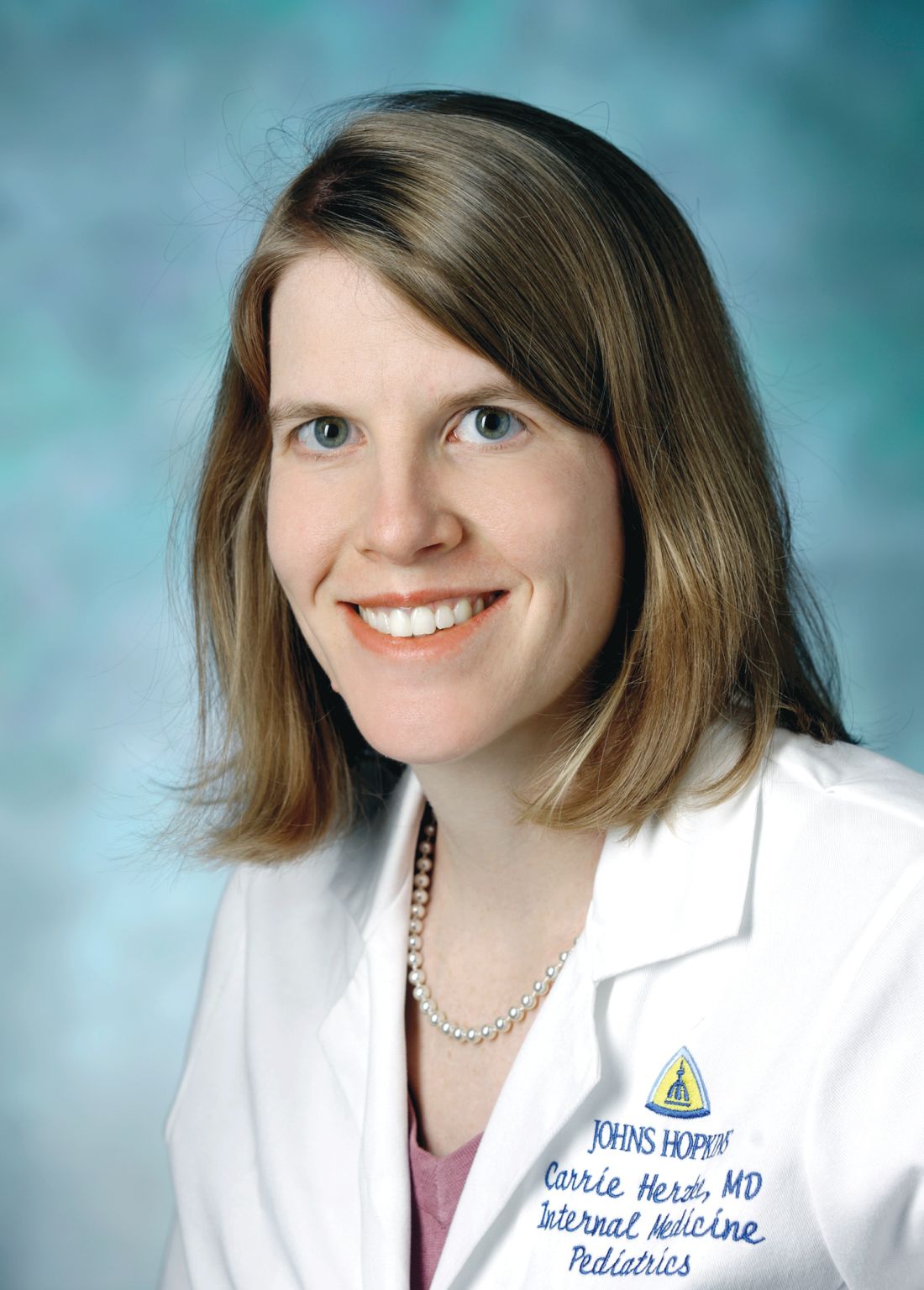
On the big stage at HM19 in late March, Carrie Herzke, MD, FAAP, FACP, SFHM, and Christopher Moriates, MD, FACP, SFHM, undertook the daunting task of summarizing a year’s worth of research relevant to the practice of hospital medicine – all within the span of an hour.
As has been standard with the “Update in Hospital Medicine” session at previous SHM Annual Conferences, the presenters touched on lighter topics in the medical literature: a prospective cohort study that found drinking coffee was inversely associated with mortality, even for those who drink up to eight cups a day; a cross-sectional observational study in which patients noted that what a physician wears is an important consideration for them during care, with a white coat preferred over formal attire as the most highly rated preference in a clinical care setting; and a study from a pediatric journal in which researchers calculated the average transit time for a Lego figurine head ingested by an adult.
But Dr. Herzke and Dr. Moriates mainly covered more serious subjects. In an interview before the session, Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, said she and Dr. Moriates chose studies across the fields of infectious diseases, cardiology, and hematology that should make hospitalists question common practices and consider changing how they practice medicine at their home institution.
Dr. Moriates, assistant dean for health care value at the University of Texas at Austin, said in an interview that their topic choices reflected the breadth and diversity of patients taken care of by hospitalists.
For example, he noted during the HM19 session that results from several studies suggest hospitalists may soon choose oral antibiotics over IV antibiotics for care of certain patient populations: the recent POET trial suggests use of oral antibiotics for patients with left-sided infective endocarditis resulted in a lower length of stay in hospital (19 inpatient days) when compared with use of IV antibiotics (3 inpatient days and 17 additional treatment days post discharge), while the OVIVA trial found a lower but noninferior treatment failure rate among patients who received oral antibiotics for bone and joint infection, compared with IV antibiotics. Although these were both well-done studies, Dr. Moriates and Dr. Herzke emphasized that the results challenge widely accepted standards of care, and it may not yet be time for a paradigm shift.
Direct oral anticoagulants (DOACs) also are being studied in patients with end-stage renal disease (ESRD) and cancer, Dr. Herzke said, and apixaban (Eliquis) 5 mg appears to be the preferred dose for a lower risk of stroke and mortality in patients with ESRD and atrial fibrillation. The speakers said there are further studies being developed for management of AF in patients with heart failure and DOACs for patients with ESRD.
Another retrospective cohort study from research in the Massachusetts Public Health Dataset found that buprenorphine may have a number needed to treat of 50 for opioid use disorder, which Dr. Moriates said is close in proximity for the number needed to treat for aspirin. “It seems like it’s time for this to become standard of care,” he said.
The speakers also highlighted common practices hospitalists should stop performing based on the latest evidence.
In one example, they revealed that there is conflicting research on angiotensin-converting enzyme (ACE) inhibitors. One study found transient preoperative interruption of ACE inhibitors was associated with a reduction in intraoperative hypotension during a noncardiac, nonvascular surgery. A second study linked ACE inhibitor use with a reduction in all-cause mortality. However, long-term use of ACE inhibitors also appears to be associated with a 14% increase in lung cancers, with an increased incidence based on longer use duration.
Hospitalists should also be aware of recommendations from a study on oxygen therapy, Dr. Herzke noted, which found that extra oxygen therapy may harm patients with MI or stroke; as a result, hospitalists should “wean oxygen as tolerated” in these patients. In addition, hospitalists also may want to consider using oral vancomycin (Vancocin) or fidaxomicin (Dificid) for treatment of Clostridium difficile infections, based on new evidence that found there is a higher cure rate for those treatments, compared with metronidazole.
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Studies that question common practices
Studies that question common practices
On the big stage at HM19 in late March, Carrie Herzke, MD, FAAP, FACP, SFHM, and Christopher Moriates, MD, FACP, SFHM, undertook the daunting task of summarizing a year’s worth of research relevant to the practice of hospital medicine – all within the span of an hour.
As has been standard with the “Update in Hospital Medicine” session at previous SHM Annual Conferences, the presenters touched on lighter topics in the medical literature: a prospective cohort study that found drinking coffee was inversely associated with mortality, even for those who drink up to eight cups a day; a cross-sectional observational study in which patients noted that what a physician wears is an important consideration for them during care, with a white coat preferred over formal attire as the most highly rated preference in a clinical care setting; and a study from a pediatric journal in which researchers calculated the average transit time for a Lego figurine head ingested by an adult.
But Dr. Herzke and Dr. Moriates mainly covered more serious subjects. In an interview before the session, Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, said she and Dr. Moriates chose studies across the fields of infectious diseases, cardiology, and hematology that should make hospitalists question common practices and consider changing how they practice medicine at their home institution.
Dr. Moriates, assistant dean for health care value at the University of Texas at Austin, said in an interview that their topic choices reflected the breadth and diversity of patients taken care of by hospitalists.
For example, he noted during the HM19 session that results from several studies suggest hospitalists may soon choose oral antibiotics over IV antibiotics for care of certain patient populations: the recent POET trial suggests use of oral antibiotics for patients with left-sided infective endocarditis resulted in a lower length of stay in hospital (19 inpatient days) when compared with use of IV antibiotics (3 inpatient days and 17 additional treatment days post discharge), while the OVIVA trial found a lower but noninferior treatment failure rate among patients who received oral antibiotics for bone and joint infection, compared with IV antibiotics. Although these were both well-done studies, Dr. Moriates and Dr. Herzke emphasized that the results challenge widely accepted standards of care, and it may not yet be time for a paradigm shift.
Direct oral anticoagulants (DOACs) also are being studied in patients with end-stage renal disease (ESRD) and cancer, Dr. Herzke said, and apixaban (Eliquis) 5 mg appears to be the preferred dose for a lower risk of stroke and mortality in patients with ESRD and atrial fibrillation. The speakers said there are further studies being developed for management of AF in patients with heart failure and DOACs for patients with ESRD.
Another retrospective cohort study from research in the Massachusetts Public Health Dataset found that buprenorphine may have a number needed to treat of 50 for opioid use disorder, which Dr. Moriates said is close in proximity for the number needed to treat for aspirin. “It seems like it’s time for this to become standard of care,” he said.
The speakers also highlighted common practices hospitalists should stop performing based on the latest evidence.
In one example, they revealed that there is conflicting research on angiotensin-converting enzyme (ACE) inhibitors. One study found transient preoperative interruption of ACE inhibitors was associated with a reduction in intraoperative hypotension during a noncardiac, nonvascular surgery. A second study linked ACE inhibitor use with a reduction in all-cause mortality. However, long-term use of ACE inhibitors also appears to be associated with a 14% increase in lung cancers, with an increased incidence based on longer use duration.
Hospitalists should also be aware of recommendations from a study on oxygen therapy, Dr. Herzke noted, which found that extra oxygen therapy may harm patients with MI or stroke; as a result, hospitalists should “wean oxygen as tolerated” in these patients. In addition, hospitalists also may want to consider using oral vancomycin (Vancocin) or fidaxomicin (Dificid) for treatment of Clostridium difficile infections, based on new evidence that found there is a higher cure rate for those treatments, compared with metronidazole.
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
On the big stage at HM19 in late March, Carrie Herzke, MD, FAAP, FACP, SFHM, and Christopher Moriates, MD, FACP, SFHM, undertook the daunting task of summarizing a year’s worth of research relevant to the practice of hospital medicine – all within the span of an hour.
As has been standard with the “Update in Hospital Medicine” session at previous SHM Annual Conferences, the presenters touched on lighter topics in the medical literature: a prospective cohort study that found drinking coffee was inversely associated with mortality, even for those who drink up to eight cups a day; a cross-sectional observational study in which patients noted that what a physician wears is an important consideration for them during care, with a white coat preferred over formal attire as the most highly rated preference in a clinical care setting; and a study from a pediatric journal in which researchers calculated the average transit time for a Lego figurine head ingested by an adult.
But Dr. Herzke and Dr. Moriates mainly covered more serious subjects. In an interview before the session, Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, said she and Dr. Moriates chose studies across the fields of infectious diseases, cardiology, and hematology that should make hospitalists question common practices and consider changing how they practice medicine at their home institution.
Dr. Moriates, assistant dean for health care value at the University of Texas at Austin, said in an interview that their topic choices reflected the breadth and diversity of patients taken care of by hospitalists.
For example, he noted during the HM19 session that results from several studies suggest hospitalists may soon choose oral antibiotics over IV antibiotics for care of certain patient populations: the recent POET trial suggests use of oral antibiotics for patients with left-sided infective endocarditis resulted in a lower length of stay in hospital (19 inpatient days) when compared with use of IV antibiotics (3 inpatient days and 17 additional treatment days post discharge), while the OVIVA trial found a lower but noninferior treatment failure rate among patients who received oral antibiotics for bone and joint infection, compared with IV antibiotics. Although these were both well-done studies, Dr. Moriates and Dr. Herzke emphasized that the results challenge widely accepted standards of care, and it may not yet be time for a paradigm shift.
Direct oral anticoagulants (DOACs) also are being studied in patients with end-stage renal disease (ESRD) and cancer, Dr. Herzke said, and apixaban (Eliquis) 5 mg appears to be the preferred dose for a lower risk of stroke and mortality in patients with ESRD and atrial fibrillation. The speakers said there are further studies being developed for management of AF in patients with heart failure and DOACs for patients with ESRD.
Another retrospective cohort study from research in the Massachusetts Public Health Dataset found that buprenorphine may have a number needed to treat of 50 for opioid use disorder, which Dr. Moriates said is close in proximity for the number needed to treat for aspirin. “It seems like it’s time for this to become standard of care,” he said.
The speakers also highlighted common practices hospitalists should stop performing based on the latest evidence.
In one example, they revealed that there is conflicting research on angiotensin-converting enzyme (ACE) inhibitors. One study found transient preoperative interruption of ACE inhibitors was associated with a reduction in intraoperative hypotension during a noncardiac, nonvascular surgery. A second study linked ACE inhibitor use with a reduction in all-cause mortality. However, long-term use of ACE inhibitors also appears to be associated with a 14% increase in lung cancers, with an increased incidence based on longer use duration.
Hospitalists should also be aware of recommendations from a study on oxygen therapy, Dr. Herzke noted, which found that extra oxygen therapy may harm patients with MI or stroke; as a result, hospitalists should “wean oxygen as tolerated” in these patients. In addition, hospitalists also may want to consider using oral vancomycin (Vancocin) or fidaxomicin (Dificid) for treatment of Clostridium difficile infections, based on new evidence that found there is a higher cure rate for those treatments, compared with metronidazole.
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
HM19 Day One highlights: Plenary and sepsis updates (VIDEO)

Dr. Kranthi Sitammagari of Atrium Health in Monroe, N.C., and Dr. Marina Farah of Farah MD Consulting in Corvallis, Ore., offer their expert analysis of the plenary session and Updates on Sepsis session at HM19.

Dr. Kranthi Sitammagari of Atrium Health in Monroe, N.C., and Dr. Marina Farah of Farah MD Consulting in Corvallis, Ore., offer their expert analysis of the plenary session and Updates on Sepsis session at HM19.

Dr. Kranthi Sitammagari of Atrium Health in Monroe, N.C., and Dr. Marina Farah of Farah MD Consulting in Corvallis, Ore., offer their expert analysis of the plenary session and Updates on Sepsis session at HM19.
HM19 Day One highlights: Pulmonary, critical care, and perioperative care updates (VIDEO)
Marina Farah, MD, MHA, and Kranthi Sitammagari, MD, editorial board members for The Hospitalist, discuss Day One highlights from HM19.

Marina Farah, MD, MHA, and Kranthi Sitammagari, MD, editorial board members for The Hospitalist, discuss Day One highlights from HM19.

Marina Farah, MD, MHA, and Kranthi Sitammagari, MD, editorial board members for The Hospitalist, discuss Day One highlights from HM19.

It’s not too early to get ready for HM20
Hospitalist Benji K. Mathews, MD, SFHM, CLHM, will bring a unique commitment to medical education to HM20, which will be held next year on April 16-18 in San Diego.
Dr. Mathews enjoys receiving technological gadgets periodically at his home. Just ask his elementary school–age children: They’ve learned how to use handheld ultrasound devices on each other.
“They’re able to find their siblings’ kidneys and hearts,” said Dr. Mathews, an assistant professor of medicine at the University of Minnesota, Minneapolis, and a hospitalist with HealthPartners in Saint Paul, Minn. “I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more!”
Society of Hospital Medicine members and nonmembers who would like to submit proposals for workshops and didactic sessions at HM20 must move quickly. “The open call for content opened in January 2019, providing enough time to prepare and submit,” Dr. Mathews said. “The HM20 call for content will stay open for 2 weeks after HM19 is wrapped up.”
Dr. Mathews expects HM20 will build upon the successes of this year’s conference and support SHM’s commitment to diversity in voices and programming. More than 4,000 attendees are expected.
“HM20 is a team effort with a diverse group serving on the annual meeting planning committee,” he said. “In conjunction with the submissions we receive from the open call, the Annual Conference Committee really builds on the momentum and feedback from attendees from the previous year’s annual meeting. We will identify popular sessions and topics and also review the data we receive from attendees about how they rated sessions and speakers. The chair and committee members will review all of these metrics and use them to plan HM20.”
Dr. Mathews said several topics will get special emphasis in 2020. “We would like to have more content for nurse practitioners and physician assistants and continued representation from the broad range of hospitalists throughout the nation in academic and community settings,” he said.
“We’re also hoping to provide more credit offerings in addition to those we now offer via the American Academy of Family Physicians and the American Osteopathic Association. Next year, we’re hoping to offer pharmacology credit.”
In addition, he said, “we hope to have focused content on diversity issues such as women in hospital medicine and gender and racial bias. We also plan to provide a continued focus on integration of work and life and topics in technology such as bedside ultrasound and telemedicine.”
Technology will be more than a topic at HM20. SHM plans to embrace it in the conference itself to a greater extent than ever before. “We hope to build an online interactive schedule so that attendees may search tracks by day and credit type and schedule their sessions ahead of time,” Dr. Mathews said. “There will still be a PDF schedule, but we hope to push a more interactive, paperless version. We also hope to have e-posters for the first time at HM20.”
The emphasis on technology is a perfect fit for Dr. Mathews, who’s a pioneer in the use of bedside ultrasound. “I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine,” he said. “The group and mentors provided opportunities to develop further niches in my practice. I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound. Now, I continue to teach clinicians, educators, and learners.”
Dr. Mathews has no relevant disclosures.
Hospitalist Benji K. Mathews, MD, SFHM, CLHM, will bring a unique commitment to medical education to HM20, which will be held next year on April 16-18 in San Diego.
Dr. Mathews enjoys receiving technological gadgets periodically at his home. Just ask his elementary school–age children: They’ve learned how to use handheld ultrasound devices on each other.
“They’re able to find their siblings’ kidneys and hearts,” said Dr. Mathews, an assistant professor of medicine at the University of Minnesota, Minneapolis, and a hospitalist with HealthPartners in Saint Paul, Minn. “I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more!”
Society of Hospital Medicine members and nonmembers who would like to submit proposals for workshops and didactic sessions at HM20 must move quickly. “The open call for content opened in January 2019, providing enough time to prepare and submit,” Dr. Mathews said. “The HM20 call for content will stay open for 2 weeks after HM19 is wrapped up.”
Dr. Mathews expects HM20 will build upon the successes of this year’s conference and support SHM’s commitment to diversity in voices and programming. More than 4,000 attendees are expected.
“HM20 is a team effort with a diverse group serving on the annual meeting planning committee,” he said. “In conjunction with the submissions we receive from the open call, the Annual Conference Committee really builds on the momentum and feedback from attendees from the previous year’s annual meeting. We will identify popular sessions and topics and also review the data we receive from attendees about how they rated sessions and speakers. The chair and committee members will review all of these metrics and use them to plan HM20.”
Dr. Mathews said several topics will get special emphasis in 2020. “We would like to have more content for nurse practitioners and physician assistants and continued representation from the broad range of hospitalists throughout the nation in academic and community settings,” he said.
“We’re also hoping to provide more credit offerings in addition to those we now offer via the American Academy of Family Physicians and the American Osteopathic Association. Next year, we’re hoping to offer pharmacology credit.”
In addition, he said, “we hope to have focused content on diversity issues such as women in hospital medicine and gender and racial bias. We also plan to provide a continued focus on integration of work and life and topics in technology such as bedside ultrasound and telemedicine.”
Technology will be more than a topic at HM20. SHM plans to embrace it in the conference itself to a greater extent than ever before. “We hope to build an online interactive schedule so that attendees may search tracks by day and credit type and schedule their sessions ahead of time,” Dr. Mathews said. “There will still be a PDF schedule, but we hope to push a more interactive, paperless version. We also hope to have e-posters for the first time at HM20.”
The emphasis on technology is a perfect fit for Dr. Mathews, who’s a pioneer in the use of bedside ultrasound. “I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine,” he said. “The group and mentors provided opportunities to develop further niches in my practice. I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound. Now, I continue to teach clinicians, educators, and learners.”
Dr. Mathews has no relevant disclosures.
Hospitalist Benji K. Mathews, MD, SFHM, CLHM, will bring a unique commitment to medical education to HM20, which will be held next year on April 16-18 in San Diego.
Dr. Mathews enjoys receiving technological gadgets periodically at his home. Just ask his elementary school–age children: They’ve learned how to use handheld ultrasound devices on each other.
“They’re able to find their siblings’ kidneys and hearts,” said Dr. Mathews, an assistant professor of medicine at the University of Minnesota, Minneapolis, and a hospitalist with HealthPartners in Saint Paul, Minn. “I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more!”
Society of Hospital Medicine members and nonmembers who would like to submit proposals for workshops and didactic sessions at HM20 must move quickly. “The open call for content opened in January 2019, providing enough time to prepare and submit,” Dr. Mathews said. “The HM20 call for content will stay open for 2 weeks after HM19 is wrapped up.”
Dr. Mathews expects HM20 will build upon the successes of this year’s conference and support SHM’s commitment to diversity in voices and programming. More than 4,000 attendees are expected.
“HM20 is a team effort with a diverse group serving on the annual meeting planning committee,” he said. “In conjunction with the submissions we receive from the open call, the Annual Conference Committee really builds on the momentum and feedback from attendees from the previous year’s annual meeting. We will identify popular sessions and topics and also review the data we receive from attendees about how they rated sessions and speakers. The chair and committee members will review all of these metrics and use them to plan HM20.”
Dr. Mathews said several topics will get special emphasis in 2020. “We would like to have more content for nurse practitioners and physician assistants and continued representation from the broad range of hospitalists throughout the nation in academic and community settings,” he said.
“We’re also hoping to provide more credit offerings in addition to those we now offer via the American Academy of Family Physicians and the American Osteopathic Association. Next year, we’re hoping to offer pharmacology credit.”
In addition, he said, “we hope to have focused content on diversity issues such as women in hospital medicine and gender and racial bias. We also plan to provide a continued focus on integration of work and life and topics in technology such as bedside ultrasound and telemedicine.”
Technology will be more than a topic at HM20. SHM plans to embrace it in the conference itself to a greater extent than ever before. “We hope to build an online interactive schedule so that attendees may search tracks by day and credit type and schedule their sessions ahead of time,” Dr. Mathews said. “There will still be a PDF schedule, but we hope to push a more interactive, paperless version. We also hope to have e-posters for the first time at HM20.”
The emphasis on technology is a perfect fit for Dr. Mathews, who’s a pioneer in the use of bedside ultrasound. “I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine,” he said. “The group and mentors provided opportunities to develop further niches in my practice. I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound. Now, I continue to teach clinicians, educators, and learners.”
Dr. Mathews has no relevant disclosures.
Welcome to Day 3 of HM19
We have reached the final day of another SHM annual conference. What a spectacular ride it has been! On the first day, we heard about the success of the first National Hospitalist Day and how hospital medicine continues to evolve with the health care landscape in the United States and beyond. Throughout the course of the meeting, you have learned about critical updates in our specialty that will support hospitalists’ quest to lead the change. As health care transforms, we are well positioned to innovate in support of our peers and patients.
The importance of high-value care has been a theme of HM19, balanced with the high value of physician well-being. With inspiring keynotes from Marc Harrison, MD, on influencing lives more effectively and more affordably to approaches to fighting burnout from Tait Shanafelt, MD, hospital medicine as a specialty has the power to transform health care for patients and providers alike. I hope you also had the chance to attend the sessions on clinical updates, diagnostic reasoning, practice management, and career development, to name just a few.
The final day of the meeting is no exception when it comes to impactful topics and memorable sessions. Beginning at 7:30 a.m., you’ll find a number of sessions and workshops to round out your conference experience. Our popular “Stump the Professor” series is back, focused on challenging clinical unknowns. In addition, “Medical Jeopardy,” tips on being a successful teaching attending, best practices for promoting diversity in HMGs, the history of hospitals, and updates on LGBTQ health are just a few of the topics you’ll have a chance to immerse yourself in today.
Because of the proximity to the nation’s capital, we also are looking forward to Hill Day today, when hospitalists will travel to Capitol Hill to meet with legislators to discuss issues and policy affecting hospital medicine. This is yet another example of how hospitalists and SHM are partnering to be a voice for clinicians in important health care policy conversations.
As the conference concludes, I thank you for joining us and being a part of the hospital medicine movement. We hope you will continue to engage with SHM throughout the year as you further connect with colleagues via special interest groups, chapters, and committees. If you’re new to SHM, we invite you to discover all the options that your membership offers. We look forward to seeing you next year at Hospital Medicine 2020 (HM20) in San Diego, from April 15-18!
Dr. Frost is the incoming president of the Society of Hospital Medicine and the national medical director of hospital-based services at LifePoint Health in Brentwood, Tennessee.
We have reached the final day of another SHM annual conference. What a spectacular ride it has been! On the first day, we heard about the success of the first National Hospitalist Day and how hospital medicine continues to evolve with the health care landscape in the United States and beyond. Throughout the course of the meeting, you have learned about critical updates in our specialty that will support hospitalists’ quest to lead the change. As health care transforms, we are well positioned to innovate in support of our peers and patients.
The importance of high-value care has been a theme of HM19, balanced with the high value of physician well-being. With inspiring keynotes from Marc Harrison, MD, on influencing lives more effectively and more affordably to approaches to fighting burnout from Tait Shanafelt, MD, hospital medicine as a specialty has the power to transform health care for patients and providers alike. I hope you also had the chance to attend the sessions on clinical updates, diagnostic reasoning, practice management, and career development, to name just a few.
The final day of the meeting is no exception when it comes to impactful topics and memorable sessions. Beginning at 7:30 a.m., you’ll find a number of sessions and workshops to round out your conference experience. Our popular “Stump the Professor” series is back, focused on challenging clinical unknowns. In addition, “Medical Jeopardy,” tips on being a successful teaching attending, best practices for promoting diversity in HMGs, the history of hospitals, and updates on LGBTQ health are just a few of the topics you’ll have a chance to immerse yourself in today.
Because of the proximity to the nation’s capital, we also are looking forward to Hill Day today, when hospitalists will travel to Capitol Hill to meet with legislators to discuss issues and policy affecting hospital medicine. This is yet another example of how hospitalists and SHM are partnering to be a voice for clinicians in important health care policy conversations.
As the conference concludes, I thank you for joining us and being a part of the hospital medicine movement. We hope you will continue to engage with SHM throughout the year as you further connect with colleagues via special interest groups, chapters, and committees. If you’re new to SHM, we invite you to discover all the options that your membership offers. We look forward to seeing you next year at Hospital Medicine 2020 (HM20) in San Diego, from April 15-18!
Dr. Frost is the incoming president of the Society of Hospital Medicine and the national medical director of hospital-based services at LifePoint Health in Brentwood, Tennessee.
We have reached the final day of another SHM annual conference. What a spectacular ride it has been! On the first day, we heard about the success of the first National Hospitalist Day and how hospital medicine continues to evolve with the health care landscape in the United States and beyond. Throughout the course of the meeting, you have learned about critical updates in our specialty that will support hospitalists’ quest to lead the change. As health care transforms, we are well positioned to innovate in support of our peers and patients.
The importance of high-value care has been a theme of HM19, balanced with the high value of physician well-being. With inspiring keynotes from Marc Harrison, MD, on influencing lives more effectively and more affordably to approaches to fighting burnout from Tait Shanafelt, MD, hospital medicine as a specialty has the power to transform health care for patients and providers alike. I hope you also had the chance to attend the sessions on clinical updates, diagnostic reasoning, practice management, and career development, to name just a few.
The final day of the meeting is no exception when it comes to impactful topics and memorable sessions. Beginning at 7:30 a.m., you’ll find a number of sessions and workshops to round out your conference experience. Our popular “Stump the Professor” series is back, focused on challenging clinical unknowns. In addition, “Medical Jeopardy,” tips on being a successful teaching attending, best practices for promoting diversity in HMGs, the history of hospitals, and updates on LGBTQ health are just a few of the topics you’ll have a chance to immerse yourself in today.
Because of the proximity to the nation’s capital, we also are looking forward to Hill Day today, when hospitalists will travel to Capitol Hill to meet with legislators to discuss issues and policy affecting hospital medicine. This is yet another example of how hospitalists and SHM are partnering to be a voice for clinicians in important health care policy conversations.
As the conference concludes, I thank you for joining us and being a part of the hospital medicine movement. We hope you will continue to engage with SHM throughout the year as you further connect with colleagues via special interest groups, chapters, and committees. If you’re new to SHM, we invite you to discover all the options that your membership offers. We look forward to seeing you next year at Hospital Medicine 2020 (HM20) in San Diego, from April 15-18!
Dr. Frost is the incoming president of the Society of Hospital Medicine and the national medical director of hospital-based services at LifePoint Health in Brentwood, Tennessee.