User login
A transgender adolescent with chronic pain, depression, and PTSD
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
Resilience: Our only remedy?
Resilience is like patience; we all wish we had more of it, but we hope to avoid getting it the hard way. This wasn’t really an area of interest for me, until it needed to be. When one academic year brings the suicide of one colleague and the murder of another, resilience becomes the only alternative to despair.
I realize that even though the particular pain or trauma we endured may be unique, it’s becoming increasingly common. The alarming studies of resident depression and suicide are too difficult for us to ignore. Now we must look in that evidence-based mirror and decide where we will go from here, as a profession and as trainees. The 2018 American Psychiatric Association annual meeting gave us a rude awakening that we may not have it figured out. Even during a year-long theme on wellness, and several sessions at the meeting focusing on the same, we all found ourselves mourning the loss of 2 colleagues to suicide that very weekend only a few miles away from the gathering of the world’s experts.
It brought an eerie element to the conversation.
The wellness “window dressing” will not get the job done. I recently had a candid discussion with a mentor in administrative leadership, and his words surprised as well as challenged me. He told me that the “system” will not save you. You must save yourself. I have decided to respectfully reject that. I think everyone should be involved, including the “system” that is entrusted with my training, and the least that it ought to ensure is that I get out alive.
Has that really become too much to ask of our profession?
We must hold our system to a higher standard. More mindfulness and better breathing will surely be helpful—but I hope we can begin to admit that this is not the answer. Unfortunately, the culture of “pay your dues” and “you know how much harder it was when I was a resident?” is still the norm. We now receive our training in an environment where the pressure is extraordinarily high, the margin for error very low, and the possibility of support is almost a fantasy. “Sure, you can get the help you need ... but don’t take time off or you will be off cycle and create extra work for all your colleagues, who are also equally stressed and will hate you. In the meantime … enjoy this free ice cream and breathing exercise to mindfully cope with the madness around you.”
The perfectly resilient resident may very well be a mythical figure, a clinical unicorn, that we continue chasing. This is the resident who remarkably discovers posttraumatic growth in every stressor. The vicarious trauma they experience from their patients only bolsters their deep compassion, and they thrive under pressure, so we can continue to pile it on. In our search for this “super resident,” we seem to continue to lose a few ordinary residents along the way.
Are we brave enough as a health care culture to take a closer look at the way we are training the next generation of healers? As I get to the end of this article, I wish I had more answers. I’m just a trainee. What do I know? My fear is that we’ve been avoiding this question altogether and have had our eyes closed to the real problem while pacifying ourselves with one “wellness” activity after another. My sincere hope is that this article will make you angry enough to be driven by a conviction that this is not
Resilience is like patience; we all wish we had more of it, but we hope to avoid getting it the hard way. This wasn’t really an area of interest for me, until it needed to be. When one academic year brings the suicide of one colleague and the murder of another, resilience becomes the only alternative to despair.
I realize that even though the particular pain or trauma we endured may be unique, it’s becoming increasingly common. The alarming studies of resident depression and suicide are too difficult for us to ignore. Now we must look in that evidence-based mirror and decide where we will go from here, as a profession and as trainees. The 2018 American Psychiatric Association annual meeting gave us a rude awakening that we may not have it figured out. Even during a year-long theme on wellness, and several sessions at the meeting focusing on the same, we all found ourselves mourning the loss of 2 colleagues to suicide that very weekend only a few miles away from the gathering of the world’s experts.
It brought an eerie element to the conversation.
The wellness “window dressing” will not get the job done. I recently had a candid discussion with a mentor in administrative leadership, and his words surprised as well as challenged me. He told me that the “system” will not save you. You must save yourself. I have decided to respectfully reject that. I think everyone should be involved, including the “system” that is entrusted with my training, and the least that it ought to ensure is that I get out alive.
Has that really become too much to ask of our profession?
We must hold our system to a higher standard. More mindfulness and better breathing will surely be helpful—but I hope we can begin to admit that this is not the answer. Unfortunately, the culture of “pay your dues” and “you know how much harder it was when I was a resident?” is still the norm. We now receive our training in an environment where the pressure is extraordinarily high, the margin for error very low, and the possibility of support is almost a fantasy. “Sure, you can get the help you need ... but don’t take time off or you will be off cycle and create extra work for all your colleagues, who are also equally stressed and will hate you. In the meantime … enjoy this free ice cream and breathing exercise to mindfully cope with the madness around you.”
The perfectly resilient resident may very well be a mythical figure, a clinical unicorn, that we continue chasing. This is the resident who remarkably discovers posttraumatic growth in every stressor. The vicarious trauma they experience from their patients only bolsters their deep compassion, and they thrive under pressure, so we can continue to pile it on. In our search for this “super resident,” we seem to continue to lose a few ordinary residents along the way.
Are we brave enough as a health care culture to take a closer look at the way we are training the next generation of healers? As I get to the end of this article, I wish I had more answers. I’m just a trainee. What do I know? My fear is that we’ve been avoiding this question altogether and have had our eyes closed to the real problem while pacifying ourselves with one “wellness” activity after another. My sincere hope is that this article will make you angry enough to be driven by a conviction that this is not
Resilience is like patience; we all wish we had more of it, but we hope to avoid getting it the hard way. This wasn’t really an area of interest for me, until it needed to be. When one academic year brings the suicide of one colleague and the murder of another, resilience becomes the only alternative to despair.
I realize that even though the particular pain or trauma we endured may be unique, it’s becoming increasingly common. The alarming studies of resident depression and suicide are too difficult for us to ignore. Now we must look in that evidence-based mirror and decide where we will go from here, as a profession and as trainees. The 2018 American Psychiatric Association annual meeting gave us a rude awakening that we may not have it figured out. Even during a year-long theme on wellness, and several sessions at the meeting focusing on the same, we all found ourselves mourning the loss of 2 colleagues to suicide that very weekend only a few miles away from the gathering of the world’s experts.
It brought an eerie element to the conversation.
The wellness “window dressing” will not get the job done. I recently had a candid discussion with a mentor in administrative leadership, and his words surprised as well as challenged me. He told me that the “system” will not save you. You must save yourself. I have decided to respectfully reject that. I think everyone should be involved, including the “system” that is entrusted with my training, and the least that it ought to ensure is that I get out alive.
Has that really become too much to ask of our profession?
We must hold our system to a higher standard. More mindfulness and better breathing will surely be helpful—but I hope we can begin to admit that this is not the answer. Unfortunately, the culture of “pay your dues” and “you know how much harder it was when I was a resident?” is still the norm. We now receive our training in an environment where the pressure is extraordinarily high, the margin for error very low, and the possibility of support is almost a fantasy. “Sure, you can get the help you need ... but don’t take time off or you will be off cycle and create extra work for all your colleagues, who are also equally stressed and will hate you. In the meantime … enjoy this free ice cream and breathing exercise to mindfully cope with the madness around you.”
The perfectly resilient resident may very well be a mythical figure, a clinical unicorn, that we continue chasing. This is the resident who remarkably discovers posttraumatic growth in every stressor. The vicarious trauma they experience from their patients only bolsters their deep compassion, and they thrive under pressure, so we can continue to pile it on. In our search for this “super resident,” we seem to continue to lose a few ordinary residents along the way.
Are we brave enough as a health care culture to take a closer look at the way we are training the next generation of healers? As I get to the end of this article, I wish I had more answers. I’m just a trainee. What do I know? My fear is that we’ve been avoiding this question altogether and have had our eyes closed to the real problem while pacifying ourselves with one “wellness” activity after another. My sincere hope is that this article will make you angry enough to be driven by a conviction that this is not
Promoting wellness during residency
The rate of burnout among physicians is disturbingly high, and wellness promotion is needed at all levels of training. While rigorous clinical training is necessary to build competence for making life-or-death decisions, training should not cause an indifference toward life or death. Because many physicians experience burnout during residency, we all must commit to wellness, which directly leads to healthier professionals and improved patient care.
Ey et al1 evaluated the feasibility and application of a wellness program for residents/fellows and faculty in an academic health center over 10 years. They concluded that a comprehensive model of care was viable and well-valued, based on high levels of physician satisfaction with the program. This model, which involves educational outreach, direct care, and consultation, inspired me to reflect on the resident burnout prevention strategies employed by the residency program in which I am currently training.
Even in situations where a formal wellness program does not exist, measures that promote resident well-being can be embedded and easily adapted:
- Education on recognizing the early signs of burnout or establishing a “buddy system” can promote a help-seeking culture and ease the transition into residency.
- Faculty who provide feedback in the “sandwich method” (praise followed by corrective feedback followed by more praise) can help promote self-confidence among residents.
- Process groups and monthly meetings with chief residents present opportunities for professional development and for residents to express concerns.
- Social gatherings that encourage team building and regular interaction among residents, attendings, and family members help build a comforting sense of community.
- A residency program director and faculty who adopt open-door policies and foster personal attention and guidance are also essential.
A recent cross-sectional analysis found that building competence, autonomy, coping mechanisms, adequate sleep, and social relatedness were associated with resident well-being.2 Hence, these factors should be integrated within residency training programs.
Residency should be approached as an engagement between colleagues where autonomy and confidence are promoted while residents acquire clinical skills within a wellness-promoting, learning environment. Demanding schedules may limit access to a dedicated wellness program; however, it is essential that a system be established to quickly identify and mitigate burnout. We all strive to be the best in our respective fields, and we must re-evaluate how we achieve excellent training while developing proper skills for future success. As physicians, we are not machines; our humanity connects us with our patients, explains life-changing news, or consoles the bereaved when there is loss of life. We must embrace our humanity and be mindful that physicians experiencing burnout cannot deliver high-quality care. Early detection and prevention strategies during residency training are key.
1. Ey S, Moffit M, Kinzie JM, et al. Feasibility of a comprehensive wellness and suicide prevention program: a decade of caring for physicians in training and practice. J Grad Med Educ. 2016;8(5):747-753.
2. Raj KS. Well-being in residency: a systematic review. J Grad Med Educ. 2016;8(5):674-684.
The rate of burnout among physicians is disturbingly high, and wellness promotion is needed at all levels of training. While rigorous clinical training is necessary to build competence for making life-or-death decisions, training should not cause an indifference toward life or death. Because many physicians experience burnout during residency, we all must commit to wellness, which directly leads to healthier professionals and improved patient care.
Ey et al1 evaluated the feasibility and application of a wellness program for residents/fellows and faculty in an academic health center over 10 years. They concluded that a comprehensive model of care was viable and well-valued, based on high levels of physician satisfaction with the program. This model, which involves educational outreach, direct care, and consultation, inspired me to reflect on the resident burnout prevention strategies employed by the residency program in which I am currently training.
Even in situations where a formal wellness program does not exist, measures that promote resident well-being can be embedded and easily adapted:
- Education on recognizing the early signs of burnout or establishing a “buddy system” can promote a help-seeking culture and ease the transition into residency.
- Faculty who provide feedback in the “sandwich method” (praise followed by corrective feedback followed by more praise) can help promote self-confidence among residents.
- Process groups and monthly meetings with chief residents present opportunities for professional development and for residents to express concerns.
- Social gatherings that encourage team building and regular interaction among residents, attendings, and family members help build a comforting sense of community.
- A residency program director and faculty who adopt open-door policies and foster personal attention and guidance are also essential.
A recent cross-sectional analysis found that building competence, autonomy, coping mechanisms, adequate sleep, and social relatedness were associated with resident well-being.2 Hence, these factors should be integrated within residency training programs.
Residency should be approached as an engagement between colleagues where autonomy and confidence are promoted while residents acquire clinical skills within a wellness-promoting, learning environment. Demanding schedules may limit access to a dedicated wellness program; however, it is essential that a system be established to quickly identify and mitigate burnout. We all strive to be the best in our respective fields, and we must re-evaluate how we achieve excellent training while developing proper skills for future success. As physicians, we are not machines; our humanity connects us with our patients, explains life-changing news, or consoles the bereaved when there is loss of life. We must embrace our humanity and be mindful that physicians experiencing burnout cannot deliver high-quality care. Early detection and prevention strategies during residency training are key.
The rate of burnout among physicians is disturbingly high, and wellness promotion is needed at all levels of training. While rigorous clinical training is necessary to build competence for making life-or-death decisions, training should not cause an indifference toward life or death. Because many physicians experience burnout during residency, we all must commit to wellness, which directly leads to healthier professionals and improved patient care.
Ey et al1 evaluated the feasibility and application of a wellness program for residents/fellows and faculty in an academic health center over 10 years. They concluded that a comprehensive model of care was viable and well-valued, based on high levels of physician satisfaction with the program. This model, which involves educational outreach, direct care, and consultation, inspired me to reflect on the resident burnout prevention strategies employed by the residency program in which I am currently training.
Even in situations where a formal wellness program does not exist, measures that promote resident well-being can be embedded and easily adapted:
- Education on recognizing the early signs of burnout or establishing a “buddy system” can promote a help-seeking culture and ease the transition into residency.
- Faculty who provide feedback in the “sandwich method” (praise followed by corrective feedback followed by more praise) can help promote self-confidence among residents.
- Process groups and monthly meetings with chief residents present opportunities for professional development and for residents to express concerns.
- Social gatherings that encourage team building and regular interaction among residents, attendings, and family members help build a comforting sense of community.
- A residency program director and faculty who adopt open-door policies and foster personal attention and guidance are also essential.
A recent cross-sectional analysis found that building competence, autonomy, coping mechanisms, adequate sleep, and social relatedness were associated with resident well-being.2 Hence, these factors should be integrated within residency training programs.
Residency should be approached as an engagement between colleagues where autonomy and confidence are promoted while residents acquire clinical skills within a wellness-promoting, learning environment. Demanding schedules may limit access to a dedicated wellness program; however, it is essential that a system be established to quickly identify and mitigate burnout. We all strive to be the best in our respective fields, and we must re-evaluate how we achieve excellent training while developing proper skills for future success. As physicians, we are not machines; our humanity connects us with our patients, explains life-changing news, or consoles the bereaved when there is loss of life. We must embrace our humanity and be mindful that physicians experiencing burnout cannot deliver high-quality care. Early detection and prevention strategies during residency training are key.
1. Ey S, Moffit M, Kinzie JM, et al. Feasibility of a comprehensive wellness and suicide prevention program: a decade of caring for physicians in training and practice. J Grad Med Educ. 2016;8(5):747-753.
2. Raj KS. Well-being in residency: a systematic review. J Grad Med Educ. 2016;8(5):674-684.
1. Ey S, Moffit M, Kinzie JM, et al. Feasibility of a comprehensive wellness and suicide prevention program: a decade of caring for physicians in training and practice. J Grad Med Educ. 2016;8(5):747-753.
2. Raj KS. Well-being in residency: a systematic review. J Grad Med Educ. 2016;8(5):674-684.
Family therapy and cultural conflicts
I recently had the privilege of treating a family who spoke my first language, Hindi. My patient, Ms. M, was 16 years old and struggling to adjust to her new life in the United States, having recently come from India. America’s schooling, culture, and “open society” was a contrast to her life in a semi-rural town, especially her close-knit family structure in which her parents and siblings are everything. Due to their cultural beliefs and religious faith in Islam, both Ms. M and her father were initially resistant to begin treatment for her depression and anxiety. “Let’s give it a trial” was the attitude I finally got from the father. But to me, there was a clear discordance in the communication among the family members in addition to the primary mental illness that led them to come for treatment. I was attracted to work with this family because I had a reasonable understanding of their faith, their culture, and their family system, and I have an inclination toward spirituality. Even though I recognized this family’s social isolation, I wondered why they were still in a state of unrest, given their deep commitment to their faith.
Ms. M was isolating herself at home, in an environment that wasn’t supportive of talking about her concerns. These included being bullied for being “different,” for how she dressed, and for having home-cooked traditional meals for lunch, and being unable to socialize with most of her male peers, except for those from her same community. This led her to dream of returning to India.
The family did not have a social life. Ms. M told me, “I wanted to socialize, but I cannot because of my faith and religion.” So she chose to wear attire to identify with her mother and her culture of origin. She also did this to hide her emotional pain from enduring trauma related to bullying at her school. It was a challenge to understand how faith, resilience, and trauma were intermingled in Ms. M and her family.
I saw Ms. M and her family for 12 one-hour family psychotherapy sessions. The initial session unfolded uneasily. It was a challenge to build rapport and help them understand how family therapy works. Circular inquiries to each family member, specifically to get the mother’s point of view, brought mourning, shame, and guilt to this family. The importance of marriage, education, and immigration were processed in reference to their culture and their incomplete acculturation to life in the United States.
I wondered if there were other families with different cultural backgrounds who struggled with similar conflicts. I also wondered if those families understood the value of family therapy or had ever experienced this therapeutic process.
The 3 key signs that made me believe that this family was making progress through our work together included:
- They complied with treatment; the family never missed a session.
- The parents acknowledged that their daughter was doing better.
- The mother brought me a dinner as a gesture of gratitude in our last session. This is a particularly meaningful gesture on the part of people with their cultural background.
I clearly remember our first meeting, when Ms. M asked
I recently had the privilege of treating a family who spoke my first language, Hindi. My patient, Ms. M, was 16 years old and struggling to adjust to her new life in the United States, having recently come from India. America’s schooling, culture, and “open society” was a contrast to her life in a semi-rural town, especially her close-knit family structure in which her parents and siblings are everything. Due to their cultural beliefs and religious faith in Islam, both Ms. M and her father were initially resistant to begin treatment for her depression and anxiety. “Let’s give it a trial” was the attitude I finally got from the father. But to me, there was a clear discordance in the communication among the family members in addition to the primary mental illness that led them to come for treatment. I was attracted to work with this family because I had a reasonable understanding of their faith, their culture, and their family system, and I have an inclination toward spirituality. Even though I recognized this family’s social isolation, I wondered why they were still in a state of unrest, given their deep commitment to their faith.
Ms. M was isolating herself at home, in an environment that wasn’t supportive of talking about her concerns. These included being bullied for being “different,” for how she dressed, and for having home-cooked traditional meals for lunch, and being unable to socialize with most of her male peers, except for those from her same community. This led her to dream of returning to India.
The family did not have a social life. Ms. M told me, “I wanted to socialize, but I cannot because of my faith and religion.” So she chose to wear attire to identify with her mother and her culture of origin. She also did this to hide her emotional pain from enduring trauma related to bullying at her school. It was a challenge to understand how faith, resilience, and trauma were intermingled in Ms. M and her family.
I saw Ms. M and her family for 12 one-hour family psychotherapy sessions. The initial session unfolded uneasily. It was a challenge to build rapport and help them understand how family therapy works. Circular inquiries to each family member, specifically to get the mother’s point of view, brought mourning, shame, and guilt to this family. The importance of marriage, education, and immigration were processed in reference to their culture and their incomplete acculturation to life in the United States.
I wondered if there were other families with different cultural backgrounds who struggled with similar conflicts. I also wondered if those families understood the value of family therapy or had ever experienced this therapeutic process.
The 3 key signs that made me believe that this family was making progress through our work together included:
- They complied with treatment; the family never missed a session.
- The parents acknowledged that their daughter was doing better.
- The mother brought me a dinner as a gesture of gratitude in our last session. This is a particularly meaningful gesture on the part of people with their cultural background.
I clearly remember our first meeting, when Ms. M asked
I recently had the privilege of treating a family who spoke my first language, Hindi. My patient, Ms. M, was 16 years old and struggling to adjust to her new life in the United States, having recently come from India. America’s schooling, culture, and “open society” was a contrast to her life in a semi-rural town, especially her close-knit family structure in which her parents and siblings are everything. Due to their cultural beliefs and religious faith in Islam, both Ms. M and her father were initially resistant to begin treatment for her depression and anxiety. “Let’s give it a trial” was the attitude I finally got from the father. But to me, there was a clear discordance in the communication among the family members in addition to the primary mental illness that led them to come for treatment. I was attracted to work with this family because I had a reasonable understanding of their faith, their culture, and their family system, and I have an inclination toward spirituality. Even though I recognized this family’s social isolation, I wondered why they were still in a state of unrest, given their deep commitment to their faith.
Ms. M was isolating herself at home, in an environment that wasn’t supportive of talking about her concerns. These included being bullied for being “different,” for how she dressed, and for having home-cooked traditional meals for lunch, and being unable to socialize with most of her male peers, except for those from her same community. This led her to dream of returning to India.
The family did not have a social life. Ms. M told me, “I wanted to socialize, but I cannot because of my faith and religion.” So she chose to wear attire to identify with her mother and her culture of origin. She also did this to hide her emotional pain from enduring trauma related to bullying at her school. It was a challenge to understand how faith, resilience, and trauma were intermingled in Ms. M and her family.
I saw Ms. M and her family for 12 one-hour family psychotherapy sessions. The initial session unfolded uneasily. It was a challenge to build rapport and help them understand how family therapy works. Circular inquiries to each family member, specifically to get the mother’s point of view, brought mourning, shame, and guilt to this family. The importance of marriage, education, and immigration were processed in reference to their culture and their incomplete acculturation to life in the United States.
I wondered if there were other families with different cultural backgrounds who struggled with similar conflicts. I also wondered if those families understood the value of family therapy or had ever experienced this therapeutic process.
The 3 key signs that made me believe that this family was making progress through our work together included:
- They complied with treatment; the family never missed a session.
- The parents acknowledged that their daughter was doing better.
- The mother brought me a dinner as a gesture of gratitude in our last session. This is a particularly meaningful gesture on the part of people with their cultural background.
I clearly remember our first meeting, when Ms. M asked
Proactive consultation: A new model of care in consultation-liaison psychiatry
During my residency training, I was trained in the standard “reactive” psychiatric consultation model. In this system, I would see consults placed by the primary team after they identified a behavioral issue in a patient. As a trainee, I experienced frequent frustrations working in this model: Consults that are discharge-dependent (“Can you see the patient before he is discharged this morning?”), consults for acute behavioral dysregulation (“The patient is near the elevator, can you come see him ASAP?”), or consults for consequences of poor management of alcohol/benzodiazepine withdrawal (“The patient is confused and trying to leave”).
As a fellow in consultation-liaison (C-L) psychiatry, I was introduced to the “proactive” consultation model, which avoids some of these issues. In this article, which is intended for residents who have not been exposed to this new approach, I explain how the proactive model changes our experience as C-L clinicians.
The Behavioral Intervention Team
At Yale New Haven Hospital, the Behavioral Intervention Team (BIT) is a proactive, multidisciplinary psychiatric consultation service that serves the internal medicine units at the hospital. The team consists of nurse practitioners, nurse liaison specialists, social workers, and psychiatrists. The team identifies and removes behavioral barriers in the care of hospitalized mentally ill patients.
The BIT collaborates closely with the medical team through formal and informal consultation; co-management of behavioral issues; education of medical, nursing, and social work staff; and direct care of complex patients with behavioral disorders. The BIT assists the medical team with transitions to appropriate outpatient and inpatient psychiatric care. The team also manages the relationship with the insurer when a patient requires a stay in a psychiatric unit.
This model has a critical financial benefit in reducing the length of stay, but it also has many other benefits. It focuses on early recognition and treatment, and helps mitigate the effects of mental or substance use disorders on patients’ recovery. BIT members educate their peers regarding management of a multitude of behavioral issues. This fosters extensive informal collaboration (“curbside consultation”), which helps patients who did not receive a formal consult. The model distributes work more rationally among different professional specialists. It yields a relationship with medical teams that is not only more effective, but also more enjoyable. In the BIT model, psychiatrists pick the cases where they feel they can have the most impact, and avoid the cases they feel they cannot have any.1-3
CASE A better approach to alcohol withdrawal
Mr. X, age 56, has a history of alcohol use disorder, hypertension, and coronary artery disease. He’s had multiple past admissions for complicated alcohol withdrawal. He is transferred from a local community hospital, where he had presented with chest pain. His last drink was 2 days prior to admission, and his blood alcohol level is <10 mg/dL.
During Mr. X’s previous hospitalizations, psychiatric consults were performed in the standard reactive model. The primary team initially prescribed an ineffective dosage of benzodiazepines for his alcohol withdrawal. This escalated his withdrawal into delirium tremens, after which psychiatry was involved. Due to this early ineffective management, the patient had a prolonged medical ICU stay and overall stay, experienced increased medical complications, and required increased staff resources because he was extremely agitated.
Continued to: During this hospitalization...
During this hospitalization, Mr. X arrives with similar medical complaints. The nurse practitioner on the BIT service, who screened all admissions each day, examines the prior notes (she finds the team sign-outs to be particularly useful). She suggests a psychiatric consult on Day 1 of the admission, which the primary medical team orders. The BIT nurse practitioner gives apt recommendations of evidence-based management, including a benzodiazepine taper, high-dose thiamine, and psychopharmacologic approaches to severe agitation. The nurse liaison specialist on the service makes behavioral plans for managing agitation, which she communicates to the nurses caring for Mr. X.
Because his withdrawal is managed more promptly, Mr. X’s length of stay is shorter and he does not experience any medical complications. The BIT social worker helps find appropriate aftercare options, including residential treatment and Alcoholics Anonymous meetings, to which the patient agrees.
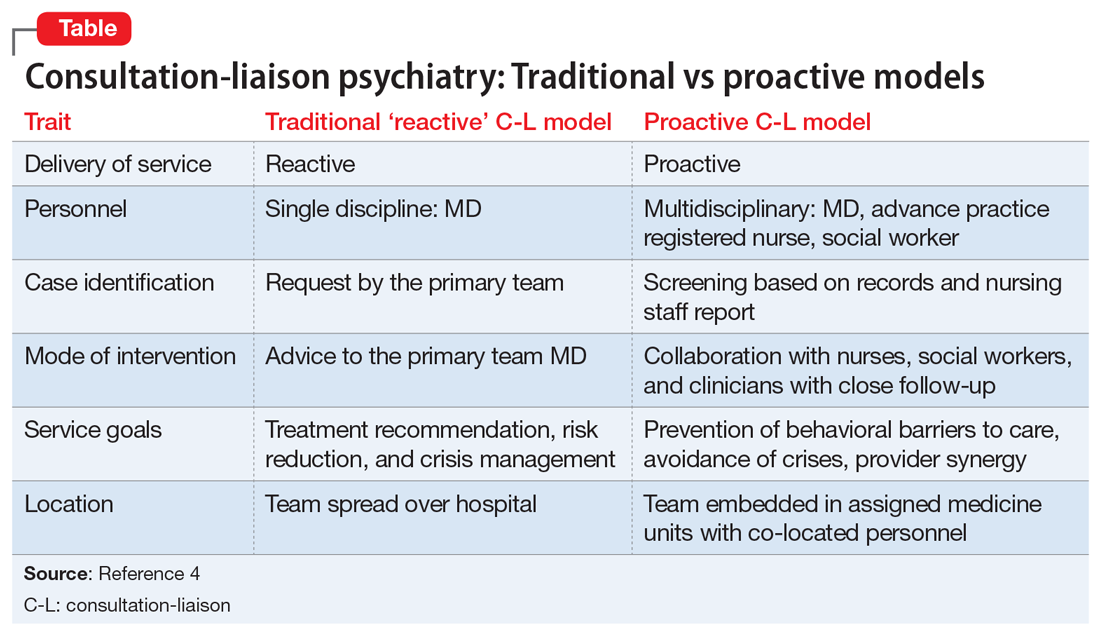
Participating in this case was highly educational for me as a trainee. This case is but one example among many where proactive consultation provided prompt care, lowered the rate of complications, reduced length of stay, and resulted in greater provider satisfaction. The Table4 contrasts the proactive and reactive consultation models. The following 5 factors are critical in the proactive consultation model4,5:
1. Standardized and reliable procedure screening of all admissions, involving a mental health professional, through record review and staff contact. This screening should identify patients with issues who will benefit specifically from in-hospital services, rather than just patients with any psychiatric issue. An electronic medical record is essential to efficient screening, team communication, and progress monitoring. Truly integrated consultation would be impossible with a paper chart.
Continued to: 2. Rapid intervention...
2. Rapid intervention that anticipates impending problems before a cascade of complications starts.
3. Collaborative engagement with the primary medical team, sharing the burden of caring for the complex inpatient, and transmitting critical behavioral management skills to all caregivers, including the skill of recognizing patients who can benefit from a psychiatric consultation.
4. Daily and close contact between behavioral and medical teams, ensuring that treatment recommendations are understood, enacted, and reinforced, ineffective treatments are discontinued, and new problems are addressed before complicating consequences arise. Dedicating specific personnel to specific hospital units and placing them in rounds simplifies communication and speeds intervention implementation.
5. A multidisciplinary consultation team, offering a range of responses, including informal curbside consultation, consultation with an advanced practice registered nurse, social work interventions, advice to discharge planning teams, psychological services, and access to specialized providers, such as addiction teams, as well as traditional consultation with an experienced psychiatrist.
Research has shown the effectiveness of proactive, embedded, multidisciplinary approaches.1-3,5 It was a gratifying experience to work in this model. I worked intimately with medical clinicians, and shared the burden of responsibilities leading to optimal patient outcomes. The proactive consultation model truly re-emphasizes the “liaison” component of C-L psychiatry, as it was originally envisioned.
1. Sledge WH, Gueorguieva R, Desan P, et al. Multidisciplinary proactive psychiatric consultation service: impact on length of stay for medical inpatients. Psychother Psychosom. 2015;84(4):208-216.
2. Desan PH, Zimbrean PC, Weinstein AJ, et al. Proactive psychiatric consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011;52(6):513-520.
3. Sledge WH, Bozzo J, White-McCullum BA, et al. The cost-benefit from the perspective of the hospital of a proactive psychiatric consultation service on inpatient general medicine services. Health Econ Outcome Res Open Access. 2016;2(4):122.
4. Sledge WH, Lee HB. Proactive psychiatric consultation for hospitalized patients, a plan for the future. Health Affairs. www.healthaffairs.org/do/10.1377/hblog20150528.048026/full/. Published May 28, 2015. Accessed September 12, 2018.
5. Desan P, Lee H, Zimbrean P, et al. New models of psychiatric consultation in the general medical hospital: liaison psychiatry is back. Psychiatr Ann. 2017;47:355-361.
During my residency training, I was trained in the standard “reactive” psychiatric consultation model. In this system, I would see consults placed by the primary team after they identified a behavioral issue in a patient. As a trainee, I experienced frequent frustrations working in this model: Consults that are discharge-dependent (“Can you see the patient before he is discharged this morning?”), consults for acute behavioral dysregulation (“The patient is near the elevator, can you come see him ASAP?”), or consults for consequences of poor management of alcohol/benzodiazepine withdrawal (“The patient is confused and trying to leave”).
As a fellow in consultation-liaison (C-L) psychiatry, I was introduced to the “proactive” consultation model, which avoids some of these issues. In this article, which is intended for residents who have not been exposed to this new approach, I explain how the proactive model changes our experience as C-L clinicians.
The Behavioral Intervention Team
At Yale New Haven Hospital, the Behavioral Intervention Team (BIT) is a proactive, multidisciplinary psychiatric consultation service that serves the internal medicine units at the hospital. The team consists of nurse practitioners, nurse liaison specialists, social workers, and psychiatrists. The team identifies and removes behavioral barriers in the care of hospitalized mentally ill patients.
The BIT collaborates closely with the medical team through formal and informal consultation; co-management of behavioral issues; education of medical, nursing, and social work staff; and direct care of complex patients with behavioral disorders. The BIT assists the medical team with transitions to appropriate outpatient and inpatient psychiatric care. The team also manages the relationship with the insurer when a patient requires a stay in a psychiatric unit.
This model has a critical financial benefit in reducing the length of stay, but it also has many other benefits. It focuses on early recognition and treatment, and helps mitigate the effects of mental or substance use disorders on patients’ recovery. BIT members educate their peers regarding management of a multitude of behavioral issues. This fosters extensive informal collaboration (“curbside consultation”), which helps patients who did not receive a formal consult. The model distributes work more rationally among different professional specialists. It yields a relationship with medical teams that is not only more effective, but also more enjoyable. In the BIT model, psychiatrists pick the cases where they feel they can have the most impact, and avoid the cases they feel they cannot have any.1-3
CASE A better approach to alcohol withdrawal
Mr. X, age 56, has a history of alcohol use disorder, hypertension, and coronary artery disease. He’s had multiple past admissions for complicated alcohol withdrawal. He is transferred from a local community hospital, where he had presented with chest pain. His last drink was 2 days prior to admission, and his blood alcohol level is <10 mg/dL.
During Mr. X’s previous hospitalizations, psychiatric consults were performed in the standard reactive model. The primary team initially prescribed an ineffective dosage of benzodiazepines for his alcohol withdrawal. This escalated his withdrawal into delirium tremens, after which psychiatry was involved. Due to this early ineffective management, the patient had a prolonged medical ICU stay and overall stay, experienced increased medical complications, and required increased staff resources because he was extremely agitated.
Continued to: During this hospitalization...
During this hospitalization, Mr. X arrives with similar medical complaints. The nurse practitioner on the BIT service, who screened all admissions each day, examines the prior notes (she finds the team sign-outs to be particularly useful). She suggests a psychiatric consult on Day 1 of the admission, which the primary medical team orders. The BIT nurse practitioner gives apt recommendations of evidence-based management, including a benzodiazepine taper, high-dose thiamine, and psychopharmacologic approaches to severe agitation. The nurse liaison specialist on the service makes behavioral plans for managing agitation, which she communicates to the nurses caring for Mr. X.
Because his withdrawal is managed more promptly, Mr. X’s length of stay is shorter and he does not experience any medical complications. The BIT social worker helps find appropriate aftercare options, including residential treatment and Alcoholics Anonymous meetings, to which the patient agrees.
Participating in this case was highly educational for me as a trainee. This case is but one example among many where proactive consultation provided prompt care, lowered the rate of complications, reduced length of stay, and resulted in greater provider satisfaction. The Table4 contrasts the proactive and reactive consultation models. The following 5 factors are critical in the proactive consultation model4,5:
1. Standardized and reliable procedure screening of all admissions, involving a mental health professional, through record review and staff contact. This screening should identify patients with issues who will benefit specifically from in-hospital services, rather than just patients with any psychiatric issue. An electronic medical record is essential to efficient screening, team communication, and progress monitoring. Truly integrated consultation would be impossible with a paper chart.
Continued to: 2. Rapid intervention...
2. Rapid intervention that anticipates impending problems before a cascade of complications starts.
3. Collaborative engagement with the primary medical team, sharing the burden of caring for the complex inpatient, and transmitting critical behavioral management skills to all caregivers, including the skill of recognizing patients who can benefit from a psychiatric consultation.
4. Daily and close contact between behavioral and medical teams, ensuring that treatment recommendations are understood, enacted, and reinforced, ineffective treatments are discontinued, and new problems are addressed before complicating consequences arise. Dedicating specific personnel to specific hospital units and placing them in rounds simplifies communication and speeds intervention implementation.
5. A multidisciplinary consultation team, offering a range of responses, including informal curbside consultation, consultation with an advanced practice registered nurse, social work interventions, advice to discharge planning teams, psychological services, and access to specialized providers, such as addiction teams, as well as traditional consultation with an experienced psychiatrist.
Research has shown the effectiveness of proactive, embedded, multidisciplinary approaches.1-3,5 It was a gratifying experience to work in this model. I worked intimately with medical clinicians, and shared the burden of responsibilities leading to optimal patient outcomes. The proactive consultation model truly re-emphasizes the “liaison” component of C-L psychiatry, as it was originally envisioned.
During my residency training, I was trained in the standard “reactive” psychiatric consultation model. In this system, I would see consults placed by the primary team after they identified a behavioral issue in a patient. As a trainee, I experienced frequent frustrations working in this model: Consults that are discharge-dependent (“Can you see the patient before he is discharged this morning?”), consults for acute behavioral dysregulation (“The patient is near the elevator, can you come see him ASAP?”), or consults for consequences of poor management of alcohol/benzodiazepine withdrawal (“The patient is confused and trying to leave”).
As a fellow in consultation-liaison (C-L) psychiatry, I was introduced to the “proactive” consultation model, which avoids some of these issues. In this article, which is intended for residents who have not been exposed to this new approach, I explain how the proactive model changes our experience as C-L clinicians.
The Behavioral Intervention Team
At Yale New Haven Hospital, the Behavioral Intervention Team (BIT) is a proactive, multidisciplinary psychiatric consultation service that serves the internal medicine units at the hospital. The team consists of nurse practitioners, nurse liaison specialists, social workers, and psychiatrists. The team identifies and removes behavioral barriers in the care of hospitalized mentally ill patients.
The BIT collaborates closely with the medical team through formal and informal consultation; co-management of behavioral issues; education of medical, nursing, and social work staff; and direct care of complex patients with behavioral disorders. The BIT assists the medical team with transitions to appropriate outpatient and inpatient psychiatric care. The team also manages the relationship with the insurer when a patient requires a stay in a psychiatric unit.
This model has a critical financial benefit in reducing the length of stay, but it also has many other benefits. It focuses on early recognition and treatment, and helps mitigate the effects of mental or substance use disorders on patients’ recovery. BIT members educate their peers regarding management of a multitude of behavioral issues. This fosters extensive informal collaboration (“curbside consultation”), which helps patients who did not receive a formal consult. The model distributes work more rationally among different professional specialists. It yields a relationship with medical teams that is not only more effective, but also more enjoyable. In the BIT model, psychiatrists pick the cases where they feel they can have the most impact, and avoid the cases they feel they cannot have any.1-3
CASE A better approach to alcohol withdrawal
Mr. X, age 56, has a history of alcohol use disorder, hypertension, and coronary artery disease. He’s had multiple past admissions for complicated alcohol withdrawal. He is transferred from a local community hospital, where he had presented with chest pain. His last drink was 2 days prior to admission, and his blood alcohol level is <10 mg/dL.
During Mr. X’s previous hospitalizations, psychiatric consults were performed in the standard reactive model. The primary team initially prescribed an ineffective dosage of benzodiazepines for his alcohol withdrawal. This escalated his withdrawal into delirium tremens, after which psychiatry was involved. Due to this early ineffective management, the patient had a prolonged medical ICU stay and overall stay, experienced increased medical complications, and required increased staff resources because he was extremely agitated.
Continued to: During this hospitalization...
During this hospitalization, Mr. X arrives with similar medical complaints. The nurse practitioner on the BIT service, who screened all admissions each day, examines the prior notes (she finds the team sign-outs to be particularly useful). She suggests a psychiatric consult on Day 1 of the admission, which the primary medical team orders. The BIT nurse practitioner gives apt recommendations of evidence-based management, including a benzodiazepine taper, high-dose thiamine, and psychopharmacologic approaches to severe agitation. The nurse liaison specialist on the service makes behavioral plans for managing agitation, which she communicates to the nurses caring for Mr. X.
Because his withdrawal is managed more promptly, Mr. X’s length of stay is shorter and he does not experience any medical complications. The BIT social worker helps find appropriate aftercare options, including residential treatment and Alcoholics Anonymous meetings, to which the patient agrees.
Participating in this case was highly educational for me as a trainee. This case is but one example among many where proactive consultation provided prompt care, lowered the rate of complications, reduced length of stay, and resulted in greater provider satisfaction. The Table4 contrasts the proactive and reactive consultation models. The following 5 factors are critical in the proactive consultation model4,5:
1. Standardized and reliable procedure screening of all admissions, involving a mental health professional, through record review and staff contact. This screening should identify patients with issues who will benefit specifically from in-hospital services, rather than just patients with any psychiatric issue. An electronic medical record is essential to efficient screening, team communication, and progress monitoring. Truly integrated consultation would be impossible with a paper chart.
Continued to: 2. Rapid intervention...
2. Rapid intervention that anticipates impending problems before a cascade of complications starts.
3. Collaborative engagement with the primary medical team, sharing the burden of caring for the complex inpatient, and transmitting critical behavioral management skills to all caregivers, including the skill of recognizing patients who can benefit from a psychiatric consultation.
4. Daily and close contact between behavioral and medical teams, ensuring that treatment recommendations are understood, enacted, and reinforced, ineffective treatments are discontinued, and new problems are addressed before complicating consequences arise. Dedicating specific personnel to specific hospital units and placing them in rounds simplifies communication and speeds intervention implementation.
5. A multidisciplinary consultation team, offering a range of responses, including informal curbside consultation, consultation with an advanced practice registered nurse, social work interventions, advice to discharge planning teams, psychological services, and access to specialized providers, such as addiction teams, as well as traditional consultation with an experienced psychiatrist.
Research has shown the effectiveness of proactive, embedded, multidisciplinary approaches.1-3,5 It was a gratifying experience to work in this model. I worked intimately with medical clinicians, and shared the burden of responsibilities leading to optimal patient outcomes. The proactive consultation model truly re-emphasizes the “liaison” component of C-L psychiatry, as it was originally envisioned.
1. Sledge WH, Gueorguieva R, Desan P, et al. Multidisciplinary proactive psychiatric consultation service: impact on length of stay for medical inpatients. Psychother Psychosom. 2015;84(4):208-216.
2. Desan PH, Zimbrean PC, Weinstein AJ, et al. Proactive psychiatric consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011;52(6):513-520.
3. Sledge WH, Bozzo J, White-McCullum BA, et al. The cost-benefit from the perspective of the hospital of a proactive psychiatric consultation service on inpatient general medicine services. Health Econ Outcome Res Open Access. 2016;2(4):122.
4. Sledge WH, Lee HB. Proactive psychiatric consultation for hospitalized patients, a plan for the future. Health Affairs. www.healthaffairs.org/do/10.1377/hblog20150528.048026/full/. Published May 28, 2015. Accessed September 12, 2018.
5. Desan P, Lee H, Zimbrean P, et al. New models of psychiatric consultation in the general medical hospital: liaison psychiatry is back. Psychiatr Ann. 2017;47:355-361.
1. Sledge WH, Gueorguieva R, Desan P, et al. Multidisciplinary proactive psychiatric consultation service: impact on length of stay for medical inpatients. Psychother Psychosom. 2015;84(4):208-216.
2. Desan PH, Zimbrean PC, Weinstein AJ, et al. Proactive psychiatric consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011;52(6):513-520.
3. Sledge WH, Bozzo J, White-McCullum BA, et al. The cost-benefit from the perspective of the hospital of a proactive psychiatric consultation service on inpatient general medicine services. Health Econ Outcome Res Open Access. 2016;2(4):122.
4. Sledge WH, Lee HB. Proactive psychiatric consultation for hospitalized patients, a plan for the future. Health Affairs. www.healthaffairs.org/do/10.1377/hblog20150528.048026/full/. Published May 28, 2015. Accessed September 12, 2018.
5. Desan P, Lee H, Zimbrean P, et al. New models of psychiatric consultation in the general medical hospital: liaison psychiatry is back. Psychiatr Ann. 2017;47:355-361.
How to make psychiatry residency more rewarding
During my residency, I have taken advantage of several opportunities that helped me develop and become more confident as I assumed the role of Academic Chief Resident in my final year of residency. In this article, I describe some of these opportunities, including seeking extra supervision while providing psychotherapy, engaging in psychotherapy for oneself, becoming part of leadership, and participating in quality improvement (QI) projects.
Obtain extra supervision while providing psychotherapy. I feel it is important to become comfortable with different types of therapy during residency. There are various opportunities to receive additional education via 1- and 2-year courses. I attended the Prelude t
Consider seeking out psychotherapy. When I started providing therapy to my patients, I became aware of how important it is to invest in your own personal therapy to understand your mind. I researched the importance of personal therapy for psychiatric clinicians, and to my surprise there have been lengthy debates on both its positive and negative impacts. However, I have come to believe that personal therapy is an important part of training for mental health professionals because it helps us better understand ourselves, since it is impossible to take the therapist’s mind out of the session. Although personal psychotherapy is not required, residency is an opportune time to pursue it.
Get involved and become part of leadership. I always believed that when united, we are stronger. It is a great privilege that as residents, we can become an integral part of advocacy and leadership in different organizations at both the state and national level. Here are 2 examples of how I got involved:
- The American Psychiatric Association (APA). When I attended the APA to present my posters for the first time, I wanted to become more actively involved. So I contacted my district branch representatives for guidance. I attended meetings and became involved in the Brooklyn District Branch as a resident representative. I was elected APA Area 2 Resident Fellow Member Deputy representative (a 2-year position). In this position, I represent residents and fellows from New York in the APA assembly. This has been a gratifying experience, and I have come to appreciate the proceedings of the Assembly and the amount of work that goes into creating Action Papers and Policy Statements.
- The Committee of Interns and Residents (CIR). Representation in CIR is extremely important in this political climate. The resident CIR Delegates are selected via elections. Delegates have an excellent opportunity to attend the Delegate Conference to learn how CIR operates and represent the department in CIR meetings. CIR is extremely supportive of resident involvement in QI projects and provides opportunities to chair a quality council for residents.
Participate in QI projects. Involvement in QI projects provided me with the opportunity to learn unique skills, including how to think creatively, design a study, and work with statisticians to extract and analyze data. The main focus of my research has been resident well-being and burnout.
These are a few of the wonderful opportunities I have been able to experience during my residency. I would love to hear from other residents about their similar experiences.
During my residency, I have taken advantage of several opportunities that helped me develop and become more confident as I assumed the role of Academic Chief Resident in my final year of residency. In this article, I describe some of these opportunities, including seeking extra supervision while providing psychotherapy, engaging in psychotherapy for oneself, becoming part of leadership, and participating in quality improvement (QI) projects.
Obtain extra supervision while providing psychotherapy. I feel it is important to become comfortable with different types of therapy during residency. There are various opportunities to receive additional education via 1- and 2-year courses. I attended the Prelude t
Consider seeking out psychotherapy. When I started providing therapy to my patients, I became aware of how important it is to invest in your own personal therapy to understand your mind. I researched the importance of personal therapy for psychiatric clinicians, and to my surprise there have been lengthy debates on both its positive and negative impacts. However, I have come to believe that personal therapy is an important part of training for mental health professionals because it helps us better understand ourselves, since it is impossible to take the therapist’s mind out of the session. Although personal psychotherapy is not required, residency is an opportune time to pursue it.
Get involved and become part of leadership. I always believed that when united, we are stronger. It is a great privilege that as residents, we can become an integral part of advocacy and leadership in different organizations at both the state and national level. Here are 2 examples of how I got involved:
- The American Psychiatric Association (APA). When I attended the APA to present my posters for the first time, I wanted to become more actively involved. So I contacted my district branch representatives for guidance. I attended meetings and became involved in the Brooklyn District Branch as a resident representative. I was elected APA Area 2 Resident Fellow Member Deputy representative (a 2-year position). In this position, I represent residents and fellows from New York in the APA assembly. This has been a gratifying experience, and I have come to appreciate the proceedings of the Assembly and the amount of work that goes into creating Action Papers and Policy Statements.
- The Committee of Interns and Residents (CIR). Representation in CIR is extremely important in this political climate. The resident CIR Delegates are selected via elections. Delegates have an excellent opportunity to attend the Delegate Conference to learn how CIR operates and represent the department in CIR meetings. CIR is extremely supportive of resident involvement in QI projects and provides opportunities to chair a quality council for residents.
Participate in QI projects. Involvement in QI projects provided me with the opportunity to learn unique skills, including how to think creatively, design a study, and work with statisticians to extract and analyze data. The main focus of my research has been resident well-being and burnout.
These are a few of the wonderful opportunities I have been able to experience during my residency. I would love to hear from other residents about their similar experiences.
During my residency, I have taken advantage of several opportunities that helped me develop and become more confident as I assumed the role of Academic Chief Resident in my final year of residency. In this article, I describe some of these opportunities, including seeking extra supervision while providing psychotherapy, engaging in psychotherapy for oneself, becoming part of leadership, and participating in quality improvement (QI) projects.
Obtain extra supervision while providing psychotherapy. I feel it is important to become comfortable with different types of therapy during residency. There are various opportunities to receive additional education via 1- and 2-year courses. I attended the Prelude t
Consider seeking out psychotherapy. When I started providing therapy to my patients, I became aware of how important it is to invest in your own personal therapy to understand your mind. I researched the importance of personal therapy for psychiatric clinicians, and to my surprise there have been lengthy debates on both its positive and negative impacts. However, I have come to believe that personal therapy is an important part of training for mental health professionals because it helps us better understand ourselves, since it is impossible to take the therapist’s mind out of the session. Although personal psychotherapy is not required, residency is an opportune time to pursue it.
Get involved and become part of leadership. I always believed that when united, we are stronger. It is a great privilege that as residents, we can become an integral part of advocacy and leadership in different organizations at both the state and national level. Here are 2 examples of how I got involved:
- The American Psychiatric Association (APA). When I attended the APA to present my posters for the first time, I wanted to become more actively involved. So I contacted my district branch representatives for guidance. I attended meetings and became involved in the Brooklyn District Branch as a resident representative. I was elected APA Area 2 Resident Fellow Member Deputy representative (a 2-year position). In this position, I represent residents and fellows from New York in the APA assembly. This has been a gratifying experience, and I have come to appreciate the proceedings of the Assembly and the amount of work that goes into creating Action Papers and Policy Statements.
- The Committee of Interns and Residents (CIR). Representation in CIR is extremely important in this political climate. The resident CIR Delegates are selected via elections. Delegates have an excellent opportunity to attend the Delegate Conference to learn how CIR operates and represent the department in CIR meetings. CIR is extremely supportive of resident involvement in QI projects and provides opportunities to chair a quality council for residents.
Participate in QI projects. Involvement in QI projects provided me with the opportunity to learn unique skills, including how to think creatively, design a study, and work with statisticians to extract and analyze data. The main focus of my research has been resident well-being and burnout.
These are a few of the wonderful opportunities I have been able to experience during my residency. I would love to hear from other residents about their similar experiences.
Embracing therapeutic silence: A resident’s perspective on learning psychotherapy
There is a tendency among young psychiatric residents, including me, to experience significant anxiety when providing outpatient psychotherapy for the first time. This anxiety often leads to rigid adherence to structured sessions aimed at a specific therapeutic target. Unfortunately, as patients begin to stray from the mold, this model breaks down and leaves the resident with little direction.
As a resident with an engineering background, I felt a strong affinity for this targeted approach, and have struggled for direction with patients whose symptoms or willingness to engage therapeutically did not match this method. I have slowly come to appreciate a more nimble approach that balances elements of both a structured method (such as cognitive-behavioral therapy [CBT]) with more free-flowing psychoanalytic techniques. This approach is based on several principles, including relinquishing a desire for a grand therapeutic arc, gaining comfort with silence, and, finally, allowing the patient to do the work.
Perhaps the most difficult part of this evolving realization is learning to resist the desire for an overarching path from session to session. As a novice therapist, I struggled with the apparent disconnect from session to session, and attempted to force this need for a therapeutic arc on each subsequent visit. This meant that rather than meeting the patient in his or her current state, I was forever reaching to the past, attempting to create a link between what was discussed previously to the topic of today’s session. While some patients readily identified with the concepts of CBT—where maladaptive cognitions are identified and challenged via reflection on past progress—there was another subset of patients who seemed unwilling to do so.
In his Notes On Memory and Desire,1 psychoanalyst Wilfred Bion proclaimed, “Do not remember past sessions.” As I discussed this concept in psychotherapy supervision, I began to understand the value of a less directed approach, and to try it with patients. I soon discovered interactions were more rewarding, and I gained a deeper understanding than I had before. Without a formulaic approach, patients were free to give voice to any issue, whether or not it conformed to their perceived “chief complaint.” It was refreshing to see the work progress over time as we began to slowly integrate the seemingly disparate themes of each session.
In addition to the naive idea of forcing a formulaic arc on the therapeutic process, I felt a strong desire for tangible results. Perhaps it was my engineering side yearning for the quantifiable, but nonetheless, I fell into the trap of trying to push patients to gain insights they may have not been ready to make. This led to dissatisfaction on both sides. I was reminded of another directive from Bion: “Desires for results, cure, or even understanding must not be allowed to proliferate.”1 It was interesting: the less I focused on results, the more patients began to open up and explore. By using their present experiences to examine patterns of behavior, we were able to slowly reach new levels of understanding.
The corollary to gaining comfort with relinquishing my desire for results was gaining comfort with silence and learning to meet patients where they are. The concept of using nonverbal cues to communicate is not a novel one. However, the idea that one might communicate by doing nothing at all is somewhat profound. I began to explore the use of silence with my patients, and have found an unknown richness that was previously hidden by my own tendency to interject. Psychotherapist Mark Epstein wrote, “When a therapist can sit with a patient without an agenda, without trying to force an experience, without thinking that she knows what is going to happen or who this person is…when he falls silent…the possibility of some real, spontaneous, unscripted communication exists.”2 Sitting in silence and allowing my patients to grow in their own insight has given them a sense of empowerment and mastery, and has greatly enriched our sessions.
Psychotherapy is not an easy thing for most embryonic psychiatrists or therapists, and many cling to formulaic methods because such methods are an easy approach. Initially, I, too, clung to this rigid approach, but it ultimately left me unfulfilled. I have learned to be more nimble, embrace silence, and relinquish my desire for results. I was initially uncomfortable with this unstructured model of psychotherapeutic interaction, preferring the more concrete thinking I had come to expect from engineering. It is likely that few residents will share this unique background, and thus may not struggle as I have, but I believe that the process of adaptation and change is relevant to all. As a young psychiatrist, I have gained much joy from being able to work with patients in psychotherapy. It is my hope that other young trainees, regardless of background, will learn to let go of their preconceived ideas and embrace change, for it is only through change that we grow.
1. Bion WR. Wilfred R. Bion: notes on memory and desire. In: Aguayo J, Malin B, eds. Wilfred Bion: Los Angeles seminars and supervision. London, UK: Karnac; 2013:136-138.
2. Epstein M. Remembering. In: Thoughts without a thinker. New York, NY: Basic Books; 1995:187-189.
There is a tendency among young psychiatric residents, including me, to experience significant anxiety when providing outpatient psychotherapy for the first time. This anxiety often leads to rigid adherence to structured sessions aimed at a specific therapeutic target. Unfortunately, as patients begin to stray from the mold, this model breaks down and leaves the resident with little direction.
As a resident with an engineering background, I felt a strong affinity for this targeted approach, and have struggled for direction with patients whose symptoms or willingness to engage therapeutically did not match this method. I have slowly come to appreciate a more nimble approach that balances elements of both a structured method (such as cognitive-behavioral therapy [CBT]) with more free-flowing psychoanalytic techniques. This approach is based on several principles, including relinquishing a desire for a grand therapeutic arc, gaining comfort with silence, and, finally, allowing the patient to do the work.
Perhaps the most difficult part of this evolving realization is learning to resist the desire for an overarching path from session to session. As a novice therapist, I struggled with the apparent disconnect from session to session, and attempted to force this need for a therapeutic arc on each subsequent visit. This meant that rather than meeting the patient in his or her current state, I was forever reaching to the past, attempting to create a link between what was discussed previously to the topic of today’s session. While some patients readily identified with the concepts of CBT—where maladaptive cognitions are identified and challenged via reflection on past progress—there was another subset of patients who seemed unwilling to do so.
In his Notes On Memory and Desire,1 psychoanalyst Wilfred Bion proclaimed, “Do not remember past sessions.” As I discussed this concept in psychotherapy supervision, I began to understand the value of a less directed approach, and to try it with patients. I soon discovered interactions were more rewarding, and I gained a deeper understanding than I had before. Without a formulaic approach, patients were free to give voice to any issue, whether or not it conformed to their perceived “chief complaint.” It was refreshing to see the work progress over time as we began to slowly integrate the seemingly disparate themes of each session.
In addition to the naive idea of forcing a formulaic arc on the therapeutic process, I felt a strong desire for tangible results. Perhaps it was my engineering side yearning for the quantifiable, but nonetheless, I fell into the trap of trying to push patients to gain insights they may have not been ready to make. This led to dissatisfaction on both sides. I was reminded of another directive from Bion: “Desires for results, cure, or even understanding must not be allowed to proliferate.”1 It was interesting: the less I focused on results, the more patients began to open up and explore. By using their present experiences to examine patterns of behavior, we were able to slowly reach new levels of understanding.
The corollary to gaining comfort with relinquishing my desire for results was gaining comfort with silence and learning to meet patients where they are. The concept of using nonverbal cues to communicate is not a novel one. However, the idea that one might communicate by doing nothing at all is somewhat profound. I began to explore the use of silence with my patients, and have found an unknown richness that was previously hidden by my own tendency to interject. Psychotherapist Mark Epstein wrote, “When a therapist can sit with a patient without an agenda, without trying to force an experience, without thinking that she knows what is going to happen or who this person is…when he falls silent…the possibility of some real, spontaneous, unscripted communication exists.”2 Sitting in silence and allowing my patients to grow in their own insight has given them a sense of empowerment and mastery, and has greatly enriched our sessions.
Psychotherapy is not an easy thing for most embryonic psychiatrists or therapists, and many cling to formulaic methods because such methods are an easy approach. Initially, I, too, clung to this rigid approach, but it ultimately left me unfulfilled. I have learned to be more nimble, embrace silence, and relinquish my desire for results. I was initially uncomfortable with this unstructured model of psychotherapeutic interaction, preferring the more concrete thinking I had come to expect from engineering. It is likely that few residents will share this unique background, and thus may not struggle as I have, but I believe that the process of adaptation and change is relevant to all. As a young psychiatrist, I have gained much joy from being able to work with patients in psychotherapy. It is my hope that other young trainees, regardless of background, will learn to let go of their preconceived ideas and embrace change, for it is only through change that we grow.
There is a tendency among young psychiatric residents, including me, to experience significant anxiety when providing outpatient psychotherapy for the first time. This anxiety often leads to rigid adherence to structured sessions aimed at a specific therapeutic target. Unfortunately, as patients begin to stray from the mold, this model breaks down and leaves the resident with little direction.
As a resident with an engineering background, I felt a strong affinity for this targeted approach, and have struggled for direction with patients whose symptoms or willingness to engage therapeutically did not match this method. I have slowly come to appreciate a more nimble approach that balances elements of both a structured method (such as cognitive-behavioral therapy [CBT]) with more free-flowing psychoanalytic techniques. This approach is based on several principles, including relinquishing a desire for a grand therapeutic arc, gaining comfort with silence, and, finally, allowing the patient to do the work.
Perhaps the most difficult part of this evolving realization is learning to resist the desire for an overarching path from session to session. As a novice therapist, I struggled with the apparent disconnect from session to session, and attempted to force this need for a therapeutic arc on each subsequent visit. This meant that rather than meeting the patient in his or her current state, I was forever reaching to the past, attempting to create a link between what was discussed previously to the topic of today’s session. While some patients readily identified with the concepts of CBT—where maladaptive cognitions are identified and challenged via reflection on past progress—there was another subset of patients who seemed unwilling to do so.
In his Notes On Memory and Desire,1 psychoanalyst Wilfred Bion proclaimed, “Do not remember past sessions.” As I discussed this concept in psychotherapy supervision, I began to understand the value of a less directed approach, and to try it with patients. I soon discovered interactions were more rewarding, and I gained a deeper understanding than I had before. Without a formulaic approach, patients were free to give voice to any issue, whether or not it conformed to their perceived “chief complaint.” It was refreshing to see the work progress over time as we began to slowly integrate the seemingly disparate themes of each session.
In addition to the naive idea of forcing a formulaic arc on the therapeutic process, I felt a strong desire for tangible results. Perhaps it was my engineering side yearning for the quantifiable, but nonetheless, I fell into the trap of trying to push patients to gain insights they may have not been ready to make. This led to dissatisfaction on both sides. I was reminded of another directive from Bion: “Desires for results, cure, or even understanding must not be allowed to proliferate.”1 It was interesting: the less I focused on results, the more patients began to open up and explore. By using their present experiences to examine patterns of behavior, we were able to slowly reach new levels of understanding.
The corollary to gaining comfort with relinquishing my desire for results was gaining comfort with silence and learning to meet patients where they are. The concept of using nonverbal cues to communicate is not a novel one. However, the idea that one might communicate by doing nothing at all is somewhat profound. I began to explore the use of silence with my patients, and have found an unknown richness that was previously hidden by my own tendency to interject. Psychotherapist Mark Epstein wrote, “When a therapist can sit with a patient without an agenda, without trying to force an experience, without thinking that she knows what is going to happen or who this person is…when he falls silent…the possibility of some real, spontaneous, unscripted communication exists.”2 Sitting in silence and allowing my patients to grow in their own insight has given them a sense of empowerment and mastery, and has greatly enriched our sessions.
Psychotherapy is not an easy thing for most embryonic psychiatrists or therapists, and many cling to formulaic methods because such methods are an easy approach. Initially, I, too, clung to this rigid approach, but it ultimately left me unfulfilled. I have learned to be more nimble, embrace silence, and relinquish my desire for results. I was initially uncomfortable with this unstructured model of psychotherapeutic interaction, preferring the more concrete thinking I had come to expect from engineering. It is likely that few residents will share this unique background, and thus may not struggle as I have, but I believe that the process of adaptation and change is relevant to all. As a young psychiatrist, I have gained much joy from being able to work with patients in psychotherapy. It is my hope that other young trainees, regardless of background, will learn to let go of their preconceived ideas and embrace change, for it is only through change that we grow.
1. Bion WR. Wilfred R. Bion: notes on memory and desire. In: Aguayo J, Malin B, eds. Wilfred Bion: Los Angeles seminars and supervision. London, UK: Karnac; 2013:136-138.
2. Epstein M. Remembering. In: Thoughts without a thinker. New York, NY: Basic Books; 1995:187-189.
1. Bion WR. Wilfred R. Bion: notes on memory and desire. In: Aguayo J, Malin B, eds. Wilfred Bion: Los Angeles seminars and supervision. London, UK: Karnac; 2013:136-138.
2. Epstein M. Remembering. In: Thoughts without a thinker. New York, NY: Basic Books; 1995:187-189.
Was this your first one? Lessons in empathy and mourning
“Was this your first one?”
You might be asked this question in several circumstances. Was this your first 5K run? Was this your first time taking the MCAT? For me, I was asked if this was the first time a patient had died while in my care as a resident.
As it turns out, this was the first patient who died under my care. This seemed obvious to everyone around me because when I received the news, offhandedly, days after my patient’s discharge, I cried. My colleagues’ responses to my tears were kind and supportive. No one was callous or judgmental. I was given time to compose myself before continuing my rounds for the day. Yet, the most common question asked of me was, “Was this your first one?”
The implication of this question was that these situations would become easier and less emotional over time. Everyone believed my tears were a special response, privileged only to my first experience. This was conveyed to me as if it was a chance to explain my emotions. As if grieving alone was not sufficient to explain tears, I began to run through the reasons for my behavior, and my mind rapidly searched for answers. I thought:
- “I saw this patient daily for weeks, and I was close to him.”
- “There was an element of suicidality in this case, so it was different.”
- “After all, this was my first experience like this.”
In reality, these reasons were irrelevant and not needed to explain my tears. I was mourning the loss of a life—someone I had come to know well—and this was a life that ultimately could not be saved by the health care system.
These were my feelings during the July of my intern year. It is now a year later; I have since experienced an incredible number of moments that warranted mourning. There were oncology patients with advanced diseases who needed help disclosing their prognosis to family members. There were days when I was tasked with altering treatment courses from aggressive treatment to comfort measures only. There was the Christmas Eve when a pair of brothers dropped off their elderly father in the emergency department because no one was able or willing to care for him at home.
These moments can come fast, and they occur more frequently than one might imagine. Each is worthy of mourning. Each is worthy of tears, whether it is my first loss or my 50th. But the reality is that I could not function in my job and care for all my patients equally if I stopped every time to acknowledge my emotions. As much as it causes my stomach to turn, I understand the “Was this your first one?” phenomenon. To outwardly express your emotions and openly mourn in the moment, you need to have the time and allow yourself the vulnerability to do so. After your “first one,” you realize that mournful moments can occur regularly and you must choose to process emotions on your own time because you don’t have the luxury of processing a loss of life in the present moment.
Continue to: This is not to diminish...
This is not to diminish the importance of mourning or belittle the experience of processing one’s emotions. It simply highlights the importance of self-care. Emotions need to be processed outside of the hustle and bustle of the work day. There are other patients who require and deserve their clinician’s undivided attention. To truly provide patients with the highest quality of care, I find caring for myself and processing my reactions to daily events to be essential. Writing down my thoughts or talking to loved ones are ways that help me process my experiences. Taking a trip out of town, going for a hike, or watching a movie also are ways to help create balance in an emotionally charged career. I hope to use my new understanding of the “first one” phenomenon as a reminder to maintain my own well-being. In doing so, I can be attuned to my patients’ needs and provide them with empathic care. Even though my outward expression may change as I learn to process these moments differently, I want to treat each patient with the same level of empathy, value, and compassion as my first one.
“Was this your first one?”
You might be asked this question in several circumstances. Was this your first 5K run? Was this your first time taking the MCAT? For me, I was asked if this was the first time a patient had died while in my care as a resident.
As it turns out, this was the first patient who died under my care. This seemed obvious to everyone around me because when I received the news, offhandedly, days after my patient’s discharge, I cried. My colleagues’ responses to my tears were kind and supportive. No one was callous or judgmental. I was given time to compose myself before continuing my rounds for the day. Yet, the most common question asked of me was, “Was this your first one?”
The implication of this question was that these situations would become easier and less emotional over time. Everyone believed my tears were a special response, privileged only to my first experience. This was conveyed to me as if it was a chance to explain my emotions. As if grieving alone was not sufficient to explain tears, I began to run through the reasons for my behavior, and my mind rapidly searched for answers. I thought:
- “I saw this patient daily for weeks, and I was close to him.”
- “There was an element of suicidality in this case, so it was different.”
- “After all, this was my first experience like this.”
In reality, these reasons were irrelevant and not needed to explain my tears. I was mourning the loss of a life—someone I had come to know well—and this was a life that ultimately could not be saved by the health care system.
These were my feelings during the July of my intern year. It is now a year later; I have since experienced an incredible number of moments that warranted mourning. There were oncology patients with advanced diseases who needed help disclosing their prognosis to family members. There were days when I was tasked with altering treatment courses from aggressive treatment to comfort measures only. There was the Christmas Eve when a pair of brothers dropped off their elderly father in the emergency department because no one was able or willing to care for him at home.
These moments can come fast, and they occur more frequently than one might imagine. Each is worthy of mourning. Each is worthy of tears, whether it is my first loss or my 50th. But the reality is that I could not function in my job and care for all my patients equally if I stopped every time to acknowledge my emotions. As much as it causes my stomach to turn, I understand the “Was this your first one?” phenomenon. To outwardly express your emotions and openly mourn in the moment, you need to have the time and allow yourself the vulnerability to do so. After your “first one,” you realize that mournful moments can occur regularly and you must choose to process emotions on your own time because you don’t have the luxury of processing a loss of life in the present moment.
Continue to: This is not to diminish...
This is not to diminish the importance of mourning or belittle the experience of processing one’s emotions. It simply highlights the importance of self-care. Emotions need to be processed outside of the hustle and bustle of the work day. There are other patients who require and deserve their clinician’s undivided attention. To truly provide patients with the highest quality of care, I find caring for myself and processing my reactions to daily events to be essential. Writing down my thoughts or talking to loved ones are ways that help me process my experiences. Taking a trip out of town, going for a hike, or watching a movie also are ways to help create balance in an emotionally charged career. I hope to use my new understanding of the “first one” phenomenon as a reminder to maintain my own well-being. In doing so, I can be attuned to my patients’ needs and provide them with empathic care. Even though my outward expression may change as I learn to process these moments differently, I want to treat each patient with the same level of empathy, value, and compassion as my first one.
“Was this your first one?”
You might be asked this question in several circumstances. Was this your first 5K run? Was this your first time taking the MCAT? For me, I was asked if this was the first time a patient had died while in my care as a resident.
As it turns out, this was the first patient who died under my care. This seemed obvious to everyone around me because when I received the news, offhandedly, days after my patient’s discharge, I cried. My colleagues’ responses to my tears were kind and supportive. No one was callous or judgmental. I was given time to compose myself before continuing my rounds for the day. Yet, the most common question asked of me was, “Was this your first one?”
The implication of this question was that these situations would become easier and less emotional over time. Everyone believed my tears were a special response, privileged only to my first experience. This was conveyed to me as if it was a chance to explain my emotions. As if grieving alone was not sufficient to explain tears, I began to run through the reasons for my behavior, and my mind rapidly searched for answers. I thought:
- “I saw this patient daily for weeks, and I was close to him.”
- “There was an element of suicidality in this case, so it was different.”
- “After all, this was my first experience like this.”
In reality, these reasons were irrelevant and not needed to explain my tears. I was mourning the loss of a life—someone I had come to know well—and this was a life that ultimately could not be saved by the health care system.
These were my feelings during the July of my intern year. It is now a year later; I have since experienced an incredible number of moments that warranted mourning. There were oncology patients with advanced diseases who needed help disclosing their prognosis to family members. There were days when I was tasked with altering treatment courses from aggressive treatment to comfort measures only. There was the Christmas Eve when a pair of brothers dropped off their elderly father in the emergency department because no one was able or willing to care for him at home.
These moments can come fast, and they occur more frequently than one might imagine. Each is worthy of mourning. Each is worthy of tears, whether it is my first loss or my 50th. But the reality is that I could not function in my job and care for all my patients equally if I stopped every time to acknowledge my emotions. As much as it causes my stomach to turn, I understand the “Was this your first one?” phenomenon. To outwardly express your emotions and openly mourn in the moment, you need to have the time and allow yourself the vulnerability to do so. After your “first one,” you realize that mournful moments can occur regularly and you must choose to process emotions on your own time because you don’t have the luxury of processing a loss of life in the present moment.
Continue to: This is not to diminish...
This is not to diminish the importance of mourning or belittle the experience of processing one’s emotions. It simply highlights the importance of self-care. Emotions need to be processed outside of the hustle and bustle of the work day. There are other patients who require and deserve their clinician’s undivided attention. To truly provide patients with the highest quality of care, I find caring for myself and processing my reactions to daily events to be essential. Writing down my thoughts or talking to loved ones are ways that help me process my experiences. Taking a trip out of town, going for a hike, or watching a movie also are ways to help create balance in an emotionally charged career. I hope to use my new understanding of the “first one” phenomenon as a reminder to maintain my own well-being. In doing so, I can be attuned to my patients’ needs and provide them with empathic care. Even though my outward expression may change as I learn to process these moments differently, I want to treat each patient with the same level of empathy, value, and compassion as my first one.
Yoga’s lesson for a young psychiatrist
I have often turned to yoga for my own reprieve; I find the heat, breath, and movement exhilarating. Training to become a yoga teacher has taught me that medicine, not unlike yoga, requires patience and resiliency.
It is 3
4
Let me tell you, when you’re getting certified in Advanced Cardiac Life Support, you go to a class on a Saturday, there are snacks, and your instructor will probably be a paramedic who is earning side cash teaching CPR. You will watch funny videos—we even danced to the Bee Gees’ Stayin’ Alive. But this is not funny, nor is it fun. And my head is spinning so fast, the sound of the Bee Gees smears to silence.
I take off my white coat and trot to the center of the room. The lights are bright, I am hot, and people are moving really fast. I feel like I’m in a vignette. It seems like we’re in the fourth movement of a Shostakovich symphony, the attending is cueing, up and down, like Bernstein conducting the Philharmonic, her arms are flailing; this production is hers and everyone is in sync. The man’s skin is pale, almost gray, he smells like sweat and urine and vomit. His irises are blue, blue like the ocean. His beard is thick and opaque, speckled with premature dots of gray. He looks calm. Listless. Dead. He is looking at me, like the Mona Lisa, as if beckoning me to save him, to give him another chance. At life. I put my hands gently on his sternum and I start my round of chest compressions. His skin is rubbery. I feel like I’m breaking his ribs, am I? This is not like the class. The cardiac monitor flatlines. Was it like that before? I think so, I’m not really sure. The attending stops conducting and runs over. Someone taps me and says it’s time to switch. Shortly thereafter, time of death is pronounced. “Damn it,” I hear the attending exclaim quietly but deliberately. I am hot, and I have a headache. I take off my gloves. Where’s my cell phone? I’m going to check Facebook, maybe ESPN.com. I feel heavy. And then I’m sitting at the computer screen again, after the rain. The attending comes back to her seat. She has a green smoothie, she takes a sip, and is slow to return the oversized cup to the table.
This night 3 years ago remains vivid. I am looking at her now. The unabashed attending. We are all looking at her.
She pulls out a petite makeup case and opens an oval mirror. She applies 2 thin lines of lustrous lip gloss, smacks her lips, grounding herself, then places the mirror back in her bag. She takes one deep breath, pauses briefly, and, letting go, she sits up tall, her dignity restored, then looks at me and claps, “Come on, doctor, we’ve got more patients to see.”
That night in the ER, I experienced how troubling it is losing a life with the burden of responsibility, but also the beauty of Aparigraha, letting go, and moving forward. I learned this lesson, unspoken, from an admirable attending, and was reminded of it 3 years later as I pursued a deeper understanding of yoga.
I have often turned to yoga for my own reprieve; I find the heat, breath, and movement exhilarating. Training to become a yoga teacher has taught me that medicine, not unlike yoga, requires patience and resiliency.
It is 3
4
Let me tell you, when you’re getting certified in Advanced Cardiac Life Support, you go to a class on a Saturday, there are snacks, and your instructor will probably be a paramedic who is earning side cash teaching CPR. You will watch funny videos—we even danced to the Bee Gees’ Stayin’ Alive. But this is not funny, nor is it fun. And my head is spinning so fast, the sound of the Bee Gees smears to silence.
I take off my white coat and trot to the center of the room. The lights are bright, I am hot, and people are moving really fast. I feel like I’m in a vignette. It seems like we’re in the fourth movement of a Shostakovich symphony, the attending is cueing, up and down, like Bernstein conducting the Philharmonic, her arms are flailing; this production is hers and everyone is in sync. The man’s skin is pale, almost gray, he smells like sweat and urine and vomit. His irises are blue, blue like the ocean. His beard is thick and opaque, speckled with premature dots of gray. He looks calm. Listless. Dead. He is looking at me, like the Mona Lisa, as if beckoning me to save him, to give him another chance. At life. I put my hands gently on his sternum and I start my round of chest compressions. His skin is rubbery. I feel like I’m breaking his ribs, am I? This is not like the class. The cardiac monitor flatlines. Was it like that before? I think so, I’m not really sure. The attending stops conducting and runs over. Someone taps me and says it’s time to switch. Shortly thereafter, time of death is pronounced. “Damn it,” I hear the attending exclaim quietly but deliberately. I am hot, and I have a headache. I take off my gloves. Where’s my cell phone? I’m going to check Facebook, maybe ESPN.com. I feel heavy. And then I’m sitting at the computer screen again, after the rain. The attending comes back to her seat. She has a green smoothie, she takes a sip, and is slow to return the oversized cup to the table.
This night 3 years ago remains vivid. I am looking at her now. The unabashed attending. We are all looking at her.
She pulls out a petite makeup case and opens an oval mirror. She applies 2 thin lines of lustrous lip gloss, smacks her lips, grounding herself, then places the mirror back in her bag. She takes one deep breath, pauses briefly, and, letting go, she sits up tall, her dignity restored, then looks at me and claps, “Come on, doctor, we’ve got more patients to see.”
That night in the ER, I experienced how troubling it is losing a life with the burden of responsibility, but also the beauty of Aparigraha, letting go, and moving forward. I learned this lesson, unspoken, from an admirable attending, and was reminded of it 3 years later as I pursued a deeper understanding of yoga.
I have often turned to yoga for my own reprieve; I find the heat, breath, and movement exhilarating. Training to become a yoga teacher has taught me that medicine, not unlike yoga, requires patience and resiliency.
It is 3
4
Let me tell you, when you’re getting certified in Advanced Cardiac Life Support, you go to a class on a Saturday, there are snacks, and your instructor will probably be a paramedic who is earning side cash teaching CPR. You will watch funny videos—we even danced to the Bee Gees’ Stayin’ Alive. But this is not funny, nor is it fun. And my head is spinning so fast, the sound of the Bee Gees smears to silence.
I take off my white coat and trot to the center of the room. The lights are bright, I am hot, and people are moving really fast. I feel like I’m in a vignette. It seems like we’re in the fourth movement of a Shostakovich symphony, the attending is cueing, up and down, like Bernstein conducting the Philharmonic, her arms are flailing; this production is hers and everyone is in sync. The man’s skin is pale, almost gray, he smells like sweat and urine and vomit. His irises are blue, blue like the ocean. His beard is thick and opaque, speckled with premature dots of gray. He looks calm. Listless. Dead. He is looking at me, like the Mona Lisa, as if beckoning me to save him, to give him another chance. At life. I put my hands gently on his sternum and I start my round of chest compressions. His skin is rubbery. I feel like I’m breaking his ribs, am I? This is not like the class. The cardiac monitor flatlines. Was it like that before? I think so, I’m not really sure. The attending stops conducting and runs over. Someone taps me and says it’s time to switch. Shortly thereafter, time of death is pronounced. “Damn it,” I hear the attending exclaim quietly but deliberately. I am hot, and I have a headache. I take off my gloves. Where’s my cell phone? I’m going to check Facebook, maybe ESPN.com. I feel heavy. And then I’m sitting at the computer screen again, after the rain. The attending comes back to her seat. She has a green smoothie, she takes a sip, and is slow to return the oversized cup to the table.
This night 3 years ago remains vivid. I am looking at her now. The unabashed attending. We are all looking at her.
She pulls out a petite makeup case and opens an oval mirror. She applies 2 thin lines of lustrous lip gloss, smacks her lips, grounding herself, then places the mirror back in her bag. She takes one deep breath, pauses briefly, and, letting go, she sits up tall, her dignity restored, then looks at me and claps, “Come on, doctor, we’ve got more patients to see.”
That night in the ER, I experienced how troubling it is losing a life with the burden of responsibility, but also the beauty of Aparigraha, letting go, and moving forward. I learned this lesson, unspoken, from an admirable attending, and was reminded of it 3 years later as I pursued a deeper understanding of yoga.
Diagnosed with a chronic illness: Should you tell your patients?
Physicians are not immune to chronic illness. Those who choose to continue working after being diagnosed with a chronic illness need to decide whether or not to tell their patients. The idea of physicians being a “blank slate” to their patients would be challenged by such self-disclosure. But ignoring an obvious change in the therapeutic space could be detrimental to your patient’s therapy.1 Every patient has his or her own ideas or perceptions about their physician that contribute to how likely they are to continue to engage in therapy or take prescribed medications. Could letting your patients know you have a chronic illness threaten the image they have of you, and potentially jeopardize their treatment?
Physician factors
Once diagnosed with a chronic illness, a physician who previously defined his or her identity as a clinician now must also assume the role of a patient. This transition gives rise to anxiety. Patient encounters may give a physician the opportunity to feel safe to discuss such anxiety.2 However, patients often view their physicians as omnipotent. When their physician admits weakness and vulnerability, that perception may be damaged.3 This damage could manifest as medication nonadherence, missed appointments, or even termination of treatment. A fear of such abandonment may lead a physician to not disclose his or her illness. To avoid discussing this uncomfortable topic, a physician might be more defensive in his or her interactions with the patient.2
Patient factors
Every patient presents with unique characteristics that contribute to the patient–physician relationship. Receiving news that one’s physician has a chronic or severe illness will elicit different reactions in each patient. These reactions will vary depending upon the patient’s pathology, stage of treatment, and background.3 The previous work done between the patient and physician is crucial in predicting the treatment course after the physician discloses that he or she has a chronic illness. Also, patients may notice the physical changes of their physician’s illness. Deciding to disclose—or to not disclose—something that is obvious can elicit feelings of worry, anger, or even triumph in the patient.3
CASES
Two patients, two different responses
Dr. T recently was diagnosed with leukemia and has begun to receive treatment. He decides to continue working. Since receiving the diagnosis, he finds himself more anxious. Adding to his anxiety is the question of whether or not he should tell his patients about his diagnosis. He decides to tell 2 of his patients—Mr. G and Ms. N—and receives a drastically different response from each of them.
Mr. G, age 45, has been Dr. T’s patient for 2 years. He is married, has 2 children, and works at a car dealership. Mr. G initially presented for treatment of depressive symptoms after his mother died. Those symptoms were stabilized with medicatio
Dr. T discloses the news of his illness to Mr. G at their next appointment. Mr. G offers his condolences and speaks about how on one hand, he is sympathetic and wishes to be supportive, but on the other hand, he fears another loss in his life. Mr. G thanks Dr. T for disclosing this news and hopes they can begin to discuss this situation in therapy. He remains compliant with appointments.
Ms. N, age 59, has been Dr. T’s patient for 6 months. She was diagnosed with schizophrenia when she was in her early 20s. She is single, unemployed, lives alone, and lacks social support. Ms. N has a history of multiple hospitalizations. She has a pattern of presenting to an emergency department and asking to be admitted whenever she faces an acute stressor.
Continue to: Ms. N came to Dr. T through another psychiatrist...
Ms. N came to Dr. T through another psychiatrist and Dr. T continues to provide medication management. He has implemented a biweekly appointment schedule for supportive therapy to work on Ms. N’s personal goals to cook more, clean her house, and lose weight. They also address issues regarding her father and his absence in her life since she was age 18.
During their next appointment, Dr. T discloses the news of his illness to Ms. N. Ms. N asks, “Are you sure?” Dr. T confirms and asks her how she feels about this news. She replies, “It’s fine.” Soon after, she stops attending her biweekly appointments and is lost to follow-up.
Consider your patient’s ability to cope
Dr. T faced the challenge of whether to disclose his diagnosis to his patients. He understood the potential implications on his therapeutic work and his battles with his own anxiety. Ultimately, he decided to tell his patients, but he did not consider how they might have been able to handle such news.
Mr. G was receptive to the news and remained engaged in treatment after learning of Dr. T’s illness. His ability to do so likely was the result of many factors. Mr. G is a high-functioning individual who seems to have a secure attachment style. He is able to express his conflicts. He has had good relationships in his life, was able to work through his mother’s death, and is engaged in treatment to help him cope with the inevitable loss of his father. Mr. G can handle the potential loss of his physician because he has shown his ability to cope with such losses in his life.
Continue to: On the other hand...
On the other hand, although Ms. N stated that the news of Dr. T’s diagnosis was “fine,” she was soon lost to follow-up, which suggests she was unable to handle the news. This is supported by her history of unstable relationships. Her insecure attachment style likely contributed to her inability to handle stressors, as evidenced by her frequent requests for admission. Dr. T also should have considered the possibility of transference, given that Ms. N struggled with abandonment by her father. Dr. T’s potential departure could represent such abandonment. In a patient such as Ms. N, being upfront about having a chronic illness would be more harmful than beneficial.
Maintain a patient-focused view
Receiving a diagnosis of a severe or chronic illness can be extremely stressful for physicians. Adopting the new identity of patient in addition to that of physician can cause tremendous anxiety. If you decide to continue working with your patients, it is crucial to be mindful of this anxiety and its potential to influence your decision to disclose your diagnosis to your patients. Do not allow your anxiety to contaminate the therapeutic work. Maintaining a patient-focused view of treatment will allow you to determine each patient’s ability to process disclosure vs nondisclosure of your diagnosis. Ultimately, this will help determine which patients you should tell, and which ones you should not.
1. Abend SM. Serious illness in the analyst: countertransference considerations. J Am Psychoanal Assoc. 1982;30(2):365-379.
2. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
3. Torrigiani MG, Marzi A. When the analyst is physically ill: vicissitudes in the analytical relationship. Int J Psychoanal. 2005;86(pt 5):1373-1389.
Physicians are not immune to chronic illness. Those who choose to continue working after being diagnosed with a chronic illness need to decide whether or not to tell their patients. The idea of physicians being a “blank slate” to their patients would be challenged by such self-disclosure. But ignoring an obvious change in the therapeutic space could be detrimental to your patient’s therapy.1 Every patient has his or her own ideas or perceptions about their physician that contribute to how likely they are to continue to engage in therapy or take prescribed medications. Could letting your patients know you have a chronic illness threaten the image they have of you, and potentially jeopardize their treatment?
Physician factors
Once diagnosed with a chronic illness, a physician who previously defined his or her identity as a clinician now must also assume the role of a patient. This transition gives rise to anxiety. Patient encounters may give a physician the opportunity to feel safe to discuss such anxiety.2 However, patients often view their physicians as omnipotent. When their physician admits weakness and vulnerability, that perception may be damaged.3 This damage could manifest as medication nonadherence, missed appointments, or even termination of treatment. A fear of such abandonment may lead a physician to not disclose his or her illness. To avoid discussing this uncomfortable topic, a physician might be more defensive in his or her interactions with the patient.2
Patient factors
Every patient presents with unique characteristics that contribute to the patient–physician relationship. Receiving news that one’s physician has a chronic or severe illness will elicit different reactions in each patient. These reactions will vary depending upon the patient’s pathology, stage of treatment, and background.3 The previous work done between the patient and physician is crucial in predicting the treatment course after the physician discloses that he or she has a chronic illness. Also, patients may notice the physical changes of their physician’s illness. Deciding to disclose—or to not disclose—something that is obvious can elicit feelings of worry, anger, or even triumph in the patient.3
CASES
Two patients, two different responses
Dr. T recently was diagnosed with leukemia and has begun to receive treatment. He decides to continue working. Since receiving the diagnosis, he finds himself more anxious. Adding to his anxiety is the question of whether or not he should tell his patients about his diagnosis. He decides to tell 2 of his patients—Mr. G and Ms. N—and receives a drastically different response from each of them.
Mr. G, age 45, has been Dr. T’s patient for 2 years. He is married, has 2 children, and works at a car dealership. Mr. G initially presented for treatment of depressive symptoms after his mother died. Those symptoms were stabilized with medicatio
Dr. T discloses the news of his illness to Mr. G at their next appointment. Mr. G offers his condolences and speaks about how on one hand, he is sympathetic and wishes to be supportive, but on the other hand, he fears another loss in his life. Mr. G thanks Dr. T for disclosing this news and hopes they can begin to discuss this situation in therapy. He remains compliant with appointments.
Ms. N, age 59, has been Dr. T’s patient for 6 months. She was diagnosed with schizophrenia when she was in her early 20s. She is single, unemployed, lives alone, and lacks social support. Ms. N has a history of multiple hospitalizations. She has a pattern of presenting to an emergency department and asking to be admitted whenever she faces an acute stressor.
Continue to: Ms. N came to Dr. T through another psychiatrist...
Ms. N came to Dr. T through another psychiatrist and Dr. T continues to provide medication management. He has implemented a biweekly appointment schedule for supportive therapy to work on Ms. N’s personal goals to cook more, clean her house, and lose weight. They also address issues regarding her father and his absence in her life since she was age 18.
During their next appointment, Dr. T discloses the news of his illness to Ms. N. Ms. N asks, “Are you sure?” Dr. T confirms and asks her how she feels about this news. She replies, “It’s fine.” Soon after, she stops attending her biweekly appointments and is lost to follow-up.
Consider your patient’s ability to cope
Dr. T faced the challenge of whether to disclose his diagnosis to his patients. He understood the potential implications on his therapeutic work and his battles with his own anxiety. Ultimately, he decided to tell his patients, but he did not consider how they might have been able to handle such news.
Mr. G was receptive to the news and remained engaged in treatment after learning of Dr. T’s illness. His ability to do so likely was the result of many factors. Mr. G is a high-functioning individual who seems to have a secure attachment style. He is able to express his conflicts. He has had good relationships in his life, was able to work through his mother’s death, and is engaged in treatment to help him cope with the inevitable loss of his father. Mr. G can handle the potential loss of his physician because he has shown his ability to cope with such losses in his life.
Continue to: On the other hand...
On the other hand, although Ms. N stated that the news of Dr. T’s diagnosis was “fine,” she was soon lost to follow-up, which suggests she was unable to handle the news. This is supported by her history of unstable relationships. Her insecure attachment style likely contributed to her inability to handle stressors, as evidenced by her frequent requests for admission. Dr. T also should have considered the possibility of transference, given that Ms. N struggled with abandonment by her father. Dr. T’s potential departure could represent such abandonment. In a patient such as Ms. N, being upfront about having a chronic illness would be more harmful than beneficial.
Maintain a patient-focused view
Receiving a diagnosis of a severe or chronic illness can be extremely stressful for physicians. Adopting the new identity of patient in addition to that of physician can cause tremendous anxiety. If you decide to continue working with your patients, it is crucial to be mindful of this anxiety and its potential to influence your decision to disclose your diagnosis to your patients. Do not allow your anxiety to contaminate the therapeutic work. Maintaining a patient-focused view of treatment will allow you to determine each patient’s ability to process disclosure vs nondisclosure of your diagnosis. Ultimately, this will help determine which patients you should tell, and which ones you should not.
Physicians are not immune to chronic illness. Those who choose to continue working after being diagnosed with a chronic illness need to decide whether or not to tell their patients. The idea of physicians being a “blank slate” to their patients would be challenged by such self-disclosure. But ignoring an obvious change in the therapeutic space could be detrimental to your patient’s therapy.1 Every patient has his or her own ideas or perceptions about their physician that contribute to how likely they are to continue to engage in therapy or take prescribed medications. Could letting your patients know you have a chronic illness threaten the image they have of you, and potentially jeopardize their treatment?
Physician factors
Once diagnosed with a chronic illness, a physician who previously defined his or her identity as a clinician now must also assume the role of a patient. This transition gives rise to anxiety. Patient encounters may give a physician the opportunity to feel safe to discuss such anxiety.2 However, patients often view their physicians as omnipotent. When their physician admits weakness and vulnerability, that perception may be damaged.3 This damage could manifest as medication nonadherence, missed appointments, or even termination of treatment. A fear of such abandonment may lead a physician to not disclose his or her illness. To avoid discussing this uncomfortable topic, a physician might be more defensive in his or her interactions with the patient.2
Patient factors
Every patient presents with unique characteristics that contribute to the patient–physician relationship. Receiving news that one’s physician has a chronic or severe illness will elicit different reactions in each patient. These reactions will vary depending upon the patient’s pathology, stage of treatment, and background.3 The previous work done between the patient and physician is crucial in predicting the treatment course after the physician discloses that he or she has a chronic illness. Also, patients may notice the physical changes of their physician’s illness. Deciding to disclose—or to not disclose—something that is obvious can elicit feelings of worry, anger, or even triumph in the patient.3
CASES
Two patients, two different responses
Dr. T recently was diagnosed with leukemia and has begun to receive treatment. He decides to continue working. Since receiving the diagnosis, he finds himself more anxious. Adding to his anxiety is the question of whether or not he should tell his patients about his diagnosis. He decides to tell 2 of his patients—Mr. G and Ms. N—and receives a drastically different response from each of them.
Mr. G, age 45, has been Dr. T’s patient for 2 years. He is married, has 2 children, and works at a car dealership. Mr. G initially presented for treatment of depressive symptoms after his mother died. Those symptoms were stabilized with medicatio
Dr. T discloses the news of his illness to Mr. G at their next appointment. Mr. G offers his condolences and speaks about how on one hand, he is sympathetic and wishes to be supportive, but on the other hand, he fears another loss in his life. Mr. G thanks Dr. T for disclosing this news and hopes they can begin to discuss this situation in therapy. He remains compliant with appointments.
Ms. N, age 59, has been Dr. T’s patient for 6 months. She was diagnosed with schizophrenia when she was in her early 20s. She is single, unemployed, lives alone, and lacks social support. Ms. N has a history of multiple hospitalizations. She has a pattern of presenting to an emergency department and asking to be admitted whenever she faces an acute stressor.
Continue to: Ms. N came to Dr. T through another psychiatrist...
Ms. N came to Dr. T through another psychiatrist and Dr. T continues to provide medication management. He has implemented a biweekly appointment schedule for supportive therapy to work on Ms. N’s personal goals to cook more, clean her house, and lose weight. They also address issues regarding her father and his absence in her life since she was age 18.
During their next appointment, Dr. T discloses the news of his illness to Ms. N. Ms. N asks, “Are you sure?” Dr. T confirms and asks her how she feels about this news. She replies, “It’s fine.” Soon after, she stops attending her biweekly appointments and is lost to follow-up.
Consider your patient’s ability to cope
Dr. T faced the challenge of whether to disclose his diagnosis to his patients. He understood the potential implications on his therapeutic work and his battles with his own anxiety. Ultimately, he decided to tell his patients, but he did not consider how they might have been able to handle such news.
Mr. G was receptive to the news and remained engaged in treatment after learning of Dr. T’s illness. His ability to do so likely was the result of many factors. Mr. G is a high-functioning individual who seems to have a secure attachment style. He is able to express his conflicts. He has had good relationships in his life, was able to work through his mother’s death, and is engaged in treatment to help him cope with the inevitable loss of his father. Mr. G can handle the potential loss of his physician because he has shown his ability to cope with such losses in his life.
Continue to: On the other hand...
On the other hand, although Ms. N stated that the news of Dr. T’s diagnosis was “fine,” she was soon lost to follow-up, which suggests she was unable to handle the news. This is supported by her history of unstable relationships. Her insecure attachment style likely contributed to her inability to handle stressors, as evidenced by her frequent requests for admission. Dr. T also should have considered the possibility of transference, given that Ms. N struggled with abandonment by her father. Dr. T’s potential departure could represent such abandonment. In a patient such as Ms. N, being upfront about having a chronic illness would be more harmful than beneficial.
Maintain a patient-focused view
Receiving a diagnosis of a severe or chronic illness can be extremely stressful for physicians. Adopting the new identity of patient in addition to that of physician can cause tremendous anxiety. If you decide to continue working with your patients, it is crucial to be mindful of this anxiety and its potential to influence your decision to disclose your diagnosis to your patients. Do not allow your anxiety to contaminate the therapeutic work. Maintaining a patient-focused view of treatment will allow you to determine each patient’s ability to process disclosure vs nondisclosure of your diagnosis. Ultimately, this will help determine which patients you should tell, and which ones you should not.
1. Abend SM. Serious illness in the analyst: countertransference considerations. J Am Psychoanal Assoc. 1982;30(2):365-379.
2. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
3. Torrigiani MG, Marzi A. When the analyst is physically ill: vicissitudes in the analytical relationship. Int J Psychoanal. 2005;86(pt 5):1373-1389.
1. Abend SM. Serious illness in the analyst: countertransference considerations. J Am Psychoanal Assoc. 1982;30(2):365-379.
2. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
3. Torrigiani MG, Marzi A. When the analyst is physically ill: vicissitudes in the analytical relationship. Int J Psychoanal. 2005;86(pt 5):1373-1389.