User login
The Herbal Hospitalist
In 2002, the NIH surveyed more than 30,000 U.S. adults regarding their use of complementary and alternative medicine (CAM).1 This survey revealed that approximately 40% of U.S. adults had used some form of CAM in the past year. When one excludes prayer as a CAM modality, the most common modality used was the category of natural products (i.e., herbs and dietary supplements).
This has significant implications for all healthcare providers, but especially for those who practice in the hospital environment. Herbs can be potentially toxic in their own right and can cause drug-herb interactions as well. Such adverse effects may be particularly important in hospitalized patients undergoing surgery or who are acutely ill and exposed to a number of narrow-window therapeutic pharmaceuticals. Thus, it is imperative for hospital physicians to have a basic understanding of some of the risks, challenges, and potential benefits of herbs.
Use of Herbs by Hospitalized Patients
Surveys performed in the United States and around the world consistently demonstrate that the use of dietary supplements and herbs tends to be higher (as is all CAM usage) in individuals with chronic or incurable diseases. This is especially true for conditions such as HIV, diabetes, heart disease, and cancer.2–6 Thus, considering the complexity of illness of most hospitalized patients, it should not be surprising that use of herbs and dietary supplements is high in the hospital population. This has been borne out in several national and international studies.
A study reported in the Annals of Emergency Medicine in 2000 found that 56% of ED patients had tried alternative therapies in the past.7 The most frequently tried alternative therapies were massage therapy (31%), chiropractic (30%), and herbs (24%). Interestingly, 70% of the respondents who had tried these alternative therapies did not inform their physicians, highlighting a challenge for physicians and caregivers in the hospital setting.
Kay and colleagues reported 1,017 patients presenting for a preanesthetic evaluation prior to surgery.8 They found that 482 of 755 (64%) of patients had used at least one natural product. The majority of these were vitamin users, but several herbs with potential importance in the hospital setting were used as well: garlic extract (43%), ginkgo (32%), St. John’s wort (30%), ephedra (18%), and echinacea (12%).
Pediatric patients are not immune to the use of herbs and dietary supplement either. A survey at Children’s Hospital in Boston looked at 1,100 patients younger than 18 during their preoperative visit.9 A total of 1,021 surveys were completed and, of these, 30% patients indicated that they had tried one or more complementary and alternative therapies in the past year before surgery. Importantly, 13% had used herbal remedies before surgery.
Finally, international studies confirm similar usage patterns in adult hospital patients in Germany, Spain, Hong Kong, and Australia.10–13 Thus, it appears well established that the use of dietary supplements has become a fixed part of conventional healthcare. Recognizing that a significant percentage of patients under our care are using herbs is the first step in bringing critically needed information and guidance to our patients.
Herb Toxicity and Herb–Drug Interactions
There are many well-recognized herbal toxicities and/or drug-herb interactions with which all clinicians should have some degree of familiarity. For example, St. John’s wort stimulation of the cytochrome P450 enzyme system resulting in enhanced metabolism of several pharmaceutical drugs has been well reported. Ephedra’s ability to induce elevated blood pressure, stroke, and MI also received a great deal of publicity. (Note: Ephedra sales were banned by the FDA in 2004. However the prohibition excluded ephedra-containing teas, and—despite the ban—many internet sites still have ephedra available for purchase. Thus, be aware that your patients may still have access to ephedra.)
Which herbs might have specific importance in the hospital setting? This question was answered to some degree by researchers at the University of Chicago in 2001.14 The authors reviewed the literature on commonly used herbal medications in the context of the perioperative period and attempted to provide rationale strategies for managing their preoperative use. They identified echinacea, ephedra, garlic, ginkgo, ginseng, kava, St. John’s wort, and valerian as commonly used herbal medications that could pose a concern during the perioperative period.
Direct effects include bleeding from garlic, ginkgo, and ginseng; cardiovascular instability from ephedra; and hypoglycemia from ginseng. Pharmacodynamic herb-drug interactions include potentiation of the sedative effects of anesthetic by kava and valerian. Pharmacokinetic herb-drug interactions include increased metabolism of many drugs used in the perioperative period by St. John’s wort. (The findings are outlined in “Table 1. Clinically Important Effects and Perioperative Concerns of Eight Herbal Medicines and Recommendations for Discontinuation of Use Before Surgery,” p. 16.)
These authors concluded, “during the preoperative evaluation, physicians should explicitly elicit and document a history of herbal medication use. Physicians should be familiar with the potential perioperative effects of the commonly used herbal medications to prevent, recognize, and treat potentially serious problems associated with their use and discontinuation.”
However, it is quite clear that the numbers of herbs that patients can encounter seem almost limitless, and there is no way for any clinician to maintain currency with every potential toxicity or other adverse event. Because of the phenomenon of new herbs becoming popular almost on a monthly basis, the use of textbooks to assist the hospital clinician in identifying potentially toxic herbs or drug–herb interactions has limited utility.
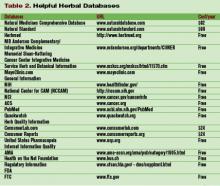
For the most part, databases that maintain greater currency of such reports are most helpful. Some of this information can be found in nonproprietary sites (see “Table 2. Helpful Herbal Databases,” to right), whereas others require a subscription. In the latter category, Natural Medicines Comprehensive Database (www.naturaldatabase.com) is a helpful and extremely comprehensive resource. It is laid out in a systematic fashion that makes it easy to identify an herb of interest, discover if there are potential adverse effects, and also provide patient handout information to patients.
Future Directions
Some of the bloom is off the rose in terms of enthusiasm for dietary supplements and herbs as a panacea for all human ills. Increasingly, consumers are becoming savvy with regard to challenges related to quality of products including contamination and lack of standardization. In addition, the common mythologies that “herbs are natural and therefore safe” or that “if two doses of an herb are good, 10 must be better” are slowly becoming recognized as the dangerous platitudes that they are. A more rationale approach to herbal use is slowly emerging.
With a more informed public and better resources for physicians to counsel patients and consumers, it is possible that we will see beneficial dietary supplements and herbs assume a helpful role in managing common problems. For example, valerian may be of significant benefit in helping restructure sleep patterns in patients with insomnia (possibly with fewer side effects than benzodiazepines and less expense than some of the newer hypnotics). Still, long-term studies are generally lacking, so final determination of the role of valerian in the physician’s armamentarium await such studies.
At the Mayo Clinic, many such studies are under way. The use of valerian as a sleep aid for patients undergoing chemotherapy is nearing completion. Another study looking at the role of American ginseng (Panax quinquefolius) as a treatment for cancer-related fatigue has just gotten under way. As these and dozens of similar studies at research institutions across the country are completed, the missing pieces in the herb story will begin to be filled in.
Until all the answers are in, clinicians need to remember that herbs are popular and will probably be part of our healthcare system for the foreseeable future. Although many herbs have promising data to suggest we may welcome them into our repertoire of agents, the focus in the hospital (for now) must be to make sure our patients do not suffer harm from such agents. By working with them in a collaborative partnership and sharing the data we do have at hand, we can ensure that our patients have the information they need to make informed decisions about their decision to use (or not to use) herbs. TH
Brent Bauer, MD, is consultant director for the Complementary and Alternative Medicine Program, Mayo Clinic Rochester.
References
- Barnes P, Powell-Griner E, McFann K, et al. CDC Advance Data Report #343. Complementary and alternative medicine use among adults: United States, 2002; May 27, 2004.
- Hsiao AF, Wong MD, Kanouse DE, et al. Complementary and alternative medicine use and substitution for conventional therapy by HIV-infected patients. J Acquir Immune Defic Syndr. 2003;33:157-165.
- Yeh GY, Eisenberg DM, Davis RB, et al. Use of complementary and alternative medicine among persons with diabetes mellitus: results of a national survey. Am J Public Health. 2002;92:1648-1652.
- Wood MJ, Stewart RL, Merry H, et al. Use of complementary and alternative medical therapies in patients with cardiovascular disease. Am Heart J. 2003;145:806-812.
- Liu EH, Turner LM, Lin SX, et al. Use of alternative medicine by patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2000;120:335-341.
- Richardson MA, Sanders T, Palmer JL, et al. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505-2514.
- Gulla J, Singer AJ. Use of alternative therapies among emergency department patients. Ann Emerg Med. 2000;35:226-228.
- Kaye AD, Clarke RC, Sabar R, et al. Herbal medicines: current trends in anesthesiology practice—a hospital survey. J Clin Anesth. 2000;12:468-471.
- Lin YC, Bioteau AB, Ferrari LR, et al. The use of herbs and complementary and alternative medicine in pediatric preoperative patients. J Clin Anesth. 2004;16:4-6.
- Huber R, Koch D, Beiser I, et al. Experience and attitudes towards CAM—a survey of internal and psychosomatic patients in a German university hospital. Altern Ther Health Med. 2004;10:32-36.
- Valencia Orgaz O, Orts Castro A, Castells Armenter MV, et al. Assessing preoperative use of medicinal plants during preanesthetic interviews. Rev Esp Anestesiol Reanim. 2005;52:453-458. Spanish.
- Critchley LA, Chen DQ, Lee A, et al. A survey of Chinese herbal medicine intake amongst preoperative patients in Hong Kong. Anaesth Intensive Care. 2005;33:506-513.
- Grauer RP, Thomas RD, Tronson MD, et al. Preoperative use of herbal medicines and vitamin supplements. Anaesth Intensive Care. 2004;32:173-177.
- Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA. 2001;286:208-216.
In 2002, the NIH surveyed more than 30,000 U.S. adults regarding their use of complementary and alternative medicine (CAM).1 This survey revealed that approximately 40% of U.S. adults had used some form of CAM in the past year. When one excludes prayer as a CAM modality, the most common modality used was the category of natural products (i.e., herbs and dietary supplements).
This has significant implications for all healthcare providers, but especially for those who practice in the hospital environment. Herbs can be potentially toxic in their own right and can cause drug-herb interactions as well. Such adverse effects may be particularly important in hospitalized patients undergoing surgery or who are acutely ill and exposed to a number of narrow-window therapeutic pharmaceuticals. Thus, it is imperative for hospital physicians to have a basic understanding of some of the risks, challenges, and potential benefits of herbs.
Use of Herbs by Hospitalized Patients
Surveys performed in the United States and around the world consistently demonstrate that the use of dietary supplements and herbs tends to be higher (as is all CAM usage) in individuals with chronic or incurable diseases. This is especially true for conditions such as HIV, diabetes, heart disease, and cancer.2–6 Thus, considering the complexity of illness of most hospitalized patients, it should not be surprising that use of herbs and dietary supplements is high in the hospital population. This has been borne out in several national and international studies.
A study reported in the Annals of Emergency Medicine in 2000 found that 56% of ED patients had tried alternative therapies in the past.7 The most frequently tried alternative therapies were massage therapy (31%), chiropractic (30%), and herbs (24%). Interestingly, 70% of the respondents who had tried these alternative therapies did not inform their physicians, highlighting a challenge for physicians and caregivers in the hospital setting.
Kay and colleagues reported 1,017 patients presenting for a preanesthetic evaluation prior to surgery.8 They found that 482 of 755 (64%) of patients had used at least one natural product. The majority of these were vitamin users, but several herbs with potential importance in the hospital setting were used as well: garlic extract (43%), ginkgo (32%), St. John’s wort (30%), ephedra (18%), and echinacea (12%).
Pediatric patients are not immune to the use of herbs and dietary supplement either. A survey at Children’s Hospital in Boston looked at 1,100 patients younger than 18 during their preoperative visit.9 A total of 1,021 surveys were completed and, of these, 30% patients indicated that they had tried one or more complementary and alternative therapies in the past year before surgery. Importantly, 13% had used herbal remedies before surgery.
Finally, international studies confirm similar usage patterns in adult hospital patients in Germany, Spain, Hong Kong, and Australia.10–13 Thus, it appears well established that the use of dietary supplements has become a fixed part of conventional healthcare. Recognizing that a significant percentage of patients under our care are using herbs is the first step in bringing critically needed information and guidance to our patients.
Herb Toxicity and Herb–Drug Interactions
There are many well-recognized herbal toxicities and/or drug-herb interactions with which all clinicians should have some degree of familiarity. For example, St. John’s wort stimulation of the cytochrome P450 enzyme system resulting in enhanced metabolism of several pharmaceutical drugs has been well reported. Ephedra’s ability to induce elevated blood pressure, stroke, and MI also received a great deal of publicity. (Note: Ephedra sales were banned by the FDA in 2004. However the prohibition excluded ephedra-containing teas, and—despite the ban—many internet sites still have ephedra available for purchase. Thus, be aware that your patients may still have access to ephedra.)
Which herbs might have specific importance in the hospital setting? This question was answered to some degree by researchers at the University of Chicago in 2001.14 The authors reviewed the literature on commonly used herbal medications in the context of the perioperative period and attempted to provide rationale strategies for managing their preoperative use. They identified echinacea, ephedra, garlic, ginkgo, ginseng, kava, St. John’s wort, and valerian as commonly used herbal medications that could pose a concern during the perioperative period.
Direct effects include bleeding from garlic, ginkgo, and ginseng; cardiovascular instability from ephedra; and hypoglycemia from ginseng. Pharmacodynamic herb-drug interactions include potentiation of the sedative effects of anesthetic by kava and valerian. Pharmacokinetic herb-drug interactions include increased metabolism of many drugs used in the perioperative period by St. John’s wort. (The findings are outlined in “Table 1. Clinically Important Effects and Perioperative Concerns of Eight Herbal Medicines and Recommendations for Discontinuation of Use Before Surgery,” p. 16.)
These authors concluded, “during the preoperative evaluation, physicians should explicitly elicit and document a history of herbal medication use. Physicians should be familiar with the potential perioperative effects of the commonly used herbal medications to prevent, recognize, and treat potentially serious problems associated with their use and discontinuation.”
However, it is quite clear that the numbers of herbs that patients can encounter seem almost limitless, and there is no way for any clinician to maintain currency with every potential toxicity or other adverse event. Because of the phenomenon of new herbs becoming popular almost on a monthly basis, the use of textbooks to assist the hospital clinician in identifying potentially toxic herbs or drug–herb interactions has limited utility.
For the most part, databases that maintain greater currency of such reports are most helpful. Some of this information can be found in nonproprietary sites (see “Table 2. Helpful Herbal Databases,” to right), whereas others require a subscription. In the latter category, Natural Medicines Comprehensive Database (www.naturaldatabase.com) is a helpful and extremely comprehensive resource. It is laid out in a systematic fashion that makes it easy to identify an herb of interest, discover if there are potential adverse effects, and also provide patient handout information to patients.
Future Directions
Some of the bloom is off the rose in terms of enthusiasm for dietary supplements and herbs as a panacea for all human ills. Increasingly, consumers are becoming savvy with regard to challenges related to quality of products including contamination and lack of standardization. In addition, the common mythologies that “herbs are natural and therefore safe” or that “if two doses of an herb are good, 10 must be better” are slowly becoming recognized as the dangerous platitudes that they are. A more rationale approach to herbal use is slowly emerging.
With a more informed public and better resources for physicians to counsel patients and consumers, it is possible that we will see beneficial dietary supplements and herbs assume a helpful role in managing common problems. For example, valerian may be of significant benefit in helping restructure sleep patterns in patients with insomnia (possibly with fewer side effects than benzodiazepines and less expense than some of the newer hypnotics). Still, long-term studies are generally lacking, so final determination of the role of valerian in the physician’s armamentarium await such studies.
At the Mayo Clinic, many such studies are under way. The use of valerian as a sleep aid for patients undergoing chemotherapy is nearing completion. Another study looking at the role of American ginseng (Panax quinquefolius) as a treatment for cancer-related fatigue has just gotten under way. As these and dozens of similar studies at research institutions across the country are completed, the missing pieces in the herb story will begin to be filled in.
Until all the answers are in, clinicians need to remember that herbs are popular and will probably be part of our healthcare system for the foreseeable future. Although many herbs have promising data to suggest we may welcome them into our repertoire of agents, the focus in the hospital (for now) must be to make sure our patients do not suffer harm from such agents. By working with them in a collaborative partnership and sharing the data we do have at hand, we can ensure that our patients have the information they need to make informed decisions about their decision to use (or not to use) herbs. TH
Brent Bauer, MD, is consultant director for the Complementary and Alternative Medicine Program, Mayo Clinic Rochester.
References
- Barnes P, Powell-Griner E, McFann K, et al. CDC Advance Data Report #343. Complementary and alternative medicine use among adults: United States, 2002; May 27, 2004.
- Hsiao AF, Wong MD, Kanouse DE, et al. Complementary and alternative medicine use and substitution for conventional therapy by HIV-infected patients. J Acquir Immune Defic Syndr. 2003;33:157-165.
- Yeh GY, Eisenberg DM, Davis RB, et al. Use of complementary and alternative medicine among persons with diabetes mellitus: results of a national survey. Am J Public Health. 2002;92:1648-1652.
- Wood MJ, Stewart RL, Merry H, et al. Use of complementary and alternative medical therapies in patients with cardiovascular disease. Am Heart J. 2003;145:806-812.
- Liu EH, Turner LM, Lin SX, et al. Use of alternative medicine by patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2000;120:335-341.
- Richardson MA, Sanders T, Palmer JL, et al. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505-2514.
- Gulla J, Singer AJ. Use of alternative therapies among emergency department patients. Ann Emerg Med. 2000;35:226-228.
- Kaye AD, Clarke RC, Sabar R, et al. Herbal medicines: current trends in anesthesiology practice—a hospital survey. J Clin Anesth. 2000;12:468-471.
- Lin YC, Bioteau AB, Ferrari LR, et al. The use of herbs and complementary and alternative medicine in pediatric preoperative patients. J Clin Anesth. 2004;16:4-6.
- Huber R, Koch D, Beiser I, et al. Experience and attitudes towards CAM—a survey of internal and psychosomatic patients in a German university hospital. Altern Ther Health Med. 2004;10:32-36.
- Valencia Orgaz O, Orts Castro A, Castells Armenter MV, et al. Assessing preoperative use of medicinal plants during preanesthetic interviews. Rev Esp Anestesiol Reanim. 2005;52:453-458. Spanish.
- Critchley LA, Chen DQ, Lee A, et al. A survey of Chinese herbal medicine intake amongst preoperative patients in Hong Kong. Anaesth Intensive Care. 2005;33:506-513.
- Grauer RP, Thomas RD, Tronson MD, et al. Preoperative use of herbal medicines and vitamin supplements. Anaesth Intensive Care. 2004;32:173-177.
- Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA. 2001;286:208-216.
In 2002, the NIH surveyed more than 30,000 U.S. adults regarding their use of complementary and alternative medicine (CAM).1 This survey revealed that approximately 40% of U.S. adults had used some form of CAM in the past year. When one excludes prayer as a CAM modality, the most common modality used was the category of natural products (i.e., herbs and dietary supplements).
This has significant implications for all healthcare providers, but especially for those who practice in the hospital environment. Herbs can be potentially toxic in their own right and can cause drug-herb interactions as well. Such adverse effects may be particularly important in hospitalized patients undergoing surgery or who are acutely ill and exposed to a number of narrow-window therapeutic pharmaceuticals. Thus, it is imperative for hospital physicians to have a basic understanding of some of the risks, challenges, and potential benefits of herbs.
Use of Herbs by Hospitalized Patients
Surveys performed in the United States and around the world consistently demonstrate that the use of dietary supplements and herbs tends to be higher (as is all CAM usage) in individuals with chronic or incurable diseases. This is especially true for conditions such as HIV, diabetes, heart disease, and cancer.2–6 Thus, considering the complexity of illness of most hospitalized patients, it should not be surprising that use of herbs and dietary supplements is high in the hospital population. This has been borne out in several national and international studies.
A study reported in the Annals of Emergency Medicine in 2000 found that 56% of ED patients had tried alternative therapies in the past.7 The most frequently tried alternative therapies were massage therapy (31%), chiropractic (30%), and herbs (24%). Interestingly, 70% of the respondents who had tried these alternative therapies did not inform their physicians, highlighting a challenge for physicians and caregivers in the hospital setting.
Kay and colleagues reported 1,017 patients presenting for a preanesthetic evaluation prior to surgery.8 They found that 482 of 755 (64%) of patients had used at least one natural product. The majority of these were vitamin users, but several herbs with potential importance in the hospital setting were used as well: garlic extract (43%), ginkgo (32%), St. John’s wort (30%), ephedra (18%), and echinacea (12%).
Pediatric patients are not immune to the use of herbs and dietary supplement either. A survey at Children’s Hospital in Boston looked at 1,100 patients younger than 18 during their preoperative visit.9 A total of 1,021 surveys were completed and, of these, 30% patients indicated that they had tried one or more complementary and alternative therapies in the past year before surgery. Importantly, 13% had used herbal remedies before surgery.
Finally, international studies confirm similar usage patterns in adult hospital patients in Germany, Spain, Hong Kong, and Australia.10–13 Thus, it appears well established that the use of dietary supplements has become a fixed part of conventional healthcare. Recognizing that a significant percentage of patients under our care are using herbs is the first step in bringing critically needed information and guidance to our patients.
Herb Toxicity and Herb–Drug Interactions
There are many well-recognized herbal toxicities and/or drug-herb interactions with which all clinicians should have some degree of familiarity. For example, St. John’s wort stimulation of the cytochrome P450 enzyme system resulting in enhanced metabolism of several pharmaceutical drugs has been well reported. Ephedra’s ability to induce elevated blood pressure, stroke, and MI also received a great deal of publicity. (Note: Ephedra sales were banned by the FDA in 2004. However the prohibition excluded ephedra-containing teas, and—despite the ban—many internet sites still have ephedra available for purchase. Thus, be aware that your patients may still have access to ephedra.)
Which herbs might have specific importance in the hospital setting? This question was answered to some degree by researchers at the University of Chicago in 2001.14 The authors reviewed the literature on commonly used herbal medications in the context of the perioperative period and attempted to provide rationale strategies for managing their preoperative use. They identified echinacea, ephedra, garlic, ginkgo, ginseng, kava, St. John’s wort, and valerian as commonly used herbal medications that could pose a concern during the perioperative period.
Direct effects include bleeding from garlic, ginkgo, and ginseng; cardiovascular instability from ephedra; and hypoglycemia from ginseng. Pharmacodynamic herb-drug interactions include potentiation of the sedative effects of anesthetic by kava and valerian. Pharmacokinetic herb-drug interactions include increased metabolism of many drugs used in the perioperative period by St. John’s wort. (The findings are outlined in “Table 1. Clinically Important Effects and Perioperative Concerns of Eight Herbal Medicines and Recommendations for Discontinuation of Use Before Surgery,” p. 16.)
These authors concluded, “during the preoperative evaluation, physicians should explicitly elicit and document a history of herbal medication use. Physicians should be familiar with the potential perioperative effects of the commonly used herbal medications to prevent, recognize, and treat potentially serious problems associated with their use and discontinuation.”
However, it is quite clear that the numbers of herbs that patients can encounter seem almost limitless, and there is no way for any clinician to maintain currency with every potential toxicity or other adverse event. Because of the phenomenon of new herbs becoming popular almost on a monthly basis, the use of textbooks to assist the hospital clinician in identifying potentially toxic herbs or drug–herb interactions has limited utility.
For the most part, databases that maintain greater currency of such reports are most helpful. Some of this information can be found in nonproprietary sites (see “Table 2. Helpful Herbal Databases,” to right), whereas others require a subscription. In the latter category, Natural Medicines Comprehensive Database (www.naturaldatabase.com) is a helpful and extremely comprehensive resource. It is laid out in a systematic fashion that makes it easy to identify an herb of interest, discover if there are potential adverse effects, and also provide patient handout information to patients.
Future Directions
Some of the bloom is off the rose in terms of enthusiasm for dietary supplements and herbs as a panacea for all human ills. Increasingly, consumers are becoming savvy with regard to challenges related to quality of products including contamination and lack of standardization. In addition, the common mythologies that “herbs are natural and therefore safe” or that “if two doses of an herb are good, 10 must be better” are slowly becoming recognized as the dangerous platitudes that they are. A more rationale approach to herbal use is slowly emerging.
With a more informed public and better resources for physicians to counsel patients and consumers, it is possible that we will see beneficial dietary supplements and herbs assume a helpful role in managing common problems. For example, valerian may be of significant benefit in helping restructure sleep patterns in patients with insomnia (possibly with fewer side effects than benzodiazepines and less expense than some of the newer hypnotics). Still, long-term studies are generally lacking, so final determination of the role of valerian in the physician’s armamentarium await such studies.
At the Mayo Clinic, many such studies are under way. The use of valerian as a sleep aid for patients undergoing chemotherapy is nearing completion. Another study looking at the role of American ginseng (Panax quinquefolius) as a treatment for cancer-related fatigue has just gotten under way. As these and dozens of similar studies at research institutions across the country are completed, the missing pieces in the herb story will begin to be filled in.
Until all the answers are in, clinicians need to remember that herbs are popular and will probably be part of our healthcare system for the foreseeable future. Although many herbs have promising data to suggest we may welcome them into our repertoire of agents, the focus in the hospital (for now) must be to make sure our patients do not suffer harm from such agents. By working with them in a collaborative partnership and sharing the data we do have at hand, we can ensure that our patients have the information they need to make informed decisions about their decision to use (or not to use) herbs. TH
Brent Bauer, MD, is consultant director for the Complementary and Alternative Medicine Program, Mayo Clinic Rochester.
References
- Barnes P, Powell-Griner E, McFann K, et al. CDC Advance Data Report #343. Complementary and alternative medicine use among adults: United States, 2002; May 27, 2004.
- Hsiao AF, Wong MD, Kanouse DE, et al. Complementary and alternative medicine use and substitution for conventional therapy by HIV-infected patients. J Acquir Immune Defic Syndr. 2003;33:157-165.
- Yeh GY, Eisenberg DM, Davis RB, et al. Use of complementary and alternative medicine among persons with diabetes mellitus: results of a national survey. Am J Public Health. 2002;92:1648-1652.
- Wood MJ, Stewart RL, Merry H, et al. Use of complementary and alternative medical therapies in patients with cardiovascular disease. Am Heart J. 2003;145:806-812.
- Liu EH, Turner LM, Lin SX, et al. Use of alternative medicine by patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2000;120:335-341.
- Richardson MA, Sanders T, Palmer JL, et al. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505-2514.
- Gulla J, Singer AJ. Use of alternative therapies among emergency department patients. Ann Emerg Med. 2000;35:226-228.
- Kaye AD, Clarke RC, Sabar R, et al. Herbal medicines: current trends in anesthesiology practice—a hospital survey. J Clin Anesth. 2000;12:468-471.
- Lin YC, Bioteau AB, Ferrari LR, et al. The use of herbs and complementary and alternative medicine in pediatric preoperative patients. J Clin Anesth. 2004;16:4-6.
- Huber R, Koch D, Beiser I, et al. Experience and attitudes towards CAM—a survey of internal and psychosomatic patients in a German university hospital. Altern Ther Health Med. 2004;10:32-36.
- Valencia Orgaz O, Orts Castro A, Castells Armenter MV, et al. Assessing preoperative use of medicinal plants during preanesthetic interviews. Rev Esp Anestesiol Reanim. 2005;52:453-458. Spanish.
- Critchley LA, Chen DQ, Lee A, et al. A survey of Chinese herbal medicine intake amongst preoperative patients in Hong Kong. Anaesth Intensive Care. 2005;33:506-513.
- Grauer RP, Thomas RD, Tronson MD, et al. Preoperative use of herbal medicines and vitamin supplements. Anaesth Intensive Care. 2004;32:173-177.
- Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA. 2001;286:208-216.