User login
ADHD: Putting the Pieces Together
CE/CME No: CR-1501
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain the attention-deficit/hyperactivity disorder (ADHD) diagnostic criteria of inattention, hyperactivity, and/or impulsivity as defined in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR), and the DSM-5 update.
• Discuss the American Academy of Pediatrics clinical practice guideline for evaluation, diagnosis, treatment, and monitoring of children and adolescents with ADHD.
• Describe the classes of medications available to treat ADHD, the indications for each, and the forms available (eg, short- versus long-acting, tablets, capsules, patches, liquids).
• Identify environmental factors at home and in school that can affect a child’s ADHD and know how to address them.
• Understand and provide support for the parent’s role in managing a child’s ADHD.
FACULTY
Amy Chandler is a family nurse practitioner at Peninsula Surgical Group in Salisbury, Maryland. Mary Parsons is an Assistant Professor at the University of Maryland School of Nursing in Baltimore. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.25 hours of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of January 2015.
Article begins on next page >>
Hyperactivity, impulsivity, disruptive behavior, lack of focus—the symptoms of attention-deficit/hyperactivity disorder can negatively impact children and their families. Primary care providers have the opportunity to bring a semblance of order to chaos, and improve quality of life for all involved, by identifying affected patients and providing effective treatment options. Here is everything you need to know.
Attention-deficit/hyperactivity disorder (ADHD) is a diagnosis on the rise. In 2011, approximately 11% of school-aged children had ever been diagnosed with ADHD—an increase of 2 million children since 2003.1 Another analysis found that, while more children ages 8 to 15 years were diagnosed with ADHD than with any other mental health disorder, only about half had received treatment for it.2 Since the majority of children—65% to 85%—are diagnosed in the primary care setting,3 there is a clear need for primary care clinicians to be up-to-date on the diagnosis and treatment of this disorder.
To enhance both evidence-based practice and quality outcomes for the child and family dealing with this chronic and challenging disorder, an overview of the latest information about ADHD is presented here. In addition to diagnostic criteria, clinical presentation, screening methods, and treatment options, a discussion of the parental role in ADHD management and a medication reference guide are also provided (the latter to facilitate appropriate selection of initial pharmacologic therapy).
INTRODUCTION
ADHD is characterized by persistent patterns of hyperactivity-impulsivity and/or inattention4 and is diagnosed about twice as often in boys as in girls.2 The hyperactive-impulsive form usually manifests before age 7, while the inattentive form may not be apparent until age 8 or 9.5 Although symptoms may wane with maturity, they persist into adulthood for about 50% of patients.6
ADHD can impair academic performance, disrupt familial and interpersonal relationships, and lead to social isolation and low self-esteem.4 Clinicians should be mindful of the potential negative long-term effects of ADHD, which include increased risk for substance abuse and other antisocial activities and fewer vocational opportunities.7
The economic impact of ADHD is also significant. An often-cited 2007 cost-of-illness analysis estimated a minimum annual societal cost of $42.5 billion for pediatric ADHD. A more likely estimate is twice that and highlights the public health importance of ADHD to health care practitioners, families, and society.8
ETIOLOGY
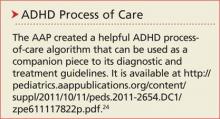
Currently, a single cause for ADHD has not been established, although research supports a genetic basis, with secondary factors (eg, environmental influences) also involved.9 Ongoing studies have identified numerous genes that contribute to ADHD.10 The disorder has also been seen in children with brain damage, including perinatal brain damage, fetal alcohol syndrome, and Down syndrome.11
MRI studies have shown brain patterns that link ADHD with decreased functioning in the cingulo-frontal-parietal (CFP) cognitive-attention network. Specifically, impairment in the dorsal anterior midcingulate cortex, termed the daMCC, is responsible for inappropriate or excessive motor behavior, while alterations in the dorsolateral prefrontal cortex, or DLPFC, have adverse effects on the ability to think ahead, plan, and reason.12 With this knowledge, clinicians can choose medications that target specific areas of the brain, if appropriate.
Environmental influences
Two factors hypothesized to influence ADHD symptoms are nutrition and the home environment. Many studies have examined the effects of refined sugar, additives, and preservatives on ADHD symptoms. Results indicate that, while monitoring a child’s intake of these ingredients may be beneficial from a nutritional standpoint, it is unlikely that they significantly affect ADHD symptoms.10,13,14
Given ADHD’s genetic component, parents may have ADHD themselves—making it more difficult for them to provide consistency and structure in the home environment.15,16 Chaotic living situations can exacerbate ADHD symptoms,11 and research indicates that mothers with ADHD are more likely to engage in negative parenting, with higher demands and little praise, than mothers without the disorder.15 They may exhibit less patience and feel the need to control the child’s environment, even during playtime.17 Preschool hyperactivity has been identified in children whose parents exhibit coercive, overstimulating, negative, or inconsistent parenting.18
Next page: Making the Diagnosis >>
MAKING THE DIAGNOSIS
Presenting behaviors
Symptoms of ADHD typically manifest in academic settings. The greater frequency of ADHD diagnosis and treatment in boys may derive from differences in how the genders externalize behaviors.19 While boys often exhibit more impulsive and aggressive behavior, girls internalize symptoms and are more likely to be inattentive. As a result, girls are less likely to be disruptive in the classroom and may not be referred for evaluation. Boys, on the other hand, may be overdiagnosed due to their disruptive behaviors.19 Daley indicates that inattention (eg, daydreaming) and hyperactivity (eg, fidgeting) symptoms become more apparent in structured settings, such as a classroom.15
Any child who requires a mental health assessment should also be screened for ADHD; if the results of the screening suggest ADHD, a full evaluation is warranted.20
Diagnostic criteria
According to the American Psychiatric Association’s criteria—outlined in the Diagnostic and Statistical Manual of Mental Disorders–IV (Text Revision) (DSM-IV-TR) and the subsequent DSM-5—the diagnosis of ADHD requires that the patient have at least six symptoms of inattention, hyperactivity, and/or impulsivity.4,21,22 For patients ages 17 or older, the DSM-5 requires five symptoms of inattention or hyperactivity-impulsivity.21
Children are usually unable to complete one task prior to starting another and are easily distracted by noises otherwise ignored by others (eg, lawnmowing, background conversation).4 They may also exhibit excessive fidgeting and interrupt formal conversations or lectures.4 Inappropriate behavior relative to the child’s developmental level must have been present for at least six months prior to age 7 (according to DSM-IV-TR)4 or age 12 (DSM-5).21
In addition to exhibiting the above symptoms for a minimum of six months, impairment must be observed in at least two settings (home, school, or work), with obvious clinical impairment in social, academic, or occupational functioning.4 ADHD symptoms can vary depending on the setting; the child may have more difficulty paying attention and following directions in a classroom filled with children than in an environment with less stimuli (eg, one-on-one home situations).11
Children who exhibit ADHD symptoms in only one setting may actually have problems secondary to cognition, emotional maturity, or feelings of well-being in a particular setting.11 Therefore, the clinician must rely on multiple sources of information (eg, parents, teachers, other caregivers) in order to make the diagnosis of ADHD.23 A teacher should have had regular contact with the child for at least four to six months in order to provide an accurate evaluation of symptoms and their persistence.5
Assessment scales
Validated parent and teacher instruments, along with the DSM-IV-TR criteria, can be used to obtain data to support a diagnosis of ADHD.5,24
The Conners Comprehensive Behavior Rating Scales and the ADHD Rating Scale IV (DSM-IV) can be used by teachers and parents to document behaviors of preschool-aged children.5
The Vanderbilt Assessment Scales, which have been validated in both primary care and referral settings, may be used for children older than 4.5
More information about rating scales is available at the National Resource Center on ADHD website (www.help4adhd.org/en/treatment/scales).
In addition to parent- or teacher-reported data, further evidence of functional impairment may be gleaned through a review of report cards, standardized testing, and school records (eg, attendance or disciplinary actions).24
Differential diagnosis
The differential diagnosis should include other mental health conditions, sleep disorders, and any possible underlying medical or developmental problems.24 Hyperthyroidism and lead toxicity, as examples, could elicit symptoms consistent with ADHD.11 When the diagnosis is in doubt, coexisting conditions are present, or treatment options are in question, the primary care clinician should refer the patient to a pediatric or mental health specialist for further evaluation.23
BEFORE TREATMENT
After the diagnosis is made but before treatment commences, a complete review of systems, physical and psychologic evaluation, cardiac and sleep history, thorough family history pertaining to mental health and medical conditions, and an age-appropriate interview are required.24 The exam results assist in identifying other concerns that would indicate the need for appropriate diagnostic testing and/or referral (see Table 1).
Although stimulant treatment for ADHD has not been shown to increase cardiovascular events in otherwise healthy young people,25 experts differ in their opinions about the need for screening ECG prior to treatment initiation. The American Heart Association recommends a screening ECG before stimulant therapy is initiated,26 while the American Academy of Pediatrics (AAP) does not, as long as the history and exam results yield no cardiac findings.27 Since the Prescribing Information for most ADHD medications cautions against use in patients with known serious cardiac abnormalities, if exam findings suggest the possibility of cardiovascular disease, further evaluation with ECG and referral to a pediatric cardiologist are indicated.26,28
In the interview, the clinician should explore the patient’s perception of his or her behavior in response to family and social relationships and academic performance (eg, parent-teacher communication, report cards, detentions, suspensions). The psychosocial history may provide an explanation for acute onset of symptoms or coexisting disorders. Family history provides valuable insight regarding the health and cognitive abilities of family members, as well as the possibility of genetic influences on the child.24
Parents should be advised that ADHD is a chronic condition that requires a long-term treatment approach for symptoms that may last into adulthood. Identification of goals and treatment success depend on collaborative efforts with parents, teachers, clinicians, caregivers, and mental health clinicians.24
Continue for parents and ADHD >>
PARENTS AND ADHD
Stress
Caregivers for a child with ADHD are burdened with the ongoing challenges of the child’s inability to follow rules and his or her continual struggles with academics and peer relationships.29 These hardships stress parents’ patience, often resulting in parental impulsive reactivity (eg, physical punishment of the child).
In addition, social isolation for both children and parents is common because of the judgmental scrutiny of other parents whose children are not affected by ADHD.30 Parents’ career and social activities may be interrupted, adding to the sense of guilt, blame, burnout, and depression often associated with parenting a child with ADHD.29
While some parenting stress is expected, those who are unable to cope with everyday events are more likely to experience conflict and anger, further increasing the child’s anxiety and emotional state.31 This dysfunctional environment prohibits the adoption of positive parenting techniques and ultimately contributes to more psychologic distress and harm to the parent-child relationship.31
Support
Once a child is diagnosed with ADHD, parents require adequate education to bolster their understanding of how to manage their child’s symptoms.29 Establishing effective support systems—whether a spouse, family member, friend, or another parent whose child has ADHD—is imperative to enable parents to cope with the stress and to promote positive parenting, which has been shown to decrease symptomatic behavior.32
Furthermore, understanding the individual child’s traits will help the parents channel his or her energy into personal areas of interest, such as sports or creative outlets (art, dance, theater).32
Training
Parenting styles may play a role in the management of a child’s ADHD.9,11 Encouraging parents to learn how to change their responses to their child’s behavior through evidence-based behavioral training can be one of the most effective interventions for both parents and children.33 Parents who participate in this training gain greater behavioral understanding and treatment satisfaction, and their children experience significant improvement in conduct and other symptoms.23
TREATMENT OPTIONS
Choice of treatment depends on patient age, the severity of functional impairment, and the individual needs of the child. Treatment may include behavioral therapy, medication administration, or a combination of the two.23
Behavioral therapy
Behavioral therapists can provide parents and teachers with evidence-based training to understand and manage ADHD conduct.34 Parents and teachers are taught to recognize the effects of environmental factors on behavior and then to modify environments and daily schedules and set appropriate limits. They learn how to reinforce positive behavior, identify triggers, and decrease inappropriate behavior, using calm disciplinary approaches that lead to positive parent-child and teacher-student relationships.23,34
Collaborative efforts between parents and teachers are crucial to the child’s treatment plan, and individualized educational plans should be implemented to enhance academic performance, social skills, and self-esteem. For example, teachers can send home daily report cards to assist parents with monitoring core symptoms and treatment efficacy.35
Behavioral therapy classes for both parent and child, or for parents only, usually meet weekly for eight to 20 weeks. Parents learn how to build positive relationships, set limits, and respond consistently with rewards or punishments (eg, consequences, time-outs). Less effective outcomes were noted when such interventions were tried by parents without adequate training.14,24,33
Medications have been found to be more effective to treat ADHD symptoms than behavioral therapy alone, and parents and teachers report higher satisfaction with treatment plans that combine behavior modification with pharmacologic therapy.23
Next: Medication recommendations >>
MEDICATION RECOMMENDATIONS
AAP medication recommendations are age-specific and should be used only if the patient meets DSM-IV-TR criteria.24 An overview of both stimulant and nonstimulant treatment options for ADHD is provided in the Figure.
When an ADHD treatment regimen does not result in improved symptoms and functioning, the clinician should revisit the treatment plan and differential diagnosis. After reevaluation, the clinician may choose to add or change medication type or dose, adjust behavioral therapy, or consider the possibility of language or learning disabilities, mental health disorders, other psychosocial stressors, or poor adherence to the treatment plan.24
Parents may refuse stimulant therapy for their child, fearing future drug use (or abuse) in adolescence.24 Clinicians should respect parents’ decisions to defer stimulant therapy, while at the same time clarifying concerns or misunderstandings in order to provide optimal care for the child.24 Studies have demonstrated that stimulant treatment for ADHD has a protective effect, with outcomes suggesting significantly decreased risk for drug or alcohol dependence.36
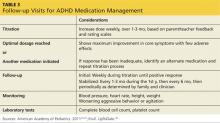
Clinician-provided anticipatory education about dose titration, expected treatment results, and potential adverse effects will help prepare parents for the ADHD medication management process.23 The length of time needed for dose titration varies by class of ADHD medication (see Table 2). For stimulants, effects on core symptoms may be seen within the first week. Nonstimulants take longer: up to six weeks for atomoxetine and up to four weeks for the a2-adrenergic agonists.24
Stimulants
Evidence strongly supports stimulants as first-line treatment for ADHD in children ages 6 and older.23 Stimulants are safe and efficacious in reducing the core symptoms of inattention, hyperactivity, and impulsivity.23 The initial choice of stimulant depends on the individual child’s needs. It should be noted that, although decreased growth rates have been observed in children taking stimulants, this effect ends by the third year of treatment.38 If maximum doses are reached and desired effects are not achieved with the first stimulant, choosing an alternate drug in the stimulant class may be an effective option.24 Clinicians may also consider other drug classes based on the comprehensive exam, adverse effects profile, contraindications, and individual responses.
Nonstimulants
Nonstimulant medications include atomoxetine and the a2-adrenergic agonists extended-release clonidine and extended-release guanfacine.24
Atomoxetine. Atomoxetine is a selective norepinephrine-reuptake inhibitor that may be prescribed if substance abuse or diversion is suspected or if stimulant therapy is contraindicated, undesirable, or unsuccessful.24,39 Using weight-based dosing for titration,37 the first week of therapy should begin with a half-dose to minimize sedation or gastrointestinal symptoms.24 While atomoxetine can be quite effective, caution should be used when prescribing this agent, as it carries a black box warning for suicidal ideation.24
α2-Adrenergic agonists. Both extended-release clonidine and extended-release guanfacine are α2-adrenergic agonists that may be beneficial when stimulants and atomoxetine have failed or when there are coexisting conditions.37 Either clonidine or guanfacine can be given in combination with a stimulant, if stimulant or atomoxetine treatment alone is unsuccessful or if adverse effects are unacceptable.24,39 Sedative effects and withdrawal irritability are more common with clonidine than with guanfacine, and when discontinued, these medications should be tapered to avoid blood pressure changes.24,40
Age-specific recommendations
Medications should be selected based on age ranges. In preschool-age children (ages 4 to 5), methylphenidate is recommended when target behaviors and impaired functioning persist for nine months in both home and day care/school settings, despite behavioral therapy.23,24 As examples, medication may be warranted if the child poses a significant risk of injury to other children or caregivers and/or faces expulsion from preschool or day care because of his or her behaviors.34
Risks and benefits should be considered carefully before medical therapy is initiated in this group. Further, the lowest possible starting dose of methylphenidate is preferred for preschoolers due to their slower metabolism.24 While dextroamphetamine is FDA approved for children younger than 6, efficacy and safety have not been proven in this age group and the AAP does not recommend it.23
For children ages 6 to 18, the AAP recommends combined treatment with medication and evidence-based behavioral training for the patient, parent, and teacher. In the adolescent population, evidence supports use of stimulants as first-line therapy, but with close monitoring for medication misuse.23 Misuse may become apparent through increased prescription refills; if identified, ADHD medication should be discontinued and substance abuse treatment initiated before ADHD therapy recommences.24
Continue for dosing and special considerations >>
Dosing and special considerations
Initiation of ADHD medication is usually begun over the weekend to allow parents time to observe for adverse effects, to better manage the drug titration process, and to minimize academic disruptions.41 Although more expensive, the extended-release formulas are often selected to eliminate the need for multiple doses and to decrease perceived stigma associated with medication administration at school.24 Longer-acting formulations have also been shown to increase treatment adherence. Adding shorter-acting doses in late afternoon, however, may be helpful if the child experiences difficulty concentrating (eg, on homework, sports, driving).24
Although drug holidays are not usually recommended, children can be evaluated for this individually. For example, a child whose ADHD symptoms primarily involve inattention may only require medication on school days.37
Follow-up
During the titration process, which can take up to three months, weekly clinician contacts—some by phone—to monitor effectiveness, adherence, and adverse effects are recommended (see Table 3). Blood pressure and heart rate should be monitored carefully and titration continued as needed until optimal response to treatment has been achieved.24 Monitoring should continue every three months for the first year of treatment and biannually thereafter.24 After several years, it is reasonable to consider a closely monitored drug-free trial period to determine if medication is still necessary.24 Finally, clinicians should remain cognizant of the potential cardiovascular effects of longer-term stimulant use and adhere to clinical guidelines.42
If coexisting conditions such as severe mood or anxiety disorders are present and improvement is not noted in core ADHD symptoms after three months of treatment, the patient should be referred to a mental health specialist.23
CONCLUSION
Primary care providers must be knowledgeable about ADHD and offer appropriate evidence-based interventions, treatments, and supportive measures to patients and families dealing with this disorder. Clinicians should know what resources are available for parents of children with ADHD. Psychoeducation for parents, families, and teachers is imperative to ensure positive home and school environments. Each treatment plan requires an individual approach, and optimal use of all available resources is desirable. Implementing evidence-based recommendations will increase the overall quality of life for children and families dealing with ADHD and optimize behavioral outcomes.
The authors would like to thank Laurie Rockelli, PhD, RN, PMHCNS-BC, and William Campbell, EdD, RN, for their revisions and support in the completion of this article.
1. Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34-46.
2. Merikangas KR, He JP, Brody D, et al. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81.
3. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85(9):890-896.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
5. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: clinical features and evaluation. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-clinical-features-and-evaluation?source=see_link. Accessed December 15, 2014.
6. Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122(5): 97-109.
7. Danckaerts M, Sonuga-Barke E, Coghill D, et al. The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. 2010;19(2):83-105.
8. Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambul Pediatr. 2007;7(1 suppl):121-131.
9. Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry Hum Dev. 2010;41(2):168-192.
10. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: epidemiology and pathogenesis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-epidemiology-and-pathogenesis?source=see_link. Accessed December 15, 2014.
11. Marcdante KJ, Kliegman RM, Jenson HB, Behrman RE. Attention-deficit/hyperactivity disorder. In: Merrit J, Cicalese B, eds. Nelson Essentials of Pediatrics. 6th ed. Philadelphia, PA: Saunders Elsevier; 2011:50-52.
12. Bush G. Cingulate, frontal, and parietal cortical dysfunction in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69(12):1160-1167.
13. CDC. Facts about ADHD. www.cdc.gov/NCBDDD/adhd/facts.html. Accessed December 15, 2014.
14. Rajwan E, Chacko A, Moeller M. Nonpharmacological interventions for preschool ADHD: state of the evidence and implications for practice. Prof Psychol Res Pr. 2012;43(5):520-526.
15. Daley D. Attention deficit hyperactivity disorder: a review of the essential facts. Child Care Health Dev. 2006;32(2):193-204.
16. van der Oord S, Bögels S, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud. 2012;21(1):139-147.
17. Zisser AR, Eyberg SM. Maternal ADHD: parent-child interactions and relations with child disruptive behavior. Child Fam Behavior Ther. 2012;34(1):33-52.
18. Daley D, Jones K, Hutchings J, Thompson M. Attention deficit hyperactivity disorder in pre-school children: current findings, recommended interventions and future directions. Child Care Health Dev. 2009;35(6):754-766.
19. Bruchmüller K, Margraf J, Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J Consult Clin Psychol. 2012;80(1):128-138.
20. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894-921.
21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
22. American Psychiatric Association. Highlights of Changes from DSM-IV-TR to DSM-5. www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf. Accessed December 15, 2014.
23. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-1022.
24. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. Supplemental information. Implementing the key action statements: an algorithm and explanation for process of care for the evaluation, diagnosis, treatment, and monitoring of ADHD in children and adolescents. http://pediatrics.aappublications.org/content/suppl/2011/10/11/peds.2011-2654.DC1/zpe611117822p.pdf. Accessed December 15, 2014.
25. Olfson M, Huang C, Gerhard T, et al. Stimulants and cardiovascular events in youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(2):147-156.
26. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117(18):2407-2423.
27. Perrin JM, Friedman RA, Knilans TK, et al. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
28. Berger S. Cardiac evaluation of patients receiving pharmacotherapy for attention deficit hyperactivity disorder. www.uptodate.com/contents/cardiac-evaluation-of-patients-receiving-pharmacotherapy-for-attention-deficit-hyperactivity-disorder?source=see_link. Accessed December 15, 2014.
29. Ho SC, Chien WT, Wang L. Parents’ perceptions of care-giving to a child with attention deficit hyperactivity disorder: an exploratory study. Contemp Nurse. 2011;40(1):41-56.
30. Moen ØL, Hall-Lord ML, Hedelin B. Contending and adapting every day: Norwegian parents’ lived experience of having a child with ADHD. J Fam Nursing. 2011;17(4):441-462.
31. Theule J, Wiener J, Rogers M, Marton I. Predicting parenting stress in families of children with ADHD: parent and contextual factors. J Child Fam Stud. 2011;20(5):640-647.
32. Brown RP, Gerbarg PL. Non-Drug Treatments for ADHD. New York, NY: Norton & Company; 2012:5-26.
33. Jones K, Daley D, Hutchings J, et al. Efficacy of the Incredible Years Basic parent training programme as an early intervention for children with conduct problems and ADHD. Child Care Health Dev. 2007;33(6):749-756.
34. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: overview of treatment and prognosis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-overview-of-treatment-and-prognosis?source=see_link. Accessed December 15, 2014.
35. Fabiano GA, Vujnovic RK, Pelham WE, et al. Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychol Rev. 2010;39(2):219-239.
36. Wilens TE, Faraone SV, Biederman J, Gunawardene, S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003; 111(1):179-185.
37. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: treatment with medications. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-treatment-with-medications?source=see_link. Accessed November 10, 2014.
38. Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1014–1026.
39. Krull KR. Pharmacology of drugs used to treat attention deficit hyperactivity disorder in children and adolescents. www.uptodate.com/contents/pharmacology-of-drugs-used-to-treat-attention-deficit-hyperactivity-disorder-in-children-and-adolescents?source=see_link. Accessed December 15, 2014.
40. Scahill L. Alpha-2 adrenergic agonists in children with inattention, hyperactivity and impulsiveness. CNS Drugs. 2009;23(suppl 1):43-49.
41. Krull KR. Patient information: treatment of attention deficit hyperactivity disorder in children (beyond the basics). www.uptodate.com/contents/treatment-of-attention-deficit-hyperactivity-disorder-in-children-beyond-the-basics?source=related_link. Accessed December 15, 2014.
42. Hammerness PG, Perrin JM, Shelley-Abrahamson R, Wilens TE. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: update and clinical recommendations. J Am Acad Child Adolesc Psychiatry. 2011;50(10):978-990.
CE/CME No: CR-1501
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain the attention-deficit/hyperactivity disorder (ADHD) diagnostic criteria of inattention, hyperactivity, and/or impulsivity as defined in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR), and the DSM-5 update.
• Discuss the American Academy of Pediatrics clinical practice guideline for evaluation, diagnosis, treatment, and monitoring of children and adolescents with ADHD.
• Describe the classes of medications available to treat ADHD, the indications for each, and the forms available (eg, short- versus long-acting, tablets, capsules, patches, liquids).
• Identify environmental factors at home and in school that can affect a child’s ADHD and know how to address them.
• Understand and provide support for the parent’s role in managing a child’s ADHD.
FACULTY
Amy Chandler is a family nurse practitioner at Peninsula Surgical Group in Salisbury, Maryland. Mary Parsons is an Assistant Professor at the University of Maryland School of Nursing in Baltimore. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.25 hours of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of January 2015.
Article begins on next page >>
Hyperactivity, impulsivity, disruptive behavior, lack of focus—the symptoms of attention-deficit/hyperactivity disorder can negatively impact children and their families. Primary care providers have the opportunity to bring a semblance of order to chaos, and improve quality of life for all involved, by identifying affected patients and providing effective treatment options. Here is everything you need to know.
Attention-deficit/hyperactivity disorder (ADHD) is a diagnosis on the rise. In 2011, approximately 11% of school-aged children had ever been diagnosed with ADHD—an increase of 2 million children since 2003.1 Another analysis found that, while more children ages 8 to 15 years were diagnosed with ADHD than with any other mental health disorder, only about half had received treatment for it.2 Since the majority of children—65% to 85%—are diagnosed in the primary care setting,3 there is a clear need for primary care clinicians to be up-to-date on the diagnosis and treatment of this disorder.
To enhance both evidence-based practice and quality outcomes for the child and family dealing with this chronic and challenging disorder, an overview of the latest information about ADHD is presented here. In addition to diagnostic criteria, clinical presentation, screening methods, and treatment options, a discussion of the parental role in ADHD management and a medication reference guide are also provided (the latter to facilitate appropriate selection of initial pharmacologic therapy).
INTRODUCTION
ADHD is characterized by persistent patterns of hyperactivity-impulsivity and/or inattention4 and is diagnosed about twice as often in boys as in girls.2 The hyperactive-impulsive form usually manifests before age 7, while the inattentive form may not be apparent until age 8 or 9.5 Although symptoms may wane with maturity, they persist into adulthood for about 50% of patients.6
ADHD can impair academic performance, disrupt familial and interpersonal relationships, and lead to social isolation and low self-esteem.4 Clinicians should be mindful of the potential negative long-term effects of ADHD, which include increased risk for substance abuse and other antisocial activities and fewer vocational opportunities.7
The economic impact of ADHD is also significant. An often-cited 2007 cost-of-illness analysis estimated a minimum annual societal cost of $42.5 billion for pediatric ADHD. A more likely estimate is twice that and highlights the public health importance of ADHD to health care practitioners, families, and society.8
ETIOLOGY
Currently, a single cause for ADHD has not been established, although research supports a genetic basis, with secondary factors (eg, environmental influences) also involved.9 Ongoing studies have identified numerous genes that contribute to ADHD.10 The disorder has also been seen in children with brain damage, including perinatal brain damage, fetal alcohol syndrome, and Down syndrome.11
MRI studies have shown brain patterns that link ADHD with decreased functioning in the cingulo-frontal-parietal (CFP) cognitive-attention network. Specifically, impairment in the dorsal anterior midcingulate cortex, termed the daMCC, is responsible for inappropriate or excessive motor behavior, while alterations in the dorsolateral prefrontal cortex, or DLPFC, have adverse effects on the ability to think ahead, plan, and reason.12 With this knowledge, clinicians can choose medications that target specific areas of the brain, if appropriate.
Environmental influences
Two factors hypothesized to influence ADHD symptoms are nutrition and the home environment. Many studies have examined the effects of refined sugar, additives, and preservatives on ADHD symptoms. Results indicate that, while monitoring a child’s intake of these ingredients may be beneficial from a nutritional standpoint, it is unlikely that they significantly affect ADHD symptoms.10,13,14
Given ADHD’s genetic component, parents may have ADHD themselves—making it more difficult for them to provide consistency and structure in the home environment.15,16 Chaotic living situations can exacerbate ADHD symptoms,11 and research indicates that mothers with ADHD are more likely to engage in negative parenting, with higher demands and little praise, than mothers without the disorder.15 They may exhibit less patience and feel the need to control the child’s environment, even during playtime.17 Preschool hyperactivity has been identified in children whose parents exhibit coercive, overstimulating, negative, or inconsistent parenting.18
Next page: Making the Diagnosis >>
MAKING THE DIAGNOSIS
Presenting behaviors
Symptoms of ADHD typically manifest in academic settings. The greater frequency of ADHD diagnosis and treatment in boys may derive from differences in how the genders externalize behaviors.19 While boys often exhibit more impulsive and aggressive behavior, girls internalize symptoms and are more likely to be inattentive. As a result, girls are less likely to be disruptive in the classroom and may not be referred for evaluation. Boys, on the other hand, may be overdiagnosed due to their disruptive behaviors.19 Daley indicates that inattention (eg, daydreaming) and hyperactivity (eg, fidgeting) symptoms become more apparent in structured settings, such as a classroom.15
Any child who requires a mental health assessment should also be screened for ADHD; if the results of the screening suggest ADHD, a full evaluation is warranted.20
Diagnostic criteria
According to the American Psychiatric Association’s criteria—outlined in the Diagnostic and Statistical Manual of Mental Disorders–IV (Text Revision) (DSM-IV-TR) and the subsequent DSM-5—the diagnosis of ADHD requires that the patient have at least six symptoms of inattention, hyperactivity, and/or impulsivity.4,21,22 For patients ages 17 or older, the DSM-5 requires five symptoms of inattention or hyperactivity-impulsivity.21
Children are usually unable to complete one task prior to starting another and are easily distracted by noises otherwise ignored by others (eg, lawnmowing, background conversation).4 They may also exhibit excessive fidgeting and interrupt formal conversations or lectures.4 Inappropriate behavior relative to the child’s developmental level must have been present for at least six months prior to age 7 (according to DSM-IV-TR)4 or age 12 (DSM-5).21
In addition to exhibiting the above symptoms for a minimum of six months, impairment must be observed in at least two settings (home, school, or work), with obvious clinical impairment in social, academic, or occupational functioning.4 ADHD symptoms can vary depending on the setting; the child may have more difficulty paying attention and following directions in a classroom filled with children than in an environment with less stimuli (eg, one-on-one home situations).11
Children who exhibit ADHD symptoms in only one setting may actually have problems secondary to cognition, emotional maturity, or feelings of well-being in a particular setting.11 Therefore, the clinician must rely on multiple sources of information (eg, parents, teachers, other caregivers) in order to make the diagnosis of ADHD.23 A teacher should have had regular contact with the child for at least four to six months in order to provide an accurate evaluation of symptoms and their persistence.5
Assessment scales
Validated parent and teacher instruments, along with the DSM-IV-TR criteria, can be used to obtain data to support a diagnosis of ADHD.5,24
The Conners Comprehensive Behavior Rating Scales and the ADHD Rating Scale IV (DSM-IV) can be used by teachers and parents to document behaviors of preschool-aged children.5
The Vanderbilt Assessment Scales, which have been validated in both primary care and referral settings, may be used for children older than 4.5
More information about rating scales is available at the National Resource Center on ADHD website (www.help4adhd.org/en/treatment/scales).
In addition to parent- or teacher-reported data, further evidence of functional impairment may be gleaned through a review of report cards, standardized testing, and school records (eg, attendance or disciplinary actions).24
Differential diagnosis
The differential diagnosis should include other mental health conditions, sleep disorders, and any possible underlying medical or developmental problems.24 Hyperthyroidism and lead toxicity, as examples, could elicit symptoms consistent with ADHD.11 When the diagnosis is in doubt, coexisting conditions are present, or treatment options are in question, the primary care clinician should refer the patient to a pediatric or mental health specialist for further evaluation.23
BEFORE TREATMENT
After the diagnosis is made but before treatment commences, a complete review of systems, physical and psychologic evaluation, cardiac and sleep history, thorough family history pertaining to mental health and medical conditions, and an age-appropriate interview are required.24 The exam results assist in identifying other concerns that would indicate the need for appropriate diagnostic testing and/or referral (see Table 1).
Although stimulant treatment for ADHD has not been shown to increase cardiovascular events in otherwise healthy young people,25 experts differ in their opinions about the need for screening ECG prior to treatment initiation. The American Heart Association recommends a screening ECG before stimulant therapy is initiated,26 while the American Academy of Pediatrics (AAP) does not, as long as the history and exam results yield no cardiac findings.27 Since the Prescribing Information for most ADHD medications cautions against use in patients with known serious cardiac abnormalities, if exam findings suggest the possibility of cardiovascular disease, further evaluation with ECG and referral to a pediatric cardiologist are indicated.26,28
In the interview, the clinician should explore the patient’s perception of his or her behavior in response to family and social relationships and academic performance (eg, parent-teacher communication, report cards, detentions, suspensions). The psychosocial history may provide an explanation for acute onset of symptoms or coexisting disorders. Family history provides valuable insight regarding the health and cognitive abilities of family members, as well as the possibility of genetic influences on the child.24
Parents should be advised that ADHD is a chronic condition that requires a long-term treatment approach for symptoms that may last into adulthood. Identification of goals and treatment success depend on collaborative efforts with parents, teachers, clinicians, caregivers, and mental health clinicians.24
Continue for parents and ADHD >>
PARENTS AND ADHD
Stress
Caregivers for a child with ADHD are burdened with the ongoing challenges of the child’s inability to follow rules and his or her continual struggles with academics and peer relationships.29 These hardships stress parents’ patience, often resulting in parental impulsive reactivity (eg, physical punishment of the child).
In addition, social isolation for both children and parents is common because of the judgmental scrutiny of other parents whose children are not affected by ADHD.30 Parents’ career and social activities may be interrupted, adding to the sense of guilt, blame, burnout, and depression often associated with parenting a child with ADHD.29
While some parenting stress is expected, those who are unable to cope with everyday events are more likely to experience conflict and anger, further increasing the child’s anxiety and emotional state.31 This dysfunctional environment prohibits the adoption of positive parenting techniques and ultimately contributes to more psychologic distress and harm to the parent-child relationship.31
Support
Once a child is diagnosed with ADHD, parents require adequate education to bolster their understanding of how to manage their child’s symptoms.29 Establishing effective support systems—whether a spouse, family member, friend, or another parent whose child has ADHD—is imperative to enable parents to cope with the stress and to promote positive parenting, which has been shown to decrease symptomatic behavior.32
Furthermore, understanding the individual child’s traits will help the parents channel his or her energy into personal areas of interest, such as sports or creative outlets (art, dance, theater).32
Training
Parenting styles may play a role in the management of a child’s ADHD.9,11 Encouraging parents to learn how to change their responses to their child’s behavior through evidence-based behavioral training can be one of the most effective interventions for both parents and children.33 Parents who participate in this training gain greater behavioral understanding and treatment satisfaction, and their children experience significant improvement in conduct and other symptoms.23
TREATMENT OPTIONS
Choice of treatment depends on patient age, the severity of functional impairment, and the individual needs of the child. Treatment may include behavioral therapy, medication administration, or a combination of the two.23
Behavioral therapy
Behavioral therapists can provide parents and teachers with evidence-based training to understand and manage ADHD conduct.34 Parents and teachers are taught to recognize the effects of environmental factors on behavior and then to modify environments and daily schedules and set appropriate limits. They learn how to reinforce positive behavior, identify triggers, and decrease inappropriate behavior, using calm disciplinary approaches that lead to positive parent-child and teacher-student relationships.23,34
Collaborative efforts between parents and teachers are crucial to the child’s treatment plan, and individualized educational plans should be implemented to enhance academic performance, social skills, and self-esteem. For example, teachers can send home daily report cards to assist parents with monitoring core symptoms and treatment efficacy.35
Behavioral therapy classes for both parent and child, or for parents only, usually meet weekly for eight to 20 weeks. Parents learn how to build positive relationships, set limits, and respond consistently with rewards or punishments (eg, consequences, time-outs). Less effective outcomes were noted when such interventions were tried by parents without adequate training.14,24,33
Medications have been found to be more effective to treat ADHD symptoms than behavioral therapy alone, and parents and teachers report higher satisfaction with treatment plans that combine behavior modification with pharmacologic therapy.23
Next: Medication recommendations >>
MEDICATION RECOMMENDATIONS
AAP medication recommendations are age-specific and should be used only if the patient meets DSM-IV-TR criteria.24 An overview of both stimulant and nonstimulant treatment options for ADHD is provided in the Figure.
When an ADHD treatment regimen does not result in improved symptoms and functioning, the clinician should revisit the treatment plan and differential diagnosis. After reevaluation, the clinician may choose to add or change medication type or dose, adjust behavioral therapy, or consider the possibility of language or learning disabilities, mental health disorders, other psychosocial stressors, or poor adherence to the treatment plan.24
Parents may refuse stimulant therapy for their child, fearing future drug use (or abuse) in adolescence.24 Clinicians should respect parents’ decisions to defer stimulant therapy, while at the same time clarifying concerns or misunderstandings in order to provide optimal care for the child.24 Studies have demonstrated that stimulant treatment for ADHD has a protective effect, with outcomes suggesting significantly decreased risk for drug or alcohol dependence.36
Clinician-provided anticipatory education about dose titration, expected treatment results, and potential adverse effects will help prepare parents for the ADHD medication management process.23 The length of time needed for dose titration varies by class of ADHD medication (see Table 2). For stimulants, effects on core symptoms may be seen within the first week. Nonstimulants take longer: up to six weeks for atomoxetine and up to four weeks for the a2-adrenergic agonists.24
Stimulants
Evidence strongly supports stimulants as first-line treatment for ADHD in children ages 6 and older.23 Stimulants are safe and efficacious in reducing the core symptoms of inattention, hyperactivity, and impulsivity.23 The initial choice of stimulant depends on the individual child’s needs. It should be noted that, although decreased growth rates have been observed in children taking stimulants, this effect ends by the third year of treatment.38 If maximum doses are reached and desired effects are not achieved with the first stimulant, choosing an alternate drug in the stimulant class may be an effective option.24 Clinicians may also consider other drug classes based on the comprehensive exam, adverse effects profile, contraindications, and individual responses.
Nonstimulants
Nonstimulant medications include atomoxetine and the a2-adrenergic agonists extended-release clonidine and extended-release guanfacine.24
Atomoxetine. Atomoxetine is a selective norepinephrine-reuptake inhibitor that may be prescribed if substance abuse or diversion is suspected or if stimulant therapy is contraindicated, undesirable, or unsuccessful.24,39 Using weight-based dosing for titration,37 the first week of therapy should begin with a half-dose to minimize sedation or gastrointestinal symptoms.24 While atomoxetine can be quite effective, caution should be used when prescribing this agent, as it carries a black box warning for suicidal ideation.24
α2-Adrenergic agonists. Both extended-release clonidine and extended-release guanfacine are α2-adrenergic agonists that may be beneficial when stimulants and atomoxetine have failed or when there are coexisting conditions.37 Either clonidine or guanfacine can be given in combination with a stimulant, if stimulant or atomoxetine treatment alone is unsuccessful or if adverse effects are unacceptable.24,39 Sedative effects and withdrawal irritability are more common with clonidine than with guanfacine, and when discontinued, these medications should be tapered to avoid blood pressure changes.24,40
Age-specific recommendations
Medications should be selected based on age ranges. In preschool-age children (ages 4 to 5), methylphenidate is recommended when target behaviors and impaired functioning persist for nine months in both home and day care/school settings, despite behavioral therapy.23,24 As examples, medication may be warranted if the child poses a significant risk of injury to other children or caregivers and/or faces expulsion from preschool or day care because of his or her behaviors.34
Risks and benefits should be considered carefully before medical therapy is initiated in this group. Further, the lowest possible starting dose of methylphenidate is preferred for preschoolers due to their slower metabolism.24 While dextroamphetamine is FDA approved for children younger than 6, efficacy and safety have not been proven in this age group and the AAP does not recommend it.23
For children ages 6 to 18, the AAP recommends combined treatment with medication and evidence-based behavioral training for the patient, parent, and teacher. In the adolescent population, evidence supports use of stimulants as first-line therapy, but with close monitoring for medication misuse.23 Misuse may become apparent through increased prescription refills; if identified, ADHD medication should be discontinued and substance abuse treatment initiated before ADHD therapy recommences.24
Continue for dosing and special considerations >>
Dosing and special considerations
Initiation of ADHD medication is usually begun over the weekend to allow parents time to observe for adverse effects, to better manage the drug titration process, and to minimize academic disruptions.41 Although more expensive, the extended-release formulas are often selected to eliminate the need for multiple doses and to decrease perceived stigma associated with medication administration at school.24 Longer-acting formulations have also been shown to increase treatment adherence. Adding shorter-acting doses in late afternoon, however, may be helpful if the child experiences difficulty concentrating (eg, on homework, sports, driving).24
Although drug holidays are not usually recommended, children can be evaluated for this individually. For example, a child whose ADHD symptoms primarily involve inattention may only require medication on school days.37
Follow-up
During the titration process, which can take up to three months, weekly clinician contacts—some by phone—to monitor effectiveness, adherence, and adverse effects are recommended (see Table 3). Blood pressure and heart rate should be monitored carefully and titration continued as needed until optimal response to treatment has been achieved.24 Monitoring should continue every three months for the first year of treatment and biannually thereafter.24 After several years, it is reasonable to consider a closely monitored drug-free trial period to determine if medication is still necessary.24 Finally, clinicians should remain cognizant of the potential cardiovascular effects of longer-term stimulant use and adhere to clinical guidelines.42
If coexisting conditions such as severe mood or anxiety disorders are present and improvement is not noted in core ADHD symptoms after three months of treatment, the patient should be referred to a mental health specialist.23
CONCLUSION
Primary care providers must be knowledgeable about ADHD and offer appropriate evidence-based interventions, treatments, and supportive measures to patients and families dealing with this disorder. Clinicians should know what resources are available for parents of children with ADHD. Psychoeducation for parents, families, and teachers is imperative to ensure positive home and school environments. Each treatment plan requires an individual approach, and optimal use of all available resources is desirable. Implementing evidence-based recommendations will increase the overall quality of life for children and families dealing with ADHD and optimize behavioral outcomes.
The authors would like to thank Laurie Rockelli, PhD, RN, PMHCNS-BC, and William Campbell, EdD, RN, for their revisions and support in the completion of this article.
CE/CME No: CR-1501
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain the attention-deficit/hyperactivity disorder (ADHD) diagnostic criteria of inattention, hyperactivity, and/or impulsivity as defined in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR), and the DSM-5 update.
• Discuss the American Academy of Pediatrics clinical practice guideline for evaluation, diagnosis, treatment, and monitoring of children and adolescents with ADHD.
• Describe the classes of medications available to treat ADHD, the indications for each, and the forms available (eg, short- versus long-acting, tablets, capsules, patches, liquids).
• Identify environmental factors at home and in school that can affect a child’s ADHD and know how to address them.
• Understand and provide support for the parent’s role in managing a child’s ADHD.
FACULTY
Amy Chandler is a family nurse practitioner at Peninsula Surgical Group in Salisbury, Maryland. Mary Parsons is an Assistant Professor at the University of Maryland School of Nursing in Baltimore. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.25 hours of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of January 2015.
Article begins on next page >>
Hyperactivity, impulsivity, disruptive behavior, lack of focus—the symptoms of attention-deficit/hyperactivity disorder can negatively impact children and their families. Primary care providers have the opportunity to bring a semblance of order to chaos, and improve quality of life for all involved, by identifying affected patients and providing effective treatment options. Here is everything you need to know.
Attention-deficit/hyperactivity disorder (ADHD) is a diagnosis on the rise. In 2011, approximately 11% of school-aged children had ever been diagnosed with ADHD—an increase of 2 million children since 2003.1 Another analysis found that, while more children ages 8 to 15 years were diagnosed with ADHD than with any other mental health disorder, only about half had received treatment for it.2 Since the majority of children—65% to 85%—are diagnosed in the primary care setting,3 there is a clear need for primary care clinicians to be up-to-date on the diagnosis and treatment of this disorder.
To enhance both evidence-based practice and quality outcomes for the child and family dealing with this chronic and challenging disorder, an overview of the latest information about ADHD is presented here. In addition to diagnostic criteria, clinical presentation, screening methods, and treatment options, a discussion of the parental role in ADHD management and a medication reference guide are also provided (the latter to facilitate appropriate selection of initial pharmacologic therapy).
INTRODUCTION
ADHD is characterized by persistent patterns of hyperactivity-impulsivity and/or inattention4 and is diagnosed about twice as often in boys as in girls.2 The hyperactive-impulsive form usually manifests before age 7, while the inattentive form may not be apparent until age 8 or 9.5 Although symptoms may wane with maturity, they persist into adulthood for about 50% of patients.6
ADHD can impair academic performance, disrupt familial and interpersonal relationships, and lead to social isolation and low self-esteem.4 Clinicians should be mindful of the potential negative long-term effects of ADHD, which include increased risk for substance abuse and other antisocial activities and fewer vocational opportunities.7
The economic impact of ADHD is also significant. An often-cited 2007 cost-of-illness analysis estimated a minimum annual societal cost of $42.5 billion for pediatric ADHD. A more likely estimate is twice that and highlights the public health importance of ADHD to health care practitioners, families, and society.8
ETIOLOGY
Currently, a single cause for ADHD has not been established, although research supports a genetic basis, with secondary factors (eg, environmental influences) also involved.9 Ongoing studies have identified numerous genes that contribute to ADHD.10 The disorder has also been seen in children with brain damage, including perinatal brain damage, fetal alcohol syndrome, and Down syndrome.11
MRI studies have shown brain patterns that link ADHD with decreased functioning in the cingulo-frontal-parietal (CFP) cognitive-attention network. Specifically, impairment in the dorsal anterior midcingulate cortex, termed the daMCC, is responsible for inappropriate or excessive motor behavior, while alterations in the dorsolateral prefrontal cortex, or DLPFC, have adverse effects on the ability to think ahead, plan, and reason.12 With this knowledge, clinicians can choose medications that target specific areas of the brain, if appropriate.
Environmental influences
Two factors hypothesized to influence ADHD symptoms are nutrition and the home environment. Many studies have examined the effects of refined sugar, additives, and preservatives on ADHD symptoms. Results indicate that, while monitoring a child’s intake of these ingredients may be beneficial from a nutritional standpoint, it is unlikely that they significantly affect ADHD symptoms.10,13,14
Given ADHD’s genetic component, parents may have ADHD themselves—making it more difficult for them to provide consistency and structure in the home environment.15,16 Chaotic living situations can exacerbate ADHD symptoms,11 and research indicates that mothers with ADHD are more likely to engage in negative parenting, with higher demands and little praise, than mothers without the disorder.15 They may exhibit less patience and feel the need to control the child’s environment, even during playtime.17 Preschool hyperactivity has been identified in children whose parents exhibit coercive, overstimulating, negative, or inconsistent parenting.18
Next page: Making the Diagnosis >>
MAKING THE DIAGNOSIS
Presenting behaviors
Symptoms of ADHD typically manifest in academic settings. The greater frequency of ADHD diagnosis and treatment in boys may derive from differences in how the genders externalize behaviors.19 While boys often exhibit more impulsive and aggressive behavior, girls internalize symptoms and are more likely to be inattentive. As a result, girls are less likely to be disruptive in the classroom and may not be referred for evaluation. Boys, on the other hand, may be overdiagnosed due to their disruptive behaviors.19 Daley indicates that inattention (eg, daydreaming) and hyperactivity (eg, fidgeting) symptoms become more apparent in structured settings, such as a classroom.15
Any child who requires a mental health assessment should also be screened for ADHD; if the results of the screening suggest ADHD, a full evaluation is warranted.20
Diagnostic criteria
According to the American Psychiatric Association’s criteria—outlined in the Diagnostic and Statistical Manual of Mental Disorders–IV (Text Revision) (DSM-IV-TR) and the subsequent DSM-5—the diagnosis of ADHD requires that the patient have at least six symptoms of inattention, hyperactivity, and/or impulsivity.4,21,22 For patients ages 17 or older, the DSM-5 requires five symptoms of inattention or hyperactivity-impulsivity.21
Children are usually unable to complete one task prior to starting another and are easily distracted by noises otherwise ignored by others (eg, lawnmowing, background conversation).4 They may also exhibit excessive fidgeting and interrupt formal conversations or lectures.4 Inappropriate behavior relative to the child’s developmental level must have been present for at least six months prior to age 7 (according to DSM-IV-TR)4 or age 12 (DSM-5).21
In addition to exhibiting the above symptoms for a minimum of six months, impairment must be observed in at least two settings (home, school, or work), with obvious clinical impairment in social, academic, or occupational functioning.4 ADHD symptoms can vary depending on the setting; the child may have more difficulty paying attention and following directions in a classroom filled with children than in an environment with less stimuli (eg, one-on-one home situations).11
Children who exhibit ADHD symptoms in only one setting may actually have problems secondary to cognition, emotional maturity, or feelings of well-being in a particular setting.11 Therefore, the clinician must rely on multiple sources of information (eg, parents, teachers, other caregivers) in order to make the diagnosis of ADHD.23 A teacher should have had regular contact with the child for at least four to six months in order to provide an accurate evaluation of symptoms and their persistence.5
Assessment scales
Validated parent and teacher instruments, along with the DSM-IV-TR criteria, can be used to obtain data to support a diagnosis of ADHD.5,24
The Conners Comprehensive Behavior Rating Scales and the ADHD Rating Scale IV (DSM-IV) can be used by teachers and parents to document behaviors of preschool-aged children.5
The Vanderbilt Assessment Scales, which have been validated in both primary care and referral settings, may be used for children older than 4.5
More information about rating scales is available at the National Resource Center on ADHD website (www.help4adhd.org/en/treatment/scales).
In addition to parent- or teacher-reported data, further evidence of functional impairment may be gleaned through a review of report cards, standardized testing, and school records (eg, attendance or disciplinary actions).24
Differential diagnosis
The differential diagnosis should include other mental health conditions, sleep disorders, and any possible underlying medical or developmental problems.24 Hyperthyroidism and lead toxicity, as examples, could elicit symptoms consistent with ADHD.11 When the diagnosis is in doubt, coexisting conditions are present, or treatment options are in question, the primary care clinician should refer the patient to a pediatric or mental health specialist for further evaluation.23
BEFORE TREATMENT
After the diagnosis is made but before treatment commences, a complete review of systems, physical and psychologic evaluation, cardiac and sleep history, thorough family history pertaining to mental health and medical conditions, and an age-appropriate interview are required.24 The exam results assist in identifying other concerns that would indicate the need for appropriate diagnostic testing and/or referral (see Table 1).
Although stimulant treatment for ADHD has not been shown to increase cardiovascular events in otherwise healthy young people,25 experts differ in their opinions about the need for screening ECG prior to treatment initiation. The American Heart Association recommends a screening ECG before stimulant therapy is initiated,26 while the American Academy of Pediatrics (AAP) does not, as long as the history and exam results yield no cardiac findings.27 Since the Prescribing Information for most ADHD medications cautions against use in patients with known serious cardiac abnormalities, if exam findings suggest the possibility of cardiovascular disease, further evaluation with ECG and referral to a pediatric cardiologist are indicated.26,28
In the interview, the clinician should explore the patient’s perception of his or her behavior in response to family and social relationships and academic performance (eg, parent-teacher communication, report cards, detentions, suspensions). The psychosocial history may provide an explanation for acute onset of symptoms or coexisting disorders. Family history provides valuable insight regarding the health and cognitive abilities of family members, as well as the possibility of genetic influences on the child.24
Parents should be advised that ADHD is a chronic condition that requires a long-term treatment approach for symptoms that may last into adulthood. Identification of goals and treatment success depend on collaborative efforts with parents, teachers, clinicians, caregivers, and mental health clinicians.24
Continue for parents and ADHD >>
PARENTS AND ADHD
Stress
Caregivers for a child with ADHD are burdened with the ongoing challenges of the child’s inability to follow rules and his or her continual struggles with academics and peer relationships.29 These hardships stress parents’ patience, often resulting in parental impulsive reactivity (eg, physical punishment of the child).
In addition, social isolation for both children and parents is common because of the judgmental scrutiny of other parents whose children are not affected by ADHD.30 Parents’ career and social activities may be interrupted, adding to the sense of guilt, blame, burnout, and depression often associated with parenting a child with ADHD.29
While some parenting stress is expected, those who are unable to cope with everyday events are more likely to experience conflict and anger, further increasing the child’s anxiety and emotional state.31 This dysfunctional environment prohibits the adoption of positive parenting techniques and ultimately contributes to more psychologic distress and harm to the parent-child relationship.31
Support
Once a child is diagnosed with ADHD, parents require adequate education to bolster their understanding of how to manage their child’s symptoms.29 Establishing effective support systems—whether a spouse, family member, friend, or another parent whose child has ADHD—is imperative to enable parents to cope with the stress and to promote positive parenting, which has been shown to decrease symptomatic behavior.32
Furthermore, understanding the individual child’s traits will help the parents channel his or her energy into personal areas of interest, such as sports or creative outlets (art, dance, theater).32
Training
Parenting styles may play a role in the management of a child’s ADHD.9,11 Encouraging parents to learn how to change their responses to their child’s behavior through evidence-based behavioral training can be one of the most effective interventions for both parents and children.33 Parents who participate in this training gain greater behavioral understanding and treatment satisfaction, and their children experience significant improvement in conduct and other symptoms.23
TREATMENT OPTIONS
Choice of treatment depends on patient age, the severity of functional impairment, and the individual needs of the child. Treatment may include behavioral therapy, medication administration, or a combination of the two.23
Behavioral therapy
Behavioral therapists can provide parents and teachers with evidence-based training to understand and manage ADHD conduct.34 Parents and teachers are taught to recognize the effects of environmental factors on behavior and then to modify environments and daily schedules and set appropriate limits. They learn how to reinforce positive behavior, identify triggers, and decrease inappropriate behavior, using calm disciplinary approaches that lead to positive parent-child and teacher-student relationships.23,34
Collaborative efforts between parents and teachers are crucial to the child’s treatment plan, and individualized educational plans should be implemented to enhance academic performance, social skills, and self-esteem. For example, teachers can send home daily report cards to assist parents with monitoring core symptoms and treatment efficacy.35
Behavioral therapy classes for both parent and child, or for parents only, usually meet weekly for eight to 20 weeks. Parents learn how to build positive relationships, set limits, and respond consistently with rewards or punishments (eg, consequences, time-outs). Less effective outcomes were noted when such interventions were tried by parents without adequate training.14,24,33
Medications have been found to be more effective to treat ADHD symptoms than behavioral therapy alone, and parents and teachers report higher satisfaction with treatment plans that combine behavior modification with pharmacologic therapy.23
Next: Medication recommendations >>
MEDICATION RECOMMENDATIONS
AAP medication recommendations are age-specific and should be used only if the patient meets DSM-IV-TR criteria.24 An overview of both stimulant and nonstimulant treatment options for ADHD is provided in the Figure.
When an ADHD treatment regimen does not result in improved symptoms and functioning, the clinician should revisit the treatment plan and differential diagnosis. After reevaluation, the clinician may choose to add or change medication type or dose, adjust behavioral therapy, or consider the possibility of language or learning disabilities, mental health disorders, other psychosocial stressors, or poor adherence to the treatment plan.24
Parents may refuse stimulant therapy for their child, fearing future drug use (or abuse) in adolescence.24 Clinicians should respect parents’ decisions to defer stimulant therapy, while at the same time clarifying concerns or misunderstandings in order to provide optimal care for the child.24 Studies have demonstrated that stimulant treatment for ADHD has a protective effect, with outcomes suggesting significantly decreased risk for drug or alcohol dependence.36
Clinician-provided anticipatory education about dose titration, expected treatment results, and potential adverse effects will help prepare parents for the ADHD medication management process.23 The length of time needed for dose titration varies by class of ADHD medication (see Table 2). For stimulants, effects on core symptoms may be seen within the first week. Nonstimulants take longer: up to six weeks for atomoxetine and up to four weeks for the a2-adrenergic agonists.24
Stimulants
Evidence strongly supports stimulants as first-line treatment for ADHD in children ages 6 and older.23 Stimulants are safe and efficacious in reducing the core symptoms of inattention, hyperactivity, and impulsivity.23 The initial choice of stimulant depends on the individual child’s needs. It should be noted that, although decreased growth rates have been observed in children taking stimulants, this effect ends by the third year of treatment.38 If maximum doses are reached and desired effects are not achieved with the first stimulant, choosing an alternate drug in the stimulant class may be an effective option.24 Clinicians may also consider other drug classes based on the comprehensive exam, adverse effects profile, contraindications, and individual responses.
Nonstimulants
Nonstimulant medications include atomoxetine and the a2-adrenergic agonists extended-release clonidine and extended-release guanfacine.24
Atomoxetine. Atomoxetine is a selective norepinephrine-reuptake inhibitor that may be prescribed if substance abuse or diversion is suspected or if stimulant therapy is contraindicated, undesirable, or unsuccessful.24,39 Using weight-based dosing for titration,37 the first week of therapy should begin with a half-dose to minimize sedation or gastrointestinal symptoms.24 While atomoxetine can be quite effective, caution should be used when prescribing this agent, as it carries a black box warning for suicidal ideation.24
α2-Adrenergic agonists. Both extended-release clonidine and extended-release guanfacine are α2-adrenergic agonists that may be beneficial when stimulants and atomoxetine have failed or when there are coexisting conditions.37 Either clonidine or guanfacine can be given in combination with a stimulant, if stimulant or atomoxetine treatment alone is unsuccessful or if adverse effects are unacceptable.24,39 Sedative effects and withdrawal irritability are more common with clonidine than with guanfacine, and when discontinued, these medications should be tapered to avoid blood pressure changes.24,40
Age-specific recommendations
Medications should be selected based on age ranges. In preschool-age children (ages 4 to 5), methylphenidate is recommended when target behaviors and impaired functioning persist for nine months in both home and day care/school settings, despite behavioral therapy.23,24 As examples, medication may be warranted if the child poses a significant risk of injury to other children or caregivers and/or faces expulsion from preschool or day care because of his or her behaviors.34
Risks and benefits should be considered carefully before medical therapy is initiated in this group. Further, the lowest possible starting dose of methylphenidate is preferred for preschoolers due to their slower metabolism.24 While dextroamphetamine is FDA approved for children younger than 6, efficacy and safety have not been proven in this age group and the AAP does not recommend it.23
For children ages 6 to 18, the AAP recommends combined treatment with medication and evidence-based behavioral training for the patient, parent, and teacher. In the adolescent population, evidence supports use of stimulants as first-line therapy, but with close monitoring for medication misuse.23 Misuse may become apparent through increased prescription refills; if identified, ADHD medication should be discontinued and substance abuse treatment initiated before ADHD therapy recommences.24
Continue for dosing and special considerations >>
Dosing and special considerations
Initiation of ADHD medication is usually begun over the weekend to allow parents time to observe for adverse effects, to better manage the drug titration process, and to minimize academic disruptions.41 Although more expensive, the extended-release formulas are often selected to eliminate the need for multiple doses and to decrease perceived stigma associated with medication administration at school.24 Longer-acting formulations have also been shown to increase treatment adherence. Adding shorter-acting doses in late afternoon, however, may be helpful if the child experiences difficulty concentrating (eg, on homework, sports, driving).24
Although drug holidays are not usually recommended, children can be evaluated for this individually. For example, a child whose ADHD symptoms primarily involve inattention may only require medication on school days.37
Follow-up
During the titration process, which can take up to three months, weekly clinician contacts—some by phone—to monitor effectiveness, adherence, and adverse effects are recommended (see Table 3). Blood pressure and heart rate should be monitored carefully and titration continued as needed until optimal response to treatment has been achieved.24 Monitoring should continue every three months for the first year of treatment and biannually thereafter.24 After several years, it is reasonable to consider a closely monitored drug-free trial period to determine if medication is still necessary.24 Finally, clinicians should remain cognizant of the potential cardiovascular effects of longer-term stimulant use and adhere to clinical guidelines.42
If coexisting conditions such as severe mood or anxiety disorders are present and improvement is not noted in core ADHD symptoms after three months of treatment, the patient should be referred to a mental health specialist.23
CONCLUSION
Primary care providers must be knowledgeable about ADHD and offer appropriate evidence-based interventions, treatments, and supportive measures to patients and families dealing with this disorder. Clinicians should know what resources are available for parents of children with ADHD. Psychoeducation for parents, families, and teachers is imperative to ensure positive home and school environments. Each treatment plan requires an individual approach, and optimal use of all available resources is desirable. Implementing evidence-based recommendations will increase the overall quality of life for children and families dealing with ADHD and optimize behavioral outcomes.
The authors would like to thank Laurie Rockelli, PhD, RN, PMHCNS-BC, and William Campbell, EdD, RN, for their revisions and support in the completion of this article.
1. Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34-46.
2. Merikangas KR, He JP, Brody D, et al. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81.
3. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85(9):890-896.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
5. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: clinical features and evaluation. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-clinical-features-and-evaluation?source=see_link. Accessed December 15, 2014.
6. Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122(5): 97-109.
7. Danckaerts M, Sonuga-Barke E, Coghill D, et al. The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. 2010;19(2):83-105.
8. Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambul Pediatr. 2007;7(1 suppl):121-131.
9. Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry Hum Dev. 2010;41(2):168-192.
10. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: epidemiology and pathogenesis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-epidemiology-and-pathogenesis?source=see_link. Accessed December 15, 2014.
11. Marcdante KJ, Kliegman RM, Jenson HB, Behrman RE. Attention-deficit/hyperactivity disorder. In: Merrit J, Cicalese B, eds. Nelson Essentials of Pediatrics. 6th ed. Philadelphia, PA: Saunders Elsevier; 2011:50-52.
12. Bush G. Cingulate, frontal, and parietal cortical dysfunction in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69(12):1160-1167.
13. CDC. Facts about ADHD. www.cdc.gov/NCBDDD/adhd/facts.html. Accessed December 15, 2014.
14. Rajwan E, Chacko A, Moeller M. Nonpharmacological interventions for preschool ADHD: state of the evidence and implications for practice. Prof Psychol Res Pr. 2012;43(5):520-526.
15. Daley D. Attention deficit hyperactivity disorder: a review of the essential facts. Child Care Health Dev. 2006;32(2):193-204.
16. van der Oord S, Bögels S, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud. 2012;21(1):139-147.
17. Zisser AR, Eyberg SM. Maternal ADHD: parent-child interactions and relations with child disruptive behavior. Child Fam Behavior Ther. 2012;34(1):33-52.
18. Daley D, Jones K, Hutchings J, Thompson M. Attention deficit hyperactivity disorder in pre-school children: current findings, recommended interventions and future directions. Child Care Health Dev. 2009;35(6):754-766.
19. Bruchmüller K, Margraf J, Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J Consult Clin Psychol. 2012;80(1):128-138.
20. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894-921.
21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
22. American Psychiatric Association. Highlights of Changes from DSM-IV-TR to DSM-5. www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf. Accessed December 15, 2014.
23. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-1022.
24. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. Supplemental information. Implementing the key action statements: an algorithm and explanation for process of care for the evaluation, diagnosis, treatment, and monitoring of ADHD in children and adolescents. http://pediatrics.aappublications.org/content/suppl/2011/10/11/peds.2011-2654.DC1/zpe611117822p.pdf. Accessed December 15, 2014.
25. Olfson M, Huang C, Gerhard T, et al. Stimulants and cardiovascular events in youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(2):147-156.
26. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117(18):2407-2423.
27. Perrin JM, Friedman RA, Knilans TK, et al. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
28. Berger S. Cardiac evaluation of patients receiving pharmacotherapy for attention deficit hyperactivity disorder. www.uptodate.com/contents/cardiac-evaluation-of-patients-receiving-pharmacotherapy-for-attention-deficit-hyperactivity-disorder?source=see_link. Accessed December 15, 2014.
29. Ho SC, Chien WT, Wang L. Parents’ perceptions of care-giving to a child with attention deficit hyperactivity disorder: an exploratory study. Contemp Nurse. 2011;40(1):41-56.
30. Moen ØL, Hall-Lord ML, Hedelin B. Contending and adapting every day: Norwegian parents’ lived experience of having a child with ADHD. J Fam Nursing. 2011;17(4):441-462.
31. Theule J, Wiener J, Rogers M, Marton I. Predicting parenting stress in families of children with ADHD: parent and contextual factors. J Child Fam Stud. 2011;20(5):640-647.
32. Brown RP, Gerbarg PL. Non-Drug Treatments for ADHD. New York, NY: Norton & Company; 2012:5-26.
33. Jones K, Daley D, Hutchings J, et al. Efficacy of the Incredible Years Basic parent training programme as an early intervention for children with conduct problems and ADHD. Child Care Health Dev. 2007;33(6):749-756.
34. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: overview of treatment and prognosis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-overview-of-treatment-and-prognosis?source=see_link. Accessed December 15, 2014.
35. Fabiano GA, Vujnovic RK, Pelham WE, et al. Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychol Rev. 2010;39(2):219-239.
36. Wilens TE, Faraone SV, Biederman J, Gunawardene, S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003; 111(1):179-185.
37. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: treatment with medications. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-treatment-with-medications?source=see_link. Accessed November 10, 2014.
38. Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1014–1026.
39. Krull KR. Pharmacology of drugs used to treat attention deficit hyperactivity disorder in children and adolescents. www.uptodate.com/contents/pharmacology-of-drugs-used-to-treat-attention-deficit-hyperactivity-disorder-in-children-and-adolescents?source=see_link. Accessed December 15, 2014.
40. Scahill L. Alpha-2 adrenergic agonists in children with inattention, hyperactivity and impulsiveness. CNS Drugs. 2009;23(suppl 1):43-49.
41. Krull KR. Patient information: treatment of attention deficit hyperactivity disorder in children (beyond the basics). www.uptodate.com/contents/treatment-of-attention-deficit-hyperactivity-disorder-in-children-beyond-the-basics?source=related_link. Accessed December 15, 2014.
42. Hammerness PG, Perrin JM, Shelley-Abrahamson R, Wilens TE. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: update and clinical recommendations. J Am Acad Child Adolesc Psychiatry. 2011;50(10):978-990.
1. Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34-46.
2. Merikangas KR, He JP, Brody D, et al. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81.
3. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85(9):890-896.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
5. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: clinical features and evaluation. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-clinical-features-and-evaluation?source=see_link. Accessed December 15, 2014.
6. Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122(5): 97-109.
7. Danckaerts M, Sonuga-Barke E, Coghill D, et al. The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. 2010;19(2):83-105.
8. Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambul Pediatr. 2007;7(1 suppl):121-131.
9. Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry Hum Dev. 2010;41(2):168-192.
10. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: epidemiology and pathogenesis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-epidemiology-and-pathogenesis?source=see_link. Accessed December 15, 2014.
11. Marcdante KJ, Kliegman RM, Jenson HB, Behrman RE. Attention-deficit/hyperactivity disorder. In: Merrit J, Cicalese B, eds. Nelson Essentials of Pediatrics. 6th ed. Philadelphia, PA: Saunders Elsevier; 2011:50-52.
12. Bush G. Cingulate, frontal, and parietal cortical dysfunction in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69(12):1160-1167.
13. CDC. Facts about ADHD. www.cdc.gov/NCBDDD/adhd/facts.html. Accessed December 15, 2014.
14. Rajwan E, Chacko A, Moeller M. Nonpharmacological interventions for preschool ADHD: state of the evidence and implications for practice. Prof Psychol Res Pr. 2012;43(5):520-526.
15. Daley D. Attention deficit hyperactivity disorder: a review of the essential facts. Child Care Health Dev. 2006;32(2):193-204.
16. van der Oord S, Bögels S, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud. 2012;21(1):139-147.
17. Zisser AR, Eyberg SM. Maternal ADHD: parent-child interactions and relations with child disruptive behavior. Child Fam Behavior Ther. 2012;34(1):33-52.
18. Daley D, Jones K, Hutchings J, Thompson M. Attention deficit hyperactivity disorder in pre-school children: current findings, recommended interventions and future directions. Child Care Health Dev. 2009;35(6):754-766.
19. Bruchmüller K, Margraf J, Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J Consult Clin Psychol. 2012;80(1):128-138.
20. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894-921.
21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
22. American Psychiatric Association. Highlights of Changes from DSM-IV-TR to DSM-5. www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf. Accessed December 15, 2014.
23. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-1022.
24. American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder. Supplemental information. Implementing the key action statements: an algorithm and explanation for process of care for the evaluation, diagnosis, treatment, and monitoring of ADHD in children and adolescents. http://pediatrics.aappublications.org/content/suppl/2011/10/11/peds.2011-2654.DC1/zpe611117822p.pdf. Accessed December 15, 2014.
25. Olfson M, Huang C, Gerhard T, et al. Stimulants and cardiovascular events in youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(2):147-156.
26. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117(18):2407-2423.
27. Perrin JM, Friedman RA, Knilans TK, et al. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
28. Berger S. Cardiac evaluation of patients receiving pharmacotherapy for attention deficit hyperactivity disorder. www.uptodate.com/contents/cardiac-evaluation-of-patients-receiving-pharmacotherapy-for-attention-deficit-hyperactivity-disorder?source=see_link. Accessed December 15, 2014.
29. Ho SC, Chien WT, Wang L. Parents’ perceptions of care-giving to a child with attention deficit hyperactivity disorder: an exploratory study. Contemp Nurse. 2011;40(1):41-56.
30. Moen ØL, Hall-Lord ML, Hedelin B. Contending and adapting every day: Norwegian parents’ lived experience of having a child with ADHD. J Fam Nursing. 2011;17(4):441-462.
31. Theule J, Wiener J, Rogers M, Marton I. Predicting parenting stress in families of children with ADHD: parent and contextual factors. J Child Fam Stud. 2011;20(5):640-647.
32. Brown RP, Gerbarg PL. Non-Drug Treatments for ADHD. New York, NY: Norton & Company; 2012:5-26.
33. Jones K, Daley D, Hutchings J, et al. Efficacy of the Incredible Years Basic parent training programme as an early intervention for children with conduct problems and ADHD. Child Care Health Dev. 2007;33(6):749-756.
34. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: overview of treatment and prognosis. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-overview-of-treatment-and-prognosis?source=see_link. Accessed December 15, 2014.
35. Fabiano GA, Vujnovic RK, Pelham WE, et al. Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychol Rev. 2010;39(2):219-239.
36. Wilens TE, Faraone SV, Biederman J, Gunawardene, S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003; 111(1):179-185.
37. Krull KR. Attention deficit hyperactivity disorder in children and adolescents: treatment with medications. www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-treatment-with-medications?source=see_link. Accessed November 10, 2014.
38. Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1014–1026.
39. Krull KR. Pharmacology of drugs used to treat attention deficit hyperactivity disorder in children and adolescents. www.uptodate.com/contents/pharmacology-of-drugs-used-to-treat-attention-deficit-hyperactivity-disorder-in-children-and-adolescents?source=see_link. Accessed December 15, 2014.
40. Scahill L. Alpha-2 adrenergic agonists in children with inattention, hyperactivity and impulsiveness. CNS Drugs. 2009;23(suppl 1):43-49.
41. Krull KR. Patient information: treatment of attention deficit hyperactivity disorder in children (beyond the basics). www.uptodate.com/contents/treatment-of-attention-deficit-hyperactivity-disorder-in-children-beyond-the-basics?source=related_link. Accessed December 15, 2014.
42. Hammerness PG, Perrin JM, Shelley-Abrahamson R, Wilens TE. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: update and clinical recommendations. J Am Acad Child Adolesc Psychiatry. 2011;50(10):978-990.