User login
Diffuse rash and cough in elderly woman with a UTI
A 66-YEAR-OLD WOMAN came into the emergency department with a diffuse rash and a cough. She had a rash on the palms of her hands, which had developed the day before, but had improved a bit. She also had a rash on her feet, legs, and lower abdomen, which had developed that morning.
She said that over the previous 2 days she’d had a fever, dry cough, and some difficulty breathing. Her past medical history was significant for asthma, diabetes, hypertension, and osteoarthritis. Her medications included atenolol, celecoxib, metformin, pioglitazone, and an albuterol inhaler, as needed. In addition, she was on the ninth day of a 10-day course of nitrofurantoin for acute cystitis. She was allergic to ampicillin and erythromycin.
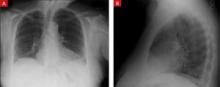
On physical exam, she had a fever of 101.5°F. On lung examination, she had diffuse wheezes and mild bibasilar crackles. Examination of her skin revealed a nonpainful, nonpruritic, erythematous, maculopapular rash located on the palms and legs (FIGURES 1A AND 1B), as well as on her lower abdomen. Chest radiograph showed mild opacification in the bases of the lungs (FIGURES 2A AND 2B). Her labs were significant for a white blood cell (WBC) count of 11.3 ×103/mm3.
What is your diagnosis?
FIGURE 1
Rash on hands, feet, legs, and lower abdomen
The patient had generalized palmar erythema with 1- to 2-mm papules (A). She also had an erythematous maculopapular rash that extended from the medial and dorsal aspects of her feet cranially to her lower abdomen (B).
FIGURE 2
Mild opacification in lung bases
A posterior-anterior chest radiograph revealed bilateral lower lung opacities that were greater on the left side than on the right (A). A lateral chest radiograph revealed a positive spine sign: failure of the vertebral bodies to become more radiolucent as one looks down the spinal column, suggesting a posterior-inferior lung infiltrate that opacifies the normally radiolucent vertebral bodies of the lower chest (B).
Diagnosis: nitrofurantoin-induced lung disease
Nitrofurantoin (Macrodantin, Macrobid) is frequently used as first-line treatment for uncomplicated urinary tract infections (UTIs) and as prophylaxis for recurrent UTIs. Although generally well tolerated, it has a rare but serious side effect profile, including aplastic anemia, peripheral neuropathy, liver toxicity, and—as in the case of this patient—pulmonary toxicity.1
Nitrofurantoin-induced lung disease has an incidence of 3 cases per 1000 patients.2 Not surprisingly, elderly women are often affected, as this population is particularly susceptible to UTIs (and their recurrence), and thus are prescribed nitrofurantoin.3 The pathophysiology of the acute and chronic form of this drug reaction is unknown, but may be either an immunologic hypersensitivity reaction or a direct cytotoxic effect by nitrofurantoin or its metabolites on the lung parenchyma.4
The acute presentation begins within 3 weeks of initiation of nitrofurantoin. The most common symptoms include fever, dry cough, and dyspnea. Less common symptoms include an erythematous maculopapular rash, fatigue, arthralgias/myalgias, and anorexia. Patients may experience bronchospasm and have audible wheezing on exam. Eight percent of patients will have an abnormal chest radiograph, most often showing diffuse interstitial infiltrates or pleural effusions. An elevated WBC count appears in 40% of patients, many having an eosinophilia, and an elevated erythrocyte sedimentation rate may be present.5 Pulmonary function tests (PFTs), if performed, will show a restrictive pattern and a V/Q scan will show a ventilation-perfusion mismatch.2
The chronic presentation is much less common than the acute form. It occurs in patients on daily nitrofurantoin and its onset is delayed months to years after initiation of therapy. Symptoms are insidious and include cough and gradually worsening dyspnea on exertion. Physical exam may reveal wheezing or crackles and chest radiograph can show interstitial or alveolar infiltrates, as well as pleural effusions. Laboratory evaluation is similar to the acute form, and PFT findings also reveal a restrictive pattern.
Computed tomography has variable findings, such as ground-glass opacities, interstitial fibrosis, consolidation, peribronchial thickening, and centrilobular nodules. Lung biopsies have shown varying pathologic features: nonspecific interstitial pneumonia, pulmonary fibrosis, bronchiolitis obliterans organizing pneumonia, and hypersensitivity pneumonitis. 6,7
Differential Dx includes anaphylaxis, pneumonia
The differential diagnosis for nitrofurantoin-induced lung disease includes anaphylaxis, asthma, bronchitis, and pneumonia. Drug anaphylaxis typically occurs within hours of administration and often has skin findings of urticaria, pruritus, and angioedema of the oral mucosa. Patients may present with dyspnea, wheezing, stridor, hypoxemia, and respiratory distress.8
Although asthma, bronchitis, and pneumonia can present with a fever, cough, and radiograph findings, they are not usually associated with a rash. Identifying and removing the offending agent—a medication—is key in differentiating this disease from other common lung ailments.
Stop the offending agent, consider corticosteroids
Immediately discontinuing nitrofurantoin is usually sufficient to resolve the symptoms of acute nitrofurantoin-induced lung disease, often within 24 to 48 hours. Chest radiograph and PFT changes resolve within weeks of discontinuation. (Reintroducing nitrofurantoin to the patient will produce similar symptoms with a more rapid onset.) Corticosteroids are often used to treat this lung injury, although their effectiveness remains unproven.
With the chronic reaction, nitrofurantoin therapy is stopped and most patients are started on corticosteroids, typically dosed at 20 to 40 mg per day with a prolonged taper over several months. With treatment, many patients recover from their chronic pulmonary reaction, although it may take months to years.3 Some patients may never fully recover and continue to have symptoms, radiographic findings, and PFT changes characteristic of pulmonary fibrosis.
More seriously, nitrofurantoin-induced lung disease may require hospitalization. Rare cases have required lung transplantation and others have resulted in death due to respiratory failure.1
A speedy recovery for our patient
We told our patient to discontinue the nitrofurantoin, and we opted not to start her on corticosteroids. Her symptoms resolved within 3 days of discontinuing the medication, and she had no return of her UTI symptoms. Her rash also resolved within 5 days.
CORRESPONDENCE: Drew C. Baird, MD, Department of Family and Community Medicine, Carl R. Darnall Army Medical Center, 36000 Darnall Loop, Fort Hood, TX 76544; drew.baird@us.army.mil
1. Goemaere N, Grijm K, van Hal P, et al. Nitrofurantoin-induced pulmonary fibrosis: a case report. J Med Case Reports. 2008;2:169.-
2. Hainer BL, White AA. Nitrofurantoin pulmonary toxicity. J Fam Pract. 1981;13:817-823.
3. Bhullar S, Lele SM, Kraman S. Severe nitrofurantoin lung disease resolving without the use of steroids. J Postgrad Med. 2007;53:111-113.
4. Peall AF, Hodges A. Concomitant pulmonary and hepatic toxicity secondary to nitrofurantoin: a case report. J Med Case Reports. 2007;1:59.-
5. Holmberg L, Boman G, Bottiger LE, et al. Adverse reactions to nitrofurantoin. Analysis of 921 reports. Am J Med. 1980;69:733-738.
6. Mendez JL, Nadrous HF, Hartman TE, et al. Chronic nitrofurantoin-induced lung disease. Mayo Clin Proc. 2005;80:1298-1302.
7. Cameron RJ, Kolbe J, Wilsher ML, et al. Bronchiolitis obliterans organizing pneumonia associated with the use of nitrofurantoin. Thorax. 2000;55:249-251.
8. Tang AW. A practical guide to anaphylaxis. Am Fam Physician. 2003;68:1325-1332.
A 66-YEAR-OLD WOMAN came into the emergency department with a diffuse rash and a cough. She had a rash on the palms of her hands, which had developed the day before, but had improved a bit. She also had a rash on her feet, legs, and lower abdomen, which had developed that morning.
She said that over the previous 2 days she’d had a fever, dry cough, and some difficulty breathing. Her past medical history was significant for asthma, diabetes, hypertension, and osteoarthritis. Her medications included atenolol, celecoxib, metformin, pioglitazone, and an albuterol inhaler, as needed. In addition, she was on the ninth day of a 10-day course of nitrofurantoin for acute cystitis. She was allergic to ampicillin and erythromycin.
On physical exam, she had a fever of 101.5°F. On lung examination, she had diffuse wheezes and mild bibasilar crackles. Examination of her skin revealed a nonpainful, nonpruritic, erythematous, maculopapular rash located on the palms and legs (FIGURES 1A AND 1B), as well as on her lower abdomen. Chest radiograph showed mild opacification in the bases of the lungs (FIGURES 2A AND 2B). Her labs were significant for a white blood cell (WBC) count of 11.3 ×103/mm3.
What is your diagnosis?
FIGURE 1
Rash on hands, feet, legs, and lower abdomen
The patient had generalized palmar erythema with 1- to 2-mm papules (A). She also had an erythematous maculopapular rash that extended from the medial and dorsal aspects of her feet cranially to her lower abdomen (B).
FIGURE 2
Mild opacification in lung bases
A posterior-anterior chest radiograph revealed bilateral lower lung opacities that were greater on the left side than on the right (A). A lateral chest radiograph revealed a positive spine sign: failure of the vertebral bodies to become more radiolucent as one looks down the spinal column, suggesting a posterior-inferior lung infiltrate that opacifies the normally radiolucent vertebral bodies of the lower chest (B).
Diagnosis: nitrofurantoin-induced lung disease
Nitrofurantoin (Macrodantin, Macrobid) is frequently used as first-line treatment for uncomplicated urinary tract infections (UTIs) and as prophylaxis for recurrent UTIs. Although generally well tolerated, it has a rare but serious side effect profile, including aplastic anemia, peripheral neuropathy, liver toxicity, and—as in the case of this patient—pulmonary toxicity.1
Nitrofurantoin-induced lung disease has an incidence of 3 cases per 1000 patients.2 Not surprisingly, elderly women are often affected, as this population is particularly susceptible to UTIs (and their recurrence), and thus are prescribed nitrofurantoin.3 The pathophysiology of the acute and chronic form of this drug reaction is unknown, but may be either an immunologic hypersensitivity reaction or a direct cytotoxic effect by nitrofurantoin or its metabolites on the lung parenchyma.4
The acute presentation begins within 3 weeks of initiation of nitrofurantoin. The most common symptoms include fever, dry cough, and dyspnea. Less common symptoms include an erythematous maculopapular rash, fatigue, arthralgias/myalgias, and anorexia. Patients may experience bronchospasm and have audible wheezing on exam. Eight percent of patients will have an abnormal chest radiograph, most often showing diffuse interstitial infiltrates or pleural effusions. An elevated WBC count appears in 40% of patients, many having an eosinophilia, and an elevated erythrocyte sedimentation rate may be present.5 Pulmonary function tests (PFTs), if performed, will show a restrictive pattern and a V/Q scan will show a ventilation-perfusion mismatch.2
The chronic presentation is much less common than the acute form. It occurs in patients on daily nitrofurantoin and its onset is delayed months to years after initiation of therapy. Symptoms are insidious and include cough and gradually worsening dyspnea on exertion. Physical exam may reveal wheezing or crackles and chest radiograph can show interstitial or alveolar infiltrates, as well as pleural effusions. Laboratory evaluation is similar to the acute form, and PFT findings also reveal a restrictive pattern.
Computed tomography has variable findings, such as ground-glass opacities, interstitial fibrosis, consolidation, peribronchial thickening, and centrilobular nodules. Lung biopsies have shown varying pathologic features: nonspecific interstitial pneumonia, pulmonary fibrosis, bronchiolitis obliterans organizing pneumonia, and hypersensitivity pneumonitis. 6,7
Differential Dx includes anaphylaxis, pneumonia
The differential diagnosis for nitrofurantoin-induced lung disease includes anaphylaxis, asthma, bronchitis, and pneumonia. Drug anaphylaxis typically occurs within hours of administration and often has skin findings of urticaria, pruritus, and angioedema of the oral mucosa. Patients may present with dyspnea, wheezing, stridor, hypoxemia, and respiratory distress.8
Although asthma, bronchitis, and pneumonia can present with a fever, cough, and radiograph findings, they are not usually associated with a rash. Identifying and removing the offending agent—a medication—is key in differentiating this disease from other common lung ailments.
Stop the offending agent, consider corticosteroids
Immediately discontinuing nitrofurantoin is usually sufficient to resolve the symptoms of acute nitrofurantoin-induced lung disease, often within 24 to 48 hours. Chest radiograph and PFT changes resolve within weeks of discontinuation. (Reintroducing nitrofurantoin to the patient will produce similar symptoms with a more rapid onset.) Corticosteroids are often used to treat this lung injury, although their effectiveness remains unproven.
With the chronic reaction, nitrofurantoin therapy is stopped and most patients are started on corticosteroids, typically dosed at 20 to 40 mg per day with a prolonged taper over several months. With treatment, many patients recover from their chronic pulmonary reaction, although it may take months to years.3 Some patients may never fully recover and continue to have symptoms, radiographic findings, and PFT changes characteristic of pulmonary fibrosis.
More seriously, nitrofurantoin-induced lung disease may require hospitalization. Rare cases have required lung transplantation and others have resulted in death due to respiratory failure.1
A speedy recovery for our patient
We told our patient to discontinue the nitrofurantoin, and we opted not to start her on corticosteroids. Her symptoms resolved within 3 days of discontinuing the medication, and she had no return of her UTI symptoms. Her rash also resolved within 5 days.
CORRESPONDENCE: Drew C. Baird, MD, Department of Family and Community Medicine, Carl R. Darnall Army Medical Center, 36000 Darnall Loop, Fort Hood, TX 76544; drew.baird@us.army.mil
A 66-YEAR-OLD WOMAN came into the emergency department with a diffuse rash and a cough. She had a rash on the palms of her hands, which had developed the day before, but had improved a bit. She also had a rash on her feet, legs, and lower abdomen, which had developed that morning.
She said that over the previous 2 days she’d had a fever, dry cough, and some difficulty breathing. Her past medical history was significant for asthma, diabetes, hypertension, and osteoarthritis. Her medications included atenolol, celecoxib, metformin, pioglitazone, and an albuterol inhaler, as needed. In addition, she was on the ninth day of a 10-day course of nitrofurantoin for acute cystitis. She was allergic to ampicillin and erythromycin.
On physical exam, she had a fever of 101.5°F. On lung examination, she had diffuse wheezes and mild bibasilar crackles. Examination of her skin revealed a nonpainful, nonpruritic, erythematous, maculopapular rash located on the palms and legs (FIGURES 1A AND 1B), as well as on her lower abdomen. Chest radiograph showed mild opacification in the bases of the lungs (FIGURES 2A AND 2B). Her labs were significant for a white blood cell (WBC) count of 11.3 ×103/mm3.
What is your diagnosis?
FIGURE 1
Rash on hands, feet, legs, and lower abdomen
The patient had generalized palmar erythema with 1- to 2-mm papules (A). She also had an erythematous maculopapular rash that extended from the medial and dorsal aspects of her feet cranially to her lower abdomen (B).
FIGURE 2
Mild opacification in lung bases
A posterior-anterior chest radiograph revealed bilateral lower lung opacities that were greater on the left side than on the right (A). A lateral chest radiograph revealed a positive spine sign: failure of the vertebral bodies to become more radiolucent as one looks down the spinal column, suggesting a posterior-inferior lung infiltrate that opacifies the normally radiolucent vertebral bodies of the lower chest (B).
Diagnosis: nitrofurantoin-induced lung disease
Nitrofurantoin (Macrodantin, Macrobid) is frequently used as first-line treatment for uncomplicated urinary tract infections (UTIs) and as prophylaxis for recurrent UTIs. Although generally well tolerated, it has a rare but serious side effect profile, including aplastic anemia, peripheral neuropathy, liver toxicity, and—as in the case of this patient—pulmonary toxicity.1
Nitrofurantoin-induced lung disease has an incidence of 3 cases per 1000 patients.2 Not surprisingly, elderly women are often affected, as this population is particularly susceptible to UTIs (and their recurrence), and thus are prescribed nitrofurantoin.3 The pathophysiology of the acute and chronic form of this drug reaction is unknown, but may be either an immunologic hypersensitivity reaction or a direct cytotoxic effect by nitrofurantoin or its metabolites on the lung parenchyma.4
The acute presentation begins within 3 weeks of initiation of nitrofurantoin. The most common symptoms include fever, dry cough, and dyspnea. Less common symptoms include an erythematous maculopapular rash, fatigue, arthralgias/myalgias, and anorexia. Patients may experience bronchospasm and have audible wheezing on exam. Eight percent of patients will have an abnormal chest radiograph, most often showing diffuse interstitial infiltrates or pleural effusions. An elevated WBC count appears in 40% of patients, many having an eosinophilia, and an elevated erythrocyte sedimentation rate may be present.5 Pulmonary function tests (PFTs), if performed, will show a restrictive pattern and a V/Q scan will show a ventilation-perfusion mismatch.2
The chronic presentation is much less common than the acute form. It occurs in patients on daily nitrofurantoin and its onset is delayed months to years after initiation of therapy. Symptoms are insidious and include cough and gradually worsening dyspnea on exertion. Physical exam may reveal wheezing or crackles and chest radiograph can show interstitial or alveolar infiltrates, as well as pleural effusions. Laboratory evaluation is similar to the acute form, and PFT findings also reveal a restrictive pattern.
Computed tomography has variable findings, such as ground-glass opacities, interstitial fibrosis, consolidation, peribronchial thickening, and centrilobular nodules. Lung biopsies have shown varying pathologic features: nonspecific interstitial pneumonia, pulmonary fibrosis, bronchiolitis obliterans organizing pneumonia, and hypersensitivity pneumonitis. 6,7
Differential Dx includes anaphylaxis, pneumonia
The differential diagnosis for nitrofurantoin-induced lung disease includes anaphylaxis, asthma, bronchitis, and pneumonia. Drug anaphylaxis typically occurs within hours of administration and often has skin findings of urticaria, pruritus, and angioedema of the oral mucosa. Patients may present with dyspnea, wheezing, stridor, hypoxemia, and respiratory distress.8
Although asthma, bronchitis, and pneumonia can present with a fever, cough, and radiograph findings, they are not usually associated with a rash. Identifying and removing the offending agent—a medication—is key in differentiating this disease from other common lung ailments.
Stop the offending agent, consider corticosteroids
Immediately discontinuing nitrofurantoin is usually sufficient to resolve the symptoms of acute nitrofurantoin-induced lung disease, often within 24 to 48 hours. Chest radiograph and PFT changes resolve within weeks of discontinuation. (Reintroducing nitrofurantoin to the patient will produce similar symptoms with a more rapid onset.) Corticosteroids are often used to treat this lung injury, although their effectiveness remains unproven.
With the chronic reaction, nitrofurantoin therapy is stopped and most patients are started on corticosteroids, typically dosed at 20 to 40 mg per day with a prolonged taper over several months. With treatment, many patients recover from their chronic pulmonary reaction, although it may take months to years.3 Some patients may never fully recover and continue to have symptoms, radiographic findings, and PFT changes characteristic of pulmonary fibrosis.
More seriously, nitrofurantoin-induced lung disease may require hospitalization. Rare cases have required lung transplantation and others have resulted in death due to respiratory failure.1
A speedy recovery for our patient
We told our patient to discontinue the nitrofurantoin, and we opted not to start her on corticosteroids. Her symptoms resolved within 3 days of discontinuing the medication, and she had no return of her UTI symptoms. Her rash also resolved within 5 days.
CORRESPONDENCE: Drew C. Baird, MD, Department of Family and Community Medicine, Carl R. Darnall Army Medical Center, 36000 Darnall Loop, Fort Hood, TX 76544; drew.baird@us.army.mil
1. Goemaere N, Grijm K, van Hal P, et al. Nitrofurantoin-induced pulmonary fibrosis: a case report. J Med Case Reports. 2008;2:169.-
2. Hainer BL, White AA. Nitrofurantoin pulmonary toxicity. J Fam Pract. 1981;13:817-823.
3. Bhullar S, Lele SM, Kraman S. Severe nitrofurantoin lung disease resolving without the use of steroids. J Postgrad Med. 2007;53:111-113.
4. Peall AF, Hodges A. Concomitant pulmonary and hepatic toxicity secondary to nitrofurantoin: a case report. J Med Case Reports. 2007;1:59.-
5. Holmberg L, Boman G, Bottiger LE, et al. Adverse reactions to nitrofurantoin. Analysis of 921 reports. Am J Med. 1980;69:733-738.
6. Mendez JL, Nadrous HF, Hartman TE, et al. Chronic nitrofurantoin-induced lung disease. Mayo Clin Proc. 2005;80:1298-1302.
7. Cameron RJ, Kolbe J, Wilsher ML, et al. Bronchiolitis obliterans organizing pneumonia associated with the use of nitrofurantoin. Thorax. 2000;55:249-251.
8. Tang AW. A practical guide to anaphylaxis. Am Fam Physician. 2003;68:1325-1332.
1. Goemaere N, Grijm K, van Hal P, et al. Nitrofurantoin-induced pulmonary fibrosis: a case report. J Med Case Reports. 2008;2:169.-
2. Hainer BL, White AA. Nitrofurantoin pulmonary toxicity. J Fam Pract. 1981;13:817-823.
3. Bhullar S, Lele SM, Kraman S. Severe nitrofurantoin lung disease resolving without the use of steroids. J Postgrad Med. 2007;53:111-113.
4. Peall AF, Hodges A. Concomitant pulmonary and hepatic toxicity secondary to nitrofurantoin: a case report. J Med Case Reports. 2007;1:59.-
5. Holmberg L, Boman G, Bottiger LE, et al. Adverse reactions to nitrofurantoin. Analysis of 921 reports. Am J Med. 1980;69:733-738.
6. Mendez JL, Nadrous HF, Hartman TE, et al. Chronic nitrofurantoin-induced lung disease. Mayo Clin Proc. 2005;80:1298-1302.
7. Cameron RJ, Kolbe J, Wilsher ML, et al. Bronchiolitis obliterans organizing pneumonia associated with the use of nitrofurantoin. Thorax. 2000;55:249-251.
8. Tang AW. A practical guide to anaphylaxis. Am Fam Physician. 2003;68:1325-1332.