User login
Can scribes boost FPs’ efficiency and job satisfaction?
ABSTRACT
Purpose Research in other medical specialties has shown that the addition of medical scribes to the clinical team enhances physicians’ practice experience and increases productivity. To date, literature on the implementation of scribes in primary care is limited. To determine the feasibility and benefits of implementing scribes in family medicine, we undertook a pilot mixed-method quality improvement (QI) study.
Methods In 2014, we incorporated 4 part-time scribes into an academic family medicine practice consisting of 7 physicians. We then measured, via survey and time-tracking data, the impact the scribes had on physician office hours and productivity, time spent on documentation, perceptions of work-life balance, and physician and patient satisfaction.
Results Six of the 7 faculty physicians participated. This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family physicians spent on charting, improved work-life balance, and had good patient acceptance. Specifically, the physicians spent an average of 5.1 fewer hours/week (hrs/wk) on documentation, while various measures of productivity revealed increases ranging from 9.2% to 28.8%. Perhaps most important of all, when the results of the pilot study were annualized, they were projected to generate $168,600 per year—more than twice the $79,500 annual cost of 2 full-time equivalent scribes.
Surveys assessing work-life balance demonstrated improvement in the physicians’ perception of the administrative burden/paperwork related to practice and a decrease in their perception of the extent to which work encroached on their personal lives. In addition, survey data from 313 patients at the time of their ambulatory visit with a scribe present revealed a high level of comfort. Likewise, surveys completed by physicians after 55 clinical sessions (ie, blocks of consecutive, uninterrupted patient appointments; there are usually 2 sessions per day) revealed good to excellent ratings more than 90% of the time.
Conclusion In an outpatient family medicine clinic, the use of scribes substantially improved physicians’ efficiency, job satisfaction, and productivity without negatively impacting the patient experience.
While electronic medical records (EMRs) are important tools for improving patient care and communication, they bring with them an additional administrative burden for health care providers. In the emergency medicine literature, scribes have been reported to reduce that burden and improve clinicians’ productivity and satisfaction.1-4 Additionally, studies have reported increases in patient volume, generated billings, and provider morale, as well as decreases in emergency department (ED) lengths of stay.5 A recent review of the emergency medicine literature concluded that scribes have “the ability to allay the burden of documentation, improve throughput in the ED, and potentially enhance doctors’ satisfaction.”6
Similar benefits following scribe implementation have been reported in the literature of other specialties. A maternal-fetal medicine practice reported significant increases in generated billings and reimbursement.7 Increases in physician productivity and improvements in physician-patient interactions were reported in a cardiology clinic,8 and a urology practice reported high satisfaction and acceptance rates among both patients and physicians.9
Practice management literature and an article in The New York Times have anecdotally described the benefits of scribes in clinical practice10-12 with the latter noting that, “Physicians who use [scribes] say they feel liberated from the constant note-taking ...” and that “scribes have helped restore joy in the practice of medicine.”10
A small retrospective review that appeared in The Journal of Family Practice last year looked at the quality of scribes’ notes and found that they were rated slightly higher than physicians’ notes—at least for diabetes visits. However, it did not address the issues of physician productivity or satisfaction. (See "Medical scribes: How do their notes stack up?" 2016;65:155-159.)
The only family medicine study that we did find that addressed these 2 issues was one done in Oregon. The study noted that scribes enabled physicians to see 24 patients per day—up from 18, with accompanying improvements in physician “quality of life.”13 Absent from the literature are quantitative data on the feasibility and benefits of implementing scribes in family medicine.
Could a study at our facility offer some insights? In light of the paucity of published data on scribes in family medicine, and the fact that a survey conducted at our health center revealed that our faculty physicians felt overburdened by the administrative demands of clinical practice,14 we decided to study whether scribes might improve the work climate for clinicians at our family medicine residency training site. Our goal was to assess the impact of scribes on physician and patient satisfaction and on hours physicians spent on administrative tasks generated by clinical care.
METHODS
The study took place at the Barre Family Health Center (BFHC), a rural, freestanding family health center/residency site owned and operated by UMassMemorial Health Care (UMMHC), the major teaching/clinical affiliate of the University of Massachusetts Medical School. The health care providers of BFHC conduct 40,000 patient visits annually. Without scribes, the physicians typically dictated their notes at the end of the day, and they became available for review/sign off usually within 24 hours.
Six of the 7 faculty physicians working at BFHC in 2014 (including the lead author) participated in the pilot study (the seventh declined to participate). Three male and 3 female physicians between the ages of 34 and 65 years participated; they had been in practice between 5 and 40 years. All of the physicians had used an EMR for 5 years or more, and all but 2 had previously used a paper record. Residents and advanced practitioners did not participate because limited funding allowed for the hiring of only 2 full-time equivalent (FTE; 4 part-time) scribes.
Contracting for services. We contracted with an outside vendor for scribe services. Prior to their arrival at our health care center, the scribes received online training on medical vocabulary, note structure, billing and coding, and patient confidentiality (HIPAA). Once they arrived, on-site training detailed workflow, precharting, use of templates, the EMR and chart organization, and billing. In addition to typing notes into the EMR during patient visits, the scribes helped develop processes for scheduling, alerting patients to the scribe’s role, and defining when scribes should and should not be present in the exam room. The chief scribe created a monthly schedule, which enabled staff to determine which physician schedules should have extra appointment slots added. This was imperative because our parent institution mandated that new initiatives yield a 25% return on investment (ROI).
Using standard scripting and consent methods, nursing staff informed patients during rooming that the provider was working with a scribe, explained the scribe’s role, and asked about any objections to the scribe’s presence. Patients could decline scribe involvement, and all scribes were routinely excused during genital and rectal examinations.
Data collection
Data were collected during the 6-month trial period from May through October of 2014. The number of hours physicians spent at BFHC and at home working on clinical documentation was collected using a smartphone time-tracking application for two 3-week periods: the first period was in April 2014, before the scribes came on board; the second period was at the end of the 6-month scribe implementation period. In order to assess effects on productivity and whether the project was meeting the required ROI for continuation, we included a retrospective review of the EMR for both of the 3-week periods to document total clinical hours, number of clinic sessions (blocks of consecutive, uninterrupted appointments), average hours per session, the number of patient appointments scheduled per session, and the number of patient visits actually conducted per session (accounting for no-shows and unused appointments).
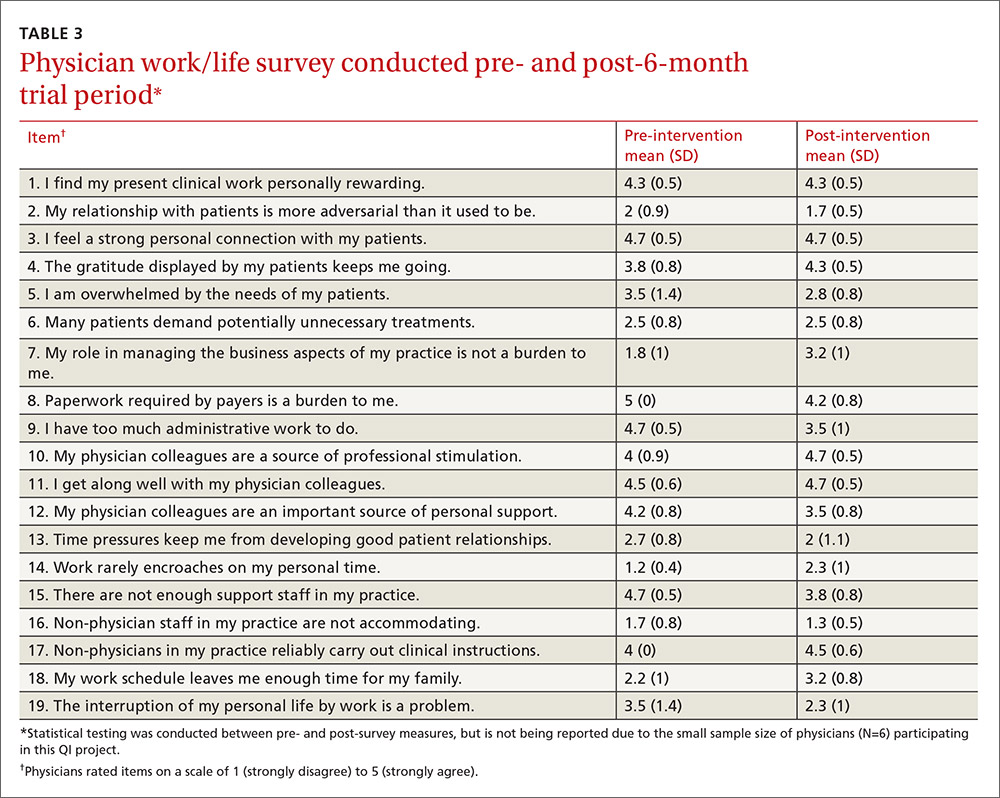
Physician work-life balance. We utilized 19 questions most relevant to this project’s focus from the 36-item Physician Work-Life Survey.15 Items were scored on a 5-point Likert scale ranging from ‘strongly disagree’ (1) to ‘strongly agree’ (5). The BFHC ambulatory manager distributed surveys to physicians immediately prior to the trial with scribes and 2 weeks after the conclusion of the 6-month trial.
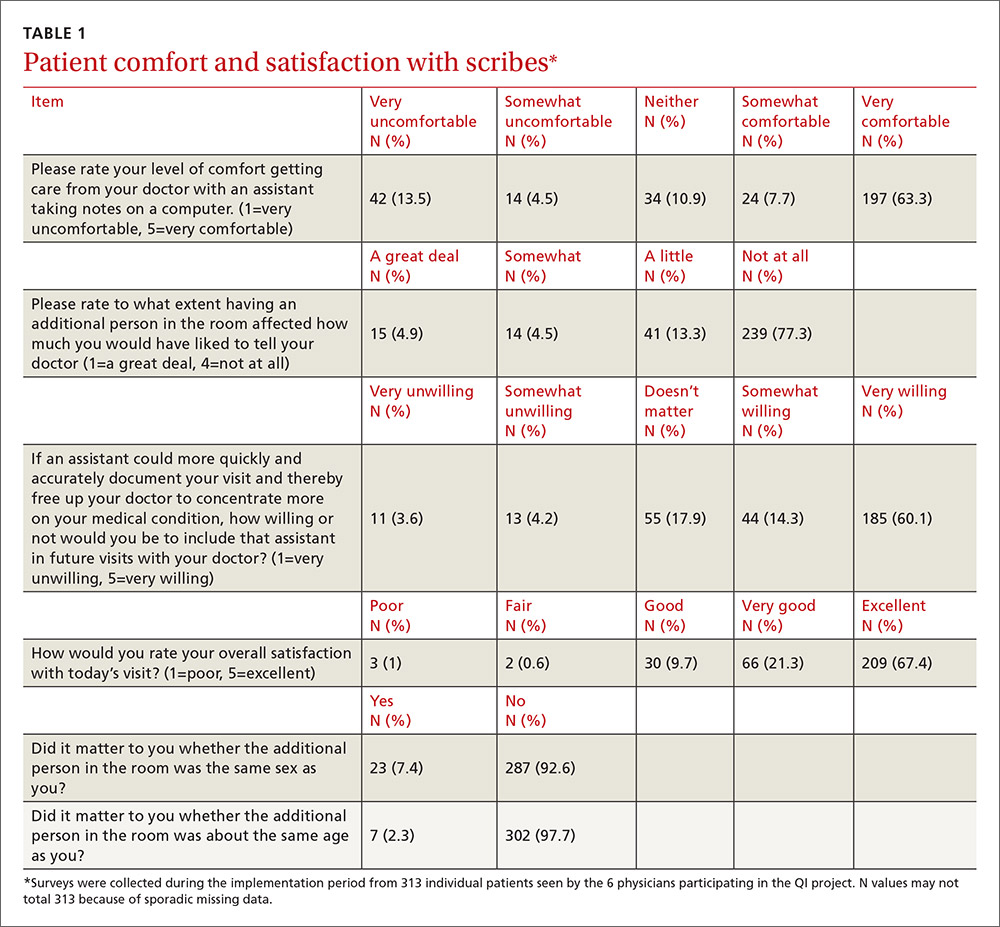
Patient and provider satisfaction. During the 6-month intervention period, satisfaction surveys9 were distributed to patients by scribes at the end of the office visit and to physicians at the end of each scribed session, after notes were completed and reviewed. Patient surveys consisted of 6 closed-end questions regarding comfort level with the scribe in the exam room, willingness to have a scribe present for subsequent visits, importance of the scribe being the same gender/age as the patient, and overall satisfaction with the scribe’s presence (TABLE 1).
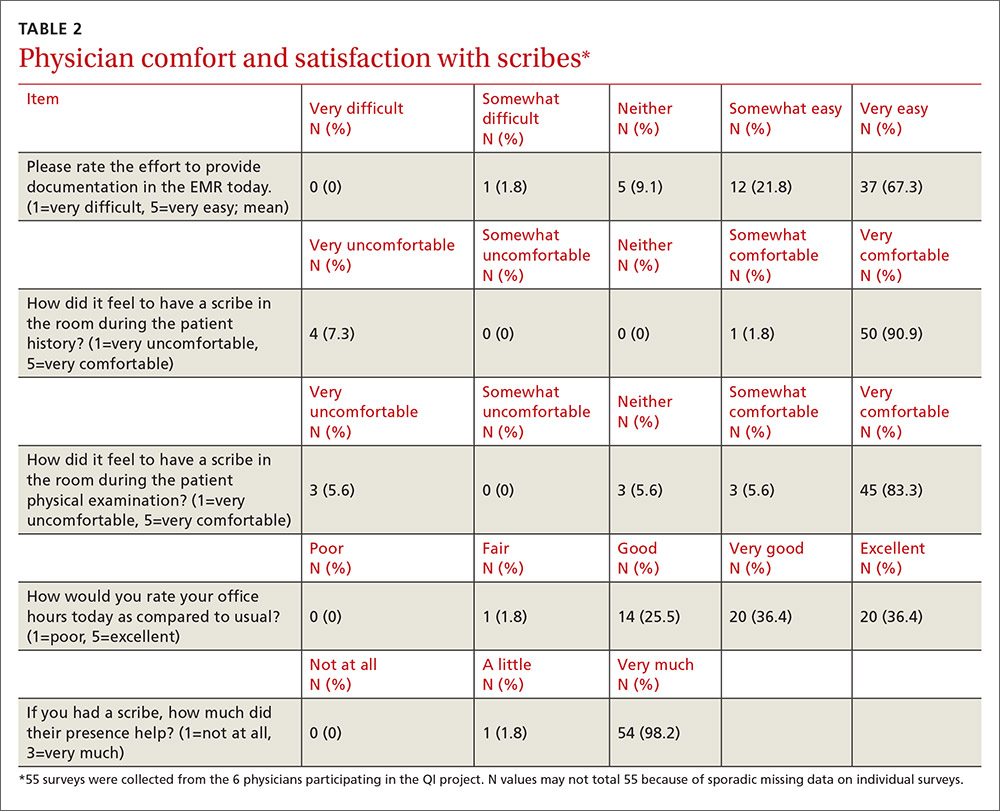
Physician surveys included 5 closed-end questions9 regarding comfort level with the scribe’s presence, ease of EMR documentation, change in office hours with having a scribe for that day’s session(s), and overall helpfulness of the scribe (TABLE 2). Open-ended questions on both surveys asked for additional comments or concerns regarding scribes and the scribe’s impact on patient encounters.
Our goal was to collect a minimum of 100 completed patient surveys and 50 completed physician surveys representing as many different patient demographics, visit types, days of the week, and times of day as possible. Surveys were anonymous and distributed during the second and third months of the trial, giving the scribes a one-month training and adjustment period.
Impact assessment, professional development needs. At the end of the 6-month study period, we held 2 focus groups—one with nurses and one with scribes. From the nurses, we solicited insights regarding the impact of scribes on patient volume, patient satisfaction, visit flow, and EMR documentation.
Scribes were asked about job skills needed, amount of training received, comfort in the exam room (both for themselves and patients), frequency of feedback received, balancing physician style with EMR documentation needs, and lessons learned.
Data analysis
Data were analyzed using the software SPSS V22.0. Univariate statistics were used to analyze patient and physician satisfaction, as well as clinic volume, time tracking, and EMR documentation. Initially, bivariate statistics were used to examine pre- and post-trial physician and patient data, but then non-parametric comparisons were used because of small sample sizes (and the resulting data being distributed abnormally). Detailed focus group notes were reviewed by all study investigators and summarized for dominant themes to support the quantitative evaluation. Lastly, the study was evaluated by the University of Massachusetts Institutional Review Board and was waived from review/oversight because of its QI intent.
RESULTS
Physician findings. Fifty-five physician surveys were completed during the 6-month period (TABLE 2). All of the physicians who were asked to complete this short survey at the end of the day (after reviewing notes with their scribe) did so. Physicians reported a high degree of satisfaction with collaboration with scribes. Their comments reflected positive experiences, including an improved ability to remain on schedule, having assistance finding important information in the record, and having notes completed at the end of the session.
TABLE 3 shows high satisfaction with clinical roles and colleagues with no substantive changes over time regarding these questions. However, the incorporation of scribes had a positive impact on issues related to physician morale, due to changes in paperwork, administrative duties, and work schedules.
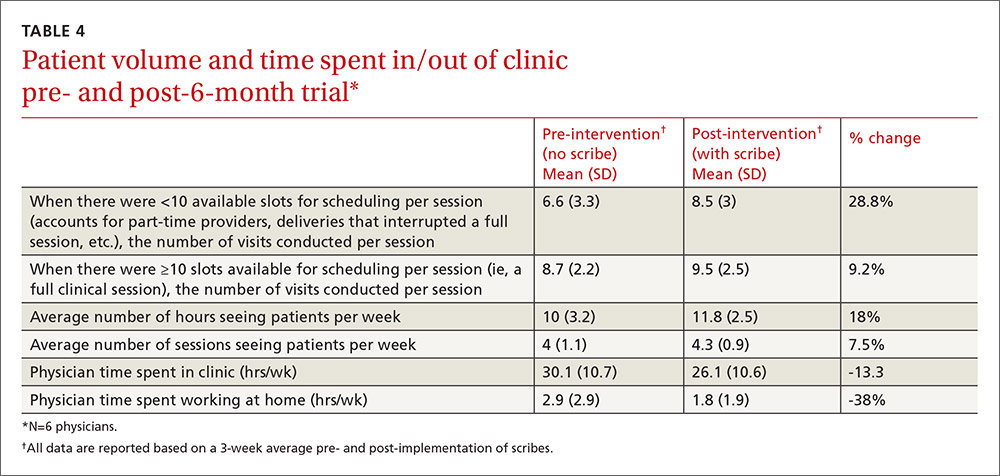
Review of patient scheduling and documentation (TABLE 4) revealed visits per clinical session increased 28.8% from 6.6 to 8.5, and for sessions with 10 or more appointment slots available, billable visits increased 9.2% from 8.7 to 9.5. This increase was a result of adding an additional appointment slot to the schedule when a scribe was assigned and a greater physician willingness to overbook when scribe assistance was available.
A comparison of time tracking pre- and post-intervention showed a 13% decrease in time spent in the clinic, from a 3-week average of 30.1 hrs/wk to 26.1 hrs/wk (TABLE 4). Time spent working at home decreased 38%, from a 3-week average of 2.9 hrs/wk to 1.8 hrs/wk. These reductions occurred despite average scheduled clinic hours being 18% higher (35.5 vs 30.1) during the post- vs pre-intervention measurement periods.
Patient findings. TABLE 1 summarizes the 313 patient responses. Less than 10% of patients declined to have a scribe during the visit. Patients reported a high level of comfort with the scribe and indicated that having a scribe in the room had little impact on what they would have liked to tell their doctor. Nearly all open-ended comments were positive and reflected feelings that the scribe’s presence enabled their provider to focus more on them and less on the computer.
Focus group findings
The scribe focus group identified a number of skills thought to be necessary to be successful in the job, including typing quickly; having technology/computer-searching strategy skills; and being detail-oriented, organized, and able to multitask. Scribes estimated that it took 2 to 6 weeks to feel comfortable doing the job. Physician feedback was preferred at the end of every session.
Lastly, the 4 scribes identified several challenges that should be addressed in future training, such as how to: 1. document a visit when the patient has a complicated medical history and the communication between the doctor and the patient is implicit; 2. incorporate the particulars of a visit into a patient’s full medical history; and 3. sift through the volume of previous notes when a physician has been seeing a patient for a long period of time.
The nurses’ focus group identified many positive effects on patient care. They reported no significant challenges with introducing scribes to patients. Improvements in timely availability of documentation enhanced their ability to respond quickly and more completely to patient queries. The nurses noted that the use of scribes improved patient care and made them “a better practice.”
DISCUSSION
This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family practitioners spent on charting, improved work-life balance, and had good patient acceptance. Our time-tracking studies demonstrated that physicians spent 5.1 fewer hrs/wk working—4 fewer hrs/wk in the clinic, and 1.1 fewer hrs/wk outside of the clinic—while clinical hours and productivity per session increased. Patients reported high satisfaction with scribed visits and a willingness to have scribes in the future. Creating notes in real time and having immediate availability after the session was a plus for nursing staff in providing follow-up patient care.
Concerns by physicians that having another person in the room would alter the physician-patient relationship were not substantiated, perhaps because the staff routinely obtained consent and explained the scribe’s role. Consistent with previous work, we found no suggestion that a scribe’s presence affected patients’ willingness to discuss sensitive issues.9 Patients reacted positively to scribes who enabled physicians to focus more on the patient and less on charting.
Despite increased patient volume, physician morale improved. Physicians left work more than an hour earlier per day, on average, and spent over 1 hour less per week working on clinical documentation outside the office. Physician surveys showed an improvement in perceptions of how much work encroached on their personal life, consistent with the time-tracking data. These results have significant implications for clinician retention, productivity, and satisfaction.
Since our site is an academic training site, one might wonder how residents and advanced practitioners viewed this implementation, as they were not initially included. From the perspective of the administrators, this was a feasibility study. Clinicians who were not included understood that if this pilot was successful, the use of scribes would be expanded in the future. In fact, because of these positive results, our institution has expanded the scribe program, so that it now covers all clinical sessions for faculty in our center and is rolling out a similar program in 3 other departmental academic practices.
Financial implications. At the beginning of this initiative, our institution required that we cover the cost of the program plus generate a 25% ROI. Using a conservative 9.2% increase in billable visits, we extrapolated that utilizing 2 FTE scribes would result in an additional 860 visits annually. Per our hospital’s finance department, estimated revenue generated by our facility-based practice per visit is $196, including ancillaries. That means that additional visits would generate an estimated $168,600 annually—more than twice the $79,500 annual cost of 2 FTE scribes, yielding a 112% ROI. Furthermore, patient access improved by making more visits available. Beyond the positive direct ROI, the improvements in physician morale and work-life balance have positive implications for retention, likely substantially increasing the long-term, overall ROI.
Challenges. Implementing a new program in a large organization proved to be challenging. The biggest hurdle was convincing our institution’s administration and finance department that this new expense would pay for itself in both tangible (increased visits per session) and intangible (increased physician satisfaction and retention) ways. A cost-sharing arrangement proposed by our department’s administrator convinced hospital administration to move forward. Additional challenges included delays in getting the scribe program started because of vendor selection, purchasing new laptops for scribes, hiring and training scribes, developing new EMR templates, validating provider productivity, and legal/compliance approval of the scribe’s EMR documentation processes to meet third-party and accuracy/quality requirements—all taking longer than anticipated. However, we believe that our results indicate significant potential for other primary care practices.
Limitations. The number of physicians in the study was small, and they all worked in the same location. Social desirability could have biased patient and provider feedback, but our quantitative results were consistent with subjective assessments, suggesting that information bias potential was low. Patient and provider survey findings were also supported by qualitative assessments from both scribes and nursing staff. The size of the project did not lend itself to an analysis controlling for clustering by physician and/or scribe. The focus group discussions were not subject to rigorous qualitative analysis, potentially increasing the risk of biased interpretation. Lastly, we did not have the ability to directly compare sessions with and without scribes during the pilot.
Similarity to other findings. Despite these limitations, our findings are remarkably similar to those of Howard, et al,16 on the pilot implementation of scribes in a community health center, including good patient and clinician acceptance and increased productivity that more than offset the cost of the scribes. We expect that others implementing scribe services in primary care settings will experience similar results.
CORRESPONDENCE
Stephen T. Earls, MD, 151 Worcester Road, Barre, MA 01005; stephen.earls@umassmemorial.org.
ACKNOWLEDGEMENT
The authors gratefully acknowledge the assistance of Barbara Fisher, MBA, vice president for ambulatory services; Nicholas Comeau, BS; and Brenda Rivard, administrative lead, Barre Family Health Center, UMassMemorial Health Care, in the preparation and execution of this study.
1. Walker K, Ben-Meir M, O’Mullane P, et al. Scribes in an Australian private emergency department: a description of physician productivity. Emerg Med Australas. 2014;26:543-548.
2. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
3. Expanded scribe role boosts staff morale. ED Manag. 2009;21:75-77.
4. Scribes, EMR please docs, save $600,000. ED Manag. 2009;21:117-118.
5. Bastani A, Shaqiri B, Palomba K, et al. An ED scribe program is able to improve throughput time and patient satisfaction. Am J Emerg Med. 2014;32:399-402.
6. Cabilan CJ, Eley RM. Review article: potential of medical scribes to allay the burden of documentation and enhance efficiency in Australian emergency departments. Emerg Med Australas. 2015 Aug 13. [Epub ahead of print]
7. Hegstrom L, Leslie J, Hutchinson E, et al. Medical scribes: are scribe programs cost effective in an outpatient MFM setting? Am J Obstet Gynecol. 2013;208:S240.
8. Campbell LL, Case D, Crocker JE, et al. Using medical scribes in a physician practice. J AHIMA. 2012;83:64-69.
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262.
10. Hafner K. A busy doctor’s right hand, ever ready to type. The New York Times. January 12, 2014. Available at: https://www.nytimes.com/2014/01/14/health/a-busy-doctors-right-hand-ever-ready-to-type.html?_r=0. Accessed February 6, 2017.
11. Brady K, Shariff A. Virtual medical scribes: making electronic medical records work for you. J Med Pract Manage. 2013;29:133-136.
12. Baugh R, Jones JE, Troff K, et al. Medical scribes. J Med Pract Manage. 2012;28:195-197.
13. Grimshaw H. Physician scribes improve productivity. Oak Street Medical allows doctors to spend more face time with patients, improve job satisfaction. MGMA Connex. 2012;12:27-28.
14. Morehead Associates, Inc. UMassMemorial Health Care: Physician Satisfaction Survey. 2013.
15. Konrad TR, Williams ES, Linzer M, et al. Measuring physician job satisfaction in a changing workplace and challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37:1174-1182.
16. Howard KA, Helé K, Salibi N, et al. BTW Informing change. Blue Shield of California Foundation. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Available at: http://informingchange.com/cat-publications/adapting-the-ehr-scribe-model-to-community-health-centers-the-experience-of-shasta-community-health-centers-pilot. Accessed November 6, 2015.
ABSTRACT
Purpose Research in other medical specialties has shown that the addition of medical scribes to the clinical team enhances physicians’ practice experience and increases productivity. To date, literature on the implementation of scribes in primary care is limited. To determine the feasibility and benefits of implementing scribes in family medicine, we undertook a pilot mixed-method quality improvement (QI) study.
Methods In 2014, we incorporated 4 part-time scribes into an academic family medicine practice consisting of 7 physicians. We then measured, via survey and time-tracking data, the impact the scribes had on physician office hours and productivity, time spent on documentation, perceptions of work-life balance, and physician and patient satisfaction.
Results Six of the 7 faculty physicians participated. This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family physicians spent on charting, improved work-life balance, and had good patient acceptance. Specifically, the physicians spent an average of 5.1 fewer hours/week (hrs/wk) on documentation, while various measures of productivity revealed increases ranging from 9.2% to 28.8%. Perhaps most important of all, when the results of the pilot study were annualized, they were projected to generate $168,600 per year—more than twice the $79,500 annual cost of 2 full-time equivalent scribes.
Surveys assessing work-life balance demonstrated improvement in the physicians’ perception of the administrative burden/paperwork related to practice and a decrease in their perception of the extent to which work encroached on their personal lives. In addition, survey data from 313 patients at the time of their ambulatory visit with a scribe present revealed a high level of comfort. Likewise, surveys completed by physicians after 55 clinical sessions (ie, blocks of consecutive, uninterrupted patient appointments; there are usually 2 sessions per day) revealed good to excellent ratings more than 90% of the time.
Conclusion In an outpatient family medicine clinic, the use of scribes substantially improved physicians’ efficiency, job satisfaction, and productivity without negatively impacting the patient experience.
While electronic medical records (EMRs) are important tools for improving patient care and communication, they bring with them an additional administrative burden for health care providers. In the emergency medicine literature, scribes have been reported to reduce that burden and improve clinicians’ productivity and satisfaction.1-4 Additionally, studies have reported increases in patient volume, generated billings, and provider morale, as well as decreases in emergency department (ED) lengths of stay.5 A recent review of the emergency medicine literature concluded that scribes have “the ability to allay the burden of documentation, improve throughput in the ED, and potentially enhance doctors’ satisfaction.”6
Similar benefits following scribe implementation have been reported in the literature of other specialties. A maternal-fetal medicine practice reported significant increases in generated billings and reimbursement.7 Increases in physician productivity and improvements in physician-patient interactions were reported in a cardiology clinic,8 and a urology practice reported high satisfaction and acceptance rates among both patients and physicians.9
Practice management literature and an article in The New York Times have anecdotally described the benefits of scribes in clinical practice10-12 with the latter noting that, “Physicians who use [scribes] say they feel liberated from the constant note-taking ...” and that “scribes have helped restore joy in the practice of medicine.”10
A small retrospective review that appeared in The Journal of Family Practice last year looked at the quality of scribes’ notes and found that they were rated slightly higher than physicians’ notes—at least for diabetes visits. However, it did not address the issues of physician productivity or satisfaction. (See "Medical scribes: How do their notes stack up?" 2016;65:155-159.)
The only family medicine study that we did find that addressed these 2 issues was one done in Oregon. The study noted that scribes enabled physicians to see 24 patients per day—up from 18, with accompanying improvements in physician “quality of life.”13 Absent from the literature are quantitative data on the feasibility and benefits of implementing scribes in family medicine.
Could a study at our facility offer some insights? In light of the paucity of published data on scribes in family medicine, and the fact that a survey conducted at our health center revealed that our faculty physicians felt overburdened by the administrative demands of clinical practice,14 we decided to study whether scribes might improve the work climate for clinicians at our family medicine residency training site. Our goal was to assess the impact of scribes on physician and patient satisfaction and on hours physicians spent on administrative tasks generated by clinical care.
METHODS
The study took place at the Barre Family Health Center (BFHC), a rural, freestanding family health center/residency site owned and operated by UMassMemorial Health Care (UMMHC), the major teaching/clinical affiliate of the University of Massachusetts Medical School. The health care providers of BFHC conduct 40,000 patient visits annually. Without scribes, the physicians typically dictated their notes at the end of the day, and they became available for review/sign off usually within 24 hours.
Six of the 7 faculty physicians working at BFHC in 2014 (including the lead author) participated in the pilot study (the seventh declined to participate). Three male and 3 female physicians between the ages of 34 and 65 years participated; they had been in practice between 5 and 40 years. All of the physicians had used an EMR for 5 years or more, and all but 2 had previously used a paper record. Residents and advanced practitioners did not participate because limited funding allowed for the hiring of only 2 full-time equivalent (FTE; 4 part-time) scribes.
Contracting for services. We contracted with an outside vendor for scribe services. Prior to their arrival at our health care center, the scribes received online training on medical vocabulary, note structure, billing and coding, and patient confidentiality (HIPAA). Once they arrived, on-site training detailed workflow, precharting, use of templates, the EMR and chart organization, and billing. In addition to typing notes into the EMR during patient visits, the scribes helped develop processes for scheduling, alerting patients to the scribe’s role, and defining when scribes should and should not be present in the exam room. The chief scribe created a monthly schedule, which enabled staff to determine which physician schedules should have extra appointment slots added. This was imperative because our parent institution mandated that new initiatives yield a 25% return on investment (ROI).
Using standard scripting and consent methods, nursing staff informed patients during rooming that the provider was working with a scribe, explained the scribe’s role, and asked about any objections to the scribe’s presence. Patients could decline scribe involvement, and all scribes were routinely excused during genital and rectal examinations.
Data collection
Data were collected during the 6-month trial period from May through October of 2014. The number of hours physicians spent at BFHC and at home working on clinical documentation was collected using a smartphone time-tracking application for two 3-week periods: the first period was in April 2014, before the scribes came on board; the second period was at the end of the 6-month scribe implementation period. In order to assess effects on productivity and whether the project was meeting the required ROI for continuation, we included a retrospective review of the EMR for both of the 3-week periods to document total clinical hours, number of clinic sessions (blocks of consecutive, uninterrupted appointments), average hours per session, the number of patient appointments scheduled per session, and the number of patient visits actually conducted per session (accounting for no-shows and unused appointments).
Physician work-life balance. We utilized 19 questions most relevant to this project’s focus from the 36-item Physician Work-Life Survey.15 Items were scored on a 5-point Likert scale ranging from ‘strongly disagree’ (1) to ‘strongly agree’ (5). The BFHC ambulatory manager distributed surveys to physicians immediately prior to the trial with scribes and 2 weeks after the conclusion of the 6-month trial.
Patient and provider satisfaction. During the 6-month intervention period, satisfaction surveys9 were distributed to patients by scribes at the end of the office visit and to physicians at the end of each scribed session, after notes were completed and reviewed. Patient surveys consisted of 6 closed-end questions regarding comfort level with the scribe in the exam room, willingness to have a scribe present for subsequent visits, importance of the scribe being the same gender/age as the patient, and overall satisfaction with the scribe’s presence (TABLE 1).
Physician surveys included 5 closed-end questions9 regarding comfort level with the scribe’s presence, ease of EMR documentation, change in office hours with having a scribe for that day’s session(s), and overall helpfulness of the scribe (TABLE 2). Open-ended questions on both surveys asked for additional comments or concerns regarding scribes and the scribe’s impact on patient encounters.
Our goal was to collect a minimum of 100 completed patient surveys and 50 completed physician surveys representing as many different patient demographics, visit types, days of the week, and times of day as possible. Surveys were anonymous and distributed during the second and third months of the trial, giving the scribes a one-month training and adjustment period.
Impact assessment, professional development needs. At the end of the 6-month study period, we held 2 focus groups—one with nurses and one with scribes. From the nurses, we solicited insights regarding the impact of scribes on patient volume, patient satisfaction, visit flow, and EMR documentation.
Scribes were asked about job skills needed, amount of training received, comfort in the exam room (both for themselves and patients), frequency of feedback received, balancing physician style with EMR documentation needs, and lessons learned.
Data analysis
Data were analyzed using the software SPSS V22.0. Univariate statistics were used to analyze patient and physician satisfaction, as well as clinic volume, time tracking, and EMR documentation. Initially, bivariate statistics were used to examine pre- and post-trial physician and patient data, but then non-parametric comparisons were used because of small sample sizes (and the resulting data being distributed abnormally). Detailed focus group notes were reviewed by all study investigators and summarized for dominant themes to support the quantitative evaluation. Lastly, the study was evaluated by the University of Massachusetts Institutional Review Board and was waived from review/oversight because of its QI intent.
RESULTS
Physician findings. Fifty-five physician surveys were completed during the 6-month period (TABLE 2). All of the physicians who were asked to complete this short survey at the end of the day (after reviewing notes with their scribe) did so. Physicians reported a high degree of satisfaction with collaboration with scribes. Their comments reflected positive experiences, including an improved ability to remain on schedule, having assistance finding important information in the record, and having notes completed at the end of the session.
TABLE 3 shows high satisfaction with clinical roles and colleagues with no substantive changes over time regarding these questions. However, the incorporation of scribes had a positive impact on issues related to physician morale, due to changes in paperwork, administrative duties, and work schedules.
Review of patient scheduling and documentation (TABLE 4) revealed visits per clinical session increased 28.8% from 6.6 to 8.5, and for sessions with 10 or more appointment slots available, billable visits increased 9.2% from 8.7 to 9.5. This increase was a result of adding an additional appointment slot to the schedule when a scribe was assigned and a greater physician willingness to overbook when scribe assistance was available.
A comparison of time tracking pre- and post-intervention showed a 13% decrease in time spent in the clinic, from a 3-week average of 30.1 hrs/wk to 26.1 hrs/wk (TABLE 4). Time spent working at home decreased 38%, from a 3-week average of 2.9 hrs/wk to 1.8 hrs/wk. These reductions occurred despite average scheduled clinic hours being 18% higher (35.5 vs 30.1) during the post- vs pre-intervention measurement periods.
Patient findings. TABLE 1 summarizes the 313 patient responses. Less than 10% of patients declined to have a scribe during the visit. Patients reported a high level of comfort with the scribe and indicated that having a scribe in the room had little impact on what they would have liked to tell their doctor. Nearly all open-ended comments were positive and reflected feelings that the scribe’s presence enabled their provider to focus more on them and less on the computer.
Focus group findings
The scribe focus group identified a number of skills thought to be necessary to be successful in the job, including typing quickly; having technology/computer-searching strategy skills; and being detail-oriented, organized, and able to multitask. Scribes estimated that it took 2 to 6 weeks to feel comfortable doing the job. Physician feedback was preferred at the end of every session.
Lastly, the 4 scribes identified several challenges that should be addressed in future training, such as how to: 1. document a visit when the patient has a complicated medical history and the communication between the doctor and the patient is implicit; 2. incorporate the particulars of a visit into a patient’s full medical history; and 3. sift through the volume of previous notes when a physician has been seeing a patient for a long period of time.
The nurses’ focus group identified many positive effects on patient care. They reported no significant challenges with introducing scribes to patients. Improvements in timely availability of documentation enhanced their ability to respond quickly and more completely to patient queries. The nurses noted that the use of scribes improved patient care and made them “a better practice.”
DISCUSSION
This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family practitioners spent on charting, improved work-life balance, and had good patient acceptance. Our time-tracking studies demonstrated that physicians spent 5.1 fewer hrs/wk working—4 fewer hrs/wk in the clinic, and 1.1 fewer hrs/wk outside of the clinic—while clinical hours and productivity per session increased. Patients reported high satisfaction with scribed visits and a willingness to have scribes in the future. Creating notes in real time and having immediate availability after the session was a plus for nursing staff in providing follow-up patient care.
Concerns by physicians that having another person in the room would alter the physician-patient relationship were not substantiated, perhaps because the staff routinely obtained consent and explained the scribe’s role. Consistent with previous work, we found no suggestion that a scribe’s presence affected patients’ willingness to discuss sensitive issues.9 Patients reacted positively to scribes who enabled physicians to focus more on the patient and less on charting.
Despite increased patient volume, physician morale improved. Physicians left work more than an hour earlier per day, on average, and spent over 1 hour less per week working on clinical documentation outside the office. Physician surveys showed an improvement in perceptions of how much work encroached on their personal life, consistent with the time-tracking data. These results have significant implications for clinician retention, productivity, and satisfaction.
Since our site is an academic training site, one might wonder how residents and advanced practitioners viewed this implementation, as they were not initially included. From the perspective of the administrators, this was a feasibility study. Clinicians who were not included understood that if this pilot was successful, the use of scribes would be expanded in the future. In fact, because of these positive results, our institution has expanded the scribe program, so that it now covers all clinical sessions for faculty in our center and is rolling out a similar program in 3 other departmental academic practices.
Financial implications. At the beginning of this initiative, our institution required that we cover the cost of the program plus generate a 25% ROI. Using a conservative 9.2% increase in billable visits, we extrapolated that utilizing 2 FTE scribes would result in an additional 860 visits annually. Per our hospital’s finance department, estimated revenue generated by our facility-based practice per visit is $196, including ancillaries. That means that additional visits would generate an estimated $168,600 annually—more than twice the $79,500 annual cost of 2 FTE scribes, yielding a 112% ROI. Furthermore, patient access improved by making more visits available. Beyond the positive direct ROI, the improvements in physician morale and work-life balance have positive implications for retention, likely substantially increasing the long-term, overall ROI.
Challenges. Implementing a new program in a large organization proved to be challenging. The biggest hurdle was convincing our institution’s administration and finance department that this new expense would pay for itself in both tangible (increased visits per session) and intangible (increased physician satisfaction and retention) ways. A cost-sharing arrangement proposed by our department’s administrator convinced hospital administration to move forward. Additional challenges included delays in getting the scribe program started because of vendor selection, purchasing new laptops for scribes, hiring and training scribes, developing new EMR templates, validating provider productivity, and legal/compliance approval of the scribe’s EMR documentation processes to meet third-party and accuracy/quality requirements—all taking longer than anticipated. However, we believe that our results indicate significant potential for other primary care practices.
Limitations. The number of physicians in the study was small, and they all worked in the same location. Social desirability could have biased patient and provider feedback, but our quantitative results were consistent with subjective assessments, suggesting that information bias potential was low. Patient and provider survey findings were also supported by qualitative assessments from both scribes and nursing staff. The size of the project did not lend itself to an analysis controlling for clustering by physician and/or scribe. The focus group discussions were not subject to rigorous qualitative analysis, potentially increasing the risk of biased interpretation. Lastly, we did not have the ability to directly compare sessions with and without scribes during the pilot.
Similarity to other findings. Despite these limitations, our findings are remarkably similar to those of Howard, et al,16 on the pilot implementation of scribes in a community health center, including good patient and clinician acceptance and increased productivity that more than offset the cost of the scribes. We expect that others implementing scribe services in primary care settings will experience similar results.
CORRESPONDENCE
Stephen T. Earls, MD, 151 Worcester Road, Barre, MA 01005; stephen.earls@umassmemorial.org.
ACKNOWLEDGEMENT
The authors gratefully acknowledge the assistance of Barbara Fisher, MBA, vice president for ambulatory services; Nicholas Comeau, BS; and Brenda Rivard, administrative lead, Barre Family Health Center, UMassMemorial Health Care, in the preparation and execution of this study.
ABSTRACT
Purpose Research in other medical specialties has shown that the addition of medical scribes to the clinical team enhances physicians’ practice experience and increases productivity. To date, literature on the implementation of scribes in primary care is limited. To determine the feasibility and benefits of implementing scribes in family medicine, we undertook a pilot mixed-method quality improvement (QI) study.
Methods In 2014, we incorporated 4 part-time scribes into an academic family medicine practice consisting of 7 physicians. We then measured, via survey and time-tracking data, the impact the scribes had on physician office hours and productivity, time spent on documentation, perceptions of work-life balance, and physician and patient satisfaction.
Results Six of the 7 faculty physicians participated. This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family physicians spent on charting, improved work-life balance, and had good patient acceptance. Specifically, the physicians spent an average of 5.1 fewer hours/week (hrs/wk) on documentation, while various measures of productivity revealed increases ranging from 9.2% to 28.8%. Perhaps most important of all, when the results of the pilot study were annualized, they were projected to generate $168,600 per year—more than twice the $79,500 annual cost of 2 full-time equivalent scribes.
Surveys assessing work-life balance demonstrated improvement in the physicians’ perception of the administrative burden/paperwork related to practice and a decrease in their perception of the extent to which work encroached on their personal lives. In addition, survey data from 313 patients at the time of their ambulatory visit with a scribe present revealed a high level of comfort. Likewise, surveys completed by physicians after 55 clinical sessions (ie, blocks of consecutive, uninterrupted patient appointments; there are usually 2 sessions per day) revealed good to excellent ratings more than 90% of the time.
Conclusion In an outpatient family medicine clinic, the use of scribes substantially improved physicians’ efficiency, job satisfaction, and productivity without negatively impacting the patient experience.
While electronic medical records (EMRs) are important tools for improving patient care and communication, they bring with them an additional administrative burden for health care providers. In the emergency medicine literature, scribes have been reported to reduce that burden and improve clinicians’ productivity and satisfaction.1-4 Additionally, studies have reported increases in patient volume, generated billings, and provider morale, as well as decreases in emergency department (ED) lengths of stay.5 A recent review of the emergency medicine literature concluded that scribes have “the ability to allay the burden of documentation, improve throughput in the ED, and potentially enhance doctors’ satisfaction.”6
Similar benefits following scribe implementation have been reported in the literature of other specialties. A maternal-fetal medicine practice reported significant increases in generated billings and reimbursement.7 Increases in physician productivity and improvements in physician-patient interactions were reported in a cardiology clinic,8 and a urology practice reported high satisfaction and acceptance rates among both patients and physicians.9
Practice management literature and an article in The New York Times have anecdotally described the benefits of scribes in clinical practice10-12 with the latter noting that, “Physicians who use [scribes] say they feel liberated from the constant note-taking ...” and that “scribes have helped restore joy in the practice of medicine.”10
A small retrospective review that appeared in The Journal of Family Practice last year looked at the quality of scribes’ notes and found that they were rated slightly higher than physicians’ notes—at least for diabetes visits. However, it did not address the issues of physician productivity or satisfaction. (See "Medical scribes: How do their notes stack up?" 2016;65:155-159.)
The only family medicine study that we did find that addressed these 2 issues was one done in Oregon. The study noted that scribes enabled physicians to see 24 patients per day—up from 18, with accompanying improvements in physician “quality of life.”13 Absent from the literature are quantitative data on the feasibility and benefits of implementing scribes in family medicine.
Could a study at our facility offer some insights? In light of the paucity of published data on scribes in family medicine, and the fact that a survey conducted at our health center revealed that our faculty physicians felt overburdened by the administrative demands of clinical practice,14 we decided to study whether scribes might improve the work climate for clinicians at our family medicine residency training site. Our goal was to assess the impact of scribes on physician and patient satisfaction and on hours physicians spent on administrative tasks generated by clinical care.
METHODS
The study took place at the Barre Family Health Center (BFHC), a rural, freestanding family health center/residency site owned and operated by UMassMemorial Health Care (UMMHC), the major teaching/clinical affiliate of the University of Massachusetts Medical School. The health care providers of BFHC conduct 40,000 patient visits annually. Without scribes, the physicians typically dictated their notes at the end of the day, and they became available for review/sign off usually within 24 hours.
Six of the 7 faculty physicians working at BFHC in 2014 (including the lead author) participated in the pilot study (the seventh declined to participate). Three male and 3 female physicians between the ages of 34 and 65 years participated; they had been in practice between 5 and 40 years. All of the physicians had used an EMR for 5 years or more, and all but 2 had previously used a paper record. Residents and advanced practitioners did not participate because limited funding allowed for the hiring of only 2 full-time equivalent (FTE; 4 part-time) scribes.
Contracting for services. We contracted with an outside vendor for scribe services. Prior to their arrival at our health care center, the scribes received online training on medical vocabulary, note structure, billing and coding, and patient confidentiality (HIPAA). Once they arrived, on-site training detailed workflow, precharting, use of templates, the EMR and chart organization, and billing. In addition to typing notes into the EMR during patient visits, the scribes helped develop processes for scheduling, alerting patients to the scribe’s role, and defining when scribes should and should not be present in the exam room. The chief scribe created a monthly schedule, which enabled staff to determine which physician schedules should have extra appointment slots added. This was imperative because our parent institution mandated that new initiatives yield a 25% return on investment (ROI).
Using standard scripting and consent methods, nursing staff informed patients during rooming that the provider was working with a scribe, explained the scribe’s role, and asked about any objections to the scribe’s presence. Patients could decline scribe involvement, and all scribes were routinely excused during genital and rectal examinations.
Data collection
Data were collected during the 6-month trial period from May through October of 2014. The number of hours physicians spent at BFHC and at home working on clinical documentation was collected using a smartphone time-tracking application for two 3-week periods: the first period was in April 2014, before the scribes came on board; the second period was at the end of the 6-month scribe implementation period. In order to assess effects on productivity and whether the project was meeting the required ROI for continuation, we included a retrospective review of the EMR for both of the 3-week periods to document total clinical hours, number of clinic sessions (blocks of consecutive, uninterrupted appointments), average hours per session, the number of patient appointments scheduled per session, and the number of patient visits actually conducted per session (accounting for no-shows and unused appointments).
Physician work-life balance. We utilized 19 questions most relevant to this project’s focus from the 36-item Physician Work-Life Survey.15 Items were scored on a 5-point Likert scale ranging from ‘strongly disagree’ (1) to ‘strongly agree’ (5). The BFHC ambulatory manager distributed surveys to physicians immediately prior to the trial with scribes and 2 weeks after the conclusion of the 6-month trial.
Patient and provider satisfaction. During the 6-month intervention period, satisfaction surveys9 were distributed to patients by scribes at the end of the office visit and to physicians at the end of each scribed session, after notes were completed and reviewed. Patient surveys consisted of 6 closed-end questions regarding comfort level with the scribe in the exam room, willingness to have a scribe present for subsequent visits, importance of the scribe being the same gender/age as the patient, and overall satisfaction with the scribe’s presence (TABLE 1).
Physician surveys included 5 closed-end questions9 regarding comfort level with the scribe’s presence, ease of EMR documentation, change in office hours with having a scribe for that day’s session(s), and overall helpfulness of the scribe (TABLE 2). Open-ended questions on both surveys asked for additional comments or concerns regarding scribes and the scribe’s impact on patient encounters.
Our goal was to collect a minimum of 100 completed patient surveys and 50 completed physician surveys representing as many different patient demographics, visit types, days of the week, and times of day as possible. Surveys were anonymous and distributed during the second and third months of the trial, giving the scribes a one-month training and adjustment period.
Impact assessment, professional development needs. At the end of the 6-month study period, we held 2 focus groups—one with nurses and one with scribes. From the nurses, we solicited insights regarding the impact of scribes on patient volume, patient satisfaction, visit flow, and EMR documentation.
Scribes were asked about job skills needed, amount of training received, comfort in the exam room (both for themselves and patients), frequency of feedback received, balancing physician style with EMR documentation needs, and lessons learned.
Data analysis
Data were analyzed using the software SPSS V22.0. Univariate statistics were used to analyze patient and physician satisfaction, as well as clinic volume, time tracking, and EMR documentation. Initially, bivariate statistics were used to examine pre- and post-trial physician and patient data, but then non-parametric comparisons were used because of small sample sizes (and the resulting data being distributed abnormally). Detailed focus group notes were reviewed by all study investigators and summarized for dominant themes to support the quantitative evaluation. Lastly, the study was evaluated by the University of Massachusetts Institutional Review Board and was waived from review/oversight because of its QI intent.
RESULTS
Physician findings. Fifty-five physician surveys were completed during the 6-month period (TABLE 2). All of the physicians who were asked to complete this short survey at the end of the day (after reviewing notes with their scribe) did so. Physicians reported a high degree of satisfaction with collaboration with scribes. Their comments reflected positive experiences, including an improved ability to remain on schedule, having assistance finding important information in the record, and having notes completed at the end of the session.
TABLE 3 shows high satisfaction with clinical roles and colleagues with no substantive changes over time regarding these questions. However, the incorporation of scribes had a positive impact on issues related to physician morale, due to changes in paperwork, administrative duties, and work schedules.
Review of patient scheduling and documentation (TABLE 4) revealed visits per clinical session increased 28.8% from 6.6 to 8.5, and for sessions with 10 or more appointment slots available, billable visits increased 9.2% from 8.7 to 9.5. This increase was a result of adding an additional appointment slot to the schedule when a scribe was assigned and a greater physician willingness to overbook when scribe assistance was available.
A comparison of time tracking pre- and post-intervention showed a 13% decrease in time spent in the clinic, from a 3-week average of 30.1 hrs/wk to 26.1 hrs/wk (TABLE 4). Time spent working at home decreased 38%, from a 3-week average of 2.9 hrs/wk to 1.8 hrs/wk. These reductions occurred despite average scheduled clinic hours being 18% higher (35.5 vs 30.1) during the post- vs pre-intervention measurement periods.
Patient findings. TABLE 1 summarizes the 313 patient responses. Less than 10% of patients declined to have a scribe during the visit. Patients reported a high level of comfort with the scribe and indicated that having a scribe in the room had little impact on what they would have liked to tell their doctor. Nearly all open-ended comments were positive and reflected feelings that the scribe’s presence enabled their provider to focus more on them and less on the computer.
Focus group findings
The scribe focus group identified a number of skills thought to be necessary to be successful in the job, including typing quickly; having technology/computer-searching strategy skills; and being detail-oriented, organized, and able to multitask. Scribes estimated that it took 2 to 6 weeks to feel comfortable doing the job. Physician feedback was preferred at the end of every session.
Lastly, the 4 scribes identified several challenges that should be addressed in future training, such as how to: 1. document a visit when the patient has a complicated medical history and the communication between the doctor and the patient is implicit; 2. incorporate the particulars of a visit into a patient’s full medical history; and 3. sift through the volume of previous notes when a physician has been seeing a patient for a long period of time.
The nurses’ focus group identified many positive effects on patient care. They reported no significant challenges with introducing scribes to patients. Improvements in timely availability of documentation enhanced their ability to respond quickly and more completely to patient queries. The nurses noted that the use of scribes improved patient care and made them “a better practice.”
DISCUSSION
This study demonstrated that the use of scribes in a busy academic primary care practice substantially reduced the amount of time that family practitioners spent on charting, improved work-life balance, and had good patient acceptance. Our time-tracking studies demonstrated that physicians spent 5.1 fewer hrs/wk working—4 fewer hrs/wk in the clinic, and 1.1 fewer hrs/wk outside of the clinic—while clinical hours and productivity per session increased. Patients reported high satisfaction with scribed visits and a willingness to have scribes in the future. Creating notes in real time and having immediate availability after the session was a plus for nursing staff in providing follow-up patient care.
Concerns by physicians that having another person in the room would alter the physician-patient relationship were not substantiated, perhaps because the staff routinely obtained consent and explained the scribe’s role. Consistent with previous work, we found no suggestion that a scribe’s presence affected patients’ willingness to discuss sensitive issues.9 Patients reacted positively to scribes who enabled physicians to focus more on the patient and less on charting.
Despite increased patient volume, physician morale improved. Physicians left work more than an hour earlier per day, on average, and spent over 1 hour less per week working on clinical documentation outside the office. Physician surveys showed an improvement in perceptions of how much work encroached on their personal life, consistent with the time-tracking data. These results have significant implications for clinician retention, productivity, and satisfaction.
Since our site is an academic training site, one might wonder how residents and advanced practitioners viewed this implementation, as they were not initially included. From the perspective of the administrators, this was a feasibility study. Clinicians who were not included understood that if this pilot was successful, the use of scribes would be expanded in the future. In fact, because of these positive results, our institution has expanded the scribe program, so that it now covers all clinical sessions for faculty in our center and is rolling out a similar program in 3 other departmental academic practices.
Financial implications. At the beginning of this initiative, our institution required that we cover the cost of the program plus generate a 25% ROI. Using a conservative 9.2% increase in billable visits, we extrapolated that utilizing 2 FTE scribes would result in an additional 860 visits annually. Per our hospital’s finance department, estimated revenue generated by our facility-based practice per visit is $196, including ancillaries. That means that additional visits would generate an estimated $168,600 annually—more than twice the $79,500 annual cost of 2 FTE scribes, yielding a 112% ROI. Furthermore, patient access improved by making more visits available. Beyond the positive direct ROI, the improvements in physician morale and work-life balance have positive implications for retention, likely substantially increasing the long-term, overall ROI.
Challenges. Implementing a new program in a large organization proved to be challenging. The biggest hurdle was convincing our institution’s administration and finance department that this new expense would pay for itself in both tangible (increased visits per session) and intangible (increased physician satisfaction and retention) ways. A cost-sharing arrangement proposed by our department’s administrator convinced hospital administration to move forward. Additional challenges included delays in getting the scribe program started because of vendor selection, purchasing new laptops for scribes, hiring and training scribes, developing new EMR templates, validating provider productivity, and legal/compliance approval of the scribe’s EMR documentation processes to meet third-party and accuracy/quality requirements—all taking longer than anticipated. However, we believe that our results indicate significant potential for other primary care practices.
Limitations. The number of physicians in the study was small, and they all worked in the same location. Social desirability could have biased patient and provider feedback, but our quantitative results were consistent with subjective assessments, suggesting that information bias potential was low. Patient and provider survey findings were also supported by qualitative assessments from both scribes and nursing staff. The size of the project did not lend itself to an analysis controlling for clustering by physician and/or scribe. The focus group discussions were not subject to rigorous qualitative analysis, potentially increasing the risk of biased interpretation. Lastly, we did not have the ability to directly compare sessions with and without scribes during the pilot.
Similarity to other findings. Despite these limitations, our findings are remarkably similar to those of Howard, et al,16 on the pilot implementation of scribes in a community health center, including good patient and clinician acceptance and increased productivity that more than offset the cost of the scribes. We expect that others implementing scribe services in primary care settings will experience similar results.
CORRESPONDENCE
Stephen T. Earls, MD, 151 Worcester Road, Barre, MA 01005; stephen.earls@umassmemorial.org.
ACKNOWLEDGEMENT
The authors gratefully acknowledge the assistance of Barbara Fisher, MBA, vice president for ambulatory services; Nicholas Comeau, BS; and Brenda Rivard, administrative lead, Barre Family Health Center, UMassMemorial Health Care, in the preparation and execution of this study.
1. Walker K, Ben-Meir M, O’Mullane P, et al. Scribes in an Australian private emergency department: a description of physician productivity. Emerg Med Australas. 2014;26:543-548.
2. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
3. Expanded scribe role boosts staff morale. ED Manag. 2009;21:75-77.
4. Scribes, EMR please docs, save $600,000. ED Manag. 2009;21:117-118.
5. Bastani A, Shaqiri B, Palomba K, et al. An ED scribe program is able to improve throughput time and patient satisfaction. Am J Emerg Med. 2014;32:399-402.
6. Cabilan CJ, Eley RM. Review article: potential of medical scribes to allay the burden of documentation and enhance efficiency in Australian emergency departments. Emerg Med Australas. 2015 Aug 13. [Epub ahead of print]
7. Hegstrom L, Leslie J, Hutchinson E, et al. Medical scribes: are scribe programs cost effective in an outpatient MFM setting? Am J Obstet Gynecol. 2013;208:S240.
8. Campbell LL, Case D, Crocker JE, et al. Using medical scribes in a physician practice. J AHIMA. 2012;83:64-69.
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262.
10. Hafner K. A busy doctor’s right hand, ever ready to type. The New York Times. January 12, 2014. Available at: https://www.nytimes.com/2014/01/14/health/a-busy-doctors-right-hand-ever-ready-to-type.html?_r=0. Accessed February 6, 2017.
11. Brady K, Shariff A. Virtual medical scribes: making electronic medical records work for you. J Med Pract Manage. 2013;29:133-136.
12. Baugh R, Jones JE, Troff K, et al. Medical scribes. J Med Pract Manage. 2012;28:195-197.
13. Grimshaw H. Physician scribes improve productivity. Oak Street Medical allows doctors to spend more face time with patients, improve job satisfaction. MGMA Connex. 2012;12:27-28.
14. Morehead Associates, Inc. UMassMemorial Health Care: Physician Satisfaction Survey. 2013.
15. Konrad TR, Williams ES, Linzer M, et al. Measuring physician job satisfaction in a changing workplace and challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37:1174-1182.
16. Howard KA, Helé K, Salibi N, et al. BTW Informing change. Blue Shield of California Foundation. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Available at: http://informingchange.com/cat-publications/adapting-the-ehr-scribe-model-to-community-health-centers-the-experience-of-shasta-community-health-centers-pilot. Accessed November 6, 2015.
1. Walker K, Ben-Meir M, O’Mullane P, et al. Scribes in an Australian private emergency department: a description of physician productivity. Emerg Med Australas. 2014;26:543-548.
2. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
3. Expanded scribe role boosts staff morale. ED Manag. 2009;21:75-77.
4. Scribes, EMR please docs, save $600,000. ED Manag. 2009;21:117-118.
5. Bastani A, Shaqiri B, Palomba K, et al. An ED scribe program is able to improve throughput time and patient satisfaction. Am J Emerg Med. 2014;32:399-402.
6. Cabilan CJ, Eley RM. Review article: potential of medical scribes to allay the burden of documentation and enhance efficiency in Australian emergency departments. Emerg Med Australas. 2015 Aug 13. [Epub ahead of print]
7. Hegstrom L, Leslie J, Hutchinson E, et al. Medical scribes: are scribe programs cost effective in an outpatient MFM setting? Am J Obstet Gynecol. 2013;208:S240.
8. Campbell LL, Case D, Crocker JE, et al. Using medical scribes in a physician practice. J AHIMA. 2012;83:64-69.
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262.
10. Hafner K. A busy doctor’s right hand, ever ready to type. The New York Times. January 12, 2014. Available at: https://www.nytimes.com/2014/01/14/health/a-busy-doctors-right-hand-ever-ready-to-type.html?_r=0. Accessed February 6, 2017.
11. Brady K, Shariff A. Virtual medical scribes: making electronic medical records work for you. J Med Pract Manage. 2013;29:133-136.
12. Baugh R, Jones JE, Troff K, et al. Medical scribes. J Med Pract Manage. 2012;28:195-197.
13. Grimshaw H. Physician scribes improve productivity. Oak Street Medical allows doctors to spend more face time with patients, improve job satisfaction. MGMA Connex. 2012;12:27-28.
14. Morehead Associates, Inc. UMassMemorial Health Care: Physician Satisfaction Survey. 2013.
15. Konrad TR, Williams ES, Linzer M, et al. Measuring physician job satisfaction in a changing workplace and challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37:1174-1182.
16. Howard KA, Helé K, Salibi N, et al. BTW Informing change. Blue Shield of California Foundation. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Available at: http://informingchange.com/cat-publications/adapting-the-ehr-scribe-model-to-community-health-centers-the-experience-of-shasta-community-health-centers-pilot. Accessed November 6, 2015.
Is extended-release oxybutynin (Ditropan XL) or tolterodine (Detrol) more effective in the treatment of an overactive bladder?
BACKGROUND: Anticholinergic medications are the mainstay of pharmacologic therapy for an overactive bladder (defined as urge incontinence, urgency, or frequency). Immediate-release oxybutynin and tolterodine (the most popular options) are equally effective, but tolterodine has a better side effect profile. The efficacy and tolerability of the newly developed extended-release oxybutynin is compared with tolterodine in this study.
POPULATION STUDIED: The investigators enrolled 378 mostly white (87%), mostly women (83%) participants aged 21 to 87 years (mean=59 years); 88% of the participants completed the study. The patients were required to experience between 7 and 50 episodes of urge incontinence per week and 10 or more voids in a 24-hour period. The study was conducted in 37 specialty outpatient-based practices across the United States. Previous exposure or response to therapy did not preclude participation. Patients were excluded if they had uncontrolled medical conditions, significant risk for urinary retention, or incontinence related to prostatitis, interstitial cystitis, urinary tract obstruction, urethral diverticulum, bladder tumor, bladder stone, prostate cancer, or urinary tract infection. Other exclusions included pelvic organ prolapse, pregnancy, and potential poor adherence to therapy.
STUDY DESIGN AND VALIDITY: This was a prospective randomized controlled trial (RCT) sponsored by the makers of oxybutynin. The study participants were treated for 12 weeks with either oxybutynin 10 mg per day or tolterodine 2 mg twice daily. Stratified randomization insured equal representation of mild incontinence (≤21 episodes weekly) and moderate to severe incontinence (>21 episodes weekly) within each treatment group. Study visits occurred at weeks 2, 4, 8, and 12. Each subject kept a 24-hour urinary diary documenting micturition frequency and the number and nature of incontinence episodes during the 7-day period before each study visit. The participants were asked at each visit about adverse events or unusual symptoms. This study was well designed, avoiding bias with a double-blind double-dummy stratified randomization approach. Dropout rates were similar for the 2 groups. Formal intention-to-treat analysis was not possible, but the authors stated that analysis of partial data from dropouts was not different from reported results. The study may not be generalizable to most primary care populations, since patients were recruited exclusively from specialty practices. The authors adjusted for the nonsignificant baseline differences in incontinence frequency; this is statistically valid but not necessary in an randomized controlled trial. Without this adjustment, outcome differences between the 2 medications were substantially smaller and no longer statistically significant.
OUTCOMES MEASURED: The primary outcome measured was baseline versus end of study (week 12) episodes of urge incontinence. Total episodes of incontinence, micturition frequency, and medication side effects were secondary outcomes.
RESULTS: Both treatment groups showed a substantial reduction in urge incontinence, total incontinence, and micturition frequency. Urge incontinence decreased 76% in the oxybutynin-treated group and 68% in the tolterodine-treated group (P=.03). Total incontinence episodes in the oxybutynin-treated group dropped 75% from 28.6 to 7.1 episodes per week, while decreasing 66% from 27.0 to 9.3 episodes per week in the tolterodine-treated group. The net difference between the groups was 3.8 (P=.02) or 2.1 (P=NS) fewer episodes of incontinence per week with extended-release oxybutynin, adjusting or not adjusting for the baseline difference between the groups. Weekly bathroom trips declined by 27% in the oxybutynin-treated group versus 22% in the tolterodine-treated group (P=.02). Rates of side effects were similar for oxybutynin compared with tolterodine.
Oxybutynin and tolterodine both produce a marked decrease in symptoms in patients with an overactive bladder. These medications have a similar cost ($78 monthly) and side effect profile, but extended-release oxybutynin is modestly more effective than tolterodine. This small advantage may be important to patients in whom a decrease of 2 to 4 fewer episodes of incontinence per week represents a substantial improvement. However, the combination of anticholinergic medication and behavioral therapy provides an even greater benefit than pharmacotherapy alone.1
BACKGROUND: Anticholinergic medications are the mainstay of pharmacologic therapy for an overactive bladder (defined as urge incontinence, urgency, or frequency). Immediate-release oxybutynin and tolterodine (the most popular options) are equally effective, but tolterodine has a better side effect profile. The efficacy and tolerability of the newly developed extended-release oxybutynin is compared with tolterodine in this study.
POPULATION STUDIED: The investigators enrolled 378 mostly white (87%), mostly women (83%) participants aged 21 to 87 years (mean=59 years); 88% of the participants completed the study. The patients were required to experience between 7 and 50 episodes of urge incontinence per week and 10 or more voids in a 24-hour period. The study was conducted in 37 specialty outpatient-based practices across the United States. Previous exposure or response to therapy did not preclude participation. Patients were excluded if they had uncontrolled medical conditions, significant risk for urinary retention, or incontinence related to prostatitis, interstitial cystitis, urinary tract obstruction, urethral diverticulum, bladder tumor, bladder stone, prostate cancer, or urinary tract infection. Other exclusions included pelvic organ prolapse, pregnancy, and potential poor adherence to therapy.
STUDY DESIGN AND VALIDITY: This was a prospective randomized controlled trial (RCT) sponsored by the makers of oxybutynin. The study participants were treated for 12 weeks with either oxybutynin 10 mg per day or tolterodine 2 mg twice daily. Stratified randomization insured equal representation of mild incontinence (≤21 episodes weekly) and moderate to severe incontinence (>21 episodes weekly) within each treatment group. Study visits occurred at weeks 2, 4, 8, and 12. Each subject kept a 24-hour urinary diary documenting micturition frequency and the number and nature of incontinence episodes during the 7-day period before each study visit. The participants were asked at each visit about adverse events or unusual symptoms. This study was well designed, avoiding bias with a double-blind double-dummy stratified randomization approach. Dropout rates were similar for the 2 groups. Formal intention-to-treat analysis was not possible, but the authors stated that analysis of partial data from dropouts was not different from reported results. The study may not be generalizable to most primary care populations, since patients were recruited exclusively from specialty practices. The authors adjusted for the nonsignificant baseline differences in incontinence frequency; this is statistically valid but not necessary in an randomized controlled trial. Without this adjustment, outcome differences between the 2 medications were substantially smaller and no longer statistically significant.
OUTCOMES MEASURED: The primary outcome measured was baseline versus end of study (week 12) episodes of urge incontinence. Total episodes of incontinence, micturition frequency, and medication side effects were secondary outcomes.
RESULTS: Both treatment groups showed a substantial reduction in urge incontinence, total incontinence, and micturition frequency. Urge incontinence decreased 76% in the oxybutynin-treated group and 68% in the tolterodine-treated group (P=.03). Total incontinence episodes in the oxybutynin-treated group dropped 75% from 28.6 to 7.1 episodes per week, while decreasing 66% from 27.0 to 9.3 episodes per week in the tolterodine-treated group. The net difference between the groups was 3.8 (P=.02) or 2.1 (P=NS) fewer episodes of incontinence per week with extended-release oxybutynin, adjusting or not adjusting for the baseline difference between the groups. Weekly bathroom trips declined by 27% in the oxybutynin-treated group versus 22% in the tolterodine-treated group (P=.02). Rates of side effects were similar for oxybutynin compared with tolterodine.
Oxybutynin and tolterodine both produce a marked decrease in symptoms in patients with an overactive bladder. These medications have a similar cost ($78 monthly) and side effect profile, but extended-release oxybutynin is modestly more effective than tolterodine. This small advantage may be important to patients in whom a decrease of 2 to 4 fewer episodes of incontinence per week represents a substantial improvement. However, the combination of anticholinergic medication and behavioral therapy provides an even greater benefit than pharmacotherapy alone.1
BACKGROUND: Anticholinergic medications are the mainstay of pharmacologic therapy for an overactive bladder (defined as urge incontinence, urgency, or frequency). Immediate-release oxybutynin and tolterodine (the most popular options) are equally effective, but tolterodine has a better side effect profile. The efficacy and tolerability of the newly developed extended-release oxybutynin is compared with tolterodine in this study.
POPULATION STUDIED: The investigators enrolled 378 mostly white (87%), mostly women (83%) participants aged 21 to 87 years (mean=59 years); 88% of the participants completed the study. The patients were required to experience between 7 and 50 episodes of urge incontinence per week and 10 or more voids in a 24-hour period. The study was conducted in 37 specialty outpatient-based practices across the United States. Previous exposure or response to therapy did not preclude participation. Patients were excluded if they had uncontrolled medical conditions, significant risk for urinary retention, or incontinence related to prostatitis, interstitial cystitis, urinary tract obstruction, urethral diverticulum, bladder tumor, bladder stone, prostate cancer, or urinary tract infection. Other exclusions included pelvic organ prolapse, pregnancy, and potential poor adherence to therapy.
STUDY DESIGN AND VALIDITY: This was a prospective randomized controlled trial (RCT) sponsored by the makers of oxybutynin. The study participants were treated for 12 weeks with either oxybutynin 10 mg per day or tolterodine 2 mg twice daily. Stratified randomization insured equal representation of mild incontinence (≤21 episodes weekly) and moderate to severe incontinence (>21 episodes weekly) within each treatment group. Study visits occurred at weeks 2, 4, 8, and 12. Each subject kept a 24-hour urinary diary documenting micturition frequency and the number and nature of incontinence episodes during the 7-day period before each study visit. The participants were asked at each visit about adverse events or unusual symptoms. This study was well designed, avoiding bias with a double-blind double-dummy stratified randomization approach. Dropout rates were similar for the 2 groups. Formal intention-to-treat analysis was not possible, but the authors stated that analysis of partial data from dropouts was not different from reported results. The study may not be generalizable to most primary care populations, since patients were recruited exclusively from specialty practices. The authors adjusted for the nonsignificant baseline differences in incontinence frequency; this is statistically valid but not necessary in an randomized controlled trial. Without this adjustment, outcome differences between the 2 medications were substantially smaller and no longer statistically significant.
OUTCOMES MEASURED: The primary outcome measured was baseline versus end of study (week 12) episodes of urge incontinence. Total episodes of incontinence, micturition frequency, and medication side effects were secondary outcomes.
RESULTS: Both treatment groups showed a substantial reduction in urge incontinence, total incontinence, and micturition frequency. Urge incontinence decreased 76% in the oxybutynin-treated group and 68% in the tolterodine-treated group (P=.03). Total incontinence episodes in the oxybutynin-treated group dropped 75% from 28.6 to 7.1 episodes per week, while decreasing 66% from 27.0 to 9.3 episodes per week in the tolterodine-treated group. The net difference between the groups was 3.8 (P=.02) or 2.1 (P=NS) fewer episodes of incontinence per week with extended-release oxybutynin, adjusting or not adjusting for the baseline difference between the groups. Weekly bathroom trips declined by 27% in the oxybutynin-treated group versus 22% in the tolterodine-treated group (P=.02). Rates of side effects were similar for oxybutynin compared with tolterodine.
Oxybutynin and tolterodine both produce a marked decrease in symptoms in patients with an overactive bladder. These medications have a similar cost ($78 monthly) and side effect profile, but extended-release oxybutynin is modestly more effective than tolterodine. This small advantage may be important to patients in whom a decrease of 2 to 4 fewer episodes of incontinence per week represents a substantial improvement. However, the combination of anticholinergic medication and behavioral therapy provides an even greater benefit than pharmacotherapy alone.1
Physicians’ Advice to Quit Smoking
METHODS: We examined data from the ationally representative 1996-1997 Community Tracking Study Household Survey. We used multivariate logistic regression to model receipt of cessation advice in a sample of 8229 smokers aged 18 years and older who made at least one visit to a physician in the past year.
RESULTS: Less than 50% of the subjects reported receiving cessation advice. Advice was less likely for patients who were younger, men, African American, uninsured, healthier, lower health care services users, or lighter smokers, and more likely for those with military health insurance, who attended hospital outpatient clinics, or who belonged to health maintenance organizations.
CONCLUSIONS: Physicians continue to miss opportunities to provide smoking cessation advice, a potentially lifesaving intervention. Given the adverse health consequences of tobacco use and the demonstrated benefit of advice to quit, physicians need to improve their cessation counseling efforts.
Cigarette smoking is the leading preventable cause of death and disability in the United States.1 Because the majority of people who smoke visit a physician each year, physicians are in a key position to promote cessation.2 Although some research has suggested that simple physician cessation counseling without additional counseling or pharmacotherapy does not improve long-term cessation rates,3-5 most studies,6-8 including the 1996 Agency for Health Care Policy and Research (AHCPR) Tobacco Cessation Guideline9 and a recent Cochrane Collaboration review,10 suggest that even simple advice from a physician is effective in promoting long-term cessation, and the AHCPR guideline gave cessation counseling its highest recommendation.
However, in 1991 only 37% of smokers nationally reported being advised to quit by their providers during the previous year.2 The authors of another study11 estimated that 46% of smokers in Rhode Island had been advised to quit in 1990, and the Stanford Five-City Project12 reported that only 50% of smokers in 1989 to 1990 had ever been advised to quit. Although cessation counseling was reported to have almost doubled from 1991 to 1993, it then declined by 1995.13 Factors observed to be associated with a greater likelihood of cessation advice include seeing a primary care physician, having a routine checkup, having cardiovascular or chronic pulmonary disease, and being pregnant.2,11,14,15 Some studies have shown that minority group members are less likely to have received cessation advice.2,15 Other studies have revealed a mixed picture, showing Hispanics to be less likely to receive counseling12,14 and African Americans more likely to receive this advice,14 or no difference.13
We measured the percentage of smokers reporting they had received smoking cessation advice from a physician during a 12-month interval, using data from a recent nationally representative survey. Also, we investigated relationships between the odds of respondents reporting cessation advice from a physician and respondents’ characteristics, including sociodemographic factors, health insurance status, physician continuity, intensity of smoking, and health status.
Methods
Data Source
We used data from the Community Tracking Study (CTS) Household Survey conducted in 1996 and 1997,16 a telephone survey of individuals representing the US housed, noninstitutionalized population. The survey used a stratified multistage area probability sampling design, and information was recorded about smoking behaviors and interventions, sociodemographics, health insurance, utilization, and health status. For our study, we included the 8229 subjects aged 18 years and older who were current smokers and had made at least one visit to a physician in the previous 12 months.
Dependent Variable
Subjects were asked: “During the past 12 months, did any medical doctor advise you to stop smoking?” This measure has demonstrated reliability and validity.12,17
Independent Variables
We included sociodemographics (age, sex, education, household income as a percentage of poverty level, race or ethnicity, employment status, and residence location), health insurance status, usual care location, provider continuity, smoking intensity, utilization (number of physician visits, emergency room visits, and hospitalizations) and the physical and mental component summary scales of the Medical Outcomes Study 12-item Short-Form Health Survey (SF-12) for perceived health status.18
Analysis
We used weights provided on the public use files to yield population estimates adjusted for survey oversampling and nonresponse. Because of the complex survey design of the CTS, we conducted analyses with SUDAAN19 software, which uses the method of Taylor series linearization for producing appropriate standard errors and 95% confidence intervals. Logistic regression analyses were performed to obtain odds ratios adjusted for potential confounders.
Results
The baseline characteristics of the sample are presented in Table 1. Overall, 48% of subjects, all of whom were smokers who had visited a clinic at least once in 12 months, had received cessation advice from a physician during this time period. Persons reporting the highest prevalence of cessation advice (>56%) included those who smoked more than 2 packs per day, had perceived health status categorized as fair or poor, had at least one hospitalization, made 4 or more physician visits, were aged 65 years or older, had Medicare, or had military coverage. Persons reporting the lowest prevalence of cessation advice (<40%) included those who lacked health insurance, did not smoke every day, lacked a usual care site or identified an emergency room or other location, had perceived health status categorized as excellent, or had made only one visit to a physician in 12 months.
Multivariate evaluation Table 2 revealed lower odds of receiving advice among persons who were younger, men, African American, uninsured, healthier on the SF-12 subscales, lower users of health care services, lighter smokers, or who lacked a usual care location or used an emergency room or other location. The odds of receiving advice were increased for persons with military health insurance and those who received their care in hospital clinics.
Discussion
Less than 50% of the surveyed patients reported that they had been counseled to quit smoking by a physician during the 12-month period. This finding is similar to earlier published reports,2,11-13 indicating that little progress has been made toward achieving national health goals for 20009,20 and performance standards for health plans.21 Since by 1996 and 1997, the years the CTS was administered, ample evidence supported use of brief motivational counseling,6-9 it is unfortunate that rates of physicians’ cessation counseling advice had not improved substantially compared with earlier reports. Further, the low rate of physician cessation advice we observed likely indicates that more intensive cessation services were even less frequently offered. For example, the benefits of pharmacotherapy had been well documented by the time the CTS was administered,22 but it seems unlikely that medications for cessation would have been recommended to respondents who reported they did not receive cessation advice.
We observed significant associations between lower rates of physicians’ cessation advice and several patient factors. First, lower rates of physician counseling were reported by persons with the lowest current burden of smoking-related illness, including those who were younger, had better perceived health status, and had lower smoking intensity. Although greater attention to persons with end-organ damage is understandable, cessation advice for primary prevention, such as to younger persons, might yield the greatest long-term benefit. Second, men were less likely to report receiving cessation advice, even after adjusting for their lower utilization of health care services. This finding, consistent with observations indicating that men are much less likely than women to receive preventive care,23 suggests that approaches to helping men become more effective consumers of health care need to be developed.24 Third, respondents who lacked a usual care location or used an emergency room or other location were less likely to report they received cessation advice, supporting approaches to health care delivery that promote continuity of care. Fourth, persons who lacked health insurance were less likely to report they received cessation advice independent of other factors. Given that such persons frequently face myriad obstacles to accessing health care, including financial barriers to pharmacotherapy for cessation, efforts aimed at increasing the provision of cessation counseling services to these persons are warranted. Finally, the lower rates of physician counseling among African Americans, independent of other factors, demands attention, especially because African Americans have been targeted by cigarette manufacturers, advertisers, and merchants.24-28 Efforts to increase cessation counseling provided to African Americans who smoke might help reduce disparities in health status.
Limitations
Our study is subject to several limitations. It is difficult to assess the reliability and validity of patient reports, and it is possible that recall of physicians’ advice to quit could deteriorate as the interval between administration of the survey and the clinical encounter lengthened. However, past studies have supported the validity of patient report of physicians’ cessation advice.12,17 Also, although we were not able to account for the time interval since the last visit, we were able to adjust for respondents’ total number of clinical encounters in 12 months. Given that respondents had roughly 4 visits on average, we believe the magnitude of recall bias would be low.
Although it is possible that the observed relationships could be the result of confounding by unmeasured or incompletely measured factors, the richness of our data source allowed us to control for a wide range of potential confounders. The inferences that can be drawn from these results are further strengthened by the survey design and the recency of the data.
Many physician-level and system-level factors could not be evaluated, so future exploration of contextual factors is warranted. What specific features of hospital clinics, health maintenance organizations, or military coverage account for higher rates of cessation advice? Might physicians who practice in such settings have greater access to systems that help identify smokers, thereby improving cessation interventions?
Conclusions
Although the 1996 AHCPR smoking cessation guideline9 gives counseling its highest recommendation, our findings suggest that physicians are performing poorly on this measure, with little improvement since the early 1990s. Many physicians might benefit from being trained in the use of brief counseling techniques that have been found effective.9,10 System changes designed to promote cessation should be implemented in clinical settings. For example, physicians are more likely to provide cessation advice when patients’ smoking status is routinely identified in the medical record.29,30,31 Funds from tobacco settlements could provide the funding for system-level interventions but reportedly are infrequently being applied toward smoking cessation efforts.32
Tobacco cessation has received increasing attention, especially because the effectiveness of counseling and pharmacotherapy has been unequivocally demonstrated during the past several years. However, this study reveals a troubling lack of improvement in physicians’ cessation advice during this time. Sometimes 50% means the glass is half full. However, given the serious health consequences of tobacco use and the demonstrated benefit of physicians’ advice to quit,6-10 in this situation the glass remains half empty.
Acknowledgments
Our study was funded in part through the Robert Wood Johnson Foundation under its Changes in Health Care Financing and Organization Program.
1. for Disease Control and Prevention. Reducing the health consequences of smoking: 25 years of progress-a report of the Surgeon General. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1989. DHHS publication no. (CDC) 89-8411.
2. for Disease Control and Prevention. Physician and other health-care professional counseling of smokers to quit: United States, 1991. MMWR Morb Mortal Wkly Rep 1993;42:854-57.
3. SR, Coates TJ, Richard RJ, et al. Training physicians in counseling about smoking cessation: a randomized trial of the “Quit for Life” program. Ann Intern Med 1989;110:640-47.
4. SR, Richard RJ, Duncan CL, et al. Training physicians about smoking cessation: a controlled trial in private practices. J Gen Intern Med 1989;4:482-29.
5. H, Susman JL, Davis C, Gilbert C. Physician counseling for smoking cessation: is the glass half empty? J Fam Pract 1995;40:148-52.
6. MAH, Wilson C, Taylor C, Baker CD. Effect of general practitioners’ advice against smoking. BMJ 1979;2:231-35.
7. D, Wood G, Johnston N, Sicuvella J. Randomized clinical trial of supportive follow-up for cigarette smokers in a family practice. Can Med Assoc J 1982;126:127-29.
8. JK, Kristeller J, Goldberg R, et al. Increasing the efficacy of physician-delivered smoking interventions: a randomized clinical trial. J Gen Intern Med 1991;6:1-8.
9. MC, Bailey WC, Cohen SJ, et al. Smoking cessation. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1996. AHCPR publication no. 96-0692.
10. C, Ketteridge S. Physician advice for smoking cessation. In: The Cochrane library Oxford, England: Update Software; 1999.
11. MG, Niaura R, Willey-Lessne C, et al. Physicians counseling smokers: a population-based survey of patients’ perceptions of health care provider-delivered smoking cessation interventions. Arch Intern Med 1997;157:1313-19.
12. E, Winkleby MA, Altman DG, Rockhill B, Fortmann SP. Predictors of physician’s smoking cessation advice. JAMA 1991;266:3139-44.
13. AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA 1998;279:604-8.
14. EA, Pierce JP, Johnson M, Bal D. Physician advice to quit smoking: results from the 1990 California Tobacco Survey. J Gen Intern Med 1993;8:549-53.
15. RF, Remington PL, Sienko DG, Davis RM. Are physicians advising smokers to quit? The patient’s perspective. JAMA 1987;257:1916-19.
16. P, Blumenthal D, Corrigan JM, et al. The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 1996;33:195-206.
17. SP, Sallis JF, Magnus PM, Farquhar JW. Attitudes and practices of physicians regarding hypertension and smoking: the Stanford Five City Project. Prev Med 1985;14:70-80.
18. J , Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33.
19. Triangle Institute. SUDAAN. Professional software for survey data analysis. Version 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997.
20. Department of Health and Human Services. Healthy people 2000: national health promotion and disease prevention objectives. Washington, DC: US Department of Health and Human Services; 1991. Publication (PHS) 91-50213.
21. Committee for Quality Assurance. HEDIS 3.0, vol 2: technical specifications. Washington, DC: National Committee for Quality Assurance; 1997.
22. MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation: a meta-analysis. JAMA 1994;271:1940-47.
23. R, Lion J, Anderson OW. Two decades of health services research: social survey trends in use and expenditures. Cambridge, Mass: Ballinger; 1976.
24. P, Clancy CM, Naumburg EH. Sex, access, and excess. Ann Intern Med 1995;123:548-50.
25. CC, Yanek LR, Stillman FA, Becker DM. Reducing cigarette sales to minors in an urban setting: issues and opportunities for merchant intervention. Am J Prev Med 1998;14:138-42.
26. CC, Swank RT, Stillman FA, Harris DX, Watson HW, Becker DM. Cigarette sales to African-American and white minors in low-income areas of Baltimore. Am J Public Health 1997;87:652-54.
27. RM. Current trends in cigarette advertising and marketing. N Engl J Med 1987;216:725-32.
28. R. Race, sex, economics and tobacco advertising. J Natl Med Assoc 1989;81:1119-24.
29. KM, Giovino G, Mendicino AJ. Cigarette advertising and black-white differences in brand preference. Public Health Rep 1987;102:699-701.
30. MC, Jorenby DE, Schensky AE, Smith SS, Bauer RR, Baker TB. Smoking status as the new vital sign: effect on assessment and intervention in patients who smoke. Mayo Clin Proc 1995;70:209-13.
31. SJ, Christen AG, Katz BP, et al. Counseling medical and dental patients about cigarette smoking: the impact of nicotine gum and chart reminders. Am J Public Health 1987;77:313-16.
32. G. States plan assorted uses for tobacco settlement. Wall Street Journal New York, NY; August 24, 1999:A4.
METHODS: We examined data from the ationally representative 1996-1997 Community Tracking Study Household Survey. We used multivariate logistic regression to model receipt of cessation advice in a sample of 8229 smokers aged 18 years and older who made at least one visit to a physician in the past year.
RESULTS: Less than 50% of the subjects reported receiving cessation advice. Advice was less likely for patients who were younger, men, African American, uninsured, healthier, lower health care services users, or lighter smokers, and more likely for those with military health insurance, who attended hospital outpatient clinics, or who belonged to health maintenance organizations.
CONCLUSIONS: Physicians continue to miss opportunities to provide smoking cessation advice, a potentially lifesaving intervention. Given the adverse health consequences of tobacco use and the demonstrated benefit of advice to quit, physicians need to improve their cessation counseling efforts.
Cigarette smoking is the leading preventable cause of death and disability in the United States.1 Because the majority of people who smoke visit a physician each year, physicians are in a key position to promote cessation.2 Although some research has suggested that simple physician cessation counseling without additional counseling or pharmacotherapy does not improve long-term cessation rates,3-5 most studies,6-8 including the 1996 Agency for Health Care Policy and Research (AHCPR) Tobacco Cessation Guideline9 and a recent Cochrane Collaboration review,10 suggest that even simple advice from a physician is effective in promoting long-term cessation, and the AHCPR guideline gave cessation counseling its highest recommendation.
However, in 1991 only 37% of smokers nationally reported being advised to quit by their providers during the previous year.2 The authors of another study11 estimated that 46% of smokers in Rhode Island had been advised to quit in 1990, and the Stanford Five-City Project12 reported that only 50% of smokers in 1989 to 1990 had ever been advised to quit. Although cessation counseling was reported to have almost doubled from 1991 to 1993, it then declined by 1995.13 Factors observed to be associated with a greater likelihood of cessation advice include seeing a primary care physician, having a routine checkup, having cardiovascular or chronic pulmonary disease, and being pregnant.2,11,14,15 Some studies have shown that minority group members are less likely to have received cessation advice.2,15 Other studies have revealed a mixed picture, showing Hispanics to be less likely to receive counseling12,14 and African Americans more likely to receive this advice,14 or no difference.13
We measured the percentage of smokers reporting they had received smoking cessation advice from a physician during a 12-month interval, using data from a recent nationally representative survey. Also, we investigated relationships between the odds of respondents reporting cessation advice from a physician and respondents’ characteristics, including sociodemographic factors, health insurance status, physician continuity, intensity of smoking, and health status.
Methods
Data Source
We used data from the Community Tracking Study (CTS) Household Survey conducted in 1996 and 1997,16 a telephone survey of individuals representing the US housed, noninstitutionalized population. The survey used a stratified multistage area probability sampling design, and information was recorded about smoking behaviors and interventions, sociodemographics, health insurance, utilization, and health status. For our study, we included the 8229 subjects aged 18 years and older who were current smokers and had made at least one visit to a physician in the previous 12 months.
Dependent Variable
Subjects were asked: “During the past 12 months, did any medical doctor advise you to stop smoking?” This measure has demonstrated reliability and validity.12,17
Independent Variables
We included sociodemographics (age, sex, education, household income as a percentage of poverty level, race or ethnicity, employment status, and residence location), health insurance status, usual care location, provider continuity, smoking intensity, utilization (number of physician visits, emergency room visits, and hospitalizations) and the physical and mental component summary scales of the Medical Outcomes Study 12-item Short-Form Health Survey (SF-12) for perceived health status.18
Analysis
We used weights provided on the public use files to yield population estimates adjusted for survey oversampling and nonresponse. Because of the complex survey design of the CTS, we conducted analyses with SUDAAN19 software, which uses the method of Taylor series linearization for producing appropriate standard errors and 95% confidence intervals. Logistic regression analyses were performed to obtain odds ratios adjusted for potential confounders.
Results
The baseline characteristics of the sample are presented in Table 1. Overall, 48% of subjects, all of whom were smokers who had visited a clinic at least once in 12 months, had received cessation advice from a physician during this time period. Persons reporting the highest prevalence of cessation advice (>56%) included those who smoked more than 2 packs per day, had perceived health status categorized as fair or poor, had at least one hospitalization, made 4 or more physician visits, were aged 65 years or older, had Medicare, or had military coverage. Persons reporting the lowest prevalence of cessation advice (<40%) included those who lacked health insurance, did not smoke every day, lacked a usual care site or identified an emergency room or other location, had perceived health status categorized as excellent, or had made only one visit to a physician in 12 months.
Multivariate evaluation Table 2 revealed lower odds of receiving advice among persons who were younger, men, African American, uninsured, healthier on the SF-12 subscales, lower users of health care services, lighter smokers, or who lacked a usual care location or used an emergency room or other location. The odds of receiving advice were increased for persons with military health insurance and those who received their care in hospital clinics.
Discussion
Less than 50% of the surveyed patients reported that they had been counseled to quit smoking by a physician during the 12-month period. This finding is similar to earlier published reports,2,11-13 indicating that little progress has been made toward achieving national health goals for 20009,20 and performance standards for health plans.21 Since by 1996 and 1997, the years the CTS was administered, ample evidence supported use of brief motivational counseling,6-9 it is unfortunate that rates of physicians’ cessation counseling advice had not improved substantially compared with earlier reports. Further, the low rate of physician cessation advice we observed likely indicates that more intensive cessation services were even less frequently offered. For example, the benefits of pharmacotherapy had been well documented by the time the CTS was administered,22 but it seems unlikely that medications for cessation would have been recommended to respondents who reported they did not receive cessation advice.
We observed significant associations between lower rates of physicians’ cessation advice and several patient factors. First, lower rates of physician counseling were reported by persons with the lowest current burden of smoking-related illness, including those who were younger, had better perceived health status, and had lower smoking intensity. Although greater attention to persons with end-organ damage is understandable, cessation advice for primary prevention, such as to younger persons, might yield the greatest long-term benefit. Second, men were less likely to report receiving cessation advice, even after adjusting for their lower utilization of health care services. This finding, consistent with observations indicating that men are much less likely than women to receive preventive care,23 suggests that approaches to helping men become more effective consumers of health care need to be developed.24 Third, respondents who lacked a usual care location or used an emergency room or other location were less likely to report they received cessation advice, supporting approaches to health care delivery that promote continuity of care. Fourth, persons who lacked health insurance were less likely to report they received cessation advice independent of other factors. Given that such persons frequently face myriad obstacles to accessing health care, including financial barriers to pharmacotherapy for cessation, efforts aimed at increasing the provision of cessation counseling services to these persons are warranted. Finally, the lower rates of physician counseling among African Americans, independent of other factors, demands attention, especially because African Americans have been targeted by cigarette manufacturers, advertisers, and merchants.24-28 Efforts to increase cessation counseling provided to African Americans who smoke might help reduce disparities in health status.
Limitations
Our study is subject to several limitations. It is difficult to assess the reliability and validity of patient reports, and it is possible that recall of physicians’ advice to quit could deteriorate as the interval between administration of the survey and the clinical encounter lengthened. However, past studies have supported the validity of patient report of physicians’ cessation advice.12,17 Also, although we were not able to account for the time interval since the last visit, we were able to adjust for respondents’ total number of clinical encounters in 12 months. Given that respondents had roughly 4 visits on average, we believe the magnitude of recall bias would be low.
Although it is possible that the observed relationships could be the result of confounding by unmeasured or incompletely measured factors, the richness of our data source allowed us to control for a wide range of potential confounders. The inferences that can be drawn from these results are further strengthened by the survey design and the recency of the data.
Many physician-level and system-level factors could not be evaluated, so future exploration of contextual factors is warranted. What specific features of hospital clinics, health maintenance organizations, or military coverage account for higher rates of cessation advice? Might physicians who practice in such settings have greater access to systems that help identify smokers, thereby improving cessation interventions?
Conclusions
Although the 1996 AHCPR smoking cessation guideline9 gives counseling its highest recommendation, our findings suggest that physicians are performing poorly on this measure, with little improvement since the early 1990s. Many physicians might benefit from being trained in the use of brief counseling techniques that have been found effective.9,10 System changes designed to promote cessation should be implemented in clinical settings. For example, physicians are more likely to provide cessation advice when patients’ smoking status is routinely identified in the medical record.29,30,31 Funds from tobacco settlements could provide the funding for system-level interventions but reportedly are infrequently being applied toward smoking cessation efforts.32
Tobacco cessation has received increasing attention, especially because the effectiveness of counseling and pharmacotherapy has been unequivocally demonstrated during the past several years. However, this study reveals a troubling lack of improvement in physicians’ cessation advice during this time. Sometimes 50% means the glass is half full. However, given the serious health consequences of tobacco use and the demonstrated benefit of physicians’ advice to quit,6-10 in this situation the glass remains half empty.
Acknowledgments
Our study was funded in part through the Robert Wood Johnson Foundation under its Changes in Health Care Financing and Organization Program.
METHODS: We examined data from the ationally representative 1996-1997 Community Tracking Study Household Survey. We used multivariate logistic regression to model receipt of cessation advice in a sample of 8229 smokers aged 18 years and older who made at least one visit to a physician in the past year.
RESULTS: Less than 50% of the subjects reported receiving cessation advice. Advice was less likely for patients who were younger, men, African American, uninsured, healthier, lower health care services users, or lighter smokers, and more likely for those with military health insurance, who attended hospital outpatient clinics, or who belonged to health maintenance organizations.
CONCLUSIONS: Physicians continue to miss opportunities to provide smoking cessation advice, a potentially lifesaving intervention. Given the adverse health consequences of tobacco use and the demonstrated benefit of advice to quit, physicians need to improve their cessation counseling efforts.
Cigarette smoking is the leading preventable cause of death and disability in the United States.1 Because the majority of people who smoke visit a physician each year, physicians are in a key position to promote cessation.2 Although some research has suggested that simple physician cessation counseling without additional counseling or pharmacotherapy does not improve long-term cessation rates,3-5 most studies,6-8 including the 1996 Agency for Health Care Policy and Research (AHCPR) Tobacco Cessation Guideline9 and a recent Cochrane Collaboration review,10 suggest that even simple advice from a physician is effective in promoting long-term cessation, and the AHCPR guideline gave cessation counseling its highest recommendation.
However, in 1991 only 37% of smokers nationally reported being advised to quit by their providers during the previous year.2 The authors of another study11 estimated that 46% of smokers in Rhode Island had been advised to quit in 1990, and the Stanford Five-City Project12 reported that only 50% of smokers in 1989 to 1990 had ever been advised to quit. Although cessation counseling was reported to have almost doubled from 1991 to 1993, it then declined by 1995.13 Factors observed to be associated with a greater likelihood of cessation advice include seeing a primary care physician, having a routine checkup, having cardiovascular or chronic pulmonary disease, and being pregnant.2,11,14,15 Some studies have shown that minority group members are less likely to have received cessation advice.2,15 Other studies have revealed a mixed picture, showing Hispanics to be less likely to receive counseling12,14 and African Americans more likely to receive this advice,14 or no difference.13
We measured the percentage of smokers reporting they had received smoking cessation advice from a physician during a 12-month interval, using data from a recent nationally representative survey. Also, we investigated relationships between the odds of respondents reporting cessation advice from a physician and respondents’ characteristics, including sociodemographic factors, health insurance status, physician continuity, intensity of smoking, and health status.
Methods
Data Source
We used data from the Community Tracking Study (CTS) Household Survey conducted in 1996 and 1997,16 a telephone survey of individuals representing the US housed, noninstitutionalized population. The survey used a stratified multistage area probability sampling design, and information was recorded about smoking behaviors and interventions, sociodemographics, health insurance, utilization, and health status. For our study, we included the 8229 subjects aged 18 years and older who were current smokers and had made at least one visit to a physician in the previous 12 months.
Dependent Variable
Subjects were asked: “During the past 12 months, did any medical doctor advise you to stop smoking?” This measure has demonstrated reliability and validity.12,17
Independent Variables
We included sociodemographics (age, sex, education, household income as a percentage of poverty level, race or ethnicity, employment status, and residence location), health insurance status, usual care location, provider continuity, smoking intensity, utilization (number of physician visits, emergency room visits, and hospitalizations) and the physical and mental component summary scales of the Medical Outcomes Study 12-item Short-Form Health Survey (SF-12) for perceived health status.18
Analysis
We used weights provided on the public use files to yield population estimates adjusted for survey oversampling and nonresponse. Because of the complex survey design of the CTS, we conducted analyses with SUDAAN19 software, which uses the method of Taylor series linearization for producing appropriate standard errors and 95% confidence intervals. Logistic regression analyses were performed to obtain odds ratios adjusted for potential confounders.
Results
The baseline characteristics of the sample are presented in Table 1. Overall, 48% of subjects, all of whom were smokers who had visited a clinic at least once in 12 months, had received cessation advice from a physician during this time period. Persons reporting the highest prevalence of cessation advice (>56%) included those who smoked more than 2 packs per day, had perceived health status categorized as fair or poor, had at least one hospitalization, made 4 or more physician visits, were aged 65 years or older, had Medicare, or had military coverage. Persons reporting the lowest prevalence of cessation advice (<40%) included those who lacked health insurance, did not smoke every day, lacked a usual care site or identified an emergency room or other location, had perceived health status categorized as excellent, or had made only one visit to a physician in 12 months.
Multivariate evaluation Table 2 revealed lower odds of receiving advice among persons who were younger, men, African American, uninsured, healthier on the SF-12 subscales, lower users of health care services, lighter smokers, or who lacked a usual care location or used an emergency room or other location. The odds of receiving advice were increased for persons with military health insurance and those who received their care in hospital clinics.
Discussion
Less than 50% of the surveyed patients reported that they had been counseled to quit smoking by a physician during the 12-month period. This finding is similar to earlier published reports,2,11-13 indicating that little progress has been made toward achieving national health goals for 20009,20 and performance standards for health plans.21 Since by 1996 and 1997, the years the CTS was administered, ample evidence supported use of brief motivational counseling,6-9 it is unfortunate that rates of physicians’ cessation counseling advice had not improved substantially compared with earlier reports. Further, the low rate of physician cessation advice we observed likely indicates that more intensive cessation services were even less frequently offered. For example, the benefits of pharmacotherapy had been well documented by the time the CTS was administered,22 but it seems unlikely that medications for cessation would have been recommended to respondents who reported they did not receive cessation advice.
We observed significant associations between lower rates of physicians’ cessation advice and several patient factors. First, lower rates of physician counseling were reported by persons with the lowest current burden of smoking-related illness, including those who were younger, had better perceived health status, and had lower smoking intensity. Although greater attention to persons with end-organ damage is understandable, cessation advice for primary prevention, such as to younger persons, might yield the greatest long-term benefit. Second, men were less likely to report receiving cessation advice, even after adjusting for their lower utilization of health care services. This finding, consistent with observations indicating that men are much less likely than women to receive preventive care,23 suggests that approaches to helping men become more effective consumers of health care need to be developed.24 Third, respondents who lacked a usual care location or used an emergency room or other location were less likely to report they received cessation advice, supporting approaches to health care delivery that promote continuity of care. Fourth, persons who lacked health insurance were less likely to report they received cessation advice independent of other factors. Given that such persons frequently face myriad obstacles to accessing health care, including financial barriers to pharmacotherapy for cessation, efforts aimed at increasing the provision of cessation counseling services to these persons are warranted. Finally, the lower rates of physician counseling among African Americans, independent of other factors, demands attention, especially because African Americans have been targeted by cigarette manufacturers, advertisers, and merchants.24-28 Efforts to increase cessation counseling provided to African Americans who smoke might help reduce disparities in health status.
Limitations
Our study is subject to several limitations. It is difficult to assess the reliability and validity of patient reports, and it is possible that recall of physicians’ advice to quit could deteriorate as the interval between administration of the survey and the clinical encounter lengthened. However, past studies have supported the validity of patient report of physicians’ cessation advice.12,17 Also, although we were not able to account for the time interval since the last visit, we were able to adjust for respondents’ total number of clinical encounters in 12 months. Given that respondents had roughly 4 visits on average, we believe the magnitude of recall bias would be low.
Although it is possible that the observed relationships could be the result of confounding by unmeasured or incompletely measured factors, the richness of our data source allowed us to control for a wide range of potential confounders. The inferences that can be drawn from these results are further strengthened by the survey design and the recency of the data.
Many physician-level and system-level factors could not be evaluated, so future exploration of contextual factors is warranted. What specific features of hospital clinics, health maintenance organizations, or military coverage account for higher rates of cessation advice? Might physicians who practice in such settings have greater access to systems that help identify smokers, thereby improving cessation interventions?
Conclusions
Although the 1996 AHCPR smoking cessation guideline9 gives counseling its highest recommendation, our findings suggest that physicians are performing poorly on this measure, with little improvement since the early 1990s. Many physicians might benefit from being trained in the use of brief counseling techniques that have been found effective.9,10 System changes designed to promote cessation should be implemented in clinical settings. For example, physicians are more likely to provide cessation advice when patients’ smoking status is routinely identified in the medical record.29,30,31 Funds from tobacco settlements could provide the funding for system-level interventions but reportedly are infrequently being applied toward smoking cessation efforts.32
Tobacco cessation has received increasing attention, especially because the effectiveness of counseling and pharmacotherapy has been unequivocally demonstrated during the past several years. However, this study reveals a troubling lack of improvement in physicians’ cessation advice during this time. Sometimes 50% means the glass is half full. However, given the serious health consequences of tobacco use and the demonstrated benefit of physicians’ advice to quit,6-10 in this situation the glass remains half empty.
Acknowledgments
Our study was funded in part through the Robert Wood Johnson Foundation under its Changes in Health Care Financing and Organization Program.
1. for Disease Control and Prevention. Reducing the health consequences of smoking: 25 years of progress-a report of the Surgeon General. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1989. DHHS publication no. (CDC) 89-8411.
2. for Disease Control and Prevention. Physician and other health-care professional counseling of smokers to quit: United States, 1991. MMWR Morb Mortal Wkly Rep 1993;42:854-57.
3. SR, Coates TJ, Richard RJ, et al. Training physicians in counseling about smoking cessation: a randomized trial of the “Quit for Life” program. Ann Intern Med 1989;110:640-47.
4. SR, Richard RJ, Duncan CL, et al. Training physicians about smoking cessation: a controlled trial in private practices. J Gen Intern Med 1989;4:482-29.
5. H, Susman JL, Davis C, Gilbert C. Physician counseling for smoking cessation: is the glass half empty? J Fam Pract 1995;40:148-52.
6. MAH, Wilson C, Taylor C, Baker CD. Effect of general practitioners’ advice against smoking. BMJ 1979;2:231-35.
7. D, Wood G, Johnston N, Sicuvella J. Randomized clinical trial of supportive follow-up for cigarette smokers in a family practice. Can Med Assoc J 1982;126:127-29.
8. JK, Kristeller J, Goldberg R, et al. Increasing the efficacy of physician-delivered smoking interventions: a randomized clinical trial. J Gen Intern Med 1991;6:1-8.
9. MC, Bailey WC, Cohen SJ, et al. Smoking cessation. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1996. AHCPR publication no. 96-0692.
10. C, Ketteridge S. Physician advice for smoking cessation. In: The Cochrane library Oxford, England: Update Software; 1999.
11. MG, Niaura R, Willey-Lessne C, et al. Physicians counseling smokers: a population-based survey of patients’ perceptions of health care provider-delivered smoking cessation interventions. Arch Intern Med 1997;157:1313-19.
12. E, Winkleby MA, Altman DG, Rockhill B, Fortmann SP. Predictors of physician’s smoking cessation advice. JAMA 1991;266:3139-44.
13. AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA 1998;279:604-8.
14. EA, Pierce JP, Johnson M, Bal D. Physician advice to quit smoking: results from the 1990 California Tobacco Survey. J Gen Intern Med 1993;8:549-53.
15. RF, Remington PL, Sienko DG, Davis RM. Are physicians advising smokers to quit? The patient’s perspective. JAMA 1987;257:1916-19.
16. P, Blumenthal D, Corrigan JM, et al. The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 1996;33:195-206.
17. SP, Sallis JF, Magnus PM, Farquhar JW. Attitudes and practices of physicians regarding hypertension and smoking: the Stanford Five City Project. Prev Med 1985;14:70-80.
18. J , Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33.
19. Triangle Institute. SUDAAN. Professional software for survey data analysis. Version 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997.
20. Department of Health and Human Services. Healthy people 2000: national health promotion and disease prevention objectives. Washington, DC: US Department of Health and Human Services; 1991. Publication (PHS) 91-50213.
21. Committee for Quality Assurance. HEDIS 3.0, vol 2: technical specifications. Washington, DC: National Committee for Quality Assurance; 1997.
22. MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation: a meta-analysis. JAMA 1994;271:1940-47.
23. R, Lion J, Anderson OW. Two decades of health services research: social survey trends in use and expenditures. Cambridge, Mass: Ballinger; 1976.
24. P, Clancy CM, Naumburg EH. Sex, access, and excess. Ann Intern Med 1995;123:548-50.
25. CC, Yanek LR, Stillman FA, Becker DM. Reducing cigarette sales to minors in an urban setting: issues and opportunities for merchant intervention. Am J Prev Med 1998;14:138-42.
26. CC, Swank RT, Stillman FA, Harris DX, Watson HW, Becker DM. Cigarette sales to African-American and white minors in low-income areas of Baltimore. Am J Public Health 1997;87:652-54.
27. RM. Current trends in cigarette advertising and marketing. N Engl J Med 1987;216:725-32.
28. R. Race, sex, economics and tobacco advertising. J Natl Med Assoc 1989;81:1119-24.
29. KM, Giovino G, Mendicino AJ. Cigarette advertising and black-white differences in brand preference. Public Health Rep 1987;102:699-701.
30. MC, Jorenby DE, Schensky AE, Smith SS, Bauer RR, Baker TB. Smoking status as the new vital sign: effect on assessment and intervention in patients who smoke. Mayo Clin Proc 1995;70:209-13.
31. SJ, Christen AG, Katz BP, et al. Counseling medical and dental patients about cigarette smoking: the impact of nicotine gum and chart reminders. Am J Public Health 1987;77:313-16.
32. G. States plan assorted uses for tobacco settlement. Wall Street Journal New York, NY; August 24, 1999:A4.
1. for Disease Control and Prevention. Reducing the health consequences of smoking: 25 years of progress-a report of the Surgeon General. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1989. DHHS publication no. (CDC) 89-8411.
2. for Disease Control and Prevention. Physician and other health-care professional counseling of smokers to quit: United States, 1991. MMWR Morb Mortal Wkly Rep 1993;42:854-57.
3. SR, Coates TJ, Richard RJ, et al. Training physicians in counseling about smoking cessation: a randomized trial of the “Quit for Life” program. Ann Intern Med 1989;110:640-47.
4. SR, Richard RJ, Duncan CL, et al. Training physicians about smoking cessation: a controlled trial in private practices. J Gen Intern Med 1989;4:482-29.
5. H, Susman JL, Davis C, Gilbert C. Physician counseling for smoking cessation: is the glass half empty? J Fam Pract 1995;40:148-52.
6. MAH, Wilson C, Taylor C, Baker CD. Effect of general practitioners’ advice against smoking. BMJ 1979;2:231-35.
7. D, Wood G, Johnston N, Sicuvella J. Randomized clinical trial of supportive follow-up for cigarette smokers in a family practice. Can Med Assoc J 1982;126:127-29.
8. JK, Kristeller J, Goldberg R, et al. Increasing the efficacy of physician-delivered smoking interventions: a randomized clinical trial. J Gen Intern Med 1991;6:1-8.
9. MC, Bailey WC, Cohen SJ, et al. Smoking cessation. Rockville, Md: US Department of Health and Human Services, Public Health Service; 1996. AHCPR publication no. 96-0692.
10. C, Ketteridge S. Physician advice for smoking cessation. In: The Cochrane library Oxford, England: Update Software; 1999.
11. MG, Niaura R, Willey-Lessne C, et al. Physicians counseling smokers: a population-based survey of patients’ perceptions of health care provider-delivered smoking cessation interventions. Arch Intern Med 1997;157:1313-19.
12. E, Winkleby MA, Altman DG, Rockhill B, Fortmann SP. Predictors of physician’s smoking cessation advice. JAMA 1991;266:3139-44.
13. AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA 1998;279:604-8.
14. EA, Pierce JP, Johnson M, Bal D. Physician advice to quit smoking: results from the 1990 California Tobacco Survey. J Gen Intern Med 1993;8:549-53.
15. RF, Remington PL, Sienko DG, Davis RM. Are physicians advising smokers to quit? The patient’s perspective. JAMA 1987;257:1916-19.
16. P, Blumenthal D, Corrigan JM, et al. The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 1996;33:195-206.
17. SP, Sallis JF, Magnus PM, Farquhar JW. Attitudes and practices of physicians regarding hypertension and smoking: the Stanford Five City Project. Prev Med 1985;14:70-80.
18. J , Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33.
19. Triangle Institute. SUDAAN. Professional software for survey data analysis. Version 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997.
20. Department of Health and Human Services. Healthy people 2000: national health promotion and disease prevention objectives. Washington, DC: US Department of Health and Human Services; 1991. Publication (PHS) 91-50213.
21. Committee for Quality Assurance. HEDIS 3.0, vol 2: technical specifications. Washington, DC: National Committee for Quality Assurance; 1997.
22. MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation: a meta-analysis. JAMA 1994;271:1940-47.
23. R, Lion J, Anderson OW. Two decades of health services research: social survey trends in use and expenditures. Cambridge, Mass: Ballinger; 1976.
24. P, Clancy CM, Naumburg EH. Sex, access, and excess. Ann Intern Med 1995;123:548-50.
25. CC, Yanek LR, Stillman FA, Becker DM. Reducing cigarette sales to minors in an urban setting: issues and opportunities for merchant intervention. Am J Prev Med 1998;14:138-42.
26. CC, Swank RT, Stillman FA, Harris DX, Watson HW, Becker DM. Cigarette sales to African-American and white minors in low-income areas of Baltimore. Am J Public Health 1997;87:652-54.
27. RM. Current trends in cigarette advertising and marketing. N Engl J Med 1987;216:725-32.
28. R. Race, sex, economics and tobacco advertising. J Natl Med Assoc 1989;81:1119-24.
29. KM, Giovino G, Mendicino AJ. Cigarette advertising and black-white differences in brand preference. Public Health Rep 1987;102:699-701.
30. MC, Jorenby DE, Schensky AE, Smith SS, Bauer RR, Baker TB. Smoking status as the new vital sign: effect on assessment and intervention in patients who smoke. Mayo Clin Proc 1995;70:209-13.
31. SJ, Christen AG, Katz BP, et al. Counseling medical and dental patients about cigarette smoking: the impact of nicotine gum and chart reminders. Am J Public Health 1987;77:313-16.
32. G. States plan assorted uses for tobacco settlement. Wall Street Journal New York, NY; August 24, 1999:A4.