User login
Biomarkers: Their potential in the diagnosis and treatment of heart failure
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
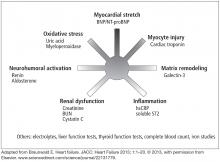
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
KEY POINTS
- The usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.
- For risk stratification in heart failure (HF), biomarkers that reflect renal insufficiency are especially powerful prognosticators.
- In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF.
- In general, point-of-care assays are often more variable than the same tests done in clinical laboratories; sample collection, handling, and processing also introduce variability.