User login
Overreliance on subspecialty in a case of endocarditis
Story
DB was a 20-year-old woman who presented to her primary care physician (PCP) with fever and myalgias. Her past medical history was significant for open heart surgery 3 years earlier for ventricular myxoma and aortic valve repair. Her temperature in the office was 39.1 C. Her examination was otherwise unremarkable. An influenza swab was negative. Cultures were drawn and DB was sent home with instructions to increase her fluids and use acetaminophen and ibuprofen as needed. Two days later, 2 out of 2 preliminary blood cultures were reported positive for coagulase-negative, gram positive cocci in clusters. DB was referred to the hospital where she was admitted by Dr. Hospitalist.
Dr. Hospitalist performed a history and physical and noted an impression of sepsis from subacute bacterial endocarditis. He initiated intravenous vancomycin and ceftriaxone, repeated blood cultures, ordered an echocardiogram, and obtained an infectious disease (ID) consult. On hospital day 2, the ID consultant documented that DB had positive blood cultures for coagulase-negative staphylococci but no true evidence of sepsis. She was noted to be afebrile with a normal white blood cell count. Although the echocardiogram was pending, the ID consultant recommended that intravenous antibiotics be discontinued and that she was safe to be discharged home with follow-up blood cultures in 1 week. Later that day, the echocardiogram found a thickened aortic valve with an increased density that suggested possible vegetation.
On the morning of hospital day 3, DB had a Tmax (time to maximum plasma concentration) of 38.8 C overnight. The repeat blood cultures drawn on admission showed no growth to date. Dr. Hospitalist stopped the intravenous antibiotics and discharged DB to home. Unknown to Dr. Hospitalist at the time, the original cultures drawn at the PCP’s office were finalized as Staphylococcus lugdunensis.
One week later, DB followed up with her PCP. She continued to have fevers, myalgias, and fatigue. Blood cultures were obtained and reported the following day as 2 out of 2 positive for S. lugdunensis. DB once again returned to the hospital and was started on intravenous antibiotics. Two days into her second hospital stay, DB complained of feeling hot. She sat up in the bed and then went unconscious. After almost 2 hours of resuscitation, DB was pronounced dead. An autopsy was performed and identified the cause of death as bacterial endocarditis (S. lugdunensis) with massive vegetations and aortic valve rupture.
Complaint
DB’s mother immediately brought a claim against Dr. Hospitalist and the ID consultant from the first hospital stay. The complaint alleged that DB was inappropriately discharged from the first hospitalization without ongoing intravenous antibiotic therapy. As a result, DB missed 8 days of antibiotic treatment allowing her untreated infection to irreversibly damage her heart. The complaint further alleged that this gap in treatment was the proximate cause of DB’s death.
Scientific principles
Staphylococcus lugdunensis is a coagulase-negative staphylococcus (CNS). Like other CNS, S. lugdunensis in humans ranges from a harmless skin commensal to a life-threatening pathogen (as with infective endocarditis). Unlike other CNS, however, S. lugdunensis can cause severe disease reminiscent of the virulent infections frequently attributable to S. aureus. S. lugdunensis endocarditis is an aggressive infection that affects native valves with greater frequency than prosthetic valves in contrast to other CNS. S. lugdunensis native valve endocarditis is typically community acquired and is associated with a high rate of complications and death.
Complaint rebuttal and discussion
The only defense that Dr. Hospitalist offered was that he relied on his subspecialty consultant. Dr. Hospitalist argued that he was a generalist and not an expert in endocarditis or CNS. As a result, he followed the recommendations of the ID consultant and he further argued that he had the right to do so.
The plaintiff countered essentially countered with "Would you jump off the roof of a building just because someone told you to?" argument. In this case, the positive blood cultures, the history of aortic valve repair, and the suggestive echocardiogram were indisputable facts. Discovery in this case confirmed that Dr. Hospitalist never spoke with the ID consultant at any point during the first hospital stay.
Plaintiff experts argued that Dr. Hospitalist was a board-certified internist practicing hospital-based internal medicine and as such, he had or should have had the requisite knowledge, skills, and attitudes to evaluate, diagnose, and treat endocarditis. In this case, it appeared that Dr. Hospitalist "blindly" followed the recommendations of the ID consultant without considering all the evidence at hand. Plaintiff experts argued that in this situation, the standard of care required that Dr. Hospitalist question the plan of care outlined by his consultant. Had he done so, it is likely that both Dr. Hospitalist and the infectious disease consultant would have learned that the original blood cultures grew S. lugdunensis and antibiotics would never have been discontinued.
Conclusion
As the attending physicians of record, hospitalists carry the ultimate responsibility for the discharge decision. It is common to ask subspecialty consultants their opinion regarding stability for discharge and/or the need for ongoing hospital therapy. Yet, it is important for all hospitalists to remember that the consultant recommendations are just opinions that must be weighed against all the other evidence currently available. It is also helpful to have and document verbal discussions with consultants when discharge decisions are being made (and partially relied upon) with their subspecialty input.
The ID consultant in this case settled almost immediately with DB’s family. Dr. Hospitalist defended himself a little longer, but ultimately settled this case with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
DB was a 20-year-old woman who presented to her primary care physician (PCP) with fever and myalgias. Her past medical history was significant for open heart surgery 3 years earlier for ventricular myxoma and aortic valve repair. Her temperature in the office was 39.1 C. Her examination was otherwise unremarkable. An influenza swab was negative. Cultures were drawn and DB was sent home with instructions to increase her fluids and use acetaminophen and ibuprofen as needed. Two days later, 2 out of 2 preliminary blood cultures were reported positive for coagulase-negative, gram positive cocci in clusters. DB was referred to the hospital where she was admitted by Dr. Hospitalist.
Dr. Hospitalist performed a history and physical and noted an impression of sepsis from subacute bacterial endocarditis. He initiated intravenous vancomycin and ceftriaxone, repeated blood cultures, ordered an echocardiogram, and obtained an infectious disease (ID) consult. On hospital day 2, the ID consultant documented that DB had positive blood cultures for coagulase-negative staphylococci but no true evidence of sepsis. She was noted to be afebrile with a normal white blood cell count. Although the echocardiogram was pending, the ID consultant recommended that intravenous antibiotics be discontinued and that she was safe to be discharged home with follow-up blood cultures in 1 week. Later that day, the echocardiogram found a thickened aortic valve with an increased density that suggested possible vegetation.
On the morning of hospital day 3, DB had a Tmax (time to maximum plasma concentration) of 38.8 C overnight. The repeat blood cultures drawn on admission showed no growth to date. Dr. Hospitalist stopped the intravenous antibiotics and discharged DB to home. Unknown to Dr. Hospitalist at the time, the original cultures drawn at the PCP’s office were finalized as Staphylococcus lugdunensis.
One week later, DB followed up with her PCP. She continued to have fevers, myalgias, and fatigue. Blood cultures were obtained and reported the following day as 2 out of 2 positive for S. lugdunensis. DB once again returned to the hospital and was started on intravenous antibiotics. Two days into her second hospital stay, DB complained of feeling hot. She sat up in the bed and then went unconscious. After almost 2 hours of resuscitation, DB was pronounced dead. An autopsy was performed and identified the cause of death as bacterial endocarditis (S. lugdunensis) with massive vegetations and aortic valve rupture.
Complaint
DB’s mother immediately brought a claim against Dr. Hospitalist and the ID consultant from the first hospital stay. The complaint alleged that DB was inappropriately discharged from the first hospitalization without ongoing intravenous antibiotic therapy. As a result, DB missed 8 days of antibiotic treatment allowing her untreated infection to irreversibly damage her heart. The complaint further alleged that this gap in treatment was the proximate cause of DB’s death.
Scientific principles
Staphylococcus lugdunensis is a coagulase-negative staphylococcus (CNS). Like other CNS, S. lugdunensis in humans ranges from a harmless skin commensal to a life-threatening pathogen (as with infective endocarditis). Unlike other CNS, however, S. lugdunensis can cause severe disease reminiscent of the virulent infections frequently attributable to S. aureus. S. lugdunensis endocarditis is an aggressive infection that affects native valves with greater frequency than prosthetic valves in contrast to other CNS. S. lugdunensis native valve endocarditis is typically community acquired and is associated with a high rate of complications and death.
Complaint rebuttal and discussion
The only defense that Dr. Hospitalist offered was that he relied on his subspecialty consultant. Dr. Hospitalist argued that he was a generalist and not an expert in endocarditis or CNS. As a result, he followed the recommendations of the ID consultant and he further argued that he had the right to do so.
The plaintiff countered essentially countered with "Would you jump off the roof of a building just because someone told you to?" argument. In this case, the positive blood cultures, the history of aortic valve repair, and the suggestive echocardiogram were indisputable facts. Discovery in this case confirmed that Dr. Hospitalist never spoke with the ID consultant at any point during the first hospital stay.
Plaintiff experts argued that Dr. Hospitalist was a board-certified internist practicing hospital-based internal medicine and as such, he had or should have had the requisite knowledge, skills, and attitudes to evaluate, diagnose, and treat endocarditis. In this case, it appeared that Dr. Hospitalist "blindly" followed the recommendations of the ID consultant without considering all the evidence at hand. Plaintiff experts argued that in this situation, the standard of care required that Dr. Hospitalist question the plan of care outlined by his consultant. Had he done so, it is likely that both Dr. Hospitalist and the infectious disease consultant would have learned that the original blood cultures grew S. lugdunensis and antibiotics would never have been discontinued.
Conclusion
As the attending physicians of record, hospitalists carry the ultimate responsibility for the discharge decision. It is common to ask subspecialty consultants their opinion regarding stability for discharge and/or the need for ongoing hospital therapy. Yet, it is important for all hospitalists to remember that the consultant recommendations are just opinions that must be weighed against all the other evidence currently available. It is also helpful to have and document verbal discussions with consultants when discharge decisions are being made (and partially relied upon) with their subspecialty input.
The ID consultant in this case settled almost immediately with DB’s family. Dr. Hospitalist defended himself a little longer, but ultimately settled this case with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
DB was a 20-year-old woman who presented to her primary care physician (PCP) with fever and myalgias. Her past medical history was significant for open heart surgery 3 years earlier for ventricular myxoma and aortic valve repair. Her temperature in the office was 39.1 C. Her examination was otherwise unremarkable. An influenza swab was negative. Cultures were drawn and DB was sent home with instructions to increase her fluids and use acetaminophen and ibuprofen as needed. Two days later, 2 out of 2 preliminary blood cultures were reported positive for coagulase-negative, gram positive cocci in clusters. DB was referred to the hospital where she was admitted by Dr. Hospitalist.
Dr. Hospitalist performed a history and physical and noted an impression of sepsis from subacute bacterial endocarditis. He initiated intravenous vancomycin and ceftriaxone, repeated blood cultures, ordered an echocardiogram, and obtained an infectious disease (ID) consult. On hospital day 2, the ID consultant documented that DB had positive blood cultures for coagulase-negative staphylococci but no true evidence of sepsis. She was noted to be afebrile with a normal white blood cell count. Although the echocardiogram was pending, the ID consultant recommended that intravenous antibiotics be discontinued and that she was safe to be discharged home with follow-up blood cultures in 1 week. Later that day, the echocardiogram found a thickened aortic valve with an increased density that suggested possible vegetation.
On the morning of hospital day 3, DB had a Tmax (time to maximum plasma concentration) of 38.8 C overnight. The repeat blood cultures drawn on admission showed no growth to date. Dr. Hospitalist stopped the intravenous antibiotics and discharged DB to home. Unknown to Dr. Hospitalist at the time, the original cultures drawn at the PCP’s office were finalized as Staphylococcus lugdunensis.
One week later, DB followed up with her PCP. She continued to have fevers, myalgias, and fatigue. Blood cultures were obtained and reported the following day as 2 out of 2 positive for S. lugdunensis. DB once again returned to the hospital and was started on intravenous antibiotics. Two days into her second hospital stay, DB complained of feeling hot. She sat up in the bed and then went unconscious. After almost 2 hours of resuscitation, DB was pronounced dead. An autopsy was performed and identified the cause of death as bacterial endocarditis (S. lugdunensis) with massive vegetations and aortic valve rupture.
Complaint
DB’s mother immediately brought a claim against Dr. Hospitalist and the ID consultant from the first hospital stay. The complaint alleged that DB was inappropriately discharged from the first hospitalization without ongoing intravenous antibiotic therapy. As a result, DB missed 8 days of antibiotic treatment allowing her untreated infection to irreversibly damage her heart. The complaint further alleged that this gap in treatment was the proximate cause of DB’s death.
Scientific principles
Staphylococcus lugdunensis is a coagulase-negative staphylococcus (CNS). Like other CNS, S. lugdunensis in humans ranges from a harmless skin commensal to a life-threatening pathogen (as with infective endocarditis). Unlike other CNS, however, S. lugdunensis can cause severe disease reminiscent of the virulent infections frequently attributable to S. aureus. S. lugdunensis endocarditis is an aggressive infection that affects native valves with greater frequency than prosthetic valves in contrast to other CNS. S. lugdunensis native valve endocarditis is typically community acquired and is associated with a high rate of complications and death.
Complaint rebuttal and discussion
The only defense that Dr. Hospitalist offered was that he relied on his subspecialty consultant. Dr. Hospitalist argued that he was a generalist and not an expert in endocarditis or CNS. As a result, he followed the recommendations of the ID consultant and he further argued that he had the right to do so.
The plaintiff countered essentially countered with "Would you jump off the roof of a building just because someone told you to?" argument. In this case, the positive blood cultures, the history of aortic valve repair, and the suggestive echocardiogram were indisputable facts. Discovery in this case confirmed that Dr. Hospitalist never spoke with the ID consultant at any point during the first hospital stay.
Plaintiff experts argued that Dr. Hospitalist was a board-certified internist practicing hospital-based internal medicine and as such, he had or should have had the requisite knowledge, skills, and attitudes to evaluate, diagnose, and treat endocarditis. In this case, it appeared that Dr. Hospitalist "blindly" followed the recommendations of the ID consultant without considering all the evidence at hand. Plaintiff experts argued that in this situation, the standard of care required that Dr. Hospitalist question the plan of care outlined by his consultant. Had he done so, it is likely that both Dr. Hospitalist and the infectious disease consultant would have learned that the original blood cultures grew S. lugdunensis and antibiotics would never have been discontinued.
Conclusion
As the attending physicians of record, hospitalists carry the ultimate responsibility for the discharge decision. It is common to ask subspecialty consultants their opinion regarding stability for discharge and/or the need for ongoing hospital therapy. Yet, it is important for all hospitalists to remember that the consultant recommendations are just opinions that must be weighed against all the other evidence currently available. It is also helpful to have and document verbal discussions with consultants when discharge decisions are being made (and partially relied upon) with their subspecialty input.
The ID consultant in this case settled almost immediately with DB’s family. Dr. Hospitalist defended himself a little longer, but ultimately settled this case with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
A paralyzed patient with two stories in the chart
Story
BF was a 44-year-old man with essential hypertension who was admitted to the hospital with intractable low back pain and urinary retention. No antecedent trauma was reported. He was seen in the ED three times in the preceding week for similar complaints. In each case, he had relief with intravenous analgesia, but the symptoms quickly returned.
Prior to his admission he had lumbar radiography as well as an MRI of the lumbar spine. Plain films were unremarkable, but the MRI showed a potentially significant L4-L5 foraminal stenosis on the left and L5-S1 foraminal stenosis on the right. Neurosurgery (NS) reviewed the MRI and did not feel operative intervention was indicated. A bladder catheter was inserted in the ED for urinary retention. He was subsequently admitted to Dr. Hospitalist, who initiated medical treatment. Dr. Hospitalist’s admission impression:
"44 yo with low back pain and sciatica from foraminal stenosis. There is no neurologic compromise. The urinary retention is probably due to narcotic effects. This was discussed with neurosurgery from the ED. The patient will be admitted for observation, pain control, and physical therapy."
The following day, Dr. Hospitalist noted that BF’s pain was controlled but that he had weakness in his left foot. Dr. Hospitalist contacted NS and was reassured that if BF’s symptoms were improving with respect to pain, numbness, and/or weakness, then neurologic compromise was unlikely. Over the next 2 days, Dr. Hospitalist documented subjective improvement in BF’s pain with 4+/5 left lower extremity (LLE) strength.
On hospital day 4, BF was unable to move his legs. Dr. Hospitalist transferred BF later that day to a nearby hospital with on-site NS. An MRI performed there demonstrated a large T9-L5 epidural abscess. Despite emergent neurosurgical decompression, BF remained permanently paralyzed below the umbilicus.
Complaint
BF was naturally distraught with his paralysis. He claimed that he told everyone that he had numbness and weakness in both his legs from the very start and that nobody did anything to help him until it was too late. Expert review of the medical record found the following entries on the day of admission:
RN day note: "Patient complains of bilateral LE numbness, weak plantar, and dorsiflexion of LLE."
Physical therapy note: "Bilateral leg paresthesias from the waist down; absent anterior tibialis motor function; quadriceps weakness on the left."
Occupational therapy note: "Patient has sensation symptoms that are not reported in chart from prior MD evaluation."
Despite daily documentation by Dr. Hospitalist that BF was improving, chart entries by the nursing staff and the therapists on day 2 suggested the opposite.
On day 3, Dr. Hospitalist acknowledged that the low back pain had been better until the previous night. However, the strength was unchanged, and he was "still a little bit numb." A physical therapy note written 1 hour after Dr. Hospitalist examined BF and charted 4+/5 strength reported "slideboard transfers required due to inability to stand."
Scientific principles
Spinal epidural abscess (SEA) requires prompt recognition and proper management to avoid potentially disastrous complications. The classical diagnostic triad consists of fever, spinal pain, and neurologic deficits. Untreated abscesses will cause symptoms that progress in a typical sequence: 1) back pain, which is often focal and severe, 2) root pain, described as "shooting" or "electric shocks" in the distribution of the affected nerve root, 3) motor weakness, sensory changes, and bladder or bowel dysfunction, and then 4) paralysis. Once paralysis develops, it may quickly become irreversible.
Complaint rebuttal and discussion
Defense experts reinforced that SEA was a rare diagnosis and that Dr. Hospitalist appropriately performed a comprehensive admission H+P with a review of all prior ED visits and radiographic studies, and further examined BF daily and discussed BF’s case with a neurosurgical specialist who provided reassurance that no serious spinal pathology existed. Dr. Hospitalist testified that BF’s exam was dependent on patient participation and, although at times inconsistent, it suggested gradual improvement in his condition. Dr. Hospitalist also testified that he was not fully aware of the RN and therapist impressions at the time, but he trusted his own evaluations as being most accurate.
Plaintiff experts had a hard time reconciling the two conflicting stories in the chart. Additional chart review revealed that on day 2, Dr. Hospitalist inexplicably ordered a CRP and ESR that were both elevated (14.5 mg/dL and 80 mm/hr, respectively) but were never mentioned in the progress notes – nor was the rationale for ordering the studies or an impression of the results. Dr. Hospitalist testified he had no memory of ordering the studies. Moreover, the discharge summary authored by Dr. Hospitalist prior to BF transfer was contradictory to his own progress note documentation:
Hospitalist note, day 2: "There is less pain, actually no pain. The numbness or lack of sensation is improved. The ability to move his left leg is also improved; however, it is still difficult to move it and not because of pain."
Discharge summary: "There were no unifying localizing findings to suggest spinal cord compromise, and much of his symptoms may be related to pain. ... there has been no real progress made in terms of controlling his pain."
Taking all the evidence in aggregate, the plaintiff experts were critical that Dr. Hospitalist seemed unaware of the full range of patient symptoms, the laboratory evidence for an inflammatory process, the reliance on a specialist who never examined the patient, and the inadvertent or intentional chart contradictions.
Conclusion
Charting is one of the four "Cs" in reducing medicolegal risk (charting, competence, compassion, and communication). In this case, the charting by Dr. Hospitalist appeared appropriate on the surface, but inadvertently or intentionally hid the entire clinical picture. The difference in documentation between hospitalist and the RN/therapy notes in this case seems hard to explain, but various health care providers may reasonably see and chart diverse findings and impressions. However, the conflicting documentation between several of Dr. Hospitalist’s own notes severely damaged his credibility.
This case was settled for an undisclosed amount in favor of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read earlier columns online at ehospitalistnews.com/Lessons.
Story
BF was a 44-year-old man with essential hypertension who was admitted to the hospital with intractable low back pain and urinary retention. No antecedent trauma was reported. He was seen in the ED three times in the preceding week for similar complaints. In each case, he had relief with intravenous analgesia, but the symptoms quickly returned.
Prior to his admission he had lumbar radiography as well as an MRI of the lumbar spine. Plain films were unremarkable, but the MRI showed a potentially significant L4-L5 foraminal stenosis on the left and L5-S1 foraminal stenosis on the right. Neurosurgery (NS) reviewed the MRI and did not feel operative intervention was indicated. A bladder catheter was inserted in the ED for urinary retention. He was subsequently admitted to Dr. Hospitalist, who initiated medical treatment. Dr. Hospitalist’s admission impression:
"44 yo with low back pain and sciatica from foraminal stenosis. There is no neurologic compromise. The urinary retention is probably due to narcotic effects. This was discussed with neurosurgery from the ED. The patient will be admitted for observation, pain control, and physical therapy."
The following day, Dr. Hospitalist noted that BF’s pain was controlled but that he had weakness in his left foot. Dr. Hospitalist contacted NS and was reassured that if BF’s symptoms were improving with respect to pain, numbness, and/or weakness, then neurologic compromise was unlikely. Over the next 2 days, Dr. Hospitalist documented subjective improvement in BF’s pain with 4+/5 left lower extremity (LLE) strength.
On hospital day 4, BF was unable to move his legs. Dr. Hospitalist transferred BF later that day to a nearby hospital with on-site NS. An MRI performed there demonstrated a large T9-L5 epidural abscess. Despite emergent neurosurgical decompression, BF remained permanently paralyzed below the umbilicus.
Complaint
BF was naturally distraught with his paralysis. He claimed that he told everyone that he had numbness and weakness in both his legs from the very start and that nobody did anything to help him until it was too late. Expert review of the medical record found the following entries on the day of admission:
RN day note: "Patient complains of bilateral LE numbness, weak plantar, and dorsiflexion of LLE."
Physical therapy note: "Bilateral leg paresthesias from the waist down; absent anterior tibialis motor function; quadriceps weakness on the left."
Occupational therapy note: "Patient has sensation symptoms that are not reported in chart from prior MD evaluation."
Despite daily documentation by Dr. Hospitalist that BF was improving, chart entries by the nursing staff and the therapists on day 2 suggested the opposite.
On day 3, Dr. Hospitalist acknowledged that the low back pain had been better until the previous night. However, the strength was unchanged, and he was "still a little bit numb." A physical therapy note written 1 hour after Dr. Hospitalist examined BF and charted 4+/5 strength reported "slideboard transfers required due to inability to stand."
Scientific principles
Spinal epidural abscess (SEA) requires prompt recognition and proper management to avoid potentially disastrous complications. The classical diagnostic triad consists of fever, spinal pain, and neurologic deficits. Untreated abscesses will cause symptoms that progress in a typical sequence: 1) back pain, which is often focal and severe, 2) root pain, described as "shooting" or "electric shocks" in the distribution of the affected nerve root, 3) motor weakness, sensory changes, and bladder or bowel dysfunction, and then 4) paralysis. Once paralysis develops, it may quickly become irreversible.
Complaint rebuttal and discussion
Defense experts reinforced that SEA was a rare diagnosis and that Dr. Hospitalist appropriately performed a comprehensive admission H+P with a review of all prior ED visits and radiographic studies, and further examined BF daily and discussed BF’s case with a neurosurgical specialist who provided reassurance that no serious spinal pathology existed. Dr. Hospitalist testified that BF’s exam was dependent on patient participation and, although at times inconsistent, it suggested gradual improvement in his condition. Dr. Hospitalist also testified that he was not fully aware of the RN and therapist impressions at the time, but he trusted his own evaluations as being most accurate.
Plaintiff experts had a hard time reconciling the two conflicting stories in the chart. Additional chart review revealed that on day 2, Dr. Hospitalist inexplicably ordered a CRP and ESR that were both elevated (14.5 mg/dL and 80 mm/hr, respectively) but were never mentioned in the progress notes – nor was the rationale for ordering the studies or an impression of the results. Dr. Hospitalist testified he had no memory of ordering the studies. Moreover, the discharge summary authored by Dr. Hospitalist prior to BF transfer was contradictory to his own progress note documentation:
Hospitalist note, day 2: "There is less pain, actually no pain. The numbness or lack of sensation is improved. The ability to move his left leg is also improved; however, it is still difficult to move it and not because of pain."
Discharge summary: "There were no unifying localizing findings to suggest spinal cord compromise, and much of his symptoms may be related to pain. ... there has been no real progress made in terms of controlling his pain."
Taking all the evidence in aggregate, the plaintiff experts were critical that Dr. Hospitalist seemed unaware of the full range of patient symptoms, the laboratory evidence for an inflammatory process, the reliance on a specialist who never examined the patient, and the inadvertent or intentional chart contradictions.
Conclusion
Charting is one of the four "Cs" in reducing medicolegal risk (charting, competence, compassion, and communication). In this case, the charting by Dr. Hospitalist appeared appropriate on the surface, but inadvertently or intentionally hid the entire clinical picture. The difference in documentation between hospitalist and the RN/therapy notes in this case seems hard to explain, but various health care providers may reasonably see and chart diverse findings and impressions. However, the conflicting documentation between several of Dr. Hospitalist’s own notes severely damaged his credibility.
This case was settled for an undisclosed amount in favor of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read earlier columns online at ehospitalistnews.com/Lessons.
Story
BF was a 44-year-old man with essential hypertension who was admitted to the hospital with intractable low back pain and urinary retention. No antecedent trauma was reported. He was seen in the ED three times in the preceding week for similar complaints. In each case, he had relief with intravenous analgesia, but the symptoms quickly returned.
Prior to his admission he had lumbar radiography as well as an MRI of the lumbar spine. Plain films were unremarkable, but the MRI showed a potentially significant L4-L5 foraminal stenosis on the left and L5-S1 foraminal stenosis on the right. Neurosurgery (NS) reviewed the MRI and did not feel operative intervention was indicated. A bladder catheter was inserted in the ED for urinary retention. He was subsequently admitted to Dr. Hospitalist, who initiated medical treatment. Dr. Hospitalist’s admission impression:
"44 yo with low back pain and sciatica from foraminal stenosis. There is no neurologic compromise. The urinary retention is probably due to narcotic effects. This was discussed with neurosurgery from the ED. The patient will be admitted for observation, pain control, and physical therapy."
The following day, Dr. Hospitalist noted that BF’s pain was controlled but that he had weakness in his left foot. Dr. Hospitalist contacted NS and was reassured that if BF’s symptoms were improving with respect to pain, numbness, and/or weakness, then neurologic compromise was unlikely. Over the next 2 days, Dr. Hospitalist documented subjective improvement in BF’s pain with 4+/5 left lower extremity (LLE) strength.
On hospital day 4, BF was unable to move his legs. Dr. Hospitalist transferred BF later that day to a nearby hospital with on-site NS. An MRI performed there demonstrated a large T9-L5 epidural abscess. Despite emergent neurosurgical decompression, BF remained permanently paralyzed below the umbilicus.
Complaint
BF was naturally distraught with his paralysis. He claimed that he told everyone that he had numbness and weakness in both his legs from the very start and that nobody did anything to help him until it was too late. Expert review of the medical record found the following entries on the day of admission:
RN day note: "Patient complains of bilateral LE numbness, weak plantar, and dorsiflexion of LLE."
Physical therapy note: "Bilateral leg paresthesias from the waist down; absent anterior tibialis motor function; quadriceps weakness on the left."
Occupational therapy note: "Patient has sensation symptoms that are not reported in chart from prior MD evaluation."
Despite daily documentation by Dr. Hospitalist that BF was improving, chart entries by the nursing staff and the therapists on day 2 suggested the opposite.
On day 3, Dr. Hospitalist acknowledged that the low back pain had been better until the previous night. However, the strength was unchanged, and he was "still a little bit numb." A physical therapy note written 1 hour after Dr. Hospitalist examined BF and charted 4+/5 strength reported "slideboard transfers required due to inability to stand."
Scientific principles
Spinal epidural abscess (SEA) requires prompt recognition and proper management to avoid potentially disastrous complications. The classical diagnostic triad consists of fever, spinal pain, and neurologic deficits. Untreated abscesses will cause symptoms that progress in a typical sequence: 1) back pain, which is often focal and severe, 2) root pain, described as "shooting" or "electric shocks" in the distribution of the affected nerve root, 3) motor weakness, sensory changes, and bladder or bowel dysfunction, and then 4) paralysis. Once paralysis develops, it may quickly become irreversible.
Complaint rebuttal and discussion
Defense experts reinforced that SEA was a rare diagnosis and that Dr. Hospitalist appropriately performed a comprehensive admission H+P with a review of all prior ED visits and radiographic studies, and further examined BF daily and discussed BF’s case with a neurosurgical specialist who provided reassurance that no serious spinal pathology existed. Dr. Hospitalist testified that BF’s exam was dependent on patient participation and, although at times inconsistent, it suggested gradual improvement in his condition. Dr. Hospitalist also testified that he was not fully aware of the RN and therapist impressions at the time, but he trusted his own evaluations as being most accurate.
Plaintiff experts had a hard time reconciling the two conflicting stories in the chart. Additional chart review revealed that on day 2, Dr. Hospitalist inexplicably ordered a CRP and ESR that were both elevated (14.5 mg/dL and 80 mm/hr, respectively) but were never mentioned in the progress notes – nor was the rationale for ordering the studies or an impression of the results. Dr. Hospitalist testified he had no memory of ordering the studies. Moreover, the discharge summary authored by Dr. Hospitalist prior to BF transfer was contradictory to his own progress note documentation:
Hospitalist note, day 2: "There is less pain, actually no pain. The numbness or lack of sensation is improved. The ability to move his left leg is also improved; however, it is still difficult to move it and not because of pain."
Discharge summary: "There were no unifying localizing findings to suggest spinal cord compromise, and much of his symptoms may be related to pain. ... there has been no real progress made in terms of controlling his pain."
Taking all the evidence in aggregate, the plaintiff experts were critical that Dr. Hospitalist seemed unaware of the full range of patient symptoms, the laboratory evidence for an inflammatory process, the reliance on a specialist who never examined the patient, and the inadvertent or intentional chart contradictions.
Conclusion
Charting is one of the four "Cs" in reducing medicolegal risk (charting, competence, compassion, and communication). In this case, the charting by Dr. Hospitalist appeared appropriate on the surface, but inadvertently or intentionally hid the entire clinical picture. The difference in documentation between hospitalist and the RN/therapy notes in this case seems hard to explain, but various health care providers may reasonably see and chart diverse findings and impressions. However, the conflicting documentation between several of Dr. Hospitalist’s own notes severely damaged his credibility.
This case was settled for an undisclosed amount in favor of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read earlier columns online at ehospitalistnews.com/Lessons.
Medicolegal Lessons: A question of duty
Story
ML was an 83-year-old woman who presented from her assisted-living facility to her local emergency room with abdominal pain.
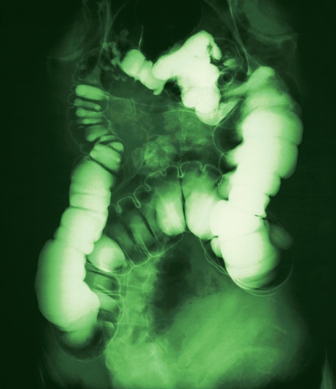
She described acute-onset epigastric pain within minutes of her evening meal. The pain was rated 5 out of 10 and was associated with some nausea but no emesis. ML had a past medical history of irritable bowel symptoms along with diverticulosis, but she was otherwise healthy and took no regular medications except for occasional loperamide. Her CBC, amylase, lipase, and chemistry panels were normal. CT scan of the abdomen showed mildly dilated loops of small bowel.
ML was admitted to the hospital by her family physician, who consulted a gastroenterologist the following morning. The gastroenterologist concluded that ML was most likely suffering from food intolerance and recommended bowel rest and observation.
ML continued to have the pain and was unable to advance her diet. On hospital day 2, the GI consultant noted that ML’s abdomen was soft and nondistended, but he ordered an acute abdominal series and requested to be called with the results. The study was not completed until 5:30 p.m. Later that evening during a routine chart check, ML’s nurse noted that the acute abdominal series had been completed, but not read. She paged the hospitalist on call to review the film so that she could contact the GI consultant pursuant to his order.
Dr. Hospitalist reviewed the film and called the nurse back to report that the film showed no free air but the colon was dilated. The nurse subsequently called the GI consultant and relayed the information. No new orders were received.
At 7 a.m. on hospital day 3, ML developed mental status changes. Her abdomen was now noted to be distended with rigidity. ML was evaluated by her family physician and the GI consultant.
A surgical consult was obtained along with further imaging, which confirmed a small bowel obstruction (SBO) with massively dilated small bowel. Morning labs also showed acute kidney injury. Formal radiology review of the abdominal series looked at by Dr. Hospitalist established the presence of significant small bowel dilatation highly concerning for SBO. ML was transferred to a larger hospital where she eventually underwent an exploratory laparotomy for perforated bowel. Following a tumultuous postoperative course including dialysis, ML expired 1 month later.
Complaint
ML’s daughter was a pediatrician at a major teaching institution nearby. She was frustrated that the original CT showed dilated small bowel and that the conclusion of her treating doctors was that her mother was suffering from "food intolerance." Together with her father, they filed suit against the hospital, the GI consultant, and Dr. Hospitalist.
ML’s family alleged that ML had small bowel obstruction from the start and should have had surgical involvement soon enough to intervene before she ultimately perforated her bowel. Surgical repair prior to perforation would have significantly changed ML’s outcome.
They further alleged that Dr. Hospitalist was negligent in her review of the abdominal radiographs and she had a duty to see and examine ML, communicate directly with the GI consultant, and obtain a STAT surgical consult.
Scientific principles
Small bowel obstruction occurs when the normal flow of intestinal contents is interrupted, and it is usually confirmed by plain abdominal radiography.
The most frequent causes are postoperative adhesions and hernias, which cause extrinsic compression of the intestine. Obstruction leads to dilation of the stomach and small intestine proximal to the blockage, while distal to the blockage the bowel will decompress as luminal contents are passed. Symptoms include obstipation, nausea, vomiting, and abdominal pain. As the small bowel dilates, its blood flow can be compromised, leading to strangulation and sepsis.
Unfortunately, there is no reliable sign or symptom differentiating patients with strangulation or impending strangulation from those in whom surgery will not be necessary.
Complaint rebuttal and discussion
For the night in question, Dr. Hospitalist asserted that she had two roles and only one of them involved ML.
First, Dr. Hospitalist was responsible for admissions and cross-coverage for her own group’s patients at night. ML was not a patient of Dr. Hospitalist or her group. ML was being cared for by her own family physician and his practice group 24/7.
Second, Dr. Hospitalist was the hospital’s overnight "house doctor" for codes, IV access, radiology "wet reads," and other emergencies. It was in this capacity that Dr. Hospitalist was contacted. Dr. Hospitalist was not a radiologist. As a house doctor, Dr. Hospitalist would be expected to look for serious and life-threatening findings and to rule out the presence of free air. Dr. Hospitalist asserted that she was never asked to see ML by the attending physician or even by the nurse.
The family argued that Dr. Hospitalist had a duty to question the nurse regarding ML’s condition and, because of the evidence for obstruction on the film, see ML for an assessment. The family argued that Dr. Hospitalist’s misinterpretation of the film (i.e., colon dilatation in the face of obvious small bowel dilatation) represented gross incompetence.
Dr. Hospitalist testified that she had no memory of ML, this case, or what she may or may not have told the nurse that night. ML’s medical record confirms that Dr. Hospitalist wrote no orders or charted any notes on her. The only documentation of Dr. Hospitalist’s "wet read" was in ML’s nursing notes.
The GI consultant testified that he had no memory of his call from the nurse with the radiograph results. The nurse testified that she wouldn’t have written "colon dilatation" if Dr. Hospitalist had told her it was small bowel.
Conclusion
The "house doc" role typically encompasses a limited scope of responsibility. But all physicians carry a professional duty to the patients that we become involved with.
By performing a "wet read" on a film of ML, Dr. Hospitalist established a doctor-patient relationship. It would have been prudent for Dr. Hospitalist to record her film interpretation herself (thus creating an opportunity for brief chart review), and to call the GI consultant with the information instead of relying on the nurse. A 1-minute conversation between Dr. Hospitalist and the GI consultant may have led to further intervention by either party.
Ultimately this case was resolved for an undisclosed amount. In the "house doc" role, Dr. Hospitalist was functioning as an employee of the hospital (despite being an independent contractor), and there were hospital care issues independent of Dr. Hospitalist. However, Dr. Hospitalist could have avoided her role in this suit with better documentation and communication.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. Read earlier columns online at ehospitalistnews.com/Lessons.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Story
ML was an 83-year-old woman who presented from her assisted-living facility to her local emergency room with abdominal pain.
She described acute-onset epigastric pain within minutes of her evening meal. The pain was rated 5 out of 10 and was associated with some nausea but no emesis. ML had a past medical history of irritable bowel symptoms along with diverticulosis, but she was otherwise healthy and took no regular medications except for occasional loperamide. Her CBC, amylase, lipase, and chemistry panels were normal. CT scan of the abdomen showed mildly dilated loops of small bowel.
ML was admitted to the hospital by her family physician, who consulted a gastroenterologist the following morning. The gastroenterologist concluded that ML was most likely suffering from food intolerance and recommended bowel rest and observation.
ML continued to have the pain and was unable to advance her diet. On hospital day 2, the GI consultant noted that ML’s abdomen was soft and nondistended, but he ordered an acute abdominal series and requested to be called with the results. The study was not completed until 5:30 p.m. Later that evening during a routine chart check, ML’s nurse noted that the acute abdominal series had been completed, but not read. She paged the hospitalist on call to review the film so that she could contact the GI consultant pursuant to his order.
Dr. Hospitalist reviewed the film and called the nurse back to report that the film showed no free air but the colon was dilated. The nurse subsequently called the GI consultant and relayed the information. No new orders were received.
At 7 a.m. on hospital day 3, ML developed mental status changes. Her abdomen was now noted to be distended with rigidity. ML was evaluated by her family physician and the GI consultant.
A surgical consult was obtained along with further imaging, which confirmed a small bowel obstruction (SBO) with massively dilated small bowel. Morning labs also showed acute kidney injury. Formal radiology review of the abdominal series looked at by Dr. Hospitalist established the presence of significant small bowel dilatation highly concerning for SBO. ML was transferred to a larger hospital where she eventually underwent an exploratory laparotomy for perforated bowel. Following a tumultuous postoperative course including dialysis, ML expired 1 month later.
Complaint
ML’s daughter was a pediatrician at a major teaching institution nearby. She was frustrated that the original CT showed dilated small bowel and that the conclusion of her treating doctors was that her mother was suffering from "food intolerance." Together with her father, they filed suit against the hospital, the GI consultant, and Dr. Hospitalist.
ML’s family alleged that ML had small bowel obstruction from the start and should have had surgical involvement soon enough to intervene before she ultimately perforated her bowel. Surgical repair prior to perforation would have significantly changed ML’s outcome.
They further alleged that Dr. Hospitalist was negligent in her review of the abdominal radiographs and she had a duty to see and examine ML, communicate directly with the GI consultant, and obtain a STAT surgical consult.
Scientific principles
Small bowel obstruction occurs when the normal flow of intestinal contents is interrupted, and it is usually confirmed by plain abdominal radiography.
The most frequent causes are postoperative adhesions and hernias, which cause extrinsic compression of the intestine. Obstruction leads to dilation of the stomach and small intestine proximal to the blockage, while distal to the blockage the bowel will decompress as luminal contents are passed. Symptoms include obstipation, nausea, vomiting, and abdominal pain. As the small bowel dilates, its blood flow can be compromised, leading to strangulation and sepsis.
Unfortunately, there is no reliable sign or symptom differentiating patients with strangulation or impending strangulation from those in whom surgery will not be necessary.
Complaint rebuttal and discussion
For the night in question, Dr. Hospitalist asserted that she had two roles and only one of them involved ML.
First, Dr. Hospitalist was responsible for admissions and cross-coverage for her own group’s patients at night. ML was not a patient of Dr. Hospitalist or her group. ML was being cared for by her own family physician and his practice group 24/7.
Second, Dr. Hospitalist was the hospital’s overnight "house doctor" for codes, IV access, radiology "wet reads," and other emergencies. It was in this capacity that Dr. Hospitalist was contacted. Dr. Hospitalist was not a radiologist. As a house doctor, Dr. Hospitalist would be expected to look for serious and life-threatening findings and to rule out the presence of free air. Dr. Hospitalist asserted that she was never asked to see ML by the attending physician or even by the nurse.
The family argued that Dr. Hospitalist had a duty to question the nurse regarding ML’s condition and, because of the evidence for obstruction on the film, see ML for an assessment. The family argued that Dr. Hospitalist’s misinterpretation of the film (i.e., colon dilatation in the face of obvious small bowel dilatation) represented gross incompetence.
Dr. Hospitalist testified that she had no memory of ML, this case, or what she may or may not have told the nurse that night. ML’s medical record confirms that Dr. Hospitalist wrote no orders or charted any notes on her. The only documentation of Dr. Hospitalist’s "wet read" was in ML’s nursing notes.
The GI consultant testified that he had no memory of his call from the nurse with the radiograph results. The nurse testified that she wouldn’t have written "colon dilatation" if Dr. Hospitalist had told her it was small bowel.
Conclusion
The "house doc" role typically encompasses a limited scope of responsibility. But all physicians carry a professional duty to the patients that we become involved with.
By performing a "wet read" on a film of ML, Dr. Hospitalist established a doctor-patient relationship. It would have been prudent for Dr. Hospitalist to record her film interpretation herself (thus creating an opportunity for brief chart review), and to call the GI consultant with the information instead of relying on the nurse. A 1-minute conversation between Dr. Hospitalist and the GI consultant may have led to further intervention by either party.
Ultimately this case was resolved for an undisclosed amount. In the "house doc" role, Dr. Hospitalist was functioning as an employee of the hospital (despite being an independent contractor), and there were hospital care issues independent of Dr. Hospitalist. However, Dr. Hospitalist could have avoided her role in this suit with better documentation and communication.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. Read earlier columns online at ehospitalistnews.com/Lessons.
Story
ML was an 83-year-old woman who presented from her assisted-living facility to her local emergency room with abdominal pain.
She described acute-onset epigastric pain within minutes of her evening meal. The pain was rated 5 out of 10 and was associated with some nausea but no emesis. ML had a past medical history of irritable bowel symptoms along with diverticulosis, but she was otherwise healthy and took no regular medications except for occasional loperamide. Her CBC, amylase, lipase, and chemistry panels were normal. CT scan of the abdomen showed mildly dilated loops of small bowel.
ML was admitted to the hospital by her family physician, who consulted a gastroenterologist the following morning. The gastroenterologist concluded that ML was most likely suffering from food intolerance and recommended bowel rest and observation.
ML continued to have the pain and was unable to advance her diet. On hospital day 2, the GI consultant noted that ML’s abdomen was soft and nondistended, but he ordered an acute abdominal series and requested to be called with the results. The study was not completed until 5:30 p.m. Later that evening during a routine chart check, ML’s nurse noted that the acute abdominal series had been completed, but not read. She paged the hospitalist on call to review the film so that she could contact the GI consultant pursuant to his order.
Dr. Hospitalist reviewed the film and called the nurse back to report that the film showed no free air but the colon was dilated. The nurse subsequently called the GI consultant and relayed the information. No new orders were received.
At 7 a.m. on hospital day 3, ML developed mental status changes. Her abdomen was now noted to be distended with rigidity. ML was evaluated by her family physician and the GI consultant.
A surgical consult was obtained along with further imaging, which confirmed a small bowel obstruction (SBO) with massively dilated small bowel. Morning labs also showed acute kidney injury. Formal radiology review of the abdominal series looked at by Dr. Hospitalist established the presence of significant small bowel dilatation highly concerning for SBO. ML was transferred to a larger hospital where she eventually underwent an exploratory laparotomy for perforated bowel. Following a tumultuous postoperative course including dialysis, ML expired 1 month later.
Complaint
ML’s daughter was a pediatrician at a major teaching institution nearby. She was frustrated that the original CT showed dilated small bowel and that the conclusion of her treating doctors was that her mother was suffering from "food intolerance." Together with her father, they filed suit against the hospital, the GI consultant, and Dr. Hospitalist.
ML’s family alleged that ML had small bowel obstruction from the start and should have had surgical involvement soon enough to intervene before she ultimately perforated her bowel. Surgical repair prior to perforation would have significantly changed ML’s outcome.
They further alleged that Dr. Hospitalist was negligent in her review of the abdominal radiographs and she had a duty to see and examine ML, communicate directly with the GI consultant, and obtain a STAT surgical consult.
Scientific principles
Small bowel obstruction occurs when the normal flow of intestinal contents is interrupted, and it is usually confirmed by plain abdominal radiography.
The most frequent causes are postoperative adhesions and hernias, which cause extrinsic compression of the intestine. Obstruction leads to dilation of the stomach and small intestine proximal to the blockage, while distal to the blockage the bowel will decompress as luminal contents are passed. Symptoms include obstipation, nausea, vomiting, and abdominal pain. As the small bowel dilates, its blood flow can be compromised, leading to strangulation and sepsis.
Unfortunately, there is no reliable sign or symptom differentiating patients with strangulation or impending strangulation from those in whom surgery will not be necessary.
Complaint rebuttal and discussion
For the night in question, Dr. Hospitalist asserted that she had two roles and only one of them involved ML.
First, Dr. Hospitalist was responsible for admissions and cross-coverage for her own group’s patients at night. ML was not a patient of Dr. Hospitalist or her group. ML was being cared for by her own family physician and his practice group 24/7.
Second, Dr. Hospitalist was the hospital’s overnight "house doctor" for codes, IV access, radiology "wet reads," and other emergencies. It was in this capacity that Dr. Hospitalist was contacted. Dr. Hospitalist was not a radiologist. As a house doctor, Dr. Hospitalist would be expected to look for serious and life-threatening findings and to rule out the presence of free air. Dr. Hospitalist asserted that she was never asked to see ML by the attending physician or even by the nurse.
The family argued that Dr. Hospitalist had a duty to question the nurse regarding ML’s condition and, because of the evidence for obstruction on the film, see ML for an assessment. The family argued that Dr. Hospitalist’s misinterpretation of the film (i.e., colon dilatation in the face of obvious small bowel dilatation) represented gross incompetence.
Dr. Hospitalist testified that she had no memory of ML, this case, or what she may or may not have told the nurse that night. ML’s medical record confirms that Dr. Hospitalist wrote no orders or charted any notes on her. The only documentation of Dr. Hospitalist’s "wet read" was in ML’s nursing notes.
The GI consultant testified that he had no memory of his call from the nurse with the radiograph results. The nurse testified that she wouldn’t have written "colon dilatation" if Dr. Hospitalist had told her it was small bowel.
Conclusion
The "house doc" role typically encompasses a limited scope of responsibility. But all physicians carry a professional duty to the patients that we become involved with.
By performing a "wet read" on a film of ML, Dr. Hospitalist established a doctor-patient relationship. It would have been prudent for Dr. Hospitalist to record her film interpretation herself (thus creating an opportunity for brief chart review), and to call the GI consultant with the information instead of relying on the nurse. A 1-minute conversation between Dr. Hospitalist and the GI consultant may have led to further intervention by either party.
Ultimately this case was resolved for an undisclosed amount. In the "house doc" role, Dr. Hospitalist was functioning as an employee of the hospital (despite being an independent contractor), and there were hospital care issues independent of Dr. Hospitalist. However, Dr. Hospitalist could have avoided her role in this suit with better documentation and communication.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. Read earlier columns online at ehospitalistnews.com/Lessons.
VTE and a debatable dose
Mr. SS was a 48-year-old man who presented to the emergency department with complaints of right calf and ankle swelling for 1 day associated with mild shortness of breath. Lower extremity ultrasound quickly confirmed an acute right femoral and popliteal deep vein thrombosis. CT angiogram of the chest was negative for pulmonary embolus (PE). Two weeks earlier, Mr. SS had suffered a traumatic right intertrochanteric hip fracture when he fell off a ladder at home. At that time, he underwent open reduction and internal fixation of the right hip without complication. He was discharged home on warfarin for venous thromboembolism (VTE) prophylaxis. At the time of his return to the hospital, his INR was 1.4 and his current level of activity was touch toe weight-bearing of the right leg.
The ED physician paged the hospitalist on call, who was already at home for the evening. Following a telephone discussion, Mr. SS was given 7.5 mg of subcutaneous fondaparinux (Arixtra) in the ED. Mr. SS was then transferred up to the regular nursing floor and admitted by a house doctor employed by the hospital. The house doctor continued the fondaparinux at a dose of 7.5mg daily.
At approximately 10 a.m. the following day, Mr. SS was up in the bathroom. He became acutely short of breath and called out for help. Before he could return to bed, he was noted to be ashen in appearance, and he lost consciousness along with his pulse and respirations. A code blue was called, but despite more than an hour of resuscitation, Mr. SS expired. An autopsy was performed and confirmed a large saddle pulmonary embolism as the cause of death. The hospitalist on call never saw Mr. SS before he died.
Complaint
Mr. SS was an English professor at the local university. He left behind a wife and four children. A relation in the medical field reviewed the records and discovered that Mr. SS only received 7.5 mg of fondaparinux despite the fact that Mr. SS weighed more than 100 kg (265 pounds). The Food and Drug Administration–approved dose of Arixtra for the treatment of acute venous thromboembolism is based on tertile of weight (5 mg if less than 50 kg; 7.5 mg if between 50-100 kg; and 10 mg if more than 100 kg). The complaint alleged that Mr. SS was underdosed and therefore needlessly developed a pulmonary embolism. Had Mr. SS received the FDA-approved dose of fondaparinux based on his weight, he would be alive and well today.
The complaint was filed against the ED physician, the hospitalist on call, and the house doctor.
Scientific principles
Outcome studies confirm that the vast majority of patients (more than 95%) who receive adequate anticoagulation in the setting of acute venous thromboembolism (DVT/PE) will be alive at discharge, 30 days, and at 1 year. In fact, of all the variables possibly associated with VTE recurrence, the only one demonstrated by logistic regression to be statistically significant with respect to VTE recurrence is the failure to achieve and maintain adequate anticoagulation. Properly conducted phase II dose ranging studies with Arixtra (REMBRANDT) ultimately led to the tertile weight-based dosing regimen that was studied in the phase III trial (MATISSE) that led to Arixtra’s FDA approval and the recommendations for dosing in the Arixtra package insert.
Complaint rebuttal and discussion
The defense argued that the dosing recommendations in the Arixtra package insert were guidelines and not in and of themselves the standard of care. Mr. SS did not have a normal INR on presentation and the defense argued it was reasonable clinical judgment on behalf of the providers involved to use that dose that best balanced efficacy and safety. The defense further argued that based on the timing of the PE (approximately 12 hours after the 7.5 mg fondaparinux dose), Mr. SS should have been in a therapeutic range in regard to drug concentration.
In other words, Mr. SS still would have had more drug in his body 12 hours after a 7.5-mg dose than he would at 24 hours following a 10-mg dose. As such, Mr. SS would have had a fatal PE regardless. The plaintiff attacked the clinical judgment defense as unreasonable. There simply was no reason not to use the proven and recommended dose for SS. To do anything less was unnecessary experimentation on Mr. SS by the physicians involved.
Ironically, during deposition testimony, the hospitalist on call confirmed that he never discussed the Arixtra dose with the ED physician. He further testified that had he known that the ED physician was only going to give 7.5 mg, he would have increased the dose to 10 mg himself.
Conclusion
It is commonplace for hospitalists to discuss admission plans of care with our ED colleagues. Rarely, however, do we have such discussions with the same granularity as if we were writing the actual orders ourselves. It is important to remember that if we rely on our ED colleagues (or a house doctor) to fulfill our responsibilities in that regard, we can get trapped by a clinical judgment decision that doesn’t really match what we would have done under the same circumstances. The hospitalist in this case never even saw Mr. SS and he didn’t write the Arixtra order, yet he was deemed culpable for the outcome. Based on deposition testimony, it was readily apparent that the ED physician simply did not know the appropriate Arixtra dosing schedule for a patient weighing more than 100 kg. The jury, however, was ultimately persuaded by the defense arguments and returned a full defense verdict in this case.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has relationships with oral anticoagulant makers Janssen, Boehringer Ingelheim, and Daiichi Sankyo.
Mr. SS was a 48-year-old man who presented to the emergency department with complaints of right calf and ankle swelling for 1 day associated with mild shortness of breath. Lower extremity ultrasound quickly confirmed an acute right femoral and popliteal deep vein thrombosis. CT angiogram of the chest was negative for pulmonary embolus (PE). Two weeks earlier, Mr. SS had suffered a traumatic right intertrochanteric hip fracture when he fell off a ladder at home. At that time, he underwent open reduction and internal fixation of the right hip without complication. He was discharged home on warfarin for venous thromboembolism (VTE) prophylaxis. At the time of his return to the hospital, his INR was 1.4 and his current level of activity was touch toe weight-bearing of the right leg.
The ED physician paged the hospitalist on call, who was already at home for the evening. Following a telephone discussion, Mr. SS was given 7.5 mg of subcutaneous fondaparinux (Arixtra) in the ED. Mr. SS was then transferred up to the regular nursing floor and admitted by a house doctor employed by the hospital. The house doctor continued the fondaparinux at a dose of 7.5mg daily.
At approximately 10 a.m. the following day, Mr. SS was up in the bathroom. He became acutely short of breath and called out for help. Before he could return to bed, he was noted to be ashen in appearance, and he lost consciousness along with his pulse and respirations. A code blue was called, but despite more than an hour of resuscitation, Mr. SS expired. An autopsy was performed and confirmed a large saddle pulmonary embolism as the cause of death. The hospitalist on call never saw Mr. SS before he died.
Complaint
Mr. SS was an English professor at the local university. He left behind a wife and four children. A relation in the medical field reviewed the records and discovered that Mr. SS only received 7.5 mg of fondaparinux despite the fact that Mr. SS weighed more than 100 kg (265 pounds). The Food and Drug Administration–approved dose of Arixtra for the treatment of acute venous thromboembolism is based on tertile of weight (5 mg if less than 50 kg; 7.5 mg if between 50-100 kg; and 10 mg if more than 100 kg). The complaint alleged that Mr. SS was underdosed and therefore needlessly developed a pulmonary embolism. Had Mr. SS received the FDA-approved dose of fondaparinux based on his weight, he would be alive and well today.
The complaint was filed against the ED physician, the hospitalist on call, and the house doctor.
Scientific principles
Outcome studies confirm that the vast majority of patients (more than 95%) who receive adequate anticoagulation in the setting of acute venous thromboembolism (DVT/PE) will be alive at discharge, 30 days, and at 1 year. In fact, of all the variables possibly associated with VTE recurrence, the only one demonstrated by logistic regression to be statistically significant with respect to VTE recurrence is the failure to achieve and maintain adequate anticoagulation. Properly conducted phase II dose ranging studies with Arixtra (REMBRANDT) ultimately led to the tertile weight-based dosing regimen that was studied in the phase III trial (MATISSE) that led to Arixtra’s FDA approval and the recommendations for dosing in the Arixtra package insert.
Complaint rebuttal and discussion
The defense argued that the dosing recommendations in the Arixtra package insert were guidelines and not in and of themselves the standard of care. Mr. SS did not have a normal INR on presentation and the defense argued it was reasonable clinical judgment on behalf of the providers involved to use that dose that best balanced efficacy and safety. The defense further argued that based on the timing of the PE (approximately 12 hours after the 7.5 mg fondaparinux dose), Mr. SS should have been in a therapeutic range in regard to drug concentration.
In other words, Mr. SS still would have had more drug in his body 12 hours after a 7.5-mg dose than he would at 24 hours following a 10-mg dose. As such, Mr. SS would have had a fatal PE regardless. The plaintiff attacked the clinical judgment defense as unreasonable. There simply was no reason not to use the proven and recommended dose for SS. To do anything less was unnecessary experimentation on Mr. SS by the physicians involved.
Ironically, during deposition testimony, the hospitalist on call confirmed that he never discussed the Arixtra dose with the ED physician. He further testified that had he known that the ED physician was only going to give 7.5 mg, he would have increased the dose to 10 mg himself.
Conclusion
It is commonplace for hospitalists to discuss admission plans of care with our ED colleagues. Rarely, however, do we have such discussions with the same granularity as if we were writing the actual orders ourselves. It is important to remember that if we rely on our ED colleagues (or a house doctor) to fulfill our responsibilities in that regard, we can get trapped by a clinical judgment decision that doesn’t really match what we would have done under the same circumstances. The hospitalist in this case never even saw Mr. SS and he didn’t write the Arixtra order, yet he was deemed culpable for the outcome. Based on deposition testimony, it was readily apparent that the ED physician simply did not know the appropriate Arixtra dosing schedule for a patient weighing more than 100 kg. The jury, however, was ultimately persuaded by the defense arguments and returned a full defense verdict in this case.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has relationships with oral anticoagulant makers Janssen, Boehringer Ingelheim, and Daiichi Sankyo.
Mr. SS was a 48-year-old man who presented to the emergency department with complaints of right calf and ankle swelling for 1 day associated with mild shortness of breath. Lower extremity ultrasound quickly confirmed an acute right femoral and popliteal deep vein thrombosis. CT angiogram of the chest was negative for pulmonary embolus (PE). Two weeks earlier, Mr. SS had suffered a traumatic right intertrochanteric hip fracture when he fell off a ladder at home. At that time, he underwent open reduction and internal fixation of the right hip without complication. He was discharged home on warfarin for venous thromboembolism (VTE) prophylaxis. At the time of his return to the hospital, his INR was 1.4 and his current level of activity was touch toe weight-bearing of the right leg.
The ED physician paged the hospitalist on call, who was already at home for the evening. Following a telephone discussion, Mr. SS was given 7.5 mg of subcutaneous fondaparinux (Arixtra) in the ED. Mr. SS was then transferred up to the regular nursing floor and admitted by a house doctor employed by the hospital. The house doctor continued the fondaparinux at a dose of 7.5mg daily.
At approximately 10 a.m. the following day, Mr. SS was up in the bathroom. He became acutely short of breath and called out for help. Before he could return to bed, he was noted to be ashen in appearance, and he lost consciousness along with his pulse and respirations. A code blue was called, but despite more than an hour of resuscitation, Mr. SS expired. An autopsy was performed and confirmed a large saddle pulmonary embolism as the cause of death. The hospitalist on call never saw Mr. SS before he died.
Complaint
Mr. SS was an English professor at the local university. He left behind a wife and four children. A relation in the medical field reviewed the records and discovered that Mr. SS only received 7.5 mg of fondaparinux despite the fact that Mr. SS weighed more than 100 kg (265 pounds). The Food and Drug Administration–approved dose of Arixtra for the treatment of acute venous thromboembolism is based on tertile of weight (5 mg if less than 50 kg; 7.5 mg if between 50-100 kg; and 10 mg if more than 100 kg). The complaint alleged that Mr. SS was underdosed and therefore needlessly developed a pulmonary embolism. Had Mr. SS received the FDA-approved dose of fondaparinux based on his weight, he would be alive and well today.
The complaint was filed against the ED physician, the hospitalist on call, and the house doctor.
Scientific principles
Outcome studies confirm that the vast majority of patients (more than 95%) who receive adequate anticoagulation in the setting of acute venous thromboembolism (DVT/PE) will be alive at discharge, 30 days, and at 1 year. In fact, of all the variables possibly associated with VTE recurrence, the only one demonstrated by logistic regression to be statistically significant with respect to VTE recurrence is the failure to achieve and maintain adequate anticoagulation. Properly conducted phase II dose ranging studies with Arixtra (REMBRANDT) ultimately led to the tertile weight-based dosing regimen that was studied in the phase III trial (MATISSE) that led to Arixtra’s FDA approval and the recommendations for dosing in the Arixtra package insert.
Complaint rebuttal and discussion
The defense argued that the dosing recommendations in the Arixtra package insert were guidelines and not in and of themselves the standard of care. Mr. SS did not have a normal INR on presentation and the defense argued it was reasonable clinical judgment on behalf of the providers involved to use that dose that best balanced efficacy and safety. The defense further argued that based on the timing of the PE (approximately 12 hours after the 7.5 mg fondaparinux dose), Mr. SS should have been in a therapeutic range in regard to drug concentration.
In other words, Mr. SS still would have had more drug in his body 12 hours after a 7.5-mg dose than he would at 24 hours following a 10-mg dose. As such, Mr. SS would have had a fatal PE regardless. The plaintiff attacked the clinical judgment defense as unreasonable. There simply was no reason not to use the proven and recommended dose for SS. To do anything less was unnecessary experimentation on Mr. SS by the physicians involved.
Ironically, during deposition testimony, the hospitalist on call confirmed that he never discussed the Arixtra dose with the ED physician. He further testified that had he known that the ED physician was only going to give 7.5 mg, he would have increased the dose to 10 mg himself.
Conclusion
It is commonplace for hospitalists to discuss admission plans of care with our ED colleagues. Rarely, however, do we have such discussions with the same granularity as if we were writing the actual orders ourselves. It is important to remember that if we rely on our ED colleagues (or a house doctor) to fulfill our responsibilities in that regard, we can get trapped by a clinical judgment decision that doesn’t really match what we would have done under the same circumstances. The hospitalist in this case never even saw Mr. SS and he didn’t write the Arixtra order, yet he was deemed culpable for the outcome. Based on deposition testimony, it was readily apparent that the ED physician simply did not know the appropriate Arixtra dosing schedule for a patient weighing more than 100 kg. The jury, however, was ultimately persuaded by the defense arguments and returned a full defense verdict in this case.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has relationships with oral anticoagulant makers Janssen, Boehringer Ingelheim, and Daiichi Sankyo.
Medicolegal lesson: Beyond the Scope
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
A painful result
The story
ET was a 40-year-old married woman and local news reporter when she presented to her local emergency department (ED) complaining of right thigh pain. ET was also a triathlete and worked out vigorously at the gym every afternoon. Her workout that day consisted of squats and other lower-leg exercises, but was otherwise uneventful. After dinner that night, she began to experience anterolateral, burning pain in her right thigh that was unresponsive to ibuprofen. Her ED evaluation was essentially normal and she was discharged with a diagnosis of muscle strain/tear with possible hematoma. ET returned to the ED at 9:30 the next morning. She was walking with difficulty and in severe 10/10 pain. She was tachycardic and her thigh was noted to be mildly swollen and severely tender on palpation. A CT scan of her right thigh was performed.
"Small amount of fluid tracking along lateral aspect of vastus lateralis muscle. Mild decreased attenuation in the distal portion of the muscle itself. Findings may suggest muscle bundle tear and adjacent hematoma. Inflammatory/infectious process cannot be entirely excluded."
Following the CT results, she was rocking and crying in bed from the pain. The ED physician called Dr. Hospitalist, who admitted ET for intravenous pain control.
ET received multiple doses of intravenous hydromorphone overnight and was intermittently sleeping and crying awake because of severe pain. Vitals that morning showed ET to be afebrile, but tachycardic and hypotensive (BP = 85/50 mm Hg). The exam of the thigh was generally unchanged. The impression remained right muscle tear with hypotension as a result of intravenous hydromorphone. Later that morning, a CBC showed a WBC 14.0 K/mcL with 68% bands. Dr. Hospitalist eventually ordered intravenous fluid boluses, intravenous clindamycin, and an anesthesia consult for patient-controlled analgesia. By late afternoon, ET had refractory hypotension and was sent to the ICU for pressor support. Ultrasound found no evidence for DVT [deep vein thrombosis] in her thigh but a CK [creatine kinase] level was more than 2,000 IU/L. A surgical consult was obtained and ET was subsequently transferred via life-flight to the nearest university hospital for fasciotomy and thigh debridement. Within 2 days of the transfer, ET had four surgeries, culminating in a right hip disarticulation for necrotizing fasciitis. She was ultimately hospitalized for 3 months. Today, she is wheelchair bound and divorced because of the effects her illness had on her marital relationship. She is unable to work and has suffered from severe depression because of the loss of her leg.
Complaint
ET and her husband immediately blamed Dr. Hospitalist and the care she received at the community hospital for a delayed diagnosis of necrotizing fasciitis. The husband, a PhD in physiology and nutrition and consultant with the NFL’s Carolina Panthers, was highly critical of the muscle tear diagnosis. He testified that he told the ED physician and Dr. Hospitalist that there was no way that his wife was in so much pain from a muscle tear. In addition, both ET and her husband testified that she suffered no injury at the gym that would account for a muscle tear/rupture in the first place. The complaint alleged that had the ED physician and Dr. Hospitalist made the correct diagnosis, ET would have undergone debridement without the need for amputation. The complaint further alleged that had the debridement occurred in a timely fashion, she would not have suffered from the protracted tertiary hospital stay and all the associated complications and medical bills.
Scientific principles
Necrotizing soft-tissue infections include necrotizing forms of cellulitis, myositis, and fasciitis. These infections are characterized clinically by fulminant tissue destruction, systemic signs of toxicity, and high mortality. Accurate diagnosis and appropriate treatment must include early surgical intervention and antibiotic therapy. It is important to consider necrotizing involvement of the muscle or fascia in the setting of fever, toxicity, soft-tissue involvement with severe pain (particularly if out of proportion to skin findings), crepitus, rapid progression of clinical manifestations, and elevated serum CK level. The diagnosis of necrotizing fasciitis is established surgically, with visualization of fascial planes and muscle tissue in the operating room.
Complaint rebuttal and discussion
The ED physician asserted that, although he was unsure what was going on with ET, he appropriately admitted her to Dr. Hospitalist for further management. ET was hemodynamically stable during her time in the ED, without signs of toxicity or fever. As a result, the ED physician could not be expected to make a diagnosis at that time or even involve surgery as this rare condition was still evolving. This opinion was echoed by multiple ED defense experts and the ED physician involved was subsequently dropped from this case. Dr. Hospitalist asserted that he was admitting ET for pain control and that the CT of the right thigh confirmed the most probable diagnosis was muscle tear with hematoma. Dr. Hospitalist asserted that he had no reason to suspect a rare diagnosis in this otherwise healthy woman. Regardless, Dr. Hospitalist argued that even had he considered necrotizing fasciitis at the time of admission, it was more likely than not going to be too late to prevent ET from losing her leg.
Plaintiff experts opined that Dr. Hospitalist should have ordered a CBC and blood cultures on admission as the CT report could not exclude an infectious process. Had a CBC been performed, it was probable that bandemia would have been present and systemic inflammatory response criteria would have been met (bandemia plus tachycardia). In addition, ET was complaining of severe pain out of proportion for exam findings, and this should have put necrotizing soft tissue infection in the differential diagnosis. The combination of systemic inflammatory response plus the severe pain would reasonably have led to a STAT surgical consult the day of admission with earlier debridement and leg-sparing surgery.
Conclusion
An individual hospitalist will admit hundreds of patients a year with routine and common problems. But admission for "pain control" is a red flag for an underlying disorder that has been missed by the ED evaluation. The diagnosis of necrotizing soft tissue infections requires a high level of suspicion. Patients that have new and persistent pain out of proportion to exam findings and in the face of high-dose opiate administration should lead to further investigation. Although ET survived, the outcome was considered catastrophic. A week before trial was to begin this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reports having no relevant financial conflicts.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
Medicolegal Review has the opportunity to become the morbidity and mortality conference of the modern era. Each month, this column presents a case vignette that explores some aspect of medicine and the applicable standard of care.
The story
ET was a 40-year-old married woman and local news reporter when she presented to her local emergency department (ED) complaining of right thigh pain. ET was also a triathlete and worked out vigorously at the gym every afternoon. Her workout that day consisted of squats and other lower-leg exercises, but was otherwise uneventful. After dinner that night, she began to experience anterolateral, burning pain in her right thigh that was unresponsive to ibuprofen. Her ED evaluation was essentially normal and she was discharged with a diagnosis of muscle strain/tear with possible hematoma. ET returned to the ED at 9:30 the next morning. She was walking with difficulty and in severe 10/10 pain. She was tachycardic and her thigh was noted to be mildly swollen and severely tender on palpation. A CT scan of her right thigh was performed.
"Small amount of fluid tracking along lateral aspect of vastus lateralis muscle. Mild decreased attenuation in the distal portion of the muscle itself. Findings may suggest muscle bundle tear and adjacent hematoma. Inflammatory/infectious process cannot be entirely excluded."
Following the CT results, she was rocking and crying in bed from the pain. The ED physician called Dr. Hospitalist, who admitted ET for intravenous pain control.
ET received multiple doses of intravenous hydromorphone overnight and was intermittently sleeping and crying awake because of severe pain. Vitals that morning showed ET to be afebrile, but tachycardic and hypotensive (BP = 85/50 mm Hg). The exam of the thigh was generally unchanged. The impression remained right muscle tear with hypotension as a result of intravenous hydromorphone. Later that morning, a CBC showed a WBC 14.0 K/mcL with 68% bands. Dr. Hospitalist eventually ordered intravenous fluid boluses, intravenous clindamycin, and an anesthesia consult for patient-controlled analgesia. By late afternoon, ET had refractory hypotension and was sent to the ICU for pressor support. Ultrasound found no evidence for DVT [deep vein thrombosis] in her thigh but a CK [creatine kinase] level was more than 2,000 IU/L. A surgical consult was obtained and ET was subsequently transferred via life-flight to the nearest university hospital for fasciotomy and thigh debridement. Within 2 days of the transfer, ET had four surgeries, culminating in a right hip disarticulation for necrotizing fasciitis. She was ultimately hospitalized for 3 months. Today, she is wheelchair bound and divorced because of the effects her illness had on her marital relationship. She is unable to work and has suffered from severe depression because of the loss of her leg.
Complaint
ET and her husband immediately blamed Dr. Hospitalist and the care she received at the community hospital for a delayed diagnosis of necrotizing fasciitis. The husband, a PhD in physiology and nutrition and consultant with the NFL’s Carolina Panthers, was highly critical of the muscle tear diagnosis. He testified that he told the ED physician and Dr. Hospitalist that there was no way that his wife was in so much pain from a muscle tear. In addition, both ET and her husband testified that she suffered no injury at the gym that would account for a muscle tear/rupture in the first place. The complaint alleged that had the ED physician and Dr. Hospitalist made the correct diagnosis, ET would have undergone debridement without the need for amputation. The complaint further alleged that had the debridement occurred in a timely fashion, she would not have suffered from the protracted tertiary hospital stay and all the associated complications and medical bills.
Scientific principles
Necrotizing soft-tissue infections include necrotizing forms of cellulitis, myositis, and fasciitis. These infections are characterized clinically by fulminant tissue destruction, systemic signs of toxicity, and high mortality. Accurate diagnosis and appropriate treatment must include early surgical intervention and antibiotic therapy. It is important to consider necrotizing involvement of the muscle or fascia in the setting of fever, toxicity, soft-tissue involvement with severe pain (particularly if out of proportion to skin findings), crepitus, rapid progression of clinical manifestations, and elevated serum CK level. The diagnosis of necrotizing fasciitis is established surgically, with visualization of fascial planes and muscle tissue in the operating room.
Complaint rebuttal and discussion
The ED physician asserted that, although he was unsure what was going on with ET, he appropriately admitted her to Dr. Hospitalist for further management. ET was hemodynamically stable during her time in the ED, without signs of toxicity or fever. As a result, the ED physician could not be expected to make a diagnosis at that time or even involve surgery as this rare condition was still evolving. This opinion was echoed by multiple ED defense experts and the ED physician involved was subsequently dropped from this case. Dr. Hospitalist asserted that he was admitting ET for pain control and that the CT of the right thigh confirmed the most probable diagnosis was muscle tear with hematoma. Dr. Hospitalist asserted that he had no reason to suspect a rare diagnosis in this otherwise healthy woman. Regardless, Dr. Hospitalist argued that even had he considered necrotizing fasciitis at the time of admission, it was more likely than not going to be too late to prevent ET from losing her leg.
Plaintiff experts opined that Dr. Hospitalist should have ordered a CBC and blood cultures on admission as the CT report could not exclude an infectious process. Had a CBC been performed, it was probable that bandemia would have been present and systemic inflammatory response criteria would have been met (bandemia plus tachycardia). In addition, ET was complaining of severe pain out of proportion for exam findings, and this should have put necrotizing soft tissue infection in the differential diagnosis. The combination of systemic inflammatory response plus the severe pain would reasonably have led to a STAT surgical consult the day of admission with earlier debridement and leg-sparing surgery.
Conclusion
An individual hospitalist will admit hundreds of patients a year with routine and common problems. But admission for "pain control" is a red flag for an underlying disorder that has been missed by the ED evaluation. The diagnosis of necrotizing soft tissue infections requires a high level of suspicion. Patients that have new and persistent pain out of proportion to exam findings and in the face of high-dose opiate administration should lead to further investigation. Although ET survived, the outcome was considered catastrophic. A week before trial was to begin this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reports having no relevant financial conflicts.
The story
ET was a 40-year-old married woman and local news reporter when she presented to her local emergency department (ED) complaining of right thigh pain. ET was also a triathlete and worked out vigorously at the gym every afternoon. Her workout that day consisted of squats and other lower-leg exercises, but was otherwise uneventful. After dinner that night, she began to experience anterolateral, burning pain in her right thigh that was unresponsive to ibuprofen. Her ED evaluation was essentially normal and she was discharged with a diagnosis of muscle strain/tear with possible hematoma. ET returned to the ED at 9:30 the next morning. She was walking with difficulty and in severe 10/10 pain. She was tachycardic and her thigh was noted to be mildly swollen and severely tender on palpation. A CT scan of her right thigh was performed.
"Small amount of fluid tracking along lateral aspect of vastus lateralis muscle. Mild decreased attenuation in the distal portion of the muscle itself. Findings may suggest muscle bundle tear and adjacent hematoma. Inflammatory/infectious process cannot be entirely excluded."
Following the CT results, she was rocking and crying in bed from the pain. The ED physician called Dr. Hospitalist, who admitted ET for intravenous pain control.
ET received multiple doses of intravenous hydromorphone overnight and was intermittently sleeping and crying awake because of severe pain. Vitals that morning showed ET to be afebrile, but tachycardic and hypotensive (BP = 85/50 mm Hg). The exam of the thigh was generally unchanged. The impression remained right muscle tear with hypotension as a result of intravenous hydromorphone. Later that morning, a CBC showed a WBC 14.0 K/mcL with 68% bands. Dr. Hospitalist eventually ordered intravenous fluid boluses, intravenous clindamycin, and an anesthesia consult for patient-controlled analgesia. By late afternoon, ET had refractory hypotension and was sent to the ICU for pressor support. Ultrasound found no evidence for DVT [deep vein thrombosis] in her thigh but a CK [creatine kinase] level was more than 2,000 IU/L. A surgical consult was obtained and ET was subsequently transferred via life-flight to the nearest university hospital for fasciotomy and thigh debridement. Within 2 days of the transfer, ET had four surgeries, culminating in a right hip disarticulation for necrotizing fasciitis. She was ultimately hospitalized for 3 months. Today, she is wheelchair bound and divorced because of the effects her illness had on her marital relationship. She is unable to work and has suffered from severe depression because of the loss of her leg.
Complaint
ET and her husband immediately blamed Dr. Hospitalist and the care she received at the community hospital for a delayed diagnosis of necrotizing fasciitis. The husband, a PhD in physiology and nutrition and consultant with the NFL’s Carolina Panthers, was highly critical of the muscle tear diagnosis. He testified that he told the ED physician and Dr. Hospitalist that there was no way that his wife was in so much pain from a muscle tear. In addition, both ET and her husband testified that she suffered no injury at the gym that would account for a muscle tear/rupture in the first place. The complaint alleged that had the ED physician and Dr. Hospitalist made the correct diagnosis, ET would have undergone debridement without the need for amputation. The complaint further alleged that had the debridement occurred in a timely fashion, she would not have suffered from the protracted tertiary hospital stay and all the associated complications and medical bills.
Scientific principles
Necrotizing soft-tissue infections include necrotizing forms of cellulitis, myositis, and fasciitis. These infections are characterized clinically by fulminant tissue destruction, systemic signs of toxicity, and high mortality. Accurate diagnosis and appropriate treatment must include early surgical intervention and antibiotic therapy. It is important to consider necrotizing involvement of the muscle or fascia in the setting of fever, toxicity, soft-tissue involvement with severe pain (particularly if out of proportion to skin findings), crepitus, rapid progression of clinical manifestations, and elevated serum CK level. The diagnosis of necrotizing fasciitis is established surgically, with visualization of fascial planes and muscle tissue in the operating room.
Complaint rebuttal and discussion
The ED physician asserted that, although he was unsure what was going on with ET, he appropriately admitted her to Dr. Hospitalist for further management. ET was hemodynamically stable during her time in the ED, without signs of toxicity or fever. As a result, the ED physician could not be expected to make a diagnosis at that time or even involve surgery as this rare condition was still evolving. This opinion was echoed by multiple ED defense experts and the ED physician involved was subsequently dropped from this case. Dr. Hospitalist asserted that he was admitting ET for pain control and that the CT of the right thigh confirmed the most probable diagnosis was muscle tear with hematoma. Dr. Hospitalist asserted that he had no reason to suspect a rare diagnosis in this otherwise healthy woman. Regardless, Dr. Hospitalist argued that even had he considered necrotizing fasciitis at the time of admission, it was more likely than not going to be too late to prevent ET from losing her leg.
Plaintiff experts opined that Dr. Hospitalist should have ordered a CBC and blood cultures on admission as the CT report could not exclude an infectious process. Had a CBC been performed, it was probable that bandemia would have been present and systemic inflammatory response criteria would have been met (bandemia plus tachycardia). In addition, ET was complaining of severe pain out of proportion for exam findings, and this should have put necrotizing soft tissue infection in the differential diagnosis. The combination of systemic inflammatory response plus the severe pain would reasonably have led to a STAT surgical consult the day of admission with earlier debridement and leg-sparing surgery.
Conclusion
An individual hospitalist will admit hundreds of patients a year with routine and common problems. But admission for "pain control" is a red flag for an underlying disorder that has been missed by the ED evaluation. The diagnosis of necrotizing soft tissue infections requires a high level of suspicion. Patients that have new and persistent pain out of proportion to exam findings and in the face of high-dose opiate administration should lead to further investigation. Although ET survived, the outcome was considered catastrophic. A week before trial was to begin this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reports having no relevant financial conflicts.
'A typical' chest pain
Story:
Mr. FW was a 69-year-old man with a history of hypertension, hyperlipidemia, generalized anxiety, and chronic low back pain who presented to the emergency department (ED) from his primary care physician’s office with substernal burning chest pain that began earlier that morning while he was shopping with his wife.
The discomfort was mild (3 out of 10) and completely resolved by the time he arrived to the ED around 12:30 p.m. The day before, he had experienced the same substernal burning chest discomfort, but it had been more intense (7 out of 10). At that time, he was outside and observed his neighbor’s dog that appeared to have the patient’s cat in its mouth and apparently sprinted almost 100 yards to reach the animals. He developed the substernal chest discomfort while running.
The pain radiated to his neck and throat. He was short of breath from the exertion. The pain resolved after 30-40 minutes of rest after taking several antacid pills. The patient stated that he was not normally that active because of his back. Patient also noted that he had a pharmacologic stress test 3 years ago because of chest symptoms, and it was completely normal. His EKG in the ED showed normal sinus rhythm, voltage criteria for LVH and nonspecific ST segment and T-wave changes in the precordial leads but was otherwise normal. A CBC, basic metabolic profile, and cardiac biomarkers were all normal.
FW was seen by Dr. Hospitalist in the ED and documented that Mr. FW was pain free. Mr. FW was then admitted to the telemetry floor for atypical chest pain/rule out MI protocol. Dr. Hospitalist put Mr. FW on telemetry monitoring, a cardiac diet, aspirin 325mg daily, PRN nitroglycerin, PRN morphine, his baseline medications (amlodipine, atorvastatin, and lorazepam) and cycled cardiac biomarkers q8hrs x 2. Dr. Hospitalist also ordered a pharmacologic stress test for the morning.
At 10 p.m. that evening, as Mr. FW was up to go to the bathroom, he called out to the nurse complaining of a sharp pain in his neck and throat accompanied by lightheadedness. His blood pressure sitting was 70/30 mm Hg. Telemetry showed new left bundle branch block (LBBB). He was helped back to bed when he became unresponsive. Mr. FW underwent resuscitation efforts for the next 45 minutes. Telemetry strips demonstrated evolution of EKG waveforms with ST elevations in the anterior leads prior to the development of LBBB.
Mr. FW was unable to be revived and was pronounced dead at 10:55 p.m. No autopsy was performed
Complaint:
Shortly before Mr. FW became unresponsive, his wife had just left the hospital for the night after the nurse reassured her that Mr. FW would be fine.
Upon learning about the ST elevations during the code blue, Mr. FW’s widow met with an attorney and filed suit. The complaint alleged that Dr. Hospitalist failed to recognize unstable angina and failed to treat Mr. FW as acute coronary syndrome (ACS). She further alleged that Dr. Hospitalist breached the standard of care for not consulting a cardiologist and for not initiating beta-blockers and anticoagulation. As a result of Dr. Hospitalist failing to recognize ACS, Mr. FW died of ST-elevation MI, she asserted.
Scientific principles:
ACS comprises unstable angina (UA), non-ST elevation myocardial infarction, ST-elevation MI, and sudden cardiac death. By definition, ACS is an inflammatory reaction in the coronary vessels and is medically treated with antiplatelet agents and anticoagulation.
In a capable hospital, often ACS will be treated with a percutaneous coronary intervention.
UA is typical cardiac chest pain that is new in onset, increasing in frequency, duration, and intensity, and/or occurring with less exertion or at rest. UA is ultimately a clinical diagnosis based almost entirely on history, although it may be associated with EKG changes during chest pain episodes. Cardiac biomarkers are expected to be normal.
Typical cardiac chest pain is substernal or, in the anterior chest, with a character of burning or chest heaviness, is precipitated by exertion and relieved by rest or nitroglycerin. Typical cardiac chest pain radiates to the neck, left shoulder, or left arm, and is associated with shortness of breath and nausea.
Atypical chest pain is often fleeting (lasts seconds to a minute), is not in the anterior chest; the character is sharp, not reliably produced by exertion nor relieved with rest or nitroglycerin, and will occur in patients without known cardiac risk factors (male sex, hypertension, smoking, diabetes, hyperlipidemia, family history).
Complaint rebuttal and discussion:
Dr. Hospitalist was adamant that this patient did not have ACS. In fact, this hospital could not do PCI and if Dr. Hospitalist thought this was ACS, he wouldn’t have accepted the patient and the patient would have been transferred to an alternative hospital.
The admission history and physical by Dr. Hospitalist noted prior episodes of chest pain with dancing and suggested that Mr. FW’s history was consistent with chronic angina and that his pain after racing across his lawn to rescue his cat was a demand ischemia phenomenon (not ACS) in a man who was usually sedentary. Dr. Hospitalist further argued that the pain could easily have been GI related because of its burning character, radiation to the throat, and relief with antacids. The patient was pain free at admission without acute changes on his EKG and had had two sets of normal biomarkers before Dr. Hospitalist left for the day. Dr. Hospitalist also argued that a cardiologist wasn’t necessary unless Mr. FW had a positive stress test the following morning.
Unfortunately, Dr. Hospitalist did not take a thorough and comprehensive history regarding Mr. FW’s chest discomfort on the day of admission. Dr. Hospitalist appeared to pay far more attention to Mr. FW’s symptoms on the previous day when he was trying to rescue his cat. On the day of admission, Mr. FW developed chest discomfort while simply walking in the grocery store with his wife. They immediately went to see their primary care physician, who obtained an EKG in the office while Mr. FW was having symptoms.
The EKG showed deeper ST depression with new T-wave inversions in the precordial leads, compared with the EKG performed at the ED several hours later. In addition, the pain lasted for almost 50 minutes, including the time during which he was driving (almost at rest) on the way to the ED. The widow’s deposition also confirmed that Mr. FW’s occasional chest discomfort while dancing the polka was not typical cardiac chest pain. The widow further confirmed that Mr. FW, despite a history of low back pain, was quite active and did not routinely experience exertional chest symptoms.
Conclusion:
Hospitalists are frequently called upon to "rule out MI." It is important, however, to distinguish patients with atypical, noncardiac chest pain from those with typical cardiac chest pain.
Patients with atypical chest pain are being admitted for observation and to rule in or rule out whether their symptoms are cardiac or not. Patients admitted with a history of typical cardiac chest pain, regardless of whether they are pain free at the time of admission, should be treated for ACS until they can receive a diagnostic cardiac catheterization or further risk stratification by a cardiologist. The jury recognized the failure of Dr. Hospitalist to perform a thorough and adequate history in this case.
The case in question occurred in a non–tort reform state. As such, there were no limits on noneconomic damages (in other words, pain and suffering). A judgment was rendered for the widow in this case with damages in the amount of $1 million.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Story:
Mr. FW was a 69-year-old man with a history of hypertension, hyperlipidemia, generalized anxiety, and chronic low back pain who presented to the emergency department (ED) from his primary care physician’s office with substernal burning chest pain that began earlier that morning while he was shopping with his wife.
The discomfort was mild (3 out of 10) and completely resolved by the time he arrived to the ED around 12:30 p.m. The day before, he had experienced the same substernal burning chest discomfort, but it had been more intense (7 out of 10). At that time, he was outside and observed his neighbor’s dog that appeared to have the patient’s cat in its mouth and apparently sprinted almost 100 yards to reach the animals. He developed the substernal chest discomfort while running.
The pain radiated to his neck and throat. He was short of breath from the exertion. The pain resolved after 30-40 minutes of rest after taking several antacid pills. The patient stated that he was not normally that active because of his back. Patient also noted that he had a pharmacologic stress test 3 years ago because of chest symptoms, and it was completely normal. His EKG in the ED showed normal sinus rhythm, voltage criteria for LVH and nonspecific ST segment and T-wave changes in the precordial leads but was otherwise normal. A CBC, basic metabolic profile, and cardiac biomarkers were all normal.
FW was seen by Dr. Hospitalist in the ED and documented that Mr. FW was pain free. Mr. FW was then admitted to the telemetry floor for atypical chest pain/rule out MI protocol. Dr. Hospitalist put Mr. FW on telemetry monitoring, a cardiac diet, aspirin 325mg daily, PRN nitroglycerin, PRN morphine, his baseline medications (amlodipine, atorvastatin, and lorazepam) and cycled cardiac biomarkers q8hrs x 2. Dr. Hospitalist also ordered a pharmacologic stress test for the morning.
At 10 p.m. that evening, as Mr. FW was up to go to the bathroom, he called out to the nurse complaining of a sharp pain in his neck and throat accompanied by lightheadedness. His blood pressure sitting was 70/30 mm Hg. Telemetry showed new left bundle branch block (LBBB). He was helped back to bed when he became unresponsive. Mr. FW underwent resuscitation efforts for the next 45 minutes. Telemetry strips demonstrated evolution of EKG waveforms with ST elevations in the anterior leads prior to the development of LBBB.
Mr. FW was unable to be revived and was pronounced dead at 10:55 p.m. No autopsy was performed
Complaint:
Shortly before Mr. FW became unresponsive, his wife had just left the hospital for the night after the nurse reassured her that Mr. FW would be fine.
Upon learning about the ST elevations during the code blue, Mr. FW’s widow met with an attorney and filed suit. The complaint alleged that Dr. Hospitalist failed to recognize unstable angina and failed to treat Mr. FW as acute coronary syndrome (ACS). She further alleged that Dr. Hospitalist breached the standard of care for not consulting a cardiologist and for not initiating beta-blockers and anticoagulation. As a result of Dr. Hospitalist failing to recognize ACS, Mr. FW died of ST-elevation MI, she asserted.
Scientific principles:
ACS comprises unstable angina (UA), non-ST elevation myocardial infarction, ST-elevation MI, and sudden cardiac death. By definition, ACS is an inflammatory reaction in the coronary vessels and is medically treated with antiplatelet agents and anticoagulation.
In a capable hospital, often ACS will be treated with a percutaneous coronary intervention.
UA is typical cardiac chest pain that is new in onset, increasing in frequency, duration, and intensity, and/or occurring with less exertion or at rest. UA is ultimately a clinical diagnosis based almost entirely on history, although it may be associated with EKG changes during chest pain episodes. Cardiac biomarkers are expected to be normal.
Typical cardiac chest pain is substernal or, in the anterior chest, with a character of burning or chest heaviness, is precipitated by exertion and relieved by rest or nitroglycerin. Typical cardiac chest pain radiates to the neck, left shoulder, or left arm, and is associated with shortness of breath and nausea.
Atypical chest pain is often fleeting (lasts seconds to a minute), is not in the anterior chest; the character is sharp, not reliably produced by exertion nor relieved with rest or nitroglycerin, and will occur in patients without known cardiac risk factors (male sex, hypertension, smoking, diabetes, hyperlipidemia, family history).
Complaint rebuttal and discussion:
Dr. Hospitalist was adamant that this patient did not have ACS. In fact, this hospital could not do PCI and if Dr. Hospitalist thought this was ACS, he wouldn’t have accepted the patient and the patient would have been transferred to an alternative hospital.
The admission history and physical by Dr. Hospitalist noted prior episodes of chest pain with dancing and suggested that Mr. FW’s history was consistent with chronic angina and that his pain after racing across his lawn to rescue his cat was a demand ischemia phenomenon (not ACS) in a man who was usually sedentary. Dr. Hospitalist further argued that the pain could easily have been GI related because of its burning character, radiation to the throat, and relief with antacids. The patient was pain free at admission without acute changes on his EKG and had had two sets of normal biomarkers before Dr. Hospitalist left for the day. Dr. Hospitalist also argued that a cardiologist wasn’t necessary unless Mr. FW had a positive stress test the following morning.
Unfortunately, Dr. Hospitalist did not take a thorough and comprehensive history regarding Mr. FW’s chest discomfort on the day of admission. Dr. Hospitalist appeared to pay far more attention to Mr. FW’s symptoms on the previous day when he was trying to rescue his cat. On the day of admission, Mr. FW developed chest discomfort while simply walking in the grocery store with his wife. They immediately went to see their primary care physician, who obtained an EKG in the office while Mr. FW was having symptoms.
The EKG showed deeper ST depression with new T-wave inversions in the precordial leads, compared with the EKG performed at the ED several hours later. In addition, the pain lasted for almost 50 minutes, including the time during which he was driving (almost at rest) on the way to the ED. The widow’s deposition also confirmed that Mr. FW’s occasional chest discomfort while dancing the polka was not typical cardiac chest pain. The widow further confirmed that Mr. FW, despite a history of low back pain, was quite active and did not routinely experience exertional chest symptoms.
Conclusion:
Hospitalists are frequently called upon to "rule out MI." It is important, however, to distinguish patients with atypical, noncardiac chest pain from those with typical cardiac chest pain.
Patients with atypical chest pain are being admitted for observation and to rule in or rule out whether their symptoms are cardiac or not. Patients admitted with a history of typical cardiac chest pain, regardless of whether they are pain free at the time of admission, should be treated for ACS until they can receive a diagnostic cardiac catheterization or further risk stratification by a cardiologist. The jury recognized the failure of Dr. Hospitalist to perform a thorough and adequate history in this case.
The case in question occurred in a non–tort reform state. As such, there were no limits on noneconomic damages (in other words, pain and suffering). A judgment was rendered for the widow in this case with damages in the amount of $1 million.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Story:
Mr. FW was a 69-year-old man with a history of hypertension, hyperlipidemia, generalized anxiety, and chronic low back pain who presented to the emergency department (ED) from his primary care physician’s office with substernal burning chest pain that began earlier that morning while he was shopping with his wife.
The discomfort was mild (3 out of 10) and completely resolved by the time he arrived to the ED around 12:30 p.m. The day before, he had experienced the same substernal burning chest discomfort, but it had been more intense (7 out of 10). At that time, he was outside and observed his neighbor’s dog that appeared to have the patient’s cat in its mouth and apparently sprinted almost 100 yards to reach the animals. He developed the substernal chest discomfort while running.
The pain radiated to his neck and throat. He was short of breath from the exertion. The pain resolved after 30-40 minutes of rest after taking several antacid pills. The patient stated that he was not normally that active because of his back. Patient also noted that he had a pharmacologic stress test 3 years ago because of chest symptoms, and it was completely normal. His EKG in the ED showed normal sinus rhythm, voltage criteria for LVH and nonspecific ST segment and T-wave changes in the precordial leads but was otherwise normal. A CBC, basic metabolic profile, and cardiac biomarkers were all normal.
FW was seen by Dr. Hospitalist in the ED and documented that Mr. FW was pain free. Mr. FW was then admitted to the telemetry floor for atypical chest pain/rule out MI protocol. Dr. Hospitalist put Mr. FW on telemetry monitoring, a cardiac diet, aspirin 325mg daily, PRN nitroglycerin, PRN morphine, his baseline medications (amlodipine, atorvastatin, and lorazepam) and cycled cardiac biomarkers q8hrs x 2. Dr. Hospitalist also ordered a pharmacologic stress test for the morning.
At 10 p.m. that evening, as Mr. FW was up to go to the bathroom, he called out to the nurse complaining of a sharp pain in his neck and throat accompanied by lightheadedness. His blood pressure sitting was 70/30 mm Hg. Telemetry showed new left bundle branch block (LBBB). He was helped back to bed when he became unresponsive. Mr. FW underwent resuscitation efforts for the next 45 minutes. Telemetry strips demonstrated evolution of EKG waveforms with ST elevations in the anterior leads prior to the development of LBBB.
Mr. FW was unable to be revived and was pronounced dead at 10:55 p.m. No autopsy was performed
Complaint:
Shortly before Mr. FW became unresponsive, his wife had just left the hospital for the night after the nurse reassured her that Mr. FW would be fine.
Upon learning about the ST elevations during the code blue, Mr. FW’s widow met with an attorney and filed suit. The complaint alleged that Dr. Hospitalist failed to recognize unstable angina and failed to treat Mr. FW as acute coronary syndrome (ACS). She further alleged that Dr. Hospitalist breached the standard of care for not consulting a cardiologist and for not initiating beta-blockers and anticoagulation. As a result of Dr. Hospitalist failing to recognize ACS, Mr. FW died of ST-elevation MI, she asserted.
Scientific principles:
ACS comprises unstable angina (UA), non-ST elevation myocardial infarction, ST-elevation MI, and sudden cardiac death. By definition, ACS is an inflammatory reaction in the coronary vessels and is medically treated with antiplatelet agents and anticoagulation.
In a capable hospital, often ACS will be treated with a percutaneous coronary intervention.
UA is typical cardiac chest pain that is new in onset, increasing in frequency, duration, and intensity, and/or occurring with less exertion or at rest. UA is ultimately a clinical diagnosis based almost entirely on history, although it may be associated with EKG changes during chest pain episodes. Cardiac biomarkers are expected to be normal.
Typical cardiac chest pain is substernal or, in the anterior chest, with a character of burning or chest heaviness, is precipitated by exertion and relieved by rest or nitroglycerin. Typical cardiac chest pain radiates to the neck, left shoulder, or left arm, and is associated with shortness of breath and nausea.
Atypical chest pain is often fleeting (lasts seconds to a minute), is not in the anterior chest; the character is sharp, not reliably produced by exertion nor relieved with rest or nitroglycerin, and will occur in patients without known cardiac risk factors (male sex, hypertension, smoking, diabetes, hyperlipidemia, family history).
Complaint rebuttal and discussion:
Dr. Hospitalist was adamant that this patient did not have ACS. In fact, this hospital could not do PCI and if Dr. Hospitalist thought this was ACS, he wouldn’t have accepted the patient and the patient would have been transferred to an alternative hospital.
The admission history and physical by Dr. Hospitalist noted prior episodes of chest pain with dancing and suggested that Mr. FW’s history was consistent with chronic angina and that his pain after racing across his lawn to rescue his cat was a demand ischemia phenomenon (not ACS) in a man who was usually sedentary. Dr. Hospitalist further argued that the pain could easily have been GI related because of its burning character, radiation to the throat, and relief with antacids. The patient was pain free at admission without acute changes on his EKG and had had two sets of normal biomarkers before Dr. Hospitalist left for the day. Dr. Hospitalist also argued that a cardiologist wasn’t necessary unless Mr. FW had a positive stress test the following morning.
Unfortunately, Dr. Hospitalist did not take a thorough and comprehensive history regarding Mr. FW’s chest discomfort on the day of admission. Dr. Hospitalist appeared to pay far more attention to Mr. FW’s symptoms on the previous day when he was trying to rescue his cat. On the day of admission, Mr. FW developed chest discomfort while simply walking in the grocery store with his wife. They immediately went to see their primary care physician, who obtained an EKG in the office while Mr. FW was having symptoms.
The EKG showed deeper ST depression with new T-wave inversions in the precordial leads, compared with the EKG performed at the ED several hours later. In addition, the pain lasted for almost 50 minutes, including the time during which he was driving (almost at rest) on the way to the ED. The widow’s deposition also confirmed that Mr. FW’s occasional chest discomfort while dancing the polka was not typical cardiac chest pain. The widow further confirmed that Mr. FW, despite a history of low back pain, was quite active and did not routinely experience exertional chest symptoms.
Conclusion:
Hospitalists are frequently called upon to "rule out MI." It is important, however, to distinguish patients with atypical, noncardiac chest pain from those with typical cardiac chest pain.
Patients with atypical chest pain are being admitted for observation and to rule in or rule out whether their symptoms are cardiac or not. Patients admitted with a history of typical cardiac chest pain, regardless of whether they are pain free at the time of admission, should be treated for ACS until they can receive a diagnostic cardiac catheterization or further risk stratification by a cardiologist. The jury recognized the failure of Dr. Hospitalist to perform a thorough and adequate history in this case.
The case in question occurred in a non–tort reform state. As such, there were no limits on noneconomic damages (in other words, pain and suffering). A judgment was rendered for the widow in this case with damages in the amount of $1 million.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Beyond the Scope
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
The story:
Mrs. AP was a 48-year-old woman who developed painless hematemesis after drinking a glass of milk during dinner. She had a past history of peptic ulcer disease with a bleeding ulcer 3 years ago that required hospitalization. Her past history was otherwise unremarkable and she denied known liver disease or excessive alcohol intake. Her family called for an ambulance as Mrs. AP felt like she was going to pass out. Her systolic blood pressures in the field were 85-90 mm Hg with heart rates above 100 bpm. Intravenous saline was initiated before arrival to the emergency department.
The ED triage nurse recorded a blood pressure of 91/57 mm Hg with a heart rate of 91 bpm. The nurses documented that they cleaned up Mrs. AP, as she had blood on her nose, face, and hands. The ED physician assessed Mrs. AP and noted that she suffered hematemesis followed by presyncope. There was minimal epigastric tenderness on examination. Labs were drawn and Mrs. AP remained on normal saline at 250 cc/hour. A short time later, the nurses document that Mrs. AP had a large brown stool.
Mrs. AP’s lab results returned the following: white blood count 16 K/L, hemoglobin (Hgb) 10 g/dL, and an INR 1.36. Electrolytes were normal except for serum bicarbonate of 15 mmol/L. Mrs. AP’s blood pressures were still running in the 90s/50s mm Hg with IV saline. The ED physician called Dr. GI for admission, but Dr. GI deferred to be primary and asked that the hospitalist on call be contacted. Over the next 2 hours, Mrs. AP remained in the ED. Orthostatics were ordered and were documented to be normal, despite a blood pressure that remained in the low 90s/50s mm Hg. The final blood pressure recording for Mrs. AP in the ED was 101/57 mmHg with a heart rate of 98 bpm. The ED physician specifically documented that he had performed a tilt test that was negative.
A little after midnight, Dr. Hospitalist saw Mrs. AP for the admission history and physical. Dr. Hospitalist noted the last set of vitals in the ED and described Mrs. AP as "hemodynamically stable." Dr. Hospitalist ordered vital signs per routine (Q4 hrs on medical telemetry), Hgb/Hct checks every 4 hours, an intravenous proton pump inhibitor, and continued IV fluid support. His plan of care noted that "GI was consulted and they will see the patient. ... I talked and discussed case and agree with plan."
At 3 a.m., Mrs. AP’s Hgb of 8 g/dL was reported to the nursing floor charge nurse. Her blood pressure and heart rate at that time were 141/62 mm Hg and 82 bpm, respectively. Approximately an hour later, Mrs. AP is complaining of nausea. Shortly after 5 a.m., Mrs. AP suffers a large-volume hematemesis with aspiration in the presence of her nurse. Her oxygen saturation dropped precipitously, and she went into cardiopulmonary arrest. Dr. Hospitalist was on the floor and responded immediately to run the code. Mrs. AP was intubated and a nasogastric tube was placed, which demonstrated a large volume of bright-red blood. Mrs. AP regained her pulse and stabilized briefly. A blood transfusion was initiated, but Mrs. AP lost her pulse again and she was unable to be resuscitated. Mrs. AP was pronounced dead at 6:30 a.m.
The complaint:
Mrs. AP’s husband quickly filed a negligent/wrongful death claim following her death. The negligence claim highlighted that her initial Hgb of 10 g/dL in the ED was already indicative of a significant bleed as she had received almost two liters of IV fluid in the field before ED arrival. The claim further explained that her Hgb of 8 g/dL at 3 a.m. confirmed an ongoing bleed that was being ignored. In summary, the claim alleged negligence on behalf of the ED physician, Dr. GI, and Dr. Hospitalist for failing to appreciate the significance of her bleed, for not placing her in the ICU with invasive monitoring, for not initiating oxygen, for not transfusing Mrs. AP after her labs demonstrated acute blood loss anemia in the face of hypotension, and for failing to emergently perform upper endoscopy to identify and treat her bleeding source.
Scientific principles:
The goal for the initial evaluation of an upper GI bleed is to assess the severity of the bleed, identify potential sources of the bleed, and determine if there are conditions present that may affect subsequent management. All patients with hemodynamic instability or active bleeding should be admitted to an ICU for resuscitation and close observation. Oxygen therapy should also be provided. Whether all patients with suspected acute upper GI bleeding require NGT placement is controversial, in part, because studies have failed to demonstrate a benefit with regard to clinical outcomes. More often, NGT lavage is used when it is unclear if a patient has ongoing bleeding and thus might benefit from an early endoscopy. Early endoscopy (within 24 hours) is recommended for most patients with acute UGI bleeding, though whether early endoscopy affects outcomes and resource utilization is unsettled. Studies have reached variable conclusions when determining whether the application of early endoscopy for risk stratification and treatment reduces resource utilization or affects patient outcomes.
Complaint rebuttal and discussion:
The defendants’ theory of the case was that Mrs. AP suffered an upper GI bleed prior to arrival to the ED that stopped bleeding. While in the ED, her vital signs and general condition improved, and there was no indication for early endoscopy as she was not orthostatic and her hemoglobin was not less than 10 g/dL. Her rebleed, while regrettable, was too big to be resuscitated. ICU care would not have changed the outcome, as Mrs. AP suffered hematemesis and aspiration in the presence of her nurse with immediate physician response.
The medical chart, however, clearly supported the proposition that Mrs. AP was hemodynamically unstable from the start. The plaintiff GI expert opined that had Mrs. AP received early endoscopy with or without sclerotherapy, Mrs. AP would have been further risk stratified to the extent that NGT placement would have been considered and/or therapy would more likely than not have prevented the subsequent large-volume hematemesis and aspiration.
Conclusion:
The scientific principles confirm that Mrs. AP should have been admitted to the ICU with closer monitoring and oxygen therapy. However, the scientific principles also refute the notion that blood transfusion, NGT lavage, or early endoscopy would have made any difference in the outcome. In hindsight, these interventions may have saved Mrs. AP’s life. But taking the facts known to the providers at the time, the case is less clear. At the time of admission, Dr. Hospitalist would have been well served to call Dr. GI to confirm and document the plan of care. According to deposition testimony, Dr. Hospitalist never spoke with Dr. GI. Such a conversation regarding the criteria for early endoscopy would have gone a long way to eliminating Dr. Hospitalist from this case at the outset. Hospitalists do have the right to rely on specialists, but in the middle of the night, we are often on our own and will be held to a "reasonable physician" standard. Dr. Hospitalist had access to the patient and the medical record – Dr. GI did not. A documented discussion with Dr. GI may have provided a better defense for Dr. Hospitalist. Ultimately, despite the issues regarding causation and the prevailing scientific principles, this case was settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
The questionable discharge
Story:
Mrs. EG was a 71-year-old woman who presented to her community hospital emergency department with complaints of 2-3 weeks of muscle weakness making it difficult to go up and down the stairs. She also complained of nonspecific abdominal discomfort with nausea, and a recent rash for which she had received corticosteroids (prednisone 10 mg daily for 1 week). Her medical history included chronic obstructive pulmonary disease with active tobacco abuse, hypertension, and hyperlipidemia. Her simvastatin had been recently discontinued by her primary care physician as a result of mildly elevated liver enzymes discovered about 4 weeks prior to her current presentation. Her medications upon presentation included a fluticasone/salmeterol inhaler, amlodipine, and hydrochlorothiazide. In the ED, the laboratory studies revealed multiple abnormalities including hyponatremia (sodium, 128 mmol/L), a low serum bicarbonate (23 mmol/L) level, thrombocytopenia (platelets, 136,000/mcL), and elevated creatine kinase (2,035 U/L) and liver enzymes (AST 245 U/L and ALT 268 U/L).
Mrs. EG was admitted for further management to Dr. Hospitalist-1 (H1).
Dr. H1 ordered imaging studies and a battery of laboratory tests. The diuretic was discontinued and intravenous hydration provided. He consulted neurology, rheumatology, and gastroenterology to aid in his evaluation. Mrs. EG was ruled out for myocardial infarction/myocarditis, and she had a CT of the abdomen/pelvis with contrast that was normal. Mrs. EG was not febrile and her blood cultures were negative. Routine primary care cancer screening was normal. Coagulation tests, thyroid-stimulating hormone level, erythrocyte sedimentation rate, C-reactive protein level, serum osmolarity, and urinalysis testing were normal. Serum aldolase was elevated 3x normal. Mrs. EG ’s muscle weakness combined with her creatine kinase, liver transaminase, and serum aldolase elevations were consistent with an inflammatory myositis. Dermatomyositis, SLE, and viral myositis with rhabdomyolysis were also a consideration but thought to be less likely. Additional neuromuscular testing was recommended by both neurology and rheumatology (electromyogram and a muscle biopsy), and both consultants felt that these tests could be safely performed in a facilitated fashion in the outpatient setting. Empiric steroid therapy for myositis was not recommended out of concern that it would limit the interpretation of the muscle biopsy. Mrs. EG qualified for skilled nursing facility care based on her physical therapy assessment; however, she declined this recommendation in favor of going home with her family.
Dr. H1 ultimately discharged Mrs. EG home on hospital day 3 without a final diagnosis, although her work-up and evaluation were still proceeding as an outpatient with a presumed autoimmune myositis. She did have abnormalities (sodium, 127 mmol/L; HCO3, 18 mmol/L; platelets, 106,000/mcL) on her morning labs. Mrs. EG left the hospital with her daughters at approximately 4 p.m.
Ten hours later, Mrs. EG returned to the hospital with profound weakness, but also worsening nausea, more diffuse and severe abdominal pain, and new complaints of shortness of breath, diarrhea, dizziness, cold sweats, and associated hypotension. Dr. Hospitalist-2 readmitted Mrs. EG, and at the time of the initial assessment and despite intravenous fluid support, Mrs. EG was hypotensive (92/59 mm Hg) with acute kidney injury (serum creatinine, 1.9 mg/dL with a baseline value of 1.0 mg/dL). Empiric antibiotics were ordered along with additional imaging studies. There was no evidence of bleeding. Unfortunately, later that morning, Mrs. EG had a respiratory arrest (HCO3, 15 mmol/L; arterial pH, 7.1). Over the next 24 hours, Mrs. EG went on to suffer multiorgan dysfunction and refractory shock, and ultimately died 5 days after her initial presentation to the hospital. Diffuse ischemic colitis was found on autopsy.
Complaint:
Three months after Mrs. EG died, the daughters filed a lawsuit on behalf of the estate for wrongful death. They alleged that Mrs. EG was discharged prematurely, as evidenced by her abnormal laboratory values on the day of discharge, the absence of a definitive discharge diagnosis, and readmission and death just 10 hours and 2 days, respectively, following her hospital release. They asserted that Mrs. EG more likely than not had an underlying endocrinopathy (such as adrenal insufficiency) and if she was to be discharged, empiric steroids should have been given to prevent her from going into adrenal crisis and shock. Had Dr. H1 kept Mrs. EG in the hospital, her condition would have been monitored, and she would have had empiric therapy with steroids and intravenous fluids before she developed hypotension and shock and the ischemic colitis that resulted in systemic acidemia and death. Furthermore, Dr. H1 discharged Mrs. EG without consideration for endocrinopathy, and this was a breach in the standard of care. Had Dr. H1 considered adrenal insufficiency, he would not have discharged Mrs. EG until the diagnosis was confirmed and the patient appropriately treated.
Scientific principles:
The decision regarding the need for acute hospital care is a combination of the acuity of the patient’s illness and the intensity of the treatment that is to be provided. Similarly, the discharge decision is related to satisfying the reason for admission. A safe discharge home typically requires patients to have the ability to perform basic activities of daily living independently or the presence of qualified family/personnel to provide assistance with such activities. There should also be assurance that the patient is able to obtain food and medications independently or with assistance from family or friends.
A final diagnosis or completely normal labs are not required for hospital discharge unless there are foreseeable consequences that such uncertainty or the degree and type of laboratory abnormality would lead to patient harm.
Complaint rebuttal and discussion:
Mrs. EG presented with a complex clinical picture at the outset for which a unifying diagnosis was uncertain. She was admitted for further evaluation and treatment, both of which she received. She was seen by several consultants and had numerous radiographic and laboratory tests. Dr. H1 testified that he considered secondary adrenal insufficiency as a cause for some of Mrs. EG’s complaints and her laboratory abnormalities (despite the historical lack of steroid exposure to the degree that one would expect to see secondary adrenal impairment); however, secondary adrenal insufficiency would not explain Mrs. EG’s thrombocytopenia or elevated serum aldolase. In addition, hypotension is associated with primary adrenal insufficiency. Mrs. EG did not demonstrate hypotension at any point in her first hospital stay. On the morning of discharge, Mrs. EG had a normal blood pressure (124/72 mm Hg) and heart rate (81 beats/min) without intravenous fluid support. Mrs. EG was afebrile with little evidence for systemic infection; her WBC was normal. She did not have diarrhea, cold sweats, or progressive abdominal complaints prior to her discharge. Her weakness was reasonably attributed to her documented myositis. In addition, Dr. H1 ordered a physical therapy assessment to evaluate Mrs. EG’s functional activities of daily living and to determine the need for inpatient rehabilitation prior to her discharge. The physical therapy assessment was limited as Mrs. EG declined to ambulate.
Despite Mrs. EG’s concerns about being discharged and her complaints of ongoing weakness, Mrs. EG herself was not interested in inpatient rehabilitation (that is, transfer to a skilled nursing facility) that would have provided a greater level of monitoring as opposed to going home. Further, the nursing staff documented that Mrs. EG was comfortable and resting in bed approximately 1 hour before she left the hospital.
The autopsy concluded that Mrs. EG died of severe systemic acidemia resulting from ischemic colitis secondary to profound hypotension. However, her ischemic colitis may have been the sole cause of the hypotension (via translocation of gram-negative bacteria and resulting sepsis) or may have resulted from it (hypoperfusion of the bowel, ischemia, and systemic acidemia). It is unlikely that her hypotension was due to adrenal crisis, as no mechanism for primary adrenal insufficiency was found at autopsy. In fact, the pathologist noted that the adrenal glands were normal (thus, autoimmune adrenalitis was ruled out).
Mrs. EG was discharged with laboratory abnormalities, but the differential diagnosis for these abnormalities did not include an immediately life-threatening entity. Dr. H1 had no basis for which to foresee Mrs. EG ’s return to the ED less than 10 hours later.
Conclusion:
Patients are discharged with laboratory abnormalities all the time. Patients have chronic conditions, and most patients will go home with laboratory abnormalities that may be unrelated to the reason for hospital admission. Hospitalists typically deal with the primary reason for admission, and once that is satisfied, the patient is transitioned to a lower level of care. However, all hospitalists need to recognize that abnormal vital signs, physical findings, or laboratory tests should be explained in the discharge summary.
Better documentation of the reason for discharge and the explanation and consideration of abnormal findings will protect the hospitalist from unnecessary litigation. Following a thorough expert review on behalf of the defense and a subsequent report outlining the questionable causation, this case was dropped without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Story:
Mrs. EG was a 71-year-old woman who presented to her community hospital emergency department with complaints of 2-3 weeks of muscle weakness making it difficult to go up and down the stairs. She also complained of nonspecific abdominal discomfort with nausea, and a recent rash for which she had received corticosteroids (prednisone 10 mg daily for 1 week). Her medical history included chronic obstructive pulmonary disease with active tobacco abuse, hypertension, and hyperlipidemia. Her simvastatin had been recently discontinued by her primary care physician as a result of mildly elevated liver enzymes discovered about 4 weeks prior to her current presentation. Her medications upon presentation included a fluticasone/salmeterol inhaler, amlodipine, and hydrochlorothiazide. In the ED, the laboratory studies revealed multiple abnormalities including hyponatremia (sodium, 128 mmol/L), a low serum bicarbonate (23 mmol/L) level, thrombocytopenia (platelets, 136,000/mcL), and elevated creatine kinase (2,035 U/L) and liver enzymes (AST 245 U/L and ALT 268 U/L).
Mrs. EG was admitted for further management to Dr. Hospitalist-1 (H1).
Dr. H1 ordered imaging studies and a battery of laboratory tests. The diuretic was discontinued and intravenous hydration provided. He consulted neurology, rheumatology, and gastroenterology to aid in his evaluation. Mrs. EG was ruled out for myocardial infarction/myocarditis, and she had a CT of the abdomen/pelvis with contrast that was normal. Mrs. EG was not febrile and her blood cultures were negative. Routine primary care cancer screening was normal. Coagulation tests, thyroid-stimulating hormone level, erythrocyte sedimentation rate, C-reactive protein level, serum osmolarity, and urinalysis testing were normal. Serum aldolase was elevated 3x normal. Mrs. EG ’s muscle weakness combined with her creatine kinase, liver transaminase, and serum aldolase elevations were consistent with an inflammatory myositis. Dermatomyositis, SLE, and viral myositis with rhabdomyolysis were also a consideration but thought to be less likely. Additional neuromuscular testing was recommended by both neurology and rheumatology (electromyogram and a muscle biopsy), and both consultants felt that these tests could be safely performed in a facilitated fashion in the outpatient setting. Empiric steroid therapy for myositis was not recommended out of concern that it would limit the interpretation of the muscle biopsy. Mrs. EG qualified for skilled nursing facility care based on her physical therapy assessment; however, she declined this recommendation in favor of going home with her family.
Dr. H1 ultimately discharged Mrs. EG home on hospital day 3 without a final diagnosis, although her work-up and evaluation were still proceeding as an outpatient with a presumed autoimmune myositis. She did have abnormalities (sodium, 127 mmol/L; HCO3, 18 mmol/L; platelets, 106,000/mcL) on her morning labs. Mrs. EG left the hospital with her daughters at approximately 4 p.m.
Ten hours later, Mrs. EG returned to the hospital with profound weakness, but also worsening nausea, more diffuse and severe abdominal pain, and new complaints of shortness of breath, diarrhea, dizziness, cold sweats, and associated hypotension. Dr. Hospitalist-2 readmitted Mrs. EG, and at the time of the initial assessment and despite intravenous fluid support, Mrs. EG was hypotensive (92/59 mm Hg) with acute kidney injury (serum creatinine, 1.9 mg/dL with a baseline value of 1.0 mg/dL). Empiric antibiotics were ordered along with additional imaging studies. There was no evidence of bleeding. Unfortunately, later that morning, Mrs. EG had a respiratory arrest (HCO3, 15 mmol/L; arterial pH, 7.1). Over the next 24 hours, Mrs. EG went on to suffer multiorgan dysfunction and refractory shock, and ultimately died 5 days after her initial presentation to the hospital. Diffuse ischemic colitis was found on autopsy.
Complaint:
Three months after Mrs. EG died, the daughters filed a lawsuit on behalf of the estate for wrongful death. They alleged that Mrs. EG was discharged prematurely, as evidenced by her abnormal laboratory values on the day of discharge, the absence of a definitive discharge diagnosis, and readmission and death just 10 hours and 2 days, respectively, following her hospital release. They asserted that Mrs. EG more likely than not had an underlying endocrinopathy (such as adrenal insufficiency) and if she was to be discharged, empiric steroids should have been given to prevent her from going into adrenal crisis and shock. Had Dr. H1 kept Mrs. EG in the hospital, her condition would have been monitored, and she would have had empiric therapy with steroids and intravenous fluids before she developed hypotension and shock and the ischemic colitis that resulted in systemic acidemia and death. Furthermore, Dr. H1 discharged Mrs. EG without consideration for endocrinopathy, and this was a breach in the standard of care. Had Dr. H1 considered adrenal insufficiency, he would not have discharged Mrs. EG until the diagnosis was confirmed and the patient appropriately treated.
Scientific principles:
The decision regarding the need for acute hospital care is a combination of the acuity of the patient’s illness and the intensity of the treatment that is to be provided. Similarly, the discharge decision is related to satisfying the reason for admission. A safe discharge home typically requires patients to have the ability to perform basic activities of daily living independently or the presence of qualified family/personnel to provide assistance with such activities. There should also be assurance that the patient is able to obtain food and medications independently or with assistance from family or friends.
A final diagnosis or completely normal labs are not required for hospital discharge unless there are foreseeable consequences that such uncertainty or the degree and type of laboratory abnormality would lead to patient harm.
Complaint rebuttal and discussion:
Mrs. EG presented with a complex clinical picture at the outset for which a unifying diagnosis was uncertain. She was admitted for further evaluation and treatment, both of which she received. She was seen by several consultants and had numerous radiographic and laboratory tests. Dr. H1 testified that he considered secondary adrenal insufficiency as a cause for some of Mrs. EG’s complaints and her laboratory abnormalities (despite the historical lack of steroid exposure to the degree that one would expect to see secondary adrenal impairment); however, secondary adrenal insufficiency would not explain Mrs. EG’s thrombocytopenia or elevated serum aldolase. In addition, hypotension is associated with primary adrenal insufficiency. Mrs. EG did not demonstrate hypotension at any point in her first hospital stay. On the morning of discharge, Mrs. EG had a normal blood pressure (124/72 mm Hg) and heart rate (81 beats/min) without intravenous fluid support. Mrs. EG was afebrile with little evidence for systemic infection; her WBC was normal. She did not have diarrhea, cold sweats, or progressive abdominal complaints prior to her discharge. Her weakness was reasonably attributed to her documented myositis. In addition, Dr. H1 ordered a physical therapy assessment to evaluate Mrs. EG’s functional activities of daily living and to determine the need for inpatient rehabilitation prior to her discharge. The physical therapy assessment was limited as Mrs. EG declined to ambulate.
Despite Mrs. EG’s concerns about being discharged and her complaints of ongoing weakness, Mrs. EG herself was not interested in inpatient rehabilitation (that is, transfer to a skilled nursing facility) that would have provided a greater level of monitoring as opposed to going home. Further, the nursing staff documented that Mrs. EG was comfortable and resting in bed approximately 1 hour before she left the hospital.
The autopsy concluded that Mrs. EG died of severe systemic acidemia resulting from ischemic colitis secondary to profound hypotension. However, her ischemic colitis may have been the sole cause of the hypotension (via translocation of gram-negative bacteria and resulting sepsis) or may have resulted from it (hypoperfusion of the bowel, ischemia, and systemic acidemia). It is unlikely that her hypotension was due to adrenal crisis, as no mechanism for primary adrenal insufficiency was found at autopsy. In fact, the pathologist noted that the adrenal glands were normal (thus, autoimmune adrenalitis was ruled out).
Mrs. EG was discharged with laboratory abnormalities, but the differential diagnosis for these abnormalities did not include an immediately life-threatening entity. Dr. H1 had no basis for which to foresee Mrs. EG ’s return to the ED less than 10 hours later.
Conclusion:
Patients are discharged with laboratory abnormalities all the time. Patients have chronic conditions, and most patients will go home with laboratory abnormalities that may be unrelated to the reason for hospital admission. Hospitalists typically deal with the primary reason for admission, and once that is satisfied, the patient is transitioned to a lower level of care. However, all hospitalists need to recognize that abnormal vital signs, physical findings, or laboratory tests should be explained in the discharge summary.
Better documentation of the reason for discharge and the explanation and consideration of abnormal findings will protect the hospitalist from unnecessary litigation. Following a thorough expert review on behalf of the defense and a subsequent report outlining the questionable causation, this case was dropped without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Story:
Mrs. EG was a 71-year-old woman who presented to her community hospital emergency department with complaints of 2-3 weeks of muscle weakness making it difficult to go up and down the stairs. She also complained of nonspecific abdominal discomfort with nausea, and a recent rash for which she had received corticosteroids (prednisone 10 mg daily for 1 week). Her medical history included chronic obstructive pulmonary disease with active tobacco abuse, hypertension, and hyperlipidemia. Her simvastatin had been recently discontinued by her primary care physician as a result of mildly elevated liver enzymes discovered about 4 weeks prior to her current presentation. Her medications upon presentation included a fluticasone/salmeterol inhaler, amlodipine, and hydrochlorothiazide. In the ED, the laboratory studies revealed multiple abnormalities including hyponatremia (sodium, 128 mmol/L), a low serum bicarbonate (23 mmol/L) level, thrombocytopenia (platelets, 136,000/mcL), and elevated creatine kinase (2,035 U/L) and liver enzymes (AST 245 U/L and ALT 268 U/L).
Mrs. EG was admitted for further management to Dr. Hospitalist-1 (H1).
Dr. H1 ordered imaging studies and a battery of laboratory tests. The diuretic was discontinued and intravenous hydration provided. He consulted neurology, rheumatology, and gastroenterology to aid in his evaluation. Mrs. EG was ruled out for myocardial infarction/myocarditis, and she had a CT of the abdomen/pelvis with contrast that was normal. Mrs. EG was not febrile and her blood cultures were negative. Routine primary care cancer screening was normal. Coagulation tests, thyroid-stimulating hormone level, erythrocyte sedimentation rate, C-reactive protein level, serum osmolarity, and urinalysis testing were normal. Serum aldolase was elevated 3x normal. Mrs. EG ’s muscle weakness combined with her creatine kinase, liver transaminase, and serum aldolase elevations were consistent with an inflammatory myositis. Dermatomyositis, SLE, and viral myositis with rhabdomyolysis were also a consideration but thought to be less likely. Additional neuromuscular testing was recommended by both neurology and rheumatology (electromyogram and a muscle biopsy), and both consultants felt that these tests could be safely performed in a facilitated fashion in the outpatient setting. Empiric steroid therapy for myositis was not recommended out of concern that it would limit the interpretation of the muscle biopsy. Mrs. EG qualified for skilled nursing facility care based on her physical therapy assessment; however, she declined this recommendation in favor of going home with her family.
Dr. H1 ultimately discharged Mrs. EG home on hospital day 3 without a final diagnosis, although her work-up and evaluation were still proceeding as an outpatient with a presumed autoimmune myositis. She did have abnormalities (sodium, 127 mmol/L; HCO3, 18 mmol/L; platelets, 106,000/mcL) on her morning labs. Mrs. EG left the hospital with her daughters at approximately 4 p.m.
Ten hours later, Mrs. EG returned to the hospital with profound weakness, but also worsening nausea, more diffuse and severe abdominal pain, and new complaints of shortness of breath, diarrhea, dizziness, cold sweats, and associated hypotension. Dr. Hospitalist-2 readmitted Mrs. EG, and at the time of the initial assessment and despite intravenous fluid support, Mrs. EG was hypotensive (92/59 mm Hg) with acute kidney injury (serum creatinine, 1.9 mg/dL with a baseline value of 1.0 mg/dL). Empiric antibiotics were ordered along with additional imaging studies. There was no evidence of bleeding. Unfortunately, later that morning, Mrs. EG had a respiratory arrest (HCO3, 15 mmol/L; arterial pH, 7.1). Over the next 24 hours, Mrs. EG went on to suffer multiorgan dysfunction and refractory shock, and ultimately died 5 days after her initial presentation to the hospital. Diffuse ischemic colitis was found on autopsy.
Complaint:
Three months after Mrs. EG died, the daughters filed a lawsuit on behalf of the estate for wrongful death. They alleged that Mrs. EG was discharged prematurely, as evidenced by her abnormal laboratory values on the day of discharge, the absence of a definitive discharge diagnosis, and readmission and death just 10 hours and 2 days, respectively, following her hospital release. They asserted that Mrs. EG more likely than not had an underlying endocrinopathy (such as adrenal insufficiency) and if she was to be discharged, empiric steroids should have been given to prevent her from going into adrenal crisis and shock. Had Dr. H1 kept Mrs. EG in the hospital, her condition would have been monitored, and she would have had empiric therapy with steroids and intravenous fluids before she developed hypotension and shock and the ischemic colitis that resulted in systemic acidemia and death. Furthermore, Dr. H1 discharged Mrs. EG without consideration for endocrinopathy, and this was a breach in the standard of care. Had Dr. H1 considered adrenal insufficiency, he would not have discharged Mrs. EG until the diagnosis was confirmed and the patient appropriately treated.
Scientific principles:
The decision regarding the need for acute hospital care is a combination of the acuity of the patient’s illness and the intensity of the treatment that is to be provided. Similarly, the discharge decision is related to satisfying the reason for admission. A safe discharge home typically requires patients to have the ability to perform basic activities of daily living independently or the presence of qualified family/personnel to provide assistance with such activities. There should also be assurance that the patient is able to obtain food and medications independently or with assistance from family or friends.
A final diagnosis or completely normal labs are not required for hospital discharge unless there are foreseeable consequences that such uncertainty or the degree and type of laboratory abnormality would lead to patient harm.
Complaint rebuttal and discussion:
Mrs. EG presented with a complex clinical picture at the outset for which a unifying diagnosis was uncertain. She was admitted for further evaluation and treatment, both of which she received. She was seen by several consultants and had numerous radiographic and laboratory tests. Dr. H1 testified that he considered secondary adrenal insufficiency as a cause for some of Mrs. EG’s complaints and her laboratory abnormalities (despite the historical lack of steroid exposure to the degree that one would expect to see secondary adrenal impairment); however, secondary adrenal insufficiency would not explain Mrs. EG’s thrombocytopenia or elevated serum aldolase. In addition, hypotension is associated with primary adrenal insufficiency. Mrs. EG did not demonstrate hypotension at any point in her first hospital stay. On the morning of discharge, Mrs. EG had a normal blood pressure (124/72 mm Hg) and heart rate (81 beats/min) without intravenous fluid support. Mrs. EG was afebrile with little evidence for systemic infection; her WBC was normal. She did not have diarrhea, cold sweats, or progressive abdominal complaints prior to her discharge. Her weakness was reasonably attributed to her documented myositis. In addition, Dr. H1 ordered a physical therapy assessment to evaluate Mrs. EG’s functional activities of daily living and to determine the need for inpatient rehabilitation prior to her discharge. The physical therapy assessment was limited as Mrs. EG declined to ambulate.
Despite Mrs. EG’s concerns about being discharged and her complaints of ongoing weakness, Mrs. EG herself was not interested in inpatient rehabilitation (that is, transfer to a skilled nursing facility) that would have provided a greater level of monitoring as opposed to going home. Further, the nursing staff documented that Mrs. EG was comfortable and resting in bed approximately 1 hour before she left the hospital.
The autopsy concluded that Mrs. EG died of severe systemic acidemia resulting from ischemic colitis secondary to profound hypotension. However, her ischemic colitis may have been the sole cause of the hypotension (via translocation of gram-negative bacteria and resulting sepsis) or may have resulted from it (hypoperfusion of the bowel, ischemia, and systemic acidemia). It is unlikely that her hypotension was due to adrenal crisis, as no mechanism for primary adrenal insufficiency was found at autopsy. In fact, the pathologist noted that the adrenal glands were normal (thus, autoimmune adrenalitis was ruled out).
Mrs. EG was discharged with laboratory abnormalities, but the differential diagnosis for these abnormalities did not include an immediately life-threatening entity. Dr. H1 had no basis for which to foresee Mrs. EG ’s return to the ED less than 10 hours later.
Conclusion:
Patients are discharged with laboratory abnormalities all the time. Patients have chronic conditions, and most patients will go home with laboratory abnormalities that may be unrelated to the reason for hospital admission. Hospitalists typically deal with the primary reason for admission, and once that is satisfied, the patient is transitioned to a lower level of care. However, all hospitalists need to recognize that abnormal vital signs, physical findings, or laboratory tests should be explained in the discharge summary.
Better documentation of the reason for discharge and the explanation and consideration of abnormal findings will protect the hospitalist from unnecessary litigation. Following a thorough expert review on behalf of the defense and a subsequent report outlining the questionable causation, this case was dropped without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Case: a real pain in the neck
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Story:
Mrs. G was a 66-year-old woman with a 6-month history of cervical radiculopathy. Following a routine preoperative preparation, she presented to the hospital on a Friday morning for an elective right anterior cervical diskectomy with fusion of C5-C6 with Dr. Neurosurgeon 1. She was planning to spend one night in the hospital.
Mrs. G had a past medical history significant for hypertension, type 2 diabetes, and asthma. Her drug allergies included codeine. She took her usual blood pressure medication the morning of surgery and she received a one-time dose of IV cefazolin for surgical site prophylaxis.
The surgery was uncomplicated, and Mrs. G arrived to the post anesthesia care unit around noon that Friday. Her initial postoperative course was uneventful until approximately 24 hours later. Mrs. G was complaining of a sore throat that limited her oral intake to the extent that she was unable to eat or drink anything for breakfast on Saturday morning. Mrs. G also complained of severe peri-incisional and right-sided neck/throat pain that required ongoing use of intravenous opiate analgesics. At 3:30 p.m., Mrs. G is noted by the nurses to have right-sided facial swelling. A cross-covering neurosurgeon (Dr. Neurosurgeon 2) is contacted via phone, and a verbal order is placed for Dr. Hospitalist-Consultant to evaluate the patient.
At 5 p.m. Saturday, Dr. Hospitalist-Consultant saw Mrs. G for a routine consult. At the time of the examination, Mrs. G was wearing a soft cervical collar. Her vital signs were: T 37.9 C, P 110 beats/min, RR 14 breaths/min, BP 150/70 mmHg. She was noted to have right-sided facial swelling with an inability to open the right eye because of swelling of the eyelid. Mrs. G denied difficulty breathing or the sensation of throat closing. There was no swelling of the lips or oral mucosa. The lungs were without wheezing or rales. Mrs. G continued to complain of severe pain at the anterior neck incision site. Dr. Hospitalist-Consultant did not remove the cervical collar to examine the incision.
Dr. Hospitalist-Consultant was unsure of the etiology for Mrs. G’s symptoms, but felt the highest item on the differential diagnosis was some sort of unilateral allergic reaction. He ordered dexamethasone, diphenhydramine, famotidine, and neuro checks every 4 hours.
Mrs. G did not improve, and her IV analgesic requirements continued to increase throughout the night. The following morning, Dr. Neurosurgeon 3 examined Mrs. G and confirmed crepitance of the face and neck. A stat CT of the neck demonstrated massive subcutaneous emphysema. She was emergently taken back to the operating room to repair an esophageal perforation. Unfortunately, a 6-month complicated hospital course ensued, which included six additional surgeries on her head and neck. Mrs. G was ultimately left with permanent right-sided nerve damage with limited use of her right arm and hand.
Complaint:
Approximately 1 year later, Dr. Hospitalist-Consultant and all of the involved neurosurgeons were sued by Mrs. G for medical negligence. Mrs. G essentially asserted a delay in diagnosis of her esophageal perforation and, as a result, the perforation enlarged unnecessarily and required a more complex repair with higher likelihood for postsurgical complications. Specifically, Mrs. G asserted that Dr. Hospitalist-Consultant performed a substandard examination by failing to remove the cervical collar and examine the surgical incision. She further asserted that Dr. Hospitalist-Consultant failed to reasonably appreciate the crepitance on palpation of her facial swelling that must have been present that Saturday. Had Dr. Hospitalist-Consultant performed an assessment within the standard of care, further imaging would have been obtained on Saturday and the esophageal perforation would have been identified 12 hours earlier. In addition, Mrs. G asserted that the dexamethasone was harmful to her and furthered her injury by blunting her immune system to the bacteria that was contaminating her mediastinum.
Scientific principles:
Anterior cervical diskectomy and fusion (ACDF) is the most common used decompressive procedure of the cervical spine. The advantages of ACDF are that it requires little manipulation of the spinal cord or cervical roots and allows for removal of both lateral and midline disk herniation and osteophytes. Disadvantages include a small risk of damage to the carotid artery, trachea, esophagus, or recurrent laryngeal nerve. Allergic drug reactions, including angioedema, can occur following surgery. However, unilateral reactions are atypical, if not case report material. If the face is involved with angioedema, the lips and oral mucosa will usually be affected.
Complaint rebuttal and discussion:
Dr. Hospitalist-Consultant testified that he called the surgeon after the consult and they discussed a "surgical complication" as a possible cause of the symptoms. There was no chart documentation that this call occurred. Although the impression section of the consult note did have "? Surgical complication," Dr. Hospitalist-Consultant did not elaborate further in his notes or during his sworn testimony as to what surgical complications he was considering.
Dr. Neurosurgeon 2 had no memory of this conversation, and he admittedly never saw Mrs. G at all. Dr. Neurosurgeon 2 was covering three hospitals that Saturday, and he was in the operating room at another facility at the time of the initial nurse contact about Mrs. G until about 11 p.m. that night.
Dr. Neurosurgeon 2 did testify that if he had been told about Mrs. G’s clinical exam, he would have asked Dr. Hospitalist-Consultant to obtain a CT of the neck. Dr. Hospitalist-Consultant testified that he did not remove the cervical collar because it was ordered by surgery, and he expected the surgeon to examine the incision. Dr. Hospitalist-Consultant further testified that he was unaware that Dr. Neurosurgeon 2 was not able to come and see Mrs. G. and assumed that Dr. Neurosurgeon 2 would take care of his patient. Dr. Hospitalist-Consultant was adamant that he had palpated Mrs. G’s face and that crepitance was not present.
The plaintiff argued that somebody had the responsibility to fully examine Mrs. G and arrive at the appropriate workup and treatment. The plaintiff was critical of Dr. Hospitalist-Consultant for not checking with the surgeon about removing the collar and not recognizing that he was the only physician that was available to attend to Mrs. G that Saturday afternoon/evening. The plaintiff also found the "allergic reaction" diagnosis unreasonable under the circumstances and the lack of crepitance implausible.
Conclusion:
Hospitalists are frequently asked to see postsurgical patients. In fact, many surgeons routinely consult hospitalists for "postoperative medical management." It is important for both the surgeon and the hospitalist to clarify lines of responsibility. In this case, the hospitalist assumed that the surgeon was going to take care of the "surgical issues." However, the surgeon was expecting Dr. Hospitalist-Consultant to perform a full postsurgical assessment, including knowledge of surgical complications.
Conversations among physicians engaging in surgical co-management should be documented including a delineation of responsibility. Had Dr. Hospitalist-Consultant done this, he may have avoided this lawsuit altogether. Ultimately, the jury in this case did not fault any of the providers as a full defense verdict was returned.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Story:
Mrs. G was a 66-year-old woman with a 6-month history of cervical radiculopathy. Following a routine preoperative preparation, she presented to the hospital on a Friday morning for an elective right anterior cervical diskectomy with fusion of C5-C6 with Dr. Neurosurgeon 1. She was planning to spend one night in the hospital.
Mrs. G had a past medical history significant for hypertension, type 2 diabetes, and asthma. Her drug allergies included codeine. She took her usual blood pressure medication the morning of surgery and she received a one-time dose of IV cefazolin for surgical site prophylaxis.
The surgery was uncomplicated, and Mrs. G arrived to the post anesthesia care unit around noon that Friday. Her initial postoperative course was uneventful until approximately 24 hours later. Mrs. G was complaining of a sore throat that limited her oral intake to the extent that she was unable to eat or drink anything for breakfast on Saturday morning. Mrs. G also complained of severe peri-incisional and right-sided neck/throat pain that required ongoing use of intravenous opiate analgesics. At 3:30 p.m., Mrs. G is noted by the nurses to have right-sided facial swelling. A cross-covering neurosurgeon (Dr. Neurosurgeon 2) is contacted via phone, and a verbal order is placed for Dr. Hospitalist-Consultant to evaluate the patient.
At 5 p.m. Saturday, Dr. Hospitalist-Consultant saw Mrs. G for a routine consult. At the time of the examination, Mrs. G was wearing a soft cervical collar. Her vital signs were: T 37.9 C, P 110 beats/min, RR 14 breaths/min, BP 150/70 mmHg. She was noted to have right-sided facial swelling with an inability to open the right eye because of swelling of the eyelid. Mrs. G denied difficulty breathing or the sensation of throat closing. There was no swelling of the lips or oral mucosa. The lungs were without wheezing or rales. Mrs. G continued to complain of severe pain at the anterior neck incision site. Dr. Hospitalist-Consultant did not remove the cervical collar to examine the incision.
Dr. Hospitalist-Consultant was unsure of the etiology for Mrs. G’s symptoms, but felt the highest item on the differential diagnosis was some sort of unilateral allergic reaction. He ordered dexamethasone, diphenhydramine, famotidine, and neuro checks every 4 hours.
Mrs. G did not improve, and her IV analgesic requirements continued to increase throughout the night. The following morning, Dr. Neurosurgeon 3 examined Mrs. G and confirmed crepitance of the face and neck. A stat CT of the neck demonstrated massive subcutaneous emphysema. She was emergently taken back to the operating room to repair an esophageal perforation. Unfortunately, a 6-month complicated hospital course ensued, which included six additional surgeries on her head and neck. Mrs. G was ultimately left with permanent right-sided nerve damage with limited use of her right arm and hand.
Complaint:
Approximately 1 year later, Dr. Hospitalist-Consultant and all of the involved neurosurgeons were sued by Mrs. G for medical negligence. Mrs. G essentially asserted a delay in diagnosis of her esophageal perforation and, as a result, the perforation enlarged unnecessarily and required a more complex repair with higher likelihood for postsurgical complications. Specifically, Mrs. G asserted that Dr. Hospitalist-Consultant performed a substandard examination by failing to remove the cervical collar and examine the surgical incision. She further asserted that Dr. Hospitalist-Consultant failed to reasonably appreciate the crepitance on palpation of her facial swelling that must have been present that Saturday. Had Dr. Hospitalist-Consultant performed an assessment within the standard of care, further imaging would have been obtained on Saturday and the esophageal perforation would have been identified 12 hours earlier. In addition, Mrs. G asserted that the dexamethasone was harmful to her and furthered her injury by blunting her immune system to the bacteria that was contaminating her mediastinum.
Scientific principles:
Anterior cervical diskectomy and fusion (ACDF) is the most common used decompressive procedure of the cervical spine. The advantages of ACDF are that it requires little manipulation of the spinal cord or cervical roots and allows for removal of both lateral and midline disk herniation and osteophytes. Disadvantages include a small risk of damage to the carotid artery, trachea, esophagus, or recurrent laryngeal nerve. Allergic drug reactions, including angioedema, can occur following surgery. However, unilateral reactions are atypical, if not case report material. If the face is involved with angioedema, the lips and oral mucosa will usually be affected.
Complaint rebuttal and discussion:
Dr. Hospitalist-Consultant testified that he called the surgeon after the consult and they discussed a "surgical complication" as a possible cause of the symptoms. There was no chart documentation that this call occurred. Although the impression section of the consult note did have "? Surgical complication," Dr. Hospitalist-Consultant did not elaborate further in his notes or during his sworn testimony as to what surgical complications he was considering.
Dr. Neurosurgeon 2 had no memory of this conversation, and he admittedly never saw Mrs. G at all. Dr. Neurosurgeon 2 was covering three hospitals that Saturday, and he was in the operating room at another facility at the time of the initial nurse contact about Mrs. G until about 11 p.m. that night.
Dr. Neurosurgeon 2 did testify that if he had been told about Mrs. G’s clinical exam, he would have asked Dr. Hospitalist-Consultant to obtain a CT of the neck. Dr. Hospitalist-Consultant testified that he did not remove the cervical collar because it was ordered by surgery, and he expected the surgeon to examine the incision. Dr. Hospitalist-Consultant further testified that he was unaware that Dr. Neurosurgeon 2 was not able to come and see Mrs. G. and assumed that Dr. Neurosurgeon 2 would take care of his patient. Dr. Hospitalist-Consultant was adamant that he had palpated Mrs. G’s face and that crepitance was not present.
The plaintiff argued that somebody had the responsibility to fully examine Mrs. G and arrive at the appropriate workup and treatment. The plaintiff was critical of Dr. Hospitalist-Consultant for not checking with the surgeon about removing the collar and not recognizing that he was the only physician that was available to attend to Mrs. G that Saturday afternoon/evening. The plaintiff also found the "allergic reaction" diagnosis unreasonable under the circumstances and the lack of crepitance implausible.
Conclusion:
Hospitalists are frequently asked to see postsurgical patients. In fact, many surgeons routinely consult hospitalists for "postoperative medical management." It is important for both the surgeon and the hospitalist to clarify lines of responsibility. In this case, the hospitalist assumed that the surgeon was going to take care of the "surgical issues." However, the surgeon was expecting Dr. Hospitalist-Consultant to perform a full postsurgical assessment, including knowledge of surgical complications.
Conversations among physicians engaging in surgical co-management should be documented including a delineation of responsibility. Had Dr. Hospitalist-Consultant done this, he may have avoided this lawsuit altogether. Ultimately, the jury in this case did not fault any of the providers as a full defense verdict was returned.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.
Medicolegal review has the opportunity to become the morbidity and mortality conference of the modern era. This column presents a case vignette that explores some aspect of medicine and the applicable standard of care. I hope to bring a critical emphasis on how physicians think and make decisions, with the ultimate goal of highlighting the lesson to be learned by all.
The more we share in our collective failures, the less likely we are to repeat those same mistakes.
Story:
Mrs. G was a 66-year-old woman with a 6-month history of cervical radiculopathy. Following a routine preoperative preparation, she presented to the hospital on a Friday morning for an elective right anterior cervical diskectomy with fusion of C5-C6 with Dr. Neurosurgeon 1. She was planning to spend one night in the hospital.
Mrs. G had a past medical history significant for hypertension, type 2 diabetes, and asthma. Her drug allergies included codeine. She took her usual blood pressure medication the morning of surgery and she received a one-time dose of IV cefazolin for surgical site prophylaxis.
The surgery was uncomplicated, and Mrs. G arrived to the post anesthesia care unit around noon that Friday. Her initial postoperative course was uneventful until approximately 24 hours later. Mrs. G was complaining of a sore throat that limited her oral intake to the extent that she was unable to eat or drink anything for breakfast on Saturday morning. Mrs. G also complained of severe peri-incisional and right-sided neck/throat pain that required ongoing use of intravenous opiate analgesics. At 3:30 p.m., Mrs. G is noted by the nurses to have right-sided facial swelling. A cross-covering neurosurgeon (Dr. Neurosurgeon 2) is contacted via phone, and a verbal order is placed for Dr. Hospitalist-Consultant to evaluate the patient.
At 5 p.m. Saturday, Dr. Hospitalist-Consultant saw Mrs. G for a routine consult. At the time of the examination, Mrs. G was wearing a soft cervical collar. Her vital signs were: T 37.9 C, P 110 beats/min, RR 14 breaths/min, BP 150/70 mmHg. She was noted to have right-sided facial swelling with an inability to open the right eye because of swelling of the eyelid. Mrs. G denied difficulty breathing or the sensation of throat closing. There was no swelling of the lips or oral mucosa. The lungs were without wheezing or rales. Mrs. G continued to complain of severe pain at the anterior neck incision site. Dr. Hospitalist-Consultant did not remove the cervical collar to examine the incision.
Dr. Hospitalist-Consultant was unsure of the etiology for Mrs. G’s symptoms, but felt the highest item on the differential diagnosis was some sort of unilateral allergic reaction. He ordered dexamethasone, diphenhydramine, famotidine, and neuro checks every 4 hours.
Mrs. G did not improve, and her IV analgesic requirements continued to increase throughout the night. The following morning, Dr. Neurosurgeon 3 examined Mrs. G and confirmed crepitance of the face and neck. A stat CT of the neck demonstrated massive subcutaneous emphysema. She was emergently taken back to the operating room to repair an esophageal perforation. Unfortunately, a 6-month complicated hospital course ensued, which included six additional surgeries on her head and neck. Mrs. G was ultimately left with permanent right-sided nerve damage with limited use of her right arm and hand.
Complaint:
Approximately 1 year later, Dr. Hospitalist-Consultant and all of the involved neurosurgeons were sued by Mrs. G for medical negligence. Mrs. G essentially asserted a delay in diagnosis of her esophageal perforation and, as a result, the perforation enlarged unnecessarily and required a more complex repair with higher likelihood for postsurgical complications. Specifically, Mrs. G asserted that Dr. Hospitalist-Consultant performed a substandard examination by failing to remove the cervical collar and examine the surgical incision. She further asserted that Dr. Hospitalist-Consultant failed to reasonably appreciate the crepitance on palpation of her facial swelling that must have been present that Saturday. Had Dr. Hospitalist-Consultant performed an assessment within the standard of care, further imaging would have been obtained on Saturday and the esophageal perforation would have been identified 12 hours earlier. In addition, Mrs. G asserted that the dexamethasone was harmful to her and furthered her injury by blunting her immune system to the bacteria that was contaminating her mediastinum.
Scientific principles:
Anterior cervical diskectomy and fusion (ACDF) is the most common used decompressive procedure of the cervical spine. The advantages of ACDF are that it requires little manipulation of the spinal cord or cervical roots and allows for removal of both lateral and midline disk herniation and osteophytes. Disadvantages include a small risk of damage to the carotid artery, trachea, esophagus, or recurrent laryngeal nerve. Allergic drug reactions, including angioedema, can occur following surgery. However, unilateral reactions are atypical, if not case report material. If the face is involved with angioedema, the lips and oral mucosa will usually be affected.
Complaint rebuttal and discussion:
Dr. Hospitalist-Consultant testified that he called the surgeon after the consult and they discussed a "surgical complication" as a possible cause of the symptoms. There was no chart documentation that this call occurred. Although the impression section of the consult note did have "? Surgical complication," Dr. Hospitalist-Consultant did not elaborate further in his notes or during his sworn testimony as to what surgical complications he was considering.
Dr. Neurosurgeon 2 had no memory of this conversation, and he admittedly never saw Mrs. G at all. Dr. Neurosurgeon 2 was covering three hospitals that Saturday, and he was in the operating room at another facility at the time of the initial nurse contact about Mrs. G until about 11 p.m. that night.
Dr. Neurosurgeon 2 did testify that if he had been told about Mrs. G’s clinical exam, he would have asked Dr. Hospitalist-Consultant to obtain a CT of the neck. Dr. Hospitalist-Consultant testified that he did not remove the cervical collar because it was ordered by surgery, and he expected the surgeon to examine the incision. Dr. Hospitalist-Consultant further testified that he was unaware that Dr. Neurosurgeon 2 was not able to come and see Mrs. G. and assumed that Dr. Neurosurgeon 2 would take care of his patient. Dr. Hospitalist-Consultant was adamant that he had palpated Mrs. G’s face and that crepitance was not present.
The plaintiff argued that somebody had the responsibility to fully examine Mrs. G and arrive at the appropriate workup and treatment. The plaintiff was critical of Dr. Hospitalist-Consultant for not checking with the surgeon about removing the collar and not recognizing that he was the only physician that was available to attend to Mrs. G that Saturday afternoon/evening. The plaintiff also found the "allergic reaction" diagnosis unreasonable under the circumstances and the lack of crepitance implausible.
Conclusion:
Hospitalists are frequently asked to see postsurgical patients. In fact, many surgeons routinely consult hospitalists for "postoperative medical management." It is important for both the surgeon and the hospitalist to clarify lines of responsibility. In this case, the hospitalist assumed that the surgeon was going to take care of the "surgical issues." However, the surgeon was expecting Dr. Hospitalist-Consultant to perform a full postsurgical assessment, including knowledge of surgical complications.
Conversations among physicians engaging in surgical co-management should be documented including a delineation of responsibility. Had Dr. Hospitalist-Consultant done this, he may have avoided this lawsuit altogether. Ultimately, the jury in this case did not fault any of the providers as a full defense verdict was returned.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He reported having no relevant financial conflicts.