User login
Immigrant with stomach pain, distension, nausea, and fever • Dx?
THE CASE
A 34-year-old Eritrean man presented to the emergency department with complaints of diffuse abdominal pain and distention. He had emigrated to the United States 3 months earlier, following 5 years in a refugee camp in Ethiopia. Two weeks earlier, the patient sought care at his primary care clinic and was diagnosed with post-operative urinary retention and constipation following a recent hemorrhoidectomy. A Foley catheter was inserted and provided a short period of relief.
Following the visit, however, his abdominal pain worsened. He also experienced increasing abdominal distention, a declining appetite, and persistent nausea. The patient said that he was unable to urinate and had not had a bowel movement in 6 days. He also described fevers, drenching night sweats, chills, and a 4-kg weight loss over 2 months.
On physical examination, the patient had a wasted appearance. He was afebrile, alert, and oriented, but anxious and writhing in pain. An abdominal examination revealed some distention, generalized guarding, and tenderness. There was dullness to percussion in all regions without rebound, and no caput medusa was noted. The remainder of the physical examination was unremarkable.
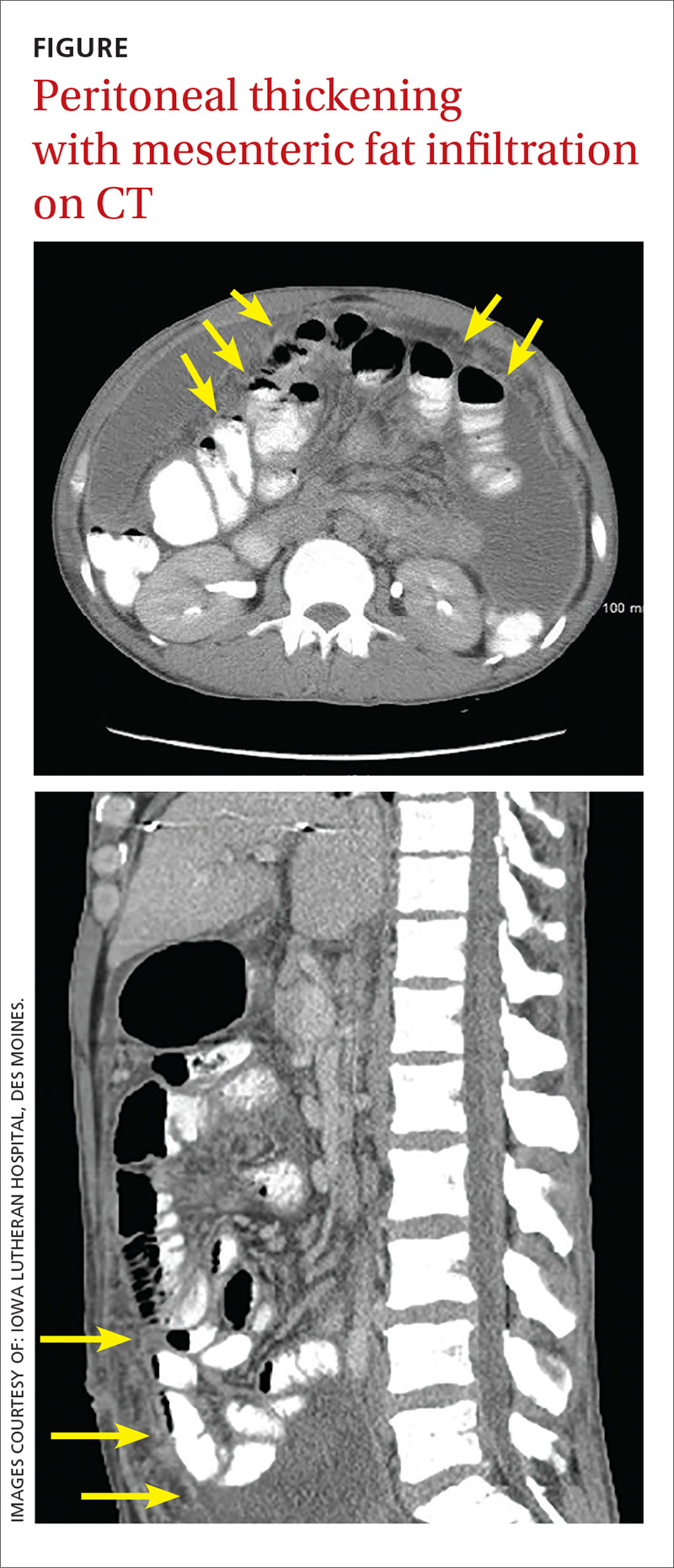
Pertinent laboratory values included negative screens for human immunodeficiency virus (HIV) 1 and 2, and a purified protein derivative test that produced 10 mm of induration at 48 hours. An interferon-gamma release assay was not performed following these results. A computerized tomography (CT) scan of the abdomen and pelvis with intravenous and oral contrast revealed thickening of the peritoneal lining with infiltration of the mesenteric fat and large loculated fluid collections in the abdominal cavity (FIGURE). A CT scan of the patient’s lungs showed some mild atelectasis with left-sided effusion.
After hospital admission, the patient spiked fevers as high as 103.3° F and developed progressively worsening ascites. An ultrasound-guided paracentesis was performed, during which almost 2 liters of yellow, hazy fluid was removed. Fluid and blood cultures were negative.
THE DIAGNOSIS
With a high clinical suspicion for tuberculosis (TB) peritonitis, we requested a surgical consultation and a peritoneal biopsy was performed. The patient was started on ethambutol, isoniazid, pyrazinamide, pyridoxine, and rifampin while the biopsy results were pending.
Pathology subsequently confirmed a diagnosis of TB peritonitis, reporting dense fibroconnective tissue with areas of chronic inflammation and occasional accumulations of histiocytes with multinucleated giant cells showing granulomatous inflammation. An acid-fast (AF) bacilli stain for Mycobacteria showed a single curved bacillus compatible with Mycobacterium tuberculosis.
The patient was discharged following a 3-week hospital stay. At his follow-up visit several weeks later, the patient reported marked improvement and increasing exercise tolerance. He had gained weight, and the abdominal distention and tenderness had resolved.
DISCUSSION
Worldwide, TB is one of the top 10 causes of death. The World Health Organization estimates that there were 1.4 million TB deaths globally in 2015.1 And while rates of TB are decreasing in the United States, there was a resurgence from 1985 to 1992.2 This was attributable to the HIV/acquired immunodeficiency syndrome epidemic, increased immigration from countries endemic for TB, and deterioration of the TB public health infrastructure.3
Transmission. M tuberculosis is a rod-shaped, nonspore-forming AF bacillus that typically infects the lungs, but may infect other areas of the body. Transmission typically occurs via airborne spread of droplets from an infected individual. Possible other methods of disease dissemination include ingestion of infected sputum, hematogenous spread from active pulmonary TB, or ingestion of contaminated milk or food.
M tuberculosis elicits a proinflammatory phase, which facilitates the formation of a granuloma within the host tissues. The host’s immune response to M tuberculosis plays a role in the risk of developing this type of TB.3
TB presentation is classified as pulmonary, extrapulmonary, or both. Clinicians are generally attentive to the classic symptoms of pulmonary TB: cough, weight loss, night sweats, and fever. Presentation of extrapulmonary TB, however, may vary.4
According to one study, the most common presenting symptoms for peritoneal TB are weight loss, abdominal pain, and/or fever, all of which our patient experienced.5 In addition, our patient was an immigrant from Africa, and black patients have been shown to have a significantly higher incidence of extrapulmonary TB than their nonblack counterparts.6 Although our patient was HIV-negative, a recent meta-analysis confirmed the strong association between extrapulmonary TB and HIV, emphasizing the importance of including HIV screens in the standard work-up for TB.7
Other symptoms may include microcytosis, anemia, thrombocytosis, and an elevated erythrocyte sedimentation rate. Although a chest x-ray is often negative, advanced imaging, such as CT or magnetic resonance imaging, is often abnormal and may point to the diagnosis.5
Treatment of extrapulmonary TB is generally the same as that for pulmonary TB and, interestingly, the incidence of multi-drug resistant extrapulmonary TB is not necessarily higher than it is for pulmonary TB (<1% vs 1.6%).3,7 In light of this, a standard regimen—like the one our patient received—is generally utilized for 6 to 9 months. Nonetheless, resistance testing should still be performed.3,4
THE TAKEAWAY
While considered uncommon, more than 20% of TB cases in the United States are extrapulmonary (the most common form is TB lymphadenitis).7,8 It is imperative to identify appropriate risk factors, including associated comorbidities, patient characteristics, and population/endemic differences in immigrant populations.
In this case, although the symptom combination of persistent abdominal pain, fever, and weight loss may not trigger suspicion of a TB diagnosis in isolation, combining the symptoms with knowledge of the patient’s immigration status should at least raise an eyebrow. Given their nonpulmonary symptoms, many of these patients will not present to pulmonologists, making diagnosis particularly relevant to primary care.
1. World Health Organization. Global tuberculosis report 2016. Available at: http://www.who.int/tb/publications/global_report/gtbr2016_executive_summary.pdf?ua=1. Accessed August 22, 2017.
2. Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350-1357.
3. Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2006. Available at: http://digitallibrary.utah.gov/awweb/awarchive?type=file&item=56908. Accessed August 3, 2017.
4. World Health Organization. Global tuberculosis report 2012. Available at: http://apps.who.int/medicinedocs/documents/s19908en/s19908en.pdf. Accessed July 27, 2017.
5. Ramesh J, Banait GS, Ormerod LP. Abdominal tuberculosis in a district general hospital: a retrospective review of 86 cases. QJM. 2008;101:189-195.
6. Fiske CT, Griffin MR, Erin H, et al. Black race, sex and extrapulmonary tuberculosis risk: an observational study. BMC Infect Dis. 2010;10:16.
7. Naing C, Mak JW, Maung M, et al. Meta-analysis: the association between HIV infection and extrapulmonary tuberculosis. Lung. 2013;191:27-34.
8. Neelakantan S, Nair PP, Emmanuel RV, et al. Diversities in presentations of extrapulmonary tuberculosis. BMJ Case Rep. 2013.
THE CASE
A 34-year-old Eritrean man presented to the emergency department with complaints of diffuse abdominal pain and distention. He had emigrated to the United States 3 months earlier, following 5 years in a refugee camp in Ethiopia. Two weeks earlier, the patient sought care at his primary care clinic and was diagnosed with post-operative urinary retention and constipation following a recent hemorrhoidectomy. A Foley catheter was inserted and provided a short period of relief.
Following the visit, however, his abdominal pain worsened. He also experienced increasing abdominal distention, a declining appetite, and persistent nausea. The patient said that he was unable to urinate and had not had a bowel movement in 6 days. He also described fevers, drenching night sweats, chills, and a 4-kg weight loss over 2 months.
On physical examination, the patient had a wasted appearance. He was afebrile, alert, and oriented, but anxious and writhing in pain. An abdominal examination revealed some distention, generalized guarding, and tenderness. There was dullness to percussion in all regions without rebound, and no caput medusa was noted. The remainder of the physical examination was unremarkable.
Pertinent laboratory values included negative screens for human immunodeficiency virus (HIV) 1 and 2, and a purified protein derivative test that produced 10 mm of induration at 48 hours. An interferon-gamma release assay was not performed following these results. A computerized tomography (CT) scan of the abdomen and pelvis with intravenous and oral contrast revealed thickening of the peritoneal lining with infiltration of the mesenteric fat and large loculated fluid collections in the abdominal cavity (FIGURE). A CT scan of the patient’s lungs showed some mild atelectasis with left-sided effusion.
After hospital admission, the patient spiked fevers as high as 103.3° F and developed progressively worsening ascites. An ultrasound-guided paracentesis was performed, during which almost 2 liters of yellow, hazy fluid was removed. Fluid and blood cultures were negative.
THE DIAGNOSIS
With a high clinical suspicion for tuberculosis (TB) peritonitis, we requested a surgical consultation and a peritoneal biopsy was performed. The patient was started on ethambutol, isoniazid, pyrazinamide, pyridoxine, and rifampin while the biopsy results were pending.
Pathology subsequently confirmed a diagnosis of TB peritonitis, reporting dense fibroconnective tissue with areas of chronic inflammation and occasional accumulations of histiocytes with multinucleated giant cells showing granulomatous inflammation. An acid-fast (AF) bacilli stain for Mycobacteria showed a single curved bacillus compatible with Mycobacterium tuberculosis.
The patient was discharged following a 3-week hospital stay. At his follow-up visit several weeks later, the patient reported marked improvement and increasing exercise tolerance. He had gained weight, and the abdominal distention and tenderness had resolved.
DISCUSSION
Worldwide, TB is one of the top 10 causes of death. The World Health Organization estimates that there were 1.4 million TB deaths globally in 2015.1 And while rates of TB are decreasing in the United States, there was a resurgence from 1985 to 1992.2 This was attributable to the HIV/acquired immunodeficiency syndrome epidemic, increased immigration from countries endemic for TB, and deterioration of the TB public health infrastructure.3
Transmission. M tuberculosis is a rod-shaped, nonspore-forming AF bacillus that typically infects the lungs, but may infect other areas of the body. Transmission typically occurs via airborne spread of droplets from an infected individual. Possible other methods of disease dissemination include ingestion of infected sputum, hematogenous spread from active pulmonary TB, or ingestion of contaminated milk or food.
M tuberculosis elicits a proinflammatory phase, which facilitates the formation of a granuloma within the host tissues. The host’s immune response to M tuberculosis plays a role in the risk of developing this type of TB.3
TB presentation is classified as pulmonary, extrapulmonary, or both. Clinicians are generally attentive to the classic symptoms of pulmonary TB: cough, weight loss, night sweats, and fever. Presentation of extrapulmonary TB, however, may vary.4
According to one study, the most common presenting symptoms for peritoneal TB are weight loss, abdominal pain, and/or fever, all of which our patient experienced.5 In addition, our patient was an immigrant from Africa, and black patients have been shown to have a significantly higher incidence of extrapulmonary TB than their nonblack counterparts.6 Although our patient was HIV-negative, a recent meta-analysis confirmed the strong association between extrapulmonary TB and HIV, emphasizing the importance of including HIV screens in the standard work-up for TB.7
Other symptoms may include microcytosis, anemia, thrombocytosis, and an elevated erythrocyte sedimentation rate. Although a chest x-ray is often negative, advanced imaging, such as CT or magnetic resonance imaging, is often abnormal and may point to the diagnosis.5
Treatment of extrapulmonary TB is generally the same as that for pulmonary TB and, interestingly, the incidence of multi-drug resistant extrapulmonary TB is not necessarily higher than it is for pulmonary TB (<1% vs 1.6%).3,7 In light of this, a standard regimen—like the one our patient received—is generally utilized for 6 to 9 months. Nonetheless, resistance testing should still be performed.3,4
THE TAKEAWAY
While considered uncommon, more than 20% of TB cases in the United States are extrapulmonary (the most common form is TB lymphadenitis).7,8 It is imperative to identify appropriate risk factors, including associated comorbidities, patient characteristics, and population/endemic differences in immigrant populations.
In this case, although the symptom combination of persistent abdominal pain, fever, and weight loss may not trigger suspicion of a TB diagnosis in isolation, combining the symptoms with knowledge of the patient’s immigration status should at least raise an eyebrow. Given their nonpulmonary symptoms, many of these patients will not present to pulmonologists, making diagnosis particularly relevant to primary care.
THE CASE
A 34-year-old Eritrean man presented to the emergency department with complaints of diffuse abdominal pain and distention. He had emigrated to the United States 3 months earlier, following 5 years in a refugee camp in Ethiopia. Two weeks earlier, the patient sought care at his primary care clinic and was diagnosed with post-operative urinary retention and constipation following a recent hemorrhoidectomy. A Foley catheter was inserted and provided a short period of relief.
Following the visit, however, his abdominal pain worsened. He also experienced increasing abdominal distention, a declining appetite, and persistent nausea. The patient said that he was unable to urinate and had not had a bowel movement in 6 days. He also described fevers, drenching night sweats, chills, and a 4-kg weight loss over 2 months.
On physical examination, the patient had a wasted appearance. He was afebrile, alert, and oriented, but anxious and writhing in pain. An abdominal examination revealed some distention, generalized guarding, and tenderness. There was dullness to percussion in all regions without rebound, and no caput medusa was noted. The remainder of the physical examination was unremarkable.
Pertinent laboratory values included negative screens for human immunodeficiency virus (HIV) 1 and 2, and a purified protein derivative test that produced 10 mm of induration at 48 hours. An interferon-gamma release assay was not performed following these results. A computerized tomography (CT) scan of the abdomen and pelvis with intravenous and oral contrast revealed thickening of the peritoneal lining with infiltration of the mesenteric fat and large loculated fluid collections in the abdominal cavity (FIGURE). A CT scan of the patient’s lungs showed some mild atelectasis with left-sided effusion.
After hospital admission, the patient spiked fevers as high as 103.3° F and developed progressively worsening ascites. An ultrasound-guided paracentesis was performed, during which almost 2 liters of yellow, hazy fluid was removed. Fluid and blood cultures were negative.
THE DIAGNOSIS
With a high clinical suspicion for tuberculosis (TB) peritonitis, we requested a surgical consultation and a peritoneal biopsy was performed. The patient was started on ethambutol, isoniazid, pyrazinamide, pyridoxine, and rifampin while the biopsy results were pending.
Pathology subsequently confirmed a diagnosis of TB peritonitis, reporting dense fibroconnective tissue with areas of chronic inflammation and occasional accumulations of histiocytes with multinucleated giant cells showing granulomatous inflammation. An acid-fast (AF) bacilli stain for Mycobacteria showed a single curved bacillus compatible with Mycobacterium tuberculosis.
The patient was discharged following a 3-week hospital stay. At his follow-up visit several weeks later, the patient reported marked improvement and increasing exercise tolerance. He had gained weight, and the abdominal distention and tenderness had resolved.
DISCUSSION
Worldwide, TB is one of the top 10 causes of death. The World Health Organization estimates that there were 1.4 million TB deaths globally in 2015.1 And while rates of TB are decreasing in the United States, there was a resurgence from 1985 to 1992.2 This was attributable to the HIV/acquired immunodeficiency syndrome epidemic, increased immigration from countries endemic for TB, and deterioration of the TB public health infrastructure.3
Transmission. M tuberculosis is a rod-shaped, nonspore-forming AF bacillus that typically infects the lungs, but may infect other areas of the body. Transmission typically occurs via airborne spread of droplets from an infected individual. Possible other methods of disease dissemination include ingestion of infected sputum, hematogenous spread from active pulmonary TB, or ingestion of contaminated milk or food.
M tuberculosis elicits a proinflammatory phase, which facilitates the formation of a granuloma within the host tissues. The host’s immune response to M tuberculosis plays a role in the risk of developing this type of TB.3
TB presentation is classified as pulmonary, extrapulmonary, or both. Clinicians are generally attentive to the classic symptoms of pulmonary TB: cough, weight loss, night sweats, and fever. Presentation of extrapulmonary TB, however, may vary.4
According to one study, the most common presenting symptoms for peritoneal TB are weight loss, abdominal pain, and/or fever, all of which our patient experienced.5 In addition, our patient was an immigrant from Africa, and black patients have been shown to have a significantly higher incidence of extrapulmonary TB than their nonblack counterparts.6 Although our patient was HIV-negative, a recent meta-analysis confirmed the strong association between extrapulmonary TB and HIV, emphasizing the importance of including HIV screens in the standard work-up for TB.7
Other symptoms may include microcytosis, anemia, thrombocytosis, and an elevated erythrocyte sedimentation rate. Although a chest x-ray is often negative, advanced imaging, such as CT or magnetic resonance imaging, is often abnormal and may point to the diagnosis.5
Treatment of extrapulmonary TB is generally the same as that for pulmonary TB and, interestingly, the incidence of multi-drug resistant extrapulmonary TB is not necessarily higher than it is for pulmonary TB (<1% vs 1.6%).3,7 In light of this, a standard regimen—like the one our patient received—is generally utilized for 6 to 9 months. Nonetheless, resistance testing should still be performed.3,4
THE TAKEAWAY
While considered uncommon, more than 20% of TB cases in the United States are extrapulmonary (the most common form is TB lymphadenitis).7,8 It is imperative to identify appropriate risk factors, including associated comorbidities, patient characteristics, and population/endemic differences in immigrant populations.
In this case, although the symptom combination of persistent abdominal pain, fever, and weight loss may not trigger suspicion of a TB diagnosis in isolation, combining the symptoms with knowledge of the patient’s immigration status should at least raise an eyebrow. Given their nonpulmonary symptoms, many of these patients will not present to pulmonologists, making diagnosis particularly relevant to primary care.
1. World Health Organization. Global tuberculosis report 2016. Available at: http://www.who.int/tb/publications/global_report/gtbr2016_executive_summary.pdf?ua=1. Accessed August 22, 2017.
2. Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350-1357.
3. Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2006. Available at: http://digitallibrary.utah.gov/awweb/awarchive?type=file&item=56908. Accessed August 3, 2017.
4. World Health Organization. Global tuberculosis report 2012. Available at: http://apps.who.int/medicinedocs/documents/s19908en/s19908en.pdf. Accessed July 27, 2017.
5. Ramesh J, Banait GS, Ormerod LP. Abdominal tuberculosis in a district general hospital: a retrospective review of 86 cases. QJM. 2008;101:189-195.
6. Fiske CT, Griffin MR, Erin H, et al. Black race, sex and extrapulmonary tuberculosis risk: an observational study. BMC Infect Dis. 2010;10:16.
7. Naing C, Mak JW, Maung M, et al. Meta-analysis: the association between HIV infection and extrapulmonary tuberculosis. Lung. 2013;191:27-34.
8. Neelakantan S, Nair PP, Emmanuel RV, et al. Diversities in presentations of extrapulmonary tuberculosis. BMJ Case Rep. 2013.
1. World Health Organization. Global tuberculosis report 2016. Available at: http://www.who.int/tb/publications/global_report/gtbr2016_executive_summary.pdf?ua=1. Accessed August 22, 2017.
2. Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350-1357.
3. Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2006. Available at: http://digitallibrary.utah.gov/awweb/awarchive?type=file&item=56908. Accessed August 3, 2017.
4. World Health Organization. Global tuberculosis report 2012. Available at: http://apps.who.int/medicinedocs/documents/s19908en/s19908en.pdf. Accessed July 27, 2017.
5. Ramesh J, Banait GS, Ormerod LP. Abdominal tuberculosis in a district general hospital: a retrospective review of 86 cases. QJM. 2008;101:189-195.
6. Fiske CT, Griffin MR, Erin H, et al. Black race, sex and extrapulmonary tuberculosis risk: an observational study. BMC Infect Dis. 2010;10:16.
7. Naing C, Mak JW, Maung M, et al. Meta-analysis: the association between HIV infection and extrapulmonary tuberculosis. Lung. 2013;191:27-34.
8. Neelakantan S, Nair PP, Emmanuel RV, et al. Diversities in presentations of extrapulmonary tuberculosis. BMJ Case Rep. 2013.