User login
It's Not About Pager Replacement
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
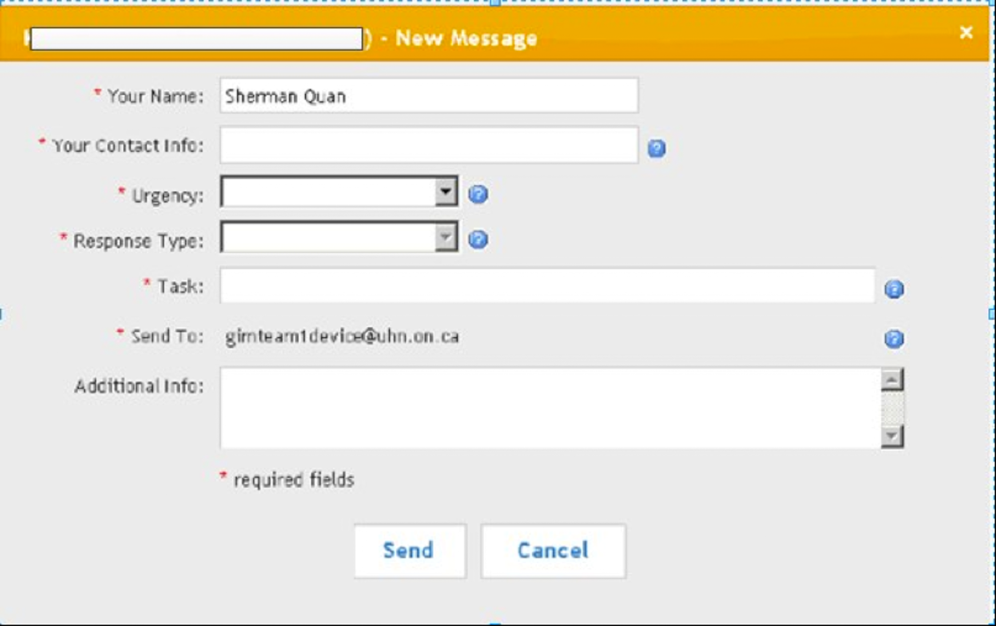
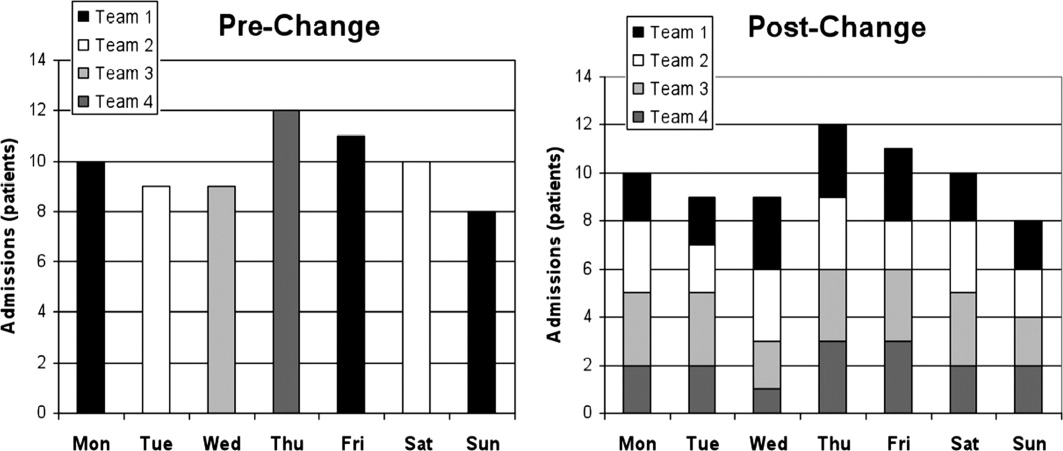
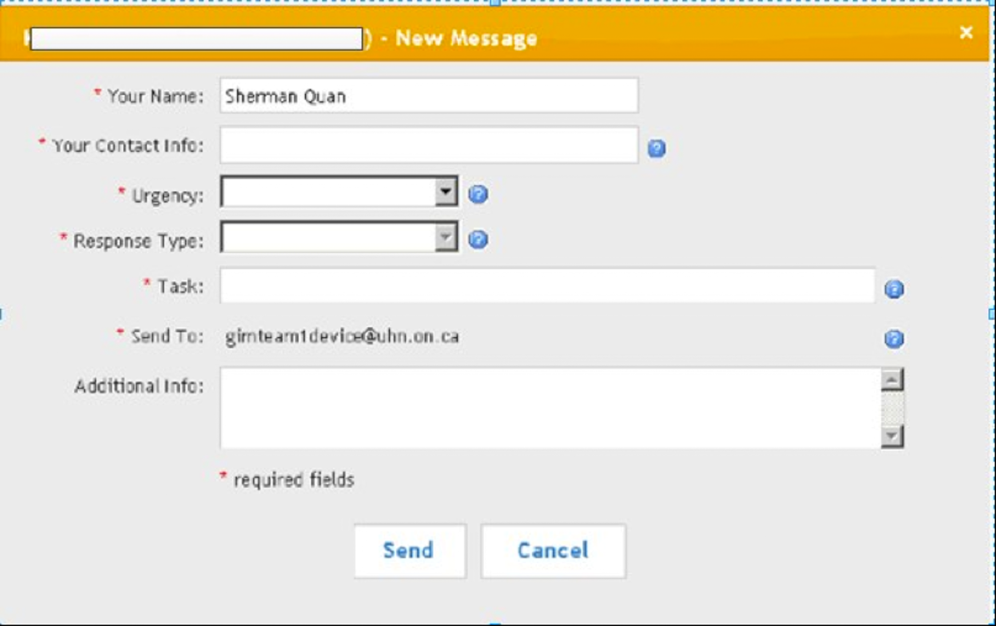
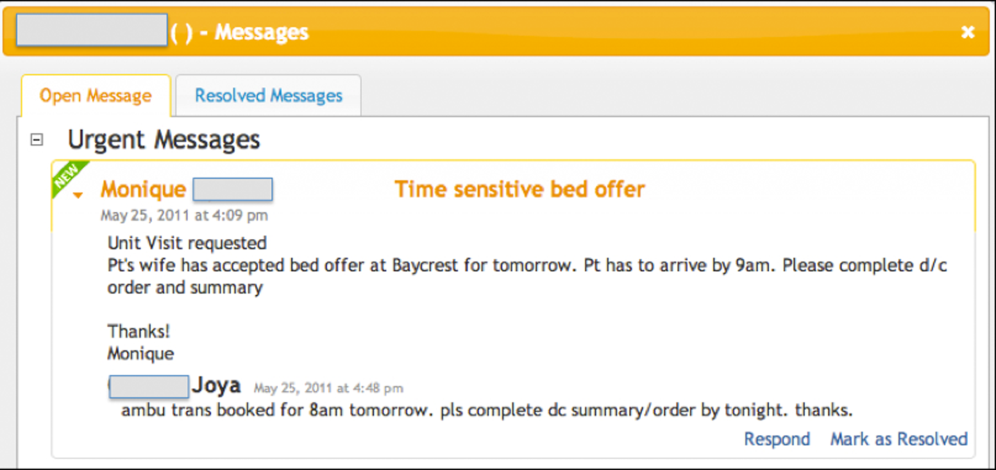
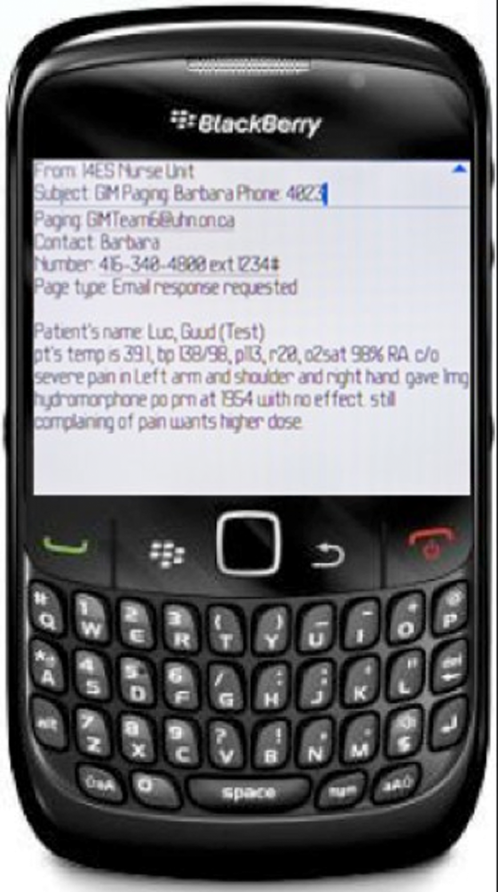
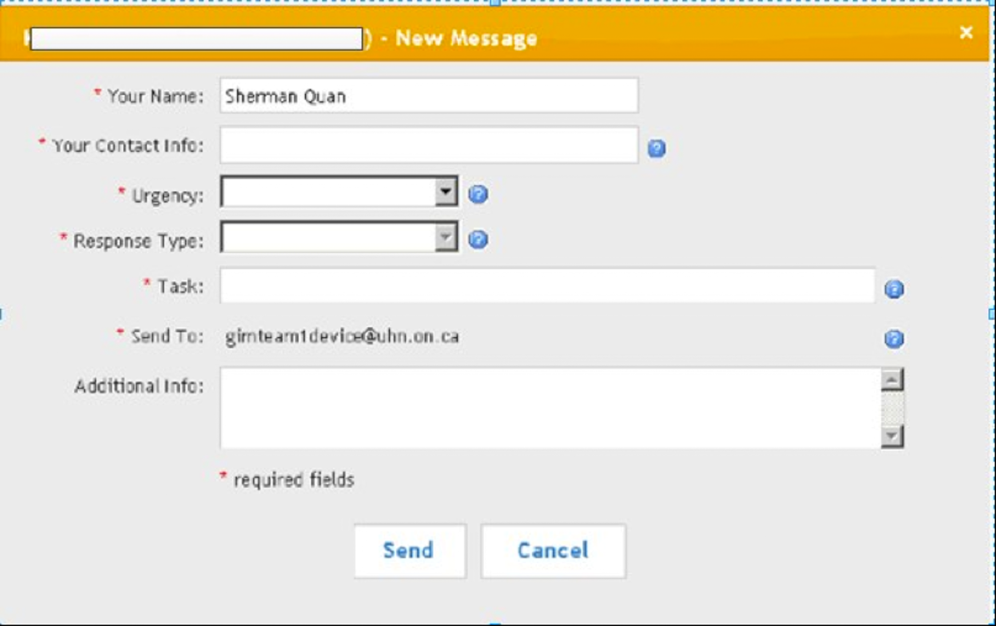
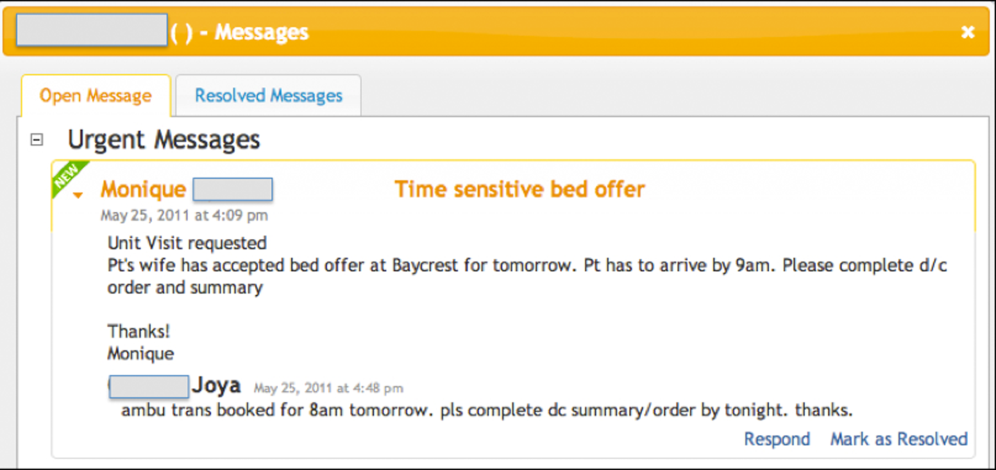
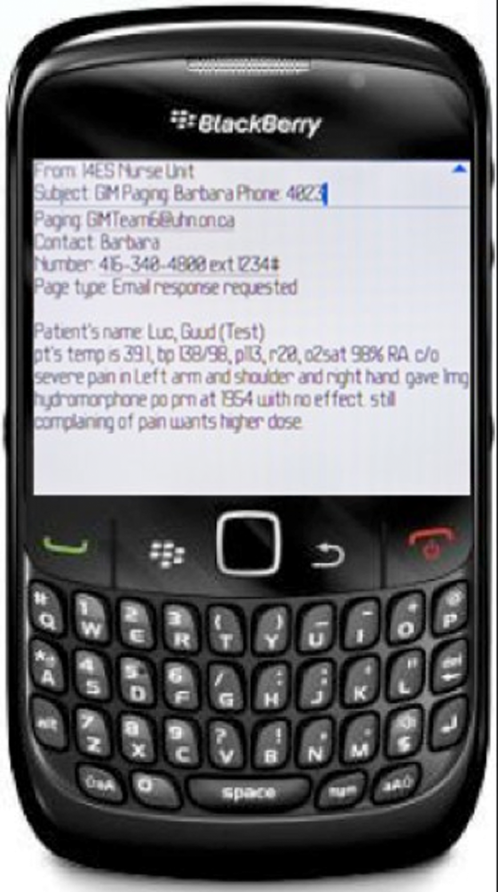
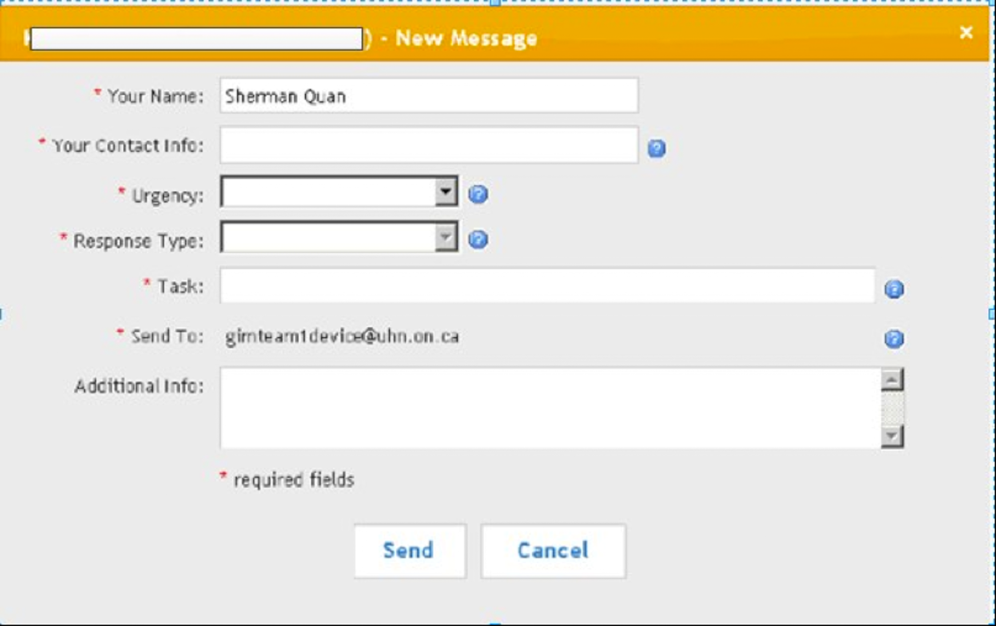
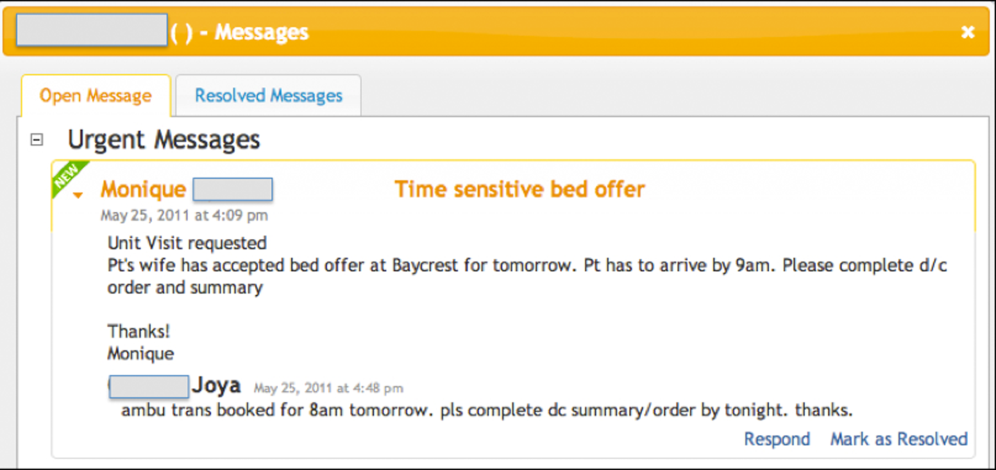
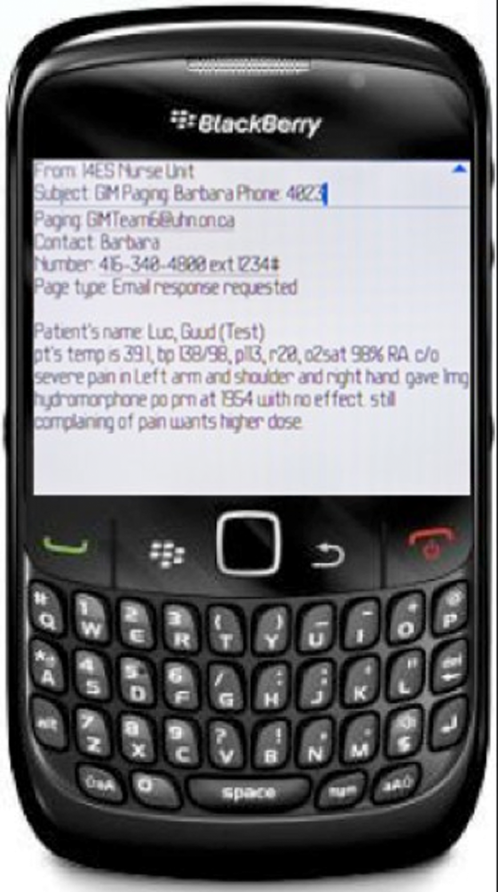
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
Copyright © 2013 Society of Hospital Medicine
Continuous Admission Model Reduces LOS
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
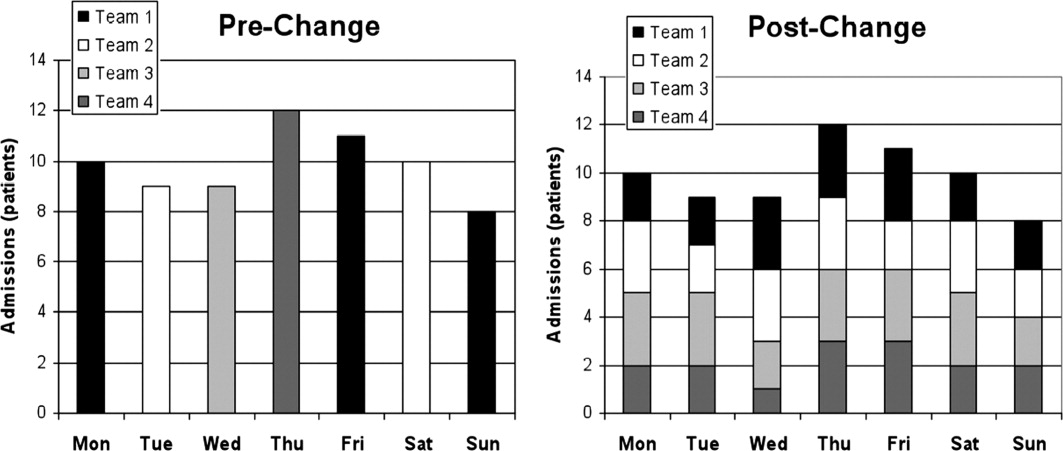
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.