User login
Hypoglycemia in Hospitalized Patients / Varghese et al.
Glycemic control in the inpatient setting has received increasing attention in recent years, with the demonstration that appropriate blood glucose (BG) control prevents adverse events in both intensive care unit (ICU) and non‐ICU settings.1 Recent recommendations set target blood glucose levels near euglycemia for most hospitalized patients.1 Unfortunately, the risk of hypoglycemia increases with tighter glycemic control,2 and hypoglycemia may result in catastrophic events.35 Although hyperglycemia is associated with postoperative infection,6 and effective management decreases wound infections,7 few reports have detailed the hypoglycemia rates among surgical patients.8 Hypoglycemia rates on medical services are as high as 28%,9, 10 and efforts to achieve more normal BG levels in hospitalized patients have been associated with more hypoglycemia.11
We undertook a study of hypoglycemia in all adult hospitalized patients receiving hypoglycemic therapy at our institution. The purpose of this study was to determine the incidence, natural history, associations, and consequences of hypoglycemia in this broad inpatient population in order to have a baseline prior to introducing any formal hospital strategies to achieve the newer targets for glycemic control.
Research Design and Methods
Thomas Jefferson University Hospital (TJUH) is a 675‐bed acute care teaching institution in center‐city Philadelphia with more than 30,000 patient admissions each year. We undertook a prospective, consecutive medical record review from August 16, 2004, to November 15, 2004, of hospitalized patients who had experienced at least 1 hypoglycemic episode, defined as at least one blood glucose (BG) 60 mg/dL within 48 hours of administration of an antihyperglycemic agent in the hospital. The definition of hypoglycemia was consistent with our hospital policies and a compromise between the BG 70 mg/dL proposed by the American Diabetes Association (ADA) hypoglycemia workgroup12 and the BG 40 mg/dL used by authors studying glycemic control in the ICU.13, 14
Hypoglycemic episodes were identified by a daily electronic search of the online medication administration record (MAR) where nurses document all point‐of‐care (POC) BG values. Two of the authors (P.V. and V.G.) reviewed the medical record for each episode and excluded pediatric (<18 years), emergency department, and maternity patients. Intensive care, step‐down, and medical/surgical unit patients were all included if the hypoglycemia had occurred within 48 hours of hospital administration of an antihyperglycemic agent. All medication orders at TJUH are placed through the computerized prescriber order entry (CPOE) system (Centricity Enterprise), which links all antihyperglycemic agents to a standardized hypoglycemia treatment protocol. The protocol includes instructions to administer glucose and/or glucagon and check the BG 15 minutes after a hypoglycemic episode. We established operational definitions prior to chart review (Appendix). A symptomatic hypoglycemia‐related adverse event was defined as any documented event occurring at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased length of hospitalization. We did not include following our hypoglycemic protocol with the administration of 50% dextrose or glucagon as a change of care, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
We searched the University Health System Consortium Clinical Database (CDB) to quantify the number of patients at TJUH receiving any antihyperglycemic agent during the study period and to identify the specific agents received. The CDB receives all patient, physician, and pharmacy dose‐ specific information from the hospital clinical and billing information systems. We defined subgroups of patients taking insulin(s) only, taking oral agent(s) only, and taking a combination.
Differences between proportions were evaluated using the chi‐square statistic; differences between means were evaluated using the Student t test. Probabilities of the null hypothesis less than .05 were considered significant.
The project was approved by the Institutional Review Board for Human Subjects at Thomas Jefferson University.
RESULTS
Over the 2‐month study period 8140 patients were admitted, of whom 2174 (27%) received an antihyperglycemic agent. Five hundred and sixty‐eight hypoglycemic episodes (BG 60 mg/dL) occurred in 265 patients. We excluded 84 episodes among 59 patients who did not receive antihyperglycemic agents, resulting in 484 episodes of hypoglycemia occurring within 48 hours of hospital administration of an antihyperglycemic agent in 206 patients, an average of 5.26 episodes per day. Of the 2174 of patients receiving antihyperglycemic agents, 206 (9.5%) experienced 1 or more episodes of hypoglycemia.
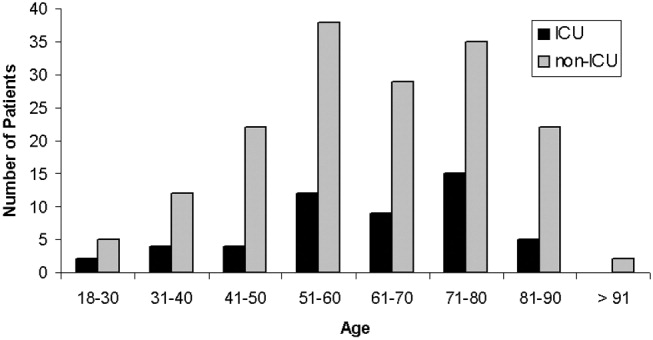
Patient ages ranged from 20 to 93 years, with an average of 62 years. Fifty‐seven percent (118 of 206) of participants were female. About one‐fourth of all episodes (23.8%) occurred in the ICU setting. The distribution of patients by decade and their ICU status are presented in Figure 1. Of the 206 patients, 29% (59) had type 1 diabetes mellitus (DM), 49% (102) had type 2 DM, 1% (2) had new‐onset diabetes, and 21% (43) had no diagnosis of DM. Of the 484 hypoglycemic episodes, 37.8% occurred in patients with type 1 DM, 46.9% in patients with type 2 DM, and 0.6% in patients with new‐onset DM. The remaining 14.5% occurred in patients with no documented history of DM, although they were receiving antihyperglycemic agents. More than 1 episode was experienced by 44% of patients, and 12% experienced 5 or more episodes.

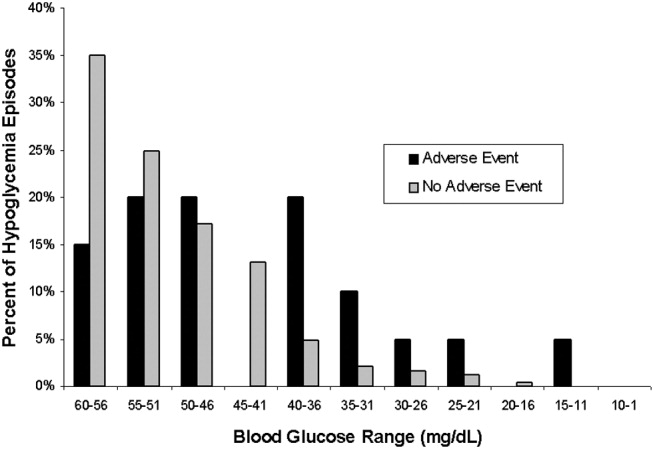
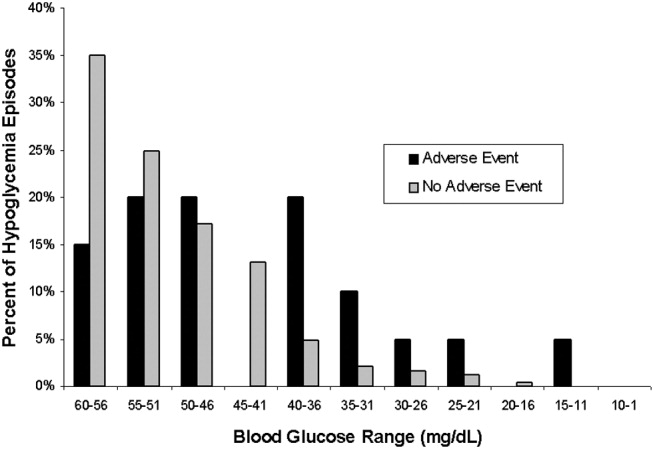
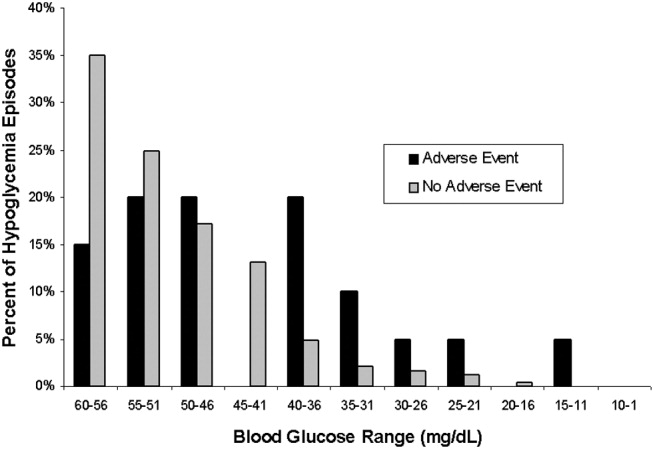
The BG was between 51 and 60 mg/dL in 282 of the episodes (58.2%), between 41 and 50 mg/dL in 149 episodes (30.8%) and 40 mg/dL or less in 53 episodes (11%). In 20 episodes (4.1% of episodes, representing fewer than 1% of all patients receiving an antihyperglycemic agent), a symptomatic hypoglycemia‐related adverse event was documented. All but 1 adverse event occurred outside the ICU. Ten of these events (2.1% of all hypoglycemic episodes) in 10 patients involved symptoms including headache, agitation, disorientation, and tremors. Of these patients 9 had type 1 DM, and 1 had type 2 DM. Six events (1.2% of hypoglycemic episodes) in 4 patients involved seizures. Two of these patients had type 1 DM, and 2 had type 2 DM. Four events (0.8% of hypoglycemic episodes) in 4 patients involved an unresponsive or unarousable state, including the sole ICU episode of symptomatic hypoglycemia. Three of these patients had type 1 DM, and 1 had type 2 DM. Patients with hypoglycemia‐related adverse events had a mean BG of 43.0 mg/dL, significantly lower (P = .01) than the mean BG of 50.9 mg/dL for hypoglycemic episodes without such events. However, 35% of these events occurred with a measured BG between 50 and 60 mg/dL. The distributions of BG values associated with symptomatic and asymptomatic events are shown in Figure 2. There is no useful threshold that separates symptomatic from asymptomatic hypoglycemia. No deaths or irreversible consequences were associated with hypoglycemia.
Approximately 40% (195 of 484) of the hypoglycemic episodes were related to decreased enteral intake (Table 1). In addition, 6.1% (30 of 484) of hypoglycemic episodes were related to insulin adjustment and 0.4% (2 of 484) to steroid withdrawal. In 43% (209 of 484) of the episodes the cause of the hypoglycemia was unclear. The remaining 10.4% of episodes were attributed to diverse causes.
| N (%) | |
|---|---|
| |
| NPO for unknown reason | 30 (6.2) |
| NPO for procedure/emntubated | 29 (6) |
| NPO for other documented reason (ie, fever/sepsis) | 10 (2.1) |
| Decreased PO intake (includes missed meal) | 126 (26) |
| No change in PO intake | 289 (59.7) |
One third of patients had a documented BG rechecked within 60 minutes, and fewer than half of the hypoglycemic patients had documented euglycemia within 2 hours of their low blood glucose measurement. The average time to documented resolution of a hypoglycemic episode was 4 hours, 3 minutes, with a median of 2 hours, 25 minutes.
Table 2 delineates the various combinations of antihyperglycemic agents that the 206 patients received in the 48 hours prior to a hypoglycemic episode. Of the 484 hypoglycemic episodes, 362 involved insulin. Of patients receiving insulin, 38 of 362 of episodes of hypoglycemia occurred in patients receiving sliding‐scale insulin (SSI) dosing as the only insulin order. In 163 hypoglycemic episodes, insulin was dosed with a combination of SSI and infusion or SSI with daily long‐acting insulin. The remaining 161 episodes involved administration of insulin to patients without an accompanying sliding‐scale order.
| |||||||
| Insulin Alone | 149 | ||||||
| Without insulin | With insulin | ||||||
| Single | Glimepiride | 1 | 4 | ||||
| Oral | Glipizide | 2 | 11 | ||||
| Agent | Glyburide | 2 | 7 | ||||
| Metformin | 5 | ||||||
| Repaglinide | 2 | ||||||
| Two | Glimepiride | AND | Metformin | 1 | |||
| Oral | Glimepiride | AND | Rosiglitazone | 1 | |||
| Agents | Glimepiride | AND | Pioglitazone | 1 | |||
| Glipizide | AND | Pioglitazone | 1 | ||||
| Glipizide | AND | Metformin | 4 | ||||
| Glyburide | AND | Metformin | 5 | ||||
| Metformin | AND | Rosiglitazone | 3 | 1 | |||
| Rosiglitazone | AND | Repaglinide | 1 | 1 | |||
| Three | Glipizide | AND | Metformin | AND | Rosiglitazone | 1 | |
| Oral | Glyburide | AND | Metformin | AND | Pioglitazone | 1 | |
| Agents | Pioglitazone | AND | Nateglinide | AND | Repaglinide | 1 | |
| TOTAL | 206 | ||||||
The prevalence of hypoglycemia did not significantly differ among patients treated with oral agents alone (9 of 85, 10.6%), patients treated with insulin alone (149 of 1497, 10%), and patients treated with both (47 of 592, 7.9%). However, there was a significant relationship between specific oral agent and probability of hypoglycemia. Glyburide was associated with a higher risk of hypoglycemia (19.1%, P < .01) than were other oral agents (Table 3).
| Oral agent | Patients with hypoglycemia | P value |
|---|---|---|
| ||
| Sulfonylureas | ||
| Glimepiride | 13.6% (8/59) | |
| Glipizide | 10.0% (19/190) | |
| Glyburide | 19.1% (18/94) | < .01 |
| Biguanide | 6.4% (22/344) | |
| Metformin | < .05 | |
| Thiazolidinediones | ||
| Pioglitazone | 5.1% (4/78) | |
| Rosiglitazone | 6.4% (6/94) | |
| Meglitinides | ||
| Nateglinide | 7.1% (1/14) | |
| Repaglinide | 7.0% (4/57) | |
DISCUSSION
Recently, many have called for substantive changes in the management of the hospitalized diabetic.15, 16 Most have recommended replacing sliding‐scale insulin with basal bolus insulin dosing and have challenged the historic tolerance of hyperglycemia during an acute hospital stay.17 However, as hospitals and physicians transform the management of inpatient hyperglycemia, they must assess the frequency of hypoglycemia and evaluate the risk/benefit ratio of strict glycemic control.18 Thus, one study found that eliminating sliding‐scale insulin markedly improved diabetes control but hypoglycemia (BG 60 mg/dL) was more frequent.10 The cost of euglycemia is hypoglycemia.2
We report a 9.5% rate of hypoglycemia among adult hospitalized patients being treated for hyperglycemia, including those in the ICU and those in non‐ICU settings. In widely publicized landmark trials, 5.2% of intensively treated surgical ICU patients14 and 18.7% of intensively treated medical ICU patients13 experienced hypoglycemia with no adverse events. Using those studies' definition of hypoglycemia (BG 40 mg/dL), only 2.4% (53 of 2174) of our patients experienced hypoglycemia. However, our survey included general medical and surgical patients as well as ICU patients treated at their physicians' discretion, reflecting the greater variability in care that exists outside a randomized, ICU trial.
We did not anticipate the duration to documented resolution of hypoglycemic episodes, nor did we anticipate the number of hypoglycemia‐related adverse events. We believe that hospitals will need to develop formal strategies to minimize the hypoglycemic risk from tight glycemic control. The frequency and duration of the time it took to recheck the glucose, coupled with the 4.1% symptomatic event rate, suggests that inpatient hypoglycemia deserves more attention. One potential focus is the interruption of nutrition, as medications may not be readjusted when patients' oral intake declines or when they travel for tests.19
More than 40% of our hypoglycemic patients experienced recurrent episodes. This may reflect a lack of adjustment of medications following hypoglycemia. However, recurrent hypoglycemia may also be explained by hypoglycemia‐associated autonomic failure and the desensitization to hypoglycemia that occurs once a patient has lower blood glucose.2 Thus, hypoglycemic patients are at high risk of repeat episodes and often require more frequent BG monitoring. Of note, patients with hypoglycemia unawareness may not have symptoms despite low BG, and thus unless they develop signs of hypoglycemia, they would not meet criteria for an adverse event in our study, despite a very low BG.
Medical error can precipitate hypoglycemia,4, 20 and the Institute for Safe Medication Practices21 and the Joint Commission on Accreditation of Healthcare Organizations22 consider insulin a high‐risk medication. We found no hypoglycemic episodes associated with a medication error. Our CPOE system eliminates ambiguity from poor penmanship, and hospital policy requires 2 nurses to check all administered insulin. However, despite the apparent lack of dispensing/administration medication errors, nearly 10% of patients receiving hypoglycemic therapy experienced iatrogenic hypoglycemia. Thus, strategies to reduce hypoglycemia must expand beyond the prevention of medication errors.
Contrary to our expectation, we found the prevalence of hypoglycemia was at least as high, if not higher, for patients taking only oral hypoglycemics than for patients taking either insulin alone or insulin in combination with oral antihyperglycemic agents. Glyburide appeared to carry the most risk both in our population and in previous studies,2325 perhaps because of a moderately active hepatic metabolite.26 The risk of hypoglycemia with different oral agents warrants further study.
The study stimulated several actions. First, we augmented the online nursing flow sheet to permit documentation of hypoglycemic episodes, including the administration of orange juice or food. Second, our CPOE system now prevents a physician from inadvertently deselecting the hypoglycemia protocol. Third, the CPOE system prompts the nurse to recheck the BG as specified in the hypoglycemia protocol. Finally, the CPOE system warns physicians to adjust antihyperglycemic agents when they institute nutritional changes. We propose that monitoring hypoglycemia rates must become a necessary component of inpatient diabetes care that is both effective and safe and plan to monitor these rates to determine the impact of interventions designed to reduce the frequency of hypoglycemia‐related adverse events.
Our study had several limitations. We only included episodes of hypoglycemia that were identified with a POC BG. This excluded patients treated for symptomatic hypoglycemia without a measured POC BG, potentially underestimating the event rate. Moreover, defining time to resolution of a hypoglycemic episode as that documented with a serum BG but not a POC BG may have resulted in overestimating the duration, and nurses may have documented POC BGs in the MAR after a substantial delay, also artificially lengthening the time to resolution. Capillary BG may underestimate the true degree of hypoglycemia,27 thus confounding the relationship between BG and adverse events. Our study was not designed to evaluate subtle suboptimal management of hyperglycemia as a cause of hypoglycemia, although expansion of the types and combinations of insulin has increased the possibility of prescribing errors. Nor were we able to assess the preventability of hypoglycemic episodes or the independent risk factors for hypoglycemia. Finally, this study originated from a single academic hospital and thus may reflect its unique idiosyncrasies.
We have reported a comprehensive survey of hypoglycemia in patients treated with antihyperglycemic agents at a single hospital. At the time the study took place, we had not instituted hospitalwide strategies to maintain BG near euglycemic targets, although such strategies have since begun. To detect untoward events that may follow from our efforts to better control hyperglycemia, we believe it is important to establish baseline measurements. Even without aiming for tighter glucose control, we identified the need to aim for and possible strategies to achieve, better prevention of hypoglycemia.
APPENDIX
SUMMARY OF DEFINITIONS FOR CHART REVIEW
New onset diabetes was defined as diabetes diagnosed during the current hospital admission when there was no previous history of diabetes.
No diabetes was defined as no history of diabetes and no diagnosis of diabetes during the index hospital stay.
Documentation was defined as any notation in the record by the physician or nurse acknowledging the hypoglycemic episode, other than the BG value itself.
Time to recheck BG was defined as the time in the MAR between a recorded BG 60 mg/dL and the next recorded BG.
Resolution was defined as the time in the MAR between a recorded BG 60 mg/dL and the first recorded BG 80 mg/dL (if, following a BG > 80 mg/dL, the next BG was 60 mg/dL, the 2 BG 60 mg/dL were defined as belonging to the same episode and that no resolution had yet occurred).
Decline in enteral intake was defined as any new NPO order on the day of the episode or missed meal within 3 hours of the episode.
Hypoglycemia‐related symptomatic adverse event was defined as any documented event at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased hospitalization. Change of care did not include following the hypoglycemic protocol and administering 50% dextrose or glucagon, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ,,.Hypoglycemia in diabetes.Diabetes Care.2003;26:1902–1912.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- .Unexpected hypoglycemia in a critically ill patient.Ann Intern Med.2002;137:110–116.
- ,.Hypoglycemia: causes, neurological manifestations and outcome.Ann Neurol.1985;17:421–430.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.J Parenter Enteral Nutr.1998;22:77–81.
- ,,,.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thor Surg.1999;67:352–362.
- ,,, et al.Inpatient management of diabetes: survey in a tertiary care center.Postgrad Med J.2003;79:585–587.
- ,.Incidence of hypoglycemia and nutritional intake in patients on a general medical unit.Nursingconnections.1989;2:33–40.
- .Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,.Eliminating sliding‐scale insulin.Diabetes Care.2005;28:1008–1011.
- American Diabetes Association Workgroup on Hypoglycemia.Defining and reporting hypoglycemia in diabetes. A report from the American Diabetes Association workgroup on hypoglycemia.Diabetes Care.2005;28:245–1249.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461
- ;,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,.Inpatient management of diabetes mellitus.Am J Med.2002;113:317–323.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolicControl Endo Pract.2004;10:77–82.
- ,,.Inpatient diabetology, the new frontier.J Gen Intern Med.2004;19:466–471.
- ,.Counterpoint: inpatient glucose management, a premature call to arms?Diabetes Care.2005;28:976–979.
- ,,,.Causes of hyperglycemia and hypoglycemia in adult inpatients.Am J Health Syst Pharm.2005;62:714–719.
- ,,.Hypoglycemia in hospitalized patients: causes and outcomes.N Engl J Med.1986;315:245–1250.
- Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed July 27,2006.
- Joint Commission on Accreditation of Healthcare Organizations. High alert medications and patient safety. Sentinel Event Alert Issue 11, November 19, 1999 Available at: http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_11.htm. Accessed July 27,2006.
- .Comparative tolerability of sulfonylureas in diabetes mellitus.Drug Saf.2000;22:313–320.
- ,,,.Individual sulfonylureas and serious hypoglycemia in older people.J Am Geriatr Soc.1996;44:751–755
- ,.Sulfonylureas. In:DeFronzo RA, ed.Current Management of Diabetes Mellitus.St. Louis, MO:Mosby;1998:96–101.
- ,,.Diabetes Mellitus in Pharmacotherapy: A Pathophysiologic Approach.6th ed.Dipiro JT, ed.New York:McGraw Hill;2005.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33:2778–2785.
Glycemic control in the inpatient setting has received increasing attention in recent years, with the demonstration that appropriate blood glucose (BG) control prevents adverse events in both intensive care unit (ICU) and non‐ICU settings.1 Recent recommendations set target blood glucose levels near euglycemia for most hospitalized patients.1 Unfortunately, the risk of hypoglycemia increases with tighter glycemic control,2 and hypoglycemia may result in catastrophic events.35 Although hyperglycemia is associated with postoperative infection,6 and effective management decreases wound infections,7 few reports have detailed the hypoglycemia rates among surgical patients.8 Hypoglycemia rates on medical services are as high as 28%,9, 10 and efforts to achieve more normal BG levels in hospitalized patients have been associated with more hypoglycemia.11
We undertook a study of hypoglycemia in all adult hospitalized patients receiving hypoglycemic therapy at our institution. The purpose of this study was to determine the incidence, natural history, associations, and consequences of hypoglycemia in this broad inpatient population in order to have a baseline prior to introducing any formal hospital strategies to achieve the newer targets for glycemic control.
Research Design and Methods
Thomas Jefferson University Hospital (TJUH) is a 675‐bed acute care teaching institution in center‐city Philadelphia with more than 30,000 patient admissions each year. We undertook a prospective, consecutive medical record review from August 16, 2004, to November 15, 2004, of hospitalized patients who had experienced at least 1 hypoglycemic episode, defined as at least one blood glucose (BG) 60 mg/dL within 48 hours of administration of an antihyperglycemic agent in the hospital. The definition of hypoglycemia was consistent with our hospital policies and a compromise between the BG 70 mg/dL proposed by the American Diabetes Association (ADA) hypoglycemia workgroup12 and the BG 40 mg/dL used by authors studying glycemic control in the ICU.13, 14
Hypoglycemic episodes were identified by a daily electronic search of the online medication administration record (MAR) where nurses document all point‐of‐care (POC) BG values. Two of the authors (P.V. and V.G.) reviewed the medical record for each episode and excluded pediatric (<18 years), emergency department, and maternity patients. Intensive care, step‐down, and medical/surgical unit patients were all included if the hypoglycemia had occurred within 48 hours of hospital administration of an antihyperglycemic agent. All medication orders at TJUH are placed through the computerized prescriber order entry (CPOE) system (Centricity Enterprise), which links all antihyperglycemic agents to a standardized hypoglycemia treatment protocol. The protocol includes instructions to administer glucose and/or glucagon and check the BG 15 minutes after a hypoglycemic episode. We established operational definitions prior to chart review (Appendix). A symptomatic hypoglycemia‐related adverse event was defined as any documented event occurring at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased length of hospitalization. We did not include following our hypoglycemic protocol with the administration of 50% dextrose or glucagon as a change of care, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
We searched the University Health System Consortium Clinical Database (CDB) to quantify the number of patients at TJUH receiving any antihyperglycemic agent during the study period and to identify the specific agents received. The CDB receives all patient, physician, and pharmacy dose‐ specific information from the hospital clinical and billing information systems. We defined subgroups of patients taking insulin(s) only, taking oral agent(s) only, and taking a combination.
Differences between proportions were evaluated using the chi‐square statistic; differences between means were evaluated using the Student t test. Probabilities of the null hypothesis less than .05 were considered significant.
The project was approved by the Institutional Review Board for Human Subjects at Thomas Jefferson University.
RESULTS
Over the 2‐month study period 8140 patients were admitted, of whom 2174 (27%) received an antihyperglycemic agent. Five hundred and sixty‐eight hypoglycemic episodes (BG 60 mg/dL) occurred in 265 patients. We excluded 84 episodes among 59 patients who did not receive antihyperglycemic agents, resulting in 484 episodes of hypoglycemia occurring within 48 hours of hospital administration of an antihyperglycemic agent in 206 patients, an average of 5.26 episodes per day. Of the 2174 of patients receiving antihyperglycemic agents, 206 (9.5%) experienced 1 or more episodes of hypoglycemia.
Patient ages ranged from 20 to 93 years, with an average of 62 years. Fifty‐seven percent (118 of 206) of participants were female. About one‐fourth of all episodes (23.8%) occurred in the ICU setting. The distribution of patients by decade and their ICU status are presented in Figure 1. Of the 206 patients, 29% (59) had type 1 diabetes mellitus (DM), 49% (102) had type 2 DM, 1% (2) had new‐onset diabetes, and 21% (43) had no diagnosis of DM. Of the 484 hypoglycemic episodes, 37.8% occurred in patients with type 1 DM, 46.9% in patients with type 2 DM, and 0.6% in patients with new‐onset DM. The remaining 14.5% occurred in patients with no documented history of DM, although they were receiving antihyperglycemic agents. More than 1 episode was experienced by 44% of patients, and 12% experienced 5 or more episodes.

The BG was between 51 and 60 mg/dL in 282 of the episodes (58.2%), between 41 and 50 mg/dL in 149 episodes (30.8%) and 40 mg/dL or less in 53 episodes (11%). In 20 episodes (4.1% of episodes, representing fewer than 1% of all patients receiving an antihyperglycemic agent), a symptomatic hypoglycemia‐related adverse event was documented. All but 1 adverse event occurred outside the ICU. Ten of these events (2.1% of all hypoglycemic episodes) in 10 patients involved symptoms including headache, agitation, disorientation, and tremors. Of these patients 9 had type 1 DM, and 1 had type 2 DM. Six events (1.2% of hypoglycemic episodes) in 4 patients involved seizures. Two of these patients had type 1 DM, and 2 had type 2 DM. Four events (0.8% of hypoglycemic episodes) in 4 patients involved an unresponsive or unarousable state, including the sole ICU episode of symptomatic hypoglycemia. Three of these patients had type 1 DM, and 1 had type 2 DM. Patients with hypoglycemia‐related adverse events had a mean BG of 43.0 mg/dL, significantly lower (P = .01) than the mean BG of 50.9 mg/dL for hypoglycemic episodes without such events. However, 35% of these events occurred with a measured BG between 50 and 60 mg/dL. The distributions of BG values associated with symptomatic and asymptomatic events are shown in Figure 2. There is no useful threshold that separates symptomatic from asymptomatic hypoglycemia. No deaths or irreversible consequences were associated with hypoglycemia.
Approximately 40% (195 of 484) of the hypoglycemic episodes were related to decreased enteral intake (Table 1). In addition, 6.1% (30 of 484) of hypoglycemic episodes were related to insulin adjustment and 0.4% (2 of 484) to steroid withdrawal. In 43% (209 of 484) of the episodes the cause of the hypoglycemia was unclear. The remaining 10.4% of episodes were attributed to diverse causes.
| N (%) | |
|---|---|
| |
| NPO for unknown reason | 30 (6.2) |
| NPO for procedure/emntubated | 29 (6) |
| NPO for other documented reason (ie, fever/sepsis) | 10 (2.1) |
| Decreased PO intake (includes missed meal) | 126 (26) |
| No change in PO intake | 289 (59.7) |
One third of patients had a documented BG rechecked within 60 minutes, and fewer than half of the hypoglycemic patients had documented euglycemia within 2 hours of their low blood glucose measurement. The average time to documented resolution of a hypoglycemic episode was 4 hours, 3 minutes, with a median of 2 hours, 25 minutes.
Table 2 delineates the various combinations of antihyperglycemic agents that the 206 patients received in the 48 hours prior to a hypoglycemic episode. Of the 484 hypoglycemic episodes, 362 involved insulin. Of patients receiving insulin, 38 of 362 of episodes of hypoglycemia occurred in patients receiving sliding‐scale insulin (SSI) dosing as the only insulin order. In 163 hypoglycemic episodes, insulin was dosed with a combination of SSI and infusion or SSI with daily long‐acting insulin. The remaining 161 episodes involved administration of insulin to patients without an accompanying sliding‐scale order.
| |||||||
| Insulin Alone | 149 | ||||||
| Without insulin | With insulin | ||||||
| Single | Glimepiride | 1 | 4 | ||||
| Oral | Glipizide | 2 | 11 | ||||
| Agent | Glyburide | 2 | 7 | ||||
| Metformin | 5 | ||||||
| Repaglinide | 2 | ||||||
| Two | Glimepiride | AND | Metformin | 1 | |||
| Oral | Glimepiride | AND | Rosiglitazone | 1 | |||
| Agents | Glimepiride | AND | Pioglitazone | 1 | |||
| Glipizide | AND | Pioglitazone | 1 | ||||
| Glipizide | AND | Metformin | 4 | ||||
| Glyburide | AND | Metformin | 5 | ||||
| Metformin | AND | Rosiglitazone | 3 | 1 | |||
| Rosiglitazone | AND | Repaglinide | 1 | 1 | |||
| Three | Glipizide | AND | Metformin | AND | Rosiglitazone | 1 | |
| Oral | Glyburide | AND | Metformin | AND | Pioglitazone | 1 | |
| Agents | Pioglitazone | AND | Nateglinide | AND | Repaglinide | 1 | |
| TOTAL | 206 | ||||||
The prevalence of hypoglycemia did not significantly differ among patients treated with oral agents alone (9 of 85, 10.6%), patients treated with insulin alone (149 of 1497, 10%), and patients treated with both (47 of 592, 7.9%). However, there was a significant relationship between specific oral agent and probability of hypoglycemia. Glyburide was associated with a higher risk of hypoglycemia (19.1%, P < .01) than were other oral agents (Table 3).
| Oral agent | Patients with hypoglycemia | P value |
|---|---|---|
| ||
| Sulfonylureas | ||
| Glimepiride | 13.6% (8/59) | |
| Glipizide | 10.0% (19/190) | |
| Glyburide | 19.1% (18/94) | < .01 |
| Biguanide | 6.4% (22/344) | |
| Metformin | < .05 | |
| Thiazolidinediones | ||
| Pioglitazone | 5.1% (4/78) | |
| Rosiglitazone | 6.4% (6/94) | |
| Meglitinides | ||
| Nateglinide | 7.1% (1/14) | |
| Repaglinide | 7.0% (4/57) | |
DISCUSSION
Recently, many have called for substantive changes in the management of the hospitalized diabetic.15, 16 Most have recommended replacing sliding‐scale insulin with basal bolus insulin dosing and have challenged the historic tolerance of hyperglycemia during an acute hospital stay.17 However, as hospitals and physicians transform the management of inpatient hyperglycemia, they must assess the frequency of hypoglycemia and evaluate the risk/benefit ratio of strict glycemic control.18 Thus, one study found that eliminating sliding‐scale insulin markedly improved diabetes control but hypoglycemia (BG 60 mg/dL) was more frequent.10 The cost of euglycemia is hypoglycemia.2
We report a 9.5% rate of hypoglycemia among adult hospitalized patients being treated for hyperglycemia, including those in the ICU and those in non‐ICU settings. In widely publicized landmark trials, 5.2% of intensively treated surgical ICU patients14 and 18.7% of intensively treated medical ICU patients13 experienced hypoglycemia with no adverse events. Using those studies' definition of hypoglycemia (BG 40 mg/dL), only 2.4% (53 of 2174) of our patients experienced hypoglycemia. However, our survey included general medical and surgical patients as well as ICU patients treated at their physicians' discretion, reflecting the greater variability in care that exists outside a randomized, ICU trial.
We did not anticipate the duration to documented resolution of hypoglycemic episodes, nor did we anticipate the number of hypoglycemia‐related adverse events. We believe that hospitals will need to develop formal strategies to minimize the hypoglycemic risk from tight glycemic control. The frequency and duration of the time it took to recheck the glucose, coupled with the 4.1% symptomatic event rate, suggests that inpatient hypoglycemia deserves more attention. One potential focus is the interruption of nutrition, as medications may not be readjusted when patients' oral intake declines or when they travel for tests.19
More than 40% of our hypoglycemic patients experienced recurrent episodes. This may reflect a lack of adjustment of medications following hypoglycemia. However, recurrent hypoglycemia may also be explained by hypoglycemia‐associated autonomic failure and the desensitization to hypoglycemia that occurs once a patient has lower blood glucose.2 Thus, hypoglycemic patients are at high risk of repeat episodes and often require more frequent BG monitoring. Of note, patients with hypoglycemia unawareness may not have symptoms despite low BG, and thus unless they develop signs of hypoglycemia, they would not meet criteria for an adverse event in our study, despite a very low BG.
Medical error can precipitate hypoglycemia,4, 20 and the Institute for Safe Medication Practices21 and the Joint Commission on Accreditation of Healthcare Organizations22 consider insulin a high‐risk medication. We found no hypoglycemic episodes associated with a medication error. Our CPOE system eliminates ambiguity from poor penmanship, and hospital policy requires 2 nurses to check all administered insulin. However, despite the apparent lack of dispensing/administration medication errors, nearly 10% of patients receiving hypoglycemic therapy experienced iatrogenic hypoglycemia. Thus, strategies to reduce hypoglycemia must expand beyond the prevention of medication errors.
Contrary to our expectation, we found the prevalence of hypoglycemia was at least as high, if not higher, for patients taking only oral hypoglycemics than for patients taking either insulin alone or insulin in combination with oral antihyperglycemic agents. Glyburide appeared to carry the most risk both in our population and in previous studies,2325 perhaps because of a moderately active hepatic metabolite.26 The risk of hypoglycemia with different oral agents warrants further study.
The study stimulated several actions. First, we augmented the online nursing flow sheet to permit documentation of hypoglycemic episodes, including the administration of orange juice or food. Second, our CPOE system now prevents a physician from inadvertently deselecting the hypoglycemia protocol. Third, the CPOE system prompts the nurse to recheck the BG as specified in the hypoglycemia protocol. Finally, the CPOE system warns physicians to adjust antihyperglycemic agents when they institute nutritional changes. We propose that monitoring hypoglycemia rates must become a necessary component of inpatient diabetes care that is both effective and safe and plan to monitor these rates to determine the impact of interventions designed to reduce the frequency of hypoglycemia‐related adverse events.
Our study had several limitations. We only included episodes of hypoglycemia that were identified with a POC BG. This excluded patients treated for symptomatic hypoglycemia without a measured POC BG, potentially underestimating the event rate. Moreover, defining time to resolution of a hypoglycemic episode as that documented with a serum BG but not a POC BG may have resulted in overestimating the duration, and nurses may have documented POC BGs in the MAR after a substantial delay, also artificially lengthening the time to resolution. Capillary BG may underestimate the true degree of hypoglycemia,27 thus confounding the relationship between BG and adverse events. Our study was not designed to evaluate subtle suboptimal management of hyperglycemia as a cause of hypoglycemia, although expansion of the types and combinations of insulin has increased the possibility of prescribing errors. Nor were we able to assess the preventability of hypoglycemic episodes or the independent risk factors for hypoglycemia. Finally, this study originated from a single academic hospital and thus may reflect its unique idiosyncrasies.
We have reported a comprehensive survey of hypoglycemia in patients treated with antihyperglycemic agents at a single hospital. At the time the study took place, we had not instituted hospitalwide strategies to maintain BG near euglycemic targets, although such strategies have since begun. To detect untoward events that may follow from our efforts to better control hyperglycemia, we believe it is important to establish baseline measurements. Even without aiming for tighter glucose control, we identified the need to aim for and possible strategies to achieve, better prevention of hypoglycemia.
APPENDIX
SUMMARY OF DEFINITIONS FOR CHART REVIEW
New onset diabetes was defined as diabetes diagnosed during the current hospital admission when there was no previous history of diabetes.
No diabetes was defined as no history of diabetes and no diagnosis of diabetes during the index hospital stay.
Documentation was defined as any notation in the record by the physician or nurse acknowledging the hypoglycemic episode, other than the BG value itself.
Time to recheck BG was defined as the time in the MAR between a recorded BG 60 mg/dL and the next recorded BG.
Resolution was defined as the time in the MAR between a recorded BG 60 mg/dL and the first recorded BG 80 mg/dL (if, following a BG > 80 mg/dL, the next BG was 60 mg/dL, the 2 BG 60 mg/dL were defined as belonging to the same episode and that no resolution had yet occurred).
Decline in enteral intake was defined as any new NPO order on the day of the episode or missed meal within 3 hours of the episode.
Hypoglycemia‐related symptomatic adverse event was defined as any documented event at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased hospitalization. Change of care did not include following the hypoglycemic protocol and administering 50% dextrose or glucagon, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
Glycemic control in the inpatient setting has received increasing attention in recent years, with the demonstration that appropriate blood glucose (BG) control prevents adverse events in both intensive care unit (ICU) and non‐ICU settings.1 Recent recommendations set target blood glucose levels near euglycemia for most hospitalized patients.1 Unfortunately, the risk of hypoglycemia increases with tighter glycemic control,2 and hypoglycemia may result in catastrophic events.35 Although hyperglycemia is associated with postoperative infection,6 and effective management decreases wound infections,7 few reports have detailed the hypoglycemia rates among surgical patients.8 Hypoglycemia rates on medical services are as high as 28%,9, 10 and efforts to achieve more normal BG levels in hospitalized patients have been associated with more hypoglycemia.11
We undertook a study of hypoglycemia in all adult hospitalized patients receiving hypoglycemic therapy at our institution. The purpose of this study was to determine the incidence, natural history, associations, and consequences of hypoglycemia in this broad inpatient population in order to have a baseline prior to introducing any formal hospital strategies to achieve the newer targets for glycemic control.
Research Design and Methods
Thomas Jefferson University Hospital (TJUH) is a 675‐bed acute care teaching institution in center‐city Philadelphia with more than 30,000 patient admissions each year. We undertook a prospective, consecutive medical record review from August 16, 2004, to November 15, 2004, of hospitalized patients who had experienced at least 1 hypoglycemic episode, defined as at least one blood glucose (BG) 60 mg/dL within 48 hours of administration of an antihyperglycemic agent in the hospital. The definition of hypoglycemia was consistent with our hospital policies and a compromise between the BG 70 mg/dL proposed by the American Diabetes Association (ADA) hypoglycemia workgroup12 and the BG 40 mg/dL used by authors studying glycemic control in the ICU.13, 14
Hypoglycemic episodes were identified by a daily electronic search of the online medication administration record (MAR) where nurses document all point‐of‐care (POC) BG values. Two of the authors (P.V. and V.G.) reviewed the medical record for each episode and excluded pediatric (<18 years), emergency department, and maternity patients. Intensive care, step‐down, and medical/surgical unit patients were all included if the hypoglycemia had occurred within 48 hours of hospital administration of an antihyperglycemic agent. All medication orders at TJUH are placed through the computerized prescriber order entry (CPOE) system (Centricity Enterprise), which links all antihyperglycemic agents to a standardized hypoglycemia treatment protocol. The protocol includes instructions to administer glucose and/or glucagon and check the BG 15 minutes after a hypoglycemic episode. We established operational definitions prior to chart review (Appendix). A symptomatic hypoglycemia‐related adverse event was defined as any documented event occurring at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased length of hospitalization. We did not include following our hypoglycemic protocol with the administration of 50% dextrose or glucagon as a change of care, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
We searched the University Health System Consortium Clinical Database (CDB) to quantify the number of patients at TJUH receiving any antihyperglycemic agent during the study period and to identify the specific agents received. The CDB receives all patient, physician, and pharmacy dose‐ specific information from the hospital clinical and billing information systems. We defined subgroups of patients taking insulin(s) only, taking oral agent(s) only, and taking a combination.
Differences between proportions were evaluated using the chi‐square statistic; differences between means were evaluated using the Student t test. Probabilities of the null hypothesis less than .05 were considered significant.
The project was approved by the Institutional Review Board for Human Subjects at Thomas Jefferson University.
RESULTS
Over the 2‐month study period 8140 patients were admitted, of whom 2174 (27%) received an antihyperglycemic agent. Five hundred and sixty‐eight hypoglycemic episodes (BG 60 mg/dL) occurred in 265 patients. We excluded 84 episodes among 59 patients who did not receive antihyperglycemic agents, resulting in 484 episodes of hypoglycemia occurring within 48 hours of hospital administration of an antihyperglycemic agent in 206 patients, an average of 5.26 episodes per day. Of the 2174 of patients receiving antihyperglycemic agents, 206 (9.5%) experienced 1 or more episodes of hypoglycemia.
Patient ages ranged from 20 to 93 years, with an average of 62 years. Fifty‐seven percent (118 of 206) of participants were female. About one‐fourth of all episodes (23.8%) occurred in the ICU setting. The distribution of patients by decade and their ICU status are presented in Figure 1. Of the 206 patients, 29% (59) had type 1 diabetes mellitus (DM), 49% (102) had type 2 DM, 1% (2) had new‐onset diabetes, and 21% (43) had no diagnosis of DM. Of the 484 hypoglycemic episodes, 37.8% occurred in patients with type 1 DM, 46.9% in patients with type 2 DM, and 0.6% in patients with new‐onset DM. The remaining 14.5% occurred in patients with no documented history of DM, although they were receiving antihyperglycemic agents. More than 1 episode was experienced by 44% of patients, and 12% experienced 5 or more episodes.

The BG was between 51 and 60 mg/dL in 282 of the episodes (58.2%), between 41 and 50 mg/dL in 149 episodes (30.8%) and 40 mg/dL or less in 53 episodes (11%). In 20 episodes (4.1% of episodes, representing fewer than 1% of all patients receiving an antihyperglycemic agent), a symptomatic hypoglycemia‐related adverse event was documented. All but 1 adverse event occurred outside the ICU. Ten of these events (2.1% of all hypoglycemic episodes) in 10 patients involved symptoms including headache, agitation, disorientation, and tremors. Of these patients 9 had type 1 DM, and 1 had type 2 DM. Six events (1.2% of hypoglycemic episodes) in 4 patients involved seizures. Two of these patients had type 1 DM, and 2 had type 2 DM. Four events (0.8% of hypoglycemic episodes) in 4 patients involved an unresponsive or unarousable state, including the sole ICU episode of symptomatic hypoglycemia. Three of these patients had type 1 DM, and 1 had type 2 DM. Patients with hypoglycemia‐related adverse events had a mean BG of 43.0 mg/dL, significantly lower (P = .01) than the mean BG of 50.9 mg/dL for hypoglycemic episodes without such events. However, 35% of these events occurred with a measured BG between 50 and 60 mg/dL. The distributions of BG values associated with symptomatic and asymptomatic events are shown in Figure 2. There is no useful threshold that separates symptomatic from asymptomatic hypoglycemia. No deaths or irreversible consequences were associated with hypoglycemia.
Approximately 40% (195 of 484) of the hypoglycemic episodes were related to decreased enteral intake (Table 1). In addition, 6.1% (30 of 484) of hypoglycemic episodes were related to insulin adjustment and 0.4% (2 of 484) to steroid withdrawal. In 43% (209 of 484) of the episodes the cause of the hypoglycemia was unclear. The remaining 10.4% of episodes were attributed to diverse causes.
| N (%) | |
|---|---|
| |
| NPO for unknown reason | 30 (6.2) |
| NPO for procedure/emntubated | 29 (6) |
| NPO for other documented reason (ie, fever/sepsis) | 10 (2.1) |
| Decreased PO intake (includes missed meal) | 126 (26) |
| No change in PO intake | 289 (59.7) |
One third of patients had a documented BG rechecked within 60 minutes, and fewer than half of the hypoglycemic patients had documented euglycemia within 2 hours of their low blood glucose measurement. The average time to documented resolution of a hypoglycemic episode was 4 hours, 3 minutes, with a median of 2 hours, 25 minutes.
Table 2 delineates the various combinations of antihyperglycemic agents that the 206 patients received in the 48 hours prior to a hypoglycemic episode. Of the 484 hypoglycemic episodes, 362 involved insulin. Of patients receiving insulin, 38 of 362 of episodes of hypoglycemia occurred in patients receiving sliding‐scale insulin (SSI) dosing as the only insulin order. In 163 hypoglycemic episodes, insulin was dosed with a combination of SSI and infusion or SSI with daily long‐acting insulin. The remaining 161 episodes involved administration of insulin to patients without an accompanying sliding‐scale order.
| |||||||
| Insulin Alone | 149 | ||||||
| Without insulin | With insulin | ||||||
| Single | Glimepiride | 1 | 4 | ||||
| Oral | Glipizide | 2 | 11 | ||||
| Agent | Glyburide | 2 | 7 | ||||
| Metformin | 5 | ||||||
| Repaglinide | 2 | ||||||
| Two | Glimepiride | AND | Metformin | 1 | |||
| Oral | Glimepiride | AND | Rosiglitazone | 1 | |||
| Agents | Glimepiride | AND | Pioglitazone | 1 | |||
| Glipizide | AND | Pioglitazone | 1 | ||||
| Glipizide | AND | Metformin | 4 | ||||
| Glyburide | AND | Metformin | 5 | ||||
| Metformin | AND | Rosiglitazone | 3 | 1 | |||
| Rosiglitazone | AND | Repaglinide | 1 | 1 | |||
| Three | Glipizide | AND | Metformin | AND | Rosiglitazone | 1 | |
| Oral | Glyburide | AND | Metformin | AND | Pioglitazone | 1 | |
| Agents | Pioglitazone | AND | Nateglinide | AND | Repaglinide | 1 | |
| TOTAL | 206 | ||||||
The prevalence of hypoglycemia did not significantly differ among patients treated with oral agents alone (9 of 85, 10.6%), patients treated with insulin alone (149 of 1497, 10%), and patients treated with both (47 of 592, 7.9%). However, there was a significant relationship between specific oral agent and probability of hypoglycemia. Glyburide was associated with a higher risk of hypoglycemia (19.1%, P < .01) than were other oral agents (Table 3).
| Oral agent | Patients with hypoglycemia | P value |
|---|---|---|
| ||
| Sulfonylureas | ||
| Glimepiride | 13.6% (8/59) | |
| Glipizide | 10.0% (19/190) | |
| Glyburide | 19.1% (18/94) | < .01 |
| Biguanide | 6.4% (22/344) | |
| Metformin | < .05 | |
| Thiazolidinediones | ||
| Pioglitazone | 5.1% (4/78) | |
| Rosiglitazone | 6.4% (6/94) | |
| Meglitinides | ||
| Nateglinide | 7.1% (1/14) | |
| Repaglinide | 7.0% (4/57) | |
DISCUSSION
Recently, many have called for substantive changes in the management of the hospitalized diabetic.15, 16 Most have recommended replacing sliding‐scale insulin with basal bolus insulin dosing and have challenged the historic tolerance of hyperglycemia during an acute hospital stay.17 However, as hospitals and physicians transform the management of inpatient hyperglycemia, they must assess the frequency of hypoglycemia and evaluate the risk/benefit ratio of strict glycemic control.18 Thus, one study found that eliminating sliding‐scale insulin markedly improved diabetes control but hypoglycemia (BG 60 mg/dL) was more frequent.10 The cost of euglycemia is hypoglycemia.2
We report a 9.5% rate of hypoglycemia among adult hospitalized patients being treated for hyperglycemia, including those in the ICU and those in non‐ICU settings. In widely publicized landmark trials, 5.2% of intensively treated surgical ICU patients14 and 18.7% of intensively treated medical ICU patients13 experienced hypoglycemia with no adverse events. Using those studies' definition of hypoglycemia (BG 40 mg/dL), only 2.4% (53 of 2174) of our patients experienced hypoglycemia. However, our survey included general medical and surgical patients as well as ICU patients treated at their physicians' discretion, reflecting the greater variability in care that exists outside a randomized, ICU trial.
We did not anticipate the duration to documented resolution of hypoglycemic episodes, nor did we anticipate the number of hypoglycemia‐related adverse events. We believe that hospitals will need to develop formal strategies to minimize the hypoglycemic risk from tight glycemic control. The frequency and duration of the time it took to recheck the glucose, coupled with the 4.1% symptomatic event rate, suggests that inpatient hypoglycemia deserves more attention. One potential focus is the interruption of nutrition, as medications may not be readjusted when patients' oral intake declines or when they travel for tests.19
More than 40% of our hypoglycemic patients experienced recurrent episodes. This may reflect a lack of adjustment of medications following hypoglycemia. However, recurrent hypoglycemia may also be explained by hypoglycemia‐associated autonomic failure and the desensitization to hypoglycemia that occurs once a patient has lower blood glucose.2 Thus, hypoglycemic patients are at high risk of repeat episodes and often require more frequent BG monitoring. Of note, patients with hypoglycemia unawareness may not have symptoms despite low BG, and thus unless they develop signs of hypoglycemia, they would not meet criteria for an adverse event in our study, despite a very low BG.
Medical error can precipitate hypoglycemia,4, 20 and the Institute for Safe Medication Practices21 and the Joint Commission on Accreditation of Healthcare Organizations22 consider insulin a high‐risk medication. We found no hypoglycemic episodes associated with a medication error. Our CPOE system eliminates ambiguity from poor penmanship, and hospital policy requires 2 nurses to check all administered insulin. However, despite the apparent lack of dispensing/administration medication errors, nearly 10% of patients receiving hypoglycemic therapy experienced iatrogenic hypoglycemia. Thus, strategies to reduce hypoglycemia must expand beyond the prevention of medication errors.
Contrary to our expectation, we found the prevalence of hypoglycemia was at least as high, if not higher, for patients taking only oral hypoglycemics than for patients taking either insulin alone or insulin in combination with oral antihyperglycemic agents. Glyburide appeared to carry the most risk both in our population and in previous studies,2325 perhaps because of a moderately active hepatic metabolite.26 The risk of hypoglycemia with different oral agents warrants further study.
The study stimulated several actions. First, we augmented the online nursing flow sheet to permit documentation of hypoglycemic episodes, including the administration of orange juice or food. Second, our CPOE system now prevents a physician from inadvertently deselecting the hypoglycemia protocol. Third, the CPOE system prompts the nurse to recheck the BG as specified in the hypoglycemia protocol. Finally, the CPOE system warns physicians to adjust antihyperglycemic agents when they institute nutritional changes. We propose that monitoring hypoglycemia rates must become a necessary component of inpatient diabetes care that is both effective and safe and plan to monitor these rates to determine the impact of interventions designed to reduce the frequency of hypoglycemia‐related adverse events.
Our study had several limitations. We only included episodes of hypoglycemia that were identified with a POC BG. This excluded patients treated for symptomatic hypoglycemia without a measured POC BG, potentially underestimating the event rate. Moreover, defining time to resolution of a hypoglycemic episode as that documented with a serum BG but not a POC BG may have resulted in overestimating the duration, and nurses may have documented POC BGs in the MAR after a substantial delay, also artificially lengthening the time to resolution. Capillary BG may underestimate the true degree of hypoglycemia,27 thus confounding the relationship between BG and adverse events. Our study was not designed to evaluate subtle suboptimal management of hyperglycemia as a cause of hypoglycemia, although expansion of the types and combinations of insulin has increased the possibility of prescribing errors. Nor were we able to assess the preventability of hypoglycemic episodes or the independent risk factors for hypoglycemia. Finally, this study originated from a single academic hospital and thus may reflect its unique idiosyncrasies.
We have reported a comprehensive survey of hypoglycemia in patients treated with antihyperglycemic agents at a single hospital. At the time the study took place, we had not instituted hospitalwide strategies to maintain BG near euglycemic targets, although such strategies have since begun. To detect untoward events that may follow from our efforts to better control hyperglycemia, we believe it is important to establish baseline measurements. Even without aiming for tighter glucose control, we identified the need to aim for and possible strategies to achieve, better prevention of hypoglycemia.
APPENDIX
SUMMARY OF DEFINITIONS FOR CHART REVIEW
New onset diabetes was defined as diabetes diagnosed during the current hospital admission when there was no previous history of diabetes.
No diabetes was defined as no history of diabetes and no diagnosis of diabetes during the index hospital stay.
Documentation was defined as any notation in the record by the physician or nurse acknowledging the hypoglycemic episode, other than the BG value itself.
Time to recheck BG was defined as the time in the MAR between a recorded BG 60 mg/dL and the next recorded BG.
Resolution was defined as the time in the MAR between a recorded BG 60 mg/dL and the first recorded BG 80 mg/dL (if, following a BG > 80 mg/dL, the next BG was 60 mg/dL, the 2 BG 60 mg/dL were defined as belonging to the same episode and that no resolution had yet occurred).
Decline in enteral intake was defined as any new NPO order on the day of the episode or missed meal within 3 hours of the episode.
Hypoglycemia‐related symptomatic adverse event was defined as any documented event at the time of the hypoglycemic episode involving symptoms, change in care, temporary or permanent injury, or increased hospitalization. Change of care did not include following the hypoglycemic protocol and administering 50% dextrose or glucagon, as we considered this usual care, unless symptoms or signs also accompanied the hypoglycemic event.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ,,.Hypoglycemia in diabetes.Diabetes Care.2003;26:1902–1912.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- .Unexpected hypoglycemia in a critically ill patient.Ann Intern Med.2002;137:110–116.
- ,.Hypoglycemia: causes, neurological manifestations and outcome.Ann Neurol.1985;17:421–430.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.J Parenter Enteral Nutr.1998;22:77–81.
- ,,,.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thor Surg.1999;67:352–362.
- ,,, et al.Inpatient management of diabetes: survey in a tertiary care center.Postgrad Med J.2003;79:585–587.
- ,.Incidence of hypoglycemia and nutritional intake in patients on a general medical unit.Nursingconnections.1989;2:33–40.
- .Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,.Eliminating sliding‐scale insulin.Diabetes Care.2005;28:1008–1011.
- American Diabetes Association Workgroup on Hypoglycemia.Defining and reporting hypoglycemia in diabetes. A report from the American Diabetes Association workgroup on hypoglycemia.Diabetes Care.2005;28:245–1249.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461
- ;,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,.Inpatient management of diabetes mellitus.Am J Med.2002;113:317–323.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolicControl Endo Pract.2004;10:77–82.
- ,,.Inpatient diabetology, the new frontier.J Gen Intern Med.2004;19:466–471.
- ,.Counterpoint: inpatient glucose management, a premature call to arms?Diabetes Care.2005;28:976–979.
- ,,,.Causes of hyperglycemia and hypoglycemia in adult inpatients.Am J Health Syst Pharm.2005;62:714–719.
- ,,.Hypoglycemia in hospitalized patients: causes and outcomes.N Engl J Med.1986;315:245–1250.
- Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed July 27,2006.
- Joint Commission on Accreditation of Healthcare Organizations. High alert medications and patient safety. Sentinel Event Alert Issue 11, November 19, 1999 Available at: http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_11.htm. Accessed July 27,2006.
- .Comparative tolerability of sulfonylureas in diabetes mellitus.Drug Saf.2000;22:313–320.
- ,,,.Individual sulfonylureas and serious hypoglycemia in older people.J Am Geriatr Soc.1996;44:751–755
- ,.Sulfonylureas. In:DeFronzo RA, ed.Current Management of Diabetes Mellitus.St. Louis, MO:Mosby;1998:96–101.
- ,,.Diabetes Mellitus in Pharmacotherapy: A Pathophysiologic Approach.6th ed.Dipiro JT, ed.New York:McGraw Hill;2005.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33:2778–2785.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ,,.Hypoglycemia in diabetes.Diabetes Care.2003;26:1902–1912.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- .Unexpected hypoglycemia in a critically ill patient.Ann Intern Med.2002;137:110–116.
- ,.Hypoglycemia: causes, neurological manifestations and outcome.Ann Neurol.1985;17:421–430.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.J Parenter Enteral Nutr.1998;22:77–81.
- ,,,.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thor Surg.1999;67:352–362.
- ,,, et al.Inpatient management of diabetes: survey in a tertiary care center.Postgrad Med J.2003;79:585–587.
- ,.Incidence of hypoglycemia and nutritional intake in patients on a general medical unit.Nursingconnections.1989;2:33–40.
- .Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,.Eliminating sliding‐scale insulin.Diabetes Care.2005;28:1008–1011.
- American Diabetes Association Workgroup on Hypoglycemia.Defining and reporting hypoglycemia in diabetes. A report from the American Diabetes Association workgroup on hypoglycemia.Diabetes Care.2005;28:245–1249.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461
- ;,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,.Inpatient management of diabetes mellitus.Am J Med.2002;113:317–323.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolicControl Endo Pract.2004;10:77–82.
- ,,.Inpatient diabetology, the new frontier.J Gen Intern Med.2004;19:466–471.
- ,.Counterpoint: inpatient glucose management, a premature call to arms?Diabetes Care.2005;28:976–979.
- ,,,.Causes of hyperglycemia and hypoglycemia in adult inpatients.Am J Health Syst Pharm.2005;62:714–719.
- ,,.Hypoglycemia in hospitalized patients: causes and outcomes.N Engl J Med.1986;315:245–1250.
- Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed July 27,2006.
- Joint Commission on Accreditation of Healthcare Organizations. High alert medications and patient safety. Sentinel Event Alert Issue 11, November 19, 1999 Available at: http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_11.htm. Accessed July 27,2006.
- .Comparative tolerability of sulfonylureas in diabetes mellitus.Drug Saf.2000;22:313–320.
- ,,,.Individual sulfonylureas and serious hypoglycemia in older people.J Am Geriatr Soc.1996;44:751–755
- ,.Sulfonylureas. In:DeFronzo RA, ed.Current Management of Diabetes Mellitus.St. Louis, MO:Mosby;1998:96–101.
- ,,.Diabetes Mellitus in Pharmacotherapy: A Pathophysiologic Approach.6th ed.Dipiro JT, ed.New York:McGraw Hill;2005.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33:2778–2785.
Copyright © 2007 Society of Hospital Medicine