User login
A Rare Case of Segmental Neurofibromatosis With Multiple Blue-Red Pseudoatrophic Plaques
In the setting of neurofibromatosis (NF), neurofibromas commonly appear as flesh-colored nodular lesions.1 The presence of blue-red pseudoatrophic neurofibromas is rare, with only 1 known case of the segmental variant.2 Microscopic examination typically reveals thick-walled blood vessels in the papillary dermis and neurofibromatous tissue in the hypodermis. The neuroid proliferation is associated with the reduction of collagen tissue. This type of neurofibroma has an early presentation and it can be helpful in the diagnosis of some cases of NF.3,4
Case Report
A 5-year-old girl presented with 2 blue-red, well-demarcated, atrophic patches on the left leg. One plaque was localized on the left thigh, which had appeared at 7 months of age, and the other was on the left calf, which presented at 2 years of age (Figure 1). The lesions were 10- to 15-cm in diameter, roughly oval shaped, and completely asymptomatic. The skin overlying the atrophic patches showed a visible venous reticulum, and palpation revealed multiple nodular lesions. Physical examination revealed no cafè au lait spots, axillary freckling, Lisch nodules, or clinical signs of NF. Her family history was negative for NF. Physical and neurologic examinations revealed no abnormalities.
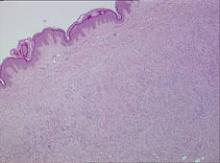
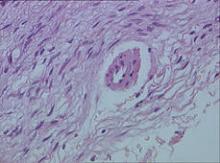
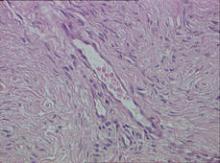
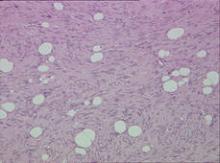
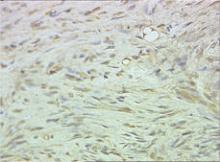
Biopsy specimens were obtained from 1 of the atrophic patches and from 1 of the nodules. Microscopic examination of the atrophic patch showed a dermal proliferation of spindle elements dispersed in loose connective tissue (Figure 2) and ectatic (Figure 3) or thick-walled (Figure 4) blood vessels. Microscopic exam-ination of the nodule disclosed a dermohypodermal neoplastic proliferation composed of monomorphic wavy nuclei cells intermingled with thin wavy collagen fibers (Figure 5). Immunohistochemicalstudy was positive for S-100 protein in the neuroid tissues (Figure 6) as well as epithelial membraneantigen and CD34; actin and CD68 were negative. Based on the histologic and clinical findings, the patient was diagnosed with segmental NF characterized by blue-red pseudoatrophic plaques.
Comment
Segmental NF, a rare condition that is 10 to 20 times less frequent than NF type I, commonly presents with unilateral neurofibromas confined to a circumscribed body segment.2,5-7 The most common cutaneous marks in this rare disease are cafè au lait spots and axillary freckling, which typically are localized to the same anatomic region. In contrast to NF type I and II, systemic involvement and malignancies are uncommon in segmental NF.8-10 Cutaneous neurofibromas are benign tumors of the peripheral nerve that appear as soft, flesh-colored or slightly tan, sessile or polypoid papules or nodules that typically range in width from a few millimeters to several centimeters. These lesions typically appear after 10 years of age.
Other rare clinical types of neurofibromas include the plexiform, diffuse, and blue-red pseudoatrophic patches.3 In particular, the blue-red pseudoatrophic variant is considered a helpful clinical hallmark for the diagnosis of NF, especially due to its early onset in the disease course. It usually appears during the first months of life or can possibly be congenital.3,11
Neurofibromas classically present as well-circumscribed dermal nodules that consist of spindle-shaped cells and bundles of eosinophilic wavy fibrous tissue in the reticular dermis, which often also affect the subcutaneous tissue. Conversely, in the blue-red pseudoatrophic variant, tumor cells are associated with less connective tissue and with a reduction of collagen in the reticular dermis from diffuse replacement of neuroid tissue, even though there are no histologic signs of true atrophy.3 Furthermore, the blue-red color is most likely due to the vascular abnormalities, such as ectatic or thick-walled blood vessels overlying the subcutaneous fibromatous tissue.
We found different descriptions of this variant of neurofibroma in the literature with some clinical or histologic differences. The lesions are described as blue-red or cerulean macules, and on histology the angiomatous component is dominant.3,12 In other reports, the main clinical feature is skin atrophy. Lesions can be classified as pseudoatrophic plaques, dermal hypoplasia, or pseudoatrophic macules,3,4,11,13,14 which are different names for the same variant of blue-red pseudoatrophic neurofibromas.
Clinical studies on this neurofibroma refer to patients affected by NF type I; in 1 case the lesions appeared as segmental NF.14
Conclusion
Segmental NF is characterized by an unusual clinical onset of multiple and localized pseudoatrophic plaques in the absence of the common clinical features of NF. We recommend that pseudoatrophic patches undergo histologic examination for early diagnosis of rare cases of NF with such an unusual presentation.
1. Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010;12:1-11.
2. Hager CM, Cohen PR, Tschen JA. Segmental neurofibromatosis: case reports and review. J Am Acad Dermatol. 1997;37(5, pt 2):864-869.
3. Westerhof W, Konrad K. Blue-red macules and pseudoatrophic macules: additional cutaneous signs in neurofibromatosis. Arch Dermatol. 1982;118:577-581.
4. Piqué E, Olivares M, Fariña MC, et al. Pseudoatrophic macules: a variant of neurofibroma. Cutis. 1996;57:100-102.
5. Roth RR, Martines R, James WD. Segmental neurofibromatosis. Arch Dermatol. 1987;123:917-920.
6. Gonzalez G, Russi ME, Lodeiros A. Bilateral segmental neurofibromatosis: a case report and review. Pediatr Neurol. 2007;36:51-53.
7. Redlick FP, Shaw J. Segmental neurofibromatosis follows Blaschko’s lines or dermatomes depending on the cell line affected: case report and literature review. J Cutan Med Surg. 2004;8:353-356.
8. Friedman DP. Segmental neurofibromatosis (NF-5): a rare form of neurofibromatosis. Am J Neuroradiol. 1991;12:971-972.
9. Dang JD, Cohen PR. Segmental neurofibromatosis and malignancy. Skinmed. 2010;8:156-159.
10. Mansur AT, Göktay F, Akkaya AD, et al. Segmental neurofibromatosis: report of 3 cases. Cutis. 2011;87:45-50.
11. Kwon KS, Seo KH, Jang HS, et al. A case of congenital reddish neurofibromatous dermal hypoplasia. Cutis. 2001;68:253-256.
12. Vabres P, de Lonlay P, Amiel J, et al. Angiomatous and cerulodermic macules: early cutaneous signs of neurofibromatosis type I [in French]. Ann Dermatol Venereol. 1998;125:593-594.
13. Misago N, Narisawa Y. Localized multiple pseudoatrophic plaques: a rare clinical form of segmental neurofibromatosis. Acta Derm Venereol. 2005;85:522-523.
14. Norris JF, Smith AG, Fletcher PJ, et al. Neurofibromatous dermal hypoplasia: a clinical, pharmacological and ultrastructural study. Br J Dermatol. 1985;112:435-441.
In the setting of neurofibromatosis (NF), neurofibromas commonly appear as flesh-colored nodular lesions.1 The presence of blue-red pseudoatrophic neurofibromas is rare, with only 1 known case of the segmental variant.2 Microscopic examination typically reveals thick-walled blood vessels in the papillary dermis and neurofibromatous tissue in the hypodermis. The neuroid proliferation is associated with the reduction of collagen tissue. This type of neurofibroma has an early presentation and it can be helpful in the diagnosis of some cases of NF.3,4
Case Report
A 5-year-old girl presented with 2 blue-red, well-demarcated, atrophic patches on the left leg. One plaque was localized on the left thigh, which had appeared at 7 months of age, and the other was on the left calf, which presented at 2 years of age (Figure 1). The lesions were 10- to 15-cm in diameter, roughly oval shaped, and completely asymptomatic. The skin overlying the atrophic patches showed a visible venous reticulum, and palpation revealed multiple nodular lesions. Physical examination revealed no cafè au lait spots, axillary freckling, Lisch nodules, or clinical signs of NF. Her family history was negative for NF. Physical and neurologic examinations revealed no abnormalities.
Biopsy specimens were obtained from 1 of the atrophic patches and from 1 of the nodules. Microscopic examination of the atrophic patch showed a dermal proliferation of spindle elements dispersed in loose connective tissue (Figure 2) and ectatic (Figure 3) or thick-walled (Figure 4) blood vessels. Microscopic exam-ination of the nodule disclosed a dermohypodermal neoplastic proliferation composed of monomorphic wavy nuclei cells intermingled with thin wavy collagen fibers (Figure 5). Immunohistochemicalstudy was positive for S-100 protein in the neuroid tissues (Figure 6) as well as epithelial membraneantigen and CD34; actin and CD68 were negative. Based on the histologic and clinical findings, the patient was diagnosed with segmental NF characterized by blue-red pseudoatrophic plaques.
Comment
Segmental NF, a rare condition that is 10 to 20 times less frequent than NF type I, commonly presents with unilateral neurofibromas confined to a circumscribed body segment.2,5-7 The most common cutaneous marks in this rare disease are cafè au lait spots and axillary freckling, which typically are localized to the same anatomic region. In contrast to NF type I and II, systemic involvement and malignancies are uncommon in segmental NF.8-10 Cutaneous neurofibromas are benign tumors of the peripheral nerve that appear as soft, flesh-colored or slightly tan, sessile or polypoid papules or nodules that typically range in width from a few millimeters to several centimeters. These lesions typically appear after 10 years of age.
Other rare clinical types of neurofibromas include the plexiform, diffuse, and blue-red pseudoatrophic patches.3 In particular, the blue-red pseudoatrophic variant is considered a helpful clinical hallmark for the diagnosis of NF, especially due to its early onset in the disease course. It usually appears during the first months of life or can possibly be congenital.3,11
Neurofibromas classically present as well-circumscribed dermal nodules that consist of spindle-shaped cells and bundles of eosinophilic wavy fibrous tissue in the reticular dermis, which often also affect the subcutaneous tissue. Conversely, in the blue-red pseudoatrophic variant, tumor cells are associated with less connective tissue and with a reduction of collagen in the reticular dermis from diffuse replacement of neuroid tissue, even though there are no histologic signs of true atrophy.3 Furthermore, the blue-red color is most likely due to the vascular abnormalities, such as ectatic or thick-walled blood vessels overlying the subcutaneous fibromatous tissue.
We found different descriptions of this variant of neurofibroma in the literature with some clinical or histologic differences. The lesions are described as blue-red or cerulean macules, and on histology the angiomatous component is dominant.3,12 In other reports, the main clinical feature is skin atrophy. Lesions can be classified as pseudoatrophic plaques, dermal hypoplasia, or pseudoatrophic macules,3,4,11,13,14 which are different names for the same variant of blue-red pseudoatrophic neurofibromas.
Clinical studies on this neurofibroma refer to patients affected by NF type I; in 1 case the lesions appeared as segmental NF.14
Conclusion
Segmental NF is characterized by an unusual clinical onset of multiple and localized pseudoatrophic plaques in the absence of the common clinical features of NF. We recommend that pseudoatrophic patches undergo histologic examination for early diagnosis of rare cases of NF with such an unusual presentation.
In the setting of neurofibromatosis (NF), neurofibromas commonly appear as flesh-colored nodular lesions.1 The presence of blue-red pseudoatrophic neurofibromas is rare, with only 1 known case of the segmental variant.2 Microscopic examination typically reveals thick-walled blood vessels in the papillary dermis and neurofibromatous tissue in the hypodermis. The neuroid proliferation is associated with the reduction of collagen tissue. This type of neurofibroma has an early presentation and it can be helpful in the diagnosis of some cases of NF.3,4
Case Report
A 5-year-old girl presented with 2 blue-red, well-demarcated, atrophic patches on the left leg. One plaque was localized on the left thigh, which had appeared at 7 months of age, and the other was on the left calf, which presented at 2 years of age (Figure 1). The lesions were 10- to 15-cm in diameter, roughly oval shaped, and completely asymptomatic. The skin overlying the atrophic patches showed a visible venous reticulum, and palpation revealed multiple nodular lesions. Physical examination revealed no cafè au lait spots, axillary freckling, Lisch nodules, or clinical signs of NF. Her family history was negative for NF. Physical and neurologic examinations revealed no abnormalities.
Biopsy specimens were obtained from 1 of the atrophic patches and from 1 of the nodules. Microscopic examination of the atrophic patch showed a dermal proliferation of spindle elements dispersed in loose connective tissue (Figure 2) and ectatic (Figure 3) or thick-walled (Figure 4) blood vessels. Microscopic exam-ination of the nodule disclosed a dermohypodermal neoplastic proliferation composed of monomorphic wavy nuclei cells intermingled with thin wavy collagen fibers (Figure 5). Immunohistochemicalstudy was positive for S-100 protein in the neuroid tissues (Figure 6) as well as epithelial membraneantigen and CD34; actin and CD68 were negative. Based on the histologic and clinical findings, the patient was diagnosed with segmental NF characterized by blue-red pseudoatrophic plaques.
Comment
Segmental NF, a rare condition that is 10 to 20 times less frequent than NF type I, commonly presents with unilateral neurofibromas confined to a circumscribed body segment.2,5-7 The most common cutaneous marks in this rare disease are cafè au lait spots and axillary freckling, which typically are localized to the same anatomic region. In contrast to NF type I and II, systemic involvement and malignancies are uncommon in segmental NF.8-10 Cutaneous neurofibromas are benign tumors of the peripheral nerve that appear as soft, flesh-colored or slightly tan, sessile or polypoid papules or nodules that typically range in width from a few millimeters to several centimeters. These lesions typically appear after 10 years of age.
Other rare clinical types of neurofibromas include the plexiform, diffuse, and blue-red pseudoatrophic patches.3 In particular, the blue-red pseudoatrophic variant is considered a helpful clinical hallmark for the diagnosis of NF, especially due to its early onset in the disease course. It usually appears during the first months of life or can possibly be congenital.3,11
Neurofibromas classically present as well-circumscribed dermal nodules that consist of spindle-shaped cells and bundles of eosinophilic wavy fibrous tissue in the reticular dermis, which often also affect the subcutaneous tissue. Conversely, in the blue-red pseudoatrophic variant, tumor cells are associated with less connective tissue and with a reduction of collagen in the reticular dermis from diffuse replacement of neuroid tissue, even though there are no histologic signs of true atrophy.3 Furthermore, the blue-red color is most likely due to the vascular abnormalities, such as ectatic or thick-walled blood vessels overlying the subcutaneous fibromatous tissue.
We found different descriptions of this variant of neurofibroma in the literature with some clinical or histologic differences. The lesions are described as blue-red or cerulean macules, and on histology the angiomatous component is dominant.3,12 In other reports, the main clinical feature is skin atrophy. Lesions can be classified as pseudoatrophic plaques, dermal hypoplasia, or pseudoatrophic macules,3,4,11,13,14 which are different names for the same variant of blue-red pseudoatrophic neurofibromas.
Clinical studies on this neurofibroma refer to patients affected by NF type I; in 1 case the lesions appeared as segmental NF.14
Conclusion
Segmental NF is characterized by an unusual clinical onset of multiple and localized pseudoatrophic plaques in the absence of the common clinical features of NF. We recommend that pseudoatrophic patches undergo histologic examination for early diagnosis of rare cases of NF with such an unusual presentation.
1. Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010;12:1-11.
2. Hager CM, Cohen PR, Tschen JA. Segmental neurofibromatosis: case reports and review. J Am Acad Dermatol. 1997;37(5, pt 2):864-869.
3. Westerhof W, Konrad K. Blue-red macules and pseudoatrophic macules: additional cutaneous signs in neurofibromatosis. Arch Dermatol. 1982;118:577-581.
4. Piqué E, Olivares M, Fariña MC, et al. Pseudoatrophic macules: a variant of neurofibroma. Cutis. 1996;57:100-102.
5. Roth RR, Martines R, James WD. Segmental neurofibromatosis. Arch Dermatol. 1987;123:917-920.
6. Gonzalez G, Russi ME, Lodeiros A. Bilateral segmental neurofibromatosis: a case report and review. Pediatr Neurol. 2007;36:51-53.
7. Redlick FP, Shaw J. Segmental neurofibromatosis follows Blaschko’s lines or dermatomes depending on the cell line affected: case report and literature review. J Cutan Med Surg. 2004;8:353-356.
8. Friedman DP. Segmental neurofibromatosis (NF-5): a rare form of neurofibromatosis. Am J Neuroradiol. 1991;12:971-972.
9. Dang JD, Cohen PR. Segmental neurofibromatosis and malignancy. Skinmed. 2010;8:156-159.
10. Mansur AT, Göktay F, Akkaya AD, et al. Segmental neurofibromatosis: report of 3 cases. Cutis. 2011;87:45-50.
11. Kwon KS, Seo KH, Jang HS, et al. A case of congenital reddish neurofibromatous dermal hypoplasia. Cutis. 2001;68:253-256.
12. Vabres P, de Lonlay P, Amiel J, et al. Angiomatous and cerulodermic macules: early cutaneous signs of neurofibromatosis type I [in French]. Ann Dermatol Venereol. 1998;125:593-594.
13. Misago N, Narisawa Y. Localized multiple pseudoatrophic plaques: a rare clinical form of segmental neurofibromatosis. Acta Derm Venereol. 2005;85:522-523.
14. Norris JF, Smith AG, Fletcher PJ, et al. Neurofibromatous dermal hypoplasia: a clinical, pharmacological and ultrastructural study. Br J Dermatol. 1985;112:435-441.
1. Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010;12:1-11.
2. Hager CM, Cohen PR, Tschen JA. Segmental neurofibromatosis: case reports and review. J Am Acad Dermatol. 1997;37(5, pt 2):864-869.
3. Westerhof W, Konrad K. Blue-red macules and pseudoatrophic macules: additional cutaneous signs in neurofibromatosis. Arch Dermatol. 1982;118:577-581.
4. Piqué E, Olivares M, Fariña MC, et al. Pseudoatrophic macules: a variant of neurofibroma. Cutis. 1996;57:100-102.
5. Roth RR, Martines R, James WD. Segmental neurofibromatosis. Arch Dermatol. 1987;123:917-920.
6. Gonzalez G, Russi ME, Lodeiros A. Bilateral segmental neurofibromatosis: a case report and review. Pediatr Neurol. 2007;36:51-53.
7. Redlick FP, Shaw J. Segmental neurofibromatosis follows Blaschko’s lines or dermatomes depending on the cell line affected: case report and literature review. J Cutan Med Surg. 2004;8:353-356.
8. Friedman DP. Segmental neurofibromatosis (NF-5): a rare form of neurofibromatosis. Am J Neuroradiol. 1991;12:971-972.
9. Dang JD, Cohen PR. Segmental neurofibromatosis and malignancy. Skinmed. 2010;8:156-159.
10. Mansur AT, Göktay F, Akkaya AD, et al. Segmental neurofibromatosis: report of 3 cases. Cutis. 2011;87:45-50.
11. Kwon KS, Seo KH, Jang HS, et al. A case of congenital reddish neurofibromatous dermal hypoplasia. Cutis. 2001;68:253-256.
12. Vabres P, de Lonlay P, Amiel J, et al. Angiomatous and cerulodermic macules: early cutaneous signs of neurofibromatosis type I [in French]. Ann Dermatol Venereol. 1998;125:593-594.
13. Misago N, Narisawa Y. Localized multiple pseudoatrophic plaques: a rare clinical form of segmental neurofibromatosis. Acta Derm Venereol. 2005;85:522-523.
14. Norris JF, Smith AG, Fletcher PJ, et al. Neurofibromatous dermal hypoplasia: a clinical, pharmacological and ultrastructural study. Br J Dermatol. 1985;112:435-441.
- Biopsy should be considered for pseudoatrophic patches to perform early diagnosis of neurofibroma-tosis (NF), which is rare.
- Blue-red or cerulean macules, especially if associated with skin atrophy, are highly suggestive of neurofibroma in a patient affected by NF.