User login
College Health May Be Full of Surprises: International Travelers and Tropical Diseases
CE/CME No: CR-1602
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain how accessibility to travel affects the etiology of illness.
• Understand the typical and atypical signs and symptoms of malaria, dengue fever, and chikungunya.
• Identify the proper laboratory workup and treatment for malaria, dengue fever, and chikungunya.
• Discuss multiple ways to prevent mosquito-borne illness in your patients and the importance of a pretravel consultation.
FACULTY
Eve B. Hoover is completing a postgraduate academic fellowship at Midwestern University at Glendale, Arizona, and practices at Logistics Health, Inc, in Phoenix.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of February 2016.
Article begins on next page >>
As the number of international travelers increases, so does the likelihood of transmission of illnesses to locations where they were previously rarely diagnosed. Clinicians at college health centers must be aware of tropical medicine diagnoses, especially in returning international students who have fever and other constitutional symptoms. This article provides a refresher regarding the diagnoses of malaria, dengue fever, and chikungunya.
Travel, whether for work, education, or pleasure, continues to increase, with the number of international travelers exceeding 1.1 billion in 2014.1 International travelers may unknowingly expose themselves and others to multiple health hazards previously thought to be foreign to the United States. Jane Zuckerman, who works with the World Health Organization (WHO), has noted that just over a century ago, the first human flew in an aircraft.2 Now, the sky is no longer the limit, and genes and micro-organisms travel as freely as their human hosts.
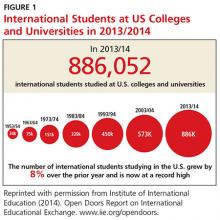
The international student population at American universities is at an all-time high (see Figure 1). Study abroad programs, which include American students who travel to developed and underdeveloped countries, also continue to increase. According to the CDC, the number of American students studying abroad has increased more than threefold in the past 20 years.3 According to the Institute of International Education, 304,467 American college students studied abroad in 2013/2014.4 Historically, most American students studied abroad in European countries, but in recent years the list of destinations has expanded, with increases in the percentage of students who travel to Africa, Asia, and the Middle East, and decreases in the percentage choosing Europe and Oceania.3
The sizable number of international students at universities, combined with the study abroad programs, have broadened the scope of the campus health care provider’s differential diagnosis. Diseases and infections that occur in developing countries can differ from those commonly seen in the US and Europe. It is important for health care providers to be reminded of conditions they seldom see and for a tropical medicine zebra to be considered in the appropriate patient population.
Continue for three causes of fever in returning travelers >>
THREE CAUSES OF FEVER IN RETURNING TRAVELERS
There are numerous etiologies for fever in the returning traveler. Factors such as location of travel, length of stay, dates of travel, date of symptom onset, risk activities undertaken, and reason for visit help determine the cause of illness.5 Two of the most commonly encountered conditions causing illness in the febrile traveler are dengue fever and malaria. Additionally, chikungunya is an emerging health concern in the US that has received increased attention following a massive outbreak in the Caribbean (which affected many American travelers) in 2013. In a retrospective study of patient records from 462 febrile adults who traveled to malaria-endemic areas, Siikamäki and colleagues found that every fourth febrile returning traveler had an illness that was potentially life-threatening.6 Understanding the possible causes of febrile illness in travelers can aid the clinician in diagnosing and correctly treating potentially life-threatening conditions.
Malaria
Malaria is a mosquito-borne illness transmitted in humans by female Anopheles mosquitoes.7 It is caused by infection with the protozoal parasites Plasmodium falciparum, P vivax, P ovale, P malariae, and occasionally other Plasmodium species.8 An infected female Anopheles mosquito transmits the parasite into a human host through a bite. The most severe form of human malaria, which can be fatal, is caused by P falciparum. Falciparum and vivax malaria are the most common forms of malaria worldwide.8
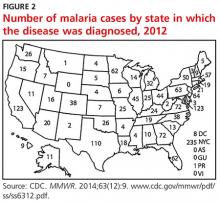
According to the WHO, there were an estimated 214 million clinical episodes of malaria worldwide, and malaria was the cause of 438,000 deaths, in 2015.9 In 2012, the CDC received reports of 1,687 cases of malaria in the US.8 The number of malaria cases has been steadily increasing since 1973.8 Figure 2 shows the number of malaria cases diagnosed in each state in 2012. The data demonstrate that malaria is the primary cause of death in travel-related fever. Malaria is also the most common single reason for travel-related fever without findings on exam or workup.
Dengue fever
Dengue is a mosquito-borne disease (transmitted by an infected Aedes mosquito) and is caused by four types of flaviviruses (DENV-1, DENV-2, DENV-3, DENV-4).10 It is the most common arboviral disease in humans.11 In 2009, the WHO revised its dengue categories to include dengue, dengue with warning signs, and severe dengue.12,13 Previously, the categories included dengue fever, dengue hemorrhagic fever, and dengue shock syndrome.
Dengue is endemic throughout the tropics and subtropics and is a leading cause of febrile illness among travelers returning from the Caribbean, South America, and South and Southeast Asia.14 There has been a 30-fold increase in dengue fever in the past 50 years.10 This illness is present in more than 100 countries; in the US, outbreaks have occurred in Florida, Hawaii, and along the Texas-Mexico border.14
Chikungunya
Chikungunya virus (CHIKV) is an arbovirus that is transmitted by Aedes mosquitoes (Aedes aegypti and Aedes albopictus).15 The term chikungunya is derived from a word in the Swahili and Maconde language that means “the one that is folded.”16 This description refers to the severe arthralgias that can cause a hunched-over gait in the patient with chikungunya.
Chikungunya historically has not had a significant impact in the Americas or Europe. However, more than one million suspected cases of chikungunya have been reported in the Americas since October 2013.16 Most cases of CHIKV infection diagnosed in the US have occurred in travelers; however, there have also been documented cases of local transmission of the virus.17 Local transmission occurs when the ill returning traveler unknowingly spreads disease, with the aid of the mosquito vector, upon return to the US.
Continue for patient presentation >>
PATIENT PRESENTATION
A 19-year-old previously healthy male student presented to the university health clinic for evaluation. During the exam, he lay on the examination table, covered with a blanket and shaking uncontrollably with intense rigors. Although he was hesitant to answer questions due to feeling so ill, he reported that he had returned from India two weeks prior and his symptoms—fever, rigors, ache, fatigue, headache, and nausea—began abruptly, hours before his arrival at the clinic.
The patient was diaphoretic and taking rapid, shallow inspirations. Assessment of vital signs revealed a blood pressure of 148/86 mm Hg; respiratory rate, 24 breaths/min; temperature, 103°F; and heart rate, 112 beats/min.
HEENT evaluation showed dry mucous membranes but no other abnormality. Neck was supple with no lymphadenopathy or nuchal rigidity. On cardiac exam, there were no murmurs or rubs. Lungs were clear to auscultation. Abdomen was soft and nontender, and bowel sounds were present in all four quadrants. There was no costovertebral angle tenderness. Skin was warm, clammy, and without rash. There were no focal neurologic deficits.
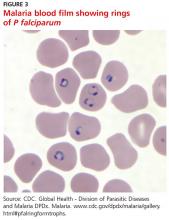
Complete blood count, comprehensive metabolic panel, and urinalysis were without abnormality. Examination of thick and thin blood smears revealed multiple red blood cells (RBCs) infected with malaria parasites and the appearance of the classic “headphone” form within the cells. Based on the in-office laboratory results of the blood smear, the patient was diagnosed with malaria.
The patient was not surprised by the diagnosis, as he had experienced these same symptoms with previous bouts of malaria. He and his family were from India, and the patient was an international college student. He had not taken malaria chemoprophylaxis prior to his most recent trip. After a short hospital admission for hydration, observation, treatment, and consultation by an infectious disease specialist, the patient was released back to the demands of college life.
Continue for signs and symptoms >>
SIGNS AND SYMPTOMS
Malaria
Signs and symptoms of malaria can vary greatly from none to illness causing death. The classic clinical features of malaria (fever, headache, back pain, chills, sweating, myalgia, nausea, vomiting, and cough) are caused by the parasite developing in RBCs, causing toxins to accumulate.18 Following the mosquito bite, there is typically an incubation period of seven to 30 days.
When first diagnosing malaria, the clinician needs to determine if the cause is P falciparum (the most severe form of malaria). If so, the clinician then must determine if the case is severe or nonsevere.7 In P falciparum infections, symptom onset can be later, especially if the patient took prophylaxis.7 Longer incubation periods are often seen with P vivax, P malariae, and P ovale infections. P vivax and P ovale can lie dormant in hepatic cells and reactivate after months or even years.7
Adults and children may experience different malaria symptoms, particularly with severe forms of the disease. Pediatric patients with severe falciparum malaria may experience respiratory distress, convulsions, and hypoglycemia more commonly than adults. More than half of adults with severe falciparum experience acute respiratory distress syndrome and acute renal failure.7 Pregnant women are at increased risk for complications.
Dengue fever
Approximately 75% of patients infected with DENV are asymptomatic.14 However, if symptomatic, the most common symptoms (fever, myalgia, headache, rash, arthralgia, abdominal pain, and nausea) begin abruptly after an incubation period of four to seven days.
Dengue can also present with atypical manifestations. In a prospective study by Nimmagadda and colleagues involving 150 participants with confirmed dengue fever, more than half of subjects had at least one atypical symptom along with more typical symptoms.10 The most common atypical manifestation was abnormal liver function, which was present in 40.6% of participants. Other atypical symptoms seen were febrile diarrhea (12%), renal failure (8%), acalculous cholecystitis (6.6%), and conduction abnormalities of the heart (6%). Less common atypical manifestations observed in this study included encephalitis, seizures, acute respiratory distress syndrome, disseminated intravascular coagulation, acute pancreatitis, myositis, and atrial fibrillation. The authors recommended that clinicians maintain a high level of vigilance for atypical manifestations of dengue fever, noting that most of the severe complications of dengue can be avoided if the disease is diagnosed correctly early in the course of illness.
Chikungunya
The typical presentation of CHIKV infection is a patient who abruptly develops fever, headache, polyarthralgia, and myalgia. The joint pain most frequently affects the small joints, such as the interphalangeal joints of the hands as well as the ankles and wrists.15 Back pain is also common, and rash is present in more than half of cases. The rash in adults can be maculopapular and in children is more often bullous. Fever, rash, and headache typically last seven to 10 days, while the arthralgia can last much longer—three to four months in a third of patients and three to five years in 10%.15
CHIKV infection that presents with typical clinical manifestations is usually self-limited; however, more severe atypical symptoms can occur and may lead to long-term morbidity. These atypical manifestations of chikungunya, which are rare, include acute disseminated encephalomyelitis, aseptic meningitis, meningoencephalitis, sensorineural hearing loss, myelitis, myeloradiculopathy, and Guillain-Barré syndrome.19 Chikungunya also has been associated with bleeding manifestations, acute renal failure, and electrolyte disturbance.19
Continue for the diagnosis >>
DIAGNOSIS
Malaria
The clinical presentation of malaria is nonspecific, so it is important to identify patients with a travel history and perform testing when this diagnosis is suspected.7,8 The gold standard for diagnosing malaria remains microscopy of thick and thin films of the patient’s peripheral blood.7 In patients with blood-stage malaria, a blood slide will show multiple infected RBCs and the appearance of the classic “headphone” form within the cells (see Figure 3). This test allows for efficient detection of malaria parasites, determination of parasite species, and calculation of percent parasitemia. Early differentiation between falciparum and nonfalciparum malaria is required, since P falciparum is the most life-threatening form of malaria.7 All of these factors are key to determining the best treatment plan for each patient.8
Rapid diagnostic tests (RDTs) and polymerase chain reaction (PCR) for malaria are increasingly available for use in US laboratories. In comparison to microscopy, these newer diagnostic tools are slower, more costly, and less readily available. For this reason, microscopy remains the most common means of diagnosis.7 PCR is helpful for species confirmation of malaria parasites and can be used to confirm a positive result on microscopy.8
It is possible for the first malaria test to be negative, and performing a repeat test the following day in a stable patient is recommended.7 However, more than three tests are not needed as long as the patient’s symptoms are not changing.
Dengue fever
Laboratory diagnosis of dengue can be confirmed with detection of DENV genomic sequences through PCR or nonstructural protein 1 antigen by immunoassay.14 Virus isolation in cell culture, detection of viral RNA by nucleic acid amplification tests, and detection of viral antigens by rapid tests or enzyme-linked immunosorbent assay (ELISA) are most useful if a patient presents within five days of fever onset.13
After five days of febrile illness, dengue viruses and antigens disappear from the blood as the specific antibody levels rise.13 Therefore, ELISA testing for immunoglobulin (Ig) M anti-DENV is a more effective lab study for dengue in patients presenting after one week. Testing for IgG anti-DENV is not recommended for making a diagnosis, however, because this antibody remains elevated for life after any DENV infection, leading to many false-positive test results. 14
A useful diagnostic aid for detecting severe dengue is the tourniquet test, which assesses for microvascular fragility. To perform the test, inflate a blood pressure cuff on the arm to midway between systolic and diastolic blood pressures, and maintain pressure for five minutes. After releasing the pressure, count the number of petechea in one square inch of skin; if 20 or more are found, the test is positive.12
Chikungunya
Chikungunya laboratory testing is limited in the US due to lack of availability. Testing is available only at the CDC, one commercial laboratory, and a few state health departments.17
The only reliable method for diagnosing CHIKV infection is through testing of blood samples. Chikungunya should not be diagnosed clinically because of the difficulty in differentiating it from dengue fever and other viral illnesses. The laboratory diagnosis of CHIKV infection can be obtained through detection of the virus, viral RNA, or specific antibodies related to chikungunya.20 Serologic detection of IgM or IgG antibodies is the most common method of diagnosis and is recommended by the CDC.20 If initial IgM and IgG testing is negative but clinical suspicion remains high, repeat testing should be done during the convalescent phase of the illness (≥ 7 days after symptom onset).21 Reverse transcriptase PCR is an effective diagnostic laboratory method for chikungunya and can be used in the first seven days of illness.20 ELISA and the hemagglutination inhibition assay can also provide diagnostic information.20
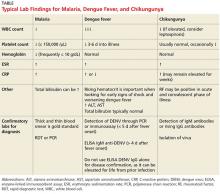
Lab findings associated with malaria, dengue fever, and chikungunya are summarized in the Table.
Continue for differentiating between dengue, malaria, and chikungunya early in presentation >>
Differentiating between dengue, malaria, and chikungunya early in presentation
Hematologic parameters can be used as a diagnostic aid when differentiating among certain causes of fever, as noted in a study by Joshi and Shah.22 In the setting of a febrile illness, thrombocytopenia (platelet count < 150,000/µL) is a predictor of malaria, especially in combination with anemia (hemoglobin < 10 g/dL). Thrombocytopenia is also common with dengue fever, but patients with dengue typically have normal hemoglobin. According to Joshi and Shah, patients having the combination of anemia and thrombocytopenia were 22 times more likely to have malaria than patients without these laboratory findings.22
Kutsuna and colleagues also found disease-specific clues in laboratory data when differentiating between dengue fever and malaria. Patients with dengue fever had significantly lower white blood cell counts than patients with malaria.23 In addition, although thrombocytopenia is seen in both dengue fever and malaria, platelet counts are lower in patients with malaria at first presentation. However, with dengue fever the platelet count can decrease three to six days into the illness when fever abates.23 Furthermore, total bilirubin tends to increase in malaria but is unaffected in dengue fever. Last, C-reactive protein can be helpful in assessing malaria severity and clinical improvement at follow-up, as well as for differentiating malaria from other conditions (eg, dengue), especially if the value is greater than 10 mg/L.23
Distinguishing chikungunya from dengue fever in the early stages of illness is difficult, and there is no pathognomonic hematologic laboratory study that helps with this task. With both diseases, the patient may have leukopenia, elevated erythrocyte sedimentation rate, and (rarely) thrombocytopenia. Chipwaza and colleagues discuss the significant overlap in symptoms in nonmalaria febrile illness. The overlap makes clinical diagnosis difficult; lab testing is essential for establishing the diagnosis.21 Once CHIKV is confirmed, the clinician is typically reassured of a more benign, self-limited course.
Continue for treatment/management >>
TREATMENT / MANAGEMENT
Malaria
The treatment of malaria varies depending on the severity of disease and the probability the organism is resistant to antimalarial drugs. The likelihood of drug resistance is determined based on the species of malaria parasite and the location where the infection occurred.24
Malaria is considered severe if one or more of the following are present: neurologic sequelae, renal failure, severe anemia, ARDS, jaundice, or parasite burden greater than 5%.8 Patients with severe malaria are treated with parenteral (IV) antimalarials; the two options for parenteral medication are quinine and artesunate.7 All patients treated with parenteral antimalarial agents should take a full course of oral medication for malaria as well. Oral antimalarial medications include, but are not limited to, quinine sulfate, atovaquone/proguanil, artemether-lumefantrine, doxycycline, clindamycin, sulfadoxine/pyrimethamine, chloroquine, and primaquine. The oral medications most commonly used to treat nonfalciparum malaria are chloroquine followed by primaquine.7 Chloroquine is not typically used for falciparum malaria due to widespread resistance.7
In cases of malaria caused by P vivax or P ovale infection, the likelihood of parasitic infection lying dormant in the liver must be considered. Additional treatment is often needed to eradicate this type of infection.7 The relapse of symptoms can occur years after the acute attack.25 Primaquine is the only approved medication for preventing and treating parasitic relapse associated with dormant infection.25
Dengue fever
The typical course of dengue follows three phases: febrile, critical, and convalescent.14 Dengue is usually a self-limiting febrile illness and typically resolves within one week after symptom onset without major complications.11 During the critical phase, most patients begin to improve, but up to 5% of cases develop concerning warning signs and symptoms that could represent a life-threatening condition that requires intense treatment and close monitoring.14 Warning signs for worsening disease are caused by marked increase in vascular permeability and include narrow pulse pressure, pleural effusions, ascites, and hemorrhagic manifestations (hematemesis, melena, menorrhagia).14
Treatment of most cases of dengue involves use of acetaminophen for comfort and fever reduction, hydration, and rest.26 Treatment of worsening dengue includes inpatient admission and possibly ICU admission for close observation and frequent monitoring.14 It is important to avoid aspirin and other NSAIDs due to the risk for bleeding complications in severe dengue.14 There are no approved antivirals for treatment of dengue. To reduce the risk for transmission of dengue, febrile patients should avoid further mosquito bites.14
Clinicians should be aware of warning signs of worsening illness with dengue fever. Signs of worsening dengue fever include postural hypotension, thrombocytopenia, decrease in serum albumin, and rising hematocrit.10
Chikungunya
CHIKV illness is usually a self-limiting condition. Diagnosis of chikungunya may take time, and providers should assume the chikungunya patient may have dengue, which has the potential to be more pathologic. Accordingly, they must watch for warning signs of dengue until CHIKV is confirmed.27
Management focuses on supportive care, including hydration and rest. Typically, the medications used are antipyretics (acetaminophen and ibuprofen) and analgesics; no antiviral medication for chikungunya is available.22 Aspirin is avoided due to the risk for Reye syndrome. Antihistamines may be helpful for patients who have an associated pruritic rash. Cold compresses can be beneficial for joint pain and swelling. Additionally, it is important to keep patients under mosquito nets during the febrile phase to decrease the risk for disease transmission.
Continue for patient education >>
PATIENT EDUCATION
Vaccination
Vaccines are not available for dengue fever, malaria, or chikungunya. However, researchers have been working on a vaccine for malaria for decades, and presently, more than 20 vaccine constructs are being tested and researched in preclinical trials.28 Similarly, efforts to develop an effective vaccine for chikungunya have been under way since the 1970s.15
Chemoprophylaxis
There are no chemoprophylaxis options available for dengue or chikungunya. The most effective measures to prevent dengue are strategies aimed at avoiding mosquito bites (ie, vector control and individual protections like repellants).16 One group of authors notes that developing a larger network of research laboratories capable of prompt diagnosis of arbovirus infections would help to better control chikungunya.
Multiple options for malaria chemoprophylaxis are available, and these vary by country of travel. Chemoprophylaxis options include doxycycline, mefloquine, atovaquone/proguanil, chloroquine, and primaquine.8 For dormant forms of malaria residing in the liver, primaquine is the only effective treatment.8
It is important to remember that no antimalarial drug is 100% protective. Malaria chemoprophylaxis reduces the risk for malaria, but it is often taken inadequately, which can delay symptom onset and lead to a false-negative result on initial blood films.5 All patients with fever who have visited a tropical country within one year of presentation should be screened for malaria.5 It is incorrect and dangerous to assume that a patient who received malaria chemoprophylaxis does not have malaria. Diagnosis of malaria requires a high index of suspicion, and clinicians must remember that malaria can occur even with perfect prophylaxis.7 Unfortunately, malaria parasites are becoming resistant to some commonly used antimalarial drugs. Resistance patterns are being tracked by the CDC.8
Pretravel visit with clinician
Many illnesses related to travel can be prevented with vaccination, chemoprophylaxis, and patient education. However, many travelers do not visit a health care professional before travel (even among those traveling to perceived “risky” destinations, such as Sub-Saharan Africa).29 In a study of ill returned travelers, Leder and colleagues found that only 40% had sought pretravel advice from providers. Interestingly, many of those ill patients who obtained a pretravel consult did not receive appropriate vaccines, such as hepatitis A or influenza vaccine. Some of these patients were diagnosed with preventable conditions.29
Open and thorough communication between clinicians and patients is paramount to protect travelers from disease and illness. Clinicians have the opportunity to greatly impact the health of their patients by recommending a pretravel consultation. What may take extra time and effort on the front end of the trip may save significant time and energy on the back end, and even save lives.
Mosquito bite avoidance
One of the most important patient education discussions in pretravel consultation is mosquito bite avoidance. Travelers should be advised to find accommodations with air conditioning and screened windows and doors.14 To avoid mosquito bites, they should cover their arms and legs adequately with proper clothing. Standing water (such as in flower pots), which can encourage mosquito breeding, should be avoided as well. Travelers should use insect repellents and insecticides, especially in cool, dark areas (eg, closets and bathrooms) where mosquitoes hide.14
Continue for follow-up >>
FOLLOW-UP
Malaria
Appropriate follow-up, need for hospitalization, and choice of medical treatment are determined by disease cause, severity of illness, and patient demographics. Follow-up is necessary to ensure improvement and no development of atypical symptoms. Additionally, the clinician needs to keep in mind the risk for malaria strains that can have a dormant stage.
Dengue fever
Clinicians must remind convalescing patients to watch for severe abdominal pain, vomiting, difficulty breathing, and signs of bleeding (epistaxis, bruising, bloody stool, and menorrhagia). Clinicians must also be attentive to changing lab values, including a decrease in platelet count and an increase in hematocrit, along with signs of hypovolemic shock, ascites, pleural effusions, and narrow pulse pressure.14
Chikungunya
Patients are reminded to keep themselves comfortable by rehydrating and treating the discomfort associated with arthralgias. In a longitudinal study of chikungunya patients, 60% experienced continued arthralgias three years after diagnosis.23,30 Patient education regarding the potential for long-term arthralgia is important, as it may impact activities of daily living and work.
Long-term NSAIDs have been used for patients with recurrent or even chronic arthralgia.31 There are limited data available on beneficial treatments, such as chloroquine sulfate or disease-modifying antirheumatic drugs, for chronic arthralgia associated with chikungunya.23 Depression and recurrent cutaneous lesions also are possible in patients with long-term symptoms.
Continue for the conclusion >>
CONCLUSION
“People, as well as pathogens, travel from all around the world in all directions.”32 With the ever-increasing mobility of populations around the world, transmission of illness and medical norms are constantly changing. All clinicians should keep in mind the less commonly seen diagnostic entities and remember the importance of obtaining a complete travel history in the febrile patient.
Early detection and appropriate supportive care of patients with dengue fever and malaria can be lifesaving. In addition, proper pretravel consultations can provide a wealth of patient education for at-risk travelers and help prevent a number of debilitating infectious diseases.
1. World Tourism Organization. Over 1.1 billion tourists travelled abroad in 2014 [press release]. January 27, 2015. http://media.unwto.org/press-release/2015-01-27/over-11-billion-tourists-travelled-abroad-2014. Accessed January 21, 2016.
2. Zuckerman JN. Public health and travel medicine: intricately intertwined. Perspect Public Health. 2012;132(5):206.
3. Rhodes G, DeRomaña I, Ebner J. Advising travelers with special needs: study abroad & other international student travel. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellow book/2016/advising-travelers-with-specific-needs/study-abroad-other-international-student-travel. Accessed January 21, 2016.
4. Institute of International Education. US study abroad: all destinations. www.iie.org/Research-and-Publications/Open-Doors/Data/US-Study-Abroad/All-Destinations/2012-14. Accessed January 21, 2016.
5. Hearn P, Johnston V. Assessment of returning travelers with fever. Medicine. 2014;42(2):66-72.
6. Siikamäki HM, Kivelä PS, Sipilä PN, et al. Fever in travelers returning from malaria-endemic areas: don’t look for malaria only. J Travel Med. 2011;18(4):239-244.
7. Walker NF, Nadjm B, Whitty CJ. Malaria. Medicine. 2014;42(2):100-106.
8. Cullen KA, Arguin PM. Malaria surveillance—United States, 2012. MMWR Surveill Summ. 2014;63(12):1-22.
9. World Health Organization. Malaria. Fact sheet no. 94. www.who.int/mediacentre/factsheets/fs094/en/. Accessed January 21, 2016.
10. Nimmagadda SS, Mahabala C, Boloor A, et al. Atypical manifestations of dengue fever (DF)—where do we stand today? J Clin Diagn Res. 2014;8(1):71-73.
11. Whitehorn J, Yacoub S, Anders KL, et al. Dengue therapeutics, chemoprophylaxis, and allied tools: state of the art and future directions. PLoS Negl Trop Dis. 2014;8(8):e3025.
12. Mayxay M, Phetsouvanh R, Moore CE, et al. Predictive diagnostic value of the tourniquet test for the diagnosis of dengue infection in adults. Trop Med Int Health. 2011;16(1):127-133.
13. World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. WHO/HTM/NTD/DEN/2009.1. www.who.int/tdr/publications/documents/dengue-diagnosis.pdf. Accessed January 21, 2016.
14. Tomashek KM, Sharp TM, Margolis HS. Infectious diseases related to travel: dengue. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/dengue. Accessed January 21, 2016.
15. Vega-Rúa A, Lourenço-de-Oliveira R, Mousson L, et al. Chikungunya virus transmission potential by local Aedes mosquitoes in the Americas and Europe. PLoS Negl Trop Dis. 2015;9(5):1-18.
16. Hrnjakovi`c Cvjetkovi`c IB, Cvjetkovi`c D, Pati`c A, et al. Chikungunya—a serious threat for public health. Med Pregl. 2015;68(3/4):122-125.
17. Lindsey NP, Prince HE, Kosoy O, et al. Chikungunya virus infections among travelers-United States, 2010-2013. Am J Trop Med Hyg. 2015;92(1):82-87.
18. CDC. Malaria. www.cdc.gov/malaria/about/disease.html. Accessed January 21, 2016.
19. Das S, Sarkar N, Majumder J, et al. Acute disseminated encephalomyelitis in a child with chikungunya virus infection. J Pediatr Infect Dis. 2014;9(1):37-41.
20. Schwartz KL, Giga A, Boggild AK. Chikungunya fever in Canada: fever and polyarthritis in a returned traveller. CMAJ. 2014;186(10):772-774.
21. Chipwaza B, Mugasa JP, Selemani M, et al. Dengue and chikungunya fever among viral diseases in outpatient febrile children in Kilosa district hospital, Tanzania. PLoS Negl Trop Dis. 2014;8(11):e3335.
22. Joshi HA, Shah SS. Platelet count—a diagnostic aid in fever. Natl J Integrated Res Med. 2013;4(3):128-132.
23. Kutsuna S, Hayakawa K, Kato Y, et al. Comparison of clinical characteristics and laboratory findings of malaria, dengue, and enteric fever in returning travelers: 8-year experience at a referral center in Tokyo, Japan. J Infect Chemother. 2015;21(4):272-276.
24. CDC. Malaria diagnosis & treatment in the United States. www.cdc.gov/malaria/diagnosis_treatment/index.html. Accessed January 21, 2016.
25. Roy M, Bouma MJ, Ionides EL, et al. The potential elimination of Plasmodium vivax malaria by relapse treatment: insights from a transmission model and surveillance data from NW India. PLoS Negl Trop Dis. 2013;7(1):e1979.
26. Tither PH. Preventing dengue and chikungunya fever among international travelers. J Am Assoc Nurse Pract. 2014;26(11):584-594.
27. Mardekian SK, Roberts AL. Diagnostic options and challenges for dengue and chikungunya viruses. Biomed Res Int. 2015;2015:834371.
28. World Health Organization. Malaria vaccine development. www.who.int/malaria/areas/vaccine/en/#. Accessed January 21, 2016.
29. Leder K, Torresi J, Libman MD, et al. GeoSentinel Surveillance of illness in returned travelers, 2007-2011. Ann Intern Med. 2013;158(6):456-468.
30. Schilte C, Staikowsky F, Couderc T, et al. Chikungunya virus-associated long-term arthralgia: a 36-month prospective longitudinal study. PLoS Negl Trop Dis. 2013;7:e2137.
31. Essackjee K, Goorah S, Ramchurn SK, et al. Prevalence of and risk factors for chronic arthralgia and rheumatoid-like polyarthritis more than 2 years after infection with chikungunya virus. Postgrad Med. 2013;89:440-447.
32. Piyaphanee W, Steffen R, Shlim DR, et al. Travel medicine for Asian travelers—do we need new approaches? J Travel Med. 2012;19(6):335-337.
CE/CME No: CR-1602
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain how accessibility to travel affects the etiology of illness.
• Understand the typical and atypical signs and symptoms of malaria, dengue fever, and chikungunya.
• Identify the proper laboratory workup and treatment for malaria, dengue fever, and chikungunya.
• Discuss multiple ways to prevent mosquito-borne illness in your patients and the importance of a pretravel consultation.
FACULTY
Eve B. Hoover is completing a postgraduate academic fellowship at Midwestern University at Glendale, Arizona, and practices at Logistics Health, Inc, in Phoenix.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of February 2016.
Article begins on next page >>
As the number of international travelers increases, so does the likelihood of transmission of illnesses to locations where they were previously rarely diagnosed. Clinicians at college health centers must be aware of tropical medicine diagnoses, especially in returning international students who have fever and other constitutional symptoms. This article provides a refresher regarding the diagnoses of malaria, dengue fever, and chikungunya.
Travel, whether for work, education, or pleasure, continues to increase, with the number of international travelers exceeding 1.1 billion in 2014.1 International travelers may unknowingly expose themselves and others to multiple health hazards previously thought to be foreign to the United States. Jane Zuckerman, who works with the World Health Organization (WHO), has noted that just over a century ago, the first human flew in an aircraft.2 Now, the sky is no longer the limit, and genes and micro-organisms travel as freely as their human hosts.
The international student population at American universities is at an all-time high (see Figure 1). Study abroad programs, which include American students who travel to developed and underdeveloped countries, also continue to increase. According to the CDC, the number of American students studying abroad has increased more than threefold in the past 20 years.3 According to the Institute of International Education, 304,467 American college students studied abroad in 2013/2014.4 Historically, most American students studied abroad in European countries, but in recent years the list of destinations has expanded, with increases in the percentage of students who travel to Africa, Asia, and the Middle East, and decreases in the percentage choosing Europe and Oceania.3
The sizable number of international students at universities, combined with the study abroad programs, have broadened the scope of the campus health care provider’s differential diagnosis. Diseases and infections that occur in developing countries can differ from those commonly seen in the US and Europe. It is important for health care providers to be reminded of conditions they seldom see and for a tropical medicine zebra to be considered in the appropriate patient population.
Continue for three causes of fever in returning travelers >>
THREE CAUSES OF FEVER IN RETURNING TRAVELERS
There are numerous etiologies for fever in the returning traveler. Factors such as location of travel, length of stay, dates of travel, date of symptom onset, risk activities undertaken, and reason for visit help determine the cause of illness.5 Two of the most commonly encountered conditions causing illness in the febrile traveler are dengue fever and malaria. Additionally, chikungunya is an emerging health concern in the US that has received increased attention following a massive outbreak in the Caribbean (which affected many American travelers) in 2013. In a retrospective study of patient records from 462 febrile adults who traveled to malaria-endemic areas, Siikamäki and colleagues found that every fourth febrile returning traveler had an illness that was potentially life-threatening.6 Understanding the possible causes of febrile illness in travelers can aid the clinician in diagnosing and correctly treating potentially life-threatening conditions.
Malaria
Malaria is a mosquito-borne illness transmitted in humans by female Anopheles mosquitoes.7 It is caused by infection with the protozoal parasites Plasmodium falciparum, P vivax, P ovale, P malariae, and occasionally other Plasmodium species.8 An infected female Anopheles mosquito transmits the parasite into a human host through a bite. The most severe form of human malaria, which can be fatal, is caused by P falciparum. Falciparum and vivax malaria are the most common forms of malaria worldwide.8
According to the WHO, there were an estimated 214 million clinical episodes of malaria worldwide, and malaria was the cause of 438,000 deaths, in 2015.9 In 2012, the CDC received reports of 1,687 cases of malaria in the US.8 The number of malaria cases has been steadily increasing since 1973.8 Figure 2 shows the number of malaria cases diagnosed in each state in 2012. The data demonstrate that malaria is the primary cause of death in travel-related fever. Malaria is also the most common single reason for travel-related fever without findings on exam or workup.
Dengue fever
Dengue is a mosquito-borne disease (transmitted by an infected Aedes mosquito) and is caused by four types of flaviviruses (DENV-1, DENV-2, DENV-3, DENV-4).10 It is the most common arboviral disease in humans.11 In 2009, the WHO revised its dengue categories to include dengue, dengue with warning signs, and severe dengue.12,13 Previously, the categories included dengue fever, dengue hemorrhagic fever, and dengue shock syndrome.
Dengue is endemic throughout the tropics and subtropics and is a leading cause of febrile illness among travelers returning from the Caribbean, South America, and South and Southeast Asia.14 There has been a 30-fold increase in dengue fever in the past 50 years.10 This illness is present in more than 100 countries; in the US, outbreaks have occurred in Florida, Hawaii, and along the Texas-Mexico border.14
Chikungunya
Chikungunya virus (CHIKV) is an arbovirus that is transmitted by Aedes mosquitoes (Aedes aegypti and Aedes albopictus).15 The term chikungunya is derived from a word in the Swahili and Maconde language that means “the one that is folded.”16 This description refers to the severe arthralgias that can cause a hunched-over gait in the patient with chikungunya.
Chikungunya historically has not had a significant impact in the Americas or Europe. However, more than one million suspected cases of chikungunya have been reported in the Americas since October 2013.16 Most cases of CHIKV infection diagnosed in the US have occurred in travelers; however, there have also been documented cases of local transmission of the virus.17 Local transmission occurs when the ill returning traveler unknowingly spreads disease, with the aid of the mosquito vector, upon return to the US.
Continue for patient presentation >>
PATIENT PRESENTATION
A 19-year-old previously healthy male student presented to the university health clinic for evaluation. During the exam, he lay on the examination table, covered with a blanket and shaking uncontrollably with intense rigors. Although he was hesitant to answer questions due to feeling so ill, he reported that he had returned from India two weeks prior and his symptoms—fever, rigors, ache, fatigue, headache, and nausea—began abruptly, hours before his arrival at the clinic.
The patient was diaphoretic and taking rapid, shallow inspirations. Assessment of vital signs revealed a blood pressure of 148/86 mm Hg; respiratory rate, 24 breaths/min; temperature, 103°F; and heart rate, 112 beats/min.
HEENT evaluation showed dry mucous membranes but no other abnormality. Neck was supple with no lymphadenopathy or nuchal rigidity. On cardiac exam, there were no murmurs or rubs. Lungs were clear to auscultation. Abdomen was soft and nontender, and bowel sounds were present in all four quadrants. There was no costovertebral angle tenderness. Skin was warm, clammy, and without rash. There were no focal neurologic deficits.
Complete blood count, comprehensive metabolic panel, and urinalysis were without abnormality. Examination of thick and thin blood smears revealed multiple red blood cells (RBCs) infected with malaria parasites and the appearance of the classic “headphone” form within the cells. Based on the in-office laboratory results of the blood smear, the patient was diagnosed with malaria.
The patient was not surprised by the diagnosis, as he had experienced these same symptoms with previous bouts of malaria. He and his family were from India, and the patient was an international college student. He had not taken malaria chemoprophylaxis prior to his most recent trip. After a short hospital admission for hydration, observation, treatment, and consultation by an infectious disease specialist, the patient was released back to the demands of college life.
Continue for signs and symptoms >>
SIGNS AND SYMPTOMS
Malaria
Signs and symptoms of malaria can vary greatly from none to illness causing death. The classic clinical features of malaria (fever, headache, back pain, chills, sweating, myalgia, nausea, vomiting, and cough) are caused by the parasite developing in RBCs, causing toxins to accumulate.18 Following the mosquito bite, there is typically an incubation period of seven to 30 days.
When first diagnosing malaria, the clinician needs to determine if the cause is P falciparum (the most severe form of malaria). If so, the clinician then must determine if the case is severe or nonsevere.7 In P falciparum infections, symptom onset can be later, especially if the patient took prophylaxis.7 Longer incubation periods are often seen with P vivax, P malariae, and P ovale infections. P vivax and P ovale can lie dormant in hepatic cells and reactivate after months or even years.7
Adults and children may experience different malaria symptoms, particularly with severe forms of the disease. Pediatric patients with severe falciparum malaria may experience respiratory distress, convulsions, and hypoglycemia more commonly than adults. More than half of adults with severe falciparum experience acute respiratory distress syndrome and acute renal failure.7 Pregnant women are at increased risk for complications.
Dengue fever
Approximately 75% of patients infected with DENV are asymptomatic.14 However, if symptomatic, the most common symptoms (fever, myalgia, headache, rash, arthralgia, abdominal pain, and nausea) begin abruptly after an incubation period of four to seven days.
Dengue can also present with atypical manifestations. In a prospective study by Nimmagadda and colleagues involving 150 participants with confirmed dengue fever, more than half of subjects had at least one atypical symptom along with more typical symptoms.10 The most common atypical manifestation was abnormal liver function, which was present in 40.6% of participants. Other atypical symptoms seen were febrile diarrhea (12%), renal failure (8%), acalculous cholecystitis (6.6%), and conduction abnormalities of the heart (6%). Less common atypical manifestations observed in this study included encephalitis, seizures, acute respiratory distress syndrome, disseminated intravascular coagulation, acute pancreatitis, myositis, and atrial fibrillation. The authors recommended that clinicians maintain a high level of vigilance for atypical manifestations of dengue fever, noting that most of the severe complications of dengue can be avoided if the disease is diagnosed correctly early in the course of illness.
Chikungunya
The typical presentation of CHIKV infection is a patient who abruptly develops fever, headache, polyarthralgia, and myalgia. The joint pain most frequently affects the small joints, such as the interphalangeal joints of the hands as well as the ankles and wrists.15 Back pain is also common, and rash is present in more than half of cases. The rash in adults can be maculopapular and in children is more often bullous. Fever, rash, and headache typically last seven to 10 days, while the arthralgia can last much longer—three to four months in a third of patients and three to five years in 10%.15
CHIKV infection that presents with typical clinical manifestations is usually self-limited; however, more severe atypical symptoms can occur and may lead to long-term morbidity. These atypical manifestations of chikungunya, which are rare, include acute disseminated encephalomyelitis, aseptic meningitis, meningoencephalitis, sensorineural hearing loss, myelitis, myeloradiculopathy, and Guillain-Barré syndrome.19 Chikungunya also has been associated with bleeding manifestations, acute renal failure, and electrolyte disturbance.19
Continue for the diagnosis >>
DIAGNOSIS
Malaria
The clinical presentation of malaria is nonspecific, so it is important to identify patients with a travel history and perform testing when this diagnosis is suspected.7,8 The gold standard for diagnosing malaria remains microscopy of thick and thin films of the patient’s peripheral blood.7 In patients with blood-stage malaria, a blood slide will show multiple infected RBCs and the appearance of the classic “headphone” form within the cells (see Figure 3). This test allows for efficient detection of malaria parasites, determination of parasite species, and calculation of percent parasitemia. Early differentiation between falciparum and nonfalciparum malaria is required, since P falciparum is the most life-threatening form of malaria.7 All of these factors are key to determining the best treatment plan for each patient.8
Rapid diagnostic tests (RDTs) and polymerase chain reaction (PCR) for malaria are increasingly available for use in US laboratories. In comparison to microscopy, these newer diagnostic tools are slower, more costly, and less readily available. For this reason, microscopy remains the most common means of diagnosis.7 PCR is helpful for species confirmation of malaria parasites and can be used to confirm a positive result on microscopy.8
It is possible for the first malaria test to be negative, and performing a repeat test the following day in a stable patient is recommended.7 However, more than three tests are not needed as long as the patient’s symptoms are not changing.
Dengue fever
Laboratory diagnosis of dengue can be confirmed with detection of DENV genomic sequences through PCR or nonstructural protein 1 antigen by immunoassay.14 Virus isolation in cell culture, detection of viral RNA by nucleic acid amplification tests, and detection of viral antigens by rapid tests or enzyme-linked immunosorbent assay (ELISA) are most useful if a patient presents within five days of fever onset.13
After five days of febrile illness, dengue viruses and antigens disappear from the blood as the specific antibody levels rise.13 Therefore, ELISA testing for immunoglobulin (Ig) M anti-DENV is a more effective lab study for dengue in patients presenting after one week. Testing for IgG anti-DENV is not recommended for making a diagnosis, however, because this antibody remains elevated for life after any DENV infection, leading to many false-positive test results. 14
A useful diagnostic aid for detecting severe dengue is the tourniquet test, which assesses for microvascular fragility. To perform the test, inflate a blood pressure cuff on the arm to midway between systolic and diastolic blood pressures, and maintain pressure for five minutes. After releasing the pressure, count the number of petechea in one square inch of skin; if 20 or more are found, the test is positive.12
Chikungunya
Chikungunya laboratory testing is limited in the US due to lack of availability. Testing is available only at the CDC, one commercial laboratory, and a few state health departments.17
The only reliable method for diagnosing CHIKV infection is through testing of blood samples. Chikungunya should not be diagnosed clinically because of the difficulty in differentiating it from dengue fever and other viral illnesses. The laboratory diagnosis of CHIKV infection can be obtained through detection of the virus, viral RNA, or specific antibodies related to chikungunya.20 Serologic detection of IgM or IgG antibodies is the most common method of diagnosis and is recommended by the CDC.20 If initial IgM and IgG testing is negative but clinical suspicion remains high, repeat testing should be done during the convalescent phase of the illness (≥ 7 days after symptom onset).21 Reverse transcriptase PCR is an effective diagnostic laboratory method for chikungunya and can be used in the first seven days of illness.20 ELISA and the hemagglutination inhibition assay can also provide diagnostic information.20
Lab findings associated with malaria, dengue fever, and chikungunya are summarized in the Table.
Continue for differentiating between dengue, malaria, and chikungunya early in presentation >>
Differentiating between dengue, malaria, and chikungunya early in presentation
Hematologic parameters can be used as a diagnostic aid when differentiating among certain causes of fever, as noted in a study by Joshi and Shah.22 In the setting of a febrile illness, thrombocytopenia (platelet count < 150,000/µL) is a predictor of malaria, especially in combination with anemia (hemoglobin < 10 g/dL). Thrombocytopenia is also common with dengue fever, but patients with dengue typically have normal hemoglobin. According to Joshi and Shah, patients having the combination of anemia and thrombocytopenia were 22 times more likely to have malaria than patients without these laboratory findings.22
Kutsuna and colleagues also found disease-specific clues in laboratory data when differentiating between dengue fever and malaria. Patients with dengue fever had significantly lower white blood cell counts than patients with malaria.23 In addition, although thrombocytopenia is seen in both dengue fever and malaria, platelet counts are lower in patients with malaria at first presentation. However, with dengue fever the platelet count can decrease three to six days into the illness when fever abates.23 Furthermore, total bilirubin tends to increase in malaria but is unaffected in dengue fever. Last, C-reactive protein can be helpful in assessing malaria severity and clinical improvement at follow-up, as well as for differentiating malaria from other conditions (eg, dengue), especially if the value is greater than 10 mg/L.23
Distinguishing chikungunya from dengue fever in the early stages of illness is difficult, and there is no pathognomonic hematologic laboratory study that helps with this task. With both diseases, the patient may have leukopenia, elevated erythrocyte sedimentation rate, and (rarely) thrombocytopenia. Chipwaza and colleagues discuss the significant overlap in symptoms in nonmalaria febrile illness. The overlap makes clinical diagnosis difficult; lab testing is essential for establishing the diagnosis.21 Once CHIKV is confirmed, the clinician is typically reassured of a more benign, self-limited course.
Continue for treatment/management >>
TREATMENT / MANAGEMENT
Malaria
The treatment of malaria varies depending on the severity of disease and the probability the organism is resistant to antimalarial drugs. The likelihood of drug resistance is determined based on the species of malaria parasite and the location where the infection occurred.24
Malaria is considered severe if one or more of the following are present: neurologic sequelae, renal failure, severe anemia, ARDS, jaundice, or parasite burden greater than 5%.8 Patients with severe malaria are treated with parenteral (IV) antimalarials; the two options for parenteral medication are quinine and artesunate.7 All patients treated with parenteral antimalarial agents should take a full course of oral medication for malaria as well. Oral antimalarial medications include, but are not limited to, quinine sulfate, atovaquone/proguanil, artemether-lumefantrine, doxycycline, clindamycin, sulfadoxine/pyrimethamine, chloroquine, and primaquine. The oral medications most commonly used to treat nonfalciparum malaria are chloroquine followed by primaquine.7 Chloroquine is not typically used for falciparum malaria due to widespread resistance.7
In cases of malaria caused by P vivax or P ovale infection, the likelihood of parasitic infection lying dormant in the liver must be considered. Additional treatment is often needed to eradicate this type of infection.7 The relapse of symptoms can occur years after the acute attack.25 Primaquine is the only approved medication for preventing and treating parasitic relapse associated with dormant infection.25
Dengue fever
The typical course of dengue follows three phases: febrile, critical, and convalescent.14 Dengue is usually a self-limiting febrile illness and typically resolves within one week after symptom onset without major complications.11 During the critical phase, most patients begin to improve, but up to 5% of cases develop concerning warning signs and symptoms that could represent a life-threatening condition that requires intense treatment and close monitoring.14 Warning signs for worsening disease are caused by marked increase in vascular permeability and include narrow pulse pressure, pleural effusions, ascites, and hemorrhagic manifestations (hematemesis, melena, menorrhagia).14
Treatment of most cases of dengue involves use of acetaminophen for comfort and fever reduction, hydration, and rest.26 Treatment of worsening dengue includes inpatient admission and possibly ICU admission for close observation and frequent monitoring.14 It is important to avoid aspirin and other NSAIDs due to the risk for bleeding complications in severe dengue.14 There are no approved antivirals for treatment of dengue. To reduce the risk for transmission of dengue, febrile patients should avoid further mosquito bites.14
Clinicians should be aware of warning signs of worsening illness with dengue fever. Signs of worsening dengue fever include postural hypotension, thrombocytopenia, decrease in serum albumin, and rising hematocrit.10
Chikungunya
CHIKV illness is usually a self-limiting condition. Diagnosis of chikungunya may take time, and providers should assume the chikungunya patient may have dengue, which has the potential to be more pathologic. Accordingly, they must watch for warning signs of dengue until CHIKV is confirmed.27
Management focuses on supportive care, including hydration and rest. Typically, the medications used are antipyretics (acetaminophen and ibuprofen) and analgesics; no antiviral medication for chikungunya is available.22 Aspirin is avoided due to the risk for Reye syndrome. Antihistamines may be helpful for patients who have an associated pruritic rash. Cold compresses can be beneficial for joint pain and swelling. Additionally, it is important to keep patients under mosquito nets during the febrile phase to decrease the risk for disease transmission.
Continue for patient education >>
PATIENT EDUCATION
Vaccination
Vaccines are not available for dengue fever, malaria, or chikungunya. However, researchers have been working on a vaccine for malaria for decades, and presently, more than 20 vaccine constructs are being tested and researched in preclinical trials.28 Similarly, efforts to develop an effective vaccine for chikungunya have been under way since the 1970s.15
Chemoprophylaxis
There are no chemoprophylaxis options available for dengue or chikungunya. The most effective measures to prevent dengue are strategies aimed at avoiding mosquito bites (ie, vector control and individual protections like repellants).16 One group of authors notes that developing a larger network of research laboratories capable of prompt diagnosis of arbovirus infections would help to better control chikungunya.
Multiple options for malaria chemoprophylaxis are available, and these vary by country of travel. Chemoprophylaxis options include doxycycline, mefloquine, atovaquone/proguanil, chloroquine, and primaquine.8 For dormant forms of malaria residing in the liver, primaquine is the only effective treatment.8
It is important to remember that no antimalarial drug is 100% protective. Malaria chemoprophylaxis reduces the risk for malaria, but it is often taken inadequately, which can delay symptom onset and lead to a false-negative result on initial blood films.5 All patients with fever who have visited a tropical country within one year of presentation should be screened for malaria.5 It is incorrect and dangerous to assume that a patient who received malaria chemoprophylaxis does not have malaria. Diagnosis of malaria requires a high index of suspicion, and clinicians must remember that malaria can occur even with perfect prophylaxis.7 Unfortunately, malaria parasites are becoming resistant to some commonly used antimalarial drugs. Resistance patterns are being tracked by the CDC.8
Pretravel visit with clinician
Many illnesses related to travel can be prevented with vaccination, chemoprophylaxis, and patient education. However, many travelers do not visit a health care professional before travel (even among those traveling to perceived “risky” destinations, such as Sub-Saharan Africa).29 In a study of ill returned travelers, Leder and colleagues found that only 40% had sought pretravel advice from providers. Interestingly, many of those ill patients who obtained a pretravel consult did not receive appropriate vaccines, such as hepatitis A or influenza vaccine. Some of these patients were diagnosed with preventable conditions.29
Open and thorough communication between clinicians and patients is paramount to protect travelers from disease and illness. Clinicians have the opportunity to greatly impact the health of their patients by recommending a pretravel consultation. What may take extra time and effort on the front end of the trip may save significant time and energy on the back end, and even save lives.
Mosquito bite avoidance
One of the most important patient education discussions in pretravel consultation is mosquito bite avoidance. Travelers should be advised to find accommodations with air conditioning and screened windows and doors.14 To avoid mosquito bites, they should cover their arms and legs adequately with proper clothing. Standing water (such as in flower pots), which can encourage mosquito breeding, should be avoided as well. Travelers should use insect repellents and insecticides, especially in cool, dark areas (eg, closets and bathrooms) where mosquitoes hide.14
Continue for follow-up >>
FOLLOW-UP
Malaria
Appropriate follow-up, need for hospitalization, and choice of medical treatment are determined by disease cause, severity of illness, and patient demographics. Follow-up is necessary to ensure improvement and no development of atypical symptoms. Additionally, the clinician needs to keep in mind the risk for malaria strains that can have a dormant stage.
Dengue fever
Clinicians must remind convalescing patients to watch for severe abdominal pain, vomiting, difficulty breathing, and signs of bleeding (epistaxis, bruising, bloody stool, and menorrhagia). Clinicians must also be attentive to changing lab values, including a decrease in platelet count and an increase in hematocrit, along with signs of hypovolemic shock, ascites, pleural effusions, and narrow pulse pressure.14
Chikungunya
Patients are reminded to keep themselves comfortable by rehydrating and treating the discomfort associated with arthralgias. In a longitudinal study of chikungunya patients, 60% experienced continued arthralgias three years after diagnosis.23,30 Patient education regarding the potential for long-term arthralgia is important, as it may impact activities of daily living and work.
Long-term NSAIDs have been used for patients with recurrent or even chronic arthralgia.31 There are limited data available on beneficial treatments, such as chloroquine sulfate or disease-modifying antirheumatic drugs, for chronic arthralgia associated with chikungunya.23 Depression and recurrent cutaneous lesions also are possible in patients with long-term symptoms.
Continue for the conclusion >>
CONCLUSION
“People, as well as pathogens, travel from all around the world in all directions.”32 With the ever-increasing mobility of populations around the world, transmission of illness and medical norms are constantly changing. All clinicians should keep in mind the less commonly seen diagnostic entities and remember the importance of obtaining a complete travel history in the febrile patient.
Early detection and appropriate supportive care of patients with dengue fever and malaria can be lifesaving. In addition, proper pretravel consultations can provide a wealth of patient education for at-risk travelers and help prevent a number of debilitating infectious diseases.
CE/CME No: CR-1602
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Explain how accessibility to travel affects the etiology of illness.
• Understand the typical and atypical signs and symptoms of malaria, dengue fever, and chikungunya.
• Identify the proper laboratory workup and treatment for malaria, dengue fever, and chikungunya.
• Discuss multiple ways to prevent mosquito-borne illness in your patients and the importance of a pretravel consultation.
FACULTY
Eve B. Hoover is completing a postgraduate academic fellowship at Midwestern University at Glendale, Arizona, and practices at Logistics Health, Inc, in Phoenix.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of February 2016.
Article begins on next page >>
As the number of international travelers increases, so does the likelihood of transmission of illnesses to locations where they were previously rarely diagnosed. Clinicians at college health centers must be aware of tropical medicine diagnoses, especially in returning international students who have fever and other constitutional symptoms. This article provides a refresher regarding the diagnoses of malaria, dengue fever, and chikungunya.
Travel, whether for work, education, or pleasure, continues to increase, with the number of international travelers exceeding 1.1 billion in 2014.1 International travelers may unknowingly expose themselves and others to multiple health hazards previously thought to be foreign to the United States. Jane Zuckerman, who works with the World Health Organization (WHO), has noted that just over a century ago, the first human flew in an aircraft.2 Now, the sky is no longer the limit, and genes and micro-organisms travel as freely as their human hosts.
The international student population at American universities is at an all-time high (see Figure 1). Study abroad programs, which include American students who travel to developed and underdeveloped countries, also continue to increase. According to the CDC, the number of American students studying abroad has increased more than threefold in the past 20 years.3 According to the Institute of International Education, 304,467 American college students studied abroad in 2013/2014.4 Historically, most American students studied abroad in European countries, but in recent years the list of destinations has expanded, with increases in the percentage of students who travel to Africa, Asia, and the Middle East, and decreases in the percentage choosing Europe and Oceania.3
The sizable number of international students at universities, combined with the study abroad programs, have broadened the scope of the campus health care provider’s differential diagnosis. Diseases and infections that occur in developing countries can differ from those commonly seen in the US and Europe. It is important for health care providers to be reminded of conditions they seldom see and for a tropical medicine zebra to be considered in the appropriate patient population.
Continue for three causes of fever in returning travelers >>
THREE CAUSES OF FEVER IN RETURNING TRAVELERS
There are numerous etiologies for fever in the returning traveler. Factors such as location of travel, length of stay, dates of travel, date of symptom onset, risk activities undertaken, and reason for visit help determine the cause of illness.5 Two of the most commonly encountered conditions causing illness in the febrile traveler are dengue fever and malaria. Additionally, chikungunya is an emerging health concern in the US that has received increased attention following a massive outbreak in the Caribbean (which affected many American travelers) in 2013. In a retrospective study of patient records from 462 febrile adults who traveled to malaria-endemic areas, Siikamäki and colleagues found that every fourth febrile returning traveler had an illness that was potentially life-threatening.6 Understanding the possible causes of febrile illness in travelers can aid the clinician in diagnosing and correctly treating potentially life-threatening conditions.
Malaria
Malaria is a mosquito-borne illness transmitted in humans by female Anopheles mosquitoes.7 It is caused by infection with the protozoal parasites Plasmodium falciparum, P vivax, P ovale, P malariae, and occasionally other Plasmodium species.8 An infected female Anopheles mosquito transmits the parasite into a human host through a bite. The most severe form of human malaria, which can be fatal, is caused by P falciparum. Falciparum and vivax malaria are the most common forms of malaria worldwide.8
According to the WHO, there were an estimated 214 million clinical episodes of malaria worldwide, and malaria was the cause of 438,000 deaths, in 2015.9 In 2012, the CDC received reports of 1,687 cases of malaria in the US.8 The number of malaria cases has been steadily increasing since 1973.8 Figure 2 shows the number of malaria cases diagnosed in each state in 2012. The data demonstrate that malaria is the primary cause of death in travel-related fever. Malaria is also the most common single reason for travel-related fever without findings on exam or workup.
Dengue fever
Dengue is a mosquito-borne disease (transmitted by an infected Aedes mosquito) and is caused by four types of flaviviruses (DENV-1, DENV-2, DENV-3, DENV-4).10 It is the most common arboviral disease in humans.11 In 2009, the WHO revised its dengue categories to include dengue, dengue with warning signs, and severe dengue.12,13 Previously, the categories included dengue fever, dengue hemorrhagic fever, and dengue shock syndrome.
Dengue is endemic throughout the tropics and subtropics and is a leading cause of febrile illness among travelers returning from the Caribbean, South America, and South and Southeast Asia.14 There has been a 30-fold increase in dengue fever in the past 50 years.10 This illness is present in more than 100 countries; in the US, outbreaks have occurred in Florida, Hawaii, and along the Texas-Mexico border.14
Chikungunya
Chikungunya virus (CHIKV) is an arbovirus that is transmitted by Aedes mosquitoes (Aedes aegypti and Aedes albopictus).15 The term chikungunya is derived from a word in the Swahili and Maconde language that means “the one that is folded.”16 This description refers to the severe arthralgias that can cause a hunched-over gait in the patient with chikungunya.
Chikungunya historically has not had a significant impact in the Americas or Europe. However, more than one million suspected cases of chikungunya have been reported in the Americas since October 2013.16 Most cases of CHIKV infection diagnosed in the US have occurred in travelers; however, there have also been documented cases of local transmission of the virus.17 Local transmission occurs when the ill returning traveler unknowingly spreads disease, with the aid of the mosquito vector, upon return to the US.
Continue for patient presentation >>
PATIENT PRESENTATION
A 19-year-old previously healthy male student presented to the university health clinic for evaluation. During the exam, he lay on the examination table, covered with a blanket and shaking uncontrollably with intense rigors. Although he was hesitant to answer questions due to feeling so ill, he reported that he had returned from India two weeks prior and his symptoms—fever, rigors, ache, fatigue, headache, and nausea—began abruptly, hours before his arrival at the clinic.
The patient was diaphoretic and taking rapid, shallow inspirations. Assessment of vital signs revealed a blood pressure of 148/86 mm Hg; respiratory rate, 24 breaths/min; temperature, 103°F; and heart rate, 112 beats/min.
HEENT evaluation showed dry mucous membranes but no other abnormality. Neck was supple with no lymphadenopathy or nuchal rigidity. On cardiac exam, there were no murmurs or rubs. Lungs were clear to auscultation. Abdomen was soft and nontender, and bowel sounds were present in all four quadrants. There was no costovertebral angle tenderness. Skin was warm, clammy, and without rash. There were no focal neurologic deficits.
Complete blood count, comprehensive metabolic panel, and urinalysis were without abnormality. Examination of thick and thin blood smears revealed multiple red blood cells (RBCs) infected with malaria parasites and the appearance of the classic “headphone” form within the cells. Based on the in-office laboratory results of the blood smear, the patient was diagnosed with malaria.
The patient was not surprised by the diagnosis, as he had experienced these same symptoms with previous bouts of malaria. He and his family were from India, and the patient was an international college student. He had not taken malaria chemoprophylaxis prior to his most recent trip. After a short hospital admission for hydration, observation, treatment, and consultation by an infectious disease specialist, the patient was released back to the demands of college life.
Continue for signs and symptoms >>
SIGNS AND SYMPTOMS
Malaria
Signs and symptoms of malaria can vary greatly from none to illness causing death. The classic clinical features of malaria (fever, headache, back pain, chills, sweating, myalgia, nausea, vomiting, and cough) are caused by the parasite developing in RBCs, causing toxins to accumulate.18 Following the mosquito bite, there is typically an incubation period of seven to 30 days.
When first diagnosing malaria, the clinician needs to determine if the cause is P falciparum (the most severe form of malaria). If so, the clinician then must determine if the case is severe or nonsevere.7 In P falciparum infections, symptom onset can be later, especially if the patient took prophylaxis.7 Longer incubation periods are often seen with P vivax, P malariae, and P ovale infections. P vivax and P ovale can lie dormant in hepatic cells and reactivate after months or even years.7
Adults and children may experience different malaria symptoms, particularly with severe forms of the disease. Pediatric patients with severe falciparum malaria may experience respiratory distress, convulsions, and hypoglycemia more commonly than adults. More than half of adults with severe falciparum experience acute respiratory distress syndrome and acute renal failure.7 Pregnant women are at increased risk for complications.
Dengue fever
Approximately 75% of patients infected with DENV are asymptomatic.14 However, if symptomatic, the most common symptoms (fever, myalgia, headache, rash, arthralgia, abdominal pain, and nausea) begin abruptly after an incubation period of four to seven days.
Dengue can also present with atypical manifestations. In a prospective study by Nimmagadda and colleagues involving 150 participants with confirmed dengue fever, more than half of subjects had at least one atypical symptom along with more typical symptoms.10 The most common atypical manifestation was abnormal liver function, which was present in 40.6% of participants. Other atypical symptoms seen were febrile diarrhea (12%), renal failure (8%), acalculous cholecystitis (6.6%), and conduction abnormalities of the heart (6%). Less common atypical manifestations observed in this study included encephalitis, seizures, acute respiratory distress syndrome, disseminated intravascular coagulation, acute pancreatitis, myositis, and atrial fibrillation. The authors recommended that clinicians maintain a high level of vigilance for atypical manifestations of dengue fever, noting that most of the severe complications of dengue can be avoided if the disease is diagnosed correctly early in the course of illness.
Chikungunya
The typical presentation of CHIKV infection is a patient who abruptly develops fever, headache, polyarthralgia, and myalgia. The joint pain most frequently affects the small joints, such as the interphalangeal joints of the hands as well as the ankles and wrists.15 Back pain is also common, and rash is present in more than half of cases. The rash in adults can be maculopapular and in children is more often bullous. Fever, rash, and headache typically last seven to 10 days, while the arthralgia can last much longer—three to four months in a third of patients and three to five years in 10%.15
CHIKV infection that presents with typical clinical manifestations is usually self-limited; however, more severe atypical symptoms can occur and may lead to long-term morbidity. These atypical manifestations of chikungunya, which are rare, include acute disseminated encephalomyelitis, aseptic meningitis, meningoencephalitis, sensorineural hearing loss, myelitis, myeloradiculopathy, and Guillain-Barré syndrome.19 Chikungunya also has been associated with bleeding manifestations, acute renal failure, and electrolyte disturbance.19
Continue for the diagnosis >>
DIAGNOSIS
Malaria
The clinical presentation of malaria is nonspecific, so it is important to identify patients with a travel history and perform testing when this diagnosis is suspected.7,8 The gold standard for diagnosing malaria remains microscopy of thick and thin films of the patient’s peripheral blood.7 In patients with blood-stage malaria, a blood slide will show multiple infected RBCs and the appearance of the classic “headphone” form within the cells (see Figure 3). This test allows for efficient detection of malaria parasites, determination of parasite species, and calculation of percent parasitemia. Early differentiation between falciparum and nonfalciparum malaria is required, since P falciparum is the most life-threatening form of malaria.7 All of these factors are key to determining the best treatment plan for each patient.8
Rapid diagnostic tests (RDTs) and polymerase chain reaction (PCR) for malaria are increasingly available for use in US laboratories. In comparison to microscopy, these newer diagnostic tools are slower, more costly, and less readily available. For this reason, microscopy remains the most common means of diagnosis.7 PCR is helpful for species confirmation of malaria parasites and can be used to confirm a positive result on microscopy.8
It is possible for the first malaria test to be negative, and performing a repeat test the following day in a stable patient is recommended.7 However, more than three tests are not needed as long as the patient’s symptoms are not changing.
Dengue fever
Laboratory diagnosis of dengue can be confirmed with detection of DENV genomic sequences through PCR or nonstructural protein 1 antigen by immunoassay.14 Virus isolation in cell culture, detection of viral RNA by nucleic acid amplification tests, and detection of viral antigens by rapid tests or enzyme-linked immunosorbent assay (ELISA) are most useful if a patient presents within five days of fever onset.13
After five days of febrile illness, dengue viruses and antigens disappear from the blood as the specific antibody levels rise.13 Therefore, ELISA testing for immunoglobulin (Ig) M anti-DENV is a more effective lab study for dengue in patients presenting after one week. Testing for IgG anti-DENV is not recommended for making a diagnosis, however, because this antibody remains elevated for life after any DENV infection, leading to many false-positive test results. 14
A useful diagnostic aid for detecting severe dengue is the tourniquet test, which assesses for microvascular fragility. To perform the test, inflate a blood pressure cuff on the arm to midway between systolic and diastolic blood pressures, and maintain pressure for five minutes. After releasing the pressure, count the number of petechea in one square inch of skin; if 20 or more are found, the test is positive.12
Chikungunya
Chikungunya laboratory testing is limited in the US due to lack of availability. Testing is available only at the CDC, one commercial laboratory, and a few state health departments.17
The only reliable method for diagnosing CHIKV infection is through testing of blood samples. Chikungunya should not be diagnosed clinically because of the difficulty in differentiating it from dengue fever and other viral illnesses. The laboratory diagnosis of CHIKV infection can be obtained through detection of the virus, viral RNA, or specific antibodies related to chikungunya.20 Serologic detection of IgM or IgG antibodies is the most common method of diagnosis and is recommended by the CDC.20 If initial IgM and IgG testing is negative but clinical suspicion remains high, repeat testing should be done during the convalescent phase of the illness (≥ 7 days after symptom onset).21 Reverse transcriptase PCR is an effective diagnostic laboratory method for chikungunya and can be used in the first seven days of illness.20 ELISA and the hemagglutination inhibition assay can also provide diagnostic information.20
Lab findings associated with malaria, dengue fever, and chikungunya are summarized in the Table.
Continue for differentiating between dengue, malaria, and chikungunya early in presentation >>
Differentiating between dengue, malaria, and chikungunya early in presentation
Hematologic parameters can be used as a diagnostic aid when differentiating among certain causes of fever, as noted in a study by Joshi and Shah.22 In the setting of a febrile illness, thrombocytopenia (platelet count < 150,000/µL) is a predictor of malaria, especially in combination with anemia (hemoglobin < 10 g/dL). Thrombocytopenia is also common with dengue fever, but patients with dengue typically have normal hemoglobin. According to Joshi and Shah, patients having the combination of anemia and thrombocytopenia were 22 times more likely to have malaria than patients without these laboratory findings.22
Kutsuna and colleagues also found disease-specific clues in laboratory data when differentiating between dengue fever and malaria. Patients with dengue fever had significantly lower white blood cell counts than patients with malaria.23 In addition, although thrombocytopenia is seen in both dengue fever and malaria, platelet counts are lower in patients with malaria at first presentation. However, with dengue fever the platelet count can decrease three to six days into the illness when fever abates.23 Furthermore, total bilirubin tends to increase in malaria but is unaffected in dengue fever. Last, C-reactive protein can be helpful in assessing malaria severity and clinical improvement at follow-up, as well as for differentiating malaria from other conditions (eg, dengue), especially if the value is greater than 10 mg/L.23
Distinguishing chikungunya from dengue fever in the early stages of illness is difficult, and there is no pathognomonic hematologic laboratory study that helps with this task. With both diseases, the patient may have leukopenia, elevated erythrocyte sedimentation rate, and (rarely) thrombocytopenia. Chipwaza and colleagues discuss the significant overlap in symptoms in nonmalaria febrile illness. The overlap makes clinical diagnosis difficult; lab testing is essential for establishing the diagnosis.21 Once CHIKV is confirmed, the clinician is typically reassured of a more benign, self-limited course.
Continue for treatment/management >>
TREATMENT / MANAGEMENT
Malaria
The treatment of malaria varies depending on the severity of disease and the probability the organism is resistant to antimalarial drugs. The likelihood of drug resistance is determined based on the species of malaria parasite and the location where the infection occurred.24
Malaria is considered severe if one or more of the following are present: neurologic sequelae, renal failure, severe anemia, ARDS, jaundice, or parasite burden greater than 5%.8 Patients with severe malaria are treated with parenteral (IV) antimalarials; the two options for parenteral medication are quinine and artesunate.7 All patients treated with parenteral antimalarial agents should take a full course of oral medication for malaria as well. Oral antimalarial medications include, but are not limited to, quinine sulfate, atovaquone/proguanil, artemether-lumefantrine, doxycycline, clindamycin, sulfadoxine/pyrimethamine, chloroquine, and primaquine. The oral medications most commonly used to treat nonfalciparum malaria are chloroquine followed by primaquine.7 Chloroquine is not typically used for falciparum malaria due to widespread resistance.7
In cases of malaria caused by P vivax or P ovale infection, the likelihood of parasitic infection lying dormant in the liver must be considered. Additional treatment is often needed to eradicate this type of infection.7 The relapse of symptoms can occur years after the acute attack.25 Primaquine is the only approved medication for preventing and treating parasitic relapse associated with dormant infection.25
Dengue fever
The typical course of dengue follows three phases: febrile, critical, and convalescent.14 Dengue is usually a self-limiting febrile illness and typically resolves within one week after symptom onset without major complications.11 During the critical phase, most patients begin to improve, but up to 5% of cases develop concerning warning signs and symptoms that could represent a life-threatening condition that requires intense treatment and close monitoring.14 Warning signs for worsening disease are caused by marked increase in vascular permeability and include narrow pulse pressure, pleural effusions, ascites, and hemorrhagic manifestations (hematemesis, melena, menorrhagia).14
Treatment of most cases of dengue involves use of acetaminophen for comfort and fever reduction, hydration, and rest.26 Treatment of worsening dengue includes inpatient admission and possibly ICU admission for close observation and frequent monitoring.14 It is important to avoid aspirin and other NSAIDs due to the risk for bleeding complications in severe dengue.14 There are no approved antivirals for treatment of dengue. To reduce the risk for transmission of dengue, febrile patients should avoid further mosquito bites.14
Clinicians should be aware of warning signs of worsening illness with dengue fever. Signs of worsening dengue fever include postural hypotension, thrombocytopenia, decrease in serum albumin, and rising hematocrit.10
Chikungunya
CHIKV illness is usually a self-limiting condition. Diagnosis of chikungunya may take time, and providers should assume the chikungunya patient may have dengue, which has the potential to be more pathologic. Accordingly, they must watch for warning signs of dengue until CHIKV is confirmed.27
Management focuses on supportive care, including hydration and rest. Typically, the medications used are antipyretics (acetaminophen and ibuprofen) and analgesics; no antiviral medication for chikungunya is available.22 Aspirin is avoided due to the risk for Reye syndrome. Antihistamines may be helpful for patients who have an associated pruritic rash. Cold compresses can be beneficial for joint pain and swelling. Additionally, it is important to keep patients under mosquito nets during the febrile phase to decrease the risk for disease transmission.
Continue for patient education >>
PATIENT EDUCATION
Vaccination
Vaccines are not available for dengue fever, malaria, or chikungunya. However, researchers have been working on a vaccine for malaria for decades, and presently, more than 20 vaccine constructs are being tested and researched in preclinical trials.28 Similarly, efforts to develop an effective vaccine for chikungunya have been under way since the 1970s.15
Chemoprophylaxis
There are no chemoprophylaxis options available for dengue or chikungunya. The most effective measures to prevent dengue are strategies aimed at avoiding mosquito bites (ie, vector control and individual protections like repellants).16 One group of authors notes that developing a larger network of research laboratories capable of prompt diagnosis of arbovirus infections would help to better control chikungunya.
Multiple options for malaria chemoprophylaxis are available, and these vary by country of travel. Chemoprophylaxis options include doxycycline, mefloquine, atovaquone/proguanil, chloroquine, and primaquine.8 For dormant forms of malaria residing in the liver, primaquine is the only effective treatment.8
It is important to remember that no antimalarial drug is 100% protective. Malaria chemoprophylaxis reduces the risk for malaria, but it is often taken inadequately, which can delay symptom onset and lead to a false-negative result on initial blood films.5 All patients with fever who have visited a tropical country within one year of presentation should be screened for malaria.5 It is incorrect and dangerous to assume that a patient who received malaria chemoprophylaxis does not have malaria. Diagnosis of malaria requires a high index of suspicion, and clinicians must remember that malaria can occur even with perfect prophylaxis.7 Unfortunately, malaria parasites are becoming resistant to some commonly used antimalarial drugs. Resistance patterns are being tracked by the CDC.8
Pretravel visit with clinician
Many illnesses related to travel can be prevented with vaccination, chemoprophylaxis, and patient education. However, many travelers do not visit a health care professional before travel (even among those traveling to perceived “risky” destinations, such as Sub-Saharan Africa).29 In a study of ill returned travelers, Leder and colleagues found that only 40% had sought pretravel advice from providers. Interestingly, many of those ill patients who obtained a pretravel consult did not receive appropriate vaccines, such as hepatitis A or influenza vaccine. Some of these patients were diagnosed with preventable conditions.29
Open and thorough communication between clinicians and patients is paramount to protect travelers from disease and illness. Clinicians have the opportunity to greatly impact the health of their patients by recommending a pretravel consultation. What may take extra time and effort on the front end of the trip may save significant time and energy on the back end, and even save lives.
Mosquito bite avoidance
One of the most important patient education discussions in pretravel consultation is mosquito bite avoidance. Travelers should be advised to find accommodations with air conditioning and screened windows and doors.14 To avoid mosquito bites, they should cover their arms and legs adequately with proper clothing. Standing water (such as in flower pots), which can encourage mosquito breeding, should be avoided as well. Travelers should use insect repellents and insecticides, especially in cool, dark areas (eg, closets and bathrooms) where mosquitoes hide.14
Continue for follow-up >>
FOLLOW-UP
Malaria
Appropriate follow-up, need for hospitalization, and choice of medical treatment are determined by disease cause, severity of illness, and patient demographics. Follow-up is necessary to ensure improvement and no development of atypical symptoms. Additionally, the clinician needs to keep in mind the risk for malaria strains that can have a dormant stage.
Dengue fever
Clinicians must remind convalescing patients to watch for severe abdominal pain, vomiting, difficulty breathing, and signs of bleeding (epistaxis, bruising, bloody stool, and menorrhagia). Clinicians must also be attentive to changing lab values, including a decrease in platelet count and an increase in hematocrit, along with signs of hypovolemic shock, ascites, pleural effusions, and narrow pulse pressure.14
Chikungunya
Patients are reminded to keep themselves comfortable by rehydrating and treating the discomfort associated with arthralgias. In a longitudinal study of chikungunya patients, 60% experienced continued arthralgias three years after diagnosis.23,30 Patient education regarding the potential for long-term arthralgia is important, as it may impact activities of daily living and work.
Long-term NSAIDs have been used for patients with recurrent or even chronic arthralgia.31 There are limited data available on beneficial treatments, such as chloroquine sulfate or disease-modifying antirheumatic drugs, for chronic arthralgia associated with chikungunya.23 Depression and recurrent cutaneous lesions also are possible in patients with long-term symptoms.
Continue for the conclusion >>
CONCLUSION
“People, as well as pathogens, travel from all around the world in all directions.”32 With the ever-increasing mobility of populations around the world, transmission of illness and medical norms are constantly changing. All clinicians should keep in mind the less commonly seen diagnostic entities and remember the importance of obtaining a complete travel history in the febrile patient.
Early detection and appropriate supportive care of patients with dengue fever and malaria can be lifesaving. In addition, proper pretravel consultations can provide a wealth of patient education for at-risk travelers and help prevent a number of debilitating infectious diseases.
1. World Tourism Organization. Over 1.1 billion tourists travelled abroad in 2014 [press release]. January 27, 2015. http://media.unwto.org/press-release/2015-01-27/over-11-billion-tourists-travelled-abroad-2014. Accessed January 21, 2016.
2. Zuckerman JN. Public health and travel medicine: intricately intertwined. Perspect Public Health. 2012;132(5):206.
3. Rhodes G, DeRomaña I, Ebner J. Advising travelers with special needs: study abroad & other international student travel. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellow book/2016/advising-travelers-with-specific-needs/study-abroad-other-international-student-travel. Accessed January 21, 2016.
4. Institute of International Education. US study abroad: all destinations. www.iie.org/Research-and-Publications/Open-Doors/Data/US-Study-Abroad/All-Destinations/2012-14. Accessed January 21, 2016.
5. Hearn P, Johnston V. Assessment of returning travelers with fever. Medicine. 2014;42(2):66-72.
6. Siikamäki HM, Kivelä PS, Sipilä PN, et al. Fever in travelers returning from malaria-endemic areas: don’t look for malaria only. J Travel Med. 2011;18(4):239-244.
7. Walker NF, Nadjm B, Whitty CJ. Malaria. Medicine. 2014;42(2):100-106.
8. Cullen KA, Arguin PM. Malaria surveillance—United States, 2012. MMWR Surveill Summ. 2014;63(12):1-22.
9. World Health Organization. Malaria. Fact sheet no. 94. www.who.int/mediacentre/factsheets/fs094/en/. Accessed January 21, 2016.
10. Nimmagadda SS, Mahabala C, Boloor A, et al. Atypical manifestations of dengue fever (DF)—where do we stand today? J Clin Diagn Res. 2014;8(1):71-73.
11. Whitehorn J, Yacoub S, Anders KL, et al. Dengue therapeutics, chemoprophylaxis, and allied tools: state of the art and future directions. PLoS Negl Trop Dis. 2014;8(8):e3025.
12. Mayxay M, Phetsouvanh R, Moore CE, et al. Predictive diagnostic value of the tourniquet test for the diagnosis of dengue infection in adults. Trop Med Int Health. 2011;16(1):127-133.
13. World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. WHO/HTM/NTD/DEN/2009.1. www.who.int/tdr/publications/documents/dengue-diagnosis.pdf. Accessed January 21, 2016.
14. Tomashek KM, Sharp TM, Margolis HS. Infectious diseases related to travel: dengue. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/dengue. Accessed January 21, 2016.
15. Vega-Rúa A, Lourenço-de-Oliveira R, Mousson L, et al. Chikungunya virus transmission potential by local Aedes mosquitoes in the Americas and Europe. PLoS Negl Trop Dis. 2015;9(5):1-18.
16. Hrnjakovi`c Cvjetkovi`c IB, Cvjetkovi`c D, Pati`c A, et al. Chikungunya—a serious threat for public health. Med Pregl. 2015;68(3/4):122-125.
17. Lindsey NP, Prince HE, Kosoy O, et al. Chikungunya virus infections among travelers-United States, 2010-2013. Am J Trop Med Hyg. 2015;92(1):82-87.
18. CDC. Malaria. www.cdc.gov/malaria/about/disease.html. Accessed January 21, 2016.
19. Das S, Sarkar N, Majumder J, et al. Acute disseminated encephalomyelitis in a child with chikungunya virus infection. J Pediatr Infect Dis. 2014;9(1):37-41.
20. Schwartz KL, Giga A, Boggild AK. Chikungunya fever in Canada: fever and polyarthritis in a returned traveller. CMAJ. 2014;186(10):772-774.
21. Chipwaza B, Mugasa JP, Selemani M, et al. Dengue and chikungunya fever among viral diseases in outpatient febrile children in Kilosa district hospital, Tanzania. PLoS Negl Trop Dis. 2014;8(11):e3335.
22. Joshi HA, Shah SS. Platelet count—a diagnostic aid in fever. Natl J Integrated Res Med. 2013;4(3):128-132.
23. Kutsuna S, Hayakawa K, Kato Y, et al. Comparison of clinical characteristics and laboratory findings of malaria, dengue, and enteric fever in returning travelers: 8-year experience at a referral center in Tokyo, Japan. J Infect Chemother. 2015;21(4):272-276.
24. CDC. Malaria diagnosis & treatment in the United States. www.cdc.gov/malaria/diagnosis_treatment/index.html. Accessed January 21, 2016.
25. Roy M, Bouma MJ, Ionides EL, et al. The potential elimination of Plasmodium vivax malaria by relapse treatment: insights from a transmission model and surveillance data from NW India. PLoS Negl Trop Dis. 2013;7(1):e1979.
26. Tither PH. Preventing dengue and chikungunya fever among international travelers. J Am Assoc Nurse Pract. 2014;26(11):584-594.
27. Mardekian SK, Roberts AL. Diagnostic options and challenges for dengue and chikungunya viruses. Biomed Res Int. 2015;2015:834371.
28. World Health Organization. Malaria vaccine development. www.who.int/malaria/areas/vaccine/en/#. Accessed January 21, 2016.
29. Leder K, Torresi J, Libman MD, et al. GeoSentinel Surveillance of illness in returned travelers, 2007-2011. Ann Intern Med. 2013;158(6):456-468.
30. Schilte C, Staikowsky F, Couderc T, et al. Chikungunya virus-associated long-term arthralgia: a 36-month prospective longitudinal study. PLoS Negl Trop Dis. 2013;7:e2137.
31. Essackjee K, Goorah S, Ramchurn SK, et al. Prevalence of and risk factors for chronic arthralgia and rheumatoid-like polyarthritis more than 2 years after infection with chikungunya virus. Postgrad Med. 2013;89:440-447.
32. Piyaphanee W, Steffen R, Shlim DR, et al. Travel medicine for Asian travelers—do we need new approaches? J Travel Med. 2012;19(6):335-337.
1. World Tourism Organization. Over 1.1 billion tourists travelled abroad in 2014 [press release]. January 27, 2015. http://media.unwto.org/press-release/2015-01-27/over-11-billion-tourists-travelled-abroad-2014. Accessed January 21, 2016.
2. Zuckerman JN. Public health and travel medicine: intricately intertwined. Perspect Public Health. 2012;132(5):206.
3. Rhodes G, DeRomaña I, Ebner J. Advising travelers with special needs: study abroad & other international student travel. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellow book/2016/advising-travelers-with-specific-needs/study-abroad-other-international-student-travel. Accessed January 21, 2016.
4. Institute of International Education. US study abroad: all destinations. www.iie.org/Research-and-Publications/Open-Doors/Data/US-Study-Abroad/All-Destinations/2012-14. Accessed January 21, 2016.
5. Hearn P, Johnston V. Assessment of returning travelers with fever. Medicine. 2014;42(2):66-72.
6. Siikamäki HM, Kivelä PS, Sipilä PN, et al. Fever in travelers returning from malaria-endemic areas: don’t look for malaria only. J Travel Med. 2011;18(4):239-244.
7. Walker NF, Nadjm B, Whitty CJ. Malaria. Medicine. 2014;42(2):100-106.
8. Cullen KA, Arguin PM. Malaria surveillance—United States, 2012. MMWR Surveill Summ. 2014;63(12):1-22.
9. World Health Organization. Malaria. Fact sheet no. 94. www.who.int/mediacentre/factsheets/fs094/en/. Accessed January 21, 2016.
10. Nimmagadda SS, Mahabala C, Boloor A, et al. Atypical manifestations of dengue fever (DF)—where do we stand today? J Clin Diagn Res. 2014;8(1):71-73.
11. Whitehorn J, Yacoub S, Anders KL, et al. Dengue therapeutics, chemoprophylaxis, and allied tools: state of the art and future directions. PLoS Negl Trop Dis. 2014;8(8):e3025.
12. Mayxay M, Phetsouvanh R, Moore CE, et al. Predictive diagnostic value of the tourniquet test for the diagnosis of dengue infection in adults. Trop Med Int Health. 2011;16(1):127-133.
13. World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. WHO/HTM/NTD/DEN/2009.1. www.who.int/tdr/publications/documents/dengue-diagnosis.pdf. Accessed January 21, 2016.
14. Tomashek KM, Sharp TM, Margolis HS. Infectious diseases related to travel: dengue. In: CDC Health Information for International Travel. wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/dengue. Accessed January 21, 2016.
15. Vega-Rúa A, Lourenço-de-Oliveira R, Mousson L, et al. Chikungunya virus transmission potential by local Aedes mosquitoes in the Americas and Europe. PLoS Negl Trop Dis. 2015;9(5):1-18.
16. Hrnjakovi`c Cvjetkovi`c IB, Cvjetkovi`c D, Pati`c A, et al. Chikungunya—a serious threat for public health. Med Pregl. 2015;68(3/4):122-125.
17. Lindsey NP, Prince HE, Kosoy O, et al. Chikungunya virus infections among travelers-United States, 2010-2013. Am J Trop Med Hyg. 2015;92(1):82-87.
18. CDC. Malaria. www.cdc.gov/malaria/about/disease.html. Accessed January 21, 2016.
19. Das S, Sarkar N, Majumder J, et al. Acute disseminated encephalomyelitis in a child with chikungunya virus infection. J Pediatr Infect Dis. 2014;9(1):37-41.
20. Schwartz KL, Giga A, Boggild AK. Chikungunya fever in Canada: fever and polyarthritis in a returned traveller. CMAJ. 2014;186(10):772-774.
21. Chipwaza B, Mugasa JP, Selemani M, et al. Dengue and chikungunya fever among viral diseases in outpatient febrile children in Kilosa district hospital, Tanzania. PLoS Negl Trop Dis. 2014;8(11):e3335.
22. Joshi HA, Shah SS. Platelet count—a diagnostic aid in fever. Natl J Integrated Res Med. 2013;4(3):128-132.
23. Kutsuna S, Hayakawa K, Kato Y, et al. Comparison of clinical characteristics and laboratory findings of malaria, dengue, and enteric fever in returning travelers: 8-year experience at a referral center in Tokyo, Japan. J Infect Chemother. 2015;21(4):272-276.
24. CDC. Malaria diagnosis & treatment in the United States. www.cdc.gov/malaria/diagnosis_treatment/index.html. Accessed January 21, 2016.
25. Roy M, Bouma MJ, Ionides EL, et al. The potential elimination of Plasmodium vivax malaria by relapse treatment: insights from a transmission model and surveillance data from NW India. PLoS Negl Trop Dis. 2013;7(1):e1979.
26. Tither PH. Preventing dengue and chikungunya fever among international travelers. J Am Assoc Nurse Pract. 2014;26(11):584-594.
27. Mardekian SK, Roberts AL. Diagnostic options and challenges for dengue and chikungunya viruses. Biomed Res Int. 2015;2015:834371.
28. World Health Organization. Malaria vaccine development. www.who.int/malaria/areas/vaccine/en/#. Accessed January 21, 2016.
29. Leder K, Torresi J, Libman MD, et al. GeoSentinel Surveillance of illness in returned travelers, 2007-2011. Ann Intern Med. 2013;158(6):456-468.
30. Schilte C, Staikowsky F, Couderc T, et al. Chikungunya virus-associated long-term arthralgia: a 36-month prospective longitudinal study. PLoS Negl Trop Dis. 2013;7:e2137.
31. Essackjee K, Goorah S, Ramchurn SK, et al. Prevalence of and risk factors for chronic arthralgia and rheumatoid-like polyarthritis more than 2 years after infection with chikungunya virus. Postgrad Med. 2013;89:440-447.
32. Piyaphanee W, Steffen R, Shlim DR, et al. Travel medicine for Asian travelers—do we need new approaches? J Travel Med. 2012;19(6):335-337.