User login
Hope for hyperhidrosis
Hyperhidrosis – excessive sweating – is one of those diagnoses that make most physicians cringe because we know that the side effects of most of the common treatments are very limiting and patients continue to be frustrated. New treatments are emerging, and although oxybutynin is not Food and Drug Administration–approved for hyperhidrosis, it does show promise.
Primary hyperhidrosis is the excessive sweating from the axilla, palms, soles, or cranial-facial area. It is a clinical diagnosis that has been occurring for more than 6 months and meets at least four1 of the following criteria:
1. It occurs in eccrine dense areas (axilla, soles, palms or head).
2. It is bilateral and symmetrical.
3. It is absent nocturnally.
4. Its onset should be before age 25 years.
5. It occurs at least weekly.
6. There is a positive family history.
7. It impairs daily activities.
If signs of underlying disease are apparent – such as palpitations, night sweats, weight loss, unilateral symptoms, anxiety, or hypertension – further workup is needed to rule out disorders such as diabetes, hyperthyroidism, pheochromocytoma, or peripheral nerve injury.1
The pathophysiology of hyperhidrosis is not clearly understood. It is believed to be due to increased cholinergic stimulation given that there is no hypertrophy or hyperplasia of the sweat gland.2 Genetics appear to play a role as there is usually a family history of the disorder.2
Topical treatments are usually first line, starting with aluminum chloride antiperspirants, or anticholinergic creams such as glycopyrrolate or glycopyrronium. Unfortunately, many patients complain of the skin irritation so they discontinue their use.1
Botulinum toxin type A is a very safe and effective way of treating hyperhidrosis and is FDA approved for that purpose.3 Its drawbacks are that it is an injection (approximately 25 in each armpit), and it is very costly, usually $1,000-1,500 per session for both underarms. There are no major side effects, and reduction in sweating lasts for 4-12 months, with a median of 6 months.3
Oral treatment of hyperhidrosis, with medications such as glycopyrrolate and benztropine, has been reserved for second- or third-line treatment because of the unwanted side effects of dry mouth and drowsiness. But more recent studies are showing favorable outcomes with oxybutynin.1
Oxybutynin is well known and FDA approved for treatment of urinary frequency, incontinence, and enuresis. Recent studies have shown great success for use to control generalized hyperhidrosis. The mechanism of action is blocking the binding of acetylcholine and numerous other neurotransmitters.2
The literature does not give clear-cut dosing because it is not approved for hyperhidrosis, but gradually increasing doses starting at 2.5 mg daily for a week, then increasing to twice daily for 2 weeks, and then to 5 mg twice daily as a continued dose appears to be the most effective regimen with few side effects. The dosage can be increased, but increased side effects are noted with doses reaching 15 mg/day.1,2
Oxybutynin is not FDA approved for the treatment of hyperhidrosis, but it is an inexpensive drug, which makes it a viable option for use off label given all of the current research with positive outcomes.
It should be noted that if patients have any urinary retention, gastric motility issues, or narrow angle glaucoma, oxybutynin is contraindicated.
More studies are on the horizon, but finally there is hope for hyperhidrosis.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Skin Appendage Disord. 2015 Mar;1(1):6-13.
2. An Bras Dermatol. 2017 Mar-Apr;92(2):217-20.
3. ISRN Dermatol. 2012. doi: 10.5402/2012/702714.
Hyperhidrosis – excessive sweating – is one of those diagnoses that make most physicians cringe because we know that the side effects of most of the common treatments are very limiting and patients continue to be frustrated. New treatments are emerging, and although oxybutynin is not Food and Drug Administration–approved for hyperhidrosis, it does show promise.
Primary hyperhidrosis is the excessive sweating from the axilla, palms, soles, or cranial-facial area. It is a clinical diagnosis that has been occurring for more than 6 months and meets at least four1 of the following criteria:
1. It occurs in eccrine dense areas (axilla, soles, palms or head).
2. It is bilateral and symmetrical.
3. It is absent nocturnally.
4. Its onset should be before age 25 years.
5. It occurs at least weekly.
6. There is a positive family history.
7. It impairs daily activities.
If signs of underlying disease are apparent – such as palpitations, night sweats, weight loss, unilateral symptoms, anxiety, or hypertension – further workup is needed to rule out disorders such as diabetes, hyperthyroidism, pheochromocytoma, or peripheral nerve injury.1
The pathophysiology of hyperhidrosis is not clearly understood. It is believed to be due to increased cholinergic stimulation given that there is no hypertrophy or hyperplasia of the sweat gland.2 Genetics appear to play a role as there is usually a family history of the disorder.2
Topical treatments are usually first line, starting with aluminum chloride antiperspirants, or anticholinergic creams such as glycopyrrolate or glycopyrronium. Unfortunately, many patients complain of the skin irritation so they discontinue their use.1
Botulinum toxin type A is a very safe and effective way of treating hyperhidrosis and is FDA approved for that purpose.3 Its drawbacks are that it is an injection (approximately 25 in each armpit), and it is very costly, usually $1,000-1,500 per session for both underarms. There are no major side effects, and reduction in sweating lasts for 4-12 months, with a median of 6 months.3
Oral treatment of hyperhidrosis, with medications such as glycopyrrolate and benztropine, has been reserved for second- or third-line treatment because of the unwanted side effects of dry mouth and drowsiness. But more recent studies are showing favorable outcomes with oxybutynin.1
Oxybutynin is well known and FDA approved for treatment of urinary frequency, incontinence, and enuresis. Recent studies have shown great success for use to control generalized hyperhidrosis. The mechanism of action is blocking the binding of acetylcholine and numerous other neurotransmitters.2
The literature does not give clear-cut dosing because it is not approved for hyperhidrosis, but gradually increasing doses starting at 2.5 mg daily for a week, then increasing to twice daily for 2 weeks, and then to 5 mg twice daily as a continued dose appears to be the most effective regimen with few side effects. The dosage can be increased, but increased side effects are noted with doses reaching 15 mg/day.1,2
Oxybutynin is not FDA approved for the treatment of hyperhidrosis, but it is an inexpensive drug, which makes it a viable option for use off label given all of the current research with positive outcomes.
It should be noted that if patients have any urinary retention, gastric motility issues, or narrow angle glaucoma, oxybutynin is contraindicated.
More studies are on the horizon, but finally there is hope for hyperhidrosis.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Skin Appendage Disord. 2015 Mar;1(1):6-13.
2. An Bras Dermatol. 2017 Mar-Apr;92(2):217-20.
3. ISRN Dermatol. 2012. doi: 10.5402/2012/702714.
Hyperhidrosis – excessive sweating – is one of those diagnoses that make most physicians cringe because we know that the side effects of most of the common treatments are very limiting and patients continue to be frustrated. New treatments are emerging, and although oxybutynin is not Food and Drug Administration–approved for hyperhidrosis, it does show promise.
Primary hyperhidrosis is the excessive sweating from the axilla, palms, soles, or cranial-facial area. It is a clinical diagnosis that has been occurring for more than 6 months and meets at least four1 of the following criteria:
1. It occurs in eccrine dense areas (axilla, soles, palms or head).
2. It is bilateral and symmetrical.
3. It is absent nocturnally.
4. Its onset should be before age 25 years.
5. It occurs at least weekly.
6. There is a positive family history.
7. It impairs daily activities.
If signs of underlying disease are apparent – such as palpitations, night sweats, weight loss, unilateral symptoms, anxiety, or hypertension – further workup is needed to rule out disorders such as diabetes, hyperthyroidism, pheochromocytoma, or peripheral nerve injury.1
The pathophysiology of hyperhidrosis is not clearly understood. It is believed to be due to increased cholinergic stimulation given that there is no hypertrophy or hyperplasia of the sweat gland.2 Genetics appear to play a role as there is usually a family history of the disorder.2
Topical treatments are usually first line, starting with aluminum chloride antiperspirants, or anticholinergic creams such as glycopyrrolate or glycopyrronium. Unfortunately, many patients complain of the skin irritation so they discontinue their use.1
Botulinum toxin type A is a very safe and effective way of treating hyperhidrosis and is FDA approved for that purpose.3 Its drawbacks are that it is an injection (approximately 25 in each armpit), and it is very costly, usually $1,000-1,500 per session for both underarms. There are no major side effects, and reduction in sweating lasts for 4-12 months, with a median of 6 months.3
Oral treatment of hyperhidrosis, with medications such as glycopyrrolate and benztropine, has been reserved for second- or third-line treatment because of the unwanted side effects of dry mouth and drowsiness. But more recent studies are showing favorable outcomes with oxybutynin.1
Oxybutynin is well known and FDA approved for treatment of urinary frequency, incontinence, and enuresis. Recent studies have shown great success for use to control generalized hyperhidrosis. The mechanism of action is blocking the binding of acetylcholine and numerous other neurotransmitters.2
The literature does not give clear-cut dosing because it is not approved for hyperhidrosis, but gradually increasing doses starting at 2.5 mg daily for a week, then increasing to twice daily for 2 weeks, and then to 5 mg twice daily as a continued dose appears to be the most effective regimen with few side effects. The dosage can be increased, but increased side effects are noted with doses reaching 15 mg/day.1,2
Oxybutynin is not FDA approved for the treatment of hyperhidrosis, but it is an inexpensive drug, which makes it a viable option for use off label given all of the current research with positive outcomes.
It should be noted that if patients have any urinary retention, gastric motility issues, or narrow angle glaucoma, oxybutynin is contraindicated.
More studies are on the horizon, but finally there is hope for hyperhidrosis.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Skin Appendage Disord. 2015 Mar;1(1):6-13.
2. An Bras Dermatol. 2017 Mar-Apr;92(2):217-20.
3. ISRN Dermatol. 2012. doi: 10.5402/2012/702714.
Testicular cancer on the rise
Testicular cancer is noted to be the most common malignant cancer among men aged 15-44 years.1 Despite its being the most common, studies show testicular cancer accounts for only 1% of cancers among men over all. Although several risk factors have been identified, there are no clear direct causes of testicular cancer, and its incidence is on the rise.
In 2004 and again in 2010, the United States Preventive Services Task Force (USPSTF) determined that routine screening in asymptomatic males for testicular cancer either by self-exam or ultrasound did not yield better health outcomes.1 A 2015 study found that testicular cancer incidence in males over 15 years in the United States rose from 5.7/100,000 in 1992 to 6.8/100,000 in 2009, with a significant annual percentage change of 1.1% (P less than .001).2 Thankfully, mortality rates have declined since the 1970s because of the improvements made in chemotherapy regimens.3
Although several studies have investigated this issue, few have been able to determine an exact cause and effect, but several theories have been put forth as likely causes in the rising rates. Most of the established risk factors – such as cryptorchidism, age, race, and exposure to estrogen-mimicking chemicals in utero – have been well described in the literature, but what other factors are affecting our youth?
Increase in sedentary lifestyle is believed to play a role, mostly in relationship to the increase in heat exposure.4 As with cryptorchidism, the elevated temperatures associated with internal body temperatures and testicular exposure to it for extended time periods makes this association reasonable.
Dietary factors have shown a strong relationship to development of testicular cancer, as well. High-fat diets and large intake of dairy products were particularly implicated and correlated regionally with the highest incidences.5 Highest rates of testicular cancer are noted to be in Denmark and other European countries in which there is a high intake of dairy products.
Physical activity such as horseback riding, bicycle riding, and motorcycle riding had varied results when studied, but repeated low-level trauma has been associated with an increased risk of testicular cancer.6
Occupations that have repeated exposure to high-heat environments, such as fireman and factory workers, also showed elevated incidences. Aircraft maintenance and handling of heavy metal and pesticides also have showed a correlation. A substantial amount of evidence indicates that environmental pollutants with estrogenic or antiandrogenic activity are associated with increasing incidence of testicular cancer.4
Genetics have the strongest correlation as a risk factor. It has been well documented that there is an eight- to tenfold increase in risk if a brother has been diagnosed with testicular cancer and a four- to sixfold in risk for the son if a father had testicular cancer. Down syndrome also showed increased genetic risk for testicular cancer.3
Although mortality rates are declining and screening for testicular cancer is not indicated, it is important to remember the risk factors and consider it in the differential diagnosis of a symptomatic male given 26%-56% of newly diagnosed testicular cancer patients were wrongly diagnosed initially.1 Dietary guidance also can be helpful for patients who do have increased risk factors; have them avoid high fat diets and excessive dairy intake. Make patients aware that testicular cancer is most common in younger men, and if they note any changes in their testicle, they should seek medical attention.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Ann Intern Med. 2010;153:396-9.
2. World J Urol. 2015 May;33(5):623-31.
3. N Engl J Med. 2014;371:2005-16.
4. CMAJ. 1999 Jan 26;160(2):213-4.
5. Nat Rev Urol. 2012;9(6):339-49.
6. Int J Cancer. 2005 Sep 1;116(3):331-9.
Testicular cancer is noted to be the most common malignant cancer among men aged 15-44 years.1 Despite its being the most common, studies show testicular cancer accounts for only 1% of cancers among men over all. Although several risk factors have been identified, there are no clear direct causes of testicular cancer, and its incidence is on the rise.
In 2004 and again in 2010, the United States Preventive Services Task Force (USPSTF) determined that routine screening in asymptomatic males for testicular cancer either by self-exam or ultrasound did not yield better health outcomes.1 A 2015 study found that testicular cancer incidence in males over 15 years in the United States rose from 5.7/100,000 in 1992 to 6.8/100,000 in 2009, with a significant annual percentage change of 1.1% (P less than .001).2 Thankfully, mortality rates have declined since the 1970s because of the improvements made in chemotherapy regimens.3
Although several studies have investigated this issue, few have been able to determine an exact cause and effect, but several theories have been put forth as likely causes in the rising rates. Most of the established risk factors – such as cryptorchidism, age, race, and exposure to estrogen-mimicking chemicals in utero – have been well described in the literature, but what other factors are affecting our youth?
Increase in sedentary lifestyle is believed to play a role, mostly in relationship to the increase in heat exposure.4 As with cryptorchidism, the elevated temperatures associated with internal body temperatures and testicular exposure to it for extended time periods makes this association reasonable.
Dietary factors have shown a strong relationship to development of testicular cancer, as well. High-fat diets and large intake of dairy products were particularly implicated and correlated regionally with the highest incidences.5 Highest rates of testicular cancer are noted to be in Denmark and other European countries in which there is a high intake of dairy products.
Physical activity such as horseback riding, bicycle riding, and motorcycle riding had varied results when studied, but repeated low-level trauma has been associated with an increased risk of testicular cancer.6
Occupations that have repeated exposure to high-heat environments, such as fireman and factory workers, also showed elevated incidences. Aircraft maintenance and handling of heavy metal and pesticides also have showed a correlation. A substantial amount of evidence indicates that environmental pollutants with estrogenic or antiandrogenic activity are associated with increasing incidence of testicular cancer.4
Genetics have the strongest correlation as a risk factor. It has been well documented that there is an eight- to tenfold increase in risk if a brother has been diagnosed with testicular cancer and a four- to sixfold in risk for the son if a father had testicular cancer. Down syndrome also showed increased genetic risk for testicular cancer.3
Although mortality rates are declining and screening for testicular cancer is not indicated, it is important to remember the risk factors and consider it in the differential diagnosis of a symptomatic male given 26%-56% of newly diagnosed testicular cancer patients were wrongly diagnosed initially.1 Dietary guidance also can be helpful for patients who do have increased risk factors; have them avoid high fat diets and excessive dairy intake. Make patients aware that testicular cancer is most common in younger men, and if they note any changes in their testicle, they should seek medical attention.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Ann Intern Med. 2010;153:396-9.
2. World J Urol. 2015 May;33(5):623-31.
3. N Engl J Med. 2014;371:2005-16.
4. CMAJ. 1999 Jan 26;160(2):213-4.
5. Nat Rev Urol. 2012;9(6):339-49.
6. Int J Cancer. 2005 Sep 1;116(3):331-9.
Testicular cancer is noted to be the most common malignant cancer among men aged 15-44 years.1 Despite its being the most common, studies show testicular cancer accounts for only 1% of cancers among men over all. Although several risk factors have been identified, there are no clear direct causes of testicular cancer, and its incidence is on the rise.
In 2004 and again in 2010, the United States Preventive Services Task Force (USPSTF) determined that routine screening in asymptomatic males for testicular cancer either by self-exam or ultrasound did not yield better health outcomes.1 A 2015 study found that testicular cancer incidence in males over 15 years in the United States rose from 5.7/100,000 in 1992 to 6.8/100,000 in 2009, with a significant annual percentage change of 1.1% (P less than .001).2 Thankfully, mortality rates have declined since the 1970s because of the improvements made in chemotherapy regimens.3
Although several studies have investigated this issue, few have been able to determine an exact cause and effect, but several theories have been put forth as likely causes in the rising rates. Most of the established risk factors – such as cryptorchidism, age, race, and exposure to estrogen-mimicking chemicals in utero – have been well described in the literature, but what other factors are affecting our youth?
Increase in sedentary lifestyle is believed to play a role, mostly in relationship to the increase in heat exposure.4 As with cryptorchidism, the elevated temperatures associated with internal body temperatures and testicular exposure to it for extended time periods makes this association reasonable.
Dietary factors have shown a strong relationship to development of testicular cancer, as well. High-fat diets and large intake of dairy products were particularly implicated and correlated regionally with the highest incidences.5 Highest rates of testicular cancer are noted to be in Denmark and other European countries in which there is a high intake of dairy products.
Physical activity such as horseback riding, bicycle riding, and motorcycle riding had varied results when studied, but repeated low-level trauma has been associated with an increased risk of testicular cancer.6
Occupations that have repeated exposure to high-heat environments, such as fireman and factory workers, also showed elevated incidences. Aircraft maintenance and handling of heavy metal and pesticides also have showed a correlation. A substantial amount of evidence indicates that environmental pollutants with estrogenic or antiandrogenic activity are associated with increasing incidence of testicular cancer.4
Genetics have the strongest correlation as a risk factor. It has been well documented that there is an eight- to tenfold increase in risk if a brother has been diagnosed with testicular cancer and a four- to sixfold in risk for the son if a father had testicular cancer. Down syndrome also showed increased genetic risk for testicular cancer.3
Although mortality rates are declining and screening for testicular cancer is not indicated, it is important to remember the risk factors and consider it in the differential diagnosis of a symptomatic male given 26%-56% of newly diagnosed testicular cancer patients were wrongly diagnosed initially.1 Dietary guidance also can be helpful for patients who do have increased risk factors; have them avoid high fat diets and excessive dairy intake. Make patients aware that testicular cancer is most common in younger men, and if they note any changes in their testicle, they should seek medical attention.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Ann Intern Med. 2010;153:396-9.
2. World J Urol. 2015 May;33(5):623-31.
3. N Engl J Med. 2014;371:2005-16.
4. CMAJ. 1999 Jan 26;160(2):213-4.
5. Nat Rev Urol. 2012;9(6):339-49.
6. Int J Cancer. 2005 Sep 1;116(3):331-9.
Educate your adolescent patients about herpes
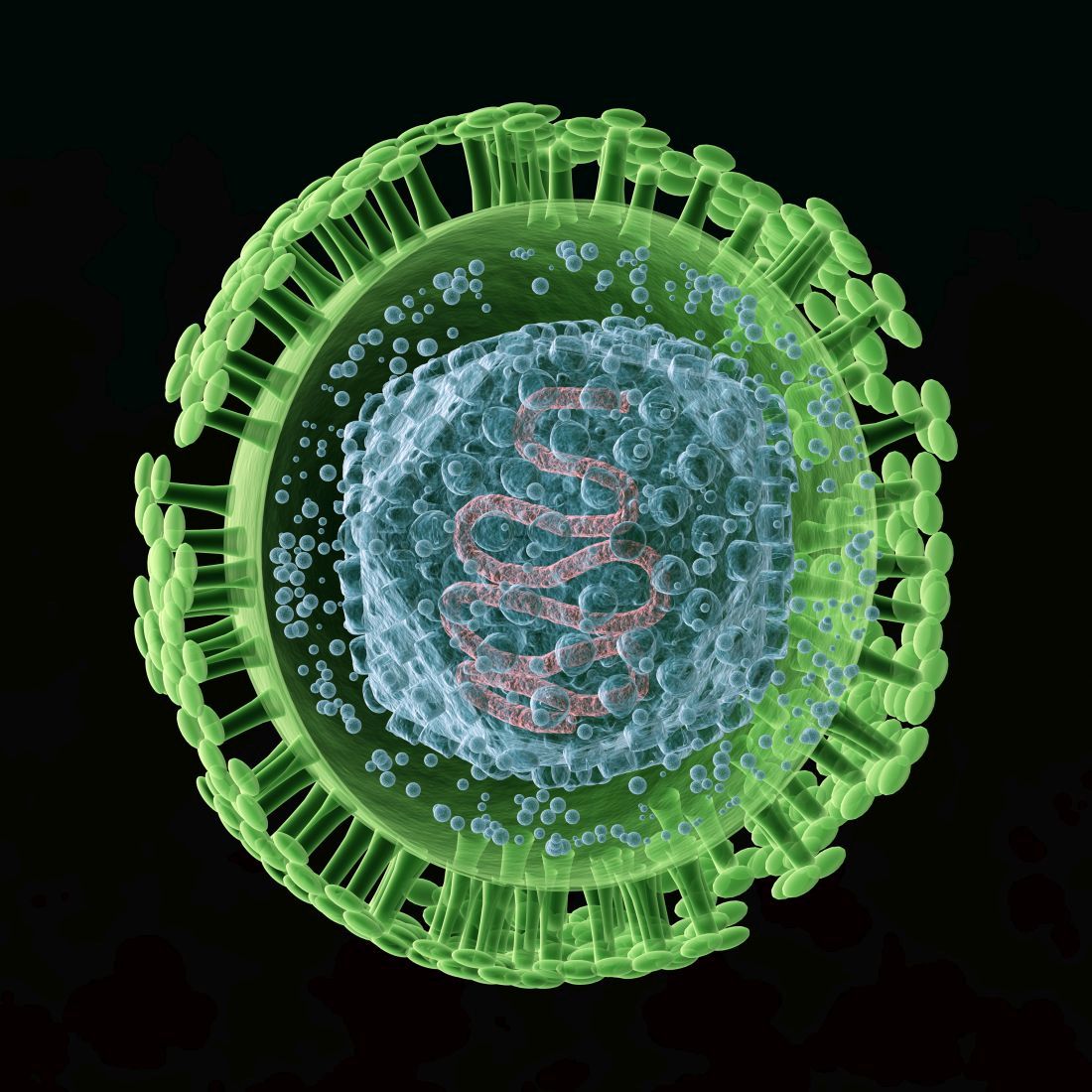
We are all familiar with the line, “Herpes lasts forever.” There is no cure for infection with a herpes virus, whether it is herpes simplex 1 (HSV-1) or herpes simplex 2 (HSV-2).
There are antivirals to reduce the length and severity of flare-ups, and continued therapy can suppress the virus, which reduces shedding. Both HSV-1 and HSV-2 can cause genital herpes and oral herpes, i.e. cold sores. HSV-1 has a milder initial episode and fewer flareups, whereas HSV-2 can have a more severe initial episode and frequent flareups.1
According to data from the National Health and Nutrition Examination Survey (NHANES) for 2015-2016, HSV-1 prevalence was 48% among 14- to 19-year-olds and HSV-2 prevalence was 12% in the same age group. Overall, age-adjusted HSV-1 prevalence was higher in females (51%) than in males (45%) in persons aged 14-49 years.2
The reality is that most people with HSV-1 or HSV-2 don’t even know they have it, as both tend to be asymptomatic. Therefore, all reported statistics are grossly underrepresenting the prevalence of the disease.
HSV is a common disease. Regardless of symptoms, shedding occurs. Although condoms reduce the risk of spread, using one doesn’t eliminate it because of the possibility of contact beyond the area covered by the condom and the ability of HSV to be passed through oral sex. The only true prevention is abstinence.
Herpes simplex virus is a sexually transmitted infection that is lifelong. Its presence can increase the risk of contracting HIV. If it is contracted in the third trimester of pregnancy or if a breakout occurs during the third trimester, risk of transmitting to the infant can occur, with devastating neurological impact. Despite the seriousness and longevity of the virus, the vast majority of people with the virus have it unknowingly, and live normal healthy lives.
It is just as important that we educate them that, if they contract herpes, it is not end of their ability to have intimate relationships. Debunking the myth that HSV-2 is a worse disease to have than HSV-1 can significantly reduce the psychological burden caused by this disease, and encourage patients to be more honest about their diagnosis. This not only will assist people in seeking medical advice if they have concerns, but it will encourage conversations about HSV, which hopefully will reduce spread of the virus.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. J Infect Dis. 2014 Feb. doi: 10.1093/infdis/jit458.
2. NCHS Data Brief, no 304. 2018 Feb.
We are all familiar with the line, “Herpes lasts forever.” There is no cure for infection with a herpes virus, whether it is herpes simplex 1 (HSV-1) or herpes simplex 2 (HSV-2).
There are antivirals to reduce the length and severity of flare-ups, and continued therapy can suppress the virus, which reduces shedding. Both HSV-1 and HSV-2 can cause genital herpes and oral herpes, i.e. cold sores. HSV-1 has a milder initial episode and fewer flareups, whereas HSV-2 can have a more severe initial episode and frequent flareups.1
According to data from the National Health and Nutrition Examination Survey (NHANES) for 2015-2016, HSV-1 prevalence was 48% among 14- to 19-year-olds and HSV-2 prevalence was 12% in the same age group. Overall, age-adjusted HSV-1 prevalence was higher in females (51%) than in males (45%) in persons aged 14-49 years.2
The reality is that most people with HSV-1 or HSV-2 don’t even know they have it, as both tend to be asymptomatic. Therefore, all reported statistics are grossly underrepresenting the prevalence of the disease.
HSV is a common disease. Regardless of symptoms, shedding occurs. Although condoms reduce the risk of spread, using one doesn’t eliminate it because of the possibility of contact beyond the area covered by the condom and the ability of HSV to be passed through oral sex. The only true prevention is abstinence.
Herpes simplex virus is a sexually transmitted infection that is lifelong. Its presence can increase the risk of contracting HIV. If it is contracted in the third trimester of pregnancy or if a breakout occurs during the third trimester, risk of transmitting to the infant can occur, with devastating neurological impact. Despite the seriousness and longevity of the virus, the vast majority of people with the virus have it unknowingly, and live normal healthy lives.
It is just as important that we educate them that, if they contract herpes, it is not end of their ability to have intimate relationships. Debunking the myth that HSV-2 is a worse disease to have than HSV-1 can significantly reduce the psychological burden caused by this disease, and encourage patients to be more honest about their diagnosis. This not only will assist people in seeking medical advice if they have concerns, but it will encourage conversations about HSV, which hopefully will reduce spread of the virus.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. J Infect Dis. 2014 Feb. doi: 10.1093/infdis/jit458.
2. NCHS Data Brief, no 304. 2018 Feb.
We are all familiar with the line, “Herpes lasts forever.” There is no cure for infection with a herpes virus, whether it is herpes simplex 1 (HSV-1) or herpes simplex 2 (HSV-2).
There are antivirals to reduce the length and severity of flare-ups, and continued therapy can suppress the virus, which reduces shedding. Both HSV-1 and HSV-2 can cause genital herpes and oral herpes, i.e. cold sores. HSV-1 has a milder initial episode and fewer flareups, whereas HSV-2 can have a more severe initial episode and frequent flareups.1
According to data from the National Health and Nutrition Examination Survey (NHANES) for 2015-2016, HSV-1 prevalence was 48% among 14- to 19-year-olds and HSV-2 prevalence was 12% in the same age group. Overall, age-adjusted HSV-1 prevalence was higher in females (51%) than in males (45%) in persons aged 14-49 years.2
The reality is that most people with HSV-1 or HSV-2 don’t even know they have it, as both tend to be asymptomatic. Therefore, all reported statistics are grossly underrepresenting the prevalence of the disease.
HSV is a common disease. Regardless of symptoms, shedding occurs. Although condoms reduce the risk of spread, using one doesn’t eliminate it because of the possibility of contact beyond the area covered by the condom and the ability of HSV to be passed through oral sex. The only true prevention is abstinence.
Herpes simplex virus is a sexually transmitted infection that is lifelong. Its presence can increase the risk of contracting HIV. If it is contracted in the third trimester of pregnancy or if a breakout occurs during the third trimester, risk of transmitting to the infant can occur, with devastating neurological impact. Despite the seriousness and longevity of the virus, the vast majority of people with the virus have it unknowingly, and live normal healthy lives.
It is just as important that we educate them that, if they contract herpes, it is not end of their ability to have intimate relationships. Debunking the myth that HSV-2 is a worse disease to have than HSV-1 can significantly reduce the psychological burden caused by this disease, and encourage patients to be more honest about their diagnosis. This not only will assist people in seeking medical advice if they have concerns, but it will encourage conversations about HSV, which hopefully will reduce spread of the virus.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. J Infect Dis. 2014 Feb. doi: 10.1093/infdis/jit458.
2. NCHS Data Brief, no 304. 2018 Feb.
Pseudotumor cerebri pediatric rates are rising
Pseudotumor cerebri, benign intracranial hypertension, and idiopathic intracranial hypertension are all terms to describe a syndrome of increased intracranial pressure, headaches, vision loss, or changes without an associated mass lesion.1 The condition was considered relatively rare, presenting most commonly in obese women in childbearing years. Surprisingly, 2
Obesity is the fastest growing morbidity among adolescents. The Centers for Disease Control and Prevention reported 32% of children 2-19 years were obese.1 This reality is impacting many areas of an adolescent’s health, but it also is changing the landscape of diseases that present in this age group. Although pediatric and adult pseudotumor cerebri always have had slightly varied features, many features were similar such as the papilledema, vision loss, headaches, and sixth nerve palsy. Obesity and female predominance tended to present more in the adult population, as many pediatric patients were not obese,2 and had fewer associated symptoms at the time of diagnosis, and the cause was thought to idiopathic.
Now, with the increase in obesity, more adolescents and more male patients are presenting with pseudotumor cerebri as a cause for their headache, and 57%-100% are obese, making it a compounding factor.3
Pediatric populations also are at risk of secondary pseudotumor cerebri, which is an increase in intracranial pressure from the use of medication, or other disease states such as anemia, kidney disease, or Down syndrome. Minocycline use is the most common medication cause and usually presents 1-2 months after normal use.4 Discontinuing the drug does lead to resolution. Retinoids, vitamin A products, growth hormone, and steroids also have been implicated. Given that acne is a common complaint amongst teens, knowledge of these side effects is important.4
In 2013, the criteria for diagnosis of pseudotumor cerebri was revised. Currently, the presence of papilledema, normal neurologic exam except for abnormal sixth cranial nerve, normal cerebral spinal fluid, elevated lumbar opening pressure, and normal imaging are needed for a definitive diagnosis. A probable diagnosis can be made if papilledema is not present but there abducens nerve palsy.2
In a routine physical exam, when I questioned a patient on any medication that was used daily, she replied she took ibuprofen daily for headaches and that she had been doing this for several months. Headaches were not in her chief complaints as she had learned to live with and ignore this symptom. Upon further evaluation, she was slightly overweight and has a questionable fundoscopic exam. After further evaluation by an ophthalmologist and a neurologist, pseudotumor cerebri was diagnosed.
Index of suspicion is key in correctly diagnosing patients, and understanding the changing landscape of medicine will lead to more thoughtful questioning during routine health exams and better outcomes for your patients.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Am J Ophthalmol. 2015 Feb;159(2):344-52.e1.
2. Horm Res Paediatr. 2014;81(4):217-25.
3. Clin Imaging. 2018 May 24. doi: 10.1016/j.clinimag.2018.05.020.
4. Am J Ophthalmol. 1998 Jul;126(1):116-21.
5. Glob Pediatr Health. 2018. doi:10.1177/2333794X18785550.
Pseudotumor cerebri, benign intracranial hypertension, and idiopathic intracranial hypertension are all terms to describe a syndrome of increased intracranial pressure, headaches, vision loss, or changes without an associated mass lesion.1 The condition was considered relatively rare, presenting most commonly in obese women in childbearing years. Surprisingly, 2
Obesity is the fastest growing morbidity among adolescents. The Centers for Disease Control and Prevention reported 32% of children 2-19 years were obese.1 This reality is impacting many areas of an adolescent’s health, but it also is changing the landscape of diseases that present in this age group. Although pediatric and adult pseudotumor cerebri always have had slightly varied features, many features were similar such as the papilledema, vision loss, headaches, and sixth nerve palsy. Obesity and female predominance tended to present more in the adult population, as many pediatric patients were not obese,2 and had fewer associated symptoms at the time of diagnosis, and the cause was thought to idiopathic.
Now, with the increase in obesity, more adolescents and more male patients are presenting with pseudotumor cerebri as a cause for their headache, and 57%-100% are obese, making it a compounding factor.3
Pediatric populations also are at risk of secondary pseudotumor cerebri, which is an increase in intracranial pressure from the use of medication, or other disease states such as anemia, kidney disease, or Down syndrome. Minocycline use is the most common medication cause and usually presents 1-2 months after normal use.4 Discontinuing the drug does lead to resolution. Retinoids, vitamin A products, growth hormone, and steroids also have been implicated. Given that acne is a common complaint amongst teens, knowledge of these side effects is important.4
In 2013, the criteria for diagnosis of pseudotumor cerebri was revised. Currently, the presence of papilledema, normal neurologic exam except for abnormal sixth cranial nerve, normal cerebral spinal fluid, elevated lumbar opening pressure, and normal imaging are needed for a definitive diagnosis. A probable diagnosis can be made if papilledema is not present but there abducens nerve palsy.2
In a routine physical exam, when I questioned a patient on any medication that was used daily, she replied she took ibuprofen daily for headaches and that she had been doing this for several months. Headaches were not in her chief complaints as she had learned to live with and ignore this symptom. Upon further evaluation, she was slightly overweight and has a questionable fundoscopic exam. After further evaluation by an ophthalmologist and a neurologist, pseudotumor cerebri was diagnosed.
Index of suspicion is key in correctly diagnosing patients, and understanding the changing landscape of medicine will lead to more thoughtful questioning during routine health exams and better outcomes for your patients.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Am J Ophthalmol. 2015 Feb;159(2):344-52.e1.
2. Horm Res Paediatr. 2014;81(4):217-25.
3. Clin Imaging. 2018 May 24. doi: 10.1016/j.clinimag.2018.05.020.
4. Am J Ophthalmol. 1998 Jul;126(1):116-21.
5. Glob Pediatr Health. 2018. doi:10.1177/2333794X18785550.
Pseudotumor cerebri, benign intracranial hypertension, and idiopathic intracranial hypertension are all terms to describe a syndrome of increased intracranial pressure, headaches, vision loss, or changes without an associated mass lesion.1 The condition was considered relatively rare, presenting most commonly in obese women in childbearing years. Surprisingly, 2
Obesity is the fastest growing morbidity among adolescents. The Centers for Disease Control and Prevention reported 32% of children 2-19 years were obese.1 This reality is impacting many areas of an adolescent’s health, but it also is changing the landscape of diseases that present in this age group. Although pediatric and adult pseudotumor cerebri always have had slightly varied features, many features were similar such as the papilledema, vision loss, headaches, and sixth nerve palsy. Obesity and female predominance tended to present more in the adult population, as many pediatric patients were not obese,2 and had fewer associated symptoms at the time of diagnosis, and the cause was thought to idiopathic.
Now, with the increase in obesity, more adolescents and more male patients are presenting with pseudotumor cerebri as a cause for their headache, and 57%-100% are obese, making it a compounding factor.3
Pediatric populations also are at risk of secondary pseudotumor cerebri, which is an increase in intracranial pressure from the use of medication, or other disease states such as anemia, kidney disease, or Down syndrome. Minocycline use is the most common medication cause and usually presents 1-2 months after normal use.4 Discontinuing the drug does lead to resolution. Retinoids, vitamin A products, growth hormone, and steroids also have been implicated. Given that acne is a common complaint amongst teens, knowledge of these side effects is important.4
In 2013, the criteria for diagnosis of pseudotumor cerebri was revised. Currently, the presence of papilledema, normal neurologic exam except for abnormal sixth cranial nerve, normal cerebral spinal fluid, elevated lumbar opening pressure, and normal imaging are needed for a definitive diagnosis. A probable diagnosis can be made if papilledema is not present but there abducens nerve palsy.2
In a routine physical exam, when I questioned a patient on any medication that was used daily, she replied she took ibuprofen daily for headaches and that she had been doing this for several months. Headaches were not in her chief complaints as she had learned to live with and ignore this symptom. Upon further evaluation, she was slightly overweight and has a questionable fundoscopic exam. After further evaluation by an ophthalmologist and a neurologist, pseudotumor cerebri was diagnosed.
Index of suspicion is key in correctly diagnosing patients, and understanding the changing landscape of medicine will lead to more thoughtful questioning during routine health exams and better outcomes for your patients.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Am J Ophthalmol. 2015 Feb;159(2):344-52.e1.
2. Horm Res Paediatr. 2014;81(4):217-25.
3. Clin Imaging. 2018 May 24. doi: 10.1016/j.clinimag.2018.05.020.
4. Am J Ophthalmol. 1998 Jul;126(1):116-21.
5. Glob Pediatr Health. 2018. doi:10.1177/2333794X18785550.
Emergency contraception ... and our duty to inform
In 2013, the emergency contraception containing levonorgestrel, most commonly known as Plan B, became available for purchase without prescription or age restriction. Yet, 5 years later, many adolescents and teens remain misinformed or uninformed completely. For the scope of this article, only levonorgestrel will be discussed, acknowledging that ulipristal acetate (Ella) is also an emergency contraception by prescription.
As providers we all recognize the challenges of engaging a teen patient long enough to have a meaningful conversation on health and wellness. There are even greater challenges when it comes to discussing sexual activity and sexually transmitted diseases. So the thought of discussing prevention of unwanted pregnancy may be daunting for most of us.
This topic has many layers. First and foremost, it touches on a hotly debated topic of where life begins, and emergency contraception may be thought to cross that line. Awareness of the option of emergency contraception is thought to give a free pass to promiscuous behavior. Some just feel there is not enough research to support the safe use of these products in adolescents. As with most things, taking the time to educate ourselves on the facts usually alleviates the conflicts.
Understanding levonorgestrel mechanism of action is important in clarifying its position in the prolife debate. The International Consortium for Emergency Contraception and the International Federation of Gynecologists and Obstetrics consider that inhibition or delay of ovulation is levonorgestrel’s mechanism of action, and that it does not prevent implantation of a fertilized egg. If taken after ovulation has occurred, it is ineffective in preventing pregnancy.1,2
Levonorgestrel emergency contraception was first approved by the Food and Drug Administration in 1999 under the brand name Plan B by Teva Women’s Health, then later Next Choice (Watson Pharma) was released. Initially, it was prescribed to be taken as a 0.75-mg tab within 72 hours of unprotected intercourse and repeated in 12 hours. Further studies revealed taking a 1.5-mg tab once was just as effective with no significant increase in adverse effects and Plan B One-Step was released.3
The Catholic Health Association presented a paper clarifying that levonorgestrel is not a postfertilization contraceptive (abortifacient), hopefully preventing delay of its use in victims of sexual assault seen in Catholic health care facilities.4
Safety for this product since its release has shown no deaths or serious complications.2 The most common side effect is nausea, usually without vomiting.2 Antinausea medication given 1 hour before can be helpful but is not routinely used. The length of menstrual cycle is shorter if given early in cycle but it may be lengthened by 2 days if taken post ovulation. It is not intended for repeated use, but 11 studies showed no adverse effects when it was used repeatedly in the same ovulatory cycle, and it was shown to be safe.2
For women whose emergency contraception failed, one study of 332 pregnant women who had used levonorgestrel found no teratogenic effect or risk of birth defects.5 Although it is not contraindicated in breastfeeding mothers, it was recommended that patients discontinue breastfeeding for 8 hours post ingestion. Recognized contraindications to oral contraceptives do not apply to levonorgestrel, given the temporary and relative low exposure to the hormone.3
As for efficacy, timing is of the essence. As stated previously, if not taken before ovulation has occurred, it is ineffective. If taken within 72 hours of unprotected intercourse, one study showed levonorgestrel would prevent 85% of pregnancies that otherwise might have occurred.3 Although the package insert says it must taken within 72 hours, studies have shown protection up to 120 hours post coitus, but that efficacy declines with every hour. Body mass index also may play a role in effectiveness, but the studies have been varied and more research is required before a determination is made.2
The annual well visit is the opportune time to educate parents and teens about abstinence, sex, sexually transmitted infections, and emergency contraception. Parents need to know the statistics of teen pregnancy and rates of STIs so they can be informed and further these conversations at home. should they find themselves in this dilemma. The websites not-2-late.com and bedsider.org are excellent sources of information on emergency contraception.
Keep in mind that 10% of all unintended pregnancies occur from nonconsensual intercourse so knowing what options are available is critical. Whether you give a handout with the information or undertake a more in-depth conversation during well visits, this is vital information that can change a person’s life.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Emergency Contraception: Questions And Answers For Decision-Makers,” International Consortium for Emergency Contraception, 2013.
2. Clin Obstet Gynecol. 2014 Dec;57(4):741-50.
3. Pediatrics 2012;130:1174-82.
4. Health Progress. 2010 Jan-Feb. 59-61.
5. Hum Reprod. 2009 Jul;24(7):1605-11.
6. Contraception. 2016 Feb;93(2):145-52.
In 2013, the emergency contraception containing levonorgestrel, most commonly known as Plan B, became available for purchase without prescription or age restriction. Yet, 5 years later, many adolescents and teens remain misinformed or uninformed completely. For the scope of this article, only levonorgestrel will be discussed, acknowledging that ulipristal acetate (Ella) is also an emergency contraception by prescription.
As providers we all recognize the challenges of engaging a teen patient long enough to have a meaningful conversation on health and wellness. There are even greater challenges when it comes to discussing sexual activity and sexually transmitted diseases. So the thought of discussing prevention of unwanted pregnancy may be daunting for most of us.
This topic has many layers. First and foremost, it touches on a hotly debated topic of where life begins, and emergency contraception may be thought to cross that line. Awareness of the option of emergency contraception is thought to give a free pass to promiscuous behavior. Some just feel there is not enough research to support the safe use of these products in adolescents. As with most things, taking the time to educate ourselves on the facts usually alleviates the conflicts.
Understanding levonorgestrel mechanism of action is important in clarifying its position in the prolife debate. The International Consortium for Emergency Contraception and the International Federation of Gynecologists and Obstetrics consider that inhibition or delay of ovulation is levonorgestrel’s mechanism of action, and that it does not prevent implantation of a fertilized egg. If taken after ovulation has occurred, it is ineffective in preventing pregnancy.1,2
Levonorgestrel emergency contraception was first approved by the Food and Drug Administration in 1999 under the brand name Plan B by Teva Women’s Health, then later Next Choice (Watson Pharma) was released. Initially, it was prescribed to be taken as a 0.75-mg tab within 72 hours of unprotected intercourse and repeated in 12 hours. Further studies revealed taking a 1.5-mg tab once was just as effective with no significant increase in adverse effects and Plan B One-Step was released.3
The Catholic Health Association presented a paper clarifying that levonorgestrel is not a postfertilization contraceptive (abortifacient), hopefully preventing delay of its use in victims of sexual assault seen in Catholic health care facilities.4
Safety for this product since its release has shown no deaths or serious complications.2 The most common side effect is nausea, usually without vomiting.2 Antinausea medication given 1 hour before can be helpful but is not routinely used. The length of menstrual cycle is shorter if given early in cycle but it may be lengthened by 2 days if taken post ovulation. It is not intended for repeated use, but 11 studies showed no adverse effects when it was used repeatedly in the same ovulatory cycle, and it was shown to be safe.2
For women whose emergency contraception failed, one study of 332 pregnant women who had used levonorgestrel found no teratogenic effect or risk of birth defects.5 Although it is not contraindicated in breastfeeding mothers, it was recommended that patients discontinue breastfeeding for 8 hours post ingestion. Recognized contraindications to oral contraceptives do not apply to levonorgestrel, given the temporary and relative low exposure to the hormone.3
As for efficacy, timing is of the essence. As stated previously, if not taken before ovulation has occurred, it is ineffective. If taken within 72 hours of unprotected intercourse, one study showed levonorgestrel would prevent 85% of pregnancies that otherwise might have occurred.3 Although the package insert says it must taken within 72 hours, studies have shown protection up to 120 hours post coitus, but that efficacy declines with every hour. Body mass index also may play a role in effectiveness, but the studies have been varied and more research is required before a determination is made.2
The annual well visit is the opportune time to educate parents and teens about abstinence, sex, sexually transmitted infections, and emergency contraception. Parents need to know the statistics of teen pregnancy and rates of STIs so they can be informed and further these conversations at home. should they find themselves in this dilemma. The websites not-2-late.com and bedsider.org are excellent sources of information on emergency contraception.
Keep in mind that 10% of all unintended pregnancies occur from nonconsensual intercourse so knowing what options are available is critical. Whether you give a handout with the information or undertake a more in-depth conversation during well visits, this is vital information that can change a person’s life.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Emergency Contraception: Questions And Answers For Decision-Makers,” International Consortium for Emergency Contraception, 2013.
2. Clin Obstet Gynecol. 2014 Dec;57(4):741-50.
3. Pediatrics 2012;130:1174-82.
4. Health Progress. 2010 Jan-Feb. 59-61.
5. Hum Reprod. 2009 Jul;24(7):1605-11.
6. Contraception. 2016 Feb;93(2):145-52.
In 2013, the emergency contraception containing levonorgestrel, most commonly known as Plan B, became available for purchase without prescription or age restriction. Yet, 5 years later, many adolescents and teens remain misinformed or uninformed completely. For the scope of this article, only levonorgestrel will be discussed, acknowledging that ulipristal acetate (Ella) is also an emergency contraception by prescription.
As providers we all recognize the challenges of engaging a teen patient long enough to have a meaningful conversation on health and wellness. There are even greater challenges when it comes to discussing sexual activity and sexually transmitted diseases. So the thought of discussing prevention of unwanted pregnancy may be daunting for most of us.
This topic has many layers. First and foremost, it touches on a hotly debated topic of where life begins, and emergency contraception may be thought to cross that line. Awareness of the option of emergency contraception is thought to give a free pass to promiscuous behavior. Some just feel there is not enough research to support the safe use of these products in adolescents. As with most things, taking the time to educate ourselves on the facts usually alleviates the conflicts.
Understanding levonorgestrel mechanism of action is important in clarifying its position in the prolife debate. The International Consortium for Emergency Contraception and the International Federation of Gynecologists and Obstetrics consider that inhibition or delay of ovulation is levonorgestrel’s mechanism of action, and that it does not prevent implantation of a fertilized egg. If taken after ovulation has occurred, it is ineffective in preventing pregnancy.1,2
Levonorgestrel emergency contraception was first approved by the Food and Drug Administration in 1999 under the brand name Plan B by Teva Women’s Health, then later Next Choice (Watson Pharma) was released. Initially, it was prescribed to be taken as a 0.75-mg tab within 72 hours of unprotected intercourse and repeated in 12 hours. Further studies revealed taking a 1.5-mg tab once was just as effective with no significant increase in adverse effects and Plan B One-Step was released.3
The Catholic Health Association presented a paper clarifying that levonorgestrel is not a postfertilization contraceptive (abortifacient), hopefully preventing delay of its use in victims of sexual assault seen in Catholic health care facilities.4
Safety for this product since its release has shown no deaths or serious complications.2 The most common side effect is nausea, usually without vomiting.2 Antinausea medication given 1 hour before can be helpful but is not routinely used. The length of menstrual cycle is shorter if given early in cycle but it may be lengthened by 2 days if taken post ovulation. It is not intended for repeated use, but 11 studies showed no adverse effects when it was used repeatedly in the same ovulatory cycle, and it was shown to be safe.2
For women whose emergency contraception failed, one study of 332 pregnant women who had used levonorgestrel found no teratogenic effect or risk of birth defects.5 Although it is not contraindicated in breastfeeding mothers, it was recommended that patients discontinue breastfeeding for 8 hours post ingestion. Recognized contraindications to oral contraceptives do not apply to levonorgestrel, given the temporary and relative low exposure to the hormone.3
As for efficacy, timing is of the essence. As stated previously, if not taken before ovulation has occurred, it is ineffective. If taken within 72 hours of unprotected intercourse, one study showed levonorgestrel would prevent 85% of pregnancies that otherwise might have occurred.3 Although the package insert says it must taken within 72 hours, studies have shown protection up to 120 hours post coitus, but that efficacy declines with every hour. Body mass index also may play a role in effectiveness, but the studies have been varied and more research is required before a determination is made.2
The annual well visit is the opportune time to educate parents and teens about abstinence, sex, sexually transmitted infections, and emergency contraception. Parents need to know the statistics of teen pregnancy and rates of STIs so they can be informed and further these conversations at home. should they find themselves in this dilemma. The websites not-2-late.com and bedsider.org are excellent sources of information on emergency contraception.
Keep in mind that 10% of all unintended pregnancies occur from nonconsensual intercourse so knowing what options are available is critical. Whether you give a handout with the information or undertake a more in-depth conversation during well visits, this is vital information that can change a person’s life.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Emergency Contraception: Questions And Answers For Decision-Makers,” International Consortium for Emergency Contraception, 2013.
2. Clin Obstet Gynecol. 2014 Dec;57(4):741-50.
3. Pediatrics 2012;130:1174-82.
4. Health Progress. 2010 Jan-Feb. 59-61.
5. Hum Reprod. 2009 Jul;24(7):1605-11.
6. Contraception. 2016 Feb;93(2):145-52.
Incredible edibles … Guilty as charged
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@MDedge.com.
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@MDedge.com.
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@MDedge.com.
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
The care of ‘down there’
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Pes planus: To treat or not to treat
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Down syndrome in adolescents
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
Steroid use in adolescents
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at pdnews@frontlinemedcom.com.