User login
A deadly chain reaction, on one condition
Story
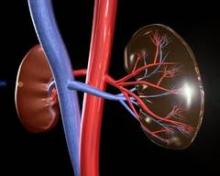
DM was a 60-year-old woman with a history of granulomatosis polyangiitis controlled with cyclophosphamide. She was sent to the hospital as a direct admission by her nephrologist because of worsening renal function and the possibility that DM was suffering from uncontrolled vasculitis. DM was admitted to the hospital by Dr. Hospitalist 1. The history and physical documented that DM was generally weak, but otherwise without specific complaints.
The serum creatinine was 3.89 mg/dL, and coagulation studies were normal. DM’s comorbidities were numerous, including hypertension, coronary artery disease, peripheral vascular disease, and paroxysmal atrial fibrillation. The referring nephrologist had already written orders for a pulsed steroid protocol (Solu-Medrol intravenously for 3 days), in addition to arranging for a renal biopsy by interventional radiology (IR) the following day.
Dr. Hospitalist 1 wrote standard admission orders and made DM nothing per os after midnight. For venous thromboembolism (VTE) prophylaxis, Dr. Hospitalist 1 also wrote for DM to receive mechanical compression to her legs and to begin Lovenox 30 mg subcutaneously daily after the biopsy, only when OK with IR.
The next day, DM was seen in the morning by her nephrologist and Dr. Hospitalist 2 on rounds. Later that afternoon, DM underwent a right renal biopsy under CT guidance by IR. A small hematoma was noted immediately following the procedure. At 8 p.m. that night, DM received 30 mg of Lovenox subcutaneously.
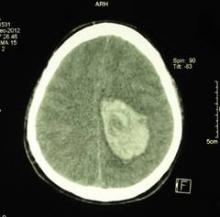
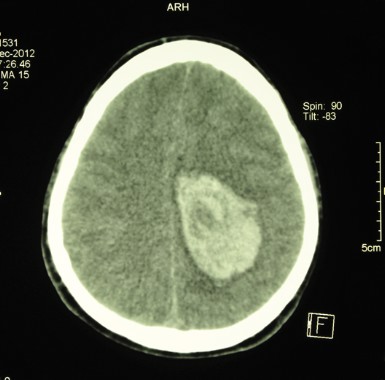
Overnight, DM became tachycardic and complained of right flank pain. Her morning labs drawn at 5 a.m. found a significant drop in her blood count (Hgb, 6.1 mg/dL) and decline in her renal function (serum creatinine, 4.46 mg/dL). A repeat CT of the abdomen and pelvis found an enlarging perinephric hematoma. Dr. Hospitalist 2 immediately moved DM to the ICU and began supportive transfusions.
DM’s blood counts and renal function stabilized over the next 24-36 hrs. However, on the evening of hospital day 4 (ICU day 2), DM experienced shortness of breath followed quickly by a ventricular fibrillation arrest. Telemetry strips before the code demonstrated ST-elevation myocardial infarction. It took almost 45minutes of resuscitation, but DM regained her pulse. At this point, she was now intubated and critically ill. Cardiology was consulted, but given DM’s recent perinephric hematoma, it was felt that she would not tolerate antiplatelet or antithrombotic therapies. Subsequent echocardiogram demonstrated a severely damaged left ventricle from her MI. Even worse, DM went into acute renal failure and shock liver with coagulopathy.
After multiple discussions with the family in the ensuing week, care was ultimately withdrawn and DM passed away.
Complaint
The family understood the bleeding risk of a renal biopsy, but they were upset to learn that DM received blood thinners around the time of her procedure. DM had a previous bleed on Coumadin years earlier, and she even had a "Coumadin allergy" documented in the chart. A lawsuit was filed and both the hospital (employer of the nurses) and Dr. Hospitalist 1 were named in the suit. The complaint alleged that it was substandard for DM to have received Lovenox in this case and that the Lovenox caused the hemorrhage, which in turn led to a myocardial infarction and death.
Scientific principles
Granulomatosis polyangiitis increases the risk for venous and arterial thrombosis. Patients at risk for thrombosis benefit from prophylactic anticoagulation. However, bleeding is the primary complication of renal biopsy and anticoagulation increases that risk. Postbiopsy bleeding can occur into one of three sites: 1) the collecting system (leading to microscopic or gross hematuria); 2) underneath the renal capsule (leading to pressure tamponade and pain); or 3) into the perinephric space (leading to hematoma formation and a possibly large drop in hemoglobin). Most clinically significant bleeding is recognized within 12-24 hours of the biopsy, but bleeding may occur up to several days after the procedure. Anticoagulation should not be used for at least 12-24 hours postbiopsy, and if possible, withholding anticoagulants for a more prolonged period of up to 1 week may be preferable.
Complaint rebuttal and discussion
Discovery in this case confirmed that the original order by Dr. Hospitalist 1 was not transcribed into the medical administration record with any conditions, and IR was not contacted to approve the Lovenox prior to administration. The nurse who gave the Lovenox was simply following the incomplete order that existed on the administration record.
As a result, the hospital settled with the plaintiff early in the process; yet the plaintiff continued to assert that the order itself (whether it was followed properly or not) was substandard and Dr. Hospitalist 1 was also negligent. Dr. Hospitalist 1 defended her Lovenox order as being appropriate and reasonable because DM was at risk for VTE, the dose prescribed was reduced for renal impairment, and it was a conditional order that required approval by interventional radiology prior to medication administration. Dr. Hospitalist 1 was resolute that if her order had just been followed, DM would never have received the medication.
Conclusion
Hospitalists write conditional orders every day. In fact, all "PRN" orders are conditional and presume the use of nursing clinical judgment. However, some conditional orders are directed at other physicians or services (for example, "Discharge the patient if OK with surgery" or "Resume Coumadin if OK with orthopedics").
Often these orders are expedient and typically replace direct communication. But hospitalists should remember that such conditional orders trigger a potential act of commission with nursing as the communication "go-between." There was nothing unreasonable about the conditional order for Lovenox in this case per se. Yet, had this order not been written at all – the chain reaction that subsequently occurred may have been avoided altogether. The jury in this case returned a defense verdict in favor of the hospitalist.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
Story
DM was a 60-year-old woman with a history of granulomatosis polyangiitis controlled with cyclophosphamide. She was sent to the hospital as a direct admission by her nephrologist because of worsening renal function and the possibility that DM was suffering from uncontrolled vasculitis. DM was admitted to the hospital by Dr. Hospitalist 1. The history and physical documented that DM was generally weak, but otherwise without specific complaints.
The serum creatinine was 3.89 mg/dL, and coagulation studies were normal. DM’s comorbidities were numerous, including hypertension, coronary artery disease, peripheral vascular disease, and paroxysmal atrial fibrillation. The referring nephrologist had already written orders for a pulsed steroid protocol (Solu-Medrol intravenously for 3 days), in addition to arranging for a renal biopsy by interventional radiology (IR) the following day.
Dr. Hospitalist 1 wrote standard admission orders and made DM nothing per os after midnight. For venous thromboembolism (VTE) prophylaxis, Dr. Hospitalist 1 also wrote for DM to receive mechanical compression to her legs and to begin Lovenox 30 mg subcutaneously daily after the biopsy, only when OK with IR.
The next day, DM was seen in the morning by her nephrologist and Dr. Hospitalist 2 on rounds. Later that afternoon, DM underwent a right renal biopsy under CT guidance by IR. A small hematoma was noted immediately following the procedure. At 8 p.m. that night, DM received 30 mg of Lovenox subcutaneously.
Overnight, DM became tachycardic and complained of right flank pain. Her morning labs drawn at 5 a.m. found a significant drop in her blood count (Hgb, 6.1 mg/dL) and decline in her renal function (serum creatinine, 4.46 mg/dL). A repeat CT of the abdomen and pelvis found an enlarging perinephric hematoma. Dr. Hospitalist 2 immediately moved DM to the ICU and began supportive transfusions.
DM’s blood counts and renal function stabilized over the next 24-36 hrs. However, on the evening of hospital day 4 (ICU day 2), DM experienced shortness of breath followed quickly by a ventricular fibrillation arrest. Telemetry strips before the code demonstrated ST-elevation myocardial infarction. It took almost 45minutes of resuscitation, but DM regained her pulse. At this point, she was now intubated and critically ill. Cardiology was consulted, but given DM’s recent perinephric hematoma, it was felt that she would not tolerate antiplatelet or antithrombotic therapies. Subsequent echocardiogram demonstrated a severely damaged left ventricle from her MI. Even worse, DM went into acute renal failure and shock liver with coagulopathy.
After multiple discussions with the family in the ensuing week, care was ultimately withdrawn and DM passed away.
Complaint
The family understood the bleeding risk of a renal biopsy, but they were upset to learn that DM received blood thinners around the time of her procedure. DM had a previous bleed on Coumadin years earlier, and she even had a "Coumadin allergy" documented in the chart. A lawsuit was filed and both the hospital (employer of the nurses) and Dr. Hospitalist 1 were named in the suit. The complaint alleged that it was substandard for DM to have received Lovenox in this case and that the Lovenox caused the hemorrhage, which in turn led to a myocardial infarction and death.
Scientific principles
Granulomatosis polyangiitis increases the risk for venous and arterial thrombosis. Patients at risk for thrombosis benefit from prophylactic anticoagulation. However, bleeding is the primary complication of renal biopsy and anticoagulation increases that risk. Postbiopsy bleeding can occur into one of three sites: 1) the collecting system (leading to microscopic or gross hematuria); 2) underneath the renal capsule (leading to pressure tamponade and pain); or 3) into the perinephric space (leading to hematoma formation and a possibly large drop in hemoglobin). Most clinically significant bleeding is recognized within 12-24 hours of the biopsy, but bleeding may occur up to several days after the procedure. Anticoagulation should not be used for at least 12-24 hours postbiopsy, and if possible, withholding anticoagulants for a more prolonged period of up to 1 week may be preferable.
Complaint rebuttal and discussion
Discovery in this case confirmed that the original order by Dr. Hospitalist 1 was not transcribed into the medical administration record with any conditions, and IR was not contacted to approve the Lovenox prior to administration. The nurse who gave the Lovenox was simply following the incomplete order that existed on the administration record.
As a result, the hospital settled with the plaintiff early in the process; yet the plaintiff continued to assert that the order itself (whether it was followed properly or not) was substandard and Dr. Hospitalist 1 was also negligent. Dr. Hospitalist 1 defended her Lovenox order as being appropriate and reasonable because DM was at risk for VTE, the dose prescribed was reduced for renal impairment, and it was a conditional order that required approval by interventional radiology prior to medication administration. Dr. Hospitalist 1 was resolute that if her order had just been followed, DM would never have received the medication.
Conclusion
Hospitalists write conditional orders every day. In fact, all "PRN" orders are conditional and presume the use of nursing clinical judgment. However, some conditional orders are directed at other physicians or services (for example, "Discharge the patient if OK with surgery" or "Resume Coumadin if OK with orthopedics").
Often these orders are expedient and typically replace direct communication. But hospitalists should remember that such conditional orders trigger a potential act of commission with nursing as the communication "go-between." There was nothing unreasonable about the conditional order for Lovenox in this case per se. Yet, had this order not been written at all – the chain reaction that subsequently occurred may have been avoided altogether. The jury in this case returned a defense verdict in favor of the hospitalist.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
Story
DM was a 60-year-old woman with a history of granulomatosis polyangiitis controlled with cyclophosphamide. She was sent to the hospital as a direct admission by her nephrologist because of worsening renal function and the possibility that DM was suffering from uncontrolled vasculitis. DM was admitted to the hospital by Dr. Hospitalist 1. The history and physical documented that DM was generally weak, but otherwise without specific complaints.
The serum creatinine was 3.89 mg/dL, and coagulation studies were normal. DM’s comorbidities were numerous, including hypertension, coronary artery disease, peripheral vascular disease, and paroxysmal atrial fibrillation. The referring nephrologist had already written orders for a pulsed steroid protocol (Solu-Medrol intravenously for 3 days), in addition to arranging for a renal biopsy by interventional radiology (IR) the following day.
Dr. Hospitalist 1 wrote standard admission orders and made DM nothing per os after midnight. For venous thromboembolism (VTE) prophylaxis, Dr. Hospitalist 1 also wrote for DM to receive mechanical compression to her legs and to begin Lovenox 30 mg subcutaneously daily after the biopsy, only when OK with IR.
The next day, DM was seen in the morning by her nephrologist and Dr. Hospitalist 2 on rounds. Later that afternoon, DM underwent a right renal biopsy under CT guidance by IR. A small hematoma was noted immediately following the procedure. At 8 p.m. that night, DM received 30 mg of Lovenox subcutaneously.
Overnight, DM became tachycardic and complained of right flank pain. Her morning labs drawn at 5 a.m. found a significant drop in her blood count (Hgb, 6.1 mg/dL) and decline in her renal function (serum creatinine, 4.46 mg/dL). A repeat CT of the abdomen and pelvis found an enlarging perinephric hematoma. Dr. Hospitalist 2 immediately moved DM to the ICU and began supportive transfusions.
DM’s blood counts and renal function stabilized over the next 24-36 hrs. However, on the evening of hospital day 4 (ICU day 2), DM experienced shortness of breath followed quickly by a ventricular fibrillation arrest. Telemetry strips before the code demonstrated ST-elevation myocardial infarction. It took almost 45minutes of resuscitation, but DM regained her pulse. At this point, she was now intubated and critically ill. Cardiology was consulted, but given DM’s recent perinephric hematoma, it was felt that she would not tolerate antiplatelet or antithrombotic therapies. Subsequent echocardiogram demonstrated a severely damaged left ventricle from her MI. Even worse, DM went into acute renal failure and shock liver with coagulopathy.
After multiple discussions with the family in the ensuing week, care was ultimately withdrawn and DM passed away.
Complaint
The family understood the bleeding risk of a renal biopsy, but they were upset to learn that DM received blood thinners around the time of her procedure. DM had a previous bleed on Coumadin years earlier, and she even had a "Coumadin allergy" documented in the chart. A lawsuit was filed and both the hospital (employer of the nurses) and Dr. Hospitalist 1 were named in the suit. The complaint alleged that it was substandard for DM to have received Lovenox in this case and that the Lovenox caused the hemorrhage, which in turn led to a myocardial infarction and death.
Scientific principles
Granulomatosis polyangiitis increases the risk for venous and arterial thrombosis. Patients at risk for thrombosis benefit from prophylactic anticoagulation. However, bleeding is the primary complication of renal biopsy and anticoagulation increases that risk. Postbiopsy bleeding can occur into one of three sites: 1) the collecting system (leading to microscopic or gross hematuria); 2) underneath the renal capsule (leading to pressure tamponade and pain); or 3) into the perinephric space (leading to hematoma formation and a possibly large drop in hemoglobin). Most clinically significant bleeding is recognized within 12-24 hours of the biopsy, but bleeding may occur up to several days after the procedure. Anticoagulation should not be used for at least 12-24 hours postbiopsy, and if possible, withholding anticoagulants for a more prolonged period of up to 1 week may be preferable.
Complaint rebuttal and discussion
Discovery in this case confirmed that the original order by Dr. Hospitalist 1 was not transcribed into the medical administration record with any conditions, and IR was not contacted to approve the Lovenox prior to administration. The nurse who gave the Lovenox was simply following the incomplete order that existed on the administration record.
As a result, the hospital settled with the plaintiff early in the process; yet the plaintiff continued to assert that the order itself (whether it was followed properly or not) was substandard and Dr. Hospitalist 1 was also negligent. Dr. Hospitalist 1 defended her Lovenox order as being appropriate and reasonable because DM was at risk for VTE, the dose prescribed was reduced for renal impairment, and it was a conditional order that required approval by interventional radiology prior to medication administration. Dr. Hospitalist 1 was resolute that if her order had just been followed, DM would never have received the medication.
Conclusion
Hospitalists write conditional orders every day. In fact, all "PRN" orders are conditional and presume the use of nursing clinical judgment. However, some conditional orders are directed at other physicians or services (for example, "Discharge the patient if OK with surgery" or "Resume Coumadin if OK with orthopedics").
Often these orders are expedient and typically replace direct communication. But hospitalists should remember that such conditional orders trigger a potential act of commission with nursing as the communication "go-between." There was nothing unreasonable about the conditional order for Lovenox in this case per se. Yet, had this order not been written at all – the chain reaction that subsequently occurred may have been avoided altogether. The jury in this case returned a defense verdict in favor of the hospitalist.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
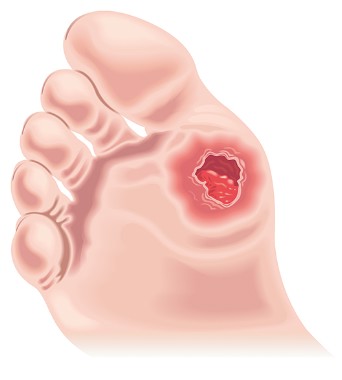
A Diabetic Foot Infection Progresses to Amputation
The Story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
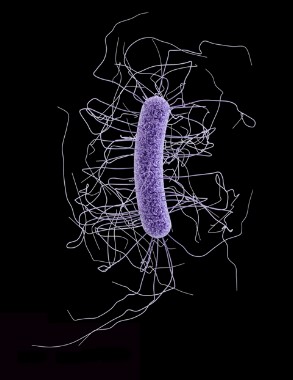
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The Story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The Story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
An unfortunate twist
The story
FR was a 55-year-old woman who developed relatively acute and diffuse upper abdominal pain shortly after finishing dinner with friends at a local restaurant. Over the next 1-2 hours and after returning home, FR’s pain became most severe and was associated with nausea and emesis. FR contacted her daughter, who came over to assist. At approximately 10:30 p.m., FR called for an ambulance and was taken to the nearest emergency department.
On arrival at the ED, FR had a normal blood pressure and heart rate, but complained of 10/10 abdominal pain. An EKG was quickly performed and was normal. On examination, FR was noted by the ED physician as "uncooperative answering questions, rocking in bed moaning." The abdomen was documented as soft but diffusely tender to palpation in all four quadrants. A posteroanterior/lateral chest radiograph (CXR), full blood chemistries, and a complete blood cell count were obtained.
The initial impression by the ED physician was biliary colic, and he also ordered a right upper quadrant ultrasound. In the meantime, FR received a "GI cocktail" (Mylanta, viscous lidocaine, and Donnatal) by mouth, along with intravenous morphine and Zofran. About 1 hour later, FR reported minimal improvement in her symptoms. The CXR, right upper quadrant ultrasound, Chem-12, lipase, and CBC all returned within normal limits.
At this point, the ED physician recommended discharge home with outpatient follow-up. The daughter, who had been with her mother all evening, became very upset and demanded that the patient be admitted because something was obviously wrong with her mother.
The ED physician called Dr. Hospitalist to admit FR for uncontrolled abdominal pain. An hour later, Dr. Hospitalist saw FR on the medical floor, by which time the daughter had left the hospital for home.
FR was lethargic from several doses of hydromorphone, but she was still complaining of severe abdominal pain. Dr. Hospitalist documented that FR had a history of hypertension, hyperlipidemia, anxiety, and depression, along with a gastric lap-band procedure 2 years ago for morbid obesity. FR’s abdomen was noted to be "reasonably soft" with hypoactive bowel sounds. The impression from Dr. Hospitalist was acute postprandial abdominal pain of unclear etiology. The plan included a routine GI consult, a routine plain film of the abdomen to look for evidence of gastric distention, keeping FR nothing per os (NPO), and continuing intravenous fluids and analgesia.
At 8:30 a.m., FR was found unresponsive and a Code Blue was called. Resuscitation efforts confirmed a profound acidemia (pH 6.55), and FR did not survive. FR was last seen by the nurses an hour earlier and had been documented as "sleeping." An autopsy was performed and discovered small bowel necrosis consistent with a small bowel volvulus.
Complaint
The daughter was shocked and upset over the sudden death of her mother. She felt that none of the medical providers took her mother’s complaints seriously because FR had a history of "anxiety." The daughter was particularly angry over the fact that the ED physician actually wanted to discharge FR in the presence of a lethal condition. She followed up with an attorney almost immediately, who had the case reviewed and subsequently filed a lawsuit.
The complaint alleged that the ED physician and Dr. Hospitalist both failed to appropriately image FR’s abdomen with either a plain abdominal radiograph and/or CT scan of the abdomen. The complaint further alleged that had they done so, the small bowel volvulus would have been discovered and successfully treated, preventing FR’s demise.
Scientific principles
Volvulus is a special form of mechanical intestinal obstruction. It results from abnormal twisting of a loop of bowel around the axis of its own mesentery and often results in ischemia or even infarction.
When it occurs in adults, volvulus usually affects the sigmoid colon or the cecum. In contrast, small bowel volvulus is relatively rare. Plain radiography and CT of the abdomen are the most practical and useful diagnostic modalities.
All patients suspected of having complicated bowel obstruction (complete obstruction, closed-loop obstruction, bowel ischemia, necrosis, or perforation) based upon clinical and radiologic examination should be taken to the operating room for abdominal exploration. Failure to identify and treat small bowel volvulus in a timely manner can lead to catastrophic results.
Complaint rebuttal and discussion
The defense in this case focused on the rarity of this condition, along with the limited time window to successfully save FR’s life. The defense argued that while FR was in the window for diagnosis and successful treatment (i.e., 10:30 p.m. until 3 a.m.), all of FR’s vital signs were normal, and her abdominal exam was inconsistent with an acute abdomen.
The plaintiff countered that mechanical bowel obstruction (not necessarily a rare volvulus) was always in the differential diagnosis for acute and severe abdominal pain, and the failure to perform plain radiography of the abdomen was in and of itself negligent. Plaintiff experts opined that had the providers in this case performed plain radiography as the standard of care required, FR’s rare diagnosis would have been discovered, even if by "accident."
Conclusion
Dr. Hospitalist documented a desire to obtain a plain abdominal radiograph, but he ordered it routine and therefore it was never performed prior to FR’s death. Had Dr. Hospitalist obtained the film STAT, more likely than not the volvulus would have been identified well within the window to get FR a surgical consult and to the operating room for treatment.
This case is another example of what turned out to be an incomplete workup from the ED in the setting of "uncontrolled pain" (see previous column). Admission for "pain control" is a red flag for an underlying disorder that has been missed by the initial ED evaluation. In this case, the workup should have reasonably included a plain radiograph of the abdomen. This case was eventually settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
The story
FR was a 55-year-old woman who developed relatively acute and diffuse upper abdominal pain shortly after finishing dinner with friends at a local restaurant. Over the next 1-2 hours and after returning home, FR’s pain became most severe and was associated with nausea and emesis. FR contacted her daughter, who came over to assist. At approximately 10:30 p.m., FR called for an ambulance and was taken to the nearest emergency department.
On arrival at the ED, FR had a normal blood pressure and heart rate, but complained of 10/10 abdominal pain. An EKG was quickly performed and was normal. On examination, FR was noted by the ED physician as "uncooperative answering questions, rocking in bed moaning." The abdomen was documented as soft but diffusely tender to palpation in all four quadrants. A posteroanterior/lateral chest radiograph (CXR), full blood chemistries, and a complete blood cell count were obtained.
The initial impression by the ED physician was biliary colic, and he also ordered a right upper quadrant ultrasound. In the meantime, FR received a "GI cocktail" (Mylanta, viscous lidocaine, and Donnatal) by mouth, along with intravenous morphine and Zofran. About 1 hour later, FR reported minimal improvement in her symptoms. The CXR, right upper quadrant ultrasound, Chem-12, lipase, and CBC all returned within normal limits.
At this point, the ED physician recommended discharge home with outpatient follow-up. The daughter, who had been with her mother all evening, became very upset and demanded that the patient be admitted because something was obviously wrong with her mother.
The ED physician called Dr. Hospitalist to admit FR for uncontrolled abdominal pain. An hour later, Dr. Hospitalist saw FR on the medical floor, by which time the daughter had left the hospital for home.
FR was lethargic from several doses of hydromorphone, but she was still complaining of severe abdominal pain. Dr. Hospitalist documented that FR had a history of hypertension, hyperlipidemia, anxiety, and depression, along with a gastric lap-band procedure 2 years ago for morbid obesity. FR’s abdomen was noted to be "reasonably soft" with hypoactive bowel sounds. The impression from Dr. Hospitalist was acute postprandial abdominal pain of unclear etiology. The plan included a routine GI consult, a routine plain film of the abdomen to look for evidence of gastric distention, keeping FR nothing per os (NPO), and continuing intravenous fluids and analgesia.
At 8:30 a.m., FR was found unresponsive and a Code Blue was called. Resuscitation efforts confirmed a profound acidemia (pH 6.55), and FR did not survive. FR was last seen by the nurses an hour earlier and had been documented as "sleeping." An autopsy was performed and discovered small bowel necrosis consistent with a small bowel volvulus.
Complaint
The daughter was shocked and upset over the sudden death of her mother. She felt that none of the medical providers took her mother’s complaints seriously because FR had a history of "anxiety." The daughter was particularly angry over the fact that the ED physician actually wanted to discharge FR in the presence of a lethal condition. She followed up with an attorney almost immediately, who had the case reviewed and subsequently filed a lawsuit.
The complaint alleged that the ED physician and Dr. Hospitalist both failed to appropriately image FR’s abdomen with either a plain abdominal radiograph and/or CT scan of the abdomen. The complaint further alleged that had they done so, the small bowel volvulus would have been discovered and successfully treated, preventing FR’s demise.
Scientific principles
Volvulus is a special form of mechanical intestinal obstruction. It results from abnormal twisting of a loop of bowel around the axis of its own mesentery and often results in ischemia or even infarction.
When it occurs in adults, volvulus usually affects the sigmoid colon or the cecum. In contrast, small bowel volvulus is relatively rare. Plain radiography and CT of the abdomen are the most practical and useful diagnostic modalities.
All patients suspected of having complicated bowel obstruction (complete obstruction, closed-loop obstruction, bowel ischemia, necrosis, or perforation) based upon clinical and radiologic examination should be taken to the operating room for abdominal exploration. Failure to identify and treat small bowel volvulus in a timely manner can lead to catastrophic results.
Complaint rebuttal and discussion
The defense in this case focused on the rarity of this condition, along with the limited time window to successfully save FR’s life. The defense argued that while FR was in the window for diagnosis and successful treatment (i.e., 10:30 p.m. until 3 a.m.), all of FR’s vital signs were normal, and her abdominal exam was inconsistent with an acute abdomen.
The plaintiff countered that mechanical bowel obstruction (not necessarily a rare volvulus) was always in the differential diagnosis for acute and severe abdominal pain, and the failure to perform plain radiography of the abdomen was in and of itself negligent. Plaintiff experts opined that had the providers in this case performed plain radiography as the standard of care required, FR’s rare diagnosis would have been discovered, even if by "accident."
Conclusion
Dr. Hospitalist documented a desire to obtain a plain abdominal radiograph, but he ordered it routine and therefore it was never performed prior to FR’s death. Had Dr. Hospitalist obtained the film STAT, more likely than not the volvulus would have been identified well within the window to get FR a surgical consult and to the operating room for treatment.
This case is another example of what turned out to be an incomplete workup from the ED in the setting of "uncontrolled pain" (see previous column). Admission for "pain control" is a red flag for an underlying disorder that has been missed by the initial ED evaluation. In this case, the workup should have reasonably included a plain radiograph of the abdomen. This case was eventually settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
The story
FR was a 55-year-old woman who developed relatively acute and diffuse upper abdominal pain shortly after finishing dinner with friends at a local restaurant. Over the next 1-2 hours and after returning home, FR’s pain became most severe and was associated with nausea and emesis. FR contacted her daughter, who came over to assist. At approximately 10:30 p.m., FR called for an ambulance and was taken to the nearest emergency department.
On arrival at the ED, FR had a normal blood pressure and heart rate, but complained of 10/10 abdominal pain. An EKG was quickly performed and was normal. On examination, FR was noted by the ED physician as "uncooperative answering questions, rocking in bed moaning." The abdomen was documented as soft but diffusely tender to palpation in all four quadrants. A posteroanterior/lateral chest radiograph (CXR), full blood chemistries, and a complete blood cell count were obtained.
The initial impression by the ED physician was biliary colic, and he also ordered a right upper quadrant ultrasound. In the meantime, FR received a "GI cocktail" (Mylanta, viscous lidocaine, and Donnatal) by mouth, along with intravenous morphine and Zofran. About 1 hour later, FR reported minimal improvement in her symptoms. The CXR, right upper quadrant ultrasound, Chem-12, lipase, and CBC all returned within normal limits.
At this point, the ED physician recommended discharge home with outpatient follow-up. The daughter, who had been with her mother all evening, became very upset and demanded that the patient be admitted because something was obviously wrong with her mother.
The ED physician called Dr. Hospitalist to admit FR for uncontrolled abdominal pain. An hour later, Dr. Hospitalist saw FR on the medical floor, by which time the daughter had left the hospital for home.
FR was lethargic from several doses of hydromorphone, but she was still complaining of severe abdominal pain. Dr. Hospitalist documented that FR had a history of hypertension, hyperlipidemia, anxiety, and depression, along with a gastric lap-band procedure 2 years ago for morbid obesity. FR’s abdomen was noted to be "reasonably soft" with hypoactive bowel sounds. The impression from Dr. Hospitalist was acute postprandial abdominal pain of unclear etiology. The plan included a routine GI consult, a routine plain film of the abdomen to look for evidence of gastric distention, keeping FR nothing per os (NPO), and continuing intravenous fluids and analgesia.
At 8:30 a.m., FR was found unresponsive and a Code Blue was called. Resuscitation efforts confirmed a profound acidemia (pH 6.55), and FR did not survive. FR was last seen by the nurses an hour earlier and had been documented as "sleeping." An autopsy was performed and discovered small bowel necrosis consistent with a small bowel volvulus.
Complaint
The daughter was shocked and upset over the sudden death of her mother. She felt that none of the medical providers took her mother’s complaints seriously because FR had a history of "anxiety." The daughter was particularly angry over the fact that the ED physician actually wanted to discharge FR in the presence of a lethal condition. She followed up with an attorney almost immediately, who had the case reviewed and subsequently filed a lawsuit.
The complaint alleged that the ED physician and Dr. Hospitalist both failed to appropriately image FR’s abdomen with either a plain abdominal radiograph and/or CT scan of the abdomen. The complaint further alleged that had they done so, the small bowel volvulus would have been discovered and successfully treated, preventing FR’s demise.
Scientific principles
Volvulus is a special form of mechanical intestinal obstruction. It results from abnormal twisting of a loop of bowel around the axis of its own mesentery and often results in ischemia or even infarction.
When it occurs in adults, volvulus usually affects the sigmoid colon or the cecum. In contrast, small bowel volvulus is relatively rare. Plain radiography and CT of the abdomen are the most practical and useful diagnostic modalities.
All patients suspected of having complicated bowel obstruction (complete obstruction, closed-loop obstruction, bowel ischemia, necrosis, or perforation) based upon clinical and radiologic examination should be taken to the operating room for abdominal exploration. Failure to identify and treat small bowel volvulus in a timely manner can lead to catastrophic results.
Complaint rebuttal and discussion
The defense in this case focused on the rarity of this condition, along with the limited time window to successfully save FR’s life. The defense argued that while FR was in the window for diagnosis and successful treatment (i.e., 10:30 p.m. until 3 a.m.), all of FR’s vital signs were normal, and her abdominal exam was inconsistent with an acute abdomen.
The plaintiff countered that mechanical bowel obstruction (not necessarily a rare volvulus) was always in the differential diagnosis for acute and severe abdominal pain, and the failure to perform plain radiography of the abdomen was in and of itself negligent. Plaintiff experts opined that had the providers in this case performed plain radiography as the standard of care required, FR’s rare diagnosis would have been discovered, even if by "accident."
Conclusion
Dr. Hospitalist documented a desire to obtain a plain abdominal radiograph, but he ordered it routine and therefore it was never performed prior to FR’s death. Had Dr. Hospitalist obtained the film STAT, more likely than not the volvulus would have been identified well within the window to get FR a surgical consult and to the operating room for treatment.
This case is another example of what turned out to be an incomplete workup from the ED in the setting of "uncontrolled pain" (see previous column). Admission for "pain control" is a red flag for an underlying disorder that has been missed by the initial ED evaluation. In this case, the workup should have reasonably included a plain radiograph of the abdomen. This case was eventually settled on behalf of the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system. Read past columns at ehospitalistnews.com/Lessons.
A diabetic foot infection progresses to amputation
The story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The story
KL was a 56-year-old man with multiple comorbidities, including obesity, coronary artery disease, hypertension, insulin-dependent diabetes, chronic kidney disease, and dyslipidemia. He presented to Hospital A with fever and chills, along with an open wound on the bottom of his left foot. Laboratory studies revealed a WBC 14,000 cells/mL and a serum creatinine of 3.1 mg/dL. KL was admitted by Dr. Hospitalist for cellulitis and an infected diabetic foot ulcer.
KL was started on intravenous vancomycin and piperacillin/tazobactam and blood cultures were drawn. A bone scan was negative for osteomyelitis. Blood cultures did not grow any bacteria, but a wound culture from his foot ulcer grew Klebsiella. Dr. Hospitalist consulted inpatient podiatry for wound debridement, but KL apparently refused in favor of being seen by his own podiatrist as an outpatient. By hospital day 2, KL was afebrile, eating well, and he was discharged on oral ciprofloxacin later that same day.
Two days after discharge, KL followed up with his primary care physician (PCP). KL was again febrile and his foot ulcer looked worse. The PCP recommended hospitalization with intravenous antibiotics, but KL was reluctant to return to the hospital. The PCP arranged for midline placement and KL was referred to a local wound clinic for intravenous vancomycin to begin the next day. KL remained on the oral ciprofloxacin.
Over the next 3 days, KL received daily intravenous vancomycin at the wound clinic. However, the foot ulcer continued to drain purulent material with associated cellulitis and advancing erythema across the forefoot. The wound nurse contacted the PCP who had sent KL to the emergency department of Hospital B. Laboratory studies revealed a WBC 18,300 cells/mL and a serum creatinine of 2.2 mg/dL. KL was informed that he needed wound debridement and was offered the same podiatrist that he refused at Hospital A. Once again, KL deferred in favor of his own podiatrist who apparently was on vacation. Blood and wound cultures were obtained and KL received a dose of intravenous amoxicillin/sulbactam in the ED, but because of his refusal to receive wound debridement and care at Hospital A or B, he was sent home that same afternoon.
KL left Hospital B and drove 2 hours to the ED of Hospital C. He was immediately admitted and intravenous vancomycin and piperacillin/tazobactam were begun. Plain films of the foot were consistent with osteomyelitis. An MRI of the foot demonstrated cellulitis, myositis, and a forefoot abscess. Within 24 hours of admission, KL developed chest pain and was subsequently ruled-in for a non–ST-elevation MI. KL ended up getting a left heart catheterization, and this delayed surgical debridement of his infected foot. Ultimately, KL did have debridement of his foot, but the infection had an advanced to the point that a below-the-knee amputation was required. Surgical pathology cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Complaint
KL was now facing life without his left leg, and he was angry and felt that the medical system had let him down. A complaint was quickly filed and alleged multiple breaches in the standard of care against multiple providers. The complaint included Dr. Hospitalist and asserted that he failed to obtain an MRI of the left foot from the very start, stopped intravenous vancomycin inappropriately, and failed to obtain infectious disease and orthopedic surgery consults.
The complaint further asserted that the PCP and the ED providers at Hospital B were negligent for not readmitting KL and obtaining infectious disease and orthopedic surgery consults. If the providers in this case had continued intravenous vancomycin throughout his case and otherwise obtained appropriate specialty care, KL’s leg would have been saved.
Scientific principles
Diabetic foot infections are associated with substantial morbidity and mortality. Important risk factors for development of diabetic foot infections include neuropathy, peripheral vascular disease, and poor glycemic control. Most diabetic foot infections are polymicrobial, but MRSA is a common pathogen. Although severe diabetic foot infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
The possibility of osteomyelitis should be considered in diabetic patients with foot wounds associated with signs of infection in the deeper soft tissues and in patients with chronic ulcers. Many patients with confirmed osteomyelitis of the foot benefit from surgical resection.
Complaint rebuttal and discussion
Although Dr. Hospitalist had a negative bone scan result, he should have considered MRSA as a pathogen for KL despite a wound culture growing Klebsiella only. Most experts agreed, however, that it would be pure speculation as to what an MRI would have shown so early in KL’s course and ultimately, Dr. Hospitalist was defensible because KL did have appropriate follow-up just 48 hours after discharge. In fact, more than 21 days from original presentation to his amputation, KL only had 3 days off of intravenous vancomycin.
As a result, defense experts focused on the failure of KL to obtain debridement as the main reason for his injury. Dr. Hospitalist, the PCP and the ED providers at Hospital B, all documented KL’s refusal to allow debridement by a podiatrist other than his own. KL denied this allegation, but the chart was consistent in this regard.
Conclusion
In the era of patient-centered care, patient wishes and preferences are important to integrate into the overall care plan. But when a patient’s wishes and preferences delay or otherwise subvert optimal care, it is vital that the hospitalist document the circumstances in their entirety. Documentation should confirm that the patient has capacity for decision making and that care recommendation benefits, risks for not following said recommendations, and care recommendation alternatives have been fully reviewed.
It is also helpful to have such discussions witnessed by other providers (that is, the nurse) so that the documentation is corroborated. The PCP and Hospital B were dismissed from the case. Hospital A settled with the plaintiff by waiving all hospital charges from his original hospitalization.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
A fatal ‘never event’
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
A tragic transition of care
The story:
JR is a 32-year-old woman with a medical history of juvenile diabetes mellitus and end-stage renal disease on intermittent hemodialysis for the past 2 years. She was admitted to the hospital with shortness of breath and was found to have a large right-sided pleural effusion with loculations. Antibiotics were initiated. On hospital day 2 she underwent a video-assisted thoracoscopy for drainage, lysis of adhesions, and placement of two chest tubes. After returning to the floor from the postanesthesia care unit, JR had difficulty achieving adequate pain control despite a hydromorphone patient-controlled analgesic pump. Additional "as needed" intravenous morphine was ordered for relief. Before going home, the attending internist checked in on JR and discontinued her intravenous fluids (D5 half-normal saline), but wrote to resume her long-acting insulin later that same evening.
At approximately 7:30 p.m., JR was found by the nurse barely breathing. Her pupils were pinpoint and her respiratory rate was only 5 breaths per minute. A code blue was called and a hospitalist responded. A combination of epinephrine, atropine, and naloxone led to a return of consciousness, and JR was never intubated. In fact, the code sheet reflected that after the naloxone, JR was now fully awake, crying, and complaining of right-sided pain.
JR subsequently complained of nausea and began to vomit. Prior to transferring her to the intensive care unit, the hospitalist placed a nasogastric tube and made JR nil per os. To complete JR’s transfer to the ICU, the hospitalist contacted a critical care attending to give report, and then wrote "holding" ICU admission orders.
JR remained on the regular nursing floor for another hour as the ICU prepared for her arrival. Just prior to leaving the floor, JR’s nurse gave her 13 units of glargine insulin as ordered earlier that afternoon by the attending internist.
JR underwent a standard admission assessment upon her arrival at the ICU. The hospitalist "holding admission orders" included regular blood glucose checks and regular insulin coverage on a sliding scale. At midnight, JR’s blood glucose was over 250 mg/dL, and she was administered 6 units of regular insulin. At 5 a.m., another blood glucose was obtained and was recorded as 114 mg/dL. At 7:45 a.m., the new day shift ICU nurse did a complete assessment and noted that JR was lethargic with slurred speech. The critical care consultant rounded on JR at approximately 10 a.m. and also noted a change in mental status. Thirty minutes later, JR became unresponsive to verbal or tactile stimuli. A point-of-care blood glucose was performed and found to be 10 mg/dL. JR was subsequently intubated, but she never regained consciousness again.
She lived for another 2 months before her family decided to stop her dialysis and she passed away.
Complaint:
The family was upset to learn that JR suffered irreversible brain injury from low blood sugar. JR had been a diabetic on insulin all of her life, and the family couldn’t understand how such a thing could happen under the watchful eye of doctors and nurses.
The complaint alleged that there was an egregious failure with respect to communication between the attending physician, the floor nurse, the hospitalist, and the critical care consultant. Specific to the hospitalist, the complaint alleged that the "holding admission orders" should have included intravenous fluids with dextrose and/or explicit instructions to not give the glargine insulin as ordered earlier that same day.
The complaint was also disparaging of the critical care consultant for not recognizing the hypoglycemia earlier, given the mental status changes that JR exhibited.
Scientific principles:
Hypoglycemia can produce a myriad of neurologic signs and symptoms, but usually presents with symptoms of increased epinephrine release (e.g., tremor, diaphoresis) followed by neurologic symptoms that include generalized seizures, bizarre behavior, coma, and focal deficits. In acute severe hypoglycemia, a bolus of 25-50 grams of dextrose should be administered intravenously, followed by a continuous dextrose infusion. Blood glucose concentrations should be measured hourly. Reversal of neurologic symptoms may lag behind normalization of glucose levels.
Complaint rebuttal and discussion
All the health care providers thought their actions were reasonable in this case.
At the time that the attending internist wrote to resume JR’s glargine and stop the dextrose-containing intravenous fluids, JR was awake and was planning to have a light dinner. The floor nurse who gave the glargine later that night testified that she had a valid order to administer the medication.
The hospitalist testified that he was there to respond to emergencies, and that he transferred care of JR to the critical care consultant by verbal report. The critical care consultant acknowledged the verbal handoff from the hospitalist, but doubts there was any discussion regarding JR’s diabetes and was adamant that she was not responsible for JR receiving two doses of insulin (glargine and regular insulin) via the orders of two other physicians before she even had the opportunity to see the patient. The critical care consultant also testified that JR’s mental status change was nonspecific and was reasonably due to the pain medications she was receiving.
The plaintiffs countered with the reality that JR, a 32-year-old woman, died from low blood sugar because she received insulin when she wasn’t allowed to eat or drink – all at the hands of the medical team.
Conclusion:
Much of the attention regarding safe transitions of care is focused on the hospital discharge. Yet discontinuity within hospital walls is frequently associated with medical errors, and communication problems represent the largest category for hospital sentinel events.
The Joint Commission, the World Health Organization, the Institute of Medicine and the National Quality Foundation have all published white paper recommendations regarding the need to improve medical handoffs. Most hospitalists probably see this case as a "system error," and sure enough following this event the hospital overhauled its policies and procedures as they related to ICU transfers. But in the world of medical malpractice, the "system" doesn’t face the jury in litigation.
Although the attending internist was eventually dropped from this case, the hospital, the critical care consultant, and the hospitalist all settled with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The story:
JR is a 32-year-old woman with a medical history of juvenile diabetes mellitus and end-stage renal disease on intermittent hemodialysis for the past 2 years. She was admitted to the hospital with shortness of breath and was found to have a large right-sided pleural effusion with loculations. Antibiotics were initiated. On hospital day 2 she underwent a video-assisted thoracoscopy for drainage, lysis of adhesions, and placement of two chest tubes. After returning to the floor from the postanesthesia care unit, JR had difficulty achieving adequate pain control despite a hydromorphone patient-controlled analgesic pump. Additional "as needed" intravenous morphine was ordered for relief. Before going home, the attending internist checked in on JR and discontinued her intravenous fluids (D5 half-normal saline), but wrote to resume her long-acting insulin later that same evening.
At approximately 7:30 p.m., JR was found by the nurse barely breathing. Her pupils were pinpoint and her respiratory rate was only 5 breaths per minute. A code blue was called and a hospitalist responded. A combination of epinephrine, atropine, and naloxone led to a return of consciousness, and JR was never intubated. In fact, the code sheet reflected that after the naloxone, JR was now fully awake, crying, and complaining of right-sided pain.
JR subsequently complained of nausea and began to vomit. Prior to transferring her to the intensive care unit, the hospitalist placed a nasogastric tube and made JR nil per os. To complete JR’s transfer to the ICU, the hospitalist contacted a critical care attending to give report, and then wrote "holding" ICU admission orders.
JR remained on the regular nursing floor for another hour as the ICU prepared for her arrival. Just prior to leaving the floor, JR’s nurse gave her 13 units of glargine insulin as ordered earlier that afternoon by the attending internist.
JR underwent a standard admission assessment upon her arrival at the ICU. The hospitalist "holding admission orders" included regular blood glucose checks and regular insulin coverage on a sliding scale. At midnight, JR’s blood glucose was over 250 mg/dL, and she was administered 6 units of regular insulin. At 5 a.m., another blood glucose was obtained and was recorded as 114 mg/dL. At 7:45 a.m., the new day shift ICU nurse did a complete assessment and noted that JR was lethargic with slurred speech. The critical care consultant rounded on JR at approximately 10 a.m. and also noted a change in mental status. Thirty minutes later, JR became unresponsive to verbal or tactile stimuli. A point-of-care blood glucose was performed and found to be 10 mg/dL. JR was subsequently intubated, but she never regained consciousness again.
She lived for another 2 months before her family decided to stop her dialysis and she passed away.
Complaint:
The family was upset to learn that JR suffered irreversible brain injury from low blood sugar. JR had been a diabetic on insulin all of her life, and the family couldn’t understand how such a thing could happen under the watchful eye of doctors and nurses.
The complaint alleged that there was an egregious failure with respect to communication between the attending physician, the floor nurse, the hospitalist, and the critical care consultant. Specific to the hospitalist, the complaint alleged that the "holding admission orders" should have included intravenous fluids with dextrose and/or explicit instructions to not give the glargine insulin as ordered earlier that same day.
The complaint was also disparaging of the critical care consultant for not recognizing the hypoglycemia earlier, given the mental status changes that JR exhibited.
Scientific principles:
Hypoglycemia can produce a myriad of neurologic signs and symptoms, but usually presents with symptoms of increased epinephrine release (e.g., tremor, diaphoresis) followed by neurologic symptoms that include generalized seizures, bizarre behavior, coma, and focal deficits. In acute severe hypoglycemia, a bolus of 25-50 grams of dextrose should be administered intravenously, followed by a continuous dextrose infusion. Blood glucose concentrations should be measured hourly. Reversal of neurologic symptoms may lag behind normalization of glucose levels.
Complaint rebuttal and discussion
All the health care providers thought their actions were reasonable in this case.
At the time that the attending internist wrote to resume JR’s glargine and stop the dextrose-containing intravenous fluids, JR was awake and was planning to have a light dinner. The floor nurse who gave the glargine later that night testified that she had a valid order to administer the medication.
The hospitalist testified that he was there to respond to emergencies, and that he transferred care of JR to the critical care consultant by verbal report. The critical care consultant acknowledged the verbal handoff from the hospitalist, but doubts there was any discussion regarding JR’s diabetes and was adamant that she was not responsible for JR receiving two doses of insulin (glargine and regular insulin) via the orders of two other physicians before she even had the opportunity to see the patient. The critical care consultant also testified that JR’s mental status change was nonspecific and was reasonably due to the pain medications she was receiving.
The plaintiffs countered with the reality that JR, a 32-year-old woman, died from low blood sugar because she received insulin when she wasn’t allowed to eat or drink – all at the hands of the medical team.
Conclusion:
Much of the attention regarding safe transitions of care is focused on the hospital discharge. Yet discontinuity within hospital walls is frequently associated with medical errors, and communication problems represent the largest category for hospital sentinel events.
The Joint Commission, the World Health Organization, the Institute of Medicine and the National Quality Foundation have all published white paper recommendations regarding the need to improve medical handoffs. Most hospitalists probably see this case as a "system error," and sure enough following this event the hospital overhauled its policies and procedures as they related to ICU transfers. But in the world of medical malpractice, the "system" doesn’t face the jury in litigation.
Although the attending internist was eventually dropped from this case, the hospital, the critical care consultant, and the hospitalist all settled with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
The story:
JR is a 32-year-old woman with a medical history of juvenile diabetes mellitus and end-stage renal disease on intermittent hemodialysis for the past 2 years. She was admitted to the hospital with shortness of breath and was found to have a large right-sided pleural effusion with loculations. Antibiotics were initiated. On hospital day 2 she underwent a video-assisted thoracoscopy for drainage, lysis of adhesions, and placement of two chest tubes. After returning to the floor from the postanesthesia care unit, JR had difficulty achieving adequate pain control despite a hydromorphone patient-controlled analgesic pump. Additional "as needed" intravenous morphine was ordered for relief. Before going home, the attending internist checked in on JR and discontinued her intravenous fluids (D5 half-normal saline), but wrote to resume her long-acting insulin later that same evening.
At approximately 7:30 p.m., JR was found by the nurse barely breathing. Her pupils were pinpoint and her respiratory rate was only 5 breaths per minute. A code blue was called and a hospitalist responded. A combination of epinephrine, atropine, and naloxone led to a return of consciousness, and JR was never intubated. In fact, the code sheet reflected that after the naloxone, JR was now fully awake, crying, and complaining of right-sided pain.
JR subsequently complained of nausea and began to vomit. Prior to transferring her to the intensive care unit, the hospitalist placed a nasogastric tube and made JR nil per os. To complete JR’s transfer to the ICU, the hospitalist contacted a critical care attending to give report, and then wrote "holding" ICU admission orders.
JR remained on the regular nursing floor for another hour as the ICU prepared for her arrival. Just prior to leaving the floor, JR’s nurse gave her 13 units of glargine insulin as ordered earlier that afternoon by the attending internist.
JR underwent a standard admission assessment upon her arrival at the ICU. The hospitalist "holding admission orders" included regular blood glucose checks and regular insulin coverage on a sliding scale. At midnight, JR’s blood glucose was over 250 mg/dL, and she was administered 6 units of regular insulin. At 5 a.m., another blood glucose was obtained and was recorded as 114 mg/dL. At 7:45 a.m., the new day shift ICU nurse did a complete assessment and noted that JR was lethargic with slurred speech. The critical care consultant rounded on JR at approximately 10 a.m. and also noted a change in mental status. Thirty minutes later, JR became unresponsive to verbal or tactile stimuli. A point-of-care blood glucose was performed and found to be 10 mg/dL. JR was subsequently intubated, but she never regained consciousness again.
She lived for another 2 months before her family decided to stop her dialysis and she passed away.
Complaint:
The family was upset to learn that JR suffered irreversible brain injury from low blood sugar. JR had been a diabetic on insulin all of her life, and the family couldn’t understand how such a thing could happen under the watchful eye of doctors and nurses.
The complaint alleged that there was an egregious failure with respect to communication between the attending physician, the floor nurse, the hospitalist, and the critical care consultant. Specific to the hospitalist, the complaint alleged that the "holding admission orders" should have included intravenous fluids with dextrose and/or explicit instructions to not give the glargine insulin as ordered earlier that same day.
The complaint was also disparaging of the critical care consultant for not recognizing the hypoglycemia earlier, given the mental status changes that JR exhibited.
Scientific principles:
Hypoglycemia can produce a myriad of neurologic signs and symptoms, but usually presents with symptoms of increased epinephrine release (e.g., tremor, diaphoresis) followed by neurologic symptoms that include generalized seizures, bizarre behavior, coma, and focal deficits. In acute severe hypoglycemia, a bolus of 25-50 grams of dextrose should be administered intravenously, followed by a continuous dextrose infusion. Blood glucose concentrations should be measured hourly. Reversal of neurologic symptoms may lag behind normalization of glucose levels.
Complaint rebuttal and discussion
All the health care providers thought their actions were reasonable in this case.
At the time that the attending internist wrote to resume JR’s glargine and stop the dextrose-containing intravenous fluids, JR was awake and was planning to have a light dinner. The floor nurse who gave the glargine later that night testified that she had a valid order to administer the medication.
The hospitalist testified that he was there to respond to emergencies, and that he transferred care of JR to the critical care consultant by verbal report. The critical care consultant acknowledged the verbal handoff from the hospitalist, but doubts there was any discussion regarding JR’s diabetes and was adamant that she was not responsible for JR receiving two doses of insulin (glargine and regular insulin) via the orders of two other physicians before she even had the opportunity to see the patient. The critical care consultant also testified that JR’s mental status change was nonspecific and was reasonably due to the pain medications she was receiving.
The plaintiffs countered with the reality that JR, a 32-year-old woman, died from low blood sugar because she received insulin when she wasn’t allowed to eat or drink – all at the hands of the medical team.
Conclusion:
Much of the attention regarding safe transitions of care is focused on the hospital discharge. Yet discontinuity within hospital walls is frequently associated with medical errors, and communication problems represent the largest category for hospital sentinel events.
The Joint Commission, the World Health Organization, the Institute of Medicine and the National Quality Foundation have all published white paper recommendations regarding the need to improve medical handoffs. Most hospitalists probably see this case as a "system error," and sure enough following this event the hospital overhauled its policies and procedures as they related to ICU transfers. But in the world of medical malpractice, the "system" doesn’t face the jury in litigation.
Although the attending internist was eventually dropped from this case, the hospital, the critical care consultant, and the hospitalist all settled with the plaintiff for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Appearances matter as time goes by
Story
M.S. was an 89-year-old woman whose medical history was consistent with chronic mesenteric ischemia (weight loss, postprandial abdominal pain, diarrhea), and a 6-cm infrarenal aortic aneurysm for which she had previously declined surgery. She was admitted to the hospital with increased abdominal pain (constant, and unrelated to meals), bloody stools, nausea with emesis, a profound leukocytosis (WBC, 56,000 cells/mcL) and renal insufficiency (creatinine ratio, 1.63 mg/dL). One week prior to this admission, she had been discharged from the same hospital following treatment for urosepsis. She had just finished 10 days of antibiotics (ceftriaxone and cephalexin) the day before this admission.
M.S. was admitted to a regular nursing floor by Dr. Hospitalist 1 and started on intravenous fluids (2L, then hep-lock) plus oral metronidazole (for suspected Clostridium difficile infection [CDI]) and oral ciprofloxacin (for possible infectious colitis/diverticulitis). No abdominal imaging was performed by the emergency room or Dr. Hospitalist 1.
For the next 2 days, M.S. was seen daily by Dr. Hospitalist 2 in conjunction with a GI consultant. The GI consultant discontinued the ciprofloxacin and both were awaiting the results of the C. difficile toxin assay. M.S. continued to have leukocytosis (WBC 36,000 cells/mcL) with a heart rate consistently greater than 90 beats/min. However, M.S. was able to achieve adequate abdominal pain control with oral acetaminophen, and she was taking a liquid diet. Dr. Hospitalist 2 commented in his progress notes that M.S. was improving clinically.
At 11 p.m. of hospital day 2, M.S. suffered a fall from her bedside commode and hit her head, causing a laceration. Nurses noted she was lethargic and hypotensive (BP 80/50 mm Hg) with labored breathing. Dr. Hospitalist 3 was contacted, but deferred a physical assessment in favor of restarting intravenous fluids (the IV fluids ordered on admission had been discontinued earlier that afternoon) and obtaining an arterial blood gas. One hour later, M.S. had a BP 102/65 mm Hg with saline running at 150 cc/hr. The arterial blood gas demonstrated a mixed respiratory and metabolic acidosis (pH, 7.06; PaCO2 21 mm Hg). Dr. Hospitalist 3 continued to defer a physical assessment and ordered a repeat arterial blood gas that showed a worsening respiratory and metabolic acidosis (pH, 7.00; PaCO2 37 mm Hg).
At 3 a.m., the nurses called a rapid response team for lethargy and tachypnea, and M.S. quickly lost her pulse. M.S. was a "Do not resuscitate/Do not intubate" patient, and she was therefore pronounced dead. No autopsy was performed.
Complaint
Although M.S. was 89 years old, the family was surprised at her passing. Prior to her last two admissions (urosepsis and this index event), M.S. was independent, lived in her own home, hosted a weekly bridge club, and routinely interacted with family and friends.
The family was particularly troubled by the laceration on her forehead, which at the time of her death, was a deep enough wound to have required stitches for closure (which had not been performed antemortem). The laceration led to discovery of the fall, which the led to the realization that no physician went to see M.S. prior to her death. The family was suspicious and contacted an attorney who had the case reviewed and subsequently filed suit.
The complaint alleged that all of the hospitalists failed to appreciate, appropriately monitor, and appropriately treat severe CDI with severe sepsis. The complaint further alleged that Dr. Hospitalist 3 breached the standard of care by failing to attend to M.S. after her fall and initiating therapies for her acidosis.
Scientific principles
C. difficile infection is one of the most common hospital-acquired (nosocomial) infections and is an increasingly frequent cause of morbidity and mortality among elderly hospitalized patients. Patients with acute CDI may develop signs of systemic toxicity with or without profuse diarrhea warranting admission to an ICU or for emergency surgery.
Guideline parameters for severe CDI include WBC count of more than 15,000 cells/mcL or a serum creatinine level equal to 1.5 times the premorbid level. Patients with severe disease should be treated with oral vancomycin (125 mg to 500 mg q.i.d.). In the setting of ileus, addition of IV metronidazole (500 mg every 8 hours) is appropriate. Intracolonic vancomycin may be considered in patients with profound ileus. Some severely ill patients with CDI require surgical intervention as a result of toxic megacolon, perforation, or impending perforation, necrotizing colitis or rapidly progressive and/or refractory disease with systemic inflammatory response syndrome leading to multiorgan system failure
Complaint rebuttal and discussion
Without an autopsy (or abdominal imaging of any kind), defense experts first argued that M.S. died from a progression of her mesenteric ischemia (gangrene, with or without perforation), not CDI. The defense further argued that if M.S. did have severe CDI, then she ultimately would have needed surgery (regardless of appropriate fluid resuscitation, ICU care, and appropriate antibiotics), and she was not an operative candidate. If M.S. had gone for surgery, she would have in all probability died intraoperatively.
In sum, the defense focused on causation, not the failures of the hospitalists to treat severe CDI. The plaintiff maintained that severe CDI was far more likely than acute mesenteric thrombosis (given her clinical presentation and pain control with acetaminophen), and that had appropriate and timely treatment been given, M.S.’s severe CDI was a reversible condition without surgery.
Conclusion
This case further highlights the importance of family perception in the circumstances surrounding death. If M.S. had not fallen and suffered a visible injury, or if Dr. Hospitalist 3 had responded immediately to the fall with care and treatment, it is very likely that this case would not have been filed.
Nonetheless, the hospitalist care appeared deficient in several important aspects – particularly the approach to sepsis and the possibility of severe CDI. Also, it is not easy to defend a hospitalist who failed to respond to an 89-year-old inpatient who is status post a fall with a deep forehead laceration and a pH of less than 7.1. That being said, this case went to trial, and the hospitalists received a full defense verdict from the jury.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
M.S. was an 89-year-old woman whose medical history was consistent with chronic mesenteric ischemia (weight loss, postprandial abdominal pain, diarrhea), and a 6-cm infrarenal aortic aneurysm for which she had previously declined surgery. She was admitted to the hospital with increased abdominal pain (constant, and unrelated to meals), bloody stools, nausea with emesis, a profound leukocytosis (WBC, 56,000 cells/mcL) and renal insufficiency (creatinine ratio, 1.63 mg/dL). One week prior to this admission, she had been discharged from the same hospital following treatment for urosepsis. She had just finished 10 days of antibiotics (ceftriaxone and cephalexin) the day before this admission.
M.S. was admitted to a regular nursing floor by Dr. Hospitalist 1 and started on intravenous fluids (2L, then hep-lock) plus oral metronidazole (for suspected Clostridium difficile infection [CDI]) and oral ciprofloxacin (for possible infectious colitis/diverticulitis). No abdominal imaging was performed by the emergency room or Dr. Hospitalist 1.
For the next 2 days, M.S. was seen daily by Dr. Hospitalist 2 in conjunction with a GI consultant. The GI consultant discontinued the ciprofloxacin and both were awaiting the results of the C. difficile toxin assay. M.S. continued to have leukocytosis (WBC 36,000 cells/mcL) with a heart rate consistently greater than 90 beats/min. However, M.S. was able to achieve adequate abdominal pain control with oral acetaminophen, and she was taking a liquid diet. Dr. Hospitalist 2 commented in his progress notes that M.S. was improving clinically.
At 11 p.m. of hospital day 2, M.S. suffered a fall from her bedside commode and hit her head, causing a laceration. Nurses noted she was lethargic and hypotensive (BP 80/50 mm Hg) with labored breathing. Dr. Hospitalist 3 was contacted, but deferred a physical assessment in favor of restarting intravenous fluids (the IV fluids ordered on admission had been discontinued earlier that afternoon) and obtaining an arterial blood gas. One hour later, M.S. had a BP 102/65 mm Hg with saline running at 150 cc/hr. The arterial blood gas demonstrated a mixed respiratory and metabolic acidosis (pH, 7.06; PaCO2 21 mm Hg). Dr. Hospitalist 3 continued to defer a physical assessment and ordered a repeat arterial blood gas that showed a worsening respiratory and metabolic acidosis (pH, 7.00; PaCO2 37 mm Hg).
At 3 a.m., the nurses called a rapid response team for lethargy and tachypnea, and M.S. quickly lost her pulse. M.S. was a "Do not resuscitate/Do not intubate" patient, and she was therefore pronounced dead. No autopsy was performed.
Complaint
Although M.S. was 89 years old, the family was surprised at her passing. Prior to her last two admissions (urosepsis and this index event), M.S. was independent, lived in her own home, hosted a weekly bridge club, and routinely interacted with family and friends.
The family was particularly troubled by the laceration on her forehead, which at the time of her death, was a deep enough wound to have required stitches for closure (which had not been performed antemortem). The laceration led to discovery of the fall, which the led to the realization that no physician went to see M.S. prior to her death. The family was suspicious and contacted an attorney who had the case reviewed and subsequently filed suit.
The complaint alleged that all of the hospitalists failed to appreciate, appropriately monitor, and appropriately treat severe CDI with severe sepsis. The complaint further alleged that Dr. Hospitalist 3 breached the standard of care by failing to attend to M.S. after her fall and initiating therapies for her acidosis.
Scientific principles
C. difficile infection is one of the most common hospital-acquired (nosocomial) infections and is an increasingly frequent cause of morbidity and mortality among elderly hospitalized patients. Patients with acute CDI may develop signs of systemic toxicity with or without profuse diarrhea warranting admission to an ICU or for emergency surgery.
Guideline parameters for severe CDI include WBC count of more than 15,000 cells/mcL or a serum creatinine level equal to 1.5 times the premorbid level. Patients with severe disease should be treated with oral vancomycin (125 mg to 500 mg q.i.d.). In the setting of ileus, addition of IV metronidazole (500 mg every 8 hours) is appropriate. Intracolonic vancomycin may be considered in patients with profound ileus. Some severely ill patients with CDI require surgical intervention as a result of toxic megacolon, perforation, or impending perforation, necrotizing colitis or rapidly progressive and/or refractory disease with systemic inflammatory response syndrome leading to multiorgan system failure
Complaint rebuttal and discussion
Without an autopsy (or abdominal imaging of any kind), defense experts first argued that M.S. died from a progression of her mesenteric ischemia (gangrene, with or without perforation), not CDI. The defense further argued that if M.S. did have severe CDI, then she ultimately would have needed surgery (regardless of appropriate fluid resuscitation, ICU care, and appropriate antibiotics), and she was not an operative candidate. If M.S. had gone for surgery, she would have in all probability died intraoperatively.
In sum, the defense focused on causation, not the failures of the hospitalists to treat severe CDI. The plaintiff maintained that severe CDI was far more likely than acute mesenteric thrombosis (given her clinical presentation and pain control with acetaminophen), and that had appropriate and timely treatment been given, M.S.’s severe CDI was a reversible condition without surgery.
Conclusion
This case further highlights the importance of family perception in the circumstances surrounding death. If M.S. had not fallen and suffered a visible injury, or if Dr. Hospitalist 3 had responded immediately to the fall with care and treatment, it is very likely that this case would not have been filed.
Nonetheless, the hospitalist care appeared deficient in several important aspects – particularly the approach to sepsis and the possibility of severe CDI. Also, it is not easy to defend a hospitalist who failed to respond to an 89-year-old inpatient who is status post a fall with a deep forehead laceration and a pH of less than 7.1. That being said, this case went to trial, and the hospitalists received a full defense verdict from the jury.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
M.S. was an 89-year-old woman whose medical history was consistent with chronic mesenteric ischemia (weight loss, postprandial abdominal pain, diarrhea), and a 6-cm infrarenal aortic aneurysm for which she had previously declined surgery. She was admitted to the hospital with increased abdominal pain (constant, and unrelated to meals), bloody stools, nausea with emesis, a profound leukocytosis (WBC, 56,000 cells/mcL) and renal insufficiency (creatinine ratio, 1.63 mg/dL). One week prior to this admission, she had been discharged from the same hospital following treatment for urosepsis. She had just finished 10 days of antibiotics (ceftriaxone and cephalexin) the day before this admission.
M.S. was admitted to a regular nursing floor by Dr. Hospitalist 1 and started on intravenous fluids (2L, then hep-lock) plus oral metronidazole (for suspected Clostridium difficile infection [CDI]) and oral ciprofloxacin (for possible infectious colitis/diverticulitis). No abdominal imaging was performed by the emergency room or Dr. Hospitalist 1.
For the next 2 days, M.S. was seen daily by Dr. Hospitalist 2 in conjunction with a GI consultant. The GI consultant discontinued the ciprofloxacin and both were awaiting the results of the C. difficile toxin assay. M.S. continued to have leukocytosis (WBC 36,000 cells/mcL) with a heart rate consistently greater than 90 beats/min. However, M.S. was able to achieve adequate abdominal pain control with oral acetaminophen, and she was taking a liquid diet. Dr. Hospitalist 2 commented in his progress notes that M.S. was improving clinically.
At 11 p.m. of hospital day 2, M.S. suffered a fall from her bedside commode and hit her head, causing a laceration. Nurses noted she was lethargic and hypotensive (BP 80/50 mm Hg) with labored breathing. Dr. Hospitalist 3 was contacted, but deferred a physical assessment in favor of restarting intravenous fluids (the IV fluids ordered on admission had been discontinued earlier that afternoon) and obtaining an arterial blood gas. One hour later, M.S. had a BP 102/65 mm Hg with saline running at 150 cc/hr. The arterial blood gas demonstrated a mixed respiratory and metabolic acidosis (pH, 7.06; PaCO2 21 mm Hg). Dr. Hospitalist 3 continued to defer a physical assessment and ordered a repeat arterial blood gas that showed a worsening respiratory and metabolic acidosis (pH, 7.00; PaCO2 37 mm Hg).
At 3 a.m., the nurses called a rapid response team for lethargy and tachypnea, and M.S. quickly lost her pulse. M.S. was a "Do not resuscitate/Do not intubate" patient, and she was therefore pronounced dead. No autopsy was performed.
Complaint
Although M.S. was 89 years old, the family was surprised at her passing. Prior to her last two admissions (urosepsis and this index event), M.S. was independent, lived in her own home, hosted a weekly bridge club, and routinely interacted with family and friends.
The family was particularly troubled by the laceration on her forehead, which at the time of her death, was a deep enough wound to have required stitches for closure (which had not been performed antemortem). The laceration led to discovery of the fall, which the led to the realization that no physician went to see M.S. prior to her death. The family was suspicious and contacted an attorney who had the case reviewed and subsequently filed suit.
The complaint alleged that all of the hospitalists failed to appreciate, appropriately monitor, and appropriately treat severe CDI with severe sepsis. The complaint further alleged that Dr. Hospitalist 3 breached the standard of care by failing to attend to M.S. after her fall and initiating therapies for her acidosis.
Scientific principles
C. difficile infection is one of the most common hospital-acquired (nosocomial) infections and is an increasingly frequent cause of morbidity and mortality among elderly hospitalized patients. Patients with acute CDI may develop signs of systemic toxicity with or without profuse diarrhea warranting admission to an ICU or for emergency surgery.
Guideline parameters for severe CDI include WBC count of more than 15,000 cells/mcL or a serum creatinine level equal to 1.5 times the premorbid level. Patients with severe disease should be treated with oral vancomycin (125 mg to 500 mg q.i.d.). In the setting of ileus, addition of IV metronidazole (500 mg every 8 hours) is appropriate. Intracolonic vancomycin may be considered in patients with profound ileus. Some severely ill patients with CDI require surgical intervention as a result of toxic megacolon, perforation, or impending perforation, necrotizing colitis or rapidly progressive and/or refractory disease with systemic inflammatory response syndrome leading to multiorgan system failure
Complaint rebuttal and discussion
Without an autopsy (or abdominal imaging of any kind), defense experts first argued that M.S. died from a progression of her mesenteric ischemia (gangrene, with or without perforation), not CDI. The defense further argued that if M.S. did have severe CDI, then she ultimately would have needed surgery (regardless of appropriate fluid resuscitation, ICU care, and appropriate antibiotics), and she was not an operative candidate. If M.S. had gone for surgery, she would have in all probability died intraoperatively.
In sum, the defense focused on causation, not the failures of the hospitalists to treat severe CDI. The plaintiff maintained that severe CDI was far more likely than acute mesenteric thrombosis (given her clinical presentation and pain control with acetaminophen), and that had appropriate and timely treatment been given, M.S.’s severe CDI was a reversible condition without surgery.
Conclusion
This case further highlights the importance of family perception in the circumstances surrounding death. If M.S. had not fallen and suffered a visible injury, or if Dr. Hospitalist 3 had responded immediately to the fall with care and treatment, it is very likely that this case would not have been filed.
Nonetheless, the hospitalist care appeared deficient in several important aspects – particularly the approach to sepsis and the possibility of severe CDI. Also, it is not easy to defend a hospitalist who failed to respond to an 89-year-old inpatient who is status post a fall with a deep forehead laceration and a pH of less than 7.1. That being said, this case went to trial, and the hospitalists received a full defense verdict from the jury.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Timing is everything
Story
Mrs. S.L. was a 58-year-old woman with a past medical history of stable chronic obstructive pulmonary disease and remote breast cancer, who presented to the hospital with a 2-3 day history of a swollen right leg. She was quickly diagnosed with a right femoral deep vein thrombosis, and she was admitted to Dr. Hospitalist for anticoagulation. Mrs. S.L. denied any chest symptoms on admission, and other than discomfort in her leg, she said she felt like her "usual self." Dr. Hospitalist ordered a heparin bolus and infusion along with monitoring of her activated partial thromboplastin time (aPTT). Mrs. S.L. had difficulty achieving therapeutic anticoagulation and, during the first night in the hospital, she received two additional heparin boluses per a heparin weight-based nomogram.
The following morning, Mrs. S.L. complained of a headache. Dr. Hospitalist was contacted and gave a verbal order for acetaminophen. A few hours later, Dr. Hospitalist visited Mrs. S.L. and noted her to be very sleepy. Dr. Hospitalist ordered a CT of the head without contrast. Several times that afternoon, the nurses documented that the patient was "sleeping" or "resting comfortably" in bed.
At 5 p.m., patient transport arrived to take Mrs. S.L. to radiology. She was unarousable and cyanotic but had a weak pulse. A Code Blue was called, and Mrs. S.L. was intubated and transferred to the ICU under the care of a critical care physician. Subsequent head imaging confirmed a large intracranial hemorrhage. Mrs. S.L. survived another 2 months in ICU, but she never regained consciousness. After discussions with the family regarding her poor prognosis, care was ultimately withdrawn.
Complaint
Following the initial Code Blue, Dr. Hospitalist called the husband and left a message that Mrs. S.L. had been transferred to the ICU. However, despite several subsequent attempts by the family to reach Dr. Hospitalist, he never actually spoke with the husband or the family about what had happened.
According to the family, they were informed that since Dr. Hospitalist was no longer involved in caring for Mrs. S.L., all information would need to come from her current care team. The family was convinced that a mistake had somehow occurred, and they contacted an attorney.
The complaint alleged that Dr. Hospitalist failed to evaluate Mrs. S.L. at the time of her headache, failed to stop her anticoagulation when she developed mental status changes, failed to ensure timely head imaging, and subsequently failed to reverse anticoagulation and/or obtain appropriate consultation to address her intracranial bleed. Had Dr. Hospitalist met the standard of care, Mrs. S.L. would be alive with minimal neurologic sequelae.
Scientific principles
Intracranial hemorrhage, primarily intracerebral hemorrhage, is the most serious and lethal complication of heparin therapy. Hemorrhagic complications are more closely related to underlying clinical risk factors than an aPTT elevation above the therapeutic range.
Patients at particular risk are those who have had recent surgery or trauma, or who have other clinical factors that predispose to bleeding, such as peptic ulcer, occult malignancy, liver disease, hemostatic defects, aged greater than 65 years, female gender, and a reduced admission hemoglobin concentration. The management of bleeding in a patient receiving heparin depends upon the location and severity of bleeding. Full neutralization of heparin effect is achieved with a dose of 1 mg protamine/100 U heparin.
Complaint rebuttal and discussion
The defense argued that the headache was a nonspecific finding and that Dr. Hospitalist was actively rounding at the time of the verbal acetaminophen order. The defense further asserted that as soon as Dr. Hospitalist was aware of the mental status change, he ordered STAT CT scan of the head to assess for a bleed and that he had a right to rely on hospital personnel to do their jobs.
Dr. Hospitalist testified that it was his expectation that he would be contacted if the study were delayed, or the results abnormal. In contrast, depositions of the primary nurse and the unit secretary revealed that the CT order was initially placed as routine, not STAT. The physician order sheet in the paper chart showed a signed CT order without a priority designation, but immediately underneath the order, the word "STAT" was written. No part of the order was dated or timed.
Dr. Hospitalist testified that the word "STAT" was his and that he wrote it contemporaneously with his order. The unit secretary testified that the word "STAT" must have been added after she took the order off, or the order would have been placed STAT. The plaintiff’s attorney hired a handwriting expert who concluded that the word "STAT" was written with a different pen than the original order, making it unlikely to have been written contemporaneously.
Regardless of the truth, the plaintiff argued that somebody made a mistake and it cost Mrs. S.L. her life. The defense countered with the argument that regardless of when the diagnosis was made, the outcome most likely would have been the same.
Conclusion
Mrs. S.L. suffered a known complication from anticoagulant therapy. Whether there was a delay in diagnosis and treatment that could have been averted, an adverse outcome remains unknown. However, Dr. Hospitalist did not help himself in several important respects.
First, he did not speak with the family after the unexpected transfer to the ICU. A demonstration of empathy may have gone a long way to avoiding the lawsuit altogether. As it was, the family interpreted Dr. Hospitalist’s reluctance to speak with them as an admission of guilt. The plaintiff further used this to portray Dr. Hospitalist to the jury as a callous physician.
Second, Dr. Hospitalist was in the habit of writing orders that were not dated or timed. The plaintiff held this up as an example of "sloppy work" – Dr. Hospitalist was not only callous, he was lazy as well.
In the end, Dr. Hospitalist was adamant that he had written orders for a STAT head CT immediately after his evaluation of Mrs. S.L. and that he did not alter the medical records. Nonetheless, he chose to settle with the plaintiff for an undisclosed amount before the jury had a chance to return a verdict. A post-trial jury survey confirmed that Dr. Hospitalist had little credibility with the jury and that he had made a wise decision to settle when he did.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
Mrs. S.L. was a 58-year-old woman with a past medical history of stable chronic obstructive pulmonary disease and remote breast cancer, who presented to the hospital with a 2-3 day history of a swollen right leg. She was quickly diagnosed with a right femoral deep vein thrombosis, and she was admitted to Dr. Hospitalist for anticoagulation. Mrs. S.L. denied any chest symptoms on admission, and other than discomfort in her leg, she said she felt like her "usual self." Dr. Hospitalist ordered a heparin bolus and infusion along with monitoring of her activated partial thromboplastin time (aPTT). Mrs. S.L. had difficulty achieving therapeutic anticoagulation and, during the first night in the hospital, she received two additional heparin boluses per a heparin weight-based nomogram.
The following morning, Mrs. S.L. complained of a headache. Dr. Hospitalist was contacted and gave a verbal order for acetaminophen. A few hours later, Dr. Hospitalist visited Mrs. S.L. and noted her to be very sleepy. Dr. Hospitalist ordered a CT of the head without contrast. Several times that afternoon, the nurses documented that the patient was "sleeping" or "resting comfortably" in bed.
At 5 p.m., patient transport arrived to take Mrs. S.L. to radiology. She was unarousable and cyanotic but had a weak pulse. A Code Blue was called, and Mrs. S.L. was intubated and transferred to the ICU under the care of a critical care physician. Subsequent head imaging confirmed a large intracranial hemorrhage. Mrs. S.L. survived another 2 months in ICU, but she never regained consciousness. After discussions with the family regarding her poor prognosis, care was ultimately withdrawn.
Complaint
Following the initial Code Blue, Dr. Hospitalist called the husband and left a message that Mrs. S.L. had been transferred to the ICU. However, despite several subsequent attempts by the family to reach Dr. Hospitalist, he never actually spoke with the husband or the family about what had happened.
According to the family, they were informed that since Dr. Hospitalist was no longer involved in caring for Mrs. S.L., all information would need to come from her current care team. The family was convinced that a mistake had somehow occurred, and they contacted an attorney.
The complaint alleged that Dr. Hospitalist failed to evaluate Mrs. S.L. at the time of her headache, failed to stop her anticoagulation when she developed mental status changes, failed to ensure timely head imaging, and subsequently failed to reverse anticoagulation and/or obtain appropriate consultation to address her intracranial bleed. Had Dr. Hospitalist met the standard of care, Mrs. S.L. would be alive with minimal neurologic sequelae.
Scientific principles
Intracranial hemorrhage, primarily intracerebral hemorrhage, is the most serious and lethal complication of heparin therapy. Hemorrhagic complications are more closely related to underlying clinical risk factors than an aPTT elevation above the therapeutic range.
Patients at particular risk are those who have had recent surgery or trauma, or who have other clinical factors that predispose to bleeding, such as peptic ulcer, occult malignancy, liver disease, hemostatic defects, aged greater than 65 years, female gender, and a reduced admission hemoglobin concentration. The management of bleeding in a patient receiving heparin depends upon the location and severity of bleeding. Full neutralization of heparin effect is achieved with a dose of 1 mg protamine/100 U heparin.
Complaint rebuttal and discussion
The defense argued that the headache was a nonspecific finding and that Dr. Hospitalist was actively rounding at the time of the verbal acetaminophen order. The defense further asserted that as soon as Dr. Hospitalist was aware of the mental status change, he ordered STAT CT scan of the head to assess for a bleed and that he had a right to rely on hospital personnel to do their jobs.
Dr. Hospitalist testified that it was his expectation that he would be contacted if the study were delayed, or the results abnormal. In contrast, depositions of the primary nurse and the unit secretary revealed that the CT order was initially placed as routine, not STAT. The physician order sheet in the paper chart showed a signed CT order without a priority designation, but immediately underneath the order, the word "STAT" was written. No part of the order was dated or timed.
Dr. Hospitalist testified that the word "STAT" was his and that he wrote it contemporaneously with his order. The unit secretary testified that the word "STAT" must have been added after she took the order off, or the order would have been placed STAT. The plaintiff’s attorney hired a handwriting expert who concluded that the word "STAT" was written with a different pen than the original order, making it unlikely to have been written contemporaneously.
Regardless of the truth, the plaintiff argued that somebody made a mistake and it cost Mrs. S.L. her life. The defense countered with the argument that regardless of when the diagnosis was made, the outcome most likely would have been the same.
Conclusion
Mrs. S.L. suffered a known complication from anticoagulant therapy. Whether there was a delay in diagnosis and treatment that could have been averted, an adverse outcome remains unknown. However, Dr. Hospitalist did not help himself in several important respects.
First, he did not speak with the family after the unexpected transfer to the ICU. A demonstration of empathy may have gone a long way to avoiding the lawsuit altogether. As it was, the family interpreted Dr. Hospitalist’s reluctance to speak with them as an admission of guilt. The plaintiff further used this to portray Dr. Hospitalist to the jury as a callous physician.
Second, Dr. Hospitalist was in the habit of writing orders that were not dated or timed. The plaintiff held this up as an example of "sloppy work" – Dr. Hospitalist was not only callous, he was lazy as well.
In the end, Dr. Hospitalist was adamant that he had written orders for a STAT head CT immediately after his evaluation of Mrs. S.L. and that he did not alter the medical records. Nonetheless, he chose to settle with the plaintiff for an undisclosed amount before the jury had a chance to return a verdict. A post-trial jury survey confirmed that Dr. Hospitalist had little credibility with the jury and that he had made a wise decision to settle when he did.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
Mrs. S.L. was a 58-year-old woman with a past medical history of stable chronic obstructive pulmonary disease and remote breast cancer, who presented to the hospital with a 2-3 day history of a swollen right leg. She was quickly diagnosed with a right femoral deep vein thrombosis, and she was admitted to Dr. Hospitalist for anticoagulation. Mrs. S.L. denied any chest symptoms on admission, and other than discomfort in her leg, she said she felt like her "usual self." Dr. Hospitalist ordered a heparin bolus and infusion along with monitoring of her activated partial thromboplastin time (aPTT). Mrs. S.L. had difficulty achieving therapeutic anticoagulation and, during the first night in the hospital, she received two additional heparin boluses per a heparin weight-based nomogram.
The following morning, Mrs. S.L. complained of a headache. Dr. Hospitalist was contacted and gave a verbal order for acetaminophen. A few hours later, Dr. Hospitalist visited Mrs. S.L. and noted her to be very sleepy. Dr. Hospitalist ordered a CT of the head without contrast. Several times that afternoon, the nurses documented that the patient was "sleeping" or "resting comfortably" in bed.
At 5 p.m., patient transport arrived to take Mrs. S.L. to radiology. She was unarousable and cyanotic but had a weak pulse. A Code Blue was called, and Mrs. S.L. was intubated and transferred to the ICU under the care of a critical care physician. Subsequent head imaging confirmed a large intracranial hemorrhage. Mrs. S.L. survived another 2 months in ICU, but she never regained consciousness. After discussions with the family regarding her poor prognosis, care was ultimately withdrawn.
Complaint
Following the initial Code Blue, Dr. Hospitalist called the husband and left a message that Mrs. S.L. had been transferred to the ICU. However, despite several subsequent attempts by the family to reach Dr. Hospitalist, he never actually spoke with the husband or the family about what had happened.
According to the family, they were informed that since Dr. Hospitalist was no longer involved in caring for Mrs. S.L., all information would need to come from her current care team. The family was convinced that a mistake had somehow occurred, and they contacted an attorney.
The complaint alleged that Dr. Hospitalist failed to evaluate Mrs. S.L. at the time of her headache, failed to stop her anticoagulation when she developed mental status changes, failed to ensure timely head imaging, and subsequently failed to reverse anticoagulation and/or obtain appropriate consultation to address her intracranial bleed. Had Dr. Hospitalist met the standard of care, Mrs. S.L. would be alive with minimal neurologic sequelae.
Scientific principles
Intracranial hemorrhage, primarily intracerebral hemorrhage, is the most serious and lethal complication of heparin therapy. Hemorrhagic complications are more closely related to underlying clinical risk factors than an aPTT elevation above the therapeutic range.
Patients at particular risk are those who have had recent surgery or trauma, or who have other clinical factors that predispose to bleeding, such as peptic ulcer, occult malignancy, liver disease, hemostatic defects, aged greater than 65 years, female gender, and a reduced admission hemoglobin concentration. The management of bleeding in a patient receiving heparin depends upon the location and severity of bleeding. Full neutralization of heparin effect is achieved with a dose of 1 mg protamine/100 U heparin.
Complaint rebuttal and discussion
The defense argued that the headache was a nonspecific finding and that Dr. Hospitalist was actively rounding at the time of the verbal acetaminophen order. The defense further asserted that as soon as Dr. Hospitalist was aware of the mental status change, he ordered STAT CT scan of the head to assess for a bleed and that he had a right to rely on hospital personnel to do their jobs.
Dr. Hospitalist testified that it was his expectation that he would be contacted if the study were delayed, or the results abnormal. In contrast, depositions of the primary nurse and the unit secretary revealed that the CT order was initially placed as routine, not STAT. The physician order sheet in the paper chart showed a signed CT order without a priority designation, but immediately underneath the order, the word "STAT" was written. No part of the order was dated or timed.
Dr. Hospitalist testified that the word "STAT" was his and that he wrote it contemporaneously with his order. The unit secretary testified that the word "STAT" must have been added after she took the order off, or the order would have been placed STAT. The plaintiff’s attorney hired a handwriting expert who concluded that the word "STAT" was written with a different pen than the original order, making it unlikely to have been written contemporaneously.
Regardless of the truth, the plaintiff argued that somebody made a mistake and it cost Mrs. S.L. her life. The defense countered with the argument that regardless of when the diagnosis was made, the outcome most likely would have been the same.
Conclusion
Mrs. S.L. suffered a known complication from anticoagulant therapy. Whether there was a delay in diagnosis and treatment that could have been averted, an adverse outcome remains unknown. However, Dr. Hospitalist did not help himself in several important respects.
First, he did not speak with the family after the unexpected transfer to the ICU. A demonstration of empathy may have gone a long way to avoiding the lawsuit altogether. As it was, the family interpreted Dr. Hospitalist’s reluctance to speak with them as an admission of guilt. The plaintiff further used this to portray Dr. Hospitalist to the jury as a callous physician.
Second, Dr. Hospitalist was in the habit of writing orders that were not dated or timed. The plaintiff held this up as an example of "sloppy work" – Dr. Hospitalist was not only callous, he was lazy as well.
In the end, Dr. Hospitalist was adamant that he had written orders for a STAT head CT immediately after his evaluation of Mrs. S.L. and that he did not alter the medical records. Nonetheless, he chose to settle with the plaintiff for an undisclosed amount before the jury had a chance to return a verdict. A post-trial jury survey confirmed that Dr. Hospitalist had little credibility with the jury and that he had made a wise decision to settle when he did.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Demands of the job
Mrs. E.D. was a 56-year-old woman who presented to the hospital following a suicide attempt. She was obese and an ex-smoker with a medical history of bipolar disease. She was found somnolent at home by her husband with vomit in her hair. She admitted to taking an overdose of her clonazepam, and he called 911.
Mrs. E.D. responded to flumazenil in the emergency department. Her labs were essentially normal including an acetaminophen level. Her CXR [chest x-ray] was interpreted as no active disease. She was admitted by Dr. Hospitalist-1 for continued observation and treatment for possible aspiration pneumonia.
For the next 48 hours, Mrs. E.D. was cared for by Dr. Hospitalist-2. Mrs. E.D.’s mental status returned to normal and her SaO2 (arterial oxygen percent saturation) greater than 94% was 2L oxygen/nasal cannula (NC). On day 2, she was noted to have bilateral crackles. An ECG performed that morning showed rate-dependent ST segment depressions in the precordial leads (heart rate, 102 bpm), compared with admission ECG. Dr. Hospitalist-2 made no mention of this finding in his progress note, and no cardiac biomarkers were obtained. Later that evening, Mrs. E.D. was transferred to the inpatient psychiatry ward for ongoing treatment of her bipolar disorder.
Mrs. E.D. participated in her therapies on the psychiatry ward, but complained of dyspnea on exertion (DOE) and shortness of breath (SOB) while lying in bed. Psychiatry ordered a chest radiograph that showed hyperinflation and chronic obstructive pulmonary disease (COPD) with mild fluid overload consistent with heart failure. Dr. Hospitalist-2 was contacted and came to see Mrs. E.D. for an evaluation. He ordered pulmonary function testing (PFT), oral prednisone for COPD, and continued oral antibiotics for aspiration pneumonia.
For the next 2 days, the psychiatry staff continued to document DOE, SOB, and wheezing and crackles on lung auscultation. PFTs demonstrated severe obstructive airway disease. Albuterol nebulizer treatments were initiated along with an ipratropium inhaler. In the early morning hours of day 9, Mrs. E.D. complained of increasing SOB. Her vital signs were BP, 180/110 mm Hg; HR, 104 bpm; and RR, 24 breaths/min. Dr. Hospitalist-2 was contacted. CXR showed bilateral pleural effusions, hyperinflation, with interstitial edema and patchy areas of consolidation. SaO2 was 83% on RA, and Mrs. E.D. was titrated to 3L O2/NC to keep her saturations greater than 92%. Later that morning, the psychiatry staff was informed that Mrs. E.D. would be evaluated by Dr. Hospitalist-1.
On the evening of day 9, Mrs. E.D. was still on the psychiatry floor. Her husband was visiting and was concerned with her breathing. Her SaO2 was 83% on 3L and she was increased to 6L of oxygen. The psychiatry staff contacted Dr. Hospitalist-1, who accepted the transfer to the regular nursing floor. Transfer orders were written by Dr. Hospitalist-1 with a diagnosis of pneumonia/COPD along with therapies for same. There is no evidence in the chart that Dr. Hospitalist-1 evaluated Mrs. E.D. prior to the transfer orders being written. Mrs. E.D. arrived to the regular nursing floor around 9 p.m. She was administered an IV antibiotic dose at 11 p.m. and was noted to be comfortable. At 11:30 p.m., Mrs. E.D. was found apneic and pulseless. She was unable to be resuscitated.
An autopsy was performed with a final anatomic diagnosis of acute subendocardial myocardial ischemic change and necrosis, severe CAD (coronary artery disease), severe chronic ischemic heart disease, severe generalized atherosclerotic vascular disease, severe chronic obstructive lung disease, and patchy bronchopneumonia.
Complaint
The husband felt as if his wife was abandoned. He was aware of her increasing respiratory symptoms while she was on the psychiatry ward and couldn’t understand why it took the doctors so long to do something. When he learned that his wife had essentially died of a "heart attack," he contacted an attorney who filed suit.
The complaint alleged that Dr. Hospitalist-1 and Dr. Hospitalist-2 both failed to diagnose her myocardial ischemia, failed to recognize her heart failure, and failed to initiate appropriate therapies to decrease her cardiac work and save her heart.
Scientific principles
The concept of "demand ischemia" refers to a mismatch between myocardial oxygen demand and supply. The 2012 Joint ESC/ACCF/AHA/WHF Third Universal Definition of MI refers to a type 2 MI when the event is secondary to ischemia due to either an increased oxygen demand or a decreased supply in the absence of an acute primary coronary thrombotic event. Myocardial oxygen demand is increased in a number of clinical settings (sepsis, tachyarrhythmia). Simultaneously, myocardial oxygen delivery may be reduced due to both tachycardia (which reduces diastolic filling time) and reduced perfusion pressure (in the setting of hypotension and/or increased cardiac filling pressures as seen in heart failure).
Complaint rebuttal and discussion
The defense asserted that Mrs. E.D. had severe COPD and pneumonia, and this was the source of her SOB and the underlying condition that caused demand ischemia. Defense experts further asserted that her severe COPD and pneumonia was treated appropriately and that there was little more that could have been done. Plaintiff experts disagreed and opined that had her true condition been recognized, additional therapies (such as beta-blockade, diuresis, intensive care) and monitoring (for lethal arrhythmia) would have been life saving.
Conclusion
Both hospitalists missed the ECG clues early in the hospital stay, and further misinterpreted the chest radiographs with respect to heart failure. Nonetheless, Dr. Hospitalist-2 was eventually dropped from the case as much of the criticism was focused on Dr. Hospitalist-1 and her failure to come and evaluate Mrs. E.D. on the day of her death.
During her deposition, Dr. Hospitalist-1 testified that she had no memory regarding the chain of events; however nurse depositions supported the notion that Dr. Hospitalist-1 never saw the patient even though she had written a full page of transfer orders. So regardless of the "battle of the experts," with respect to whether the demand ischemia could really have been treated or not, the case boiled down to a hospitalist who appeared lazy and uncaring.
The case was settled for an undisclosed amount on behalf of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Mrs. E.D. was a 56-year-old woman who presented to the hospital following a suicide attempt. She was obese and an ex-smoker with a medical history of bipolar disease. She was found somnolent at home by her husband with vomit in her hair. She admitted to taking an overdose of her clonazepam, and he called 911.
Mrs. E.D. responded to flumazenil in the emergency department. Her labs were essentially normal including an acetaminophen level. Her CXR [chest x-ray] was interpreted as no active disease. She was admitted by Dr. Hospitalist-1 for continued observation and treatment for possible aspiration pneumonia.
For the next 48 hours, Mrs. E.D. was cared for by Dr. Hospitalist-2. Mrs. E.D.’s mental status returned to normal and her SaO2 (arterial oxygen percent saturation) greater than 94% was 2L oxygen/nasal cannula (NC). On day 2, she was noted to have bilateral crackles. An ECG performed that morning showed rate-dependent ST segment depressions in the precordial leads (heart rate, 102 bpm), compared with admission ECG. Dr. Hospitalist-2 made no mention of this finding in his progress note, and no cardiac biomarkers were obtained. Later that evening, Mrs. E.D. was transferred to the inpatient psychiatry ward for ongoing treatment of her bipolar disorder.
Mrs. E.D. participated in her therapies on the psychiatry ward, but complained of dyspnea on exertion (DOE) and shortness of breath (SOB) while lying in bed. Psychiatry ordered a chest radiograph that showed hyperinflation and chronic obstructive pulmonary disease (COPD) with mild fluid overload consistent with heart failure. Dr. Hospitalist-2 was contacted and came to see Mrs. E.D. for an evaluation. He ordered pulmonary function testing (PFT), oral prednisone for COPD, and continued oral antibiotics for aspiration pneumonia.
For the next 2 days, the psychiatry staff continued to document DOE, SOB, and wheezing and crackles on lung auscultation. PFTs demonstrated severe obstructive airway disease. Albuterol nebulizer treatments were initiated along with an ipratropium inhaler. In the early morning hours of day 9, Mrs. E.D. complained of increasing SOB. Her vital signs were BP, 180/110 mm Hg; HR, 104 bpm; and RR, 24 breaths/min. Dr. Hospitalist-2 was contacted. CXR showed bilateral pleural effusions, hyperinflation, with interstitial edema and patchy areas of consolidation. SaO2 was 83% on RA, and Mrs. E.D. was titrated to 3L O2/NC to keep her saturations greater than 92%. Later that morning, the psychiatry staff was informed that Mrs. E.D. would be evaluated by Dr. Hospitalist-1.
On the evening of day 9, Mrs. E.D. was still on the psychiatry floor. Her husband was visiting and was concerned with her breathing. Her SaO2 was 83% on 3L and she was increased to 6L of oxygen. The psychiatry staff contacted Dr. Hospitalist-1, who accepted the transfer to the regular nursing floor. Transfer orders were written by Dr. Hospitalist-1 with a diagnosis of pneumonia/COPD along with therapies for same. There is no evidence in the chart that Dr. Hospitalist-1 evaluated Mrs. E.D. prior to the transfer orders being written. Mrs. E.D. arrived to the regular nursing floor around 9 p.m. She was administered an IV antibiotic dose at 11 p.m. and was noted to be comfortable. At 11:30 p.m., Mrs. E.D. was found apneic and pulseless. She was unable to be resuscitated.
An autopsy was performed with a final anatomic diagnosis of acute subendocardial myocardial ischemic change and necrosis, severe CAD (coronary artery disease), severe chronic ischemic heart disease, severe generalized atherosclerotic vascular disease, severe chronic obstructive lung disease, and patchy bronchopneumonia.
Complaint
The husband felt as if his wife was abandoned. He was aware of her increasing respiratory symptoms while she was on the psychiatry ward and couldn’t understand why it took the doctors so long to do something. When he learned that his wife had essentially died of a "heart attack," he contacted an attorney who filed suit.
The complaint alleged that Dr. Hospitalist-1 and Dr. Hospitalist-2 both failed to diagnose her myocardial ischemia, failed to recognize her heart failure, and failed to initiate appropriate therapies to decrease her cardiac work and save her heart.
Scientific principles
The concept of "demand ischemia" refers to a mismatch between myocardial oxygen demand and supply. The 2012 Joint ESC/ACCF/AHA/WHF Third Universal Definition of MI refers to a type 2 MI when the event is secondary to ischemia due to either an increased oxygen demand or a decreased supply in the absence of an acute primary coronary thrombotic event. Myocardial oxygen demand is increased in a number of clinical settings (sepsis, tachyarrhythmia). Simultaneously, myocardial oxygen delivery may be reduced due to both tachycardia (which reduces diastolic filling time) and reduced perfusion pressure (in the setting of hypotension and/or increased cardiac filling pressures as seen in heart failure).
Complaint rebuttal and discussion
The defense asserted that Mrs. E.D. had severe COPD and pneumonia, and this was the source of her SOB and the underlying condition that caused demand ischemia. Defense experts further asserted that her severe COPD and pneumonia was treated appropriately and that there was little more that could have been done. Plaintiff experts disagreed and opined that had her true condition been recognized, additional therapies (such as beta-blockade, diuresis, intensive care) and monitoring (for lethal arrhythmia) would have been life saving.
Conclusion
Both hospitalists missed the ECG clues early in the hospital stay, and further misinterpreted the chest radiographs with respect to heart failure. Nonetheless, Dr. Hospitalist-2 was eventually dropped from the case as much of the criticism was focused on Dr. Hospitalist-1 and her failure to come and evaluate Mrs. E.D. on the day of her death.
During her deposition, Dr. Hospitalist-1 testified that she had no memory regarding the chain of events; however nurse depositions supported the notion that Dr. Hospitalist-1 never saw the patient even though she had written a full page of transfer orders. So regardless of the "battle of the experts," with respect to whether the demand ischemia could really have been treated or not, the case boiled down to a hospitalist who appeared lazy and uncaring.
The case was settled for an undisclosed amount on behalf of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Mrs. E.D. was a 56-year-old woman who presented to the hospital following a suicide attempt. She was obese and an ex-smoker with a medical history of bipolar disease. She was found somnolent at home by her husband with vomit in her hair. She admitted to taking an overdose of her clonazepam, and he called 911.
Mrs. E.D. responded to flumazenil in the emergency department. Her labs were essentially normal including an acetaminophen level. Her CXR [chest x-ray] was interpreted as no active disease. She was admitted by Dr. Hospitalist-1 for continued observation and treatment for possible aspiration pneumonia.
For the next 48 hours, Mrs. E.D. was cared for by Dr. Hospitalist-2. Mrs. E.D.’s mental status returned to normal and her SaO2 (arterial oxygen percent saturation) greater than 94% was 2L oxygen/nasal cannula (NC). On day 2, she was noted to have bilateral crackles. An ECG performed that morning showed rate-dependent ST segment depressions in the precordial leads (heart rate, 102 bpm), compared with admission ECG. Dr. Hospitalist-2 made no mention of this finding in his progress note, and no cardiac biomarkers were obtained. Later that evening, Mrs. E.D. was transferred to the inpatient psychiatry ward for ongoing treatment of her bipolar disorder.
Mrs. E.D. participated in her therapies on the psychiatry ward, but complained of dyspnea on exertion (DOE) and shortness of breath (SOB) while lying in bed. Psychiatry ordered a chest radiograph that showed hyperinflation and chronic obstructive pulmonary disease (COPD) with mild fluid overload consistent with heart failure. Dr. Hospitalist-2 was contacted and came to see Mrs. E.D. for an evaluation. He ordered pulmonary function testing (PFT), oral prednisone for COPD, and continued oral antibiotics for aspiration pneumonia.
For the next 2 days, the psychiatry staff continued to document DOE, SOB, and wheezing and crackles on lung auscultation. PFTs demonstrated severe obstructive airway disease. Albuterol nebulizer treatments were initiated along with an ipratropium inhaler. In the early morning hours of day 9, Mrs. E.D. complained of increasing SOB. Her vital signs were BP, 180/110 mm Hg; HR, 104 bpm; and RR, 24 breaths/min. Dr. Hospitalist-2 was contacted. CXR showed bilateral pleural effusions, hyperinflation, with interstitial edema and patchy areas of consolidation. SaO2 was 83% on RA, and Mrs. E.D. was titrated to 3L O2/NC to keep her saturations greater than 92%. Later that morning, the psychiatry staff was informed that Mrs. E.D. would be evaluated by Dr. Hospitalist-1.
On the evening of day 9, Mrs. E.D. was still on the psychiatry floor. Her husband was visiting and was concerned with her breathing. Her SaO2 was 83% on 3L and she was increased to 6L of oxygen. The psychiatry staff contacted Dr. Hospitalist-1, who accepted the transfer to the regular nursing floor. Transfer orders were written by Dr. Hospitalist-1 with a diagnosis of pneumonia/COPD along with therapies for same. There is no evidence in the chart that Dr. Hospitalist-1 evaluated Mrs. E.D. prior to the transfer orders being written. Mrs. E.D. arrived to the regular nursing floor around 9 p.m. She was administered an IV antibiotic dose at 11 p.m. and was noted to be comfortable. At 11:30 p.m., Mrs. E.D. was found apneic and pulseless. She was unable to be resuscitated.
An autopsy was performed with a final anatomic diagnosis of acute subendocardial myocardial ischemic change and necrosis, severe CAD (coronary artery disease), severe chronic ischemic heart disease, severe generalized atherosclerotic vascular disease, severe chronic obstructive lung disease, and patchy bronchopneumonia.
Complaint
The husband felt as if his wife was abandoned. He was aware of her increasing respiratory symptoms while she was on the psychiatry ward and couldn’t understand why it took the doctors so long to do something. When he learned that his wife had essentially died of a "heart attack," he contacted an attorney who filed suit.
The complaint alleged that Dr. Hospitalist-1 and Dr. Hospitalist-2 both failed to diagnose her myocardial ischemia, failed to recognize her heart failure, and failed to initiate appropriate therapies to decrease her cardiac work and save her heart.
Scientific principles
The concept of "demand ischemia" refers to a mismatch between myocardial oxygen demand and supply. The 2012 Joint ESC/ACCF/AHA/WHF Third Universal Definition of MI refers to a type 2 MI when the event is secondary to ischemia due to either an increased oxygen demand or a decreased supply in the absence of an acute primary coronary thrombotic event. Myocardial oxygen demand is increased in a number of clinical settings (sepsis, tachyarrhythmia). Simultaneously, myocardial oxygen delivery may be reduced due to both tachycardia (which reduces diastolic filling time) and reduced perfusion pressure (in the setting of hypotension and/or increased cardiac filling pressures as seen in heart failure).
Complaint rebuttal and discussion
The defense asserted that Mrs. E.D. had severe COPD and pneumonia, and this was the source of her SOB and the underlying condition that caused demand ischemia. Defense experts further asserted that her severe COPD and pneumonia was treated appropriately and that there was little more that could have been done. Plaintiff experts disagreed and opined that had her true condition been recognized, additional therapies (such as beta-blockade, diuresis, intensive care) and monitoring (for lethal arrhythmia) would have been life saving.
Conclusion
Both hospitalists missed the ECG clues early in the hospital stay, and further misinterpreted the chest radiographs with respect to heart failure. Nonetheless, Dr. Hospitalist-2 was eventually dropped from the case as much of the criticism was focused on Dr. Hospitalist-1 and her failure to come and evaluate Mrs. E.D. on the day of her death.
During her deposition, Dr. Hospitalist-1 testified that she had no memory regarding the chain of events; however nurse depositions supported the notion that Dr. Hospitalist-1 never saw the patient even though she had written a full page of transfer orders. So regardless of the "battle of the experts," with respect to whether the demand ischemia could really have been treated or not, the case boiled down to a hospitalist who appeared lazy and uncaring.
The case was settled for an undisclosed amount on behalf of the plaintiff.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Confusion after midnight
Story
Mr. M, a 70-year-old man with a history of coronary artery disease, diabetes, hypertension, and chronic atrial fibrillation, presented to his local hospital with a 3- to 4-day history of nausea and emesis that had become coffee-ground in description. Mr. M was on chronic Coumadin therapy, and his INR (international normalized ratio) in the emergency department was 5.78. The ED physician contacted Dr. Hospitalist for admission with a working diagnosis of gastritis and coagulopathy.
Dr. Hospitalist gave the ED verbal admission orders and awaited Mr. M’s transfer to the floor. By 11:30 p.m., Mr. M was in his hospital room. Shortly after his arrival the admission nurse heard a loud bang. When she entered the room, she found Mr. M lying flat on his back on the floor. Dr. Hospitalist was notified and she ordered a stat head CT that demonstrated small bifrontal hemorrhagic contusions, a small amount of adjacent subarachnoid hemorrhage, and a small subdural bleed along the right anterior cranial fossa.
Dr. Hospitalist examined Mr. M at 2 a.m. and noted he was confused. Dr. Hospitalist contacted the neurosurgeon on call and discussed Mr. M’s head CT result. Following this phone call, Dr. Hospitalist placed orders for activated factor VII, a transfer to the neuro-ICU, and a repeat head CT in 24 hours.
One hour later, Mr. M was still on the regular nursing floor. At 3:30 a.m., Mr. M vomited, and Dr. Hospitalist was notified. A nasogastric tube and physical restraints were ordered. At 4:30 a.m., Mr. M was transferred to the neuro-ICU. The ICU nurse documented that Mr. M was agitated, confused, irritable, and unable to focus and follow commands, and had unequal pupils, garbled speech, and a Glasgow Coma Scale (GCS) score of 12. At 5 a.m., Mr. M received activated factor VII.
By 6:30 a.m., Mr. M was drowsy, nonverbal, not following commands, had unequal pupils with minimal light response, left-sided weakness, and a GCS score of 7. Dr. Hospitalist was notified and a stat head CT was repeated. The head CT showed interval development of a large subdural hematoma over the right hemisphere with considerable left shift. At 7:30 a.m., Mr. M was examined by the neurosurgeon. At this point, Mr. M had irregular respirations, he was nonresponsive to painful stimuli, and all extremities displayed weak withdrawal effort. Mr. M was rushed to the operating room to evacuate the hematoma, but he never again regained consciousness.
Mr. M experienced progressive neurologic deterioration until his life support was withdrawn 2 days later.
Complaint
Shortly after the death of her husband, the widow contacted an attorney. The complaint alleged that both Dr. Hospitalist and the neurosurgeon carelessly failed to properly examine, monitor, and treat Mr. M’s intracranial bleed.
The complaint explained that Dr. Hospitalist essentially abandoned Mr. M, failing to ensure a timely transfer to the neuro-ICU and the administration of activated factor VII. The complaint was also critical that Dr. Hospitalist didn’t immediately reverse the coagulopathy with fresh frozen plasma (FFP) and intravenous vitamin K. Had Dr. Hospitalist and the neurosurgeon acted in accordance with the prevailing standards of care, Mr. M’s intracranial bleed would have been stabilized without permanent injury, the complaint stated.
Scientific principles
Intracerebral bleeding in an anticoagulated patient, either spontaneous or trauma-induced, is a medical emergency that requires immediate treatment. Options for correction of an elevated INR include vitamin K, FFP, prothrombin complex concentrates (PCC), and activated factor VII.
The decision to use FFP or PCC for reversal depends on the availability of PCC and the degree of prolongation of the INR. If PCC is available, it will provide the most rapid reversal. Regardless of the preparations used, it is extremely important to minimize delays in their administration, in hopes of reducing the high mortality and morbidity.
Complaint rebuttal and discussion
Dr. Hospitalist defended herself by asserting that she contacted the neurosurgeon and discussed the case and the CT findings, and she relied on his expertise from that moment forward. Dr. Hospitalist further testified that the neurosurgeon specifically told her not to give vitamin K or FFP, but to give activated factor VII instead.
Dr. Hospitalist admitted that she had never treated a case of intracerebral hemorrhage before this one and certainly had never ordered activated clotting factors on her own.
The neurosurgeon testified he had no specific memory of this case or the phone call with Dr. Hospitalist, but he does not believe he would have told Dr. Hospitalist not to give vitamin K or FFP. In fact, the neurosurgery consult note clearly documented the expectation that Mr. M receive all three reversal treatments (vitamin K, FFP, and factor VIIa). More importantly, the consult note also documented the neurosurgeon’s surprise and dismay to find Mr. M in such extremis. The neurosurgeon testified that had he been aware of Mr. M’s true neurological condition, he would have intervened promptly.
Conclusion
This case incorporates several important issues previously addressed in this column over the past year. First, hospitalists need to appreciate the significance of anticoagulation and be well versed on how to correct excessive anticoagulation with or without bleeding ("Think before reversing anticoagulants").
Second, hospitalists must communicate and document clear expectations and boundaries of responsibility when working with subspecialty consultants and surgeons ("A real pain in the neck" and "Beyond the scope").
Third, regardless of consultant and/or subspecialty expertise, hospitalists are still responsible for their own scope of practice within their training, background, and experience. Hospitalists should not blindly defer to a consultant, and conversations regarding patient plans of care should be memorialized in the patient chart ("Overreliance on subspecialty in a case of endocarditis").
Had the hospitalist in this case documented her initial conversation with the neurosurgeon with an explicit transfer of responsibility regarding the intracranial bleed, it is likely that the legal outcome would have been different. As it was, the neurosurgeon in this case was eventually dropped by the plaintiff.
Dr. Hospitalist, on the other hand, ended up settling with the widow for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
Mr. M, a 70-year-old man with a history of coronary artery disease, diabetes, hypertension, and chronic atrial fibrillation, presented to his local hospital with a 3- to 4-day history of nausea and emesis that had become coffee-ground in description. Mr. M was on chronic Coumadin therapy, and his INR (international normalized ratio) in the emergency department was 5.78. The ED physician contacted Dr. Hospitalist for admission with a working diagnosis of gastritis and coagulopathy.
Dr. Hospitalist gave the ED verbal admission orders and awaited Mr. M’s transfer to the floor. By 11:30 p.m., Mr. M was in his hospital room. Shortly after his arrival the admission nurse heard a loud bang. When she entered the room, she found Mr. M lying flat on his back on the floor. Dr. Hospitalist was notified and she ordered a stat head CT that demonstrated small bifrontal hemorrhagic contusions, a small amount of adjacent subarachnoid hemorrhage, and a small subdural bleed along the right anterior cranial fossa.
Dr. Hospitalist examined Mr. M at 2 a.m. and noted he was confused. Dr. Hospitalist contacted the neurosurgeon on call and discussed Mr. M’s head CT result. Following this phone call, Dr. Hospitalist placed orders for activated factor VII, a transfer to the neuro-ICU, and a repeat head CT in 24 hours.
One hour later, Mr. M was still on the regular nursing floor. At 3:30 a.m., Mr. M vomited, and Dr. Hospitalist was notified. A nasogastric tube and physical restraints were ordered. At 4:30 a.m., Mr. M was transferred to the neuro-ICU. The ICU nurse documented that Mr. M was agitated, confused, irritable, and unable to focus and follow commands, and had unequal pupils, garbled speech, and a Glasgow Coma Scale (GCS) score of 12. At 5 a.m., Mr. M received activated factor VII.
By 6:30 a.m., Mr. M was drowsy, nonverbal, not following commands, had unequal pupils with minimal light response, left-sided weakness, and a GCS score of 7. Dr. Hospitalist was notified and a stat head CT was repeated. The head CT showed interval development of a large subdural hematoma over the right hemisphere with considerable left shift. At 7:30 a.m., Mr. M was examined by the neurosurgeon. At this point, Mr. M had irregular respirations, he was nonresponsive to painful stimuli, and all extremities displayed weak withdrawal effort. Mr. M was rushed to the operating room to evacuate the hematoma, but he never again regained consciousness.
Mr. M experienced progressive neurologic deterioration until his life support was withdrawn 2 days later.
Complaint
Shortly after the death of her husband, the widow contacted an attorney. The complaint alleged that both Dr. Hospitalist and the neurosurgeon carelessly failed to properly examine, monitor, and treat Mr. M’s intracranial bleed.
The complaint explained that Dr. Hospitalist essentially abandoned Mr. M, failing to ensure a timely transfer to the neuro-ICU and the administration of activated factor VII. The complaint was also critical that Dr. Hospitalist didn’t immediately reverse the coagulopathy with fresh frozen plasma (FFP) and intravenous vitamin K. Had Dr. Hospitalist and the neurosurgeon acted in accordance with the prevailing standards of care, Mr. M’s intracranial bleed would have been stabilized without permanent injury, the complaint stated.
Scientific principles
Intracerebral bleeding in an anticoagulated patient, either spontaneous or trauma-induced, is a medical emergency that requires immediate treatment. Options for correction of an elevated INR include vitamin K, FFP, prothrombin complex concentrates (PCC), and activated factor VII.
The decision to use FFP or PCC for reversal depends on the availability of PCC and the degree of prolongation of the INR. If PCC is available, it will provide the most rapid reversal. Regardless of the preparations used, it is extremely important to minimize delays in their administration, in hopes of reducing the high mortality and morbidity.
Complaint rebuttal and discussion
Dr. Hospitalist defended herself by asserting that she contacted the neurosurgeon and discussed the case and the CT findings, and she relied on his expertise from that moment forward. Dr. Hospitalist further testified that the neurosurgeon specifically told her not to give vitamin K or FFP, but to give activated factor VII instead.
Dr. Hospitalist admitted that she had never treated a case of intracerebral hemorrhage before this one and certainly had never ordered activated clotting factors on her own.
The neurosurgeon testified he had no specific memory of this case or the phone call with Dr. Hospitalist, but he does not believe he would have told Dr. Hospitalist not to give vitamin K or FFP. In fact, the neurosurgery consult note clearly documented the expectation that Mr. M receive all three reversal treatments (vitamin K, FFP, and factor VIIa). More importantly, the consult note also documented the neurosurgeon’s surprise and dismay to find Mr. M in such extremis. The neurosurgeon testified that had he been aware of Mr. M’s true neurological condition, he would have intervened promptly.
Conclusion
This case incorporates several important issues previously addressed in this column over the past year. First, hospitalists need to appreciate the significance of anticoagulation and be well versed on how to correct excessive anticoagulation with or without bleeding ("Think before reversing anticoagulants").
Second, hospitalists must communicate and document clear expectations and boundaries of responsibility when working with subspecialty consultants and surgeons ("A real pain in the neck" and "Beyond the scope").
Third, regardless of consultant and/or subspecialty expertise, hospitalists are still responsible for their own scope of practice within their training, background, and experience. Hospitalists should not blindly defer to a consultant, and conversations regarding patient plans of care should be memorialized in the patient chart ("Overreliance on subspecialty in a case of endocarditis").
Had the hospitalist in this case documented her initial conversation with the neurosurgeon with an explicit transfer of responsibility regarding the intracranial bleed, it is likely that the legal outcome would have been different. As it was, the neurosurgeon in this case was eventually dropped by the plaintiff.
Dr. Hospitalist, on the other hand, ended up settling with the widow for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Story
Mr. M, a 70-year-old man with a history of coronary artery disease, diabetes, hypertension, and chronic atrial fibrillation, presented to his local hospital with a 3- to 4-day history of nausea and emesis that had become coffee-ground in description. Mr. M was on chronic Coumadin therapy, and his INR (international normalized ratio) in the emergency department was 5.78. The ED physician contacted Dr. Hospitalist for admission with a working diagnosis of gastritis and coagulopathy.
Dr. Hospitalist gave the ED verbal admission orders and awaited Mr. M’s transfer to the floor. By 11:30 p.m., Mr. M was in his hospital room. Shortly after his arrival the admission nurse heard a loud bang. When she entered the room, she found Mr. M lying flat on his back on the floor. Dr. Hospitalist was notified and she ordered a stat head CT that demonstrated small bifrontal hemorrhagic contusions, a small amount of adjacent subarachnoid hemorrhage, and a small subdural bleed along the right anterior cranial fossa.
Dr. Hospitalist examined Mr. M at 2 a.m. and noted he was confused. Dr. Hospitalist contacted the neurosurgeon on call and discussed Mr. M’s head CT result. Following this phone call, Dr. Hospitalist placed orders for activated factor VII, a transfer to the neuro-ICU, and a repeat head CT in 24 hours.
One hour later, Mr. M was still on the regular nursing floor. At 3:30 a.m., Mr. M vomited, and Dr. Hospitalist was notified. A nasogastric tube and physical restraints were ordered. At 4:30 a.m., Mr. M was transferred to the neuro-ICU. The ICU nurse documented that Mr. M was agitated, confused, irritable, and unable to focus and follow commands, and had unequal pupils, garbled speech, and a Glasgow Coma Scale (GCS) score of 12. At 5 a.m., Mr. M received activated factor VII.
By 6:30 a.m., Mr. M was drowsy, nonverbal, not following commands, had unequal pupils with minimal light response, left-sided weakness, and a GCS score of 7. Dr. Hospitalist was notified and a stat head CT was repeated. The head CT showed interval development of a large subdural hematoma over the right hemisphere with considerable left shift. At 7:30 a.m., Mr. M was examined by the neurosurgeon. At this point, Mr. M had irregular respirations, he was nonresponsive to painful stimuli, and all extremities displayed weak withdrawal effort. Mr. M was rushed to the operating room to evacuate the hematoma, but he never again regained consciousness.
Mr. M experienced progressive neurologic deterioration until his life support was withdrawn 2 days later.
Complaint
Shortly after the death of her husband, the widow contacted an attorney. The complaint alleged that both Dr. Hospitalist and the neurosurgeon carelessly failed to properly examine, monitor, and treat Mr. M’s intracranial bleed.
The complaint explained that Dr. Hospitalist essentially abandoned Mr. M, failing to ensure a timely transfer to the neuro-ICU and the administration of activated factor VII. The complaint was also critical that Dr. Hospitalist didn’t immediately reverse the coagulopathy with fresh frozen plasma (FFP) and intravenous vitamin K. Had Dr. Hospitalist and the neurosurgeon acted in accordance with the prevailing standards of care, Mr. M’s intracranial bleed would have been stabilized without permanent injury, the complaint stated.
Scientific principles
Intracerebral bleeding in an anticoagulated patient, either spontaneous or trauma-induced, is a medical emergency that requires immediate treatment. Options for correction of an elevated INR include vitamin K, FFP, prothrombin complex concentrates (PCC), and activated factor VII.
The decision to use FFP or PCC for reversal depends on the availability of PCC and the degree of prolongation of the INR. If PCC is available, it will provide the most rapid reversal. Regardless of the preparations used, it is extremely important to minimize delays in their administration, in hopes of reducing the high mortality and morbidity.
Complaint rebuttal and discussion
Dr. Hospitalist defended herself by asserting that she contacted the neurosurgeon and discussed the case and the CT findings, and she relied on his expertise from that moment forward. Dr. Hospitalist further testified that the neurosurgeon specifically told her not to give vitamin K or FFP, but to give activated factor VII instead.
Dr. Hospitalist admitted that she had never treated a case of intracerebral hemorrhage before this one and certainly had never ordered activated clotting factors on her own.
The neurosurgeon testified he had no specific memory of this case or the phone call with Dr. Hospitalist, but he does not believe he would have told Dr. Hospitalist not to give vitamin K or FFP. In fact, the neurosurgery consult note clearly documented the expectation that Mr. M receive all three reversal treatments (vitamin K, FFP, and factor VIIa). More importantly, the consult note also documented the neurosurgeon’s surprise and dismay to find Mr. M in such extremis. The neurosurgeon testified that had he been aware of Mr. M’s true neurological condition, he would have intervened promptly.
Conclusion
This case incorporates several important issues previously addressed in this column over the past year. First, hospitalists need to appreciate the significance of anticoagulation and be well versed on how to correct excessive anticoagulation with or without bleeding ("Think before reversing anticoagulants").
Second, hospitalists must communicate and document clear expectations and boundaries of responsibility when working with subspecialty consultants and surgeons ("A real pain in the neck" and "Beyond the scope").
Third, regardless of consultant and/or subspecialty expertise, hospitalists are still responsible for their own scope of practice within their training, background, and experience. Hospitalists should not blindly defer to a consultant, and conversations regarding patient plans of care should be memorialized in the patient chart ("Overreliance on subspecialty in a case of endocarditis").
Had the hospitalist in this case documented her initial conversation with the neurosurgeon with an explicit transfer of responsibility regarding the intracranial bleed, it is likely that the legal outcome would have been different. As it was, the neurosurgeon in this case was eventually dropped by the plaintiff.
Dr. Hospitalist, on the other hand, ended up settling with the widow for an undisclosed amount.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.