User login
Danielle Scheurer, MD, MSCR, SFHM, is a hospitalist and the chief quality officer at the Medical University of South Carolina (MUSC) in Charleston. She is former SHM physician advisor, an SHM blogger, and member of SHM's Education Committee. She also serves as faculty of SHM's annual meeting "ABIM Maintenance of Certification (MOC) Learning Session" pre-course. Dr. Scheurer earned her undergraduate degree at Emory University in Atlanta, graduated medical school from the University of Tennessee in Knoxville, and trained at Duke University in Durham, N.C. She has served as physician editor of The Hospitalist since 2012.
Medicare’s Readmission Reduction Program Cuts $420M to U.S. Hospitals This Year
It’s that time of year again … the time when hospitals around the country are being notified of their 30-day readmission penalties from the Centers for Medicare and Medicaid Services (CMS). Now in the fourth year of the program, many hospitals have come to dread the announcement of how much they are being penalized each year.1
This year, the readmission reduction program will decrease Medicare payments within a total of 2,592 U.S. hospitals, for a combined total of $420 million. This year’s program included readmissions from July 2011 to June 2014; the program uses a three-year rolling average for its calculations.2
The readmission program, which initially was implemented through the Affordable Care Act in 2012, aimed to penalize hospitals with higher than expected 30-day readmission rates on select conditions (currently heart attack, heart failure, pneumonia, COPD, and hip/knee replacements). Medicare estimates that it spends $17 billion a year in avoidable readmissions, which prompted the initial support for the program. For each condition, CMS calculates expected readmission rates (based on risk adjustment models that include age, severity of illness, and comorbid conditions) and observed rates, and then calculates an “excess readmission ratio” for each hospital. Based on the overall ratio, the hospital is penalized up to 3% of its Medicare payments for all inpatient stays for that fiscal year. Each year, CMS reassesses the readmission rates for hospitals and readjusts the magnitude of the penalty. The purpose of the program is to incent hospitals to invest in discharge planning and care coordination efforts and do everything possible to avoid readmissions.1
Who Gets Penalized?
This year, most eligible hospitals were penalized to some extent, and all but 209 of the hospitals that were penalized last year were penalized again.
The average Medicare payment reduction will be 0.61% per patient stay.
A total of 506 hospitals will lose at least 1% of their Medicare payments, and 38 hospitals will receive the maximum 3% penalty.
Unfortunately, safety net hospitals were about 60% more likely than other hospitals to have been penalized in all three years of the program. In addition, hospitals with the lowest profit margins were 36% more likely to be penalized than those with higher margins.
Some states were disproportionately affected, with at least three-quarters of hospitals affected in Alabama, Connecticut, Florida, Massachusetts, New Jersey, New York, Rhode Island, South Carolina, Virginia, and the District of Columbia. States that fared the best were Idaho, Iowa, Kansas, Montana, Nebraska, North Dakota, and South Dakota.
Most of the 2,232 hospitals that avoided a penalty were spared because they were exempted from the program (Veterans Affairs hospitals, children’s hospitals, critical access hospitals, or those with too few Medicare patients), not because of exceptional performance.
Does the Program Work?
Despite criticism, there is no doubt that this program has forced hospitals to pay keen attention to transitions of care and avoidable readmissions. And it does appear to be an effective strategy for CMS to achieve its goals; there has been an overall decrease in 30-day readmission rates among Medicare recipients since the program began, in all types of hospitals.
Compared to 2012, there were 100,000 fewer readmissions among Medicare beneficiaries in the U.S. in 2013. As such, there is no evidence that the program will be discontinued, although it will hopefully be altered in some key aspects.3
What the Future Holds
The program has been criticized on many fronts. For one, it recalculates a three-year rolling average each year, which makes it incredibly difficult to “wash out” older (poor) performance and get off the penalty list.
In addition, critics have pointed out that the program fails to take into account the socioeconomic background of patients when assessing readmission penalties. Many argue that social determinants of readmissions that are beyond the immediate control of a hospital system can have a huge impact on readmission rates.
The National Quality Forum is examining the impact of these factors on readmissions, but this evaluation likely will take years.
In the meantime, the Hospital Readmissions Program Accuracy and Accountability Act of 2014 has been introduced as a bill that would require CMS to factor socioeconomic status into the equation when determining readmission penalties.
What All This Means for Hospitalists
All of us working within the confines of the current program can do a few things to improve our understanding and our hospitals’ performance:
- If your hospital is one that incurred a penalty, know that most “eligible” hospitals also incurred a penalty.
- Look at how your hospital fared within your state and find out if you are above or below average in the amount.3
- Continue to focus on exemplary care transition protocols, policies, and programs within your hospital system, because the penalties are unlikely to go away and are very likely to expand over time.
- Support any advocacy efforts toward improving risk adjustment methodologies for readmissions; all hospitals are likely to benefit from more accurate risk adjustments.

References
- Centers for Medicare and Medicaid Services. Readmissions reduction program. Accessed October 3, 2015.
- Rau J. Half of nation’s hospitals fail again to escape Medicare’s readmissions penalties. August 3, 2015. Accessed October 3, 2015.
- Medpac. The hospital readmission penalty: how well is it working?. Accessed October 3, 2015.
It’s that time of year again … the time when hospitals around the country are being notified of their 30-day readmission penalties from the Centers for Medicare and Medicaid Services (CMS). Now in the fourth year of the program, many hospitals have come to dread the announcement of how much they are being penalized each year.1
This year, the readmission reduction program will decrease Medicare payments within a total of 2,592 U.S. hospitals, for a combined total of $420 million. This year’s program included readmissions from July 2011 to June 2014; the program uses a three-year rolling average for its calculations.2
The readmission program, which initially was implemented through the Affordable Care Act in 2012, aimed to penalize hospitals with higher than expected 30-day readmission rates on select conditions (currently heart attack, heart failure, pneumonia, COPD, and hip/knee replacements). Medicare estimates that it spends $17 billion a year in avoidable readmissions, which prompted the initial support for the program. For each condition, CMS calculates expected readmission rates (based on risk adjustment models that include age, severity of illness, and comorbid conditions) and observed rates, and then calculates an “excess readmission ratio” for each hospital. Based on the overall ratio, the hospital is penalized up to 3% of its Medicare payments for all inpatient stays for that fiscal year. Each year, CMS reassesses the readmission rates for hospitals and readjusts the magnitude of the penalty. The purpose of the program is to incent hospitals to invest in discharge planning and care coordination efforts and do everything possible to avoid readmissions.1
Who Gets Penalized?
This year, most eligible hospitals were penalized to some extent, and all but 209 of the hospitals that were penalized last year were penalized again.
The average Medicare payment reduction will be 0.61% per patient stay.
A total of 506 hospitals will lose at least 1% of their Medicare payments, and 38 hospitals will receive the maximum 3% penalty.
Unfortunately, safety net hospitals were about 60% more likely than other hospitals to have been penalized in all three years of the program. In addition, hospitals with the lowest profit margins were 36% more likely to be penalized than those with higher margins.
Some states were disproportionately affected, with at least three-quarters of hospitals affected in Alabama, Connecticut, Florida, Massachusetts, New Jersey, New York, Rhode Island, South Carolina, Virginia, and the District of Columbia. States that fared the best were Idaho, Iowa, Kansas, Montana, Nebraska, North Dakota, and South Dakota.
Most of the 2,232 hospitals that avoided a penalty were spared because they were exempted from the program (Veterans Affairs hospitals, children’s hospitals, critical access hospitals, or those with too few Medicare patients), not because of exceptional performance.
Does the Program Work?
Despite criticism, there is no doubt that this program has forced hospitals to pay keen attention to transitions of care and avoidable readmissions. And it does appear to be an effective strategy for CMS to achieve its goals; there has been an overall decrease in 30-day readmission rates among Medicare recipients since the program began, in all types of hospitals.
Compared to 2012, there were 100,000 fewer readmissions among Medicare beneficiaries in the U.S. in 2013. As such, there is no evidence that the program will be discontinued, although it will hopefully be altered in some key aspects.3
What the Future Holds
The program has been criticized on many fronts. For one, it recalculates a three-year rolling average each year, which makes it incredibly difficult to “wash out” older (poor) performance and get off the penalty list.
In addition, critics have pointed out that the program fails to take into account the socioeconomic background of patients when assessing readmission penalties. Many argue that social determinants of readmissions that are beyond the immediate control of a hospital system can have a huge impact on readmission rates.
The National Quality Forum is examining the impact of these factors on readmissions, but this evaluation likely will take years.
In the meantime, the Hospital Readmissions Program Accuracy and Accountability Act of 2014 has been introduced as a bill that would require CMS to factor socioeconomic status into the equation when determining readmission penalties.
What All This Means for Hospitalists
All of us working within the confines of the current program can do a few things to improve our understanding and our hospitals’ performance:
- If your hospital is one that incurred a penalty, know that most “eligible” hospitals also incurred a penalty.
- Look at how your hospital fared within your state and find out if you are above or below average in the amount.3
- Continue to focus on exemplary care transition protocols, policies, and programs within your hospital system, because the penalties are unlikely to go away and are very likely to expand over time.
- Support any advocacy efforts toward improving risk adjustment methodologies for readmissions; all hospitals are likely to benefit from more accurate risk adjustments.

References
- Centers for Medicare and Medicaid Services. Readmissions reduction program. Accessed October 3, 2015.
- Rau J. Half of nation’s hospitals fail again to escape Medicare’s readmissions penalties. August 3, 2015. Accessed October 3, 2015.
- Medpac. The hospital readmission penalty: how well is it working?. Accessed October 3, 2015.
It’s that time of year again … the time when hospitals around the country are being notified of their 30-day readmission penalties from the Centers for Medicare and Medicaid Services (CMS). Now in the fourth year of the program, many hospitals have come to dread the announcement of how much they are being penalized each year.1
This year, the readmission reduction program will decrease Medicare payments within a total of 2,592 U.S. hospitals, for a combined total of $420 million. This year’s program included readmissions from July 2011 to June 2014; the program uses a three-year rolling average for its calculations.2
The readmission program, which initially was implemented through the Affordable Care Act in 2012, aimed to penalize hospitals with higher than expected 30-day readmission rates on select conditions (currently heart attack, heart failure, pneumonia, COPD, and hip/knee replacements). Medicare estimates that it spends $17 billion a year in avoidable readmissions, which prompted the initial support for the program. For each condition, CMS calculates expected readmission rates (based on risk adjustment models that include age, severity of illness, and comorbid conditions) and observed rates, and then calculates an “excess readmission ratio” for each hospital. Based on the overall ratio, the hospital is penalized up to 3% of its Medicare payments for all inpatient stays for that fiscal year. Each year, CMS reassesses the readmission rates for hospitals and readjusts the magnitude of the penalty. The purpose of the program is to incent hospitals to invest in discharge planning and care coordination efforts and do everything possible to avoid readmissions.1
Who Gets Penalized?
This year, most eligible hospitals were penalized to some extent, and all but 209 of the hospitals that were penalized last year were penalized again.
The average Medicare payment reduction will be 0.61% per patient stay.
A total of 506 hospitals will lose at least 1% of their Medicare payments, and 38 hospitals will receive the maximum 3% penalty.
Unfortunately, safety net hospitals were about 60% more likely than other hospitals to have been penalized in all three years of the program. In addition, hospitals with the lowest profit margins were 36% more likely to be penalized than those with higher margins.
Some states were disproportionately affected, with at least three-quarters of hospitals affected in Alabama, Connecticut, Florida, Massachusetts, New Jersey, New York, Rhode Island, South Carolina, Virginia, and the District of Columbia. States that fared the best were Idaho, Iowa, Kansas, Montana, Nebraska, North Dakota, and South Dakota.
Most of the 2,232 hospitals that avoided a penalty were spared because they were exempted from the program (Veterans Affairs hospitals, children’s hospitals, critical access hospitals, or those with too few Medicare patients), not because of exceptional performance.
Does the Program Work?
Despite criticism, there is no doubt that this program has forced hospitals to pay keen attention to transitions of care and avoidable readmissions. And it does appear to be an effective strategy for CMS to achieve its goals; there has been an overall decrease in 30-day readmission rates among Medicare recipients since the program began, in all types of hospitals.
Compared to 2012, there were 100,000 fewer readmissions among Medicare beneficiaries in the U.S. in 2013. As such, there is no evidence that the program will be discontinued, although it will hopefully be altered in some key aspects.3
What the Future Holds
The program has been criticized on many fronts. For one, it recalculates a three-year rolling average each year, which makes it incredibly difficult to “wash out” older (poor) performance and get off the penalty list.
In addition, critics have pointed out that the program fails to take into account the socioeconomic background of patients when assessing readmission penalties. Many argue that social determinants of readmissions that are beyond the immediate control of a hospital system can have a huge impact on readmission rates.
The National Quality Forum is examining the impact of these factors on readmissions, but this evaluation likely will take years.
In the meantime, the Hospital Readmissions Program Accuracy and Accountability Act of 2014 has been introduced as a bill that would require CMS to factor socioeconomic status into the equation when determining readmission penalties.
What All This Means for Hospitalists
All of us working within the confines of the current program can do a few things to improve our understanding and our hospitals’ performance:
- If your hospital is one that incurred a penalty, know that most “eligible” hospitals also incurred a penalty.
- Look at how your hospital fared within your state and find out if you are above or below average in the amount.3
- Continue to focus on exemplary care transition protocols, policies, and programs within your hospital system, because the penalties are unlikely to go away and are very likely to expand over time.
- Support any advocacy efforts toward improving risk adjustment methodologies for readmissions; all hospitals are likely to benefit from more accurate risk adjustments.

References
- Centers for Medicare and Medicaid Services. Readmissions reduction program. Accessed October 3, 2015.
- Rau J. Half of nation’s hospitals fail again to escape Medicare’s readmissions penalties. August 3, 2015. Accessed October 3, 2015.
- Medpac. The hospital readmission penalty: how well is it working?. Accessed October 3, 2015.
Hospitalists’ Code of Conduct Needed for Sick Day Callouts
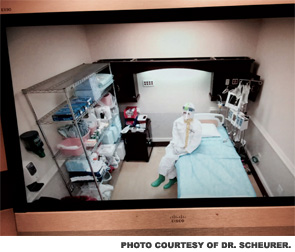
It is Tuesday morning, and I drag myself out of bed after a very restless night. It is day number three of a syndrome of fatigue, headache, and moderate productive cough. I have been on service for eight days of a two-week stretch; I am hoping to “make it to the end of the week.” I convince myself I am “not that sick” and head into work for a long day of rounds, after two cups of coffee and 600 mg of Motrin. Throughout the day, I try to hide my cough from my residents and students, and especially the nurses and my patients. I have a pocket full of cough drops and a cup of ice water at hand to stifle any coughing fits that could reveal how I actually feel. This is not the first time I have come to work only “half well.” I convince myself I am not contagious, as long as I wash my hands and control my cough. Without a fever, how could I possibly justify calling in a colleague to cover for me?
I am not alone in my psychological justifications for coming to work. A recent JAMA Pediatrics article found that 83% of clinicians admitted to coming to work while sick, while 95% admitted to knowing that it could be dangerous to their patients.1,2 The study surveyed approximately 500 attendings and 250 advanced practice providers at the Children’s Hospital of Philadelphia. A substantial minority of providers (9%) admitted to coming to work sick at least five times in the past year.
The reasons these providers gave for working in spite of being ill likely ring true with each and every hospitalist in the field: They were concerned about 1) letting down their patients or 2) hospital staffing in their absence. Most providers also expressed concern about the continuity of care for their patients in their absence. Most also admitted that they feared being ostracized by their colleagues and believed that there were unwritten but real expectations for them to work regardless of personal illness.
Historically, physicians and other healthcare providers have been widely believed to be relatively immune to mundane ailments, by themselves and by others. How incredibly rare it is to hear, “Sorry, your doctor is sick; we have to reschedule your visit.” Even when afflicted by physical impairments, physicians have long considered it more “honorable” to work through these infirmities than to resign to physical limitations and ask for help.
Misguided or Mishandled
This sense of duty starts early in medical training and continues throughout a physician’s early career. I discovered this firsthand during my internship after suffering a stress fracture in my foot. I woke up one morning with significant foot pain and swelling but hobbled through rounds without a word spoken about my limp. By the afternoon, I could hardly bear weight on my foot, so one of my fellow interns suggested I limp over to the orthopedic clinic; thankfully, they saw me the same day, diagnosed the stress fracture, and fitted me in a walking cast. The next day on rounds, when I asked my attending if we could take the elevator up the two floors to the next patient, he looked annoyed and said I could meet them there; they scurried up the stairs. For the next few weeks, I never missed a minute of work but kept trailing behind and missing key pieces of presentations and information from rounds, having to hobble back and forth to the elevator between floors.
The lesson I quickly learned back then was that if I was not “fit for duty” with any sort of physical ailment, it was clearly my problem to make up for my deficits, because the work expectations would go unchanged. Although a stress fracture did not put my patients at risk, the experience sent a strong message: Regardless of the impact on patients, it is always better to come to work than to stay home, whatever the type or degree of affliction.
The JAMA Pediatrics study did find substantial differences in the types of symptoms that would keep a provider at home: While 75% reported they would come to work with a cough and rhinorrhea, 30% would come with diarrhea, 16% would come with a fever, and only 5% would come with vomiting.
To be honest, this sounds about right in comparison to what my threshold would be, and it is about what I would accept as reasonable from a colleague. I do hope that if I were “really sick,” with fever and/or vomiting, I would have the good sense to stay home and ask for coverage, and I hope my colleagues and I would support each other in these decisions.
The study really gets at the sociocultural factors that steer physicians into making such decisions, based on the conditions for being excused that they think are socially acceptable. I suspect these are similar to those that other industries would also consider acceptable. But, of course, the difference is that workers in other industries are less likely to cause harm to large numbers of vulnerable and innocent “bystanders.” Adding to the problem, there is no good “definition” for what is “too sick”; although it is complicated and varies by person, the definition should at least take into account the level of potential contagion and risk to patients.
The authors suggest that, in order to remedy this longstanding situation, open dialogue needs to take place among physician groups to reduce the ambiguity about what is appropriate. A good start would be the generation of clear policies that restrict providers from coming to work with specifics signs/symptoms.
As hospitalists, we should all discuss the article within our groups and honestly determine in advance what our “code of conduct” should be for illnesses, based on our provider mix and our patient populations. (Decisions for ICU, medical-surgical, or oncology may vary.) This would reduce ambiguity and create new social norms about when to stay home. In addition, administrative and provider group leaders need to show strong leadership and support for such policies and ensure adequate staffing in the event of appropriate callouts. Such policies need to ensure that callouts are equitable and non-punitive. These relatively simple measures would go a long way in reducing the risk of illness among ourselves and our patients.

References
- Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: A mixed methods analysis [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0684.
- Starke JR, Jackson MA. When the health care worker is sick: primum non nocere [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0994.
It is Tuesday morning, and I drag myself out of bed after a very restless night. It is day number three of a syndrome of fatigue, headache, and moderate productive cough. I have been on service for eight days of a two-week stretch; I am hoping to “make it to the end of the week.” I convince myself I am “not that sick” and head into work for a long day of rounds, after two cups of coffee and 600 mg of Motrin. Throughout the day, I try to hide my cough from my residents and students, and especially the nurses and my patients. I have a pocket full of cough drops and a cup of ice water at hand to stifle any coughing fits that could reveal how I actually feel. This is not the first time I have come to work only “half well.” I convince myself I am not contagious, as long as I wash my hands and control my cough. Without a fever, how could I possibly justify calling in a colleague to cover for me?
I am not alone in my psychological justifications for coming to work. A recent JAMA Pediatrics article found that 83% of clinicians admitted to coming to work while sick, while 95% admitted to knowing that it could be dangerous to their patients.1,2 The study surveyed approximately 500 attendings and 250 advanced practice providers at the Children’s Hospital of Philadelphia. A substantial minority of providers (9%) admitted to coming to work sick at least five times in the past year.
The reasons these providers gave for working in spite of being ill likely ring true with each and every hospitalist in the field: They were concerned about 1) letting down their patients or 2) hospital staffing in their absence. Most providers also expressed concern about the continuity of care for their patients in their absence. Most also admitted that they feared being ostracized by their colleagues and believed that there were unwritten but real expectations for them to work regardless of personal illness.
Historically, physicians and other healthcare providers have been widely believed to be relatively immune to mundane ailments, by themselves and by others. How incredibly rare it is to hear, “Sorry, your doctor is sick; we have to reschedule your visit.” Even when afflicted by physical impairments, physicians have long considered it more “honorable” to work through these infirmities than to resign to physical limitations and ask for help.
Misguided or Mishandled
This sense of duty starts early in medical training and continues throughout a physician’s early career. I discovered this firsthand during my internship after suffering a stress fracture in my foot. I woke up one morning with significant foot pain and swelling but hobbled through rounds without a word spoken about my limp. By the afternoon, I could hardly bear weight on my foot, so one of my fellow interns suggested I limp over to the orthopedic clinic; thankfully, they saw me the same day, diagnosed the stress fracture, and fitted me in a walking cast. The next day on rounds, when I asked my attending if we could take the elevator up the two floors to the next patient, he looked annoyed and said I could meet them there; they scurried up the stairs. For the next few weeks, I never missed a minute of work but kept trailing behind and missing key pieces of presentations and information from rounds, having to hobble back and forth to the elevator between floors.
The lesson I quickly learned back then was that if I was not “fit for duty” with any sort of physical ailment, it was clearly my problem to make up for my deficits, because the work expectations would go unchanged. Although a stress fracture did not put my patients at risk, the experience sent a strong message: Regardless of the impact on patients, it is always better to come to work than to stay home, whatever the type or degree of affliction.
The JAMA Pediatrics study did find substantial differences in the types of symptoms that would keep a provider at home: While 75% reported they would come to work with a cough and rhinorrhea, 30% would come with diarrhea, 16% would come with a fever, and only 5% would come with vomiting.
To be honest, this sounds about right in comparison to what my threshold would be, and it is about what I would accept as reasonable from a colleague. I do hope that if I were “really sick,” with fever and/or vomiting, I would have the good sense to stay home and ask for coverage, and I hope my colleagues and I would support each other in these decisions.
The study really gets at the sociocultural factors that steer physicians into making such decisions, based on the conditions for being excused that they think are socially acceptable. I suspect these are similar to those that other industries would also consider acceptable. But, of course, the difference is that workers in other industries are less likely to cause harm to large numbers of vulnerable and innocent “bystanders.” Adding to the problem, there is no good “definition” for what is “too sick”; although it is complicated and varies by person, the definition should at least take into account the level of potential contagion and risk to patients.
The authors suggest that, in order to remedy this longstanding situation, open dialogue needs to take place among physician groups to reduce the ambiguity about what is appropriate. A good start would be the generation of clear policies that restrict providers from coming to work with specifics signs/symptoms.
As hospitalists, we should all discuss the article within our groups and honestly determine in advance what our “code of conduct” should be for illnesses, based on our provider mix and our patient populations. (Decisions for ICU, medical-surgical, or oncology may vary.) This would reduce ambiguity and create new social norms about when to stay home. In addition, administrative and provider group leaders need to show strong leadership and support for such policies and ensure adequate staffing in the event of appropriate callouts. Such policies need to ensure that callouts are equitable and non-punitive. These relatively simple measures would go a long way in reducing the risk of illness among ourselves and our patients.

References
- Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: A mixed methods analysis [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0684.
- Starke JR, Jackson MA. When the health care worker is sick: primum non nocere [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0994.
It is Tuesday morning, and I drag myself out of bed after a very restless night. It is day number three of a syndrome of fatigue, headache, and moderate productive cough. I have been on service for eight days of a two-week stretch; I am hoping to “make it to the end of the week.” I convince myself I am “not that sick” and head into work for a long day of rounds, after two cups of coffee and 600 mg of Motrin. Throughout the day, I try to hide my cough from my residents and students, and especially the nurses and my patients. I have a pocket full of cough drops and a cup of ice water at hand to stifle any coughing fits that could reveal how I actually feel. This is not the first time I have come to work only “half well.” I convince myself I am not contagious, as long as I wash my hands and control my cough. Without a fever, how could I possibly justify calling in a colleague to cover for me?
I am not alone in my psychological justifications for coming to work. A recent JAMA Pediatrics article found that 83% of clinicians admitted to coming to work while sick, while 95% admitted to knowing that it could be dangerous to their patients.1,2 The study surveyed approximately 500 attendings and 250 advanced practice providers at the Children’s Hospital of Philadelphia. A substantial minority of providers (9%) admitted to coming to work sick at least five times in the past year.
The reasons these providers gave for working in spite of being ill likely ring true with each and every hospitalist in the field: They were concerned about 1) letting down their patients or 2) hospital staffing in their absence. Most providers also expressed concern about the continuity of care for their patients in their absence. Most also admitted that they feared being ostracized by their colleagues and believed that there were unwritten but real expectations for them to work regardless of personal illness.
Historically, physicians and other healthcare providers have been widely believed to be relatively immune to mundane ailments, by themselves and by others. How incredibly rare it is to hear, “Sorry, your doctor is sick; we have to reschedule your visit.” Even when afflicted by physical impairments, physicians have long considered it more “honorable” to work through these infirmities than to resign to physical limitations and ask for help.
Misguided or Mishandled
This sense of duty starts early in medical training and continues throughout a physician’s early career. I discovered this firsthand during my internship after suffering a stress fracture in my foot. I woke up one morning with significant foot pain and swelling but hobbled through rounds without a word spoken about my limp. By the afternoon, I could hardly bear weight on my foot, so one of my fellow interns suggested I limp over to the orthopedic clinic; thankfully, they saw me the same day, diagnosed the stress fracture, and fitted me in a walking cast. The next day on rounds, when I asked my attending if we could take the elevator up the two floors to the next patient, he looked annoyed and said I could meet them there; they scurried up the stairs. For the next few weeks, I never missed a minute of work but kept trailing behind and missing key pieces of presentations and information from rounds, having to hobble back and forth to the elevator between floors.
The lesson I quickly learned back then was that if I was not “fit for duty” with any sort of physical ailment, it was clearly my problem to make up for my deficits, because the work expectations would go unchanged. Although a stress fracture did not put my patients at risk, the experience sent a strong message: Regardless of the impact on patients, it is always better to come to work than to stay home, whatever the type or degree of affliction.
The JAMA Pediatrics study did find substantial differences in the types of symptoms that would keep a provider at home: While 75% reported they would come to work with a cough and rhinorrhea, 30% would come with diarrhea, 16% would come with a fever, and only 5% would come with vomiting.
To be honest, this sounds about right in comparison to what my threshold would be, and it is about what I would accept as reasonable from a colleague. I do hope that if I were “really sick,” with fever and/or vomiting, I would have the good sense to stay home and ask for coverage, and I hope my colleagues and I would support each other in these decisions.
The study really gets at the sociocultural factors that steer physicians into making such decisions, based on the conditions for being excused that they think are socially acceptable. I suspect these are similar to those that other industries would also consider acceptable. But, of course, the difference is that workers in other industries are less likely to cause harm to large numbers of vulnerable and innocent “bystanders.” Adding to the problem, there is no good “definition” for what is “too sick”; although it is complicated and varies by person, the definition should at least take into account the level of potential contagion and risk to patients.
The authors suggest that, in order to remedy this longstanding situation, open dialogue needs to take place among physician groups to reduce the ambiguity about what is appropriate. A good start would be the generation of clear policies that restrict providers from coming to work with specifics signs/symptoms.
As hospitalists, we should all discuss the article within our groups and honestly determine in advance what our “code of conduct” should be for illnesses, based on our provider mix and our patient populations. (Decisions for ICU, medical-surgical, or oncology may vary.) This would reduce ambiguity and create new social norms about when to stay home. In addition, administrative and provider group leaders need to show strong leadership and support for such policies and ensure adequate staffing in the event of appropriate callouts. Such policies need to ensure that callouts are equitable and non-punitive. These relatively simple measures would go a long way in reducing the risk of illness among ourselves and our patients.

References
- Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: A mixed methods analysis [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0684.
- Starke JR, Jackson MA. When the health care worker is sick: primum non nocere [published online ahead of print July 6, 2015]. JAMA Pediatr. doi:10.1001/jamapediatrics.2015.0994.
Resident Education, Feedback, Incentives Improve Patient Satisfaction
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
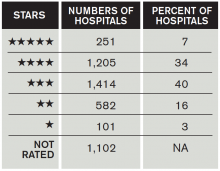
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Medical Professionalism: Its Evolution and What It Means to Hospitalists
Professionalism is an overused word in the medical industry. What exactly is meant by professionalism, and what should it mean to hospitalists? Wikipedia notes that a professional is one who earns a living from a specified activity that has standards of education and training that prepare members of the profession with the knowledge and skills necessary to perform the role required. In addition, professionals are subject to strict codes of conduct enshrining rigorous ethical and moral obligations.
Physicians are the consummate professionals; over centuries, we have been afforded the reputation of being one of the “highest-ranking” professionals within societies, along with divinity and law. We are held to very high standards, both in and out of the workplace, including arduous and rigorous standards of education and training. We are in one of the only professions that take the Hippocratic Oath at graduation. This oath requires us to swear to uphold specific ethical standards. Being a professional means we always act within our professional standards and advocate for our patients in all circumstances.1
Threats to Professionalism?
Over the past several decades, concern has been growing about a widespread decline in professionalism among physicians, a decline that extends beyond a single generation. There are many purported reasons for this erosion of professionalism; we need to first understand the threats to professionalism in order to guard against its erosion in ourselves and in the next generation of physicians.1
One major issue is that we do not have a common understanding of the nature of professionalism; the definition is both overused and misused. We often refer to professionalism by what it isn’t, rather than understanding what it is. For example, there are scores of definitions for “unprofessional” conduct in the medical industry, many of which refer to physician behaviors. These include actions that intimidate, berate, or bully others, regardless of the rationale or intent, and encompass any form of physical or psychological harm. The actions of the “disruptive physician” are often thought of as synonymous with unprofessional behavior. But professionalism is so much more than the absence of disruptive behavior. So part of the erosion of professionalism is an oversimplification of what it isn’t, rather than what it is.
Another issue with upholding professionalism over time is that many physicians forget their professional standards, because there are few “booster sessions” to remind us of why we practice medicine. Once we enter the workforce, we are confronted with so many obstacles to delivering good care to patients that we often feel overwhelmed or incapable of removing the real barriers to good care, and therefore incapable of fulfilling our mission. There are no regular “revivals” or checkpoints to refresh our memory of what we went into medicine to accomplish.
Although our ultimate goal is to take good care of patients, another threat to professionalism is that doing this often requires physicians to operate outside their “trained” knowledge and skill sets. It requires us to act on behalf of patients as an advocate in all aspects of their life, not just as a “diagnoser” or “prescriber.” As a result, maintaining the ideals of professionalism has become ever more complex, because the social determinants of health have a major impact on patient well-being and health, including access to food, housing, and transportation. Many times, diagnosing and prescribing have little impact on the patient’s outcome; these social determinants of disease take sole precedence. A patient’s education, income, and home environment have a much greater impact in determining their health outcomes than does access to prescription medications. This means that advocating for patient health and well-being extends far beyond the walls of a hospital or emergency room, a role in which most hospitalists are incapable and/or uncomfortable.1
Another major catalyst in the erosion of professionalism is the complex issue of money and income. Many physicians, including hospitalists, are “judged” by their relative value units, an indicator of the quantity and complexity of patients seen. Services not “billable” are generally delegated to others, or they go undone. Such services include communicating tirelessly with all the stakeholders in the patients’ care, including family members, primary care physicians, other physician specialists, and other disciplines. Untoward behaviors, such as “upcoding,” selecting funded patients for care, creating patient streams for highly lucrative services, and under-resourcing care provisions that “lose money”—regardless of the value to the patient—are inadvertently incentivized on individual and system levels to enhance revenue. Many hospitalists are strapped with student loans early in their careers, requiring them to earn enough to pay back these loans in a timely fashion. These perverse incentives can and often do confound our ability to act solely on behalf of our patients.2
How Do We Overcome These Threats?
The first step in reviving professionalism is to define it by what it is, not by what it isn’t. Professionalism is not the absence of bad behavior. Professionalism is the “commitment to carrying out professional responsibilities and an adherence to ethical principles.”3 Professionalism is the pursuit of the tenets of the Hippocratic Oath. As a litmus test, read and reread the oath, and honestly reflect upon your practice.
Another step is to continuously work in multidisciplinary teams, a skill that comes naturally to most hospitalists. In order to fulfill the oath, you should not work as a social worker, but you should advocate for your patients’ social work needs. You need a plethora of other disciplines to help you fulfill your role as a patient advocate. Know and respect the roles that your team members are playing, all of which are invaluable to you and your patients.
An additional step in helping you fulfill your role as a professional is to get the education and skills you need to function effectively within the complex systems in which we currently work. You should incorporate business and management education into your continuing medical education so that you can help patients traverse a system that is complex. You should know and understand the general concepts of value-based payment, insurance exchanges, federal-state-private insurances, and the basic tenets of health systems. You should know how to recognize and reduce waste and unnecessary variation in the system, and know how to measure and improve upon processes.
In the words of Emanuel Ezekiel, MD, PhD, “Learning clinical medicine is necessary for making patient well-being the physician’s primary obligation. But it is not sufficient. To promote professionalism and all that it entails (reducing errors; ensuring safe, consistent, high-quality, and convenient care; removing unnecessary services; and improving the efficiency in the delivery of services), physicians must develop better management skills … Becoming better managers will make physicians better medical professionals”.2
For those entering medical school, nine core competencies can predict success in medical school and later in practice; we should all commit to excellence in these, which go beyond clinical knowledge:
- ethical responsibility to self and others;
- reliability and dependability;
- service orientation;
- social skills;
- capacity for improvement;
- resilience and adaptability;
- cultural competence;
- oral communication; and
- teamwork.
Lastly, a critical step in preventing the erosion of professionalism in medicine is self-regulation. External regulation comes to those who refuse or are unwilling to regulate themselves. Professionalism is a set of skills that can be taught, learned, and modeled. As a new specialty, we all own the success or failure of the reputation of hospitalists as consummate professionals.1

Professionalism is an overused word in the medical industry. What exactly is meant by professionalism, and what should it mean to hospitalists? Wikipedia notes that a professional is one who earns a living from a specified activity that has standards of education and training that prepare members of the profession with the knowledge and skills necessary to perform the role required. In addition, professionals are subject to strict codes of conduct enshrining rigorous ethical and moral obligations.
Physicians are the consummate professionals; over centuries, we have been afforded the reputation of being one of the “highest-ranking” professionals within societies, along with divinity and law. We are held to very high standards, both in and out of the workplace, including arduous and rigorous standards of education and training. We are in one of the only professions that take the Hippocratic Oath at graduation. This oath requires us to swear to uphold specific ethical standards. Being a professional means we always act within our professional standards and advocate for our patients in all circumstances.1
Threats to Professionalism?
Over the past several decades, concern has been growing about a widespread decline in professionalism among physicians, a decline that extends beyond a single generation. There are many purported reasons for this erosion of professionalism; we need to first understand the threats to professionalism in order to guard against its erosion in ourselves and in the next generation of physicians.1
One major issue is that we do not have a common understanding of the nature of professionalism; the definition is both overused and misused. We often refer to professionalism by what it isn’t, rather than understanding what it is. For example, there are scores of definitions for “unprofessional” conduct in the medical industry, many of which refer to physician behaviors. These include actions that intimidate, berate, or bully others, regardless of the rationale or intent, and encompass any form of physical or psychological harm. The actions of the “disruptive physician” are often thought of as synonymous with unprofessional behavior. But professionalism is so much more than the absence of disruptive behavior. So part of the erosion of professionalism is an oversimplification of what it isn’t, rather than what it is.
Another issue with upholding professionalism over time is that many physicians forget their professional standards, because there are few “booster sessions” to remind us of why we practice medicine. Once we enter the workforce, we are confronted with so many obstacles to delivering good care to patients that we often feel overwhelmed or incapable of removing the real barriers to good care, and therefore incapable of fulfilling our mission. There are no regular “revivals” or checkpoints to refresh our memory of what we went into medicine to accomplish.
Although our ultimate goal is to take good care of patients, another threat to professionalism is that doing this often requires physicians to operate outside their “trained” knowledge and skill sets. It requires us to act on behalf of patients as an advocate in all aspects of their life, not just as a “diagnoser” or “prescriber.” As a result, maintaining the ideals of professionalism has become ever more complex, because the social determinants of health have a major impact on patient well-being and health, including access to food, housing, and transportation. Many times, diagnosing and prescribing have little impact on the patient’s outcome; these social determinants of disease take sole precedence. A patient’s education, income, and home environment have a much greater impact in determining their health outcomes than does access to prescription medications. This means that advocating for patient health and well-being extends far beyond the walls of a hospital or emergency room, a role in which most hospitalists are incapable and/or uncomfortable.1
Another major catalyst in the erosion of professionalism is the complex issue of money and income. Many physicians, including hospitalists, are “judged” by their relative value units, an indicator of the quantity and complexity of patients seen. Services not “billable” are generally delegated to others, or they go undone. Such services include communicating tirelessly with all the stakeholders in the patients’ care, including family members, primary care physicians, other physician specialists, and other disciplines. Untoward behaviors, such as “upcoding,” selecting funded patients for care, creating patient streams for highly lucrative services, and under-resourcing care provisions that “lose money”—regardless of the value to the patient—are inadvertently incentivized on individual and system levels to enhance revenue. Many hospitalists are strapped with student loans early in their careers, requiring them to earn enough to pay back these loans in a timely fashion. These perverse incentives can and often do confound our ability to act solely on behalf of our patients.2
How Do We Overcome These Threats?
The first step in reviving professionalism is to define it by what it is, not by what it isn’t. Professionalism is not the absence of bad behavior. Professionalism is the “commitment to carrying out professional responsibilities and an adherence to ethical principles.”3 Professionalism is the pursuit of the tenets of the Hippocratic Oath. As a litmus test, read and reread the oath, and honestly reflect upon your practice.
Another step is to continuously work in multidisciplinary teams, a skill that comes naturally to most hospitalists. In order to fulfill the oath, you should not work as a social worker, but you should advocate for your patients’ social work needs. You need a plethora of other disciplines to help you fulfill your role as a patient advocate. Know and respect the roles that your team members are playing, all of which are invaluable to you and your patients.
An additional step in helping you fulfill your role as a professional is to get the education and skills you need to function effectively within the complex systems in which we currently work. You should incorporate business and management education into your continuing medical education so that you can help patients traverse a system that is complex. You should know and understand the general concepts of value-based payment, insurance exchanges, federal-state-private insurances, and the basic tenets of health systems. You should know how to recognize and reduce waste and unnecessary variation in the system, and know how to measure and improve upon processes.
In the words of Emanuel Ezekiel, MD, PhD, “Learning clinical medicine is necessary for making patient well-being the physician’s primary obligation. But it is not sufficient. To promote professionalism and all that it entails (reducing errors; ensuring safe, consistent, high-quality, and convenient care; removing unnecessary services; and improving the efficiency in the delivery of services), physicians must develop better management skills … Becoming better managers will make physicians better medical professionals”.2
For those entering medical school, nine core competencies can predict success in medical school and later in practice; we should all commit to excellence in these, which go beyond clinical knowledge:
- ethical responsibility to self and others;
- reliability and dependability;
- service orientation;
- social skills;
- capacity for improvement;
- resilience and adaptability;
- cultural competence;
- oral communication; and
- teamwork.
Lastly, a critical step in preventing the erosion of professionalism in medicine is self-regulation. External regulation comes to those who refuse or are unwilling to regulate themselves. Professionalism is a set of skills that can be taught, learned, and modeled. As a new specialty, we all own the success or failure of the reputation of hospitalists as consummate professionals.1

Professionalism is an overused word in the medical industry. What exactly is meant by professionalism, and what should it mean to hospitalists? Wikipedia notes that a professional is one who earns a living from a specified activity that has standards of education and training that prepare members of the profession with the knowledge and skills necessary to perform the role required. In addition, professionals are subject to strict codes of conduct enshrining rigorous ethical and moral obligations.
Physicians are the consummate professionals; over centuries, we have been afforded the reputation of being one of the “highest-ranking” professionals within societies, along with divinity and law. We are held to very high standards, both in and out of the workplace, including arduous and rigorous standards of education and training. We are in one of the only professions that take the Hippocratic Oath at graduation. This oath requires us to swear to uphold specific ethical standards. Being a professional means we always act within our professional standards and advocate for our patients in all circumstances.1
Threats to Professionalism?
Over the past several decades, concern has been growing about a widespread decline in professionalism among physicians, a decline that extends beyond a single generation. There are many purported reasons for this erosion of professionalism; we need to first understand the threats to professionalism in order to guard against its erosion in ourselves and in the next generation of physicians.1
One major issue is that we do not have a common understanding of the nature of professionalism; the definition is both overused and misused. We often refer to professionalism by what it isn’t, rather than understanding what it is. For example, there are scores of definitions for “unprofessional” conduct in the medical industry, many of which refer to physician behaviors. These include actions that intimidate, berate, or bully others, regardless of the rationale or intent, and encompass any form of physical or psychological harm. The actions of the “disruptive physician” are often thought of as synonymous with unprofessional behavior. But professionalism is so much more than the absence of disruptive behavior. So part of the erosion of professionalism is an oversimplification of what it isn’t, rather than what it is.
Another issue with upholding professionalism over time is that many physicians forget their professional standards, because there are few “booster sessions” to remind us of why we practice medicine. Once we enter the workforce, we are confronted with so many obstacles to delivering good care to patients that we often feel overwhelmed or incapable of removing the real barriers to good care, and therefore incapable of fulfilling our mission. There are no regular “revivals” or checkpoints to refresh our memory of what we went into medicine to accomplish.
Although our ultimate goal is to take good care of patients, another threat to professionalism is that doing this often requires physicians to operate outside their “trained” knowledge and skill sets. It requires us to act on behalf of patients as an advocate in all aspects of their life, not just as a “diagnoser” or “prescriber.” As a result, maintaining the ideals of professionalism has become ever more complex, because the social determinants of health have a major impact on patient well-being and health, including access to food, housing, and transportation. Many times, diagnosing and prescribing have little impact on the patient’s outcome; these social determinants of disease take sole precedence. A patient’s education, income, and home environment have a much greater impact in determining their health outcomes than does access to prescription medications. This means that advocating for patient health and well-being extends far beyond the walls of a hospital or emergency room, a role in which most hospitalists are incapable and/or uncomfortable.1
Another major catalyst in the erosion of professionalism is the complex issue of money and income. Many physicians, including hospitalists, are “judged” by their relative value units, an indicator of the quantity and complexity of patients seen. Services not “billable” are generally delegated to others, or they go undone. Such services include communicating tirelessly with all the stakeholders in the patients’ care, including family members, primary care physicians, other physician specialists, and other disciplines. Untoward behaviors, such as “upcoding,” selecting funded patients for care, creating patient streams for highly lucrative services, and under-resourcing care provisions that “lose money”—regardless of the value to the patient—are inadvertently incentivized on individual and system levels to enhance revenue. Many hospitalists are strapped with student loans early in their careers, requiring them to earn enough to pay back these loans in a timely fashion. These perverse incentives can and often do confound our ability to act solely on behalf of our patients.2
How Do We Overcome These Threats?
The first step in reviving professionalism is to define it by what it is, not by what it isn’t. Professionalism is not the absence of bad behavior. Professionalism is the “commitment to carrying out professional responsibilities and an adherence to ethical principles.”3 Professionalism is the pursuit of the tenets of the Hippocratic Oath. As a litmus test, read and reread the oath, and honestly reflect upon your practice.
Another step is to continuously work in multidisciplinary teams, a skill that comes naturally to most hospitalists. In order to fulfill the oath, you should not work as a social worker, but you should advocate for your patients’ social work needs. You need a plethora of other disciplines to help you fulfill your role as a patient advocate. Know and respect the roles that your team members are playing, all of which are invaluable to you and your patients.
An additional step in helping you fulfill your role as a professional is to get the education and skills you need to function effectively within the complex systems in which we currently work. You should incorporate business and management education into your continuing medical education so that you can help patients traverse a system that is complex. You should know and understand the general concepts of value-based payment, insurance exchanges, federal-state-private insurances, and the basic tenets of health systems. You should know how to recognize and reduce waste and unnecessary variation in the system, and know how to measure and improve upon processes.
In the words of Emanuel Ezekiel, MD, PhD, “Learning clinical medicine is necessary for making patient well-being the physician’s primary obligation. But it is not sufficient. To promote professionalism and all that it entails (reducing errors; ensuring safe, consistent, high-quality, and convenient care; removing unnecessary services; and improving the efficiency in the delivery of services), physicians must develop better management skills … Becoming better managers will make physicians better medical professionals”.2
For those entering medical school, nine core competencies can predict success in medical school and later in practice; we should all commit to excellence in these, which go beyond clinical knowledge:
- ethical responsibility to self and others;
- reliability and dependability;
- service orientation;
- social skills;
- capacity for improvement;
- resilience and adaptability;
- cultural competence;
- oral communication; and
- teamwork.
Lastly, a critical step in preventing the erosion of professionalism in medicine is self-regulation. External regulation comes to those who refuse or are unwilling to regulate themselves. Professionalism is a set of skills that can be taught, learned, and modeled. As a new specialty, we all own the success or failure of the reputation of hospitalists as consummate professionals.1

Hospitalists Should Embrace Advances, Transparency in Health Record Technology
We are definitely in the era of data access and transparency. These days you can find information on anything and everything within a matter of seconds. You can become a subject matter expert on any topic within a matter of hours: music, cooking, foreign language, weather, travel. The possibilities are endless. That is, unless you want information on yourself—specifically, medical information.
Despite all of our advances in technology in the information era, many patients still find it extremely difficult and frustrating to gain full and transparent access to their medical records. Electronic health records (EHRs) have made it easier than ever for practitioners to find information about their patients, including pharmacy and access queries to determine what medications they are (or are not) taking, and where they have recently accessed care. But EHRs have not been widely utilized as a tool to grant extensive, real-time access to patients.
But change is afoot. Both providers and patients are now realizing the value of offering patients more open access to their medical records. Many organizations with EHRs have created patient portals, where patients can access limited portions of their medical records such as medications and allergies, can request items such as prescription refills or appointments, and can ask their providers about their care. Some medical centers are participating in OpenNotes initiatives, which give patients direct access to provider notes within the medical record.
Although these patient portals are a great first step in transparency and engagement, the information granted to patients is limited in content and timeliness. Generally, such items as test results must first be “released” by a provider before they can be viewed by the patient; some organizations have set restrictions, determining that some tests cannot be released at all (i.e., abnormal pathology or HIV test results). The rationale for such restrictions is to prevent patients from finding out sensitive information from a web page; many assume that the patient would be much better off finding out such information from a provider than a computer, and that well may be true, if the information is available in a timely fashion and is shared by a provider who can relay the information better than a computer.
Barriers Aplenty
The medical industry still has a long way to go to realize full medical record transparency for patients. One legitimate barrier is that medical records were never intended for patient view or use. Most do not read like a story; they read more like a ledger, full of medical jargon and text boxes in illogical order. This is primarily due to the fact that EHRs were designed for regulatory and billing purposes, not to eloquently—or even adequately—summarize what the patient is (or was) experiencing.
Another major barrier is that the information in the medical record is often difficult to find, and the record itself is difficult to maneuver. Experienced and trained providers, even those who have dutifully completed medical training, often find it challenging to locate exactly what they are looking for. The burden would be on the patient to learn, understand, and navigate the medical record, and few would likely undertake such a challenge.
There also are legitimate cultural barriers among providers, who will resist giving patients carte blanche access to the EHR; many providers cite concerns that if they honestly summarize sensitive information in the medical record (i.e., social habits or medication compliance issues), patients may be angered, with resultant loss of trust, retaliation, or legal action.
Clear the Hurdles, and Next Steps
There is a great story about how well medical record transparency can work, summarized in a New York Times article a few months ago.1 The story tells of 26-year-old Steven Keating, who had a “slight abnormality” on a brain CT that was done in 2007 as part of a study he had volunteered for.2 Although reassured by a “normal” follow-up scan in 2010, Keating was inquisitive, wanting to understand everything about his condition, and read voraciously about what his initial brain scan could mean. He knew the initial abnormality was near his olfactory nerve, so in 2014, when he started intermittently smelling vinegar, he suspected it might be related to the abnormality noted in his initial scan.
He sought immediate care and follow-up imaging, which showed a very large mass. Within weeks, this large astrocytoma was successfully removed; surgery was followed by chemotherapy and radiation.
Over the course of Keating’s care, he amassed more than 70 gigabytes of medical information about himself, including 10 hours of video footage from his initial surgery. Throughout the course of his illness, he remained eager to obtain all facets of his medical information, including such videos and scans, and considered these pieces of information critical to his healing process. He found that, in general, when he asked doctors to share information, he was usually granted access to what he wanted and needed, but the onus was always on him to ask. At one point he asked, “How come there isn’t a ‘share’ button at the hospital?”
Steven now has an entire website dedicated to his personal healthcare story, coupled with a passionate plea to enhance open access to medical records.2 He writes: “I have become passionate about open-sourcing the data and how we can learn through sharing. … Patients can collect their own data and they should be able to share it, amongst patients, communities, and to benefit science if desired. Healthcare should be a two-way road, patients alongside doctors and researchers as a team. The future will be driven by networked healthcare, support communities, and, I believe, patient curiosity.”
Steven was able to cobble together his medical record better than most others could, as he definitely has some advantages over many other patients; he is young, articulate, bright, and highly educated. It would be much more difficult for an older, less well educated, or disenfranchised patient to accomplish this level of understanding of and engagement in the current system. “The person with the least access to data in the system is the patient,” he writes on his website. “You can get it, but the burden is always on the patient. And it is scattered across many different silos of patient data.”
Providers and patients alike should insist on more transparency, coupled with better and more streamlined communication. As patients become more agile at maneuvering through the web portals and more engaged in their care, patients and providers gain innumerable advantages. Patients could help to find any and all medical record information that is incorrect or inconsistent, working to ensure the accuracy of the content—and get rid of “chart lore.” They could fill in missing content and update information between visits, such as changes to their social history or demographics. This is all very good timing, given the recent shift to pay for performance and population health; as financial incentives are veering away from fee for service, it is becoming more profitable to help patients stay well than to keep them sick.
As hospitalists, we should look forward to these advances in technology to enhance access to information for ourselves and for our patients. We should seek out mechanisms within our organization to enhance the speed at which open access for patients is granted, to improve patient engagement throughout the spectrum of their care.

References
- Lohr S. The healing power of your own medical records. March 31, 2015. The New York Times website.. Accessed June 1, 2015.
- Keating S. Steven Keating homepage. Accessed June 1, 2015.
We are definitely in the era of data access and transparency. These days you can find information on anything and everything within a matter of seconds. You can become a subject matter expert on any topic within a matter of hours: music, cooking, foreign language, weather, travel. The possibilities are endless. That is, unless you want information on yourself—specifically, medical information.
Despite all of our advances in technology in the information era, many patients still find it extremely difficult and frustrating to gain full and transparent access to their medical records. Electronic health records (EHRs) have made it easier than ever for practitioners to find information about their patients, including pharmacy and access queries to determine what medications they are (or are not) taking, and where they have recently accessed care. But EHRs have not been widely utilized as a tool to grant extensive, real-time access to patients.
But change is afoot. Both providers and patients are now realizing the value of offering patients more open access to their medical records. Many organizations with EHRs have created patient portals, where patients can access limited portions of their medical records such as medications and allergies, can request items such as prescription refills or appointments, and can ask their providers about their care. Some medical centers are participating in OpenNotes initiatives, which give patients direct access to provider notes within the medical record.
Although these patient portals are a great first step in transparency and engagement, the information granted to patients is limited in content and timeliness. Generally, such items as test results must first be “released” by a provider before they can be viewed by the patient; some organizations have set restrictions, determining that some tests cannot be released at all (i.e., abnormal pathology or HIV test results). The rationale for such restrictions is to prevent patients from finding out sensitive information from a web page; many assume that the patient would be much better off finding out such information from a provider than a computer, and that well may be true, if the information is available in a timely fashion and is shared by a provider who can relay the information better than a computer.
Barriers Aplenty
The medical industry still has a long way to go to realize full medical record transparency for patients. One legitimate barrier is that medical records were never intended for patient view or use. Most do not read like a story; they read more like a ledger, full of medical jargon and text boxes in illogical order. This is primarily due to the fact that EHRs were designed for regulatory and billing purposes, not to eloquently—or even adequately—summarize what the patient is (or was) experiencing.
Another major barrier is that the information in the medical record is often difficult to find, and the record itself is difficult to maneuver. Experienced and trained providers, even those who have dutifully completed medical training, often find it challenging to locate exactly what they are looking for. The burden would be on the patient to learn, understand, and navigate the medical record, and few would likely undertake such a challenge.
There also are legitimate cultural barriers among providers, who will resist giving patients carte blanche access to the EHR; many providers cite concerns that if they honestly summarize sensitive information in the medical record (i.e., social habits or medication compliance issues), patients may be angered, with resultant loss of trust, retaliation, or legal action.
Clear the Hurdles, and Next Steps
There is a great story about how well medical record transparency can work, summarized in a New York Times article a few months ago.1 The story tells of 26-year-old Steven Keating, who had a “slight abnormality” on a brain CT that was done in 2007 as part of a study he had volunteered for.2 Although reassured by a “normal” follow-up scan in 2010, Keating was inquisitive, wanting to understand everything about his condition, and read voraciously about what his initial brain scan could mean. He knew the initial abnormality was near his olfactory nerve, so in 2014, when he started intermittently smelling vinegar, he suspected it might be related to the abnormality noted in his initial scan.
He sought immediate care and follow-up imaging, which showed a very large mass. Within weeks, this large astrocytoma was successfully removed; surgery was followed by chemotherapy and radiation.
Over the course of Keating’s care, he amassed more than 70 gigabytes of medical information about himself, including 10 hours of video footage from his initial surgery. Throughout the course of his illness, he remained eager to obtain all facets of his medical information, including such videos and scans, and considered these pieces of information critical to his healing process. He found that, in general, when he asked doctors to share information, he was usually granted access to what he wanted and needed, but the onus was always on him to ask. At one point he asked, “How come there isn’t a ‘share’ button at the hospital?”
Steven now has an entire website dedicated to his personal healthcare story, coupled with a passionate plea to enhance open access to medical records.2 He writes: “I have become passionate about open-sourcing the data and how we can learn through sharing. … Patients can collect their own data and they should be able to share it, amongst patients, communities, and to benefit science if desired. Healthcare should be a two-way road, patients alongside doctors and researchers as a team. The future will be driven by networked healthcare, support communities, and, I believe, patient curiosity.”
Steven was able to cobble together his medical record better than most others could, as he definitely has some advantages over many other patients; he is young, articulate, bright, and highly educated. It would be much more difficult for an older, less well educated, or disenfranchised patient to accomplish this level of understanding of and engagement in the current system. “The person with the least access to data in the system is the patient,” he writes on his website. “You can get it, but the burden is always on the patient. And it is scattered across many different silos of patient data.”
Providers and patients alike should insist on more transparency, coupled with better and more streamlined communication. As patients become more agile at maneuvering through the web portals and more engaged in their care, patients and providers gain innumerable advantages. Patients could help to find any and all medical record information that is incorrect or inconsistent, working to ensure the accuracy of the content—and get rid of “chart lore.” They could fill in missing content and update information between visits, such as changes to their social history or demographics. This is all very good timing, given the recent shift to pay for performance and population health; as financial incentives are veering away from fee for service, it is becoming more profitable to help patients stay well than to keep them sick.
As hospitalists, we should look forward to these advances in technology to enhance access to information for ourselves and for our patients. We should seek out mechanisms within our organization to enhance the speed at which open access for patients is granted, to improve patient engagement throughout the spectrum of their care.

References
- Lohr S. The healing power of your own medical records. March 31, 2015. The New York Times website.. Accessed June 1, 2015.
- Keating S. Steven Keating homepage. Accessed June 1, 2015.
We are definitely in the era of data access and transparency. These days you can find information on anything and everything within a matter of seconds. You can become a subject matter expert on any topic within a matter of hours: music, cooking, foreign language, weather, travel. The possibilities are endless. That is, unless you want information on yourself—specifically, medical information.
Despite all of our advances in technology in the information era, many patients still find it extremely difficult and frustrating to gain full and transparent access to their medical records. Electronic health records (EHRs) have made it easier than ever for practitioners to find information about their patients, including pharmacy and access queries to determine what medications they are (or are not) taking, and where they have recently accessed care. But EHRs have not been widely utilized as a tool to grant extensive, real-time access to patients.
But change is afoot. Both providers and patients are now realizing the value of offering patients more open access to their medical records. Many organizations with EHRs have created patient portals, where patients can access limited portions of their medical records such as medications and allergies, can request items such as prescription refills or appointments, and can ask their providers about their care. Some medical centers are participating in OpenNotes initiatives, which give patients direct access to provider notes within the medical record.
Although these patient portals are a great first step in transparency and engagement, the information granted to patients is limited in content and timeliness. Generally, such items as test results must first be “released” by a provider before they can be viewed by the patient; some organizations have set restrictions, determining that some tests cannot be released at all (i.e., abnormal pathology or HIV test results). The rationale for such restrictions is to prevent patients from finding out sensitive information from a web page; many assume that the patient would be much better off finding out such information from a provider than a computer, and that well may be true, if the information is available in a timely fashion and is shared by a provider who can relay the information better than a computer.
Barriers Aplenty
The medical industry still has a long way to go to realize full medical record transparency for patients. One legitimate barrier is that medical records were never intended for patient view or use. Most do not read like a story; they read more like a ledger, full of medical jargon and text boxes in illogical order. This is primarily due to the fact that EHRs were designed for regulatory and billing purposes, not to eloquently—or even adequately—summarize what the patient is (or was) experiencing.
Another major barrier is that the information in the medical record is often difficult to find, and the record itself is difficult to maneuver. Experienced and trained providers, even those who have dutifully completed medical training, often find it challenging to locate exactly what they are looking for. The burden would be on the patient to learn, understand, and navigate the medical record, and few would likely undertake such a challenge.
There also are legitimate cultural barriers among providers, who will resist giving patients carte blanche access to the EHR; many providers cite concerns that if they honestly summarize sensitive information in the medical record (i.e., social habits or medication compliance issues), patients may be angered, with resultant loss of trust, retaliation, or legal action.
Clear the Hurdles, and Next Steps
There is a great story about how well medical record transparency can work, summarized in a New York Times article a few months ago.1 The story tells of 26-year-old Steven Keating, who had a “slight abnormality” on a brain CT that was done in 2007 as part of a study he had volunteered for.2 Although reassured by a “normal” follow-up scan in 2010, Keating was inquisitive, wanting to understand everything about his condition, and read voraciously about what his initial brain scan could mean. He knew the initial abnormality was near his olfactory nerve, so in 2014, when he started intermittently smelling vinegar, he suspected it might be related to the abnormality noted in his initial scan.
He sought immediate care and follow-up imaging, which showed a very large mass. Within weeks, this large astrocytoma was successfully removed; surgery was followed by chemotherapy and radiation.
Over the course of Keating’s care, he amassed more than 70 gigabytes of medical information about himself, including 10 hours of video footage from his initial surgery. Throughout the course of his illness, he remained eager to obtain all facets of his medical information, including such videos and scans, and considered these pieces of information critical to his healing process. He found that, in general, when he asked doctors to share information, he was usually granted access to what he wanted and needed, but the onus was always on him to ask. At one point he asked, “How come there isn’t a ‘share’ button at the hospital?”
Steven now has an entire website dedicated to his personal healthcare story, coupled with a passionate plea to enhance open access to medical records.2 He writes: “I have become passionate about open-sourcing the data and how we can learn through sharing. … Patients can collect their own data and they should be able to share it, amongst patients, communities, and to benefit science if desired. Healthcare should be a two-way road, patients alongside doctors and researchers as a team. The future will be driven by networked healthcare, support communities, and, I believe, patient curiosity.”
Steven was able to cobble together his medical record better than most others could, as he definitely has some advantages over many other patients; he is young, articulate, bright, and highly educated. It would be much more difficult for an older, less well educated, or disenfranchised patient to accomplish this level of understanding of and engagement in the current system. “The person with the least access to data in the system is the patient,” he writes on his website. “You can get it, but the burden is always on the patient. And it is scattered across many different silos of patient data.”
Providers and patients alike should insist on more transparency, coupled with better and more streamlined communication. As patients become more agile at maneuvering through the web portals and more engaged in their care, patients and providers gain innumerable advantages. Patients could help to find any and all medical record information that is incorrect or inconsistent, working to ensure the accuracy of the content—and get rid of “chart lore.” They could fill in missing content and update information between visits, such as changes to their social history or demographics. This is all very good timing, given the recent shift to pay for performance and population health; as financial incentives are veering away from fee for service, it is becoming more profitable to help patients stay well than to keep them sick.
As hospitalists, we should look forward to these advances in technology to enhance access to information for ourselves and for our patients. We should seek out mechanisms within our organization to enhance the speed at which open access for patients is granted, to improve patient engagement throughout the spectrum of their care.

References
- Lohr S. The healing power of your own medical records. March 31, 2015. The New York Times website.. Accessed June 1, 2015.
- Keating S. Steven Keating homepage. Accessed June 1, 2015.
Hospitalists Should Make Commitment to Improve Healthcare Safety
Peter Pronovost, MD, PhD, FCCM, knows how to deliver a great talk. It is no wonder he is highly sought after and was asked to speak at the plenary for SHM’s annual meeting. Dr. Pronovost, also known as the “Checklist Doctor,” knows how to combine just the right amount of sadness, inspiration, and humor to make his audience feel motivated and compelled to DO something. And, in fact, he implores you—DO something.
Most of us feel excited and inspired during the annual meeting. But those feelings serve little purpose unless we translate them into actions that will make the medical industry a better place for clinicians to work and for patients to receive care. As Dr. Pronovost said, “We are the only hope that the healthcare system has of improving quality and safety.”
He was inspired years ago by the watershed event that will forever be imprinted upon Johns Hopkins Hospital in Baltimore, the preventable death of 18-month-old Josie King on Feb. 22, 2001. Years after the event, her mother, Sorrel King, a passionate patient safety advocate, wanted to know if hospitals are any safer than they were the day that Josie died. She wanted to know what patient safety experts at Hopkins had done to ensure there would not be another Josie King story.
Patients and their families consistently voice similar desires after they have suffered preventable harm. They want to know what happened, why it happened, what it means for them, and what will be done to prevent it from happening again.1 The latter question is one I am frequently asked by patients and their families at my hospital. “What are you going to do to make sure this does not happen again?”
I would venture to guess most hospitalists have been responsible for some type of preventable patient harm during their careers. We work in complex, high-volume, unpredictable, and continuously changing environments. Many of the patients and families in our care are new to us and are with us for only short periods of time. Those of us who have been responsible for preventable patient harm know that it is an unforgettable moment in time that can weigh upon your conscious. And, of course, we all want to do something to make sure it does not happen again.
That is exactly what patients and their families expect of all of us—to DO something—and they should.
But this can be an overwhelming responsibility, especially when the root causes of harm are difficult either to identify or to fix—such as a miscommunication, a diagnostic error, or an inadequate handoff.
Which gets me back to Dr. Pronovost giving a great talk. His appeal to our audience of about 3,000 hospitalists was to DO something. To make the healthcare system improve quality and safety for future patients. To not wait until we or our colleagues are involved in a preventable harm event. To do something, anything, now, that contributes to safer care, today and every day going forward.
He ended his talk with “I will….” Dr. Pronovost (and I would venture to guess patients and their families) wants each of us to fill in the blank with a statement of personal accountability for action. Unfortunately, many of us still believe that we are personally unable to make complex systems safer for patients. Many of us still believe that patients and the systems they traverse are too complex, unpredictable, unreliable, or noncompliant.
The truth is, patients and systems are indeed complex, unpredictable, unreliable, and noncompliant. The further truth is, the only way to make care safer is for each of us to start with a collective shared mental model that we can make it better—and for each of us to commit to personal accountability for action.
My “I Will”
So, while I really enjoyed Dr. Pronovost’s talk, what I enjoyed even more was reading the section in last month’s edition of The Hospitalist in which about a half dozen hospitalists interviewed after the plenary accepted the challenge of filling in the blank “I will….” A few excerpts:
- “I will let them know that everything is possible…”
- “I will improve healthcare…”
- “[I will] make sure the patient is heard…”
By a simple proclamation of personal accountability, a mere thousand hospitalists attending an annual meeting can collectively and progressively change the safety of healthcare in thousands of hospitals around the country. It starts with thinking we can do it and publicly committing to the journey. Although we are still a relatively new specialty, we have permeated almost every hospital in the country, and we have outpaced the growth of any specialty in the history of modern medicine. We are perfectly poised to be the safety change agents for every hospital system. As Margaret Meade famously said, “Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has….”
So don’t delay. Whether or not you had the good fortune of being inspired at the SHM annual meeting, each of us owes it to our patients to commit to improving the safety of healthcare and paving the future of hospital care. Get out your pen, craft a commitment now, follow through with it, and make hospitals safer tomorrow than they were yesterday.
I will…

Reference
- Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA. 2003;289(8):1001-1007.
Peter Pronovost, MD, PhD, FCCM, knows how to deliver a great talk. It is no wonder he is highly sought after and was asked to speak at the plenary for SHM’s annual meeting. Dr. Pronovost, also known as the “Checklist Doctor,” knows how to combine just the right amount of sadness, inspiration, and humor to make his audience feel motivated and compelled to DO something. And, in fact, he implores you—DO something.
Most of us feel excited and inspired during the annual meeting. But those feelings serve little purpose unless we translate them into actions that will make the medical industry a better place for clinicians to work and for patients to receive care. As Dr. Pronovost said, “We are the only hope that the healthcare system has of improving quality and safety.”
He was inspired years ago by the watershed event that will forever be imprinted upon Johns Hopkins Hospital in Baltimore, the preventable death of 18-month-old Josie King on Feb. 22, 2001. Years after the event, her mother, Sorrel King, a passionate patient safety advocate, wanted to know if hospitals are any safer than they were the day that Josie died. She wanted to know what patient safety experts at Hopkins had done to ensure there would not be another Josie King story.
Patients and their families consistently voice similar desires after they have suffered preventable harm. They want to know what happened, why it happened, what it means for them, and what will be done to prevent it from happening again.1 The latter question is one I am frequently asked by patients and their families at my hospital. “What are you going to do to make sure this does not happen again?”
I would venture to guess most hospitalists have been responsible for some type of preventable patient harm during their careers. We work in complex, high-volume, unpredictable, and continuously changing environments. Many of the patients and families in our care are new to us and are with us for only short periods of time. Those of us who have been responsible for preventable patient harm know that it is an unforgettable moment in time that can weigh upon your conscious. And, of course, we all want to do something to make sure it does not happen again.
That is exactly what patients and their families expect of all of us—to DO something—and they should.
But this can be an overwhelming responsibility, especially when the root causes of harm are difficult either to identify or to fix—such as a miscommunication, a diagnostic error, or an inadequate handoff.
Which gets me back to Dr. Pronovost giving a great talk. His appeal to our audience of about 3,000 hospitalists was to DO something. To make the healthcare system improve quality and safety for future patients. To not wait until we or our colleagues are involved in a preventable harm event. To do something, anything, now, that contributes to safer care, today and every day going forward.
He ended his talk with “I will….” Dr. Pronovost (and I would venture to guess patients and their families) wants each of us to fill in the blank with a statement of personal accountability for action. Unfortunately, many of us still believe that we are personally unable to make complex systems safer for patients. Many of us still believe that patients and the systems they traverse are too complex, unpredictable, unreliable, or noncompliant.
The truth is, patients and systems are indeed complex, unpredictable, unreliable, and noncompliant. The further truth is, the only way to make care safer is for each of us to start with a collective shared mental model that we can make it better—and for each of us to commit to personal accountability for action.
My “I Will”
So, while I really enjoyed Dr. Pronovost’s talk, what I enjoyed even more was reading the section in last month’s edition of The Hospitalist in which about a half dozen hospitalists interviewed after the plenary accepted the challenge of filling in the blank “I will….” A few excerpts:
- “I will let them know that everything is possible…”
- “I will improve healthcare…”
- “[I will] make sure the patient is heard…”
By a simple proclamation of personal accountability, a mere thousand hospitalists attending an annual meeting can collectively and progressively change the safety of healthcare in thousands of hospitals around the country. It starts with thinking we can do it and publicly committing to the journey. Although we are still a relatively new specialty, we have permeated almost every hospital in the country, and we have outpaced the growth of any specialty in the history of modern medicine. We are perfectly poised to be the safety change agents for every hospital system. As Margaret Meade famously said, “Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has….”
So don’t delay. Whether or not you had the good fortune of being inspired at the SHM annual meeting, each of us owes it to our patients to commit to improving the safety of healthcare and paving the future of hospital care. Get out your pen, craft a commitment now, follow through with it, and make hospitals safer tomorrow than they were yesterday.
I will…

Reference
- Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA. 2003;289(8):1001-1007.
Peter Pronovost, MD, PhD, FCCM, knows how to deliver a great talk. It is no wonder he is highly sought after and was asked to speak at the plenary for SHM’s annual meeting. Dr. Pronovost, also known as the “Checklist Doctor,” knows how to combine just the right amount of sadness, inspiration, and humor to make his audience feel motivated and compelled to DO something. And, in fact, he implores you—DO something.
Most of us feel excited and inspired during the annual meeting. But those feelings serve little purpose unless we translate them into actions that will make the medical industry a better place for clinicians to work and for patients to receive care. As Dr. Pronovost said, “We are the only hope that the healthcare system has of improving quality and safety.”
He was inspired years ago by the watershed event that will forever be imprinted upon Johns Hopkins Hospital in Baltimore, the preventable death of 18-month-old Josie King on Feb. 22, 2001. Years after the event, her mother, Sorrel King, a passionate patient safety advocate, wanted to know if hospitals are any safer than they were the day that Josie died. She wanted to know what patient safety experts at Hopkins had done to ensure there would not be another Josie King story.
Patients and their families consistently voice similar desires after they have suffered preventable harm. They want to know what happened, why it happened, what it means for them, and what will be done to prevent it from happening again.1 The latter question is one I am frequently asked by patients and their families at my hospital. “What are you going to do to make sure this does not happen again?”
I would venture to guess most hospitalists have been responsible for some type of preventable patient harm during their careers. We work in complex, high-volume, unpredictable, and continuously changing environments. Many of the patients and families in our care are new to us and are with us for only short periods of time. Those of us who have been responsible for preventable patient harm know that it is an unforgettable moment in time that can weigh upon your conscious. And, of course, we all want to do something to make sure it does not happen again.
That is exactly what patients and their families expect of all of us—to DO something—and they should.
But this can be an overwhelming responsibility, especially when the root causes of harm are difficult either to identify or to fix—such as a miscommunication, a diagnostic error, or an inadequate handoff.
Which gets me back to Dr. Pronovost giving a great talk. His appeal to our audience of about 3,000 hospitalists was to DO something. To make the healthcare system improve quality and safety for future patients. To not wait until we or our colleagues are involved in a preventable harm event. To do something, anything, now, that contributes to safer care, today and every day going forward.
He ended his talk with “I will….” Dr. Pronovost (and I would venture to guess patients and their families) wants each of us to fill in the blank with a statement of personal accountability for action. Unfortunately, many of us still believe that we are personally unable to make complex systems safer for patients. Many of us still believe that patients and the systems they traverse are too complex, unpredictable, unreliable, or noncompliant.
The truth is, patients and systems are indeed complex, unpredictable, unreliable, and noncompliant. The further truth is, the only way to make care safer is for each of us to start with a collective shared mental model that we can make it better—and for each of us to commit to personal accountability for action.
My “I Will”
So, while I really enjoyed Dr. Pronovost’s talk, what I enjoyed even more was reading the section in last month’s edition of The Hospitalist in which about a half dozen hospitalists interviewed after the plenary accepted the challenge of filling in the blank “I will….” A few excerpts:
- “I will let them know that everything is possible…”
- “I will improve healthcare…”
- “[I will] make sure the patient is heard…”
By a simple proclamation of personal accountability, a mere thousand hospitalists attending an annual meeting can collectively and progressively change the safety of healthcare in thousands of hospitals around the country. It starts with thinking we can do it and publicly committing to the journey. Although we are still a relatively new specialty, we have permeated almost every hospital in the country, and we have outpaced the growth of any specialty in the history of modern medicine. We are perfectly poised to be the safety change agents for every hospital system. As Margaret Meade famously said, “Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has….”
So don’t delay. Whether or not you had the good fortune of being inspired at the SHM annual meeting, each of us owes it to our patients to commit to improving the safety of healthcare and paving the future of hospital care. Get out your pen, craft a commitment now, follow through with it, and make hospitals safer tomorrow than they were yesterday.
I will…

Reference
- Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA. 2003;289(8):1001-1007.
Why Compassion in Patient Care Should Matter to Hospitalists
Hospitalists care for a variety of different types of patients, serving anyone and everyone in need of acute care. Because of the nature of our work, it is difficult to maintain empathy and compassion for all of our patients, especially in light of our unpredictable workload, long hours, and high stress. As such, all hospitalists need to be aware of what exactly compassion is, why it matters, and what we can do to guard against its natural erosion.
What Is Compassion? What Is Empathy?
Wikipedia defines compassion as “the emotion that one feels in response to the suffering of others that motivates a desire to help.” The Latin derivation of compassion is “co-suffering.” Empathy is the ability to see and understand another’s suffering. So compassion is more than just empathy or “co-suffering”; with compassion comes yearning and a motivation to alleviate suffering in others.
Many important pieces within the definition of compassion need more explanation. Notice the three distinct “parts” of the definition: “the emotion that one feels”… “in response to the suffering of others”…“that motivates a desire to help.”
The first part outlines the fact that we have to be willing and able to conjure up an emotion toward and with our patients. Although this may sound basic, some physicians purposefully guard themselves against forming emotional responses toward or with their patients. Some actually think it will make them better—and more “objective”—providers if they guard against the (potentially) painful burden of sharing such empathic emotions.
Social science research has found that providers’ concerns about becoming emotionally exhausted might lead them to reduce their compassion for entire groups of patients, such as mentally ill or drug-addicted patient populations. There is also evidence that your ability to have empathy or compassion for another correlates with the ability to picture yourself with the same issue the patient suffers. This causes a major obstacle for many providers, who find themselves unable to relate to patients with “self-inflicted” issues, such as habits that increase the likelihood of disease (e.g. smoking) or not participating in habits that decrease the likelihood of disease or successful treatments (e.g. not exercising or not taking medications correctly).
Providers are more likely to be compassionate toward patients with whom they can identify; I would have enormous compassion for a 43-year-old female with new-onset ovarian cancer but would have less compassion for a 43-year-old male with new-onset alcohol withdrawal seizures.
The second part of the definition brings up the need to acknowledge suffering, in whatever form it takes. When we think of suffering, we often connect the idea with physical pain. But there are innumerable forms of nonphysical human suffering, including psychological and social trauma; this includes the anxiety that arises from known and unknown diagnoses and treatments and the emotional exhaustion resulting from such diagnoses and treatments. We need to be able to acknowledge all forms of suffering, not just physical suffering.
The last part of the definition shows that after we have allowed ourselves to “feel” the emotion of others and to acknowledge all walks of suffering, we then need to be motivated to help. For a hospitalist, this would mean “going the extra mile” for patients, such as continuously checking and rechecking on how treatments are (or are not) working, keeping the patient and family informed (in their terms) about what is happening, or ensuring that transitions of care (to other services or in/out of the hospital) are done with keen attention to reduce the risk of “voltage drops” in information.
Two videos help illustrate the nature of compassion (see the video sidebar for URLs). Both depict young women who have been called upon to sing the national anthem before a large crowd at an athletic gathering. Both women are clearly excellent singers, and both have a similar outcome in mind: to sing the national anthem in a manner pleasing to everyone in the crowd. In both cases, they forgot the words of the song.
In the first scenario, the woman is heckled, literally “booed,” then quickly shuffled off the ice rink after falling backwards on the ice. In the second scenario, a similarly talented young woman starts out strong, then forgets the words. An unrelated gentleman comes to her aid, puts his arm around her, and sings the words with her. As he continues, he looks to the audience, making hand signals to encourage them to join in supporting her during this presumably highly anxious moment.
The second scenario exemplifies all three components of compassion: The gentleman feels the singer’s anxiety, he acknowledges her “suffering,” and he is motivated to help. What I noticed about his assistance is that he is not even a very good singer! But his kind persuasion and ability to motivate the entire crowd in assisting her remarkably transform the outcome for both the singer and the crowd.
Though both scenarios start quite similarly, they end remarkably differently; the second scenario was completely changed by the compassion of a single person and a simple act of human kindness.
Why It Matters, and How to Build It
As depicted in these short videos, compassion can completely change outcomes. You will not find placebo-controlled randomized trials to support what I just stated. But there are plenty of social science studies to support the notion that compassion is a learned trait that can be improved or eroded over time, depending on the willingness of the person to try.
Compassion is a learned behavior. It is not a personality trait that you either have or you don’t. It is a set of behaviors and actions that can be learned and practiced, and even perfected, for those willing.
The Cleveland Clinic has created several videos (see video info box) that help us consider how to think about the nature of compassion and how to learn and practice it. A hospital is ripe with emotion in all areas, from the elevators to the hallways to the cafeteria. Due to the nature of our work, we are all at risk of compassion erosion toward our patients.
We first have to acknowledge such a risk is present and actively seek out opportunities, as depicted in these videos, to learn and practice compassion. As the Dalai Lama once said, “Compassion is a necessity, not a luxury.” We should all learn, demonstrate, and live compassion as a necessity in our practice.

Hospitalists care for a variety of different types of patients, serving anyone and everyone in need of acute care. Because of the nature of our work, it is difficult to maintain empathy and compassion for all of our patients, especially in light of our unpredictable workload, long hours, and high stress. As such, all hospitalists need to be aware of what exactly compassion is, why it matters, and what we can do to guard against its natural erosion.
What Is Compassion? What Is Empathy?
Wikipedia defines compassion as “the emotion that one feels in response to the suffering of others that motivates a desire to help.” The Latin derivation of compassion is “co-suffering.” Empathy is the ability to see and understand another’s suffering. So compassion is more than just empathy or “co-suffering”; with compassion comes yearning and a motivation to alleviate suffering in others.
Many important pieces within the definition of compassion need more explanation. Notice the three distinct “parts” of the definition: “the emotion that one feels”… “in response to the suffering of others”…“that motivates a desire to help.”
The first part outlines the fact that we have to be willing and able to conjure up an emotion toward and with our patients. Although this may sound basic, some physicians purposefully guard themselves against forming emotional responses toward or with their patients. Some actually think it will make them better—and more “objective”—providers if they guard against the (potentially) painful burden of sharing such empathic emotions.
Social science research has found that providers’ concerns about becoming emotionally exhausted might lead them to reduce their compassion for entire groups of patients, such as mentally ill or drug-addicted patient populations. There is also evidence that your ability to have empathy or compassion for another correlates with the ability to picture yourself with the same issue the patient suffers. This causes a major obstacle for many providers, who find themselves unable to relate to patients with “self-inflicted” issues, such as habits that increase the likelihood of disease (e.g. smoking) or not participating in habits that decrease the likelihood of disease or successful treatments (e.g. not exercising or not taking medications correctly).
Providers are more likely to be compassionate toward patients with whom they can identify; I would have enormous compassion for a 43-year-old female with new-onset ovarian cancer but would have less compassion for a 43-year-old male with new-onset alcohol withdrawal seizures.
The second part of the definition brings up the need to acknowledge suffering, in whatever form it takes. When we think of suffering, we often connect the idea with physical pain. But there are innumerable forms of nonphysical human suffering, including psychological and social trauma; this includes the anxiety that arises from known and unknown diagnoses and treatments and the emotional exhaustion resulting from such diagnoses and treatments. We need to be able to acknowledge all forms of suffering, not just physical suffering.
The last part of the definition shows that after we have allowed ourselves to “feel” the emotion of others and to acknowledge all walks of suffering, we then need to be motivated to help. For a hospitalist, this would mean “going the extra mile” for patients, such as continuously checking and rechecking on how treatments are (or are not) working, keeping the patient and family informed (in their terms) about what is happening, or ensuring that transitions of care (to other services or in/out of the hospital) are done with keen attention to reduce the risk of “voltage drops” in information.
Two videos help illustrate the nature of compassion (see the video sidebar for URLs). Both depict young women who have been called upon to sing the national anthem before a large crowd at an athletic gathering. Both women are clearly excellent singers, and both have a similar outcome in mind: to sing the national anthem in a manner pleasing to everyone in the crowd. In both cases, they forgot the words of the song.
In the first scenario, the woman is heckled, literally “booed,” then quickly shuffled off the ice rink after falling backwards on the ice. In the second scenario, a similarly talented young woman starts out strong, then forgets the words. An unrelated gentleman comes to her aid, puts his arm around her, and sings the words with her. As he continues, he looks to the audience, making hand signals to encourage them to join in supporting her during this presumably highly anxious moment.
The second scenario exemplifies all three components of compassion: The gentleman feels the singer’s anxiety, he acknowledges her “suffering,” and he is motivated to help. What I noticed about his assistance is that he is not even a very good singer! But his kind persuasion and ability to motivate the entire crowd in assisting her remarkably transform the outcome for both the singer and the crowd.
Though both scenarios start quite similarly, they end remarkably differently; the second scenario was completely changed by the compassion of a single person and a simple act of human kindness.
Why It Matters, and How to Build It
As depicted in these short videos, compassion can completely change outcomes. You will not find placebo-controlled randomized trials to support what I just stated. But there are plenty of social science studies to support the notion that compassion is a learned trait that can be improved or eroded over time, depending on the willingness of the person to try.
Compassion is a learned behavior. It is not a personality trait that you either have or you don’t. It is a set of behaviors and actions that can be learned and practiced, and even perfected, for those willing.
The Cleveland Clinic has created several videos (see video info box) that help us consider how to think about the nature of compassion and how to learn and practice it. A hospital is ripe with emotion in all areas, from the elevators to the hallways to the cafeteria. Due to the nature of our work, we are all at risk of compassion erosion toward our patients.
We first have to acknowledge such a risk is present and actively seek out opportunities, as depicted in these videos, to learn and practice compassion. As the Dalai Lama once said, “Compassion is a necessity, not a luxury.” We should all learn, demonstrate, and live compassion as a necessity in our practice.

Hospitalists care for a variety of different types of patients, serving anyone and everyone in need of acute care. Because of the nature of our work, it is difficult to maintain empathy and compassion for all of our patients, especially in light of our unpredictable workload, long hours, and high stress. As such, all hospitalists need to be aware of what exactly compassion is, why it matters, and what we can do to guard against its natural erosion.
What Is Compassion? What Is Empathy?
Wikipedia defines compassion as “the emotion that one feels in response to the suffering of others that motivates a desire to help.” The Latin derivation of compassion is “co-suffering.” Empathy is the ability to see and understand another’s suffering. So compassion is more than just empathy or “co-suffering”; with compassion comes yearning and a motivation to alleviate suffering in others.
Many important pieces within the definition of compassion need more explanation. Notice the three distinct “parts” of the definition: “the emotion that one feels”… “in response to the suffering of others”…“that motivates a desire to help.”
The first part outlines the fact that we have to be willing and able to conjure up an emotion toward and with our patients. Although this may sound basic, some physicians purposefully guard themselves against forming emotional responses toward or with their patients. Some actually think it will make them better—and more “objective”—providers if they guard against the (potentially) painful burden of sharing such empathic emotions.
Social science research has found that providers’ concerns about becoming emotionally exhausted might lead them to reduce their compassion for entire groups of patients, such as mentally ill or drug-addicted patient populations. There is also evidence that your ability to have empathy or compassion for another correlates with the ability to picture yourself with the same issue the patient suffers. This causes a major obstacle for many providers, who find themselves unable to relate to patients with “self-inflicted” issues, such as habits that increase the likelihood of disease (e.g. smoking) or not participating in habits that decrease the likelihood of disease or successful treatments (e.g. not exercising or not taking medications correctly).
Providers are more likely to be compassionate toward patients with whom they can identify; I would have enormous compassion for a 43-year-old female with new-onset ovarian cancer but would have less compassion for a 43-year-old male with new-onset alcohol withdrawal seizures.
The second part of the definition brings up the need to acknowledge suffering, in whatever form it takes. When we think of suffering, we often connect the idea with physical pain. But there are innumerable forms of nonphysical human suffering, including psychological and social trauma; this includes the anxiety that arises from known and unknown diagnoses and treatments and the emotional exhaustion resulting from such diagnoses and treatments. We need to be able to acknowledge all forms of suffering, not just physical suffering.
The last part of the definition shows that after we have allowed ourselves to “feel” the emotion of others and to acknowledge all walks of suffering, we then need to be motivated to help. For a hospitalist, this would mean “going the extra mile” for patients, such as continuously checking and rechecking on how treatments are (or are not) working, keeping the patient and family informed (in their terms) about what is happening, or ensuring that transitions of care (to other services or in/out of the hospital) are done with keen attention to reduce the risk of “voltage drops” in information.
Two videos help illustrate the nature of compassion (see the video sidebar for URLs). Both depict young women who have been called upon to sing the national anthem before a large crowd at an athletic gathering. Both women are clearly excellent singers, and both have a similar outcome in mind: to sing the national anthem in a manner pleasing to everyone in the crowd. In both cases, they forgot the words of the song.
In the first scenario, the woman is heckled, literally “booed,” then quickly shuffled off the ice rink after falling backwards on the ice. In the second scenario, a similarly talented young woman starts out strong, then forgets the words. An unrelated gentleman comes to her aid, puts his arm around her, and sings the words with her. As he continues, he looks to the audience, making hand signals to encourage them to join in supporting her during this presumably highly anxious moment.
The second scenario exemplifies all three components of compassion: The gentleman feels the singer’s anxiety, he acknowledges her “suffering,” and he is motivated to help. What I noticed about his assistance is that he is not even a very good singer! But his kind persuasion and ability to motivate the entire crowd in assisting her remarkably transform the outcome for both the singer and the crowd.
Though both scenarios start quite similarly, they end remarkably differently; the second scenario was completely changed by the compassion of a single person and a simple act of human kindness.
Why It Matters, and How to Build It
As depicted in these short videos, compassion can completely change outcomes. You will not find placebo-controlled randomized trials to support what I just stated. But there are plenty of social science studies to support the notion that compassion is a learned trait that can be improved or eroded over time, depending on the willingness of the person to try.
Compassion is a learned behavior. It is not a personality trait that you either have or you don’t. It is a set of behaviors and actions that can be learned and practiced, and even perfected, for those willing.
The Cleveland Clinic has created several videos (see video info box) that help us consider how to think about the nature of compassion and how to learn and practice it. A hospital is ripe with emotion in all areas, from the elevators to the hallways to the cafeteria. Due to the nature of our work, we are all at risk of compassion erosion toward our patients.
We first have to acknowledge such a risk is present and actively seek out opportunities, as depicted in these videos, to learn and practice compassion. As the Dalai Lama once said, “Compassion is a necessity, not a luxury.” We should all learn, demonstrate, and live compassion as a necessity in our practice.

Hospitalists Should Lead Training, Preparedness for Hospital Violence Prevention
On Jan. 20, a 44-year old surgeon was shot and killed in the middle of the day at one of the country’s top hospitals. Michael Davidson, MD, an endovascular surgeon at Brigham and Women’s Hospital in Boston, was in a second-floor hospital clinic when 55-year-old Stephen Pasceri asked for him by name. Dr. Davidson, the division director of endovascular cardiac surgery and assistant professor at Harvard Medical School, had taken care of Pasceri’s mother before her death in November 2014. Witnesses reported that Dr. Davidson came out to talk to Pasceri; during that conversation, Pasceri shot Dr. Davidson twice.
Dr. Davidson was quickly taken to the ED but died 12 hours later.
The shooter died of a self-inflicted gunshot wound to the head.
The motive is not clear, but Pasceri had voiced frustrations with the medical industry during the care of both his father and his mother. In addition, his mother seemed to have suffered some type of complication after a surgery performed by Dr. Davidson. Interviews of Pasceri’s relatives, friends, and neighbors found they were all shocked and dismayed. The shooter was, by all accounts, an upstanding citizen in his work, home, church, and community; he was an accountant with four children, with no past history of criminal or violent activity.1
A Disheartening Trend
Two other fatal events in medical centers occurred within weeks of the Davidson shooting. In December 2014, at Wentworth-Douglass Hospital in Dover, N.H., a man shot and killed his wife before killing himself.
Days later, at a Veterans Hospital clinic in El Paso, Texas, another shooting left both the perpetrator and a psychologist dead.2
In the healthcare setting, providers encounter many types of violence. Nonfatal violence, ranging from physical aggression to various levels of physical harm, has become commonplace. Inciters of such violence tend to be those who “can’t help themselves,” often patients with primary psychiatric illness or those with medically induced mental impairment, such as delirium or withdrawal. For these patients, there is at least some level of compassion and tolerance for their behavior, and because they tend to be relatively predictable, preparedness and mitigation of such acts can give providers some sense of control over the situation.
But the Davidson event represents a type of violence that is frightening, unpredictable, and very difficult to prevent, prepare for, or adequately handle.
Actual shootings on medical campuses are, fortunately, rare. A recent study by the Johns Hopkins Office of Critical Event Preparedness and Response found 154 hospital shootings between 2000 and 2011, resulting in 235 injured or dead victims. The most commonly occurring scenario is that of people acting against family members, with healthcare workers getting caught in the crosshairs. The most common victim is the shooter (45% of the time), and the least common victims are physicians and nurses. Over half (59%) of medical center shootings occur within the hospital; the other 41% occur somewhere else on the hospital grounds.3
So what can hospitalists and hospitals do about the real threat of physical violence and shootings within medical centers? Some have recommended metal detectors as effective barriers for preventing weapons from entering medical centers. The primary problem with this solution is that the majority of medical centers have found this plan impossible to implement, given the number of entrances in typical hospitals; Johns Hopkins for example, has more than 80 entrances. Metal detectors also require security staffing at each entrance 24/7.4
Because of the barriers, metal detectors present an insurmountable financial obstacle for most hospitals. In addition, they present an issue with public perception. Many would argue that hospitals are (and should be) places of healing and sanctuary (e.g. “safe havens”), not places for suspicion and searches. In addition, although there is evidence that the use of metal detectors results in increased confiscation of weapons, there is no evidence that they result in fewer on-site assaults.5 Further complicating matters, almost a quarter of the shootings that occur in EDs result from the perpetrator grabbing a weapon from a security guard.3
Others advocate for stricter gun control laws and enforcement, an argument that has vehement advocates and critics on both sides and is unlikely to be resolved in the near future.
Take Action: Be Prepared
In the meantime, hospitalists are left with preparedness tactics that range from situational awareness to active shooter drills. Both are equally important and should be a part of disaster preparedness at any medical center regardless of size, type, or location. Hospitalists can and should take a lead in such preparedness. Current statistics show that hospitalists are employed in at least 85% of all U.S. hospitals. With such widespread penetration, hospitalists can have a huge impact on the preparedness efforts that can prevent such acts from occurring, as well as on organizational resilience and recovery if such an act does occur.
Such training is more important in healthcare settings than other workplaces, as medical personnel have to be specially trained to resist the temptation to help. For example, active shooter training instructs personnel to run, hide, or fight, none of which come “naturally” to those trained to save and rescue for a living. This training instructs anyone in the “Hot Zone” (where life is in direct danger) to run away from the scene (always preferred if feasible), hide (barricade the door, silence any devices, and stay still), or fight (use anything in sight to fight the shooter, and work as a team if feasible). These responses are the exact opposite of what most trained healthcare personnel are accustomed to doing in cases of emergency.
In Sum
The Michael Davidson story is very sobering by all accounts. Healthcare violence such as this, while rare, is devastating.
Hospitalists should lead the way in training and preparedness for violence prevention and mitigation, including active shooter simulation scenarios. We can all have a huge impact in reducing the risk of casualties should such an unpredictable event occur in our hospital.

References
- Freyer FJ, Kowalczyk L, Murphy SP. Surgeon slain, gunman found dead in day of crisis at Brigham. January 20, 2015. The Boston Globe online. Available at: http://www.bostonglobe.com/metro/2015/01/20/boston-police-investigate-report-shooting-brigham-and-women/Jhig9z8LO8A5PH9Er4vTiP/story.html?rss_id=Top-GNP&utm_source=Managed&utm_campaign=386d2ff709-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-386d2ff709-319388717. Accessed February 5, 2015.
- Barnet S. Gun violence in hospitals: how much of a threat is it really? January 21, 2015. Becker’s Hospital Review. Available at: http://www.beckershospitalreview.com/healthcare-blog/gun-violence-in-hospitals-how-much-of-a-threat-is-it-really.html. Accessed February 5, 2015.
- Kelen GD, Catlett CL, Kubit JG, Hsieh Y-H. Hospital-based shootings in the United States: 2000 to 2011. Annals of Emergency Medicine online. September 20, 2012. Available at: http://www.annemergmed.com/article/S0196-0644%2812%2901408-4/abstract. Accessed February 5, 2015.
- Calvert S, Scharper J, Roylance F. Experts: no need for metal detectors at Hopkins. September 17, 2010. The Baltimore Sun online. Available at: http://articles.baltimoresun.com/2010-09-17/business/bs-md-hopkins-hospital-security-20100916_1_metal-detectors-healthcare-security-and-safety-hospital-security-experts. Accessed February 5, 2015.
- Rankins RC, Hendey GW. Effect of a security system on violent incidents and hidden weapons in the emergency department. Ann Emerg Med. 1999;33(6):676-679.
On Jan. 20, a 44-year old surgeon was shot and killed in the middle of the day at one of the country’s top hospitals. Michael Davidson, MD, an endovascular surgeon at Brigham and Women’s Hospital in Boston, was in a second-floor hospital clinic when 55-year-old Stephen Pasceri asked for him by name. Dr. Davidson, the division director of endovascular cardiac surgery and assistant professor at Harvard Medical School, had taken care of Pasceri’s mother before her death in November 2014. Witnesses reported that Dr. Davidson came out to talk to Pasceri; during that conversation, Pasceri shot Dr. Davidson twice.
Dr. Davidson was quickly taken to the ED but died 12 hours later.
The shooter died of a self-inflicted gunshot wound to the head.
The motive is not clear, but Pasceri had voiced frustrations with the medical industry during the care of both his father and his mother. In addition, his mother seemed to have suffered some type of complication after a surgery performed by Dr. Davidson. Interviews of Pasceri’s relatives, friends, and neighbors found they were all shocked and dismayed. The shooter was, by all accounts, an upstanding citizen in his work, home, church, and community; he was an accountant with four children, with no past history of criminal or violent activity.1
A Disheartening Trend
Two other fatal events in medical centers occurred within weeks of the Davidson shooting. In December 2014, at Wentworth-Douglass Hospital in Dover, N.H., a man shot and killed his wife before killing himself.
Days later, at a Veterans Hospital clinic in El Paso, Texas, another shooting left both the perpetrator and a psychologist dead.2
In the healthcare setting, providers encounter many types of violence. Nonfatal violence, ranging from physical aggression to various levels of physical harm, has become commonplace. Inciters of such violence tend to be those who “can’t help themselves,” often patients with primary psychiatric illness or those with medically induced mental impairment, such as delirium or withdrawal. For these patients, there is at least some level of compassion and tolerance for their behavior, and because they tend to be relatively predictable, preparedness and mitigation of such acts can give providers some sense of control over the situation.
But the Davidson event represents a type of violence that is frightening, unpredictable, and very difficult to prevent, prepare for, or adequately handle.
Actual shootings on medical campuses are, fortunately, rare. A recent study by the Johns Hopkins Office of Critical Event Preparedness and Response found 154 hospital shootings between 2000 and 2011, resulting in 235 injured or dead victims. The most commonly occurring scenario is that of people acting against family members, with healthcare workers getting caught in the crosshairs. The most common victim is the shooter (45% of the time), and the least common victims are physicians and nurses. Over half (59%) of medical center shootings occur within the hospital; the other 41% occur somewhere else on the hospital grounds.3
So what can hospitalists and hospitals do about the real threat of physical violence and shootings within medical centers? Some have recommended metal detectors as effective barriers for preventing weapons from entering medical centers. The primary problem with this solution is that the majority of medical centers have found this plan impossible to implement, given the number of entrances in typical hospitals; Johns Hopkins for example, has more than 80 entrances. Metal detectors also require security staffing at each entrance 24/7.4
Because of the barriers, metal detectors present an insurmountable financial obstacle for most hospitals. In addition, they present an issue with public perception. Many would argue that hospitals are (and should be) places of healing and sanctuary (e.g. “safe havens”), not places for suspicion and searches. In addition, although there is evidence that the use of metal detectors results in increased confiscation of weapons, there is no evidence that they result in fewer on-site assaults.5 Further complicating matters, almost a quarter of the shootings that occur in EDs result from the perpetrator grabbing a weapon from a security guard.3
Others advocate for stricter gun control laws and enforcement, an argument that has vehement advocates and critics on both sides and is unlikely to be resolved in the near future.
Take Action: Be Prepared
In the meantime, hospitalists are left with preparedness tactics that range from situational awareness to active shooter drills. Both are equally important and should be a part of disaster preparedness at any medical center regardless of size, type, or location. Hospitalists can and should take a lead in such preparedness. Current statistics show that hospitalists are employed in at least 85% of all U.S. hospitals. With such widespread penetration, hospitalists can have a huge impact on the preparedness efforts that can prevent such acts from occurring, as well as on organizational resilience and recovery if such an act does occur.
Such training is more important in healthcare settings than other workplaces, as medical personnel have to be specially trained to resist the temptation to help. For example, active shooter training instructs personnel to run, hide, or fight, none of which come “naturally” to those trained to save and rescue for a living. This training instructs anyone in the “Hot Zone” (where life is in direct danger) to run away from the scene (always preferred if feasible), hide (barricade the door, silence any devices, and stay still), or fight (use anything in sight to fight the shooter, and work as a team if feasible). These responses are the exact opposite of what most trained healthcare personnel are accustomed to doing in cases of emergency.
In Sum
The Michael Davidson story is very sobering by all accounts. Healthcare violence such as this, while rare, is devastating.
Hospitalists should lead the way in training and preparedness for violence prevention and mitigation, including active shooter simulation scenarios. We can all have a huge impact in reducing the risk of casualties should such an unpredictable event occur in our hospital.

References
- Freyer FJ, Kowalczyk L, Murphy SP. Surgeon slain, gunman found dead in day of crisis at Brigham. January 20, 2015. The Boston Globe online. Available at: http://www.bostonglobe.com/metro/2015/01/20/boston-police-investigate-report-shooting-brigham-and-women/Jhig9z8LO8A5PH9Er4vTiP/story.html?rss_id=Top-GNP&utm_source=Managed&utm_campaign=386d2ff709-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-386d2ff709-319388717. Accessed February 5, 2015.
- Barnet S. Gun violence in hospitals: how much of a threat is it really? January 21, 2015. Becker’s Hospital Review. Available at: http://www.beckershospitalreview.com/healthcare-blog/gun-violence-in-hospitals-how-much-of-a-threat-is-it-really.html. Accessed February 5, 2015.
- Kelen GD, Catlett CL, Kubit JG, Hsieh Y-H. Hospital-based shootings in the United States: 2000 to 2011. Annals of Emergency Medicine online. September 20, 2012. Available at: http://www.annemergmed.com/article/S0196-0644%2812%2901408-4/abstract. Accessed February 5, 2015.
- Calvert S, Scharper J, Roylance F. Experts: no need for metal detectors at Hopkins. September 17, 2010. The Baltimore Sun online. Available at: http://articles.baltimoresun.com/2010-09-17/business/bs-md-hopkins-hospital-security-20100916_1_metal-detectors-healthcare-security-and-safety-hospital-security-experts. Accessed February 5, 2015.
- Rankins RC, Hendey GW. Effect of a security system on violent incidents and hidden weapons in the emergency department. Ann Emerg Med. 1999;33(6):676-679.
On Jan. 20, a 44-year old surgeon was shot and killed in the middle of the day at one of the country’s top hospitals. Michael Davidson, MD, an endovascular surgeon at Brigham and Women’s Hospital in Boston, was in a second-floor hospital clinic when 55-year-old Stephen Pasceri asked for him by name. Dr. Davidson, the division director of endovascular cardiac surgery and assistant professor at Harvard Medical School, had taken care of Pasceri’s mother before her death in November 2014. Witnesses reported that Dr. Davidson came out to talk to Pasceri; during that conversation, Pasceri shot Dr. Davidson twice.
Dr. Davidson was quickly taken to the ED but died 12 hours later.
The shooter died of a self-inflicted gunshot wound to the head.
The motive is not clear, but Pasceri had voiced frustrations with the medical industry during the care of both his father and his mother. In addition, his mother seemed to have suffered some type of complication after a surgery performed by Dr. Davidson. Interviews of Pasceri’s relatives, friends, and neighbors found they were all shocked and dismayed. The shooter was, by all accounts, an upstanding citizen in his work, home, church, and community; he was an accountant with four children, with no past history of criminal or violent activity.1
A Disheartening Trend
Two other fatal events in medical centers occurred within weeks of the Davidson shooting. In December 2014, at Wentworth-Douglass Hospital in Dover, N.H., a man shot and killed his wife before killing himself.
Days later, at a Veterans Hospital clinic in El Paso, Texas, another shooting left both the perpetrator and a psychologist dead.2
In the healthcare setting, providers encounter many types of violence. Nonfatal violence, ranging from physical aggression to various levels of physical harm, has become commonplace. Inciters of such violence tend to be those who “can’t help themselves,” often patients with primary psychiatric illness or those with medically induced mental impairment, such as delirium or withdrawal. For these patients, there is at least some level of compassion and tolerance for their behavior, and because they tend to be relatively predictable, preparedness and mitigation of such acts can give providers some sense of control over the situation.
But the Davidson event represents a type of violence that is frightening, unpredictable, and very difficult to prevent, prepare for, or adequately handle.
Actual shootings on medical campuses are, fortunately, rare. A recent study by the Johns Hopkins Office of Critical Event Preparedness and Response found 154 hospital shootings between 2000 and 2011, resulting in 235 injured or dead victims. The most commonly occurring scenario is that of people acting against family members, with healthcare workers getting caught in the crosshairs. The most common victim is the shooter (45% of the time), and the least common victims are physicians and nurses. Over half (59%) of medical center shootings occur within the hospital; the other 41% occur somewhere else on the hospital grounds.3
So what can hospitalists and hospitals do about the real threat of physical violence and shootings within medical centers? Some have recommended metal detectors as effective barriers for preventing weapons from entering medical centers. The primary problem with this solution is that the majority of medical centers have found this plan impossible to implement, given the number of entrances in typical hospitals; Johns Hopkins for example, has more than 80 entrances. Metal detectors also require security staffing at each entrance 24/7.4
Because of the barriers, metal detectors present an insurmountable financial obstacle for most hospitals. In addition, they present an issue with public perception. Many would argue that hospitals are (and should be) places of healing and sanctuary (e.g. “safe havens”), not places for suspicion and searches. In addition, although there is evidence that the use of metal detectors results in increased confiscation of weapons, there is no evidence that they result in fewer on-site assaults.5 Further complicating matters, almost a quarter of the shootings that occur in EDs result from the perpetrator grabbing a weapon from a security guard.3
Others advocate for stricter gun control laws and enforcement, an argument that has vehement advocates and critics on both sides and is unlikely to be resolved in the near future.
Take Action: Be Prepared
In the meantime, hospitalists are left with preparedness tactics that range from situational awareness to active shooter drills. Both are equally important and should be a part of disaster preparedness at any medical center regardless of size, type, or location. Hospitalists can and should take a lead in such preparedness. Current statistics show that hospitalists are employed in at least 85% of all U.S. hospitals. With such widespread penetration, hospitalists can have a huge impact on the preparedness efforts that can prevent such acts from occurring, as well as on organizational resilience and recovery if such an act does occur.
Such training is more important in healthcare settings than other workplaces, as medical personnel have to be specially trained to resist the temptation to help. For example, active shooter training instructs personnel to run, hide, or fight, none of which come “naturally” to those trained to save and rescue for a living. This training instructs anyone in the “Hot Zone” (where life is in direct danger) to run away from the scene (always preferred if feasible), hide (barricade the door, silence any devices, and stay still), or fight (use anything in sight to fight the shooter, and work as a team if feasible). These responses are the exact opposite of what most trained healthcare personnel are accustomed to doing in cases of emergency.
In Sum
The Michael Davidson story is very sobering by all accounts. Healthcare violence such as this, while rare, is devastating.
Hospitalists should lead the way in training and preparedness for violence prevention and mitigation, including active shooter simulation scenarios. We can all have a huge impact in reducing the risk of casualties should such an unpredictable event occur in our hospital.

References
- Freyer FJ, Kowalczyk L, Murphy SP. Surgeon slain, gunman found dead in day of crisis at Brigham. January 20, 2015. The Boston Globe online. Available at: http://www.bostonglobe.com/metro/2015/01/20/boston-police-investigate-report-shooting-brigham-and-women/Jhig9z8LO8A5PH9Er4vTiP/story.html?rss_id=Top-GNP&utm_source=Managed&utm_campaign=386d2ff709-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-386d2ff709-319388717. Accessed February 5, 2015.
- Barnet S. Gun violence in hospitals: how much of a threat is it really? January 21, 2015. Becker’s Hospital Review. Available at: http://www.beckershospitalreview.com/healthcare-blog/gun-violence-in-hospitals-how-much-of-a-threat-is-it-really.html. Accessed February 5, 2015.
- Kelen GD, Catlett CL, Kubit JG, Hsieh Y-H. Hospital-based shootings in the United States: 2000 to 2011. Annals of Emergency Medicine online. September 20, 2012. Available at: http://www.annemergmed.com/article/S0196-0644%2812%2901408-4/abstract. Accessed February 5, 2015.
- Calvert S, Scharper J, Roylance F. Experts: no need for metal detectors at Hopkins. September 17, 2010. The Baltimore Sun online. Available at: http://articles.baltimoresun.com/2010-09-17/business/bs-md-hopkins-hospital-security-20100916_1_metal-detectors-healthcare-security-and-safety-hospital-security-experts. Accessed February 5, 2015.
- Rankins RC, Hendey GW. Effect of a security system on violent incidents and hidden weapons in the emergency department. Ann Emerg Med. 1999;33(6):676-679.
Tips for Hospitalists Managing Care of High-Profile Patients
Hospitalists around the globe have cared for their share of high profile patients, also known as very important people, or VIPs. Many of us dread the prospect of admitting a VIP to our service, knowing that such patients tend to be demanding and entitled and often want to dictate their care.
The term “VIP syndrome” was coined as early as 1964 by psychiatrist Walter Weintraub, who described how “the treatment of an influential man can be extremely hazardous for both patient and doctor.”1 He found, even back then, that the admission of VIPs to an inpatient setting was “often followed by considerable turmoil within the institution,” which can unfortunately undermine the quality of the care that the patient receives.
Some high profile—and controversial—deaths that have at least partially been attributable to VIP syndrome were those of Michael Jackson and Joan Rivers. In both cases, physicians veered from normal or usual standards to meet the apparent needs of their high profile patients. The Jackson case represented a violation of care standards: Dr. Conrad Murray administered propofol, midazolam, and lorazepam simultaneously without monitoring his patient, and this treatment resulted in cardiac arrest. The death was considered a homicide, and the physician was convicted of involuntary manslaughter and sentenced to two years in prison. In the Rivers case, the entertainer’s private ENT physician was involved in her care at a site in which he was not privileged to practice; it is unclear if the clinic was equipped to handle the complexity of her case, and she died after her airway was lost. Countless other examples of VIP quality care concerns signifying alterations in care standards based on the patient’s social status have resulted in less dramatically poor outcomes.
Some hospitals have carved out wings or floors to cater to VIP crowds. In these cases, the room and board charges are extraordinary and are billed directly “out of pocket” to the patient, bypassing insurance companies or payers. These wards or units are often staffed “ad hoc” by nurses and other care providers at very low staff-to-patient ratios, so that they can be at the beck and call of the VIP. Some of these admitted patients even bring along their private physicians and nurses, practitioners who are not privileged to practice on site but who may try to dictate the care being delivered.
The real issue, when VIP syndrome is in full swing, is that it violates many codes of medical professionalism, including those found in the Physician Charter of the ABIM Foundation, which emphasizes the guiding principles of patient welfare, autonomy, and social justice.2 Because there exists a whole cadre of patients who qualify as “VIPs” (celebrities, politicians, royalty, local board members, community leaders, and fellow physicians or healthcare administrators), it is extremely likely that each of us will be called upon to care for such a population at some point. As such, we need to have a plan for how we will manage the emotions and care of such patients, without violating any care or professionalism standards.
Roller Coaster of Emotions
My hospital recently had a VIP in for a protracted and complex illness. The patient and family became so demanding and time-consuming that we considered “rotating” them to various other units to give the physicians and staff a break. The typical emotions affiliated with such VIP cases are resentment and frustration, even hostility at times, especially when we recognize the fact that the care we are delivering is not better than average, and may actually be worse. The resentment stems from the fact that we all like to think we deliver the best care possible to all patients, regardless of their personal characteristics, because we all want and deserve the best care, regardless of our bank accounts or public popularity.
So, while none of us can or should avoid taking care of a VIP patient or family, we do have to be thoughtful—in advance—about how we will approach their care. An article from the Cleveland Clinic offers advice to clinicians taking care of these VIPs, in the form of nine guiding principles:3
- Don’t bend the rules: Although VIPs can exert immense pressure to change our practices and procedures to meet their needs, we should resist any temptation to bend to their wishes. Often, practices and procedures are in place for operational or safety reasons, and veering from them can put both practitioners and patients in harm’s way. Practitioners should be explicit in their conversations with VIP patients, explaining that they will be treated within the boundaries of all the usual operational and safety safeguards that are built into the system, for their own good.
- Work as a team: It must be made very clear to the VIP that the attending is in charge of all medical decision-making, and all other providers will be consultants in their care.
- Communicate: Structured, regular, and predictable communication is a must for the patient, family, and all other providers involved in the VIP’s care. While this can seem very time-consuming, it will save time in the end if the patient, providers, and community understand how and when communication will occur. Predictable communication can also set boundaries on how and when it is appropriate for the patient’s family to contact the attending (e.g. cell phone, text, pager, and so on).
- Carefully manage communication with media: Just as with any patient, a VIP’s confidentiality is paramount. Any media coverage should be carefully planned with the hospital’s public relations department, and the only information that should be shared is that which the patient agrees to in advance.
- Resist “chairperson’s syndrome”: This happens when the family insists on being assigned the most senior physician on staff, even when that physician might not be the one best suited for the clinical scenario. VIP care should be as close to “business as usual” as possible, including being staffed by the “best fit” attending and trainees (in teaching hospitals).
- Care should occur where it is most appropriate: This includes care in an “open” ICU, if that is the level of care needed. This conversation should also be undertaken early in the hospital stay, to ensure that the patient and family understand the rationale and need for matching their level of care with the appropriate care setting, while being mindful of privacy and security needs.
- Protect the patient’s security: High profile patients often are heavily pursued by the media, and all measures should be taken to ensure their safety, security, and privacy. These patients should be listed under an alias or as a confidential patient, to reduce the risk of HIPAA breaches by hospital staff or visitors.
- Be careful about accepting or declining gifts: Accepting and declining gifts can both be hazardous; it would be best to avoid accepting any gifts during the hospital stay, but you can offer to accept a reasonable and appropriate gift after the stay has concluded.
- Work with the patient’s personal physicians: In the event the VIP patient has personal physician(s), it is best to invite their input and show them that you value their opinion; however, it must be clear that the attending has ultimate responsibility for the care of the patient during the hospital stay and that all ordering of diagnostics and therapeutics will be done solely by the attending.

References
- Weintraub W. The VIP syndrome: A clinical study in hospital psychiatry. J Nerv Ment Dis. 1964;138(2):181-193.
- ABIM Foundation. Physician charter. Available at: http://www.abimfoundation.org/Professionalism/Physician-Charter.aspx. Accessed January 10, 2015.
- Guzman JA, Sasidhar M, Stoller JK. Caring for VIPs: nine principles. February 2011. Available at: http://www.ccjm.org/fileadmin/content_pdf/ccjm/content_2fd90f2_90.pdf. Accessed January 10, 2015.
Hospitalists around the globe have cared for their share of high profile patients, also known as very important people, or VIPs. Many of us dread the prospect of admitting a VIP to our service, knowing that such patients tend to be demanding and entitled and often want to dictate their care.
The term “VIP syndrome” was coined as early as 1964 by psychiatrist Walter Weintraub, who described how “the treatment of an influential man can be extremely hazardous for both patient and doctor.”1 He found, even back then, that the admission of VIPs to an inpatient setting was “often followed by considerable turmoil within the institution,” which can unfortunately undermine the quality of the care that the patient receives.
Some high profile—and controversial—deaths that have at least partially been attributable to VIP syndrome were those of Michael Jackson and Joan Rivers. In both cases, physicians veered from normal or usual standards to meet the apparent needs of their high profile patients. The Jackson case represented a violation of care standards: Dr. Conrad Murray administered propofol, midazolam, and lorazepam simultaneously without monitoring his patient, and this treatment resulted in cardiac arrest. The death was considered a homicide, and the physician was convicted of involuntary manslaughter and sentenced to two years in prison. In the Rivers case, the entertainer’s private ENT physician was involved in her care at a site in which he was not privileged to practice; it is unclear if the clinic was equipped to handle the complexity of her case, and she died after her airway was lost. Countless other examples of VIP quality care concerns signifying alterations in care standards based on the patient’s social status have resulted in less dramatically poor outcomes.
Some hospitals have carved out wings or floors to cater to VIP crowds. In these cases, the room and board charges are extraordinary and are billed directly “out of pocket” to the patient, bypassing insurance companies or payers. These wards or units are often staffed “ad hoc” by nurses and other care providers at very low staff-to-patient ratios, so that they can be at the beck and call of the VIP. Some of these admitted patients even bring along their private physicians and nurses, practitioners who are not privileged to practice on site but who may try to dictate the care being delivered.
The real issue, when VIP syndrome is in full swing, is that it violates many codes of medical professionalism, including those found in the Physician Charter of the ABIM Foundation, which emphasizes the guiding principles of patient welfare, autonomy, and social justice.2 Because there exists a whole cadre of patients who qualify as “VIPs” (celebrities, politicians, royalty, local board members, community leaders, and fellow physicians or healthcare administrators), it is extremely likely that each of us will be called upon to care for such a population at some point. As such, we need to have a plan for how we will manage the emotions and care of such patients, without violating any care or professionalism standards.
Roller Coaster of Emotions
My hospital recently had a VIP in for a protracted and complex illness. The patient and family became so demanding and time-consuming that we considered “rotating” them to various other units to give the physicians and staff a break. The typical emotions affiliated with such VIP cases are resentment and frustration, even hostility at times, especially when we recognize the fact that the care we are delivering is not better than average, and may actually be worse. The resentment stems from the fact that we all like to think we deliver the best care possible to all patients, regardless of their personal characteristics, because we all want and deserve the best care, regardless of our bank accounts or public popularity.
So, while none of us can or should avoid taking care of a VIP patient or family, we do have to be thoughtful—in advance—about how we will approach their care. An article from the Cleveland Clinic offers advice to clinicians taking care of these VIPs, in the form of nine guiding principles:3
- Don’t bend the rules: Although VIPs can exert immense pressure to change our practices and procedures to meet their needs, we should resist any temptation to bend to their wishes. Often, practices and procedures are in place for operational or safety reasons, and veering from them can put both practitioners and patients in harm’s way. Practitioners should be explicit in their conversations with VIP patients, explaining that they will be treated within the boundaries of all the usual operational and safety safeguards that are built into the system, for their own good.
- Work as a team: It must be made very clear to the VIP that the attending is in charge of all medical decision-making, and all other providers will be consultants in their care.
- Communicate: Structured, regular, and predictable communication is a must for the patient, family, and all other providers involved in the VIP’s care. While this can seem very time-consuming, it will save time in the end if the patient, providers, and community understand how and when communication will occur. Predictable communication can also set boundaries on how and when it is appropriate for the patient’s family to contact the attending (e.g. cell phone, text, pager, and so on).
- Carefully manage communication with media: Just as with any patient, a VIP’s confidentiality is paramount. Any media coverage should be carefully planned with the hospital’s public relations department, and the only information that should be shared is that which the patient agrees to in advance.
- Resist “chairperson’s syndrome”: This happens when the family insists on being assigned the most senior physician on staff, even when that physician might not be the one best suited for the clinical scenario. VIP care should be as close to “business as usual” as possible, including being staffed by the “best fit” attending and trainees (in teaching hospitals).
- Care should occur where it is most appropriate: This includes care in an “open” ICU, if that is the level of care needed. This conversation should also be undertaken early in the hospital stay, to ensure that the patient and family understand the rationale and need for matching their level of care with the appropriate care setting, while being mindful of privacy and security needs.
- Protect the patient’s security: High profile patients often are heavily pursued by the media, and all measures should be taken to ensure their safety, security, and privacy. These patients should be listed under an alias or as a confidential patient, to reduce the risk of HIPAA breaches by hospital staff or visitors.
- Be careful about accepting or declining gifts: Accepting and declining gifts can both be hazardous; it would be best to avoid accepting any gifts during the hospital stay, but you can offer to accept a reasonable and appropriate gift after the stay has concluded.
- Work with the patient’s personal physicians: In the event the VIP patient has personal physician(s), it is best to invite their input and show them that you value their opinion; however, it must be clear that the attending has ultimate responsibility for the care of the patient during the hospital stay and that all ordering of diagnostics and therapeutics will be done solely by the attending.

References
- Weintraub W. The VIP syndrome: A clinical study in hospital psychiatry. J Nerv Ment Dis. 1964;138(2):181-193.
- ABIM Foundation. Physician charter. Available at: http://www.abimfoundation.org/Professionalism/Physician-Charter.aspx. Accessed January 10, 2015.
- Guzman JA, Sasidhar M, Stoller JK. Caring for VIPs: nine principles. February 2011. Available at: http://www.ccjm.org/fileadmin/content_pdf/ccjm/content_2fd90f2_90.pdf. Accessed January 10, 2015.
Hospitalists around the globe have cared for their share of high profile patients, also known as very important people, or VIPs. Many of us dread the prospect of admitting a VIP to our service, knowing that such patients tend to be demanding and entitled and often want to dictate their care.
The term “VIP syndrome” was coined as early as 1964 by psychiatrist Walter Weintraub, who described how “the treatment of an influential man can be extremely hazardous for both patient and doctor.”1 He found, even back then, that the admission of VIPs to an inpatient setting was “often followed by considerable turmoil within the institution,” which can unfortunately undermine the quality of the care that the patient receives.
Some high profile—and controversial—deaths that have at least partially been attributable to VIP syndrome were those of Michael Jackson and Joan Rivers. In both cases, physicians veered from normal or usual standards to meet the apparent needs of their high profile patients. The Jackson case represented a violation of care standards: Dr. Conrad Murray administered propofol, midazolam, and lorazepam simultaneously without monitoring his patient, and this treatment resulted in cardiac arrest. The death was considered a homicide, and the physician was convicted of involuntary manslaughter and sentenced to two years in prison. In the Rivers case, the entertainer’s private ENT physician was involved in her care at a site in which he was not privileged to practice; it is unclear if the clinic was equipped to handle the complexity of her case, and she died after her airway was lost. Countless other examples of VIP quality care concerns signifying alterations in care standards based on the patient’s social status have resulted in less dramatically poor outcomes.
Some hospitals have carved out wings or floors to cater to VIP crowds. In these cases, the room and board charges are extraordinary and are billed directly “out of pocket” to the patient, bypassing insurance companies or payers. These wards or units are often staffed “ad hoc” by nurses and other care providers at very low staff-to-patient ratios, so that they can be at the beck and call of the VIP. Some of these admitted patients even bring along their private physicians and nurses, practitioners who are not privileged to practice on site but who may try to dictate the care being delivered.
The real issue, when VIP syndrome is in full swing, is that it violates many codes of medical professionalism, including those found in the Physician Charter of the ABIM Foundation, which emphasizes the guiding principles of patient welfare, autonomy, and social justice.2 Because there exists a whole cadre of patients who qualify as “VIPs” (celebrities, politicians, royalty, local board members, community leaders, and fellow physicians or healthcare administrators), it is extremely likely that each of us will be called upon to care for such a population at some point. As such, we need to have a plan for how we will manage the emotions and care of such patients, without violating any care or professionalism standards.
Roller Coaster of Emotions
My hospital recently had a VIP in for a protracted and complex illness. The patient and family became so demanding and time-consuming that we considered “rotating” them to various other units to give the physicians and staff a break. The typical emotions affiliated with such VIP cases are resentment and frustration, even hostility at times, especially when we recognize the fact that the care we are delivering is not better than average, and may actually be worse. The resentment stems from the fact that we all like to think we deliver the best care possible to all patients, regardless of their personal characteristics, because we all want and deserve the best care, regardless of our bank accounts or public popularity.
So, while none of us can or should avoid taking care of a VIP patient or family, we do have to be thoughtful—in advance—about how we will approach their care. An article from the Cleveland Clinic offers advice to clinicians taking care of these VIPs, in the form of nine guiding principles:3
- Don’t bend the rules: Although VIPs can exert immense pressure to change our practices and procedures to meet their needs, we should resist any temptation to bend to their wishes. Often, practices and procedures are in place for operational or safety reasons, and veering from them can put both practitioners and patients in harm’s way. Practitioners should be explicit in their conversations with VIP patients, explaining that they will be treated within the boundaries of all the usual operational and safety safeguards that are built into the system, for their own good.
- Work as a team: It must be made very clear to the VIP that the attending is in charge of all medical decision-making, and all other providers will be consultants in their care.
- Communicate: Structured, regular, and predictable communication is a must for the patient, family, and all other providers involved in the VIP’s care. While this can seem very time-consuming, it will save time in the end if the patient, providers, and community understand how and when communication will occur. Predictable communication can also set boundaries on how and when it is appropriate for the patient’s family to contact the attending (e.g. cell phone, text, pager, and so on).
- Carefully manage communication with media: Just as with any patient, a VIP’s confidentiality is paramount. Any media coverage should be carefully planned with the hospital’s public relations department, and the only information that should be shared is that which the patient agrees to in advance.
- Resist “chairperson’s syndrome”: This happens when the family insists on being assigned the most senior physician on staff, even when that physician might not be the one best suited for the clinical scenario. VIP care should be as close to “business as usual” as possible, including being staffed by the “best fit” attending and trainees (in teaching hospitals).
- Care should occur where it is most appropriate: This includes care in an “open” ICU, if that is the level of care needed. This conversation should also be undertaken early in the hospital stay, to ensure that the patient and family understand the rationale and need for matching their level of care with the appropriate care setting, while being mindful of privacy and security needs.
- Protect the patient’s security: High profile patients often are heavily pursued by the media, and all measures should be taken to ensure their safety, security, and privacy. These patients should be listed under an alias or as a confidential patient, to reduce the risk of HIPAA breaches by hospital staff or visitors.
- Be careful about accepting or declining gifts: Accepting and declining gifts can both be hazardous; it would be best to avoid accepting any gifts during the hospital stay, but you can offer to accept a reasonable and appropriate gift after the stay has concluded.
- Work with the patient’s personal physicians: In the event the VIP patient has personal physician(s), it is best to invite their input and show them that you value their opinion; however, it must be clear that the attending has ultimate responsibility for the care of the patient during the hospital stay and that all ordering of diagnostics and therapeutics will be done solely by the attending.

References
- Weintraub W. The VIP syndrome: A clinical study in hospital psychiatry. J Nerv Ment Dis. 1964;138(2):181-193.
- ABIM Foundation. Physician charter. Available at: http://www.abimfoundation.org/Professionalism/Physician-Charter.aspx. Accessed January 10, 2015.
- Guzman JA, Sasidhar M, Stoller JK. Caring for VIPs: nine principles. February 2011. Available at: http://www.ccjm.org/fileadmin/content_pdf/ccjm/content_2fd90f2_90.pdf. Accessed January 10, 2015.
Ebola Spurs Better Infection Prevention Practices for U.S.-based Hospitalists
In the beginning phases of the Ebola evolution in the U.S., when Thomas Duncan was declared the first probable case on U.S. soil, many American hospitals were left scared and wondering if they could adequately care for a patient with such a highly contagious infectious disease. Uneasy thoughts swirled around individual practitioners’ minds about whether they would be willing and able to safely provide care to a patient with a devastating, highly infectious disease that has a touted 50% to 70% mortality rate.
Although a handful of biohazard units in the U.S. had undertaken such care, they had done so in a true biohazard unit, which had been meticulously planned and funded for years and featured a highly trained and skilled staff of physicians, nurses, and others. Nonetheless, with the realization that U.S. hospitals would not get to choose whether or not a patient with Ebola was presented to them, massive planning ensued in thousands of U.S. hospitals.
Within days, hospitals quickly rolled out visible signage and appropriate screening tools to quickly and efficiently identify and isolate the next contagious patient on U.S. soil. As the healthcare workers at Texas Presbyterian Hospital diligently cared for Thomas Duncan, U.S. hospitals and healthcare providers were faced with the sobering reality that a healthcare worker had been infected with the deadly virus.
This was not a case of a medical missionary working in a third world country with limited protective equipment and in unsanitary conditions. This was a highly skilled nurse, with (what was at the time considered to be) adequate protective equipment, who was stricken with a highly lethal disease in the course of nursing care in a U.S. hospital.
Ebola became the leading headline for every news organization in the U.S. and beyond, causing confusion and concern among the lay public. Within U.S. healthcare systems, the signs and symptoms of Ebola began to roll easily off the tongues of both clinical and nonclinical staff, all of whom quickly became well versed on the geography of West Africa.
What happened next in the U.S. healthcare system was a dizzying series of recommendations and changes at the local, regional, and national level. This was accompanied by another sobering realization: Most U.S. hospitals are not able and should not attempt to handle patients infected with Ebola.
The concept of regionalization of Ebola care was quickly accepted as a viable model, as many U.S. hospitals did not have the volunteer workforce, facilities, disaster preparedness infrastructure, protective equipment, or training infrastructure to safely care for such a patient, even if only short-term care was required.
These regionalization efforts required unparalleled cooperation among U.S. hospital systems and created the need for complex interdependencies among federal and state agencies across the nation. Many hospitals, including my own, invested thousands of man-hours and significant fiscal resources in preparing for the possibility of an infected patient.
These efforts also prompted a series of uncomfortable conversations, especially among clinicians and bioethicists, about what level of care can be safely provided to an Ebola patient in the U.S. Clinicians and bioethicists came to the realization that an Ebola patient in the U.S. may receive a different standard of care than a patient with a different blood-borne infectious disease. The guiding principle of “staff safety first” made for further difficult conversations among clinicians, who are accustomed to putting their safety second.
With all these perturbations to the system and anxiety-laden clinical discussions, the question is, has any good occurred as a result of this viral penetration into the U.S.? I believe the answer is yes, as the rapid anticipation and planning for this level of care has spurned efforts that otherwise would have remained dormant, including:
- Unparalleled cooperation among U.S. hospitals for aiding and assisting each others’ readiness to screen accurately and safely provide first responder care;
- Remarkable cooperation and assistance from state and federal agencies in guidance, communication, and preparedness for the centers designated as regional referral centers;
- Enhanced planning and capabilities for U.S. hospitals to respond and adapt to changes in the external environment, which makes them that much more prepared to respond and adapt to the next contagious disease crisis, one that will undoubtedly occur; and
- A renewed sense of volunteerism among many clinicians, despite the possibility of personal threat.
Current estimates predict the Ebola outbreak will expand from hundreds to thousands of new cases (and deaths) per month.1 As this situation evolves, individual regionalized centers in the U.S. become more prepared (logistically and psychologically) to handle Ebola as each day passes.
The foundational structure of care designed during this outbreak can and should put the U.S. in a very good position to resiliently and effectively care for any highly contagious agent in the future. So in the face of this disruptive adversity, we should all be able to keep calm and Ebola on.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
In the beginning phases of the Ebola evolution in the U.S., when Thomas Duncan was declared the first probable case on U.S. soil, many American hospitals were left scared and wondering if they could adequately care for a patient with such a highly contagious infectious disease. Uneasy thoughts swirled around individual practitioners’ minds about whether they would be willing and able to safely provide care to a patient with a devastating, highly infectious disease that has a touted 50% to 70% mortality rate.
Although a handful of biohazard units in the U.S. had undertaken such care, they had done so in a true biohazard unit, which had been meticulously planned and funded for years and featured a highly trained and skilled staff of physicians, nurses, and others. Nonetheless, with the realization that U.S. hospitals would not get to choose whether or not a patient with Ebola was presented to them, massive planning ensued in thousands of U.S. hospitals.
Within days, hospitals quickly rolled out visible signage and appropriate screening tools to quickly and efficiently identify and isolate the next contagious patient on U.S. soil. As the healthcare workers at Texas Presbyterian Hospital diligently cared for Thomas Duncan, U.S. hospitals and healthcare providers were faced with the sobering reality that a healthcare worker had been infected with the deadly virus.
This was not a case of a medical missionary working in a third world country with limited protective equipment and in unsanitary conditions. This was a highly skilled nurse, with (what was at the time considered to be) adequate protective equipment, who was stricken with a highly lethal disease in the course of nursing care in a U.S. hospital.
Ebola became the leading headline for every news organization in the U.S. and beyond, causing confusion and concern among the lay public. Within U.S. healthcare systems, the signs and symptoms of Ebola began to roll easily off the tongues of both clinical and nonclinical staff, all of whom quickly became well versed on the geography of West Africa.
What happened next in the U.S. healthcare system was a dizzying series of recommendations and changes at the local, regional, and national level. This was accompanied by another sobering realization: Most U.S. hospitals are not able and should not attempt to handle patients infected with Ebola.
The concept of regionalization of Ebola care was quickly accepted as a viable model, as many U.S. hospitals did not have the volunteer workforce, facilities, disaster preparedness infrastructure, protective equipment, or training infrastructure to safely care for such a patient, even if only short-term care was required.
These regionalization efforts required unparalleled cooperation among U.S. hospital systems and created the need for complex interdependencies among federal and state agencies across the nation. Many hospitals, including my own, invested thousands of man-hours and significant fiscal resources in preparing for the possibility of an infected patient.
These efforts also prompted a series of uncomfortable conversations, especially among clinicians and bioethicists, about what level of care can be safely provided to an Ebola patient in the U.S. Clinicians and bioethicists came to the realization that an Ebola patient in the U.S. may receive a different standard of care than a patient with a different blood-borne infectious disease. The guiding principle of “staff safety first” made for further difficult conversations among clinicians, who are accustomed to putting their safety second.
With all these perturbations to the system and anxiety-laden clinical discussions, the question is, has any good occurred as a result of this viral penetration into the U.S.? I believe the answer is yes, as the rapid anticipation and planning for this level of care has spurned efforts that otherwise would have remained dormant, including:
- Unparalleled cooperation among U.S. hospitals for aiding and assisting each others’ readiness to screen accurately and safely provide first responder care;
- Remarkable cooperation and assistance from state and federal agencies in guidance, communication, and preparedness for the centers designated as regional referral centers;
- Enhanced planning and capabilities for U.S. hospitals to respond and adapt to changes in the external environment, which makes them that much more prepared to respond and adapt to the next contagious disease crisis, one that will undoubtedly occur; and
- A renewed sense of volunteerism among many clinicians, despite the possibility of personal threat.
Current estimates predict the Ebola outbreak will expand from hundreds to thousands of new cases (and deaths) per month.1 As this situation evolves, individual regionalized centers in the U.S. become more prepared (logistically and psychologically) to handle Ebola as each day passes.
The foundational structure of care designed during this outbreak can and should put the U.S. in a very good position to resiliently and effectively care for any highly contagious agent in the future. So in the face of this disruptive adversity, we should all be able to keep calm and Ebola on.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
In the beginning phases of the Ebola evolution in the U.S., when Thomas Duncan was declared the first probable case on U.S. soil, many American hospitals were left scared and wondering if they could adequately care for a patient with such a highly contagious infectious disease. Uneasy thoughts swirled around individual practitioners’ minds about whether they would be willing and able to safely provide care to a patient with a devastating, highly infectious disease that has a touted 50% to 70% mortality rate.
Although a handful of biohazard units in the U.S. had undertaken such care, they had done so in a true biohazard unit, which had been meticulously planned and funded for years and featured a highly trained and skilled staff of physicians, nurses, and others. Nonetheless, with the realization that U.S. hospitals would not get to choose whether or not a patient with Ebola was presented to them, massive planning ensued in thousands of U.S. hospitals.
Within days, hospitals quickly rolled out visible signage and appropriate screening tools to quickly and efficiently identify and isolate the next contagious patient on U.S. soil. As the healthcare workers at Texas Presbyterian Hospital diligently cared for Thomas Duncan, U.S. hospitals and healthcare providers were faced with the sobering reality that a healthcare worker had been infected with the deadly virus.
This was not a case of a medical missionary working in a third world country with limited protective equipment and in unsanitary conditions. This was a highly skilled nurse, with (what was at the time considered to be) adequate protective equipment, who was stricken with a highly lethal disease in the course of nursing care in a U.S. hospital.
Ebola became the leading headline for every news organization in the U.S. and beyond, causing confusion and concern among the lay public. Within U.S. healthcare systems, the signs and symptoms of Ebola began to roll easily off the tongues of both clinical and nonclinical staff, all of whom quickly became well versed on the geography of West Africa.
What happened next in the U.S. healthcare system was a dizzying series of recommendations and changes at the local, regional, and national level. This was accompanied by another sobering realization: Most U.S. hospitals are not able and should not attempt to handle patients infected with Ebola.
The concept of regionalization of Ebola care was quickly accepted as a viable model, as many U.S. hospitals did not have the volunteer workforce, facilities, disaster preparedness infrastructure, protective equipment, or training infrastructure to safely care for such a patient, even if only short-term care was required.
These regionalization efforts required unparalleled cooperation among U.S. hospital systems and created the need for complex interdependencies among federal and state agencies across the nation. Many hospitals, including my own, invested thousands of man-hours and significant fiscal resources in preparing for the possibility of an infected patient.
These efforts also prompted a series of uncomfortable conversations, especially among clinicians and bioethicists, about what level of care can be safely provided to an Ebola patient in the U.S. Clinicians and bioethicists came to the realization that an Ebola patient in the U.S. may receive a different standard of care than a patient with a different blood-borne infectious disease. The guiding principle of “staff safety first” made for further difficult conversations among clinicians, who are accustomed to putting their safety second.
With all these perturbations to the system and anxiety-laden clinical discussions, the question is, has any good occurred as a result of this viral penetration into the U.S.? I believe the answer is yes, as the rapid anticipation and planning for this level of care has spurned efforts that otherwise would have remained dormant, including:
- Unparalleled cooperation among U.S. hospitals for aiding and assisting each others’ readiness to screen accurately and safely provide first responder care;
- Remarkable cooperation and assistance from state and federal agencies in guidance, communication, and preparedness for the centers designated as regional referral centers;
- Enhanced planning and capabilities for U.S. hospitals to respond and adapt to changes in the external environment, which makes them that much more prepared to respond and adapt to the next contagious disease crisis, one that will undoubtedly occur; and
- A renewed sense of volunteerism among many clinicians, despite the possibility of personal threat.
Current estimates predict the Ebola outbreak will expand from hundreds to thousands of new cases (and deaths) per month.1 As this situation evolves, individual regionalized centers in the U.S. become more prepared (logistically and psychologically) to handle Ebola as each day passes.
The foundational structure of care designed during this outbreak can and should put the U.S. in a very good position to resiliently and effectively care for any highly contagious agent in the future. So in the face of this disruptive adversity, we should all be able to keep calm and Ebola on.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.