User login
Preparing Veterans Health Administration Psychologists to Meet the Complex Needs of Aging Veterans
The Veterans Health Administration (VHA) is understaffed for clinical psychologists who have specialty training in geriatrics (ie, geropsychologists) to meet the needs of aging veterans. Though only 16.8% of US adults are aged ≥ 65 years,1 this age group comprises 45.9% of patients within the VHA.2 The needs of older adults are complex and warrant specialized services from mental health clinicians trained to understand lifespan developmental processes, biological changes associated with aging, and changes in psychosocial functioning.
Older veterans (aged ≥ 65 years) present with higher rates of combined medical and mental health diagnoses compared to both younger veterans and older adults who are not veterans.3 Nearly 1 of 5 (18.1%) older veterans who use VHA services have confirmed mental health diagnoses, and an additional 25.5% have documented mental health concerns without a formal diagnosis in their health record.4 The clinical presentations of older veterans frequently differ from younger adults and include greater complexity. For example, older veterans face an increased risk of cognitive impairment compared to the general population, due in part to higher prevalence of posttraumatic stress, which doubles their risk of developing dementia.5 Additional examples of multicomplexity among older veterans may include co-occurring medical and psychiatric diagnoses, the presence of delirium, social isolation/loneliness, and concerns related to polypharmacy. These complex presentations result in significant challenges for mental health clinicians in areas like assessment (eg, accuracy of case conceptualization), intervention (eg, selection and prioritization), and consultation (eg, coordination among multiple medical and mental health specialists).
Older veterans also present with substantial resilience. Research has found that aging veterans exposed to trauma during their military service often review their memories and past experiences, which is known as later-adulthood trauma reengagement.6 Through this normative life review process, veterans engage with memories and experiences from their past that they previously avoided, which could lead to posttraumatic growth for some. Unfortunately, others may experience an increase in psychological distress. Mental health clinicians with specialty expertise and training in aging and lifespan development can facilitate positive outcomes to reduce distress.7
The United States in general, and the VHA specifically, face a growing shortage of geriatric mental health clinicians.
The Geriatric Scholars Program (GSP) was developed in 2008 to address the training gap and provide education in geriatrics to VHA clinicians that treat older veterans, particularly in rural areas.11,12 The GSP initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists. It was later expanded to include other disciplines (ie, social work, rehabilitation therapists, and psychiatrists). In 2013, the GSP – Psychology Track (GSP-P) was developed with funding from the VHA Offices of Rural Health and Geriatrics and Extended Care specifically for psychologists.
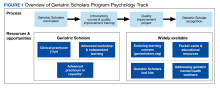
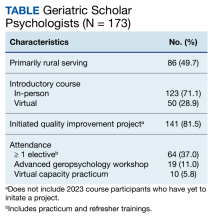
This article describes the multicomponent longitudinal GSP-P, which has evolved to meet the target audience’s ongoing needs for knowledge, skills, and opportunities to refine practice behaviors. GSP-P received the 2020 Award for Excellence in Geropsychology Training from the Council of Professional Geropsychology Training Programs. GSP-P has grown within the context of the larger GSP and aligns with the other existing elective learning opportunities (Figure 1).
Program description
Introductory Course
Psychologist subject matter experts (SMEs) developed an intensive course in geropsychology in the absence of a similar course in the geriatric medicine board review curriculum. SMEs reviewed the guidelines for practice by professional organizations like the Pikes Peak Geropsychology Competencies,which outline knowledge and skills in various domains.13 SMEs integrated this review with findings from a needs assessment for postlicensed VHA psychology staff in 4 health care systems, drafted a syllabus, and circulated it to geropsychology experts for feedback. The resulting multiday course covered general mental health as well as topics particularly salient for mental health clinicians treating older veterans including suicide prevention and posttraumatic stress disorder (PTSD).14 This Geropsychology Competencies Review Course was piloted in 1 region initially before being offered nationally in 2014.
Quality Improvement
Introductory course attendees also participate in an intensive day-long interactive workshop in quality improvement (QI). After completing these trainings, they apply what they have learned at their home facility by embarking on a QI project related to geriatrics. The QI projects reinforce learning and initiate practice changes not only for attendees but at times the larger health care system. Topics are selected by scholars in response to the needs they observe in their clinics. Recent GSP projects include efforts to increase screenings for depression and anxiety, improve adherence to VHA dementia policy, increase access to virtual care, and increase referrals to programs such as whole health or cognitive behavioral therapy for insomnia, a first-line treatment for insomnia in older adults.17 Another project targeted the improvement of referrals to the Compassionate Contact Corps in an effort to reduce social isolation and loneliness among older veterans.18 Evaluations demonstrate significant improvement in scholars’ confidence in related program development and management from precourse to 3 months postcourse.15
Webinars
The Addressing Geriatric Mental Health webinar series was created to introduce learners to topics that could not be covered in the introductory course. Topics were suggested by the expert reviewers of the curriculum or identified by the scholars themselves (eg, chronic pain, sexuality, or serious mental illness). A secondary function of the webinars was to reach a broader audience. Over time, scholars and webinar attendees requested opportunities to explore topics in greater depth (eg, PTSD later in life). These requests led the webinars to focus on annual themes.
The series is open to all disciplines of geriatric scholars, VHA staff, and non-VHA staff through the Veterans Affairs Talent Management System and the TRAIN Learning Network (train.org). Attendance for the 37 webinars was captured from logins to the virtual learning platform and may underestimate attendance if a group attended on a single screen. Average attendance increased from 157 attendees/webinar in 2015 to 418 attendees/webinar in 2023 (Figure 2). This may have been related to the increase in virtual learning during the COVID-19 pandemic, but represents a 166% increase in audience from the inaugural year of the series.
Advanced Learning Opportunities
To invest in the ongoing growth and development of introductory course graduates, GSP-P developed and offered an advanced workshop in 2019. This multiday workshop focused on further enhancement of geropsychology competencies, with an emphasis on treating older veterans with mental and physical comorbidities. Didactics and experiential learning exercises led by SMEs covered topics such as adjusting to chronic illness, capacity assessment, PTSD, insomnia and sleep changes, chronic pain, and psychological interventions in palliative care and hospice settings. Evaluation findings demonstrated significant improvements from precourse to 6 months postcourse in confidence and knowledge as
To facilitate ongoing and individually tailored learning following the advanced workshop, scholars also developed and executed independent learning plans (ILPs) during a 6-month window with consultation from an experienced geropsychologist. Fifteen of 19 scholars (78.9%) completed ILPs with an average of 3 learning goals listed. After completing the ILPs, scholars endorsed their clinical and/or personal usefulness, citing increased confidence, enhanced skills for use with patients with complex needs, personal fulfillment, and career advancement. Most scholars noted ILPs were feasible and learning resources were accessible. Overall, the evaluation found ILPs to be a valuable way to enhance psychologists’ learning and effectiveness in treating older veterans with complex health needs.20
Clinical Practica
All geriatric scholars who completed the program have additional opportunities for professional development through practicum experiences focused on specific clinical approaches to the care of older veterans, such as dementia care, pain management, geriatric assessment, and palliative care. These practica provide scholars with individualized learning experiences in an individualized or small group setting and may be conducted either in-person or virtually.
In response to an expressed need from those who completed the program, the GSP-P planning committee collaborated with an SME to develop a virtual practicum to assess patients’ decision making capacity. Evaluating capacities among older adults is a common request, yet clinicians report little to no formal training in how to conceptualize and approach these complex questions.21,22 Utilizing an evidence-informed and structured approach promotes the balancing of an older adult’s autonomy and professional ethics. Learning capacity evaluation skills could better position psychologists to not only navigate complex ethical, legal, and clinical situations, but also serve as expert consultants to interdisciplinary teams. This virtual practicum was initiated in 2022 and to date has included 10 scholars. The practicum includes multiple modalities of learning: (1) self-directed review of core concepts; (2) attendance at 4 capacity didactics focused on introduction to evaluating capacities, medical consent and decision making, financial decision making and management, and independent living; and (3) participation in 5 group consultations on capacity evaluations conducted at their home sites. During these group consultations, additional case examples were shared to reinforce capacity concepts.
Discussion
The objective of GSP-P is to enhance geropsychology practice competencies among VHA psychologists given the outsized representation of older adults within the VHA system and their complex care needs. The curricula have significantly evolved to accomplish this, expanding the reach and investing in the continuing growth and development of scholars.
There are several elements that set GSP apart from other geriatric and geropsychology continuing medical education programs. The first is that the training is veteran focused, allowing us to discuss the unique impact military service has on aging. Similarly, because all scholars work within the integrated health care system, we can introduce and review key resources and programs that benefit all veterans and their families/care partners across the system. Through the GSP, the VA invests in ongoing professional development. Scholars can participate in additional experiential practica, webinars, and advanced workshops tailored to their individual learning needs. Lastly, the GSP works to create a community among its scholars where they can not only continue to consult with presenters/instructors, but also one another. A planned future direction for the GSP-P is to incorporate quarterly office hours and discussions for alumni to develop an increased sense of community. This may strengthen commitment to the overall VA mission, leading to increased retainment of talent who now have the knowledge, skills, and confidence to care for aging veterans.
Limitations
GSP is limited by its available funding. Additionally, the number of participants who can enroll each year in GSP-P (not including webinars) is capped by policy. Another limitation is the number of QI coaches available to mentor scholars on their projects.
Conclusions
Outcomes of GSP-P have been extremely favorable. Following participation in the program, we have found a significant increase in confidence in geropsychology practice among clinicians, as well as enhanced knowledge and skills across competency domains.15,19 We have observed rising attendance in our annual webinar series and graduates of our introductory courses participate in subsequent trainings (eg, advanced workshop or virtual practicum). Several graduates of GSP-P have become board certified in geropsychology by the American Board of Geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows. This suggests that the reach of GSP-P programming may extend farther than reported in this article.
The needs of aging veterans have also changed based on cohort differences, as the population of World War II and Korean War era veterans has declined and the number of older Vietnam era veterans has grown. We expect different challenges with older Gulf War and post-9/11 era veterans. For instance, 17% of troops deployed to Iraq or Afghanistan following 9/11 experienced mild traumatic brain injury (TBI), and 59% of those experienced > 1 mild TBI.23 Research indicates that younger post-9/11 veterans have a 3-fold risk of developing early onset dementia after experiencing a TBI.24 Therefore, even though post-9/11 veterans are not older in terms of chronological age, some may experience symptoms and conditions more often occurring in older veterans. As a result, it would be beneficial for clinicians to learn about the presentation and treatment of geriatric conditions such as dementia.
Moving forward, the GSP-P should identify potential opportunities to collaborate with the non-VHA mental health community–which also faces a shortage of geriatric mental health clinicians–to extend educational opportunities to improve care for veterans in all settings (eg, cosponsor training opportunities open to both VHA and non-VHA clinicians).8,25 Many aging veterans may receive portions of their health care outside the VHA, particularly those who reside in rural areas. Additionally, as veterans age, so do their support systems (eg, family members, friends, spouses, caregivers, and even clinicians), most of whom will receive care outside of the VHA. Community education collaborations will not only improve the care of older veterans, but also the care of older adults in the general population.
Promising directions include the adoption of the GSP model in other health care settings. Recently, Indian Health Service has adapted the model, beginning with primary care clinicians and pharmacists and is beginning to expand to other disciplines. Additional investments in VHA workforce training include the availability of geropsychology internship and fellowship training opportunities through the Office of Academic Affiliations, which provide earlier opportunities to specialize in geropsychology. Continued investment in both prelicensure and postpsychology licensure training efforts are needed within the VHA to meet the geriatric mental health needs of veterans.
Acknowledgments
The authors wish to acknowledge Terri Huh, PhD, for her contributions to the development and initiation of the GSP-P. The authors also appreciate the collaboration and quality initiative training led by Carol Callaway-Lane, DNP, ACNP-BC, and her team.
1. Caplan Z, Rabe M; US Department of Commerce, US Census Bureau. The Older Population: 2020 (Census Brief No. C2020BR-07). May 2023. Accessed February 27, 2024. https://www2.census.gov/library/publications/decennial/2020/census-briefs/c2020br-07.pdf
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. VA benefits & health care utilization. Updated February 2023. Accessed February 27, 2024. https://www.va.gov/vetdata/docs/pocketcards/fy2023q2.PDF
3. O’Malley KA, Vinson L, Pless Kaiser A, Sager Z, Hinrichs K. Mental health and aging veterans: How the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
4. Greenberg G, Hoff R. FY 2021 Older Adult (65+ on October 1st) Veteran Data Sheet: National, VISN, and Healthcare System Tables. West Haven, CT: U.S. Department of Veterans Affairs, Northeast Program Evaluation Center. 2022.
5. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613. doi:10.1001/archgenpsychiatry.2010.61
6. Davison EH, Kaiser AP, Spiro A 3rd, Moye J, King LA, King DW. From late-onset stress symptomatology to later-adulthood trauma reengagement in aging combat veterans: Taking a broader view. Gerontologist. 2016;56(1):14-21. doi:10.1093/geront/gnv097
7. Kaiser AP, Boyle JT, Bamonti PM, O’Malley K, Moye J. Development, adaptation, and clinical implementation of the Later-Adulthood Trauma Reengagement (LATR) group intervention for older veterans. Psychol Serv. 2023;20(4):863-875. doi:10.1037/ser0000736
8. Moye J, Karel MJ, Stamm KE, et al. Workforce analysis of psychological practice with older adults: Growing crisis requires urgent action. Train Educ Prof Psychol. 2019;13(1):46-55. doi:10.1037/tep0000206
9. Stamm K, Lin L, Conroy J. Critical needs in geropsychology. Monitor on Psychology. 2021;52(4):21.
10. American Board of Geropsychology. Specialists. 2024. Accessed February 6, 2024. https://abgero.org/board-members/specialists/
11. Kramer BJ. The VA Geriatric Scholars Program. Fed Pract. 2015;32(5):46-48.
12. Kramer BJ, Creekmur B, Howe JL, et al. Veterans Affairs Geriatric Scholars Program: Enhancing existing primary care clinician skills in caring for older veterans. J Am Geriatr Soc. 2016;64(11):2343-2348. doi:10.1111/jgs.14382
13. Knight BG, Karel MJ, Hinrichsen GA, Qualls SH, Duffy M. Pikes Peak model for training in professional geropsychology. Am Psychol. 2009;64(3):205-14. doi:10.1037/a0015059
14. Huh JWT, Rodriguez R, Gould CE, R Brunskill S, Melendez L, Kramer BJ. Developing a program to increase geropsychology competencies of Veterans Health Administration (VHA) psychologists. Gerontol Geriatr Educ. 2020;41(4):463-479. doi:10.1080/02701960.2018.1491402
15. Huh JWT, Rodriguez RL, Gregg JJ, Scales AN, Kramer BJ, Gould CE. Improving geropsychology competencies of Veterans Affairs psychologists. J Am Geriatr Soc. 2021;69(3):798-805. doi:10.1111/jgs.17029
16. Karel MJ, Emery EE, Molinari V; CoPGTP Task Force on the Assessment of Geropsychology Competencies. Development of a tool to evaluate geropsychology knowledge and skill competencies. Int Psychogeriatr. 2010;22(6):886-896. doi:10.1017/S1041610209991736
17. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
18. Sullivan J, Gualtieri L, Campbell M, Davila H, Pendergast J, Taylor P. VA Compassionate Contact Corps: a phone-based intervention for veterans interested in speaking with peers. Innov Aging. 2021;5(Suppl 1):204. doi:10.1093/geroni/igab046.788
19. Gregg JJ, Rodriguez RL, Mehta PS, Kramer BJ, Gould CE. Enhancing specialty training in geropsychology competencies: an evaluation of a VA Geriatric Scholars Program advanced topics workshop. Gerontol Geriatr Educ. 2023;44(3):329-338. doi:10.1080/02701960.2022.2069764
20. Gould CE, Rodriguez RL, Gregg J, Mehta PS, Kramer J. Mentored independent learning plans among psychologists: a mixed methods investigation. J Amer Geriatr Soc. 2023;71(S1):S53.
21. Mullaly E, Kinsella G, Berberovic N, et al. Assessment of decision-making capacity: exploration of common practices among neuropsychologists. Aust Psychol. 2007;42:178-186. doi:10.1080/00050060601187142
22. Seyfried L, Ryan KA, Kim SYH. Assessment of decision-making capacity: Views and experiences of consultation psychiatrists. Psychosomatics. 2013;54(2):115-123. doi:10.1016/j.psym.2012.08.001
23. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257. doi:10.1097/PSY.0b013e318244c604
24. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627.doi:10.1080/02699052.2022.2033846
25. Merz CC, Koh D, Sakai EY, et al. The big shortage: Geropsychologists discuss facilitators and barriers to working in the field of aging. Transl Issues Psychol Sci. 2017;3(4):388-399. doi:10.1037/tps0000137
The Veterans Health Administration (VHA) is understaffed for clinical psychologists who have specialty training in geriatrics (ie, geropsychologists) to meet the needs of aging veterans. Though only 16.8% of US adults are aged ≥ 65 years,1 this age group comprises 45.9% of patients within the VHA.2 The needs of older adults are complex and warrant specialized services from mental health clinicians trained to understand lifespan developmental processes, biological changes associated with aging, and changes in psychosocial functioning.
Older veterans (aged ≥ 65 years) present with higher rates of combined medical and mental health diagnoses compared to both younger veterans and older adults who are not veterans.3 Nearly 1 of 5 (18.1%) older veterans who use VHA services have confirmed mental health diagnoses, and an additional 25.5% have documented mental health concerns without a formal diagnosis in their health record.4 The clinical presentations of older veterans frequently differ from younger adults and include greater complexity. For example, older veterans face an increased risk of cognitive impairment compared to the general population, due in part to higher prevalence of posttraumatic stress, which doubles their risk of developing dementia.5 Additional examples of multicomplexity among older veterans may include co-occurring medical and psychiatric diagnoses, the presence of delirium, social isolation/loneliness, and concerns related to polypharmacy. These complex presentations result in significant challenges for mental health clinicians in areas like assessment (eg, accuracy of case conceptualization), intervention (eg, selection and prioritization), and consultation (eg, coordination among multiple medical and mental health specialists).
Older veterans also present with substantial resilience. Research has found that aging veterans exposed to trauma during their military service often review their memories and past experiences, which is known as later-adulthood trauma reengagement.6 Through this normative life review process, veterans engage with memories and experiences from their past that they previously avoided, which could lead to posttraumatic growth for some. Unfortunately, others may experience an increase in psychological distress. Mental health clinicians with specialty expertise and training in aging and lifespan development can facilitate positive outcomes to reduce distress.7
The United States in general, and the VHA specifically, face a growing shortage of geriatric mental health clinicians.
The Geriatric Scholars Program (GSP) was developed in 2008 to address the training gap and provide education in geriatrics to VHA clinicians that treat older veterans, particularly in rural areas.11,12 The GSP initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists. It was later expanded to include other disciplines (ie, social work, rehabilitation therapists, and psychiatrists). In 2013, the GSP – Psychology Track (GSP-P) was developed with funding from the VHA Offices of Rural Health and Geriatrics and Extended Care specifically for psychologists.
This article describes the multicomponent longitudinal GSP-P, which has evolved to meet the target audience’s ongoing needs for knowledge, skills, and opportunities to refine practice behaviors. GSP-P received the 2020 Award for Excellence in Geropsychology Training from the Council of Professional Geropsychology Training Programs. GSP-P has grown within the context of the larger GSP and aligns with the other existing elective learning opportunities (Figure 1).
Program description
Introductory Course
Psychologist subject matter experts (SMEs) developed an intensive course in geropsychology in the absence of a similar course in the geriatric medicine board review curriculum. SMEs reviewed the guidelines for practice by professional organizations like the Pikes Peak Geropsychology Competencies,which outline knowledge and skills in various domains.13 SMEs integrated this review with findings from a needs assessment for postlicensed VHA psychology staff in 4 health care systems, drafted a syllabus, and circulated it to geropsychology experts for feedback. The resulting multiday course covered general mental health as well as topics particularly salient for mental health clinicians treating older veterans including suicide prevention and posttraumatic stress disorder (PTSD).14 This Geropsychology Competencies Review Course was piloted in 1 region initially before being offered nationally in 2014.
Quality Improvement
Introductory course attendees also participate in an intensive day-long interactive workshop in quality improvement (QI). After completing these trainings, they apply what they have learned at their home facility by embarking on a QI project related to geriatrics. The QI projects reinforce learning and initiate practice changes not only for attendees but at times the larger health care system. Topics are selected by scholars in response to the needs they observe in their clinics. Recent GSP projects include efforts to increase screenings for depression and anxiety, improve adherence to VHA dementia policy, increase access to virtual care, and increase referrals to programs such as whole health or cognitive behavioral therapy for insomnia, a first-line treatment for insomnia in older adults.17 Another project targeted the improvement of referrals to the Compassionate Contact Corps in an effort to reduce social isolation and loneliness among older veterans.18 Evaluations demonstrate significant improvement in scholars’ confidence in related program development and management from precourse to 3 months postcourse.15
Webinars
The Addressing Geriatric Mental Health webinar series was created to introduce learners to topics that could not be covered in the introductory course. Topics were suggested by the expert reviewers of the curriculum or identified by the scholars themselves (eg, chronic pain, sexuality, or serious mental illness). A secondary function of the webinars was to reach a broader audience. Over time, scholars and webinar attendees requested opportunities to explore topics in greater depth (eg, PTSD later in life). These requests led the webinars to focus on annual themes.
The series is open to all disciplines of geriatric scholars, VHA staff, and non-VHA staff through the Veterans Affairs Talent Management System and the TRAIN Learning Network (train.org). Attendance for the 37 webinars was captured from logins to the virtual learning platform and may underestimate attendance if a group attended on a single screen. Average attendance increased from 157 attendees/webinar in 2015 to 418 attendees/webinar in 2023 (Figure 2). This may have been related to the increase in virtual learning during the COVID-19 pandemic, but represents a 166% increase in audience from the inaugural year of the series.
Advanced Learning Opportunities
To invest in the ongoing growth and development of introductory course graduates, GSP-P developed and offered an advanced workshop in 2019. This multiday workshop focused on further enhancement of geropsychology competencies, with an emphasis on treating older veterans with mental and physical comorbidities. Didactics and experiential learning exercises led by SMEs covered topics such as adjusting to chronic illness, capacity assessment, PTSD, insomnia and sleep changes, chronic pain, and psychological interventions in palliative care and hospice settings. Evaluation findings demonstrated significant improvements from precourse to 6 months postcourse in confidence and knowledge as
To facilitate ongoing and individually tailored learning following the advanced workshop, scholars also developed and executed independent learning plans (ILPs) during a 6-month window with consultation from an experienced geropsychologist. Fifteen of 19 scholars (78.9%) completed ILPs with an average of 3 learning goals listed. After completing the ILPs, scholars endorsed their clinical and/or personal usefulness, citing increased confidence, enhanced skills for use with patients with complex needs, personal fulfillment, and career advancement. Most scholars noted ILPs were feasible and learning resources were accessible. Overall, the evaluation found ILPs to be a valuable way to enhance psychologists’ learning and effectiveness in treating older veterans with complex health needs.20
Clinical Practica
All geriatric scholars who completed the program have additional opportunities for professional development through practicum experiences focused on specific clinical approaches to the care of older veterans, such as dementia care, pain management, geriatric assessment, and palliative care. These practica provide scholars with individualized learning experiences in an individualized or small group setting and may be conducted either in-person or virtually.
In response to an expressed need from those who completed the program, the GSP-P planning committee collaborated with an SME to develop a virtual practicum to assess patients’ decision making capacity. Evaluating capacities among older adults is a common request, yet clinicians report little to no formal training in how to conceptualize and approach these complex questions.21,22 Utilizing an evidence-informed and structured approach promotes the balancing of an older adult’s autonomy and professional ethics. Learning capacity evaluation skills could better position psychologists to not only navigate complex ethical, legal, and clinical situations, but also serve as expert consultants to interdisciplinary teams. This virtual practicum was initiated in 2022 and to date has included 10 scholars. The practicum includes multiple modalities of learning: (1) self-directed review of core concepts; (2) attendance at 4 capacity didactics focused on introduction to evaluating capacities, medical consent and decision making, financial decision making and management, and independent living; and (3) participation in 5 group consultations on capacity evaluations conducted at their home sites. During these group consultations, additional case examples were shared to reinforce capacity concepts.
Discussion
The objective of GSP-P is to enhance geropsychology practice competencies among VHA psychologists given the outsized representation of older adults within the VHA system and their complex care needs. The curricula have significantly evolved to accomplish this, expanding the reach and investing in the continuing growth and development of scholars.
There are several elements that set GSP apart from other geriatric and geropsychology continuing medical education programs. The first is that the training is veteran focused, allowing us to discuss the unique impact military service has on aging. Similarly, because all scholars work within the integrated health care system, we can introduce and review key resources and programs that benefit all veterans and their families/care partners across the system. Through the GSP, the VA invests in ongoing professional development. Scholars can participate in additional experiential practica, webinars, and advanced workshops tailored to their individual learning needs. Lastly, the GSP works to create a community among its scholars where they can not only continue to consult with presenters/instructors, but also one another. A planned future direction for the GSP-P is to incorporate quarterly office hours and discussions for alumni to develop an increased sense of community. This may strengthen commitment to the overall VA mission, leading to increased retainment of talent who now have the knowledge, skills, and confidence to care for aging veterans.
Limitations
GSP is limited by its available funding. Additionally, the number of participants who can enroll each year in GSP-P (not including webinars) is capped by policy. Another limitation is the number of QI coaches available to mentor scholars on their projects.
Conclusions
Outcomes of GSP-P have been extremely favorable. Following participation in the program, we have found a significant increase in confidence in geropsychology practice among clinicians, as well as enhanced knowledge and skills across competency domains.15,19 We have observed rising attendance in our annual webinar series and graduates of our introductory courses participate in subsequent trainings (eg, advanced workshop or virtual practicum). Several graduates of GSP-P have become board certified in geropsychology by the American Board of Geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows. This suggests that the reach of GSP-P programming may extend farther than reported in this article.
The needs of aging veterans have also changed based on cohort differences, as the population of World War II and Korean War era veterans has declined and the number of older Vietnam era veterans has grown. We expect different challenges with older Gulf War and post-9/11 era veterans. For instance, 17% of troops deployed to Iraq or Afghanistan following 9/11 experienced mild traumatic brain injury (TBI), and 59% of those experienced > 1 mild TBI.23 Research indicates that younger post-9/11 veterans have a 3-fold risk of developing early onset dementia after experiencing a TBI.24 Therefore, even though post-9/11 veterans are not older in terms of chronological age, some may experience symptoms and conditions more often occurring in older veterans. As a result, it would be beneficial for clinicians to learn about the presentation and treatment of geriatric conditions such as dementia.
Moving forward, the GSP-P should identify potential opportunities to collaborate with the non-VHA mental health community–which also faces a shortage of geriatric mental health clinicians–to extend educational opportunities to improve care for veterans in all settings (eg, cosponsor training opportunities open to both VHA and non-VHA clinicians).8,25 Many aging veterans may receive portions of their health care outside the VHA, particularly those who reside in rural areas. Additionally, as veterans age, so do their support systems (eg, family members, friends, spouses, caregivers, and even clinicians), most of whom will receive care outside of the VHA. Community education collaborations will not only improve the care of older veterans, but also the care of older adults in the general population.
Promising directions include the adoption of the GSP model in other health care settings. Recently, Indian Health Service has adapted the model, beginning with primary care clinicians and pharmacists and is beginning to expand to other disciplines. Additional investments in VHA workforce training include the availability of geropsychology internship and fellowship training opportunities through the Office of Academic Affiliations, which provide earlier opportunities to specialize in geropsychology. Continued investment in both prelicensure and postpsychology licensure training efforts are needed within the VHA to meet the geriatric mental health needs of veterans.
Acknowledgments
The authors wish to acknowledge Terri Huh, PhD, for her contributions to the development and initiation of the GSP-P. The authors also appreciate the collaboration and quality initiative training led by Carol Callaway-Lane, DNP, ACNP-BC, and her team.
The Veterans Health Administration (VHA) is understaffed for clinical psychologists who have specialty training in geriatrics (ie, geropsychologists) to meet the needs of aging veterans. Though only 16.8% of US adults are aged ≥ 65 years,1 this age group comprises 45.9% of patients within the VHA.2 The needs of older adults are complex and warrant specialized services from mental health clinicians trained to understand lifespan developmental processes, biological changes associated with aging, and changes in psychosocial functioning.
Older veterans (aged ≥ 65 years) present with higher rates of combined medical and mental health diagnoses compared to both younger veterans and older adults who are not veterans.3 Nearly 1 of 5 (18.1%) older veterans who use VHA services have confirmed mental health diagnoses, and an additional 25.5% have documented mental health concerns without a formal diagnosis in their health record.4 The clinical presentations of older veterans frequently differ from younger adults and include greater complexity. For example, older veterans face an increased risk of cognitive impairment compared to the general population, due in part to higher prevalence of posttraumatic stress, which doubles their risk of developing dementia.5 Additional examples of multicomplexity among older veterans may include co-occurring medical and psychiatric diagnoses, the presence of delirium, social isolation/loneliness, and concerns related to polypharmacy. These complex presentations result in significant challenges for mental health clinicians in areas like assessment (eg, accuracy of case conceptualization), intervention (eg, selection and prioritization), and consultation (eg, coordination among multiple medical and mental health specialists).
Older veterans also present with substantial resilience. Research has found that aging veterans exposed to trauma during their military service often review their memories and past experiences, which is known as later-adulthood trauma reengagement.6 Through this normative life review process, veterans engage with memories and experiences from their past that they previously avoided, which could lead to posttraumatic growth for some. Unfortunately, others may experience an increase in psychological distress. Mental health clinicians with specialty expertise and training in aging and lifespan development can facilitate positive outcomes to reduce distress.7
The United States in general, and the VHA specifically, face a growing shortage of geriatric mental health clinicians.
The Geriatric Scholars Program (GSP) was developed in 2008 to address the training gap and provide education in geriatrics to VHA clinicians that treat older veterans, particularly in rural areas.11,12 The GSP initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists. It was later expanded to include other disciplines (ie, social work, rehabilitation therapists, and psychiatrists). In 2013, the GSP – Psychology Track (GSP-P) was developed with funding from the VHA Offices of Rural Health and Geriatrics and Extended Care specifically for psychologists.
This article describes the multicomponent longitudinal GSP-P, which has evolved to meet the target audience’s ongoing needs for knowledge, skills, and opportunities to refine practice behaviors. GSP-P received the 2020 Award for Excellence in Geropsychology Training from the Council of Professional Geropsychology Training Programs. GSP-P has grown within the context of the larger GSP and aligns with the other existing elective learning opportunities (Figure 1).
Program description
Introductory Course
Psychologist subject matter experts (SMEs) developed an intensive course in geropsychology in the absence of a similar course in the geriatric medicine board review curriculum. SMEs reviewed the guidelines for practice by professional organizations like the Pikes Peak Geropsychology Competencies,which outline knowledge and skills in various domains.13 SMEs integrated this review with findings from a needs assessment for postlicensed VHA psychology staff in 4 health care systems, drafted a syllabus, and circulated it to geropsychology experts for feedback. The resulting multiday course covered general mental health as well as topics particularly salient for mental health clinicians treating older veterans including suicide prevention and posttraumatic stress disorder (PTSD).14 This Geropsychology Competencies Review Course was piloted in 1 region initially before being offered nationally in 2014.
Quality Improvement
Introductory course attendees also participate in an intensive day-long interactive workshop in quality improvement (QI). After completing these trainings, they apply what they have learned at their home facility by embarking on a QI project related to geriatrics. The QI projects reinforce learning and initiate practice changes not only for attendees but at times the larger health care system. Topics are selected by scholars in response to the needs they observe in their clinics. Recent GSP projects include efforts to increase screenings for depression and anxiety, improve adherence to VHA dementia policy, increase access to virtual care, and increase referrals to programs such as whole health or cognitive behavioral therapy for insomnia, a first-line treatment for insomnia in older adults.17 Another project targeted the improvement of referrals to the Compassionate Contact Corps in an effort to reduce social isolation and loneliness among older veterans.18 Evaluations demonstrate significant improvement in scholars’ confidence in related program development and management from precourse to 3 months postcourse.15
Webinars
The Addressing Geriatric Mental Health webinar series was created to introduce learners to topics that could not be covered in the introductory course. Topics were suggested by the expert reviewers of the curriculum or identified by the scholars themselves (eg, chronic pain, sexuality, or serious mental illness). A secondary function of the webinars was to reach a broader audience. Over time, scholars and webinar attendees requested opportunities to explore topics in greater depth (eg, PTSD later in life). These requests led the webinars to focus on annual themes.
The series is open to all disciplines of geriatric scholars, VHA staff, and non-VHA staff through the Veterans Affairs Talent Management System and the TRAIN Learning Network (train.org). Attendance for the 37 webinars was captured from logins to the virtual learning platform and may underestimate attendance if a group attended on a single screen. Average attendance increased from 157 attendees/webinar in 2015 to 418 attendees/webinar in 2023 (Figure 2). This may have been related to the increase in virtual learning during the COVID-19 pandemic, but represents a 166% increase in audience from the inaugural year of the series.
Advanced Learning Opportunities
To invest in the ongoing growth and development of introductory course graduates, GSP-P developed and offered an advanced workshop in 2019. This multiday workshop focused on further enhancement of geropsychology competencies, with an emphasis on treating older veterans with mental and physical comorbidities. Didactics and experiential learning exercises led by SMEs covered topics such as adjusting to chronic illness, capacity assessment, PTSD, insomnia and sleep changes, chronic pain, and psychological interventions in palliative care and hospice settings. Evaluation findings demonstrated significant improvements from precourse to 6 months postcourse in confidence and knowledge as
To facilitate ongoing and individually tailored learning following the advanced workshop, scholars also developed and executed independent learning plans (ILPs) during a 6-month window with consultation from an experienced geropsychologist. Fifteen of 19 scholars (78.9%) completed ILPs with an average of 3 learning goals listed. After completing the ILPs, scholars endorsed their clinical and/or personal usefulness, citing increased confidence, enhanced skills for use with patients with complex needs, personal fulfillment, and career advancement. Most scholars noted ILPs were feasible and learning resources were accessible. Overall, the evaluation found ILPs to be a valuable way to enhance psychologists’ learning and effectiveness in treating older veterans with complex health needs.20
Clinical Practica
All geriatric scholars who completed the program have additional opportunities for professional development through practicum experiences focused on specific clinical approaches to the care of older veterans, such as dementia care, pain management, geriatric assessment, and palliative care. These practica provide scholars with individualized learning experiences in an individualized or small group setting and may be conducted either in-person or virtually.
In response to an expressed need from those who completed the program, the GSP-P planning committee collaborated with an SME to develop a virtual practicum to assess patients’ decision making capacity. Evaluating capacities among older adults is a common request, yet clinicians report little to no formal training in how to conceptualize and approach these complex questions.21,22 Utilizing an evidence-informed and structured approach promotes the balancing of an older adult’s autonomy and professional ethics. Learning capacity evaluation skills could better position psychologists to not only navigate complex ethical, legal, and clinical situations, but also serve as expert consultants to interdisciplinary teams. This virtual practicum was initiated in 2022 and to date has included 10 scholars. The practicum includes multiple modalities of learning: (1) self-directed review of core concepts; (2) attendance at 4 capacity didactics focused on introduction to evaluating capacities, medical consent and decision making, financial decision making and management, and independent living; and (3) participation in 5 group consultations on capacity evaluations conducted at their home sites. During these group consultations, additional case examples were shared to reinforce capacity concepts.
Discussion
The objective of GSP-P is to enhance geropsychology practice competencies among VHA psychologists given the outsized representation of older adults within the VHA system and their complex care needs. The curricula have significantly evolved to accomplish this, expanding the reach and investing in the continuing growth and development of scholars.
There are several elements that set GSP apart from other geriatric and geropsychology continuing medical education programs. The first is that the training is veteran focused, allowing us to discuss the unique impact military service has on aging. Similarly, because all scholars work within the integrated health care system, we can introduce and review key resources and programs that benefit all veterans and their families/care partners across the system. Through the GSP, the VA invests in ongoing professional development. Scholars can participate in additional experiential practica, webinars, and advanced workshops tailored to their individual learning needs. Lastly, the GSP works to create a community among its scholars where they can not only continue to consult with presenters/instructors, but also one another. A planned future direction for the GSP-P is to incorporate quarterly office hours and discussions for alumni to develop an increased sense of community. This may strengthen commitment to the overall VA mission, leading to increased retainment of talent who now have the knowledge, skills, and confidence to care for aging veterans.
Limitations
GSP is limited by its available funding. Additionally, the number of participants who can enroll each year in GSP-P (not including webinars) is capped by policy. Another limitation is the number of QI coaches available to mentor scholars on their projects.
Conclusions
Outcomes of GSP-P have been extremely favorable. Following participation in the program, we have found a significant increase in confidence in geropsychology practice among clinicians, as well as enhanced knowledge and skills across competency domains.15,19 We have observed rising attendance in our annual webinar series and graduates of our introductory courses participate in subsequent trainings (eg, advanced workshop or virtual practicum). Several graduates of GSP-P have become board certified in geropsychology by the American Board of Geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows. This suggests that the reach of GSP-P programming may extend farther than reported in this article.
The needs of aging veterans have also changed based on cohort differences, as the population of World War II and Korean War era veterans has declined and the number of older Vietnam era veterans has grown. We expect different challenges with older Gulf War and post-9/11 era veterans. For instance, 17% of troops deployed to Iraq or Afghanistan following 9/11 experienced mild traumatic brain injury (TBI), and 59% of those experienced > 1 mild TBI.23 Research indicates that younger post-9/11 veterans have a 3-fold risk of developing early onset dementia after experiencing a TBI.24 Therefore, even though post-9/11 veterans are not older in terms of chronological age, some may experience symptoms and conditions more often occurring in older veterans. As a result, it would be beneficial for clinicians to learn about the presentation and treatment of geriatric conditions such as dementia.
Moving forward, the GSP-P should identify potential opportunities to collaborate with the non-VHA mental health community–which also faces a shortage of geriatric mental health clinicians–to extend educational opportunities to improve care for veterans in all settings (eg, cosponsor training opportunities open to both VHA and non-VHA clinicians).8,25 Many aging veterans may receive portions of their health care outside the VHA, particularly those who reside in rural areas. Additionally, as veterans age, so do their support systems (eg, family members, friends, spouses, caregivers, and even clinicians), most of whom will receive care outside of the VHA. Community education collaborations will not only improve the care of older veterans, but also the care of older adults in the general population.
Promising directions include the adoption of the GSP model in other health care settings. Recently, Indian Health Service has adapted the model, beginning with primary care clinicians and pharmacists and is beginning to expand to other disciplines. Additional investments in VHA workforce training include the availability of geropsychology internship and fellowship training opportunities through the Office of Academic Affiliations, which provide earlier opportunities to specialize in geropsychology. Continued investment in both prelicensure and postpsychology licensure training efforts are needed within the VHA to meet the geriatric mental health needs of veterans.
Acknowledgments
The authors wish to acknowledge Terri Huh, PhD, for her contributions to the development and initiation of the GSP-P. The authors also appreciate the collaboration and quality initiative training led by Carol Callaway-Lane, DNP, ACNP-BC, and her team.
1. Caplan Z, Rabe M; US Department of Commerce, US Census Bureau. The Older Population: 2020 (Census Brief No. C2020BR-07). May 2023. Accessed February 27, 2024. https://www2.census.gov/library/publications/decennial/2020/census-briefs/c2020br-07.pdf
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. VA benefits & health care utilization. Updated February 2023. Accessed February 27, 2024. https://www.va.gov/vetdata/docs/pocketcards/fy2023q2.PDF
3. O’Malley KA, Vinson L, Pless Kaiser A, Sager Z, Hinrichs K. Mental health and aging veterans: How the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
4. Greenberg G, Hoff R. FY 2021 Older Adult (65+ on October 1st) Veteran Data Sheet: National, VISN, and Healthcare System Tables. West Haven, CT: U.S. Department of Veterans Affairs, Northeast Program Evaluation Center. 2022.
5. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613. doi:10.1001/archgenpsychiatry.2010.61
6. Davison EH, Kaiser AP, Spiro A 3rd, Moye J, King LA, King DW. From late-onset stress symptomatology to later-adulthood trauma reengagement in aging combat veterans: Taking a broader view. Gerontologist. 2016;56(1):14-21. doi:10.1093/geront/gnv097
7. Kaiser AP, Boyle JT, Bamonti PM, O’Malley K, Moye J. Development, adaptation, and clinical implementation of the Later-Adulthood Trauma Reengagement (LATR) group intervention for older veterans. Psychol Serv. 2023;20(4):863-875. doi:10.1037/ser0000736
8. Moye J, Karel MJ, Stamm KE, et al. Workforce analysis of psychological practice with older adults: Growing crisis requires urgent action. Train Educ Prof Psychol. 2019;13(1):46-55. doi:10.1037/tep0000206
9. Stamm K, Lin L, Conroy J. Critical needs in geropsychology. Monitor on Psychology. 2021;52(4):21.
10. American Board of Geropsychology. Specialists. 2024. Accessed February 6, 2024. https://abgero.org/board-members/specialists/
11. Kramer BJ. The VA Geriatric Scholars Program. Fed Pract. 2015;32(5):46-48.
12. Kramer BJ, Creekmur B, Howe JL, et al. Veterans Affairs Geriatric Scholars Program: Enhancing existing primary care clinician skills in caring for older veterans. J Am Geriatr Soc. 2016;64(11):2343-2348. doi:10.1111/jgs.14382
13. Knight BG, Karel MJ, Hinrichsen GA, Qualls SH, Duffy M. Pikes Peak model for training in professional geropsychology. Am Psychol. 2009;64(3):205-14. doi:10.1037/a0015059
14. Huh JWT, Rodriguez R, Gould CE, R Brunskill S, Melendez L, Kramer BJ. Developing a program to increase geropsychology competencies of Veterans Health Administration (VHA) psychologists. Gerontol Geriatr Educ. 2020;41(4):463-479. doi:10.1080/02701960.2018.1491402
15. Huh JWT, Rodriguez RL, Gregg JJ, Scales AN, Kramer BJ, Gould CE. Improving geropsychology competencies of Veterans Affairs psychologists. J Am Geriatr Soc. 2021;69(3):798-805. doi:10.1111/jgs.17029
16. Karel MJ, Emery EE, Molinari V; CoPGTP Task Force on the Assessment of Geropsychology Competencies. Development of a tool to evaluate geropsychology knowledge and skill competencies. Int Psychogeriatr. 2010;22(6):886-896. doi:10.1017/S1041610209991736
17. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
18. Sullivan J, Gualtieri L, Campbell M, Davila H, Pendergast J, Taylor P. VA Compassionate Contact Corps: a phone-based intervention for veterans interested in speaking with peers. Innov Aging. 2021;5(Suppl 1):204. doi:10.1093/geroni/igab046.788
19. Gregg JJ, Rodriguez RL, Mehta PS, Kramer BJ, Gould CE. Enhancing specialty training in geropsychology competencies: an evaluation of a VA Geriatric Scholars Program advanced topics workshop. Gerontol Geriatr Educ. 2023;44(3):329-338. doi:10.1080/02701960.2022.2069764
20. Gould CE, Rodriguez RL, Gregg J, Mehta PS, Kramer J. Mentored independent learning plans among psychologists: a mixed methods investigation. J Amer Geriatr Soc. 2023;71(S1):S53.
21. Mullaly E, Kinsella G, Berberovic N, et al. Assessment of decision-making capacity: exploration of common practices among neuropsychologists. Aust Psychol. 2007;42:178-186. doi:10.1080/00050060601187142
22. Seyfried L, Ryan KA, Kim SYH. Assessment of decision-making capacity: Views and experiences of consultation psychiatrists. Psychosomatics. 2013;54(2):115-123. doi:10.1016/j.psym.2012.08.001
23. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257. doi:10.1097/PSY.0b013e318244c604
24. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627.doi:10.1080/02699052.2022.2033846
25. Merz CC, Koh D, Sakai EY, et al. The big shortage: Geropsychologists discuss facilitators and barriers to working in the field of aging. Transl Issues Psychol Sci. 2017;3(4):388-399. doi:10.1037/tps0000137
1. Caplan Z, Rabe M; US Department of Commerce, US Census Bureau. The Older Population: 2020 (Census Brief No. C2020BR-07). May 2023. Accessed February 27, 2024. https://www2.census.gov/library/publications/decennial/2020/census-briefs/c2020br-07.pdf
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. VA benefits & health care utilization. Updated February 2023. Accessed February 27, 2024. https://www.va.gov/vetdata/docs/pocketcards/fy2023q2.PDF
3. O’Malley KA, Vinson L, Pless Kaiser A, Sager Z, Hinrichs K. Mental health and aging veterans: How the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
4. Greenberg G, Hoff R. FY 2021 Older Adult (65+ on October 1st) Veteran Data Sheet: National, VISN, and Healthcare System Tables. West Haven, CT: U.S. Department of Veterans Affairs, Northeast Program Evaluation Center. 2022.
5. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613. doi:10.1001/archgenpsychiatry.2010.61
6. Davison EH, Kaiser AP, Spiro A 3rd, Moye J, King LA, King DW. From late-onset stress symptomatology to later-adulthood trauma reengagement in aging combat veterans: Taking a broader view. Gerontologist. 2016;56(1):14-21. doi:10.1093/geront/gnv097
7. Kaiser AP, Boyle JT, Bamonti PM, O’Malley K, Moye J. Development, adaptation, and clinical implementation of the Later-Adulthood Trauma Reengagement (LATR) group intervention for older veterans. Psychol Serv. 2023;20(4):863-875. doi:10.1037/ser0000736
8. Moye J, Karel MJ, Stamm KE, et al. Workforce analysis of psychological practice with older adults: Growing crisis requires urgent action. Train Educ Prof Psychol. 2019;13(1):46-55. doi:10.1037/tep0000206
9. Stamm K, Lin L, Conroy J. Critical needs in geropsychology. Monitor on Psychology. 2021;52(4):21.
10. American Board of Geropsychology. Specialists. 2024. Accessed February 6, 2024. https://abgero.org/board-members/specialists/
11. Kramer BJ. The VA Geriatric Scholars Program. Fed Pract. 2015;32(5):46-48.
12. Kramer BJ, Creekmur B, Howe JL, et al. Veterans Affairs Geriatric Scholars Program: Enhancing existing primary care clinician skills in caring for older veterans. J Am Geriatr Soc. 2016;64(11):2343-2348. doi:10.1111/jgs.14382
13. Knight BG, Karel MJ, Hinrichsen GA, Qualls SH, Duffy M. Pikes Peak model for training in professional geropsychology. Am Psychol. 2009;64(3):205-14. doi:10.1037/a0015059
14. Huh JWT, Rodriguez R, Gould CE, R Brunskill S, Melendez L, Kramer BJ. Developing a program to increase geropsychology competencies of Veterans Health Administration (VHA) psychologists. Gerontol Geriatr Educ. 2020;41(4):463-479. doi:10.1080/02701960.2018.1491402
15. Huh JWT, Rodriguez RL, Gregg JJ, Scales AN, Kramer BJ, Gould CE. Improving geropsychology competencies of Veterans Affairs psychologists. J Am Geriatr Soc. 2021;69(3):798-805. doi:10.1111/jgs.17029
16. Karel MJ, Emery EE, Molinari V; CoPGTP Task Force on the Assessment of Geropsychology Competencies. Development of a tool to evaluate geropsychology knowledge and skill competencies. Int Psychogeriatr. 2010;22(6):886-896. doi:10.1017/S1041610209991736
17. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
18. Sullivan J, Gualtieri L, Campbell M, Davila H, Pendergast J, Taylor P. VA Compassionate Contact Corps: a phone-based intervention for veterans interested in speaking with peers. Innov Aging. 2021;5(Suppl 1):204. doi:10.1093/geroni/igab046.788
19. Gregg JJ, Rodriguez RL, Mehta PS, Kramer BJ, Gould CE. Enhancing specialty training in geropsychology competencies: an evaluation of a VA Geriatric Scholars Program advanced topics workshop. Gerontol Geriatr Educ. 2023;44(3):329-338. doi:10.1080/02701960.2022.2069764
20. Gould CE, Rodriguez RL, Gregg J, Mehta PS, Kramer J. Mentored independent learning plans among psychologists: a mixed methods investigation. J Amer Geriatr Soc. 2023;71(S1):S53.
21. Mullaly E, Kinsella G, Berberovic N, et al. Assessment of decision-making capacity: exploration of common practices among neuropsychologists. Aust Psychol. 2007;42:178-186. doi:10.1080/00050060601187142
22. Seyfried L, Ryan KA, Kim SYH. Assessment of decision-making capacity: Views and experiences of consultation psychiatrists. Psychosomatics. 2013;54(2):115-123. doi:10.1016/j.psym.2012.08.001
23. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257. doi:10.1097/PSY.0b013e318244c604
24. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627.doi:10.1080/02699052.2022.2033846
25. Merz CC, Koh D, Sakai EY, et al. The big shortage: Geropsychologists discuss facilitators and barriers to working in the field of aging. Transl Issues Psychol Sci. 2017;3(4):388-399. doi:10.1037/tps0000137
The VA Geriatric Scholars Program
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.