User login
Migraine relief in 20 minutes using eyedrops?
ILLUSTRATIVE CASE
A 35-year-old woman with no significant past medical history presents for follow-up of migraine. At the previous visit, she was prescribed sumatriptan for abortive therapy. However, she has been having significant adverse effect intolerance from the oral formulation, and the nasal formulation is cost prohibitive. What can you recommend as an alternative abortive therapy for this patient’s migraine?
Migraine is among the most common causes of disability worldwide, affecting more than 10% of the global population.2 The prevalence of migraine is between 2.6% and 21.7% across multiple countries.3 On a scale of 0% to 100%, disability caused by migraine is 43.3%, comparable to the first 2 days after an acute myocardial infarction (42.2%) and severe dementia (43.8%).4
Abortive therapy for acute migraine includes nonsteroidal anti-inflammatory drugs (NSAIDs),
Nausea and vomiting, common components of migraine (that are included in International Classification of Headache Disorders, 3rd edition [ICHD-3] criteria for migraine5) present obstacles to effective oral administration if experienced by the patient. In addition, for migraine refractory to first-line treatments, abortive options—including the recently approved
Two oral beta-blockers, propranolol and timolol, are approved by the US Food and Drug Administration for migraine prophylaxis. Unfortunately, oral beta-blockers are ineffective for abortive treatment.7 Ophthalmic timolol is typically used in the treatment of glaucoma, but there have been case reports describing its benefits in acute migraine treatment.8,9 In addition, ophthalmic timolol is far cheaper than medications such as ubrogepant.10 A 2014 case series of 7 patients discussed ophthalmic beta-blockers as an effective and possibly cheaper option for acute migraine treatment.8 A randomized, crossover, placebo-controlled pilot study of 198 migraine attacks in 10 participants using timolol eyedrops for abortive therapy found timolol was not significantly more effective than placebo.9 However, it was an underpowered pilot study, with a lack of masking and an imperfect placebo. The trial discussed here was a controlled, prospective study investigating topical beta-blockers for acute migraine treatment.
STUDY SUMMARY
Crossover study achieved primary endpoint in pain reduction
This randomized, single-center, double-masked, crossover trial compared timolol maleate ophthalmic solution 0.5% with placebo among 43 patients ages 12 or older presenting with a diagnosis of migraine based on ICHD-3 (beta) criteria. Patients were eligible if they had not taken any antimigraine medications for at least 1 month prior to the study and were excluded if they had taken systemic beta-blockers at baseline, or had asthma, bradyarrhythmias, or cardiac dysfunction.
Patients were randomized 1:1 to treatment with timolol maleate 0.5% eyedrops or placebo. At the earliest onset of migraine, patients used 1 drop of timolol maleate 0.5% or placebo in each eye; if they experienced no relief after 10 minutes, they used a second drop or matching placebo. Patients were instructed to score their headache pain on a 10-point scale prior to using the eyedrops and then again 20 minutes after treatment. If a patient had migraine with aura, they were asked to use the eyedrops at the onset of the aura but measure their score at headache onset. If no headaches developed within 20 minutes of the aura, the episode was not included for analysis. All patients were permitted to use their standard oral rescue medication if no relief occurred after 20 minutes of pain onset.
Continue to: The groups were observed...
The groups were observed for 3 months and then followed for a 1-month washout period, during which they received no study medications. The groups were then crossed over to the other treatment and were observed for another 3 months. The primary outcome was a reduction in pain score by 4 or more points, or to 0 on a 10-point pain scale, 20 minutes after treatment. The secondary outcome was nonuse of oral rescue medication.
Forty-three patients were included in a modified intention-to-treat analysis. The primary outcome was achieved in 233 of 284 (82%) timolol-treated migraines, compared to 38 of 271 (14%) placebo-treated migraines (percentage difference = 68 percentage points; 95% CI, 62-74 percentage points; P < .001). The mean pain score at the onset of migraine attacks was 6.01 for those treated with timolol and 5.93 for those treated with placebo. Patients treated with timolol had a reduction in pain of 5.98 points, compared with 0.93 points after using placebo (difference = 5.05; 95% CI, 4.19-5.91). No attacks included in the data required oral rescue medications, and there were no systemic adverse effects from the timolol eyedrops.
WHAT’S NEW
Evidence of benefit as abortive therapy for acute migraine
This randomized controlled trial (RCT) showed evidence to support timolol maleate ophthalmic solution 0.5% vs placebo for treatment of acute migraine by significantly reducing pain when taken at the onset of an acute migraine attack.
CAVEATS
Single-center trial, measuring limited response time
The generalizability of this RCT is limited because it was a single-center trial with a study population from a single region in India. It is unknown whether pain relief, adverse effects, or adherence would differ for the global population. Additionally, only migraines with headache were included in the analysis, limiting non-headache migraine subgroup-directed treatment. Also, this trial evaluated only the response to treatment at 20 minutes, and it is unknown if pain response continued for several hours. Headaches that began more than 20 minutes after the onset of aura were not evaluated.
CHALLENGES TO IMPLEMENTATION
Timolol’s systemic adverse effects require caution
Systemic beta-blocker effects (eg, bradycardia, hypotension, drowsiness, and bronchospasm) from topical timolol have been reported. Caution should be used when prescribing timolol for patients with current cardiovascular and pulmonary conditions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
- Kurian A, Reghunadhan I, Thilak P, et al. Short-term efficacy and safety of topical β-blockers (timolol maleate ophthalmic solution, 0.5%) in acute migraine: a randomized crossover trial. JAMA Ophthalmol. 2020;138:1160-1166. doi: 10.1001/jamaophthalmol.2020.3676
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743-800. doi: 10.1016/S0140-6736(15)60692-4
- Yeh WZ, Blizzard L, Taylor BV. What is the actual prevalence of migraine? Brain Behav. 2018;8:e00950. doi: 10.1002/brb3.950
- Leonardi M, Raggi A. Burden of migraine: international perspectives. Neurol Sci. 2013;34(suppl 1):S117-S118. doi: 10.1007/s10072-013-1387-8
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629-808. doi: 10.1177/0333102413485658
- Ubrogepant. GoodRx. Accessed May 23, 2022. www.goodrx.com/ubrogepant
- Orr SL, Friedman BW, Christie S, et al. Management of adults with acute migraine in the emergency department: the American Headache Society evidence assessment of parenteral pharmacotherapies. Headache. 2016;56:911-940. doi: 10.1111/head.12835
- 8. Migliazzo CV, Hagan JC III. Beta blocker eye drops for treatment of acute migraine. Mo Med. 2014;111:283-288.
- 9. Cossack M, Nabrinsky E, Turner H, et al. Timolol eyedrops in the treatment of acute migraine attacks: a randomized crossover study. JAMA Neurol. 2018;75:1024-1025. doi: 10.1001/jamaneurol.2018.0970
- 10. Timolol. GoodRx. Accessed May 23, 2022. www.goodrx.com/timolol
ILLUSTRATIVE CASE
A 35-year-old woman with no significant past medical history presents for follow-up of migraine. At the previous visit, she was prescribed sumatriptan for abortive therapy. However, she has been having significant adverse effect intolerance from the oral formulation, and the nasal formulation is cost prohibitive. What can you recommend as an alternative abortive therapy for this patient’s migraine?
Migraine is among the most common causes of disability worldwide, affecting more than 10% of the global population.2 The prevalence of migraine is between 2.6% and 21.7% across multiple countries.3 On a scale of 0% to 100%, disability caused by migraine is 43.3%, comparable to the first 2 days after an acute myocardial infarction (42.2%) and severe dementia (43.8%).4
Abortive therapy for acute migraine includes nonsteroidal anti-inflammatory drugs (NSAIDs),
Nausea and vomiting, common components of migraine (that are included in International Classification of Headache Disorders, 3rd edition [ICHD-3] criteria for migraine5) present obstacles to effective oral administration if experienced by the patient. In addition, for migraine refractory to first-line treatments, abortive options—including the recently approved
Two oral beta-blockers, propranolol and timolol, are approved by the US Food and Drug Administration for migraine prophylaxis. Unfortunately, oral beta-blockers are ineffective for abortive treatment.7 Ophthalmic timolol is typically used in the treatment of glaucoma, but there have been case reports describing its benefits in acute migraine treatment.8,9 In addition, ophthalmic timolol is far cheaper than medications such as ubrogepant.10 A 2014 case series of 7 patients discussed ophthalmic beta-blockers as an effective and possibly cheaper option for acute migraine treatment.8 A randomized, crossover, placebo-controlled pilot study of 198 migraine attacks in 10 participants using timolol eyedrops for abortive therapy found timolol was not significantly more effective than placebo.9 However, it was an underpowered pilot study, with a lack of masking and an imperfect placebo. The trial discussed here was a controlled, prospective study investigating topical beta-blockers for acute migraine treatment.
STUDY SUMMARY
Crossover study achieved primary endpoint in pain reduction
This randomized, single-center, double-masked, crossover trial compared timolol maleate ophthalmic solution 0.5% with placebo among 43 patients ages 12 or older presenting with a diagnosis of migraine based on ICHD-3 (beta) criteria. Patients were eligible if they had not taken any antimigraine medications for at least 1 month prior to the study and were excluded if they had taken systemic beta-blockers at baseline, or had asthma, bradyarrhythmias, or cardiac dysfunction.
Patients were randomized 1:1 to treatment with timolol maleate 0.5% eyedrops or placebo. At the earliest onset of migraine, patients used 1 drop of timolol maleate 0.5% or placebo in each eye; if they experienced no relief after 10 minutes, they used a second drop or matching placebo. Patients were instructed to score their headache pain on a 10-point scale prior to using the eyedrops and then again 20 minutes after treatment. If a patient had migraine with aura, they were asked to use the eyedrops at the onset of the aura but measure their score at headache onset. If no headaches developed within 20 minutes of the aura, the episode was not included for analysis. All patients were permitted to use their standard oral rescue medication if no relief occurred after 20 minutes of pain onset.
Continue to: The groups were observed...
The groups were observed for 3 months and then followed for a 1-month washout period, during which they received no study medications. The groups were then crossed over to the other treatment and were observed for another 3 months. The primary outcome was a reduction in pain score by 4 or more points, or to 0 on a 10-point pain scale, 20 minutes after treatment. The secondary outcome was nonuse of oral rescue medication.
Forty-three patients were included in a modified intention-to-treat analysis. The primary outcome was achieved in 233 of 284 (82%) timolol-treated migraines, compared to 38 of 271 (14%) placebo-treated migraines (percentage difference = 68 percentage points; 95% CI, 62-74 percentage points; P < .001). The mean pain score at the onset of migraine attacks was 6.01 for those treated with timolol and 5.93 for those treated with placebo. Patients treated with timolol had a reduction in pain of 5.98 points, compared with 0.93 points after using placebo (difference = 5.05; 95% CI, 4.19-5.91). No attacks included in the data required oral rescue medications, and there were no systemic adverse effects from the timolol eyedrops.
WHAT’S NEW
Evidence of benefit as abortive therapy for acute migraine
This randomized controlled trial (RCT) showed evidence to support timolol maleate ophthalmic solution 0.5% vs placebo for treatment of acute migraine by significantly reducing pain when taken at the onset of an acute migraine attack.
CAVEATS
Single-center trial, measuring limited response time
The generalizability of this RCT is limited because it was a single-center trial with a study population from a single region in India. It is unknown whether pain relief, adverse effects, or adherence would differ for the global population. Additionally, only migraines with headache were included in the analysis, limiting non-headache migraine subgroup-directed treatment. Also, this trial evaluated only the response to treatment at 20 minutes, and it is unknown if pain response continued for several hours. Headaches that began more than 20 minutes after the onset of aura were not evaluated.
CHALLENGES TO IMPLEMENTATION
Timolol’s systemic adverse effects require caution
Systemic beta-blocker effects (eg, bradycardia, hypotension, drowsiness, and bronchospasm) from topical timolol have been reported. Caution should be used when prescribing timolol for patients with current cardiovascular and pulmonary conditions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 35-year-old woman with no significant past medical history presents for follow-up of migraine. At the previous visit, she was prescribed sumatriptan for abortive therapy. However, she has been having significant adverse effect intolerance from the oral formulation, and the nasal formulation is cost prohibitive. What can you recommend as an alternative abortive therapy for this patient’s migraine?
Migraine is among the most common causes of disability worldwide, affecting more than 10% of the global population.2 The prevalence of migraine is between 2.6% and 21.7% across multiple countries.3 On a scale of 0% to 100%, disability caused by migraine is 43.3%, comparable to the first 2 days after an acute myocardial infarction (42.2%) and severe dementia (43.8%).4
Abortive therapy for acute migraine includes nonsteroidal anti-inflammatory drugs (NSAIDs),
Nausea and vomiting, common components of migraine (that are included in International Classification of Headache Disorders, 3rd edition [ICHD-3] criteria for migraine5) present obstacles to effective oral administration if experienced by the patient. In addition, for migraine refractory to first-line treatments, abortive options—including the recently approved
Two oral beta-blockers, propranolol and timolol, are approved by the US Food and Drug Administration for migraine prophylaxis. Unfortunately, oral beta-blockers are ineffective for abortive treatment.7 Ophthalmic timolol is typically used in the treatment of glaucoma, but there have been case reports describing its benefits in acute migraine treatment.8,9 In addition, ophthalmic timolol is far cheaper than medications such as ubrogepant.10 A 2014 case series of 7 patients discussed ophthalmic beta-blockers as an effective and possibly cheaper option for acute migraine treatment.8 A randomized, crossover, placebo-controlled pilot study of 198 migraine attacks in 10 participants using timolol eyedrops for abortive therapy found timolol was not significantly more effective than placebo.9 However, it was an underpowered pilot study, with a lack of masking and an imperfect placebo. The trial discussed here was a controlled, prospective study investigating topical beta-blockers for acute migraine treatment.
STUDY SUMMARY
Crossover study achieved primary endpoint in pain reduction
This randomized, single-center, double-masked, crossover trial compared timolol maleate ophthalmic solution 0.5% with placebo among 43 patients ages 12 or older presenting with a diagnosis of migraine based on ICHD-3 (beta) criteria. Patients were eligible if they had not taken any antimigraine medications for at least 1 month prior to the study and were excluded if they had taken systemic beta-blockers at baseline, or had asthma, bradyarrhythmias, or cardiac dysfunction.
Patients were randomized 1:1 to treatment with timolol maleate 0.5% eyedrops or placebo. At the earliest onset of migraine, patients used 1 drop of timolol maleate 0.5% or placebo in each eye; if they experienced no relief after 10 minutes, they used a second drop or matching placebo. Patients were instructed to score their headache pain on a 10-point scale prior to using the eyedrops and then again 20 minutes after treatment. If a patient had migraine with aura, they were asked to use the eyedrops at the onset of the aura but measure their score at headache onset. If no headaches developed within 20 minutes of the aura, the episode was not included for analysis. All patients were permitted to use their standard oral rescue medication if no relief occurred after 20 minutes of pain onset.
Continue to: The groups were observed...
The groups were observed for 3 months and then followed for a 1-month washout period, during which they received no study medications. The groups were then crossed over to the other treatment and were observed for another 3 months. The primary outcome was a reduction in pain score by 4 or more points, or to 0 on a 10-point pain scale, 20 minutes after treatment. The secondary outcome was nonuse of oral rescue medication.
Forty-three patients were included in a modified intention-to-treat analysis. The primary outcome was achieved in 233 of 284 (82%) timolol-treated migraines, compared to 38 of 271 (14%) placebo-treated migraines (percentage difference = 68 percentage points; 95% CI, 62-74 percentage points; P < .001). The mean pain score at the onset of migraine attacks was 6.01 for those treated with timolol and 5.93 for those treated with placebo. Patients treated with timolol had a reduction in pain of 5.98 points, compared with 0.93 points after using placebo (difference = 5.05; 95% CI, 4.19-5.91). No attacks included in the data required oral rescue medications, and there were no systemic adverse effects from the timolol eyedrops.
WHAT’S NEW
Evidence of benefit as abortive therapy for acute migraine
This randomized controlled trial (RCT) showed evidence to support timolol maleate ophthalmic solution 0.5% vs placebo for treatment of acute migraine by significantly reducing pain when taken at the onset of an acute migraine attack.
CAVEATS
Single-center trial, measuring limited response time
The generalizability of this RCT is limited because it was a single-center trial with a study population from a single region in India. It is unknown whether pain relief, adverse effects, or adherence would differ for the global population. Additionally, only migraines with headache were included in the analysis, limiting non-headache migraine subgroup-directed treatment. Also, this trial evaluated only the response to treatment at 20 minutes, and it is unknown if pain response continued for several hours. Headaches that began more than 20 minutes after the onset of aura were not evaluated.
CHALLENGES TO IMPLEMENTATION
Timolol’s systemic adverse effects require caution
Systemic beta-blocker effects (eg, bradycardia, hypotension, drowsiness, and bronchospasm) from topical timolol have been reported. Caution should be used when prescribing timolol for patients with current cardiovascular and pulmonary conditions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
- Kurian A, Reghunadhan I, Thilak P, et al. Short-term efficacy and safety of topical β-blockers (timolol maleate ophthalmic solution, 0.5%) in acute migraine: a randomized crossover trial. JAMA Ophthalmol. 2020;138:1160-1166. doi: 10.1001/jamaophthalmol.2020.3676
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743-800. doi: 10.1016/S0140-6736(15)60692-4
- Yeh WZ, Blizzard L, Taylor BV. What is the actual prevalence of migraine? Brain Behav. 2018;8:e00950. doi: 10.1002/brb3.950
- Leonardi M, Raggi A. Burden of migraine: international perspectives. Neurol Sci. 2013;34(suppl 1):S117-S118. doi: 10.1007/s10072-013-1387-8
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629-808. doi: 10.1177/0333102413485658
- Ubrogepant. GoodRx. Accessed May 23, 2022. www.goodrx.com/ubrogepant
- Orr SL, Friedman BW, Christie S, et al. Management of adults with acute migraine in the emergency department: the American Headache Society evidence assessment of parenteral pharmacotherapies. Headache. 2016;56:911-940. doi: 10.1111/head.12835
- 8. Migliazzo CV, Hagan JC III. Beta blocker eye drops for treatment of acute migraine. Mo Med. 2014;111:283-288.
- 9. Cossack M, Nabrinsky E, Turner H, et al. Timolol eyedrops in the treatment of acute migraine attacks: a randomized crossover study. JAMA Neurol. 2018;75:1024-1025. doi: 10.1001/jamaneurol.2018.0970
- 10. Timolol. GoodRx. Accessed May 23, 2022. www.goodrx.com/timolol
- Kurian A, Reghunadhan I, Thilak P, et al. Short-term efficacy and safety of topical β-blockers (timolol maleate ophthalmic solution, 0.5%) in acute migraine: a randomized crossover trial. JAMA Ophthalmol. 2020;138:1160-1166. doi: 10.1001/jamaophthalmol.2020.3676
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743-800. doi: 10.1016/S0140-6736(15)60692-4
- Yeh WZ, Blizzard L, Taylor BV. What is the actual prevalence of migraine? Brain Behav. 2018;8:e00950. doi: 10.1002/brb3.950
- Leonardi M, Raggi A. Burden of migraine: international perspectives. Neurol Sci. 2013;34(suppl 1):S117-S118. doi: 10.1007/s10072-013-1387-8
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629-808. doi: 10.1177/0333102413485658
- Ubrogepant. GoodRx. Accessed May 23, 2022. www.goodrx.com/ubrogepant
- Orr SL, Friedman BW, Christie S, et al. Management of adults with acute migraine in the emergency department: the American Headache Society evidence assessment of parenteral pharmacotherapies. Headache. 2016;56:911-940. doi: 10.1111/head.12835
- 8. Migliazzo CV, Hagan JC III. Beta blocker eye drops for treatment of acute migraine. Mo Med. 2014;111:283-288.
- 9. Cossack M, Nabrinsky E, Turner H, et al. Timolol eyedrops in the treatment of acute migraine attacks: a randomized crossover study. JAMA Neurol. 2018;75:1024-1025. doi: 10.1001/jamaneurol.2018.0970
- 10. Timolol. GoodRx. Accessed May 23, 2022. www.goodrx.com/timolol
PRACTICE CHANGER
Consider timolol maleate 0.5% eyedrops as a quick and effective abortive therapy for migraine.1
STRENGTH OF RECOMMENDATION
B: Based on a single randomized controlled trial.1
Kurian A, Reghunadhan I, Thilak P, et al. Short-term efficacy and safety of topical β-blockers (timolol maleate ophthalmic solution, 0.5%) in acute migraine: a randomized crossover trial. JAMA Ophthalmol. 2020;138:1160-1166.
Time to consider topical capsaicin for acute trauma pain?
ILLUSTRATIVE CASE
A 23-year-old man with no significant past medical history presents to an urgent care center after a fall on his right arm while playing football. He reports a pain level of 6 using the visual analog scale (VAS). Physical exam reveals minor erythema and edema of his forearm with pain to palpation. Range of motion, strength, and sensation are intact. No lacerations are present. His vital signs are normal. No fracture is found on imaging. The physician decides that treatment with a topical analgesic is reasonable for this uncomplicated contusion of the right forearm. Is there a role for topical capsaicin in the treatment of this patient’s pain?
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) are effective for the treatment of acute non–low back pain musculoskeletal injuries.2 They are generally well tolerated and just as effective as oral NSAIDS or acetaminophen for localized injuries. Their ubiquitous availability, affordability, and low adverse effect profile make them an attractive first-line treatment option for acute musculoskeletal pain.
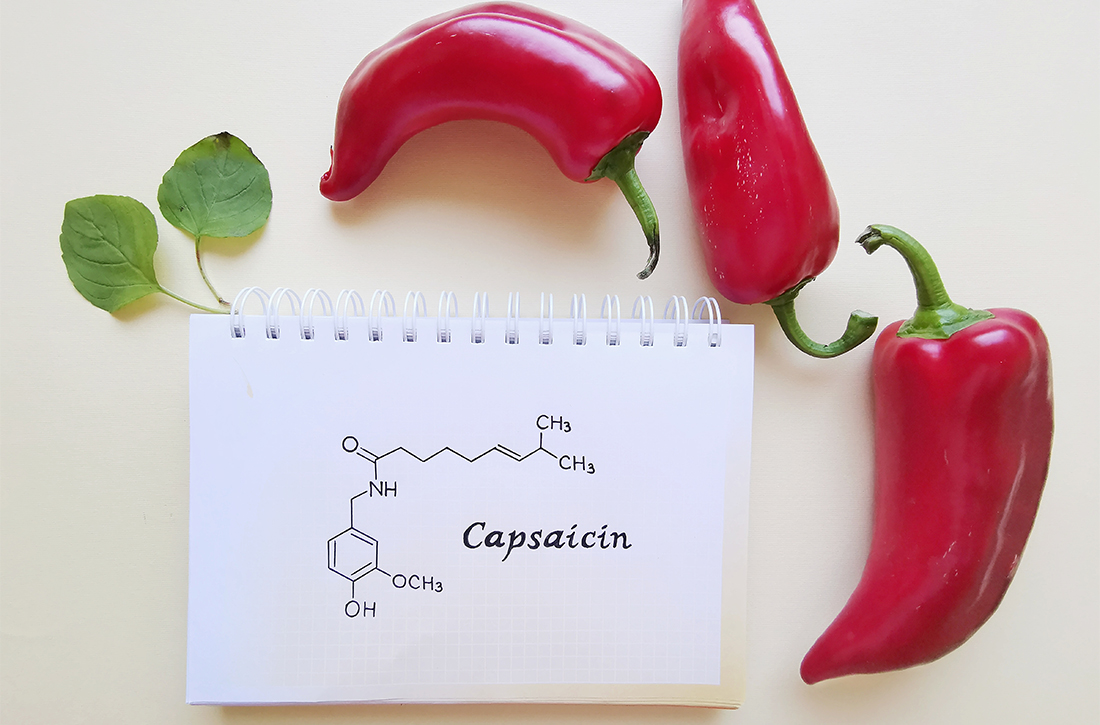
Capsaicin, a topical agent derived from a genus of red peppers, has been used for the treatment of neuropathic and chronic pain via its interactions with substance P, transient receptor potential vanilloid subtype 1 (TRPV1), and nociceptive nerve fibers.3,4 It has demonstrated effectiveness in the management of diabetic neuropathy, knee osteoarthritis, and postherpetic neuralgia, as well as various causes of pruritus.5,6
Although many studies have compared oral and topical NSAIDs, opiates, and acetaminophen, few studies have directly compared topical NSAIDs and capsaicin. This study compared the topical NSAID piroxicam with topical capsaicin.
STUDY SUMMARY
Topical capsaicin demonstrated superior pain reduction
This prospective, double-blind RCT compared the efficacy of topical capsaicin vs topical piroxicam for the treatment of acute pain following upper extremity blunt trauma. Patients (ages ≥ 18 years) who presented to a Turkish emergency department within 2 hours of upper extremity injury were randomized to receive either 0.05% capsaicin gel (n = 69) or 0.5% piroxicam gel (n = 67). Patients reported level 5 or higher pain on the VAS. Those with fractures, dislocations, skin disruption, or other trauma were excluded. Age, gender, pain duration, and mechanism of injury did not differ significantly between study groups.1
Blinding was ensured by placing the gels in opaque containers containing 30 mg of either capsaicin or piroxicam and dyeing the medicine with red and yellow food coloring. A thin layer of medication was applied to an area no larger than 5 × 5 cm on the upper extremity and rubbed for 1 minute. Patients were observed in the emergency department for 2 hours and discharged with instructions to apply the medication 3 times daily for 72 hours.
The investigators measured pain using VAS scores at 1 hour, 2 hours, 24 hours, and 72 hours after treatment. Topical capsaicin was superior to topical piroxicam at achieving both primary outcomes: a VAS score of ≤ 4 (85.5% vs 50.7%; number needed to treat [NNT] = 2.9; P < .001) and a > 50% reduction in VAS score (87% vs 62.7%; NNT = 4.1; P < .01) at the end of treatment.1 (These outcomes were based on earlier determinations of the minimal clinically important difference.7,8)
Additionally, capsaicin was more effective than piroxicam at each time interval. This difference was most pronounced at 72 hours, with a mean difference of delta VAS scores of 1.53 (95% CI, 0.85-2.221) and a mean percentage of the reduction in VAS scores of 19.7% (95% CI, 12.4%-27.2%) (P < .001).1
Reported adverse effects, such as burning, itching, and rash, were mild and infrequent and showed no significant difference between the treatment groups.
WHAT’S NEW
First study comparing topical capsaicin and a topical NSAID in acute trauma
Although both capsaicin and topical piroxicam have proven efficacy for the treatment of pain, this RCT is the first study to directly compare these agents in the setting of acute upper extremity blunt trauma. Capsaicin is currently more commonly prescribed as a treatment for chronic neuropathic pain.4,9 In this study, capsaicin demonstrated superior results in pain reduction at each assessed time interval and at the primary end point of 72 hours.
CAVEATS
Limited generalizability to lower extremity and truncal trauma
This RCT included a relatively small sample size (136 patients). Researchers evaluated only blunt upper extremity injuries; as such, the generalizability of the effectiveness of topical capsaicin in blunt lower extremity and truncal trauma is limited, especially over larger surface areas.
CHALLENGES TO IMPLEMENTATION
No major challenges found
There are no major challenges to implementing this inexpensive treatment.
1. Kocak AO, Dogruyol S, Akbas I, et al. Comparison of topical capsaicin and topical piroxicam in the treatment of acute trauma-induced pain: a randomized double-blind trial. Am J Emerg Med. 2020;38:1767-1771. doi: 10.1016/j.ajem.2020.05.104
2. Busse JW, Sadeghirad B, Oparin Y, et al. Management of acute pain from non–low back, musculoskeletal injuries: a systematic review and network meta-analysis of randomized trials. Ann Intern Med. 2020;173:730-738. doi: 10.7326/M19-3601
3. Chrubasik S, Weiser T, Beime B. Effectiveness and safety of topical capsaicin cream in the treatment of chronic soft tissue pain. Phytother Res. 2010;24:1877-1885. doi: 10.1002/ptr.3335
4. Derry S, Moore RA. Topical capsaicin (low concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2012(9):CD010111. doi: 10.1002/14651858.CD010111
5. Simpson DM, Robinson-Papp J, Van J, et al. Capsaicin 8% patch in painful diabetic peripheral neuropathy: a randomized, double-blind, placebo-controlled study. J Pain. 2017;18:42-53. doi: 10.1016/j.jpain.2016.09.008
6. Papoiu ADP, Yosipovitch G. Topical capsaicin. The fire of a ‘hot’ medicine is reignited. Expert Opin Pharmacother. 2010;11:1359-1371. doi: 10.1517/14656566.2010.481670
7. Kulkantrakorn K, Lorsuwansiri C, Meesawatsom P. 0.025% capsaicin gel for the treatment of painful diabetic neuropathy: a randomized, double-blind, crossover, placebo-controlled trial. Pain Pract. 2013;13:497-503. doi: 10.1111/papr.12013
8. Kocak AO, Ahiskalioglu A, Sengun E, et al. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: a prospective randomized study. Am J Emerg Med. 2019;37:1927-1931. doi: 10.1016/j.ajem.2019.01.015
9. Derry S, Rice ASC, Cole P, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;1(1):CD007393. doi: 10.1002/14651858.CD007393.pub4
ILLUSTRATIVE CASE
A 23-year-old man with no significant past medical history presents to an urgent care center after a fall on his right arm while playing football. He reports a pain level of 6 using the visual analog scale (VAS). Physical exam reveals minor erythema and edema of his forearm with pain to palpation. Range of motion, strength, and sensation are intact. No lacerations are present. His vital signs are normal. No fracture is found on imaging. The physician decides that treatment with a topical analgesic is reasonable for this uncomplicated contusion of the right forearm. Is there a role for topical capsaicin in the treatment of this patient’s pain?
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) are effective for the treatment of acute non–low back pain musculoskeletal injuries.2 They are generally well tolerated and just as effective as oral NSAIDS or acetaminophen for localized injuries. Their ubiquitous availability, affordability, and low adverse effect profile make them an attractive first-line treatment option for acute musculoskeletal pain.
Capsaicin, a topical agent derived from a genus of red peppers, has been used for the treatment of neuropathic and chronic pain via its interactions with substance P, transient receptor potential vanilloid subtype 1 (TRPV1), and nociceptive nerve fibers.3,4 It has demonstrated effectiveness in the management of diabetic neuropathy, knee osteoarthritis, and postherpetic neuralgia, as well as various causes of pruritus.5,6
Although many studies have compared oral and topical NSAIDs, opiates, and acetaminophen, few studies have directly compared topical NSAIDs and capsaicin. This study compared the topical NSAID piroxicam with topical capsaicin.
STUDY SUMMARY
Topical capsaicin demonstrated superior pain reduction
This prospective, double-blind RCT compared the efficacy of topical capsaicin vs topical piroxicam for the treatment of acute pain following upper extremity blunt trauma. Patients (ages ≥ 18 years) who presented to a Turkish emergency department within 2 hours of upper extremity injury were randomized to receive either 0.05% capsaicin gel (n = 69) or 0.5% piroxicam gel (n = 67). Patients reported level 5 or higher pain on the VAS. Those with fractures, dislocations, skin disruption, or other trauma were excluded. Age, gender, pain duration, and mechanism of injury did not differ significantly between study groups.1
Blinding was ensured by placing the gels in opaque containers containing 30 mg of either capsaicin or piroxicam and dyeing the medicine with red and yellow food coloring. A thin layer of medication was applied to an area no larger than 5 × 5 cm on the upper extremity and rubbed for 1 minute. Patients were observed in the emergency department for 2 hours and discharged with instructions to apply the medication 3 times daily for 72 hours.
The investigators measured pain using VAS scores at 1 hour, 2 hours, 24 hours, and 72 hours after treatment. Topical capsaicin was superior to topical piroxicam at achieving both primary outcomes: a VAS score of ≤ 4 (85.5% vs 50.7%; number needed to treat [NNT] = 2.9; P < .001) and a > 50% reduction in VAS score (87% vs 62.7%; NNT = 4.1; P < .01) at the end of treatment.1 (These outcomes were based on earlier determinations of the minimal clinically important difference.7,8)
Additionally, capsaicin was more effective than piroxicam at each time interval. This difference was most pronounced at 72 hours, with a mean difference of delta VAS scores of 1.53 (95% CI, 0.85-2.221) and a mean percentage of the reduction in VAS scores of 19.7% (95% CI, 12.4%-27.2%) (P < .001).1
Reported adverse effects, such as burning, itching, and rash, were mild and infrequent and showed no significant difference between the treatment groups.
WHAT’S NEW
First study comparing topical capsaicin and a topical NSAID in acute trauma
Although both capsaicin and topical piroxicam have proven efficacy for the treatment of pain, this RCT is the first study to directly compare these agents in the setting of acute upper extremity blunt trauma. Capsaicin is currently more commonly prescribed as a treatment for chronic neuropathic pain.4,9 In this study, capsaicin demonstrated superior results in pain reduction at each assessed time interval and at the primary end point of 72 hours.
CAVEATS
Limited generalizability to lower extremity and truncal trauma
This RCT included a relatively small sample size (136 patients). Researchers evaluated only blunt upper extremity injuries; as such, the generalizability of the effectiveness of topical capsaicin in blunt lower extremity and truncal trauma is limited, especially over larger surface areas.
CHALLENGES TO IMPLEMENTATION
No major challenges found
There are no major challenges to implementing this inexpensive treatment.
ILLUSTRATIVE CASE
A 23-year-old man with no significant past medical history presents to an urgent care center after a fall on his right arm while playing football. He reports a pain level of 6 using the visual analog scale (VAS). Physical exam reveals minor erythema and edema of his forearm with pain to palpation. Range of motion, strength, and sensation are intact. No lacerations are present. His vital signs are normal. No fracture is found on imaging. The physician decides that treatment with a topical analgesic is reasonable for this uncomplicated contusion of the right forearm. Is there a role for topical capsaicin in the treatment of this patient’s pain?
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) are effective for the treatment of acute non–low back pain musculoskeletal injuries.2 They are generally well tolerated and just as effective as oral NSAIDS or acetaminophen for localized injuries. Their ubiquitous availability, affordability, and low adverse effect profile make them an attractive first-line treatment option for acute musculoskeletal pain.
Capsaicin, a topical agent derived from a genus of red peppers, has been used for the treatment of neuropathic and chronic pain via its interactions with substance P, transient receptor potential vanilloid subtype 1 (TRPV1), and nociceptive nerve fibers.3,4 It has demonstrated effectiveness in the management of diabetic neuropathy, knee osteoarthritis, and postherpetic neuralgia, as well as various causes of pruritus.5,6
Although many studies have compared oral and topical NSAIDs, opiates, and acetaminophen, few studies have directly compared topical NSAIDs and capsaicin. This study compared the topical NSAID piroxicam with topical capsaicin.
STUDY SUMMARY
Topical capsaicin demonstrated superior pain reduction
This prospective, double-blind RCT compared the efficacy of topical capsaicin vs topical piroxicam for the treatment of acute pain following upper extremity blunt trauma. Patients (ages ≥ 18 years) who presented to a Turkish emergency department within 2 hours of upper extremity injury were randomized to receive either 0.05% capsaicin gel (n = 69) or 0.5% piroxicam gel (n = 67). Patients reported level 5 or higher pain on the VAS. Those with fractures, dislocations, skin disruption, or other trauma were excluded. Age, gender, pain duration, and mechanism of injury did not differ significantly between study groups.1
Blinding was ensured by placing the gels in opaque containers containing 30 mg of either capsaicin or piroxicam and dyeing the medicine with red and yellow food coloring. A thin layer of medication was applied to an area no larger than 5 × 5 cm on the upper extremity and rubbed for 1 minute. Patients were observed in the emergency department for 2 hours and discharged with instructions to apply the medication 3 times daily for 72 hours.
The investigators measured pain using VAS scores at 1 hour, 2 hours, 24 hours, and 72 hours after treatment. Topical capsaicin was superior to topical piroxicam at achieving both primary outcomes: a VAS score of ≤ 4 (85.5% vs 50.7%; number needed to treat [NNT] = 2.9; P < .001) and a > 50% reduction in VAS score (87% vs 62.7%; NNT = 4.1; P < .01) at the end of treatment.1 (These outcomes were based on earlier determinations of the minimal clinically important difference.7,8)
Additionally, capsaicin was more effective than piroxicam at each time interval. This difference was most pronounced at 72 hours, with a mean difference of delta VAS scores of 1.53 (95% CI, 0.85-2.221) and a mean percentage of the reduction in VAS scores of 19.7% (95% CI, 12.4%-27.2%) (P < .001).1
Reported adverse effects, such as burning, itching, and rash, were mild and infrequent and showed no significant difference between the treatment groups.
WHAT’S NEW
First study comparing topical capsaicin and a topical NSAID in acute trauma
Although both capsaicin and topical piroxicam have proven efficacy for the treatment of pain, this RCT is the first study to directly compare these agents in the setting of acute upper extremity blunt trauma. Capsaicin is currently more commonly prescribed as a treatment for chronic neuropathic pain.4,9 In this study, capsaicin demonstrated superior results in pain reduction at each assessed time interval and at the primary end point of 72 hours.
CAVEATS
Limited generalizability to lower extremity and truncal trauma
This RCT included a relatively small sample size (136 patients). Researchers evaluated only blunt upper extremity injuries; as such, the generalizability of the effectiveness of topical capsaicin in blunt lower extremity and truncal trauma is limited, especially over larger surface areas.
CHALLENGES TO IMPLEMENTATION
No major challenges found
There are no major challenges to implementing this inexpensive treatment.
1. Kocak AO, Dogruyol S, Akbas I, et al. Comparison of topical capsaicin and topical piroxicam in the treatment of acute trauma-induced pain: a randomized double-blind trial. Am J Emerg Med. 2020;38:1767-1771. doi: 10.1016/j.ajem.2020.05.104
2. Busse JW, Sadeghirad B, Oparin Y, et al. Management of acute pain from non–low back, musculoskeletal injuries: a systematic review and network meta-analysis of randomized trials. Ann Intern Med. 2020;173:730-738. doi: 10.7326/M19-3601
3. Chrubasik S, Weiser T, Beime B. Effectiveness and safety of topical capsaicin cream in the treatment of chronic soft tissue pain. Phytother Res. 2010;24:1877-1885. doi: 10.1002/ptr.3335
4. Derry S, Moore RA. Topical capsaicin (low concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2012(9):CD010111. doi: 10.1002/14651858.CD010111
5. Simpson DM, Robinson-Papp J, Van J, et al. Capsaicin 8% patch in painful diabetic peripheral neuropathy: a randomized, double-blind, placebo-controlled study. J Pain. 2017;18:42-53. doi: 10.1016/j.jpain.2016.09.008
6. Papoiu ADP, Yosipovitch G. Topical capsaicin. The fire of a ‘hot’ medicine is reignited. Expert Opin Pharmacother. 2010;11:1359-1371. doi: 10.1517/14656566.2010.481670
7. Kulkantrakorn K, Lorsuwansiri C, Meesawatsom P. 0.025% capsaicin gel for the treatment of painful diabetic neuropathy: a randomized, double-blind, crossover, placebo-controlled trial. Pain Pract. 2013;13:497-503. doi: 10.1111/papr.12013
8. Kocak AO, Ahiskalioglu A, Sengun E, et al. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: a prospective randomized study. Am J Emerg Med. 2019;37:1927-1931. doi: 10.1016/j.ajem.2019.01.015
9. Derry S, Rice ASC, Cole P, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;1(1):CD007393. doi: 10.1002/14651858.CD007393.pub4
1. Kocak AO, Dogruyol S, Akbas I, et al. Comparison of topical capsaicin and topical piroxicam in the treatment of acute trauma-induced pain: a randomized double-blind trial. Am J Emerg Med. 2020;38:1767-1771. doi: 10.1016/j.ajem.2020.05.104
2. Busse JW, Sadeghirad B, Oparin Y, et al. Management of acute pain from non–low back, musculoskeletal injuries: a systematic review and network meta-analysis of randomized trials. Ann Intern Med. 2020;173:730-738. doi: 10.7326/M19-3601
3. Chrubasik S, Weiser T, Beime B. Effectiveness and safety of topical capsaicin cream in the treatment of chronic soft tissue pain. Phytother Res. 2010;24:1877-1885. doi: 10.1002/ptr.3335
4. Derry S, Moore RA. Topical capsaicin (low concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2012(9):CD010111. doi: 10.1002/14651858.CD010111
5. Simpson DM, Robinson-Papp J, Van J, et al. Capsaicin 8% patch in painful diabetic peripheral neuropathy: a randomized, double-blind, placebo-controlled study. J Pain. 2017;18:42-53. doi: 10.1016/j.jpain.2016.09.008
6. Papoiu ADP, Yosipovitch G. Topical capsaicin. The fire of a ‘hot’ medicine is reignited. Expert Opin Pharmacother. 2010;11:1359-1371. doi: 10.1517/14656566.2010.481670
7. Kulkantrakorn K, Lorsuwansiri C, Meesawatsom P. 0.025% capsaicin gel for the treatment of painful diabetic neuropathy: a randomized, double-blind, crossover, placebo-controlled trial. Pain Pract. 2013;13:497-503. doi: 10.1111/papr.12013
8. Kocak AO, Ahiskalioglu A, Sengun E, et al. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: a prospective randomized study. Am J Emerg Med. 2019;37:1927-1931. doi: 10.1016/j.ajem.2019.01.015
9. Derry S, Rice ASC, Cole P, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;1(1):CD007393. doi: 10.1002/14651858.CD007393.pub4
PRACTICE CHANGER
Use topical capsaicin gel 0.05% for pain reduction in patients with isolated blunt injuries of the upper extremity without fracture.
STRENGTH OF RECOMMENDATION
B: Based on a single randomized controlled trial (RCT)1
Kocak AO, Dogruyol S, Akbas I, et al. Comparison of topical capsaicin and topical piroxicam in the treatment of acute trauma-induced pain: a randomized double-blind trial. Am J Emerg Med. 2020;38:1767-1771.
Getting a jump on recovery from sports-related concussion
ILLUSTRATIVE CASE
A 16-year-old girl with no chronic medical illness presents to your office with her parents after sustaining a head injury at a soccer game over the weekend. She collided with another player while attempting to head the ball. Immediately afterward, she was taken off the field and assessed. She was confused but had a normal level of consciousness and denied vision changes, weakness or tingling in her arms or legs, severe headache, or neck pain. Further testing revealed dizziness and abnormal balance. Her confusion and abnormal balance resolved after 1 day. She has had a mild headache and light sensitivity since the event. She otherwise feels well at rest in the office. She wants to recover quickly but safely and has heard conflicting statements about whether she should completely rest or start back to light activity now.
Sports-related concussions (SRCs) are highly prevalent in the United States, with as many as 3.8 million cases annually. Of those, 1.1 to 1.9 million cases are in children 18 years old or younger.2,3 SRCs are defined by the Concussion in Sport Group (CISG) 2017 consensus statement as involving the following criteria: (1) direct or indirect trauma anywhere on the body with force transmitted to the head; (2) rapid or delayed symptom presentation, typically with spontaneous resolution; (3) functional rather than structural injury; and (4) occurrence with or without loss of consciousness with stepwise symptom resolution.4
SRCs do not have a proven, effective treatment and can have short- or long-term consequences. Initial treatment includes removing athletes from play immediately after an event. The American Academy of Neurology recommends that athletes not return to play until the concussion is resolved, as judged by a health care provider, and the athlete is asymptomatic when off medication.2
The CISG recommends a 6-step approach, with each step taking at least 24 hours.4 The final step is a return to normal activity.4 This working group recommended extensive study of rehabilitation programs involving subsymptom threshold exercise (ie, exercise performed at a level that does not exacerbate symptoms) before implementation as routine practice. Evidence from a 2015 study suggests that following strict rest for 5 days until complete symptom resolution may prolong recovery compared with rest for only 1 to 2 days.5 Additionally, strict rest did not show a difference in neurocognitive or balance outcomes in that study, and the authors noted it may also negatively impact academic, sports, and social function in adolescents.5 This study looked at the potential benefit of subsymptom threshold exercise during recovery from SRC.1
STUDY SUMMARY
Light aerobic exercise may help speed recovery
This multicenter, prospective, parallel, randomized clinical trial compared subsymptom threshold aerobic exercise to placebo-like stretching. Patients were included if they were ages 13 to 18 years and presented within 10 days of an SRC, as diagnosed using the CISG criteria. Exclusion criteria included focal neurologic deficits; history of moderate or severe traumatic brain injury; inability to exercise due to orthopedic injury, cervical spine injury, diabetes, or heart disease; increased cardiac risk; or low postconcussion symptom severity. Patients with a diagnosis of and treatment with medication for attention-deficit/hyperactivity disorder (ADHD), depression, anxiety, or learning disorder were excluded, as were patients with a history of more than 3 previous concussions.
Patients in the aerobic exercise group were instructed to use a stationary bike or treadmill (or equivalent walking or jogging if they did not have access to this equipment) at a prescribed heart rate. The target heart rate was 80% of the heart rate achieved during initial assessment with the Buffalo Concussion Treadmill Test (BCTT).6 Patients in this group were instructed to exercise for 20 minutes or to the point at which their symptoms increased by 2 points (on a 10-point scale) from pre-exercise levels, whichever came first, with rest prescribed at all other times.
For the placebo-like group, a stretching instruction booklet was provided, with the goal of achieving a heart rate that was not significantly elevated. Participants in this group were told to perform the stretches for 20 minutes daily. Of note, researchers ensured the level of physician and research staff attention was similar for each patient, regardless of treatment group, to prevent intervention bias. Additionally, interventions were not initiated prior to 48 hours from the time of injury.
Continue to: The primary outcome...
The primary outcome was number of days to recovery since the date of injury. This was defined as symptom resolution to normal (as evaluated by a physician blinded to the study group) and by the patient’s ability to exercise to exhaustion without symptom exacerbation on the BCTT. Secondary outcomes measured the proportion of patients with delayed recovery (defined as recovery requiring > 30 days) and daily symptom scores.
Of 165 patients meeting the inclusion criteria, 52 patients were excluded prior to randomization (12 patients chose not to participate, 39 were excluded for lack of symptoms, and 1 withdrew due to severe symptoms on the BCTT). A total of 113 were randomized to either group, and 103 patients completed the study (10 patients did not complete the study or had another illness during the intervention). The study analysis included 52 patients in the aerobic exercise group and 51 in the placebo-like stretching group. The study was powered to detect a significant difference in recovery time.
Patients were about equally divided by sex, with a mean age of 15 years. Patients who had no previous concussion made up 50% of the aerobic group and 57% of the stretching group. The average time since injury was similar in the aerobic and stretching groups (4.9 days and 4.8 days, respectively). The aerobic exercise group recovered in a median of 13 days (interquartile range [IQR] = 10-18.5 days) compared with a median of 17 days (IQR = 13-23 days) for the stretching group (P = .009). The incidence of delayed recovery (> 30 days) was higher in the stretching group (n = 7) compared with the aerobic exercise group (n = 2) but was not statistically significant. Daily symptom reporting occurred at a high rate in both groups, with patients stating that they performed their prescribed exercise 89% of the time. No adverse events were reported.
WHAT’S NEW
First high-quality study to support evidence for early light activity
This is the first high-quality study of subsymptom threshold exercise for SRC. Its findings add to the growing body of evidence that early engagement in light aerobic activity that does not provoke symptoms (but not fully returning to sports activity) can aid in recovery from an SRC.
CAVEATS
Narrow study population limits application of findings
It is unclear if subsymptom threshold exercise is safe and effective in adolescents with a history of multiple concussions, as those with more than 3 concussions were excluded from this study. Additionally, patients with comorbidities such as ADHD, depression, anxiety, or learning disorders were not included in this study, which limits the application of these findings. The generalizability of this study is limited in younger children, adults, those with increased cardiovascular risk, and in patients with concussions that are not sports related.
CHALLENGES TO IMPLEMENTATION
More real-world studies needed to confirm benefit
The majority of adolescent athletes in this study completed the subsymptom threshold exercise in a monitored environment with trainers, heart rate monitors, and access to equipment, limiting the study’s generalizability. Additionally, physicians need to be familiar with the BCTT to assign heart rate goals and assess improvement. The study environment may be feasible for some but not others. Studies evaluating real-world settings with athletes self-monitoring for symptom threshold with stepwise evaluations are needed and may be more broadly applicable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173:319-325. doi: 10.1001/jamapediatrics.2018.4397
2. Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250-2257. doi: 10.1212/WNL.0b013e31828d57dd
3. Bryan MA, Rowhani-Rahbar A, Comstock RD, et al; Seattle Sports Concussion Research Collaborative. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138:e20154635. doi: 10.1542/peds.2015-4635
4. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51:838-847. doi: 10.1136/bjsports-2017-097699
5. Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015;135:213-223.
6. Leddy JJ, Haider MN, Willer BS. Buffalo Concussion Treadmill Test (BCTT) – Instruction Manual. Accessed March 16, 2022. https://cdn-links.lww.com/permalink/jsm/a/jsm_2020_01_28_haider_19-313_sdc1.pdf
ILLUSTRATIVE CASE
A 16-year-old girl with no chronic medical illness presents to your office with her parents after sustaining a head injury at a soccer game over the weekend. She collided with another player while attempting to head the ball. Immediately afterward, she was taken off the field and assessed. She was confused but had a normal level of consciousness and denied vision changes, weakness or tingling in her arms or legs, severe headache, or neck pain. Further testing revealed dizziness and abnormal balance. Her confusion and abnormal balance resolved after 1 day. She has had a mild headache and light sensitivity since the event. She otherwise feels well at rest in the office. She wants to recover quickly but safely and has heard conflicting statements about whether she should completely rest or start back to light activity now.
Sports-related concussions (SRCs) are highly prevalent in the United States, with as many as 3.8 million cases annually. Of those, 1.1 to 1.9 million cases are in children 18 years old or younger.2,3 SRCs are defined by the Concussion in Sport Group (CISG) 2017 consensus statement as involving the following criteria: (1) direct or indirect trauma anywhere on the body with force transmitted to the head; (2) rapid or delayed symptom presentation, typically with spontaneous resolution; (3) functional rather than structural injury; and (4) occurrence with or without loss of consciousness with stepwise symptom resolution.4
SRCs do not have a proven, effective treatment and can have short- or long-term consequences. Initial treatment includes removing athletes from play immediately after an event. The American Academy of Neurology recommends that athletes not return to play until the concussion is resolved, as judged by a health care provider, and the athlete is asymptomatic when off medication.2
The CISG recommends a 6-step approach, with each step taking at least 24 hours.4 The final step is a return to normal activity.4 This working group recommended extensive study of rehabilitation programs involving subsymptom threshold exercise (ie, exercise performed at a level that does not exacerbate symptoms) before implementation as routine practice. Evidence from a 2015 study suggests that following strict rest for 5 days until complete symptom resolution may prolong recovery compared with rest for only 1 to 2 days.5 Additionally, strict rest did not show a difference in neurocognitive or balance outcomes in that study, and the authors noted it may also negatively impact academic, sports, and social function in adolescents.5 This study looked at the potential benefit of subsymptom threshold exercise during recovery from SRC.1
STUDY SUMMARY
Light aerobic exercise may help speed recovery
This multicenter, prospective, parallel, randomized clinical trial compared subsymptom threshold aerobic exercise to placebo-like stretching. Patients were included if they were ages 13 to 18 years and presented within 10 days of an SRC, as diagnosed using the CISG criteria. Exclusion criteria included focal neurologic deficits; history of moderate or severe traumatic brain injury; inability to exercise due to orthopedic injury, cervical spine injury, diabetes, or heart disease; increased cardiac risk; or low postconcussion symptom severity. Patients with a diagnosis of and treatment with medication for attention-deficit/hyperactivity disorder (ADHD), depression, anxiety, or learning disorder were excluded, as were patients with a history of more than 3 previous concussions.
Patients in the aerobic exercise group were instructed to use a stationary bike or treadmill (or equivalent walking or jogging if they did not have access to this equipment) at a prescribed heart rate. The target heart rate was 80% of the heart rate achieved during initial assessment with the Buffalo Concussion Treadmill Test (BCTT).6 Patients in this group were instructed to exercise for 20 minutes or to the point at which their symptoms increased by 2 points (on a 10-point scale) from pre-exercise levels, whichever came first, with rest prescribed at all other times.
For the placebo-like group, a stretching instruction booklet was provided, with the goal of achieving a heart rate that was not significantly elevated. Participants in this group were told to perform the stretches for 20 minutes daily. Of note, researchers ensured the level of physician and research staff attention was similar for each patient, regardless of treatment group, to prevent intervention bias. Additionally, interventions were not initiated prior to 48 hours from the time of injury.
Continue to: The primary outcome...
The primary outcome was number of days to recovery since the date of injury. This was defined as symptom resolution to normal (as evaluated by a physician blinded to the study group) and by the patient’s ability to exercise to exhaustion without symptom exacerbation on the BCTT. Secondary outcomes measured the proportion of patients with delayed recovery (defined as recovery requiring > 30 days) and daily symptom scores.
Of 165 patients meeting the inclusion criteria, 52 patients were excluded prior to randomization (12 patients chose not to participate, 39 were excluded for lack of symptoms, and 1 withdrew due to severe symptoms on the BCTT). A total of 113 were randomized to either group, and 103 patients completed the study (10 patients did not complete the study or had another illness during the intervention). The study analysis included 52 patients in the aerobic exercise group and 51 in the placebo-like stretching group. The study was powered to detect a significant difference in recovery time.
Patients were about equally divided by sex, with a mean age of 15 years. Patients who had no previous concussion made up 50% of the aerobic group and 57% of the stretching group. The average time since injury was similar in the aerobic and stretching groups (4.9 days and 4.8 days, respectively). The aerobic exercise group recovered in a median of 13 days (interquartile range [IQR] = 10-18.5 days) compared with a median of 17 days (IQR = 13-23 days) for the stretching group (P = .009). The incidence of delayed recovery (> 30 days) was higher in the stretching group (n = 7) compared with the aerobic exercise group (n = 2) but was not statistically significant. Daily symptom reporting occurred at a high rate in both groups, with patients stating that they performed their prescribed exercise 89% of the time. No adverse events were reported.
WHAT’S NEW
First high-quality study to support evidence for early light activity
This is the first high-quality study of subsymptom threshold exercise for SRC. Its findings add to the growing body of evidence that early engagement in light aerobic activity that does not provoke symptoms (but not fully returning to sports activity) can aid in recovery from an SRC.
CAVEATS
Narrow study population limits application of findings
It is unclear if subsymptom threshold exercise is safe and effective in adolescents with a history of multiple concussions, as those with more than 3 concussions were excluded from this study. Additionally, patients with comorbidities such as ADHD, depression, anxiety, or learning disorders were not included in this study, which limits the application of these findings. The generalizability of this study is limited in younger children, adults, those with increased cardiovascular risk, and in patients with concussions that are not sports related.
CHALLENGES TO IMPLEMENTATION
More real-world studies needed to confirm benefit
The majority of adolescent athletes in this study completed the subsymptom threshold exercise in a monitored environment with trainers, heart rate monitors, and access to equipment, limiting the study’s generalizability. Additionally, physicians need to be familiar with the BCTT to assign heart rate goals and assess improvement. The study environment may be feasible for some but not others. Studies evaluating real-world settings with athletes self-monitoring for symptom threshold with stepwise evaluations are needed and may be more broadly applicable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 16-year-old girl with no chronic medical illness presents to your office with her parents after sustaining a head injury at a soccer game over the weekend. She collided with another player while attempting to head the ball. Immediately afterward, she was taken off the field and assessed. She was confused but had a normal level of consciousness and denied vision changes, weakness or tingling in her arms or legs, severe headache, or neck pain. Further testing revealed dizziness and abnormal balance. Her confusion and abnormal balance resolved after 1 day. She has had a mild headache and light sensitivity since the event. She otherwise feels well at rest in the office. She wants to recover quickly but safely and has heard conflicting statements about whether she should completely rest or start back to light activity now.
Sports-related concussions (SRCs) are highly prevalent in the United States, with as many as 3.8 million cases annually. Of those, 1.1 to 1.9 million cases are in children 18 years old or younger.2,3 SRCs are defined by the Concussion in Sport Group (CISG) 2017 consensus statement as involving the following criteria: (1) direct or indirect trauma anywhere on the body with force transmitted to the head; (2) rapid or delayed symptom presentation, typically with spontaneous resolution; (3) functional rather than structural injury; and (4) occurrence with or without loss of consciousness with stepwise symptom resolution.4
SRCs do not have a proven, effective treatment and can have short- or long-term consequences. Initial treatment includes removing athletes from play immediately after an event. The American Academy of Neurology recommends that athletes not return to play until the concussion is resolved, as judged by a health care provider, and the athlete is asymptomatic when off medication.2
The CISG recommends a 6-step approach, with each step taking at least 24 hours.4 The final step is a return to normal activity.4 This working group recommended extensive study of rehabilitation programs involving subsymptom threshold exercise (ie, exercise performed at a level that does not exacerbate symptoms) before implementation as routine practice. Evidence from a 2015 study suggests that following strict rest for 5 days until complete symptom resolution may prolong recovery compared with rest for only 1 to 2 days.5 Additionally, strict rest did not show a difference in neurocognitive or balance outcomes in that study, and the authors noted it may also negatively impact academic, sports, and social function in adolescents.5 This study looked at the potential benefit of subsymptom threshold exercise during recovery from SRC.1
STUDY SUMMARY
Light aerobic exercise may help speed recovery
This multicenter, prospective, parallel, randomized clinical trial compared subsymptom threshold aerobic exercise to placebo-like stretching. Patients were included if they were ages 13 to 18 years and presented within 10 days of an SRC, as diagnosed using the CISG criteria. Exclusion criteria included focal neurologic deficits; history of moderate or severe traumatic brain injury; inability to exercise due to orthopedic injury, cervical spine injury, diabetes, or heart disease; increased cardiac risk; or low postconcussion symptom severity. Patients with a diagnosis of and treatment with medication for attention-deficit/hyperactivity disorder (ADHD), depression, anxiety, or learning disorder were excluded, as were patients with a history of more than 3 previous concussions.
Patients in the aerobic exercise group were instructed to use a stationary bike or treadmill (or equivalent walking or jogging if they did not have access to this equipment) at a prescribed heart rate. The target heart rate was 80% of the heart rate achieved during initial assessment with the Buffalo Concussion Treadmill Test (BCTT).6 Patients in this group were instructed to exercise for 20 minutes or to the point at which their symptoms increased by 2 points (on a 10-point scale) from pre-exercise levels, whichever came first, with rest prescribed at all other times.
For the placebo-like group, a stretching instruction booklet was provided, with the goal of achieving a heart rate that was not significantly elevated. Participants in this group were told to perform the stretches for 20 minutes daily. Of note, researchers ensured the level of physician and research staff attention was similar for each patient, regardless of treatment group, to prevent intervention bias. Additionally, interventions were not initiated prior to 48 hours from the time of injury.
Continue to: The primary outcome...
The primary outcome was number of days to recovery since the date of injury. This was defined as symptom resolution to normal (as evaluated by a physician blinded to the study group) and by the patient’s ability to exercise to exhaustion without symptom exacerbation on the BCTT. Secondary outcomes measured the proportion of patients with delayed recovery (defined as recovery requiring > 30 days) and daily symptom scores.
Of 165 patients meeting the inclusion criteria, 52 patients were excluded prior to randomization (12 patients chose not to participate, 39 were excluded for lack of symptoms, and 1 withdrew due to severe symptoms on the BCTT). A total of 113 were randomized to either group, and 103 patients completed the study (10 patients did not complete the study or had another illness during the intervention). The study analysis included 52 patients in the aerobic exercise group and 51 in the placebo-like stretching group. The study was powered to detect a significant difference in recovery time.
Patients were about equally divided by sex, with a mean age of 15 years. Patients who had no previous concussion made up 50% of the aerobic group and 57% of the stretching group. The average time since injury was similar in the aerobic and stretching groups (4.9 days and 4.8 days, respectively). The aerobic exercise group recovered in a median of 13 days (interquartile range [IQR] = 10-18.5 days) compared with a median of 17 days (IQR = 13-23 days) for the stretching group (P = .009). The incidence of delayed recovery (> 30 days) was higher in the stretching group (n = 7) compared with the aerobic exercise group (n = 2) but was not statistically significant. Daily symptom reporting occurred at a high rate in both groups, with patients stating that they performed their prescribed exercise 89% of the time. No adverse events were reported.
WHAT’S NEW
First high-quality study to support evidence for early light activity
This is the first high-quality study of subsymptom threshold exercise for SRC. Its findings add to the growing body of evidence that early engagement in light aerobic activity that does not provoke symptoms (but not fully returning to sports activity) can aid in recovery from an SRC.
CAVEATS
Narrow study population limits application of findings
It is unclear if subsymptom threshold exercise is safe and effective in adolescents with a history of multiple concussions, as those with more than 3 concussions were excluded from this study. Additionally, patients with comorbidities such as ADHD, depression, anxiety, or learning disorders were not included in this study, which limits the application of these findings. The generalizability of this study is limited in younger children, adults, those with increased cardiovascular risk, and in patients with concussions that are not sports related.
CHALLENGES TO IMPLEMENTATION
More real-world studies needed to confirm benefit
The majority of adolescent athletes in this study completed the subsymptom threshold exercise in a monitored environment with trainers, heart rate monitors, and access to equipment, limiting the study’s generalizability. Additionally, physicians need to be familiar with the BCTT to assign heart rate goals and assess improvement. The study environment may be feasible for some but not others. Studies evaluating real-world settings with athletes self-monitoring for symptom threshold with stepwise evaluations are needed and may be more broadly applicable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173:319-325. doi: 10.1001/jamapediatrics.2018.4397
2. Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250-2257. doi: 10.1212/WNL.0b013e31828d57dd
3. Bryan MA, Rowhani-Rahbar A, Comstock RD, et al; Seattle Sports Concussion Research Collaborative. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138:e20154635. doi: 10.1542/peds.2015-4635
4. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51:838-847. doi: 10.1136/bjsports-2017-097699
5. Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015;135:213-223.
6. Leddy JJ, Haider MN, Willer BS. Buffalo Concussion Treadmill Test (BCTT) – Instruction Manual. Accessed March 16, 2022. https://cdn-links.lww.com/permalink/jsm/a/jsm_2020_01_28_haider_19-313_sdc1.pdf
1. Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173:319-325. doi: 10.1001/jamapediatrics.2018.4397
2. Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250-2257. doi: 10.1212/WNL.0b013e31828d57dd
3. Bryan MA, Rowhani-Rahbar A, Comstock RD, et al; Seattle Sports Concussion Research Collaborative. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138:e20154635. doi: 10.1542/peds.2015-4635
4. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51:838-847. doi: 10.1136/bjsports-2017-097699
5. Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015;135:213-223.
6. Leddy JJ, Haider MN, Willer BS. Buffalo Concussion Treadmill Test (BCTT) – Instruction Manual. Accessed March 16, 2022. https://cdn-links.lww.com/permalink/jsm/a/jsm_2020_01_28_haider_19-313_sdc1.pdf
PRACTICE CHANGER
Recommend subsymptom threshold exercise in adolescents with a sports-related concussion. Early return to light aerobic activity not only seems safe but may help speed recovery compared with stretching alone in this patient population.
STRENGTH OF RECOMMENDATION
B: Based on a single multicenter, prospective, randomized clinical trial1
Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173:319-325. doi: 10.1001/jamapediatrics.2018.4397
Alcohol abstinence reduces A-fib burden in drinkers
ILLUSTRATIVE CASE
A 61-year-old man with hypertension and paroxysmal AF presents to your office shortly after experiencing his third episode of AF in the past 6 months. He describes these episodes, which last for several days, as “just awful,” noting that when he experiences AF, he has fatigue, palpitations, and shortness of breath and “can’t stop paying attention to my heart.” The patient, who has a body mass index of 32, consumes more than 15 alcoholic drinks per week. What can you recommend to him that will decrease his likelihood of experiencing more episodes of AF?
AF is the most common sustained cardiac arrhythmia. It is associated with significant morbidity and mortality. Known risk factors include obesity, physical inactivity, sleep apnea, diabetes, and hypertension.2
According to the Centers for Disease Control and Prevention, an estimated 12.1 million people in the United States will have AF by 2030. In 2018, AF was mentioned on more than 183,000 death certificates and was the underlying cause of more than 26,000 of those deaths.3 AF is the primary diagnosis in 450,000 hospitalizations annually,4 and the death rate from AF as the primary or contributing cause of death has been rising for more than 2 decades.3
More than 50% of Americans report alcohol consumption within the past month.5 Although alcohol use is associated with new and recurrent AF, only limited prospective data show a clear and causal association between abstaining from alcohol and decreasing AF recurrence.
STUDY SUMMARY
Reduction in AF recurrence and total AF burden following alcohol abstinence
This multicenter, prospective, open-label, randomized controlled trial (N = 140) from 6 sites in Australia evaluated the impact of alcohol abstinence on both the recurrence of AF and the amount of time in AF. Study participants were ages 18 to 85 years, consumed 10 or more standard alcohol-containing drinks per week, had paroxysmal or persistent AF, and were in sinus rhythm at the time of enrollment, regardless of antiarrhythmic therapy. Exclusion criteria included alcohol dependence or abuse, severe left ventricular systolic dysfunction (ejection fraction < 35%), clinically significant noncardiac illness, and/or coexisting psychiatric disorder.1
After a 4-week run-in period, patients were randomized to either an abstinence or a control group in a 1:1 fashion. Patients enrolled in the abstinence group were encouraged to abstain from alcohol consumption for 6 months and were provided with written and oral instructions to assist with abstaining. Control group patients continued their same level of alcohol consumption. Comprehensive rhythm monitoring occurred for all patients after randomization.
Alcohol consumption was reported by both groups using a weekly alcohol diary, supplemented with a visual guide showing pictures of standard alcohol drinks. For the abstinence group, random urine testing for ethyl glucuronide (an alcohol metabolite) was possible if no alcohol intake was reported. Primary outcomes during the 6-month study included recurrence of AF and total AF burden (percentage of time in AF).
Continue to: Secondary outcomes included hospitalizations...
Secondary outcomes included hospitalizations for AF, AF symptom severity, and change in weight. Blood pressure, quality-of-life, and depression scores were missing for > 35% of patients.1
Patients were randomized evenly to the control and abstinence groups. The typical patient was an overweight male in his early 60s with paroxysmal AF, who was taking an antiarrhythmic agent. Patients in the abstinence group decreased their alcohol consumption from 16.8 to 2.1 drinks per week (87.5% reduction; mean difference = –14.7; 95% CI, –12.7 to –16.7). Patients in the control group reduced their intake from 16.4 to 13.2 drinks per week (19.5% reduction; mean difference = –3.2; 95% CI, –1.9 to –4.4).1
AF recurred in 53% vs 73% of the abstinence and control groups, respectively, with a longer period before recurrence in the abstinence group than in the control group (hazard ratio = 0.55; 95% CI, 0.36-0.84; P = .005; number needed to treat = 5). The AF burden was also lower in the abstinence group (0.5%; interquartile range [IQR] = 0.0-3.0) than in the control group (1.2%; IQR = 0.0-10.3; P = .01). The abstinence group had a lower percentage of AF hospitalizations compared with the control group (9% vs 20%), and fewer patients reporting moderate or severe AF symptoms (10% vs 32%). In addition, the abstinence group lost 3.7 kg more weight than did the control group at 6 months.1
WHAT’S NEW
Objective new evidence for effective patient counseling
Alcohol consumption and its association with the onset and recurrence of AF has been documented previously.6 This study was the first to prospectively examine if abstaining from alcohol reduces paroxysmal AF episodes in moderate drinkers.
The study identified clinically meaningful findings among those who abstained from alcohol, including decreased AF recurrence rates, increased time to recurrence, and lower overall AF burden. This provides objective evidence that can be used for motivational interviewing in patients with paroxysmal AF who may be receptive to reducing or abstaining from alcohol consumption.
Continue to: CAVEATS
CAVEATS
The narrow study population may not be widely applicable
The study population was predominantly male, in their seventh decade of life (mean age, 61), and living in Australia. Rates of AF and symptomatology differ by gender and age, making this information challenging to apply to women or older populations. The study excluded patients with alcohol dependence or abuse, left ventricular systolic dysfunction (ejection fraction < 35%), coexisting psychiatric disorders, and clinically significant noncardiac illnesses, limiting the study’s generalizability to these patient populations. Overall, AF recurrence was low in both groups despite the intervention, and the study did not evaluate the efficacy of the counseling method for abstinence.
Since publication of this article, a prospective cohort study of approximately 3800 Swiss patients with AF evaluated the effect of alcohol consumption on the rate of stroke and embolic events. That study did not find statistically significant correlations between patients who drank no alcohol per day, > 0 to < 1, 1 to < 2, or ≥ 2 drinks per day and their rate of stroke.7 However, this study did not specifically evaluate the rate of AF recurrence or time spent in AF among the cohort, which is clinically meaningful for patient morbidity.1
CHALLENGES TO IMPLEMENTATION
Patient willingness to cut alcohol consumption may be limited
The largest challenge to implementation of this intervention is most likely the willingness of patients to cut their alcohol consumption. In this study population, 697 patients were screened for enrollment and met inclusion criteria; however, 491 patients (70.4%) were not willing to consider abstinence from alcohol, and after the run-in phase, another 17 declined randomization. Many primary care physicians would likely agree that while it is easy to encourage patients to drink less, patient adherence to these recommendations, particularly abstaining, is likely to be limited.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382:20-28. doi: 10.1056/NEJMoa1817591
2. Chung MK, Eckhardt LL, Chen LY, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation. 2020;141:e750-e772. doi: 10.1161/CIR.0000000000000748
3. Atrial fibrillation. Centers for Disease Control and Prevention. Last reviewed September 27, 2021. Accessed February 9, 2022. www.cdc.gov/heartdisease/atrial_fibrillation.htm
4. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56-e528. doi: 10.1161/CIR.0000000000000659
5. Alcohol facts and statistics. National Institute on Alcohol Abuse and Alcoholism. Updated June 2021. Accessed February 9, 2022. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
6. Kodama S, Saito K, Tanaka S, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2011;57:427-436. doi: 10.1016/j.jacc.2010.08.641
7. Reddiess P, Aeschbacher S, Meyre P, et al. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ. 2021;193:E117-E123. doi: 10.1503/cmaj.200778
ILLUSTRATIVE CASE
A 61-year-old man with hypertension and paroxysmal AF presents to your office shortly after experiencing his third episode of AF in the past 6 months. He describes these episodes, which last for several days, as “just awful,” noting that when he experiences AF, he has fatigue, palpitations, and shortness of breath and “can’t stop paying attention to my heart.” The patient, who has a body mass index of 32, consumes more than 15 alcoholic drinks per week. What can you recommend to him that will decrease his likelihood of experiencing more episodes of AF?
AF is the most common sustained cardiac arrhythmia. It is associated with significant morbidity and mortality. Known risk factors include obesity, physical inactivity, sleep apnea, diabetes, and hypertension.2
According to the Centers for Disease Control and Prevention, an estimated 12.1 million people in the United States will have AF by 2030. In 2018, AF was mentioned on more than 183,000 death certificates and was the underlying cause of more than 26,000 of those deaths.3 AF is the primary diagnosis in 450,000 hospitalizations annually,4 and the death rate from AF as the primary or contributing cause of death has been rising for more than 2 decades.3
More than 50% of Americans report alcohol consumption within the past month.5 Although alcohol use is associated with new and recurrent AF, only limited prospective data show a clear and causal association between abstaining from alcohol and decreasing AF recurrence.
STUDY SUMMARY
Reduction in AF recurrence and total AF burden following alcohol abstinence
This multicenter, prospective, open-label, randomized controlled trial (N = 140) from 6 sites in Australia evaluated the impact of alcohol abstinence on both the recurrence of AF and the amount of time in AF. Study participants were ages 18 to 85 years, consumed 10 or more standard alcohol-containing drinks per week, had paroxysmal or persistent AF, and were in sinus rhythm at the time of enrollment, regardless of antiarrhythmic therapy. Exclusion criteria included alcohol dependence or abuse, severe left ventricular systolic dysfunction (ejection fraction < 35%), clinically significant noncardiac illness, and/or coexisting psychiatric disorder.1
After a 4-week run-in period, patients were randomized to either an abstinence or a control group in a 1:1 fashion. Patients enrolled in the abstinence group were encouraged to abstain from alcohol consumption for 6 months and were provided with written and oral instructions to assist with abstaining. Control group patients continued their same level of alcohol consumption. Comprehensive rhythm monitoring occurred for all patients after randomization.
Alcohol consumption was reported by both groups using a weekly alcohol diary, supplemented with a visual guide showing pictures of standard alcohol drinks. For the abstinence group, random urine testing for ethyl glucuronide (an alcohol metabolite) was possible if no alcohol intake was reported. Primary outcomes during the 6-month study included recurrence of AF and total AF burden (percentage of time in AF).
Continue to: Secondary outcomes included hospitalizations...
Secondary outcomes included hospitalizations for AF, AF symptom severity, and change in weight. Blood pressure, quality-of-life, and depression scores were missing for > 35% of patients.1
Patients were randomized evenly to the control and abstinence groups. The typical patient was an overweight male in his early 60s with paroxysmal AF, who was taking an antiarrhythmic agent. Patients in the abstinence group decreased their alcohol consumption from 16.8 to 2.1 drinks per week (87.5% reduction; mean difference = –14.7; 95% CI, –12.7 to –16.7). Patients in the control group reduced their intake from 16.4 to 13.2 drinks per week (19.5% reduction; mean difference = –3.2; 95% CI, –1.9 to –4.4).1
AF recurred in 53% vs 73% of the abstinence and control groups, respectively, with a longer period before recurrence in the abstinence group than in the control group (hazard ratio = 0.55; 95% CI, 0.36-0.84; P = .005; number needed to treat = 5). The AF burden was also lower in the abstinence group (0.5%; interquartile range [IQR] = 0.0-3.0) than in the control group (1.2%; IQR = 0.0-10.3; P = .01). The abstinence group had a lower percentage of AF hospitalizations compared with the control group (9% vs 20%), and fewer patients reporting moderate or severe AF symptoms (10% vs 32%). In addition, the abstinence group lost 3.7 kg more weight than did the control group at 6 months.1
WHAT’S NEW
Objective new evidence for effective patient counseling
Alcohol consumption and its association with the onset and recurrence of AF has been documented previously.6 This study was the first to prospectively examine if abstaining from alcohol reduces paroxysmal AF episodes in moderate drinkers.
The study identified clinically meaningful findings among those who abstained from alcohol, including decreased AF recurrence rates, increased time to recurrence, and lower overall AF burden. This provides objective evidence that can be used for motivational interviewing in patients with paroxysmal AF who may be receptive to reducing or abstaining from alcohol consumption.
Continue to: CAVEATS
CAVEATS
The narrow study population may not be widely applicable
The study population was predominantly male, in their seventh decade of life (mean age, 61), and living in Australia. Rates of AF and symptomatology differ by gender and age, making this information challenging to apply to women or older populations. The study excluded patients with alcohol dependence or abuse, left ventricular systolic dysfunction (ejection fraction < 35%), coexisting psychiatric disorders, and clinically significant noncardiac illnesses, limiting the study’s generalizability to these patient populations. Overall, AF recurrence was low in both groups despite the intervention, and the study did not evaluate the efficacy of the counseling method for abstinence.
Since publication of this article, a prospective cohort study of approximately 3800 Swiss patients with AF evaluated the effect of alcohol consumption on the rate of stroke and embolic events. That study did not find statistically significant correlations between patients who drank no alcohol per day, > 0 to < 1, 1 to < 2, or ≥ 2 drinks per day and their rate of stroke.7 However, this study did not specifically evaluate the rate of AF recurrence or time spent in AF among the cohort, which is clinically meaningful for patient morbidity.1
CHALLENGES TO IMPLEMENTATION
Patient willingness to cut alcohol consumption may be limited
The largest challenge to implementation of this intervention is most likely the willingness of patients to cut their alcohol consumption. In this study population, 697 patients were screened for enrollment and met inclusion criteria; however, 491 patients (70.4%) were not willing to consider abstinence from alcohol, and after the run-in phase, another 17 declined randomization. Many primary care physicians would likely agree that while it is easy to encourage patients to drink less, patient adherence to these recommendations, particularly abstaining, is likely to be limited.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 61-year-old man with hypertension and paroxysmal AF presents to your office shortly after experiencing his third episode of AF in the past 6 months. He describes these episodes, which last for several days, as “just awful,” noting that when he experiences AF, he has fatigue, palpitations, and shortness of breath and “can’t stop paying attention to my heart.” The patient, who has a body mass index of 32, consumes more than 15 alcoholic drinks per week. What can you recommend to him that will decrease his likelihood of experiencing more episodes of AF?
AF is the most common sustained cardiac arrhythmia. It is associated with significant morbidity and mortality. Known risk factors include obesity, physical inactivity, sleep apnea, diabetes, and hypertension.2
According to the Centers for Disease Control and Prevention, an estimated 12.1 million people in the United States will have AF by 2030. In 2018, AF was mentioned on more than 183,000 death certificates and was the underlying cause of more than 26,000 of those deaths.3 AF is the primary diagnosis in 450,000 hospitalizations annually,4 and the death rate from AF as the primary or contributing cause of death has been rising for more than 2 decades.3
More than 50% of Americans report alcohol consumption within the past month.5 Although alcohol use is associated with new and recurrent AF, only limited prospective data show a clear and causal association between abstaining from alcohol and decreasing AF recurrence.
STUDY SUMMARY
Reduction in AF recurrence and total AF burden following alcohol abstinence
This multicenter, prospective, open-label, randomized controlled trial (N = 140) from 6 sites in Australia evaluated the impact of alcohol abstinence on both the recurrence of AF and the amount of time in AF. Study participants were ages 18 to 85 years, consumed 10 or more standard alcohol-containing drinks per week, had paroxysmal or persistent AF, and were in sinus rhythm at the time of enrollment, regardless of antiarrhythmic therapy. Exclusion criteria included alcohol dependence or abuse, severe left ventricular systolic dysfunction (ejection fraction < 35%), clinically significant noncardiac illness, and/or coexisting psychiatric disorder.1
After a 4-week run-in period, patients were randomized to either an abstinence or a control group in a 1:1 fashion. Patients enrolled in the abstinence group were encouraged to abstain from alcohol consumption for 6 months and were provided with written and oral instructions to assist with abstaining. Control group patients continued their same level of alcohol consumption. Comprehensive rhythm monitoring occurred for all patients after randomization.
Alcohol consumption was reported by both groups using a weekly alcohol diary, supplemented with a visual guide showing pictures of standard alcohol drinks. For the abstinence group, random urine testing for ethyl glucuronide (an alcohol metabolite) was possible if no alcohol intake was reported. Primary outcomes during the 6-month study included recurrence of AF and total AF burden (percentage of time in AF).
Continue to: Secondary outcomes included hospitalizations...
Secondary outcomes included hospitalizations for AF, AF symptom severity, and change in weight. Blood pressure, quality-of-life, and depression scores were missing for > 35% of patients.1
Patients were randomized evenly to the control and abstinence groups. The typical patient was an overweight male in his early 60s with paroxysmal AF, who was taking an antiarrhythmic agent. Patients in the abstinence group decreased their alcohol consumption from 16.8 to 2.1 drinks per week (87.5% reduction; mean difference = –14.7; 95% CI, –12.7 to –16.7). Patients in the control group reduced their intake from 16.4 to 13.2 drinks per week (19.5% reduction; mean difference = –3.2; 95% CI, –1.9 to –4.4).1
AF recurred in 53% vs 73% of the abstinence and control groups, respectively, with a longer period before recurrence in the abstinence group than in the control group (hazard ratio = 0.55; 95% CI, 0.36-0.84; P = .005; number needed to treat = 5). The AF burden was also lower in the abstinence group (0.5%; interquartile range [IQR] = 0.0-3.0) than in the control group (1.2%; IQR = 0.0-10.3; P = .01). The abstinence group had a lower percentage of AF hospitalizations compared with the control group (9% vs 20%), and fewer patients reporting moderate or severe AF symptoms (10% vs 32%). In addition, the abstinence group lost 3.7 kg more weight than did the control group at 6 months.1
WHAT’S NEW
Objective new evidence for effective patient counseling
Alcohol consumption and its association with the onset and recurrence of AF has been documented previously.6 This study was the first to prospectively examine if abstaining from alcohol reduces paroxysmal AF episodes in moderate drinkers.
The study identified clinically meaningful findings among those who abstained from alcohol, including decreased AF recurrence rates, increased time to recurrence, and lower overall AF burden. This provides objective evidence that can be used for motivational interviewing in patients with paroxysmal AF who may be receptive to reducing or abstaining from alcohol consumption.
Continue to: CAVEATS
CAVEATS
The narrow study population may not be widely applicable
The study population was predominantly male, in their seventh decade of life (mean age, 61), and living in Australia. Rates of AF and symptomatology differ by gender and age, making this information challenging to apply to women or older populations. The study excluded patients with alcohol dependence or abuse, left ventricular systolic dysfunction (ejection fraction < 35%), coexisting psychiatric disorders, and clinically significant noncardiac illnesses, limiting the study’s generalizability to these patient populations. Overall, AF recurrence was low in both groups despite the intervention, and the study did not evaluate the efficacy of the counseling method for abstinence.
Since publication of this article, a prospective cohort study of approximately 3800 Swiss patients with AF evaluated the effect of alcohol consumption on the rate of stroke and embolic events. That study did not find statistically significant correlations between patients who drank no alcohol per day, > 0 to < 1, 1 to < 2, or ≥ 2 drinks per day and their rate of stroke.7 However, this study did not specifically evaluate the rate of AF recurrence or time spent in AF among the cohort, which is clinically meaningful for patient morbidity.1
CHALLENGES TO IMPLEMENTATION
Patient willingness to cut alcohol consumption may be limited
The largest challenge to implementation of this intervention is most likely the willingness of patients to cut their alcohol consumption. In this study population, 697 patients were screened for enrollment and met inclusion criteria; however, 491 patients (70.4%) were not willing to consider abstinence from alcohol, and after the run-in phase, another 17 declined randomization. Many primary care physicians would likely agree that while it is easy to encourage patients to drink less, patient adherence to these recommendations, particularly abstaining, is likely to be limited.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382:20-28. doi: 10.1056/NEJMoa1817591
2. Chung MK, Eckhardt LL, Chen LY, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation. 2020;141:e750-e772. doi: 10.1161/CIR.0000000000000748
3. Atrial fibrillation. Centers for Disease Control and Prevention. Last reviewed September 27, 2021. Accessed February 9, 2022. www.cdc.gov/heartdisease/atrial_fibrillation.htm
4. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56-e528. doi: 10.1161/CIR.0000000000000659
5. Alcohol facts and statistics. National Institute on Alcohol Abuse and Alcoholism. Updated June 2021. Accessed February 9, 2022. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
6. Kodama S, Saito K, Tanaka S, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2011;57:427-436. doi: 10.1016/j.jacc.2010.08.641
7. Reddiess P, Aeschbacher S, Meyre P, et al. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ. 2021;193:E117-E123. doi: 10.1503/cmaj.200778
1. Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382:20-28. doi: 10.1056/NEJMoa1817591
2. Chung MK, Eckhardt LL, Chen LY, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation. 2020;141:e750-e772. doi: 10.1161/CIR.0000000000000748
3. Atrial fibrillation. Centers for Disease Control and Prevention. Last reviewed September 27, 2021. Accessed February 9, 2022. www.cdc.gov/heartdisease/atrial_fibrillation.htm
4. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56-e528. doi: 10.1161/CIR.0000000000000659
5. Alcohol facts and statistics. National Institute on Alcohol Abuse and Alcoholism. Updated June 2021. Accessed February 9, 2022. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
6. Kodama S, Saito K, Tanaka S, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2011;57:427-436. doi: 10.1016/j.jacc.2010.08.641
7. Reddiess P, Aeschbacher S, Meyre P, et al. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ. 2021;193:E117-E123. doi: 10.1503/cmaj.200778
PRACTICE CHANGER
Counsel patients with paroxysmal or persistent atrial fibrillation (AF) who drink moderately (≥ 10 drinks per week) that they can reduce their time in AF, as well as their overall recurrence of AF, by decreasing their alcohol consumption by half or more.
STRENGTH OF RECOMMENDATION
B: Based on a well-performed randomized controlled trial1
Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382:20-28.
Is it time to approach spontaneous pneumothorax more conservatively?
ILLUSTRATIVE CASE
A 26-year-old man presents to the emergency department complaining of sudden-onset left-side chest pain and mild dyspnea that started while he was playing basketball. He denies any medical problems and takes no medications. He is able to speak in complete sentences as he answers your questions. His O2 saturation is 95% and a chest x-ray reveals a left-side, moderate-to-large pneumothorax.
A primary spontaneous pneumothorax is one that occurs in the absence of underlying clinical lung disease and is not associated with an inciting cause, such as a rib fracture.2 In the United States, the estimated incidence of primary spontaneous pneumothorax is 7.4 cases per 100,000 men and 1.2 cases per 100,000 women.3 The etiology is often unknown, but it is associated with several risk factors, including male sex, smoking, and a tall, thin body habitus.2
The management strategy for stable patients with a primary spontaneous pneumothorax largely depends on pneumothorax size and institutional practice. Multiple methods define pneumothorax size; the US standard cutoff for a small or large pneumothorax is 3 cm, between the pleural line and chest wall at the level of the apex,4 compared with 2 cm in Europe, when evaluating the distance at the hilum in an upright chest radiograph.5 The Collins method uses a formula to calculate the percentage of lung area affected based on 3 distinct measurements on a posterior/anterior upright chest radiograph.6
Management options include observation, supplemental oxygen, simple aspiration, and thoracostomy or chest tube placement. British Thoracic Society guidelines published in 2010 state that only a small pneumothorax can be managed conservatively with observation alone; for a large pneumothorax, the guidelines recommend needle aspiration to achieve lung reinflation, followed by chest tube placement if unsuccessful.5
In practice, management of a large primary spontaneous pneumothorax varies, but the most common treatment is chest tube placement.7 This procedure can be painful and may result in complications such as bleeding, infection, injury to internal structures, or the need for surgical intervention.7 In addition, once a chest tube is placed, hospital admission ensues, lasting an average of 4 days.8 Given these consequences, there is a need for safe and feasible treatment options for a large primary spontaneous pneumothorax.
STUDY SUMMARY
Observational management judged noninferior, with multiple advantages
The Primary Spontaneous Pneumothorax (PSP) trial was a prospective noninferiority trial conducted at 39 hospitals in Australia and New Zealand. This randomized controlled trial compared observational (“watch and wait”) vs interventional (chest tube placement) management of uncomplicated, unilateral, primary spontaneous pneumothorax. Patients ages 14 to 50 years with a moderate-to-large pneumothorax—32% or greater, as defined by the Collins method4—were randomly assigned to a study group to examine the primary outcome of lung reexpansion at 8 weeks.
The intervention included chest tube insertion attached to an underwater seal without suction for 1 hour, followed by an x-ray and clamping for 4 hours if there was no air leak, followed by a repeat chest x-ray. If there was no evidence of radiographic resolution, or if during observation the pneumothorax recurred, the underwater seal was recommenced and the patient was admitted to the hospital, with further intervention at the discretion of the inpatient clinicians. If radiographic improvement was seen, the tube was removed and the patient discharged.
Continue to: In contrast...
In contrast, conservative management entailed patient observation for at least 4 hours followed by a repeat chest x-ray. If after the observation period, patients were walking comfortably and without supplemental oxygen, they were discharged. Patients in the observation group underwent an intervention if they met a variety of criteria, including unstable vitals or an enlarging pneumothorax. All patients received standard care with analgesia and supplemental oxygen as needed.
A total of 316 patients were randomized, with 154 assigned to the intervention group and 162 to the observation group. The mean age for all participants was 26. Most patients were male (84.4% in the intervention group and 87.7% in the observation group) and almost half were current smokers (49.3% in the intervention and 42.5% in the observation group). The mean body mass index of participants was 21.4 in the intervention and 21.3 in the observation group. Twenty-five patients (15%) in the observation group underwent interventions for reasons specified in the research protocol (eg, “significant symptoms” such as abnormal physiologic observations and intolerable symptoms, or patient unwillingness to continue in the assigned group), and 10 patients assigned to the intervention group declined treatment.
Using a complete-case analysis, 129 of 131 patients (98.5%) in the intervention group and 118 of 125 patients (94.4%) in the observation group met the primary outcome of radiographic resolution within 8 weeks (risk difference [RD] = –4.1%; 95% CI, –8.6 to 0.5), thereby falling within the prespecified margin for noninferiority of less than 9%.
Per-protocol analysis at 8 weeks also proved observational management noninferior, with 124 of 126 patients (98.4%) in the intervention group and 123 of 130 patients (94.6%) in the observation group achieving lung reexpansion within 8 weeks (RD = –3.8%; 95% CI, –8.3 to 0.7). The time to symptom resolution was similar between groups, with a median time of 15.5 days in the intervention group compared with 14 days in the observation group (hazard ratio = 1.11; 95% CI, 0.88-1.4). A lower risk of serious adverse events (relative risk [RR] = 3.3; 95% CI, 1.37-8.1) and pneumothorax recurrence (absolute RD = 8%; 95% CI, 0.5-15.4) occurred in the observation group vs the intervention group. The average length of hospital stay for patients in the intervention group was 6.1 days, vs 1.6 days in the observation group (RR = 2.8; 95% CI, 1.8-3.6).
Two additional sensitivity analyses were performed because multiple study participants were lost to follow-up or had data collected after 8 weeks. Noninferiority was maintained when data collected after the 8-week visit were included and extended to 63 days (RD = –3.7%: 95% CI, –7.9 to 0.6). However, noninferiority was lost when missing data after 8 weeks were deemed “treatment failure” (RD = –11%; 95% CI, –18.4 to –3.5).
Continue to: WHAT'S NEW
WHAT’S NEW
Conservative management enabled most patients to avoid invasive Tx risks
In this specific patient population, conservative management of primary spontaneous pneumothorax was noninferior to interventional management and had a lower risk of serious adverse events. This management practice spared 85% of the patients from invasive intervention. As a result, they experienced a shortened hospital stay, fewer days missed from school or work, less exposure to radiation from repeat chest x-rays, and a lower rate of adverse events. Additionally, fewer of these patients had early pneumothorax recurrence.
CAVEATS
There were limitations in the trial’s original statistical design
This study had a specific follow-up timetable, and some of the participants were not examined until after the 8-week checkpoint or were lost to follow-up entirely. The authors attempted to address these limitations (and show transparency) by providing additional sensitivity analyses as well as providing the intention-to-treat and per-protocol analyses for the primary outcome at 8 weeks. Noninferiority was maintained in all analyses except for the sensitivity analysis that treated missing data as treatment failure. Therefore, the authors note these approaches result in “statistical fragility” and are exploratory.
CHALLENGES TO IMPLEMENTATION
Pneumothorax is not commonly seen in outpatient settings
Family physicians working in outpatient settings generally do not encounter pneumothorax and, using current guidelines, would refer for emergency or inpatient care. This study opens the possibility of managing selected patients in an outpatient setting; however, this would require at least a 4-hour period of observation, which may be impractical for many outpatient-based physicians. Additionally, the study uses the Collins method to define moderate-to-large pneumothorax, which is likely an uncommon practice and thus not applicable in most primary care settings.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Brown SGA, Ball EL, Perrin K, et al; PSP Investigators. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405-415. doi: 10.1056/NEJMoa1910775
2. Hallifax RJ, Goldacre R, Landray MJ, et al. Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968-2016. JAMA. 2018;320:1471-1480. doi: 10.1001/jama.2018.14299
3. Melton LJ III, Hepper NGG, Offord KP. Incidence of spontaneous pneumothorax in Olmstead County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979;120:1379-1382. doi: 10.1164/arrd.1979.120.6.1379
4. Baumann MH, Strange C, Heffner JE, et al; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119:590-602. doi: 10.1378/chest.119.2.590
5. MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(suppl):ii18-ii31. doi: 10.1136/thx.2010.136986
6. Collins CD, Lopez A, Mathie A, et al. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. Am J Roentgenol. 1995;165:1127-1130. doi: 10.2214/ajr.165.5.7572489
7. Kwiatt M, Tarbox A, Seamon MJ, et al. Thoracostomy tubes: a comprehensive review of complications and related topics. Int J Crit Illn Inj Sci. 2014;4:143-155. doi: 10.4103/2229-5151.134182
8. Maskell NA, Medford A, Gleeson FV. Seldinger chest drain insertion: simpler but not necessarily safer. Thorax. 2010;65:5-6. doi: 10.1136/thx.2009.117200
ILLUSTRATIVE CASE
A 26-year-old man presents to the emergency department complaining of sudden-onset left-side chest pain and mild dyspnea that started while he was playing basketball. He denies any medical problems and takes no medications. He is able to speak in complete sentences as he answers your questions. His O2 saturation is 95% and a chest x-ray reveals a left-side, moderate-to-large pneumothorax.
A primary spontaneous pneumothorax is one that occurs in the absence of underlying clinical lung disease and is not associated with an inciting cause, such as a rib fracture.2 In the United States, the estimated incidence of primary spontaneous pneumothorax is 7.4 cases per 100,000 men and 1.2 cases per 100,000 women.3 The etiology is often unknown, but it is associated with several risk factors, including male sex, smoking, and a tall, thin body habitus.2
The management strategy for stable patients with a primary spontaneous pneumothorax largely depends on pneumothorax size and institutional practice. Multiple methods define pneumothorax size; the US standard cutoff for a small or large pneumothorax is 3 cm, between the pleural line and chest wall at the level of the apex,4 compared with 2 cm in Europe, when evaluating the distance at the hilum in an upright chest radiograph.5 The Collins method uses a formula to calculate the percentage of lung area affected based on 3 distinct measurements on a posterior/anterior upright chest radiograph.6
Management options include observation, supplemental oxygen, simple aspiration, and thoracostomy or chest tube placement. British Thoracic Society guidelines published in 2010 state that only a small pneumothorax can be managed conservatively with observation alone; for a large pneumothorax, the guidelines recommend needle aspiration to achieve lung reinflation, followed by chest tube placement if unsuccessful.5
In practice, management of a large primary spontaneous pneumothorax varies, but the most common treatment is chest tube placement.7 This procedure can be painful and may result in complications such as bleeding, infection, injury to internal structures, or the need for surgical intervention.7 In addition, once a chest tube is placed, hospital admission ensues, lasting an average of 4 days.8 Given these consequences, there is a need for safe and feasible treatment options for a large primary spontaneous pneumothorax.
STUDY SUMMARY
Observational management judged noninferior, with multiple advantages
The Primary Spontaneous Pneumothorax (PSP) trial was a prospective noninferiority trial conducted at 39 hospitals in Australia and New Zealand. This randomized controlled trial compared observational (“watch and wait”) vs interventional (chest tube placement) management of uncomplicated, unilateral, primary spontaneous pneumothorax. Patients ages 14 to 50 years with a moderate-to-large pneumothorax—32% or greater, as defined by the Collins method4—were randomly assigned to a study group to examine the primary outcome of lung reexpansion at 8 weeks.
The intervention included chest tube insertion attached to an underwater seal without suction for 1 hour, followed by an x-ray and clamping for 4 hours if there was no air leak, followed by a repeat chest x-ray. If there was no evidence of radiographic resolution, or if during observation the pneumothorax recurred, the underwater seal was recommenced and the patient was admitted to the hospital, with further intervention at the discretion of the inpatient clinicians. If radiographic improvement was seen, the tube was removed and the patient discharged.
Continue to: In contrast...
In contrast, conservative management entailed patient observation for at least 4 hours followed by a repeat chest x-ray. If after the observation period, patients were walking comfortably and without supplemental oxygen, they were discharged. Patients in the observation group underwent an intervention if they met a variety of criteria, including unstable vitals or an enlarging pneumothorax. All patients received standard care with analgesia and supplemental oxygen as needed.
A total of 316 patients were randomized, with 154 assigned to the intervention group and 162 to the observation group. The mean age for all participants was 26. Most patients were male (84.4% in the intervention group and 87.7% in the observation group) and almost half were current smokers (49.3% in the intervention and 42.5% in the observation group). The mean body mass index of participants was 21.4 in the intervention and 21.3 in the observation group. Twenty-five patients (15%) in the observation group underwent interventions for reasons specified in the research protocol (eg, “significant symptoms” such as abnormal physiologic observations and intolerable symptoms, or patient unwillingness to continue in the assigned group), and 10 patients assigned to the intervention group declined treatment.
Using a complete-case analysis, 129 of 131 patients (98.5%) in the intervention group and 118 of 125 patients (94.4%) in the observation group met the primary outcome of radiographic resolution within 8 weeks (risk difference [RD] = –4.1%; 95% CI, –8.6 to 0.5), thereby falling within the prespecified margin for noninferiority of less than 9%.
Per-protocol analysis at 8 weeks also proved observational management noninferior, with 124 of 126 patients (98.4%) in the intervention group and 123 of 130 patients (94.6%) in the observation group achieving lung reexpansion within 8 weeks (RD = –3.8%; 95% CI, –8.3 to 0.7). The time to symptom resolution was similar between groups, with a median time of 15.5 days in the intervention group compared with 14 days in the observation group (hazard ratio = 1.11; 95% CI, 0.88-1.4). A lower risk of serious adverse events (relative risk [RR] = 3.3; 95% CI, 1.37-8.1) and pneumothorax recurrence (absolute RD = 8%; 95% CI, 0.5-15.4) occurred in the observation group vs the intervention group. The average length of hospital stay for patients in the intervention group was 6.1 days, vs 1.6 days in the observation group (RR = 2.8; 95% CI, 1.8-3.6).
Two additional sensitivity analyses were performed because multiple study participants were lost to follow-up or had data collected after 8 weeks. Noninferiority was maintained when data collected after the 8-week visit were included and extended to 63 days (RD = –3.7%: 95% CI, –7.9 to 0.6). However, noninferiority was lost when missing data after 8 weeks were deemed “treatment failure” (RD = –11%; 95% CI, –18.4 to –3.5).
Continue to: WHAT'S NEW
WHAT’S NEW
Conservative management enabled most patients to avoid invasive Tx risks
In this specific patient population, conservative management of primary spontaneous pneumothorax was noninferior to interventional management and had a lower risk of serious adverse events. This management practice spared 85% of the patients from invasive intervention. As a result, they experienced a shortened hospital stay, fewer days missed from school or work, less exposure to radiation from repeat chest x-rays, and a lower rate of adverse events. Additionally, fewer of these patients had early pneumothorax recurrence.
CAVEATS
There were limitations in the trial’s original statistical design
This study had a specific follow-up timetable, and some of the participants were not examined until after the 8-week checkpoint or were lost to follow-up entirely. The authors attempted to address these limitations (and show transparency) by providing additional sensitivity analyses as well as providing the intention-to-treat and per-protocol analyses for the primary outcome at 8 weeks. Noninferiority was maintained in all analyses except for the sensitivity analysis that treated missing data as treatment failure. Therefore, the authors note these approaches result in “statistical fragility” and are exploratory.
CHALLENGES TO IMPLEMENTATION
Pneumothorax is not commonly seen in outpatient settings
Family physicians working in outpatient settings generally do not encounter pneumothorax and, using current guidelines, would refer for emergency or inpatient care. This study opens the possibility of managing selected patients in an outpatient setting; however, this would require at least a 4-hour period of observation, which may be impractical for many outpatient-based physicians. Additionally, the study uses the Collins method to define moderate-to-large pneumothorax, which is likely an uncommon practice and thus not applicable in most primary care settings.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 26-year-old man presents to the emergency department complaining of sudden-onset left-side chest pain and mild dyspnea that started while he was playing basketball. He denies any medical problems and takes no medications. He is able to speak in complete sentences as he answers your questions. His O2 saturation is 95% and a chest x-ray reveals a left-side, moderate-to-large pneumothorax.
A primary spontaneous pneumothorax is one that occurs in the absence of underlying clinical lung disease and is not associated with an inciting cause, such as a rib fracture.2 In the United States, the estimated incidence of primary spontaneous pneumothorax is 7.4 cases per 100,000 men and 1.2 cases per 100,000 women.3 The etiology is often unknown, but it is associated with several risk factors, including male sex, smoking, and a tall, thin body habitus.2
The management strategy for stable patients with a primary spontaneous pneumothorax largely depends on pneumothorax size and institutional practice. Multiple methods define pneumothorax size; the US standard cutoff for a small or large pneumothorax is 3 cm, between the pleural line and chest wall at the level of the apex,4 compared with 2 cm in Europe, when evaluating the distance at the hilum in an upright chest radiograph.5 The Collins method uses a formula to calculate the percentage of lung area affected based on 3 distinct measurements on a posterior/anterior upright chest radiograph.6
Management options include observation, supplemental oxygen, simple aspiration, and thoracostomy or chest tube placement. British Thoracic Society guidelines published in 2010 state that only a small pneumothorax can be managed conservatively with observation alone; for a large pneumothorax, the guidelines recommend needle aspiration to achieve lung reinflation, followed by chest tube placement if unsuccessful.5
In practice, management of a large primary spontaneous pneumothorax varies, but the most common treatment is chest tube placement.7 This procedure can be painful and may result in complications such as bleeding, infection, injury to internal structures, or the need for surgical intervention.7 In addition, once a chest tube is placed, hospital admission ensues, lasting an average of 4 days.8 Given these consequences, there is a need for safe and feasible treatment options for a large primary spontaneous pneumothorax.
STUDY SUMMARY
Observational management judged noninferior, with multiple advantages
The Primary Spontaneous Pneumothorax (PSP) trial was a prospective noninferiority trial conducted at 39 hospitals in Australia and New Zealand. This randomized controlled trial compared observational (“watch and wait”) vs interventional (chest tube placement) management of uncomplicated, unilateral, primary spontaneous pneumothorax. Patients ages 14 to 50 years with a moderate-to-large pneumothorax—32% or greater, as defined by the Collins method4—were randomly assigned to a study group to examine the primary outcome of lung reexpansion at 8 weeks.
The intervention included chest tube insertion attached to an underwater seal without suction for 1 hour, followed by an x-ray and clamping for 4 hours if there was no air leak, followed by a repeat chest x-ray. If there was no evidence of radiographic resolution, or if during observation the pneumothorax recurred, the underwater seal was recommenced and the patient was admitted to the hospital, with further intervention at the discretion of the inpatient clinicians. If radiographic improvement was seen, the tube was removed and the patient discharged.
Continue to: In contrast...
In contrast, conservative management entailed patient observation for at least 4 hours followed by a repeat chest x-ray. If after the observation period, patients were walking comfortably and without supplemental oxygen, they were discharged. Patients in the observation group underwent an intervention if they met a variety of criteria, including unstable vitals or an enlarging pneumothorax. All patients received standard care with analgesia and supplemental oxygen as needed.
A total of 316 patients were randomized, with 154 assigned to the intervention group and 162 to the observation group. The mean age for all participants was 26. Most patients were male (84.4% in the intervention group and 87.7% in the observation group) and almost half were current smokers (49.3% in the intervention and 42.5% in the observation group). The mean body mass index of participants was 21.4 in the intervention and 21.3 in the observation group. Twenty-five patients (15%) in the observation group underwent interventions for reasons specified in the research protocol (eg, “significant symptoms” such as abnormal physiologic observations and intolerable symptoms, or patient unwillingness to continue in the assigned group), and 10 patients assigned to the intervention group declined treatment.
Using a complete-case analysis, 129 of 131 patients (98.5%) in the intervention group and 118 of 125 patients (94.4%) in the observation group met the primary outcome of radiographic resolution within 8 weeks (risk difference [RD] = –4.1%; 95% CI, –8.6 to 0.5), thereby falling within the prespecified margin for noninferiority of less than 9%.
Per-protocol analysis at 8 weeks also proved observational management noninferior, with 124 of 126 patients (98.4%) in the intervention group and 123 of 130 patients (94.6%) in the observation group achieving lung reexpansion within 8 weeks (RD = –3.8%; 95% CI, –8.3 to 0.7). The time to symptom resolution was similar between groups, with a median time of 15.5 days in the intervention group compared with 14 days in the observation group (hazard ratio = 1.11; 95% CI, 0.88-1.4). A lower risk of serious adverse events (relative risk [RR] = 3.3; 95% CI, 1.37-8.1) and pneumothorax recurrence (absolute RD = 8%; 95% CI, 0.5-15.4) occurred in the observation group vs the intervention group. The average length of hospital stay for patients in the intervention group was 6.1 days, vs 1.6 days in the observation group (RR = 2.8; 95% CI, 1.8-3.6).
Two additional sensitivity analyses were performed because multiple study participants were lost to follow-up or had data collected after 8 weeks. Noninferiority was maintained when data collected after the 8-week visit were included and extended to 63 days (RD = –3.7%: 95% CI, –7.9 to 0.6). However, noninferiority was lost when missing data after 8 weeks were deemed “treatment failure” (RD = –11%; 95% CI, –18.4 to –3.5).
Continue to: WHAT'S NEW
WHAT’S NEW
Conservative management enabled most patients to avoid invasive Tx risks
In this specific patient population, conservative management of primary spontaneous pneumothorax was noninferior to interventional management and had a lower risk of serious adverse events. This management practice spared 85% of the patients from invasive intervention. As a result, they experienced a shortened hospital stay, fewer days missed from school or work, less exposure to radiation from repeat chest x-rays, and a lower rate of adverse events. Additionally, fewer of these patients had early pneumothorax recurrence.
CAVEATS
There were limitations in the trial’s original statistical design
This study had a specific follow-up timetable, and some of the participants were not examined until after the 8-week checkpoint or were lost to follow-up entirely. The authors attempted to address these limitations (and show transparency) by providing additional sensitivity analyses as well as providing the intention-to-treat and per-protocol analyses for the primary outcome at 8 weeks. Noninferiority was maintained in all analyses except for the sensitivity analysis that treated missing data as treatment failure. Therefore, the authors note these approaches result in “statistical fragility” and are exploratory.
CHALLENGES TO IMPLEMENTATION
Pneumothorax is not commonly seen in outpatient settings
Family physicians working in outpatient settings generally do not encounter pneumothorax and, using current guidelines, would refer for emergency or inpatient care. This study opens the possibility of managing selected patients in an outpatient setting; however, this would require at least a 4-hour period of observation, which may be impractical for many outpatient-based physicians. Additionally, the study uses the Collins method to define moderate-to-large pneumothorax, which is likely an uncommon practice and thus not applicable in most primary care settings.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Brown SGA, Ball EL, Perrin K, et al; PSP Investigators. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405-415. doi: 10.1056/NEJMoa1910775
2. Hallifax RJ, Goldacre R, Landray MJ, et al. Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968-2016. JAMA. 2018;320:1471-1480. doi: 10.1001/jama.2018.14299
3. Melton LJ III, Hepper NGG, Offord KP. Incidence of spontaneous pneumothorax in Olmstead County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979;120:1379-1382. doi: 10.1164/arrd.1979.120.6.1379
4. Baumann MH, Strange C, Heffner JE, et al; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119:590-602. doi: 10.1378/chest.119.2.590
5. MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(suppl):ii18-ii31. doi: 10.1136/thx.2010.136986
6. Collins CD, Lopez A, Mathie A, et al. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. Am J Roentgenol. 1995;165:1127-1130. doi: 10.2214/ajr.165.5.7572489
7. Kwiatt M, Tarbox A, Seamon MJ, et al. Thoracostomy tubes: a comprehensive review of complications and related topics. Int J Crit Illn Inj Sci. 2014;4:143-155. doi: 10.4103/2229-5151.134182
8. Maskell NA, Medford A, Gleeson FV. Seldinger chest drain insertion: simpler but not necessarily safer. Thorax. 2010;65:5-6. doi: 10.1136/thx.2009.117200
1. Brown SGA, Ball EL, Perrin K, et al; PSP Investigators. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405-415. doi: 10.1056/NEJMoa1910775
2. Hallifax RJ, Goldacre R, Landray MJ, et al. Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968-2016. JAMA. 2018;320:1471-1480. doi: 10.1001/jama.2018.14299
3. Melton LJ III, Hepper NGG, Offord KP. Incidence of spontaneous pneumothorax in Olmstead County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979;120:1379-1382. doi: 10.1164/arrd.1979.120.6.1379
4. Baumann MH, Strange C, Heffner JE, et al; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119:590-602. doi: 10.1378/chest.119.2.590
5. MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(suppl):ii18-ii31. doi: 10.1136/thx.2010.136986
6. Collins CD, Lopez A, Mathie A, et al. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. Am J Roentgenol. 1995;165:1127-1130. doi: 10.2214/ajr.165.5.7572489
7. Kwiatt M, Tarbox A, Seamon MJ, et al. Thoracostomy tubes: a comprehensive review of complications and related topics. Int J Crit Illn Inj Sci. 2014;4:143-155. doi: 10.4103/2229-5151.134182
8. Maskell NA, Medford A, Gleeson FV. Seldinger chest drain insertion: simpler but not necessarily safer. Thorax. 2010;65:5-6. doi: 10.1136/thx.2009.117200
PRACTICE CHANGER
Consider observation rather than chest tube placement for primary, uncomplicated, unilateral moderate-to-large spontaneous pneumothorax in patients ages 14 to 50.
STRENGTH OF RECOMMENDATION
B: Based on a single, lower-quality randomized controlled trial1
Brown SGA, Ball EL, Perrin K, et al; PSP Investigators. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405-415. doi: 10.1056/NEJMoa1910775
Can extended anticoagulation prophylaxis after discharge prevent thromboembolism?
ILLUSTRATIVE CASE
A 67-year-old man with a history of type 2 diabetes, hypertension, and chronic congestive heart failure (ejection fraction = 30%) was admitted to the intensive care unit with a diagnosis of acute hypoxic respiratory failure. He was discharged after 10 days of inpatient treatment that included daily VTE prophylaxis with low-molecular-weight heparin (LMWH). Should he go home on VTE prophylaxis?
Patients hospitalized with nonsurgical conditions such as congestive heart failure, chronic obstructive pulmonary disease, sepsis, inflammatory bowel disease, or active cancers are at increased risk for VTE due to inflammation and immobility. In a US study of 158,325 hospitalized nonsurgical patients, including those with cancer, infections, congestive heart failure, or respiratory failure, 4% of patients developed
However, use of DOACs for short-term VTE prophylaxis as an alternative to LMWH in hospitalized patients is supported by a meta-analysis showing equivalent efficacy, safety, and cost-effectiveness.1 The current study examined DOACs for extended postdischarge use.1
STUDY SUMMARY
Significant benefit of DOACs demonstrated across 4 large trials
This meta-analysis of 4 large randomized controlled trials examined the safety and efficacy of 6 weeks of postdischarge DOAC thromboprophylaxis compared with placebo in 26,408 high-risk nonsurgical hospitalized patients.1 Patients at least 40 years old were admitted with diagnoses that included New York Heart Association (NYHA) class III or IV congestive heart failure, active cancer, acute ischemic stroke, acute respiratory failure, or infectious or inflammatory disease. Study patients also had risk factors for VTE, including age 75 and older, obesity, chronic venous insufficiency, history of VTE, history of NYHA class III or IV congestive heart failure, history of cancer, thrombophilia, hormone replacement therapy, or major surgery within the 6 to 12 weeks before current medical hospitalization.
Patients were excluded if DOACs were contraindicated or if they had active or recent bleeding, renal failure, abnormal liver values, an upcoming need for surgery, or an indication for ongoing anticoagulation. Patients in 3 studies received 6 to 10 days of enoxaparin as prophylaxis during their inpatient stay. (The fourth study did not specify length of inpatient prophylaxis or drug used.) After discharge, patients were assigned to placebo or a regimen of rivaroxaban 10 mg daily, apixaban 2.5 mg twice daily, or betrixaban 80 mg daily for a range of 30 to 45 days. The primary outcome was the composite of total VTE and VTE-related death. A secondary outcome was the occurrence of nonfatal symptomatic VTE, and the primary safety outcome was the incidence of major bleeding.
The primary outcome occurred in 2.9% of the patients in the DOAC group compared with 3.6% of patients in the placebo group (odds ratio [OR] = 0.79; 95% CI, 0.69-0.91; number needed to treat [NNT] = 143). The secondary outcome occurred in 0.48% of patients in the DOAC group compared with 0.77% of patients in the placebo group (OR = 0.62; 95% CI, 0.47-0.83; NNT = 345). Major bleeding resulting in a decrease in hemoglobin concentration of more than 2 g/L, requiring transfusion of at least 2 units of packed red blood cells, reintervention at a previous surgical site, or bleeding in a critical organ or that was fatal, occurred in 0.58% of patients in the DOAC group compared with 0.3% of patients in the placebo group (OR = 1.9; 95% CI, 1.4-2.7; number needed to harm [NNH] = 357). Nonmajor bleeding was increased in the DOAC group compared with placebo (2.2% vs 1.2%; OR = 1.8; 95% CI, 1.5-2.1; NNH = 110).
The NNT to prevent a fatal VTE was 899 patients
Continue to: WHAT'S NEW
WHAT’S NEW
Mortality and morbidity benefit with small bleeding risk
Based on this study, for every 300 high-risk patients hospitalized with nonsurgical diagnoses who are given 6 weeks of DOAC prophylaxis, there will be 2 fewer cases of VTE and VTE-related death. In this same group of patients, there will be approximately 1 major bleeding event and 3 less serious bleeds.
Patients with preexisting medical conditions such as congestive heart failure, cancer, and sepsis and those admitted to an intensive care unit are at increased risk for DVT after discharge.5 Extending DOAC prophylaxis in nonsurgical patients with serious medical conditions for 6 weeks after discharge reduces the risk of VTE or VTE-related death by 0.7% compared with placebo. Treatment in this population does incur a small increased risk of major bleeding by 0.3% in the DOAC group compared with placebo.
CAVEATS
Results cannot be generalized to all patient populations
Many high-risk patients have chronic kidney disease, and because DOACs (including apixaban, rivaroxaban, and dabigatran) are renally cleared, there are limited data to establish their safety in patients with creatinine clearance ≤ 30 mL/min. Benefits seen with DOACs cannot be extrapolated to other anticoagulation agents, including warfarin or LMWH.
In accordance with new guidelines, some of the patients in this study would now receive antiplatelet therapy, eg, poststroke patients, cancer patients, and—with the ease of DOAC use—patients with atrial fibrillation. If these patients were excluded, it is not known whether the benefit would remain. Patients included in these trials were at particularly high risk for VTE, and the benefits seen in this study cannot be generalized to a patient population with fewer VTE risk factors.
CHALLENGES TO IMPLEMENTATION
High cost and lack of updated guidelines may limit DOAC thromboprophylaxis
Cost is a concern. All the new DOACs are expensive; for example, rivaroxaban costs a little less than $500 per month.6 Obtaining insurance coverage for a novel indication may be challenging. The American Society of Hematology and others have not yet endorsed extended posthospital thromboprophylaxis in nonsurgical patients, although the use of DOACs has expanded since the last guideline revisions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Bhalla V, Lamping OF, Abdel-Latif A, et al. Contemporary meta-analysis of extended direct-acting oral anticoagulant thromboprophylaxis to prevent venous thromboembolism. Am J Med. 2020;133:1074-1081.e8. doi: 10.1016/j.amjmed.2020.01.037
2. Spyropoulos AC, Hussein M, Lin J, et al. Rates of venous thromboembolism occurrence in medical patients among the insured population. Thromb Haemost. 2009;102:951-957. doi: 10.1160/TH09-02-0073
3. Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(suppl):e195S-226S. doi: 10.1378/chest.11-2296
4. Schünemann HJ, Cushman M, Burnett AE, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018;2:3198-3225. doi: 10.1182/bloodadvances.2018022954
5. White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(suppl):I-4-I-8. doi: 10.1161/01.CIR.0000078468.11849.66
6. Rivaroxaban . GoodRx. Accessed August 10, 2021. www.goodrx.com/rivaroxaban
ILLUSTRATIVE CASE
A 67-year-old man with a history of type 2 diabetes, hypertension, and chronic congestive heart failure (ejection fraction = 30%) was admitted to the intensive care unit with a diagnosis of acute hypoxic respiratory failure. He was discharged after 10 days of inpatient treatment that included daily VTE prophylaxis with low-molecular-weight heparin (LMWH). Should he go home on VTE prophylaxis?
Patients hospitalized with nonsurgical conditions such as congestive heart failure, chronic obstructive pulmonary disease, sepsis, inflammatory bowel disease, or active cancers are at increased risk for VTE due to inflammation and immobility. In a US study of 158,325 hospitalized nonsurgical patients, including those with cancer, infections, congestive heart failure, or respiratory failure, 4% of patients developed
However, use of DOACs for short-term VTE prophylaxis as an alternative to LMWH in hospitalized patients is supported by a meta-analysis showing equivalent efficacy, safety, and cost-effectiveness.1 The current study examined DOACs for extended postdischarge use.1
STUDY SUMMARY
Significant benefit of DOACs demonstrated across 4 large trials
This meta-analysis of 4 large randomized controlled trials examined the safety and efficacy of 6 weeks of postdischarge DOAC thromboprophylaxis compared with placebo in 26,408 high-risk nonsurgical hospitalized patients.1 Patients at least 40 years old were admitted with diagnoses that included New York Heart Association (NYHA) class III or IV congestive heart failure, active cancer, acute ischemic stroke, acute respiratory failure, or infectious or inflammatory disease. Study patients also had risk factors for VTE, including age 75 and older, obesity, chronic venous insufficiency, history of VTE, history of NYHA class III or IV congestive heart failure, history of cancer, thrombophilia, hormone replacement therapy, or major surgery within the 6 to 12 weeks before current medical hospitalization.
Patients were excluded if DOACs were contraindicated or if they had active or recent bleeding, renal failure, abnormal liver values, an upcoming need for surgery, or an indication for ongoing anticoagulation. Patients in 3 studies received 6 to 10 days of enoxaparin as prophylaxis during their inpatient stay. (The fourth study did not specify length of inpatient prophylaxis or drug used.) After discharge, patients were assigned to placebo or a regimen of rivaroxaban 10 mg daily, apixaban 2.5 mg twice daily, or betrixaban 80 mg daily for a range of 30 to 45 days. The primary outcome was the composite of total VTE and VTE-related death. A secondary outcome was the occurrence of nonfatal symptomatic VTE, and the primary safety outcome was the incidence of major bleeding.
The primary outcome occurred in 2.9% of the patients in the DOAC group compared with 3.6% of patients in the placebo group (odds ratio [OR] = 0.79; 95% CI, 0.69-0.91; number needed to treat [NNT] = 143). The secondary outcome occurred in 0.48% of patients in the DOAC group compared with 0.77% of patients in the placebo group (OR = 0.62; 95% CI, 0.47-0.83; NNT = 345). Major bleeding resulting in a decrease in hemoglobin concentration of more than 2 g/L, requiring transfusion of at least 2 units of packed red blood cells, reintervention at a previous surgical site, or bleeding in a critical organ or that was fatal, occurred in 0.58% of patients in the DOAC group compared with 0.3% of patients in the placebo group (OR = 1.9; 95% CI, 1.4-2.7; number needed to harm [NNH] = 357). Nonmajor bleeding was increased in the DOAC group compared with placebo (2.2% vs 1.2%; OR = 1.8; 95% CI, 1.5-2.1; NNH = 110).
The NNT to prevent a fatal VTE was 899 patients
Continue to: WHAT'S NEW
WHAT’S NEW
Mortality and morbidity benefit with small bleeding risk
Based on this study, for every 300 high-risk patients hospitalized with nonsurgical diagnoses who are given 6 weeks of DOAC prophylaxis, there will be 2 fewer cases of VTE and VTE-related death. In this same group of patients, there will be approximately 1 major bleeding event and 3 less serious bleeds.
Patients with preexisting medical conditions such as congestive heart failure, cancer, and sepsis and those admitted to an intensive care unit are at increased risk for DVT after discharge.5 Extending DOAC prophylaxis in nonsurgical patients with serious medical conditions for 6 weeks after discharge reduces the risk of VTE or VTE-related death by 0.7% compared with placebo. Treatment in this population does incur a small increased risk of major bleeding by 0.3% in the DOAC group compared with placebo.
CAVEATS
Results cannot be generalized to all patient populations
Many high-risk patients have chronic kidney disease, and because DOACs (including apixaban, rivaroxaban, and dabigatran) are renally cleared, there are limited data to establish their safety in patients with creatinine clearance ≤ 30 mL/min. Benefits seen with DOACs cannot be extrapolated to other anticoagulation agents, including warfarin or LMWH.
In accordance with new guidelines, some of the patients in this study would now receive antiplatelet therapy, eg, poststroke patients, cancer patients, and—with the ease of DOAC use—patients with atrial fibrillation. If these patients were excluded, it is not known whether the benefit would remain. Patients included in these trials were at particularly high risk for VTE, and the benefits seen in this study cannot be generalized to a patient population with fewer VTE risk factors.
CHALLENGES TO IMPLEMENTATION
High cost and lack of updated guidelines may limit DOAC thromboprophylaxis
Cost is a concern. All the new DOACs are expensive; for example, rivaroxaban costs a little less than $500 per month.6 Obtaining insurance coverage for a novel indication may be challenging. The American Society of Hematology and others have not yet endorsed extended posthospital thromboprophylaxis in nonsurgical patients, although the use of DOACs has expanded since the last guideline revisions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 67-year-old man with a history of type 2 diabetes, hypertension, and chronic congestive heart failure (ejection fraction = 30%) was admitted to the intensive care unit with a diagnosis of acute hypoxic respiratory failure. He was discharged after 10 days of inpatient treatment that included daily VTE prophylaxis with low-molecular-weight heparin (LMWH). Should he go home on VTE prophylaxis?
Patients hospitalized with nonsurgical conditions such as congestive heart failure, chronic obstructive pulmonary disease, sepsis, inflammatory bowel disease, or active cancers are at increased risk for VTE due to inflammation and immobility. In a US study of 158,325 hospitalized nonsurgical patients, including those with cancer, infections, congestive heart failure, or respiratory failure, 4% of patients developed
However, use of DOACs for short-term VTE prophylaxis as an alternative to LMWH in hospitalized patients is supported by a meta-analysis showing equivalent efficacy, safety, and cost-effectiveness.1 The current study examined DOACs for extended postdischarge use.1
STUDY SUMMARY
Significant benefit of DOACs demonstrated across 4 large trials
This meta-analysis of 4 large randomized controlled trials examined the safety and efficacy of 6 weeks of postdischarge DOAC thromboprophylaxis compared with placebo in 26,408 high-risk nonsurgical hospitalized patients.1 Patients at least 40 years old were admitted with diagnoses that included New York Heart Association (NYHA) class III or IV congestive heart failure, active cancer, acute ischemic stroke, acute respiratory failure, or infectious or inflammatory disease. Study patients also had risk factors for VTE, including age 75 and older, obesity, chronic venous insufficiency, history of VTE, history of NYHA class III or IV congestive heart failure, history of cancer, thrombophilia, hormone replacement therapy, or major surgery within the 6 to 12 weeks before current medical hospitalization.
Patients were excluded if DOACs were contraindicated or if they had active or recent bleeding, renal failure, abnormal liver values, an upcoming need for surgery, or an indication for ongoing anticoagulation. Patients in 3 studies received 6 to 10 days of enoxaparin as prophylaxis during their inpatient stay. (The fourth study did not specify length of inpatient prophylaxis or drug used.) After discharge, patients were assigned to placebo or a regimen of rivaroxaban 10 mg daily, apixaban 2.5 mg twice daily, or betrixaban 80 mg daily for a range of 30 to 45 days. The primary outcome was the composite of total VTE and VTE-related death. A secondary outcome was the occurrence of nonfatal symptomatic VTE, and the primary safety outcome was the incidence of major bleeding.
The primary outcome occurred in 2.9% of the patients in the DOAC group compared with 3.6% of patients in the placebo group (odds ratio [OR] = 0.79; 95% CI, 0.69-0.91; number needed to treat [NNT] = 143). The secondary outcome occurred in 0.48% of patients in the DOAC group compared with 0.77% of patients in the placebo group (OR = 0.62; 95% CI, 0.47-0.83; NNT = 345). Major bleeding resulting in a decrease in hemoglobin concentration of more than 2 g/L, requiring transfusion of at least 2 units of packed red blood cells, reintervention at a previous surgical site, or bleeding in a critical organ or that was fatal, occurred in 0.58% of patients in the DOAC group compared with 0.3% of patients in the placebo group (OR = 1.9; 95% CI, 1.4-2.7; number needed to harm [NNH] = 357). Nonmajor bleeding was increased in the DOAC group compared with placebo (2.2% vs 1.2%; OR = 1.8; 95% CI, 1.5-2.1; NNH = 110).
The NNT to prevent a fatal VTE was 899 patients
Continue to: WHAT'S NEW
WHAT’S NEW
Mortality and morbidity benefit with small bleeding risk
Based on this study, for every 300 high-risk patients hospitalized with nonsurgical diagnoses who are given 6 weeks of DOAC prophylaxis, there will be 2 fewer cases of VTE and VTE-related death. In this same group of patients, there will be approximately 1 major bleeding event and 3 less serious bleeds.
Patients with preexisting medical conditions such as congestive heart failure, cancer, and sepsis and those admitted to an intensive care unit are at increased risk for DVT after discharge.5 Extending DOAC prophylaxis in nonsurgical patients with serious medical conditions for 6 weeks after discharge reduces the risk of VTE or VTE-related death by 0.7% compared with placebo. Treatment in this population does incur a small increased risk of major bleeding by 0.3% in the DOAC group compared with placebo.
CAVEATS
Results cannot be generalized to all patient populations
Many high-risk patients have chronic kidney disease, and because DOACs (including apixaban, rivaroxaban, and dabigatran) are renally cleared, there are limited data to establish their safety in patients with creatinine clearance ≤ 30 mL/min. Benefits seen with DOACs cannot be extrapolated to other anticoagulation agents, including warfarin or LMWH.
In accordance with new guidelines, some of the patients in this study would now receive antiplatelet therapy, eg, poststroke patients, cancer patients, and—with the ease of DOAC use—patients with atrial fibrillation. If these patients were excluded, it is not known whether the benefit would remain. Patients included in these trials were at particularly high risk for VTE, and the benefits seen in this study cannot be generalized to a patient population with fewer VTE risk factors.
CHALLENGES TO IMPLEMENTATION
High cost and lack of updated guidelines may limit DOAC thromboprophylaxis
Cost is a concern. All the new DOACs are expensive; for example, rivaroxaban costs a little less than $500 per month.6 Obtaining insurance coverage for a novel indication may be challenging. The American Society of Hematology and others have not yet endorsed extended posthospital thromboprophylaxis in nonsurgical patients, although the use of DOACs has expanded since the last guideline revisions.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Bhalla V, Lamping OF, Abdel-Latif A, et al. Contemporary meta-analysis of extended direct-acting oral anticoagulant thromboprophylaxis to prevent venous thromboembolism. Am J Med. 2020;133:1074-1081.e8. doi: 10.1016/j.amjmed.2020.01.037
2. Spyropoulos AC, Hussein M, Lin J, et al. Rates of venous thromboembolism occurrence in medical patients among the insured population. Thromb Haemost. 2009;102:951-957. doi: 10.1160/TH09-02-0073
3. Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(suppl):e195S-226S. doi: 10.1378/chest.11-2296
4. Schünemann HJ, Cushman M, Burnett AE, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018;2:3198-3225. doi: 10.1182/bloodadvances.2018022954
5. White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(suppl):I-4-I-8. doi: 10.1161/01.CIR.0000078468.11849.66
6. Rivaroxaban . GoodRx. Accessed August 10, 2021. www.goodrx.com/rivaroxaban
1. Bhalla V, Lamping OF, Abdel-Latif A, et al. Contemporary meta-analysis of extended direct-acting oral anticoagulant thromboprophylaxis to prevent venous thromboembolism. Am J Med. 2020;133:1074-1081.e8. doi: 10.1016/j.amjmed.2020.01.037
2. Spyropoulos AC, Hussein M, Lin J, et al. Rates of venous thromboembolism occurrence in medical patients among the insured population. Thromb Haemost. 2009;102:951-957. doi: 10.1160/TH09-02-0073
3. Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(suppl):e195S-226S. doi: 10.1378/chest.11-2296
4. Schünemann HJ, Cushman M, Burnett AE, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018;2:3198-3225. doi: 10.1182/bloodadvances.2018022954
5. White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(suppl):I-4-I-8. doi: 10.1161/01.CIR.0000078468.11849.66
6. Rivaroxaban . GoodRx. Accessed August 10, 2021. www.goodrx.com/rivaroxaban
PRACTICE CHANGER
Treat seriously ill patients with a
STRENGTH OF RECOMMENDATION
A: Meta-analysis of randomized clinical trials1
Bhalla V, Lamping OF, Abdel-Latif A, et al. Contemporary meta-analysis of extended direct-acting oral anticoagulant thromboprophylaxis to prevent venous thromboembolism. Am J Med. 2020;133:1074-1081.e8. doi: 10.1016/j.amjmed.2020.01.037